medicolegal autopsy
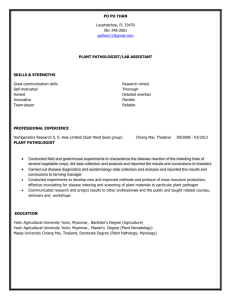
advertisement

MEDICOLEGAL AUTOPSY WILLIAM A. COX, M.D. FORENSIC PATHOLOGIST/NEUROPATHOLOGIST September 28, 2009 Forensic Pathology is the study of the physiologic processes that ultimately lead to death and the circumstances under which these processes were placed in motion. To accomplish this end it is implicit that a thorough external and internal examination of the deceased be undertaken. Prior to commencing with the examination of the deceased it is essential the forensic pathologist has an understanding of the circumstances that lead to the death, which not only includes knowledge of the medical history, but the scene in which the body was found. In regard to the latter, the forensic pathologist should speak to the investigator that went to the scene as well as review any photographs taken. Should the death have involved response of a police department, they should be spoken to. Under certain circumstances it may be necessary for the forensic pathologist doing the autopsy to have gone to the scene; this is especially true in homicides, deaths of an infant or child, or any death in which the forensic investigator and or police officer have concerns at the scene. In the death of an infant or child, a scene reenactment with use of a mannequin, either before or after the autopsy is highly encouraged. The deceased should arrive at the medical examiner or coroner’s office exactly as it was found at the scene; no clothing, jewelry, etc should have been removed from the deceased. If the deceased has an article of clothing, etc. that was utilized in bringing about their death, i.e. belt, etc. about their neck, it should remain on the body as it was found. If a gun was utilized in bringing about their death, it should not be removed until the forensic investigator and or the forensic pathologist has seen the body and has photographed the scene. The forensic pathologist prior to doing the autopsy should examine all physical evidence at the scene that was or appeared to be related to the decease death. Prior to removal of the body from the scene, the temperature of the environment should be taken and if deemed necessary that of the body. This information is very helpful in determining time of death. Upon arrival at the morgue the body should be photographed as it is before any clothing, jewelry is removed. Following taking the photographs, the clothing and jewelry should be examined as to how they are arranged on the body and their condition, i.e. stained with blood, feces, urine, gastric contents, grease, dirt, etc. noted. Pragmatically, this should be accomplished at the scene due to the fact in the removal of the body from the scene; the position of the articles of clothing and jewelry may have changed. Attention to such details as tears in the clothing, broken or lost buttons, whether the clothing is in the form of being properly worn or in a state of disarray and whether jewelry is complete and in proper position is important. All of these features should be described in the autopsy report. The clothing, jewelry and any other articles should be removed from the body, each being described and photographed with each placed in a separate plastic bag, being certain that the clothing is dry. All such bagged clothing, etc. should be placed in a large plastic bag, properly labeled and sealed. Any significant evidence on the clothing, such as tears, defects due to missiles or sharp objects should be described and photographed. If at all possible the clothing should be removed intact, without the aid of scissors or any other instrument. All defects in the clothing should be measured as to size of defect and where it is from accepted landmarks, i.e., collar, buttons etc. in inches. If projectiles are discovered in the clothing or body bag, their position should be documented, the missile photographed, and placed in an evidence envelope, then sealed and properly labeled noting name of the deceased, case number, date and time and where found in reference to the body. All pockets should be examined and their contents described and placed in a sealed plastic bag, which then is placed in a secure storage area. External Examination Following removal of the clothing the body is weighed and length is determined. If at all possible the weight of the body should be determined by scale and not estimated. If you have to estimate the weight, so state in your report. The length of the body should be given in inches. If you chose to use the metric system, give its equivalence in inches. Prior to commencing with the external examination identification of the body must be accomplished. If for whatever reason this cannot be accomplished at the moment, before the body is released from the morgue, it must be positively identified, however that is accomplished. 2 If it is apparent that death was by violent means, whether as the result of a homicide, suicide, motor vehicular accident, etc., CAT scans, MRIs, x-rays should be reviewed and or their reports. If prior to the body arriving at the morgue this was not accomplished then x-rays should be taken at the morgue. Knowing where a projectile is in the body prior to doing the autopsy is immensely helpful. If there are fractures of the extremities, etc., having a record of their site and the bones involved aids in the completion, value and thoroughness of the report. Note the general condition of the body (well developed, well nourished, appearance consistent with known age), race, color of the skin. If it is apparent that the deceased is white, however, their skin hue suggest an individual not of European ancestry, it is helpful to further clarify their ethnicity, such as American Indian, Hispanic, middle eastern, central or south Asia. The deceased hair should be described noting the color, texture, straight or curly, distribution and length in inches. The overall configuration of the head should be noted. In the normal person, the skull viewed laterally is of an oval shape, larger above than below, and wider behind than in front. In the infant note the condition of the fontanelles. The anterior fontanell (site of junction of the coronal and sagittal sutures, which is called bregma) normally closes by the age of 16 to 18 months. The junction of the sagittal and lambdoidal sutures is known as lambda, the site of the posterior fontanelle, which normally closes by the age of 1 or 2 months. Delayed closure of the fontanelles is frequently noted in hydrocephalus, congenital syphilis and cretinism. Bulging fontanelles suggest increased intracranial pressure. Sunken fontanelles are indicative of dehydration. The average circumference of the skull measured on a plane with the supraorbital ridges and the occipital protuberance is 13 inches at birth, 18 inches at one year, 20 inches at 7 years, and 22 inches in adulthood. The circumference of the skull equals that of the thorax (just below the nipples) up to the age of 2 years. Premature closure of the cranial sutures (craniostenosis) may result in a small skull (microcephaly) or an abnormally shaped skull. A large skull is characteristic of hydrocephalus. In hydrocephalus, the fontanelles are bulging, and the bones of the skull have a “cracked-pot” sound on percussion (Macewen’s sign). An increased size of the skull is also characteristic of Paget’s disease; the forehead is prominent and the face is small (“acorn” skull). In 3 acromegaly, the head and face are larger than normal, the supraorbital ridges prominent and the forehead receding. Oxycephaly or “tower skull” is a vertically elongated skull with an increased vertical diameter and markedly reduced anterior-posterior diameter; it is seen in craniostenosis. Although rare today, in congenital syphilis, the frontal and parietal eminences are also prominent and the skull, when viewed from above, appears like a cross-bun. The prominence of the frontal and parietal bones is called the natiform bossings of Parrot and is due to the deposition of subperiosteal new bone. A palpable hard tumor of any bone of the skull is suggestive of an osteoma. A metastatic carcinoma may produce nodular swellings. A common cause of focal enlargement is a hematoma. A scalp wound that is gaping indicates the aponeurosis has been lacerated. Small pumps in the occipital portion of the head may be due to enlarged lymph nodes or rheumatic nodules. Focal enlargements may also be due to epidermoid cysts, sebaceous cysts or lipomas. Softening of the skull, which is called craniotabes, is detected by pressing on the skull behind the pinna. It occurs in osteogenesis imperfecta, hydrocephalus, congenital syphilis, and hyperparathyroidism. If the hair has been dyed that should be noted. If the deceased has a mustache or any type of beard this should be described noting color and length. The hair in the axillae, on the trunk, pubic region and extremities should be noted. Absence of hair on the anterior chest of a male is called pectoral alopecia, which, although not necessarily abnormal, suggests the possibility of feminization that in turn may be related to cirrhosis or endocrinopathy. If there has been an injury to the scalp and there is suspicion of a homicide, than hairs should be plucked and retained for possible later comparison. The eyebrows should be examined noting any loss. As an example, there is a characteristic loss of hair over the outer third or more, on either side, in myxedema. Although uncommon today, in secondary syphilis, there is patchy or uneven loss of hair. When examining the eyelids note any change in color, swelling, lacerations, contusions, etc. If the eyelid’s margins appear red and swollen this is indicative of inflammation and 4 is called Blepharitis. Focal redness and swelling at the edge of the lid is referred to as a stye or hordeolum, which is due to an infection of Zeis’ glands or the sebaceous glands. A chalazion is on the inner surface of the eyelid, feels like a bead and is a granuloma of the Meibomian glands. Zanthelasma palpebrarum are single or multiple flattened yellow or orange plaques over the inner ends of the upper eyelids and less frequently over the lower eyelids. Incomplete closure of the palpebral fissures can be seen in the deceased as a normal finding. However, it can be a reflection of short eyelids (lagophthalmos), eversion of the free edge of the eyelid (ectropion), exophthalmos (due to tumor, inflammation, thyroid disease or trauma), facial paralysis or large eyeballs. Periobital ecchymosis is an important observation and is considered to be the result of a skull fracture until proven otherwise. The eyes are than described noting the clearness of the cornea, color of the irides, the presence or absence of arcus senilis, position of the pupils, and their confirmation, i.e., size, equal, round, regular. A cone-shaped projection of the cornea is characteristic of keratoconus, an idiopathic degenerative disease. A corneal opacity is called a nebula if it is faint and cloud-like; a macula, if it is denser; and leukoma, if white and opaque. The presence of corneal arcus in a young person strongly suggests a disturbance in lipid metabolism. Small gray or yellowish nodules characterize Phlyctenular keratitis over the cornea. It occurs in malnourished children who have tuberculosis and less frequently in adults who had tuberculosis in childhood. Whitish plaques are indicative of deposition of calcium in the cornea and are referred to as Band keratitis. The conjunctivae should be examined noting the presence or absence of petechiae, hemorrhage or jaundice. A faint blue tinge is common in anemia and debility. A pearly white sclera is seen in anemia. Deep blue sclera is pathognomonic of osteogenesis imperfecta. The eyeballs should be palpated to determine whether prosthesis is present. This simple examination can elevate much embarrassment in the future. The initial examination of the oral cavity should include the lips. Generalized swelling of the lips is suggestive of angioneurotic edema. Localized swelling may occur as the result of inflammation, trauma, insect bite, carcinoma or corrosive poisoning. Thick lips may be racial, artificially induced, or the result of acromegaly, myxedema or macrocheilia 5 (permanent swelling of the lips that results from greatly distended lymphatic spaces). Thinness of the lips may be racial (American Indians) or familial characteristic. The color of the lips is an important observation to note. The lips may be purple due to peripheral or central cyanosis or to methemoglobinemia. Pale lips are a sign of anemia. The oral cavity is examined for the presence or absence of teeth and if present the condition and number. The permanent teeth are thirty-two in numbers and consist of four incisors, two canines, four premolars or bicuspids, and six molars in each jaw. Teeth, which show evidence of being loose, recently dislodged by hemorrhage in the alveolar sockets, chipped or broken, should be described. Pitting of the teeth may occur as a result of excessive fluorine; a peculiar oval shape notching of the biting edges may affect the first permanent molars (mulberry molars). The teeth may be widely spaced as in acromegaly or hyperparathyroidism or commonly following extraction. Precise charting of the teeth for identification should be reserved for the Forensic Dentist or Dentist. The gums should be examined as feasible. A black line along the gingival margins when teeth are present suggests deposition of bismuth or lead sulfide. Dilantin may give rise to swollen gums. There may also be a lesion projecting from the gums or peridental structures (epulis). If it is possible observe the buccal mucous membrane. A pale brown or gray patches of pigmentation suggest adrenocortical insufficiency, however, similar pigmentation may occur as the result of heredity or heavy metal intoxication. Fordyce’s spots are small yellowish-brown slightly raised spots due to normal sebaceous glands. If the decease has dentures, they should be described as to whether they are in the maxillary and/or mandibular region and their condition. There are some cases in which the teeth are received in a separate container with the body; this should be recorded. The oral mucosa, frenula and visible tongue are than described as to the presence or absence of trauma. If the tongue or lips have evidence of a piercing that should be noted. The external auditory canals, external ears and nares should be inspected. The presence of a cauliflower ear indicates repeated blunt force injuries. Small hard nodules over the helix and antihelix suggest gouty tophi. Furuncles, sebaceous cysts, chondromata, hematomata, aneurysms, lupus and other skin diseases are all fairly common over the 6 external ear. The external ear may be discolored because of cyanosis, frostbite, hematoma, occhronosis or angiomata. Enlargement of the nose occurs commonly in myxedema, acromegaly and rhinophyma. Rhinophyma is a massive or bulbous nose with coarse pitted and flushed skin near its tip. It is commonly seen in elderly persons with acne rosacea (facial erythemia associated with pimples). Redness of the tip of the nose can be seen in infection; it can also be seen in chronic alcoholism, skin disorders, polycythemia and mitral stenosis. If there are earpiercings or piercing of the ala nasae or nasal septum they should be described. The facial bones should be palpated noting any deformities. Excessive prominence of the forehead or supra-orbital ridges may be due to acromegaly, leontiasis ossium (Hyperostosis frontalis interna or Morgagni-Stewart-Morel syndrome and may be associated with hypertrichosis and obesity; most commonly affects women near menopause), exostosis, tumors or bossing. The acromegalic has an ape-like facies with prominent lower jaw (proganathism); coarse features; large nose, lips and ears; prominent forehead and cheek bones; and widely spaced teeth. In Cushing’s syndrome, there is a “moon” face. The face is rounded in shape with excessive growth of hair (hirsutism). The mitral facies is characterized by prominence of the malar eminences and high coloring of the cheeks. A “sallow” or “muddy” complexion, owing to pallor, with a yellowish-brown cast suggests chronic debility. Icterus is commonly more apparent on the face than elsewhere. Similarly, cyanosis is quite apparent especially over the lips, cheeks and ear lobes. Increased pigmentation, brown in color, is characteristic of Addison’s disease; grayish-black or grayish-blue, of argyria; grayish-blue, of hemochromatosis; circumscribed brown patches, of chloasma; and blue ears, of ochronosis (alkaptonuric ochronosis is an autosomal recessive metabolic disorder that causes an excess of homogentisic acid resulting in adverse pigmentation, calcification, and inflammation of cartilaginous and related tissues throughout the body. It is due to incomplete metabolism of homogentisic acid, tyrosine and phenylalanine). An area of blue-gray discoloration behind the ear lobe overlying the mastoid region is suggestive of a basilar skull fracture (Battle’s sign). The neck should than be examined noting the position of the larynx and trachea, whether they are in the midline, and palpated to detect enlarged lymph nodes, thyroid or any mass 7 lesion. Attention to the presence of neck vessel distention should be noted. A yellowish patch of skin on the neck associated with a decrease in skin elasticity occurs in pseudoxanthoma elasticum. Decreased elasticity of the skin is also seen in dehydration, cachexia, and Apert’s syndrome (congenital disorder characterized by malformations of the skull, face, hands and feet), which may be associated with webbing (oblique fold of skin posteriorly extending from the neck to the shoulders, Turner’s syndrome). Examined the neck closely for scars. These often can be difficult to identify unless you pay particular attention to them. If the decease has a tracheostomy in place this should be recorded. The thorax is than examined noting its configuration, whether there is an increase in anterior-posterior diameter (emphysema); the normal chest in cross section is elliptical, the transverse diameter being greater than the anterior-posterior diameter in a ratio of 7 to 5. Note if there is evidence of curvature of the thoracic vertebral column, i.e., exaggeration of the angular curvature of the thoracic spine with the convexity directed posteriorly (kyphosis). If severe, this can give rise to crowding of the ribs anteriorly along with bulging of the sternum anteriorly giving rise to a pigeon breast appearance. Remember the trachea and mediastinum will be deviated to the same direction. Some cases will present with sharp anterior (forward) angulation of the vertebral column, which is due to the collapse of one or more vertebrae. You may see deviation of the spine to one side or the other, which is referred to as scoliosis (right sided deviation is the most common, that is the convexity of the curve is to the right). The hump that is formed is due to angles of the posteriorly rotated ribs and not the spine. Scoliosis can follow weakness or paralysis of the muscles on one side of the vertebral column. This may occur after injury or destructive disease of the vertebral bodies, shortening of one lower limb or following poliomyelitis, which is rarely seen today. Congenital scoliosis due to failure of development of a part of a vertebral body or bodies is quite rare. In both males and females the breast should be examined noting symmetry, presence of masses and scars. The degree of pigmentation of the areola should be noted. Increased pigmentation is characteristic of adrenocortical insufficiency. The normal nipple points slightly downwards and outwards. Change in direction of the axis of the nipple is a 8 frequent sign of carcinoma, the nipple pointing to the lesion. If retraction is seen, it is of importance only if recent and if such is the case it is suggestive of an underlying carcinoma. Piercing of a nipple or nipples should be noted. You may see affections of the skin of the chest such as tinea versicolor, a yellowish patch which appears rather frequently in older males in the upper mid-chest in the presence of underlying coronary artery disease. Vesicular lesions may be seen running in the distribution of nerve roots, which suggest herpes zoster. The abdomen is than examined noting the presence or absence of protuberance or retraction, hernias, abnormal veins and discoloration. The normal contour of the abdomen is gently convex from side to side and front to back. Concavity suggests emaciation or negative nitrogen balance, and increased convexity suggests increased abdominal contents such as gas, ascities, fat, or neoplastic disease. If the enlargement is confined to the upper abdomen, there may be hepatomegaly, hydrops of the gallbladder, pancreatic cyst or gastric dilatation. A bluish discoloration confined to the umbilical area is called Cullen’s sign, which in the absence of local trauma or blood dyscrasia, suggest the possibility of a ruptured ectopic pregnancy in the female or a ruptured spleen in the male or nonpregnant female; if associated with bluish discoloration extending into the flank (Turner’s sign) it suggest pancreatic necrosis with retroperitoneal or intraabdominal bleeding. If veins are noted radiating outwards from the umbilicus producing caput medusae, this is suggestive of obstruction of the portal vein. When these veins can be seen extending from the axilla to Scarpa’s femoral triangle bilaterally, this is evidence for obstruction of the vena cava. Note if there is a piercing of the umbilicus. Examination of the lower vertebral column should be accomplished looking for exaggeration of the normal hallowness (lordosis). This is indicative of postural weakness, congenital dislocation of the hips or spondylolisthesis. Lordosis, which has been described clinically due to ascities, pregnancy, or is secondary to hip joint disease with flexion, may disappear after death. In the male, the external genitalia are examined noting general development, infection, trauma, position of the testes, palpable tumors, including presence of a hernia, hydrocele, hematocele and edema of the scrotum and penis, which is often seen in severe cardiac failure or iatrogenic fluid overload. If either testis is absent, careful palpation of the 9 inguinal region may locate the undescended testis in the inguinal canal. If this is the case do not confuse this with cryptorchism; in cryptorchism, the homolateral side of the scrotum is empty and poorly developed. When examining the testes, a hard area must be regarded as a malignant tumor until proven otherwise. If the long diameter of the testis is less than 3.5 cm this should raise a suspicion of Klinefeter’s syndrome. The presence or absence of circumcision should be noted. If uncircumcised, the foreskin should be retracted to look for infection of the glans (balanitis) or tumor. If retraction is not possible owing to a tight foreskin, the term phimosis is applied. If the foreskin is retracted but cannot be extended, the term paraphimosis is used. In either event, poor hygiene with consequent infection and fibrosis is the underlying cause. Note the presence of piercings. If a fibrous plaque is noted involving the corpora cavernosa this should raise the suspicion of Peyronie’s disease. Most tumors of the penis are malignant but usually involve the glans or foreskin and rarely the shaft. In the female the entire vulva should be inspected. The vulva refers to the genital structures visible externally. It includes the mons veneris (or pubis), labia majora, labia minora, clitoris, vestibule, urinary meatus, hymen, Bartholin’s glands and vaginal orifice. The mons veneris is above the level of the pubis and is normally covered with abundant hair of fine texture. Its distribution, amount and texture should be noted. The labia major are then inspected. The labia majora extend from the mons veneris anteriorly to the perineal body posteriorly. They correspond to the scrotum of the male. Swelling or masses may be present as a result of hernia, hydrocoele, trauma (hematoma), or edema. Ulcerative lesions from malignancy or infection may also occur. The labia minora extend anteriorly to form a hood for the clitoris and posteriorly to merge with the labia majora to form the fourchette. Significant primary abnormalities of the labia minora are rare. Note the presence of piercings. The clitoris occurs at the anterior end of the labia minora; it corresponds to the male penis. Hypertrophy of the clitoris suggests androgenic excess. Ulceration suggests possibility of neoplasm. 10 The urethral meatus is located below the clitoris. The orifices of Skene’s glands with para-urethral ducts are pinpoint in size and open on each side of the lateral margins of the urethra. A caruncle is a bright red polypoid lesion at the urethral orifice. Bartholin’s glands (vulvovaginal) glands are located beneath the fascia of the lower third of the vagina, and their ducts open just lateral to the vaginal introitus at the lower pole of the labia minora. Redness and pouting of the orifices of Bartholin’s glands is indicative of inflammation, often gonorrheal. Atrophy of the external genitalia is physiologic in the postmenopausal era and results in thin, dry, shrunken skin. Subcutaneous fat is lost. Exaggeration of the normal postmenopausal atrophy may result in a condition called kraurosis (or shrunken) vulvae. The postmenopausal vulva may also show lesions called leukoplakia, which are whitish, thickened, elevated and paler than the surrounding skin. These lesions are considered to be precancerous. The anus should be inspected looking for hemorroids, foreign bodies, infection, ulcers, dilatation, funnel-shaped, contusions, lacerations and evidence of tumors. It is important that you take the time to do an anal exam for it is not unheard of to fine a packet or packets containing drugs, money, etc. in the intergluteal (natal) cleft. The upper extremities followed by the lower extremities are than examined noting their length, deformities, including palpable fractures, edema, atrophy of the musculature, digital clubbing, gangrene, joint disease, ulcers, dermatitis or vascular disease. Examination of the nails may give insight into an abnormality owing solely to local disease or may provide evidence for systemic disorders. As an example, spoon-shaped nails are characteristic of the Patterson-Brown-Kelly or Plummer-Vinson syndrome (sideropenic dysphagia which manifest as a triad of dysphagia due to esophageal webs, glossitis, and iron deficiency anemia), but more frequently are the result of congenital anomalies or trauma. Linear and petechial hemorrhages are often seen beneath the nails in subacute bacterial endocarditis. They may also occur in other diseases such as trichinosis, but most often appear after known or unknown trauma in otherwise normal persons. Color changes are most common as the result of trauma, the nail becoming black in its entirety or in any part. A grayish or purplish blue tint is seen in argyria and in methemoglobinemia. A purplish-blue tint arouses suspicion of arterial oxygen 11 unsaturation or decreased peripheral blood flow. If color changes are due to a systemic disorder, the nails of the fingers and toes should be similarly affected. The presence of cyanosis of the toenails while the fingernails are pink suggests either a patent ductus arteriosus with reversed flow, or vascular abnormality of the lower extremities (arterial inflow inadequacy or impaired venous outflow). Occasionally in cirrhosis or in conditions associated with a decrease in serum albumin, you may see a thin ribbon of erythema distally with the remainder of the distal half of the nail occupied by a band of pallor. The proximal half of the nail is erythematous. Bony growths giving rise to swelling of the interphalangeal joints (Haygarth’s nodosities), especially when associated with tapered fingers, interosseous muscle atrophy and ulnar deviation of the fingers is characteristic of rheumatoid arthritis. The skin of the fingers may be firmly adherent and difficult to pinch due to scleroderma or sclerodactylia. The fingers may be long and thin (arachnodactylia) as in Marfan’s syndrome or sicklemia. The fifth finger may be disproportionately small as in Down’s syndrome, in which it is also curved inward owing to a small middle phalanx. This finding may be associated with a simian hand, there being a single transverse crease running from the thumb to the third finger. The thenar and hypothenar eminences are somewhat rounded. Flattening of these eminences may be due to peripheral nerve lesions, amyotrophic lateral sclerosis, syringomyelia or rheumatoid arthritis. Hands and fingers should be inspected for injuries and the presence of foreign material, which may have potential evidenturary value. Such material should be removed with extreme care so as to not traumatize the finger nail bed, thus inducing artifact. Lastly, make certain all digits are accounted for; this can elevate the potential for embarrassement later on. Pes planus or flat foot may be congenital or acquired. Pes cavus or contracted foot may be congenital or acquired from high heels, poliomyelitis or other neuropathy; the longitudinal arch is abnormally high while the toes tend to be dorsiflexed at the metatarsophalangeal joints. Equinus deformity is characterized by downward pointing of the foot, calcaneus by upward pointing, varus by inversion, and valgus by eversion. Any 12 combination of these may occur in clubbed foot (talipes). Equinus deformity alone may be the result of peroneal nerve paralysis. The skin is examined as to its overall appearance, pliability and texture. Note the coloration; if the deceased is black comment on the degree of pigmentation. Vitiligo (depigmentation of patches of skin) or hyperpigmentation are common in traumatized areas of the skin in blacks. Note the presence of jaundice, which manifest itself by a diffuse lemon-yellow coloration to the skin seen first in the sclera, where its color can range from light to dark yellow. The most intense jaundice is due to complete bile duct obstruction and liver failure. Some patients with septicemia can also show slight yellow discoloration to the skin with or without scattered petechiae. The skin of the elderly often show diffuse patches of ecchymoses (patchy red to redpurple coloration) due to blood escaping into the soft tissue immediately beneath the skin due to ruptured blood vessels. They are typically seen on the forearms, anterior and posterior surface, back of hands and anterior surface of the legs. They are accompanied by poor skin turgor (this is the lack of the skin to change shape and then return to normal). It is determined by pinching the skin on the back of the hand or forearm between two fingers, so that it forms a tent, for a few seconds and then released. Skin with poor turgor remains in the tented position returning slowly to its normal position. Decreased skin turgor is a manifestation of dehydration and/or a loss in the skins normal elasticity, which is common in the elderly. There are a number of terms, which are used to describe primary lesions of the skin. A macule is a focal change in color. There is neither elevation nor depression, only a flat visible patch of color of variable size and shape. The underlying reason for the color may have been introduced externally (tattoo), or from within (erythematous eruption due to breakdown of certain drugs). It may be the result of pigmentary changes (freckle, or the light brown patch with irregular contour in polyostotic fibrous dysplasia, or with smooth borders in neurofibromatosis). It may be due to the presence of blood. Hemorrhagic lesions of the skin are called petechiae if less than 2 mm in diameter, purpura if 2 to 5 mm in diameter, ecchymosis if over 5 mm in diameter, and hematoma if the lesion is raised. A papule is a circumscribed solid elevation of the skin of normal or abnormal color varying in size from a pinpoint to a pea, or 5 mm or less in elevation. A wart is a 13 papular lesion. Lichen planus is characterized by shiny violaceous papules. A mole (nevus or birthmark) is a congenital and localized abnormality of the nature of hypertrophy or hyperplasia of some elements of the skin or subcutaneous tissue. A vascular nevus may be either capillary or port-wine stain, and if raised, cavernous. An arterial spider is so called because it is shaped like the body and legs of a spider with a central arteriole from which radiates hair-like branches for a distance of about 0.5 to 1 cm. Its background is erythematous. It is seen most commonly in areas drained by the superior vena cava and rarely occurs on the lower trunk and legs. It occurs in liver disease, occasionally in preganancy and sometimes in normal persons. Morgan’s spots (cherry angiomata, senile angiomas) are bright red in color, flat or slightly elevated and occur commonly on the front of the chest and on the abdomen. Morgan’s spots increase in size and number with age. Their significance and underlying causation is not known. A nodule is a circumscribed solid elevation of the skin and is larger than a pea, or more than 5 mm in elevation. Nodules may be seen in tuberculosis, syphilis and erythema nodosum. When nodules are larger than the size of a cherry, they are usually referred to as tumors, which typically have variability in size. Another elevated lesion is the comedo or blackhead owing to a black dot of oxidized fat at the top of a collection of sebaceous material and keratin, or a milium or whitehead containing either sebaceous or cornified material. A wheal is a circumscribed, edematous, pinkish elevation of the skin, often with irregular borders extending for variable lengths from the central lesion. Wheals are characteristic of insect bites and urticaria. A vesicle is a pinhead to pea-sized circumscribed elevation of the epidermis containing clear or opaque fluid, or it may be blood-tinged. Vesicles characterize Hepres labialis. If larger than a pea, they are called bullae or blebs (blisters). Bullous lesions occur in erythema multiforme or pemphigus. If there is evidence of edema in the dependent areas, ankles, this should be recorded. If it is bilateral at the level of the ankles this is suggestive of congestive heart failure (CHF). If it is involving one leg or foot this is diagnostic of venous thrombosis. Edema of the dorsum (back) of the hand can be a reflection of inflammation, thrombophlebitis, venous obstruction or lymphatic disease. Localized swelling of the hand may be due to tenosynovitis or a ganglion. 14 Postmortem Changes Either before commencing with the external exam or immediately thereafter three fundamental postmortem changes should be noted. The first is the determination of the state of rigor mortis. Immediately after death the musculature is relaxed or another way of expressing it is that the muscles are flaccid. This is followed shortly by generalized stiffening of the muscles, which is called rigor mortis. Rigor mortis involves both voluntary (skeletal) and involuntary (smooth) muscles and is due to physiochemical changes in muscle protein. Typically it develops first in the jaw muscles, proceeding to the neck, face and upper extremities, then the lower extremities with the ankles coming last. It disappears in the same order. It should be understood this sequence is not always constant, symmetrical or regular. The degree to which rigor develops is dependent on the decedent’s muscular development. The elderly, infants, young children or debilitated typically have poorly developed rigor. A complete discussion of rigor will be given in a subsequent article. The second postmortem change to be analyzed for is livor mortis. Livor mortis is the result of blood settling in the superficial blood vessels in the dependent parts of the body. A deceased lying on their back (supine) will show livor mortis on the back with the exception of pressure points, i.e. those parts of the body in direct contact with a surface. This is due to the fact that the superficial vessels are compressed at points of contact. These points in a supine decedent would be the occipital scalp, scapular areas, buttocks, posterior aspect of the thighs and calves, and both heels. If the decedent dies prone then the pressure points will be over the anterior aspect of the head and trunk including the forehead, nose, cheek if the head is turned to a side, chin, chest, lower abdomen and anterior thighs. The color of livor is quite variable and in dark skinned people can be difficult to see. While commonly some shade of blue, it can show a rich red hue if the body was kept in the refrigerator. A complete discussion of livor will be given in a subsequent article. Body temperature should also be noted, which is called algor mortis. The body begins to cool almost immediately after death and will continue until it reaches environmental temperature. The rapidity of which body temperature declines after death is dependent upon body temperature at the time of death, relation of body surface area to weight 15 (children, debilitated and dehydrated cool much more rapidly then well nourished adults or those who are obese), amount and kind of clothing worn at the time of death, environmental temperature and the presence of air movement and whether the deceased was in water (a body will cool much more rapidly in water than air). A complete discussion of algor mortis will be given in a subsequent article. Scars and Identifying Marks The entire surface area of the body should be inspected for surgically induced and traumatic scars, vaccination marks, amputations, congenital malformations such as club foot, harelip, cleft palate and skin lesions such as pigmented nevi, port-wine stain (naevous flammeus/vascular birthmark), salmon patch (midline nevus flammeus occurring in the glabellar region or on one upper eyelid) should be described, measured, placed on a body diagram and photographed. Failure to note a scar, birthmark, etc. can raise an unwanted query into the thoroughness of your autopsy. Tattoos These should be noted separately from scars and identifying marks. Each tattoo should be described, placed on a body diagram, and photographed. If you cannot delineate the tattoo so state, do not guess. Failure to denote a tattoo or misrepresent it can come back to haunt you in the courtroom. Evidence of Therapeutic Procedures As part of the external examination, the pathologist should document evidence of all medical procedures accomplished in the antemortem period. Prior to doing the case the pathologist should be knowledgeable as to what is in the medical records. This may necessitate speaking to the physicians involved in treatment of the patient. What is absolutely essential is the pathologist has a clear understanding of the decedents medical history before doing the case. All tubes, catheters, IVs, needle puncture sites, band-aids, gauze, surgical dressings and underlying surgical incisions should be noted. Evidence of External Injuries Should the decedent been the victim of trauma, whether that be due to blunt force, gunshot wounds, stabbing, or lacerations, the pathologist must familiarize himself with their presentation at the time first seen at the hospital and compare that to what is present at the time of his examination. On occasion, stab wounds, lacerations, gunshot wounds 16 are cut through in an effort to save the person’s life. The decedent may be an organ donor, in which the skin is taken and along with it a contusion. In such cases insist on photographs being taken before any organ donation procedures are accomplished. The pathologist also must be cognizant of iatrogenically induced antemortem injuries due to physical manipulation of the patient prior to or immediately after death, this includes evidence of blunt force trauma due to improper handling of the decedent. The above issues are not as relevant if the decedent is autopsied shortly after death, especially if he is transported directly from the scene to the morgue or if the victim was found alive, transported to a hospital, but dies before any therapeutic procedures can be accomplished. Where the problem arises is when the victim is found alive and is transported to a medical facility where treatment is affected. In this case the pathologist must differentiate between trauma incident to the assault and iatrogenically induced trauma, such as ecchymoses adjacent to surgical incisions, needle puncture sites, IVs, and rib fractures with associated intercostals hemorrhage due to external cardiac resuscitation. On a rare occasion the patient is admitted to the hospital due to blunt force trauma, gunshot wound, etc. and dies as the direct result of a medical misadventure. The pathologist should be aware of this eventuality and where appropriate place it into his report as well as on the death certificate. Should the information be learned through attendance at a hospital Quality Assurance Committee Meeting, the pathologist will be precluded from testifying as to the exact nature of the misadventure, but must advise the district attorney or prosecuting attorney as well as defense council of the misadventure, who in turn can address the issue with the hospital personnel involved in the treatment of the patient. The pathologist should focus in on evidence of acute injury, i.e. that which occurred in the immediate antemortem period. All gunshot wounds, stab wounds, incised wounds, lacerations, contusions and abrasions must be measured (preferably in inches, however, the metric system can be used as long as you give the corresponding measurement in inches), placed on a body diagram, described and photographed. If there are multiple gunshot, stab or incised wounds, they should be numbered, with the numerical designation appearing in the photographs, body diagrams and written description. The above injuries should be noted in a logical sequence, however, the pathologists should 17 make certain that all understand the numerical sequence given is for identification purposes only and do not constitute the number in which the injuries were inflicted. When describing gunshot, stab or incised wounds, and lacerations, it should be done in reference to fixed anatomical landmarks, i.e. gunshot wound (GSW) labeled #1 is located 20 inches from the top of the head and 10 inches to the left of the anterior midline within the superior aspect of the left lateral anterior abdominal region. Often it can be difficult to delineate the difference between incised wounds and lacerations. Incised wounds typically have sharp edges and generally no rim of abrasion or contusion. Lacerations typically show irregular edges and not uncommonly have abraded or contused margins. Also, the inside surface of lacerations may show connective tissue strands extending from one side of the laceration to the other (bridges). The difference between lacerations and incised wounds will be discussed in greater detail in a subsequent article. What may appear to be an insignificant abrasion or contusion must be recorded. These injuries can play a substantive role in reconstructing the circumstances immediately prior to death of the victim, i.e. abrasions or contusions of the knuckles, scratches (linear abrasions) on the back of the hands, forearms, neck etc. A representative number of tissue samples should be taken, most especially of contusions, for microscopic examination. This is done not so much for dating the contusion, but to verify that they are contusions and not nevi or birthmarks. Remember, council has the right to have another expert examine the autopsy report, photographs, etc. Even though you have 6 3 contusions and all present at the autopsy agree they are contusions, you must verify they are contusions, otherwise an opposing expert can testify to the contusions being birthmarks or nevi, and at that point it is up to the jury to decide. Remember, the prosecution must prove their case beyond reasonable doubt; the defense need only create doubt in one jurors mind. Following a description of the acute injuries the pathologist should than describe those contusions, abrasions, etc. that have the appearance of being older. The documentation procedure is the same as for the acute injuries. To aid the differentiation process between acute and older injuries an appropriate number of tissue samples should be taken for microscopic examination. 18 A technique that can prove to be very helpful in making certain you are seeing all contusions is to place the body back in the cooler after your initial exam and re-examine the body the next morning. By doing this you are giving the blood time to settle into the surrounding soft tissue of the traumatized area. This is especially useful in suspected child and elderly abuse cases. If there are many wounds present of a similar nature, i.e. contusions, abrasions, stab wounds occurring within a finite anatomical region, they can be grouped, the exact number given and the minimum to maximum variation in size and if appropriate color variations noted. Internal Examination Body Incision: A description of the type of incision used to open the body should be given. As an example, the usual Y shaped incision is accomplished, with the superior aspect of the Y extending to the lateral ramifications of the tip of the shoulder, etc. At no time should this incision pass through gunshot wounds, stab wounds or incised wounds. The description of the Y shaped incision should be followed by a description of the subcutaneous tissue and muscle. If a pneumothorax is suspected, water is placed in the trough created by reflection of the skin and underlying soft tissue of the chest laterally and the rib cage, after which the pleural cavity is punctured under the water line. Evidence of Internal Injury In a systematic fashion, following the organization of the internal organs in the autopsy protocol, all internal organs involved with traumatic injury should be described. This includes ribs and vertebrae. In those cases which involve gunshot or stab wounds it is recommended the pathologist proceed with the documentation in the same sequence as the described external injuries to preserve continuity and establish correlation. As an example, a gunshot wound of entrance is followed by a description of how it proceeded through the body, giving its path in three dimensions, describing each organ in the sequence the projectile would have involved them, finishing where the missile is found or the exit wound it produced. In essence, in cases involving missiles or stabbing the pathologist does two autopsies. The first is devoted to the organs penetrated or perforated and the second being the standard examination of the internal organs. Also, by 19 placing the description of the external and internal injuries in sequence, this aids those who read the autopsy protocol (district or prosecuting and criminal defense attorneys) to more readily comprehend the cause and effect relationship. This same line of thought applies to blunt force traumatic injuries. It is important to follow the external description of these injuries by the internal description of the stated injuries; following the same numerical sequence utilized externally. This aids greatly in understanding cause and effect. It is difficult to determine the pathway of missiles or stab wounds once the organs have been removed. It is not necessary to dictate each organ again under internal examination. Gunshot wounds and stab wounds will be described in greater detail in a subsequent article. Internal Examination As the peritoneal cavity is exposed the presence of fluid, blood or exudates should be described and the quantity recorded. If there is evidence of exudates a swab should be taken for culture before anything is done; this is taken despite the less than sterile environment of the autopsy suite. If the deceased is pregnant the pathologist should examine the large abdominal veins for air before the chest is opened and the internal mammary veins excised. The omentum should then be inspected noting its position, thickness, color and the presence of masses. If there is evidence of peritonitis it should be described. Adhesions should be noted. The position of the abdominal organs should then be ascertained. Typically cutting through the ribs adjacent to the costochondral junction opens the chest. If, however, the spinal cord is going to be examined, then the chest should be opened more laterally beginning at the level of the anterior axillary line. This gives you more room to make your electric saw cuts into the vertebral column. The pleural cavity should be examined before removing the sternum to prevent blood draining from the subclavian and jugular veins and internal mammary arteries and veins contaminating the pleural cavity fluid if it exists. If fluid is present it must be described and measured. All adhesions must be noted. Before any blood is removed from either the pleural or abdominal cavity in gunshot wound cases, care needs to be taken to make certain no missiles or fragments thereof, are inadvertently removed. 20 In those cases in which there is an allegation of an iatrogenic cause of death due to perforation or incision of an organ or failure of a graft, etc., if possible, a hematocrit and hemoglobin level should be determined of the blood in the respective cavity. Although everyone in the autopsy suite will have no issue from experience alone to realize what is in the cavity is blood, council for the defendant, will insist that it was fluid stained with blood and hence the perforation, etc of an organ was not responsible for the deceased demise. Again, as best as you can, try not to leave any room for doubt. Chest Before any of the organs are removed from the chest, their position should be noted. The pericardial cavity is inspected, first noting its external transparency and color. The pericardial sac is then opened with examination of the inside color and the consistency and amount of fluid recorded. If exudates are noted a swab should be taken; if blood is seen its quantity is recorded. Should adhesions be identified they are described and their position noted. The epicardium is then examined describing its color, transparency, degree of fat, appearance of blood vessels, presence of petechiae and ecchymosis/contusions. At this time blood samples should be taken from the right atrium/right ventricle and the iliac veins for toxicology noting where the samples are taken from. Blood cultures, if they are going to be taken should be done from the right atrium. The superior vena cava and its branches, aorta and the vessels arising from the arch should be inspected. The superior vena cava and the inferior vena cava as well as the epicardial vessels should be inspected for gas bubbles in the blood. The main pulmonary artery is opened and examined prior to removal of the heart. The heart is then removed. The visceral pleural surface of the lungs is examined noting coloration, transparency, presence of blebs or bullae (cyst), fibrosis and tumors. The esophagus should be ligated and then transected above the ligation at the level of the arch of the aorta. Following removal of the organs in the thorax the pleural surface (parietal pleura) of the ribs, intercostals spaces, thoracic spine and diaphragm are examined. Abdomen The entire gastrointestinal tract is examined noting the presence or absence of the appendix. If the appendix is not present make certain you have examined the lower right 21 abdominal quadrant for a scar; sometimes they can be difficult to see. When examining the gastrointestinal tract note its length, diameter, color, presence or absence of diverticulae or fistualae. At this point I would suggest taking samples of bile from the gallbladder and urine from the urinary bladder for toxicology. It is best to do this before removing the gastrointestinal tract, thus avoiding the possibility of lacerating either organ, most especially the latter and losing material for toxicology. Following this ligate the gastrointestinal tract at the duodenojejunal junction with a double ligature cutting between the ligatures. Then double ligate the proximal esophagus and cut between the ligatures. Remove the distal esophagus with attached stomach, duodenum and pancreas, being careful not to puncture the stomach; this is followed by removal of the gastrointestinal tract. When the rectum is incised, it should be inspected for foreign objects (packets containing drugs, money etc). At this point if an additional sample of blood is needed it can be taken from the inferior vena cava. The abdominal and pelvic viscera are than removed. Following their removal the abdominal cavity, pelvic walls, pubic rami, symphysis and lumbar vertebrae are examined. To aid this examination the iliopsoas muscles should be dissected from their attachment along the lateral surface of the vertebral bodies of T12-L4. Head The external surface of the scalp is inspected looking for any evidence of injury. A single sentence stating how the scalp is reflected should then be made, i.e. the cranial cavity is entered through a bitemporal scalp incision with reflection of the scalp anteriorly and posteriorly. The undersurface of the scalp is then examined for evidence of injury. If contusions or lacerations are seen note their number, relationship to one another, whether over the convexity, lateral, anterior, posterior, relationship to underlying plates of the calvarium (frontal, parietal, occipital, squamousal portion of the temporal or greater wing of the sphenoid bone) and whether above or below the rim of the hat line. When the calvarium is removed only an electric saw should be used; if at all possible avoid using a hammer and chisel since these may produce fractures, such as linear skull fractures extending into the middle fossae. Also, if improper autopsy technique is used two types of artifactual hemorrhage can result, one of which is intracranial. In those cases in which head injury is either noted or suspected on external examination, the head 22 should not be opened until the thorax has been opened and the heart removed. If blood is not allowed to drain from the passively congested head, damage to the dura or venous sinuses by the electric saw used to remove the calvarium can give rise to escaping of the blood into the subdural space thus simulating a subdural hemorrhage occurring before (antemortem) the victim died. Also, passive congestion of the head can involve the vessels of the scalp, thus enhancing a contusion of the scalp, which if no other cause of death is determined can give rise to a false determination of cause of death as do to blunt force trauma to the head. The second variety of postmortem hemorrhage due to improper autopsy technique has been discussed under pleural cavities. If the subclavian veins, jugular veins or internal mammary vessels are damaged as a result of removal of the sternum before the pleural cavities are inspected allowing for postmortem drainage, the blood accumulated can be attributed to antemortem injury. There is one exception to using an electric saw to remove the calvarium and that is in patients suspected of having Creutzfeldt-Jakob disease (CJD). In these cases it is recommended you use a handsaw or if you intend to use an electric saw have access to air that cannot be contaminated by the bone dust. Upon removal of the calvarium its thickness should be examined, transmission of light, presence of fractures, bullet holes, burr holes or evidence of neoplastic disease should be noted. The brain is then examined as it rest within the base of the skull, noting its symmetry, appearance of the leptomeninges (are they clear, cloudy, or opaque, is an exudates present, do they have a yellow coloration, are they thickened), appearance of the convolutions (are they flattened or are the gyri narrowed, are the sulci narrowed or widened) is there any evidence of neoplastic disease. Note the presence of epidural, subdural or subarachnoid hemorrohage. If there is evidence of hemorrhage describe its appearance (whether clotted or liquid) and quantity and whether a membrane is present. If a membrane is present, does it surround the entire clot? If a membrane is present it is important that sections be taken for microscopic examination to determine its age. The brain is gently removed from the base of the skull and weighed. Following removal the fissures are inspected. 23 The base of the brain in then examined, inspecting the circle of Wills and the main arteries, looking for atherosclerosis, thrombosis, aneurysm, and anomalies. Examine the brain for evidence of increase in intracranial pressure demonstrated by grooving of the unci, cerebellar tonsils or cingulate gyri. The cerebellum, brainstem and cranial nerves are then inspected. The pituitary is removed from the hypophyseal fossa, examined, noting its size, configuration, presence of hemorrhage, cysts, inflammation, or neoplastic disease; it is then placed in formaldehyde along with the brain for fixation. The recommended period of fixation is at least 2 weeks to 4 weeks. If the deceased brain contains a substantive quantity of subdural and or subarachnoid hemorrhage, especially at the base of the brain in the region of the circle of Willis, the quantity and location should be determined in the fresh state. If there is any adherent blood in the region of the circle of Willis or brainstem this should be gently washed away, exposing the underlying blood vessels before placing the brain in formaldehyde. If you fix the brain with blood on the surface, especially at the base of the brain, the blood will adhere to the underlying vessels precluding any attempt at examination following fixation due to the fact that when you try to remove the clotted blood from the underlying vessels they will tear. Also, blood on the brain will impair the ability of formaldehyde to fix the brain properly. If you find the formaldehyde has a pink to red color after a day or two, replace it with fresh formaldehyde. The venous sinuses are examined following which the dura is stripped from the calvarium and the base of the skull. These structures are then inspected for fractures and any other diagnostic pathology. If fractures are identified, note their length, course and whether they are depressed. Neck Organs In your dissection of the neck organs note the presence of hemorrhage in the cervical neck muscles. Examine the hyoid bones, thyroid cartilage and most especially its superior horns, cricoid, laryngeal, epiglottic and tracheal cartilages for fractures. Carefully inspect the epiglottic, laryngeal and tracheal lumens for any foreign material keeping in mind the possibility of postmortem spillage if food or gastric contents was initially seen in the oral cavity or posterior oropharynx. Examine the mucosa of the 24 epiglottis, larynx and trachea looking for evidence of edema, inflammation, ulcers, and neoplastic disease. Is there evidence of external compression? Note the size, number and location of the parathyroids. If there is no morphologic evidence of diagnostic pathology a representative gland should be placed in the stock jar. Examine the thyroid gland noting its size, shape, weight, appearance of its surface and anatomic location. When you serially section the gland record the presence of nodularity, cysts, and evidence of neoplastic disease. Even if the gland appears normal retain a section in the stock jar. In those who still have a definable thymus note its size, color, consistency, and weight. When weighing any organ, should it be recognized that the weight is less or greater than for that age group the expected range should be also given. Serially section the gland looking for any significant pathology and then place a section in the stock jar. Dissection of the Internal Organs The pathologist should then proceed with the dissection of the internal organs. This portion of the autopsy should follow a normal sequence, heart, aorta, lungs, gallbladder, liver, gastrointestinal tract, mesentery including the condition of the vessels, pancreas, spleen, adrenals, kidneys, bladder, ureters, uterus, fallopian tubes, ovaries, prostate, seminal vesicles, testes, retroperitoneum and bone marrow. If the case warrants the spinal cord should be examined in-situ and then carefully removed without stretching, thus avoiding artifactual lesions. Each individual organ should be described separately. It is not recommended the pathologist incorporate into a single sentence a generalized, superficial statement of a variety of organs. As an example, “the heart, lungs, liver, spleen, adrenal glands, pancreas, etc. are otherwise normal.” What in effect the pathologist has done is cast doubt on the thoroughness of his examination as well as making a universal judgment that all of these organs presented no evidence of significant diagnostic pathology. In effect he has precluded anyone who may read his report from reaching another conclusion based on his findings. In short the pathologist is “stacking-the-deck;” good science is never about “stacking-the-deck,” whether that be using one sentence to describe a myriad of organs or purposely destroying anatomical drawings and notes taken at the time of autopsy so that you can never be called to question regarding your 25 observations, it is about presenting well thought out scientific evidence to support the stated conclusions. When doing an autopsy a very simple precept should be kept in mind, “several months from now, when I am sitting before a judge, jury, prosecuting and defense attorney, how will my work be judged?” The description of each organ does not have to be lengthy. It should include for each organ a concise, non ambiguous, description of weight, size, configuration, surface color, consistency and the presence of pathologic changes over and above those given under “evidence of internal injuries.” When discussing size do not use metaphors, such as “the size of a golf ball, small stone, etc” or reference to nonfamiliar objects such as “a millet seed” or a “roc’s egg.” In determining size utilize the metric system in three planes, typically length, width and thickness. Generally the brain, lungs, liver and spleen are weighed and not measured. There are also other accepted indicators of size. For example, in the liver, blunting of the inferior border is an indication of an increase in size, whereas sharpness is an indication of atrophy. A tense capsule is an indication of an increase in size; laxness indicates atrophy. Configuration is anything that deviates from normal. Most organs have a delicate, smooth, glistening, transparent capsule of serosa. The pathologist should look for evidence of thickening, coarseness, or dullness. Consistency refers to the softness or firmness as determined by pressure of your finger. Cohesion is a measure of the strength within tissue that holds it together, the resistance of the tissue to cutting, pressure or pulling. An organ with reduced cohesion is friable, whereas with increase cohesion it is tough or leathery. As an example, with the normal liver you should be able to gently squeeze the thumb and forefinger together through a slice 1 to 2 cm in thickness, whereas in a cirrhotic liver the consistency will be leatherlike. Every organ’s color should be noted. The color an organ will show naturally is a reflection of the quantity of blood within its vessels. There are, however, other colors, which can be seen such as yellow to orange due to jaundice or fatty infiltration, brown due to lipofuscin or hemosiderin, pale coloration due to anemia or loss of blood and dark red due to congestion. 26 Structure refers to an organs visible architecture, e.g., cortex and medulla in the kidneys, follicles in the spleen, lobules in the liver. If these organs are involved with a disease these anatomical findings may be indistinct or greatly exaggerated. Heart The hearts configuration and weight should be noted. This is followed by a description of the color, opacity, fat distribution of the epicardial surface; origin of the coronary arteries and condition of the ostia; dissection of each coronary artery noting course, degree of involvement with atherosclerosis, occlusions; right atrial examination including condition of the endocardium, patency of foramen ovale, auricular appendage, presence of thrombi; right ventricle examination noting presence of dilation and or hypertrophy, measuring thickness of the wall, measure diameter of tricuspid valve, noting condition of leaflets, measure diameter of pulmonic valve noting condition of cusps; note diameter of pulmonary artery and presence of atherosclerosis; left atrium examination noting condition of endocardium, auricular appendage, presence of thrombi; left ventricle examination noting thickness of wall as well as that of the septum, presence of dilatation, condition of endocardium, measure diameter of mitral valve and record condition of leaflets; measure aortic valve and not condition of leaflets; examine chordae tendineae for thickness, fusion, color, presence of fibrosis; serially section myocardium noting presence or hemorrhage, necrosis and fibrosis. Aorta and its Major Branches Determine diameter, color of intima, presence of atherosclerosis, note whether ulceration or calcification is present, if an aneurysm is present note type, measure length, internal diameter, degree of obstruction to flow and evidence of dissection. In regard to the major branches (brachiocephalic, left common carotid, left subclavian, celiac trunk, superior and inferior mesenteric and common iliacs) inspect the initial 2 to 3 cm. It is not recommended that you completely dissect the common carotids unless the case warrants it. The common carotids are utilized by the funeral homes for the purpose of embalming. Vena Cava and its Major Tributaries Inspect the degree of patency; appearance of the intima; presence of neoplastic disease in wall; external compromise. 27 Pulmonary Artery and Veins Note condition of wall; the presence of emboli or thrombi, are they adherent. Cervical, Mediastinal and Hilar Lymph Node. Note their size, color, and effacement of parenchyma. Laryngotracheobronchial Tree The larynx should be opened along its posterior midline with the mucosa being visualized by pulling apart of the lateral walls breaking the ossified thyroid cartilage. The trachea and bronchi are also opened posteriorly. If you suspect aspiration or drowning it is best to do an in-situ examination (Rokitansky method) through an anterior dissection. Note the color of the mucosa, its thickness and the contents within the lumen; is there evidence of a fistula or neoplastic disease. Esophagus Note the diameter, presence of diverticulae, ulcers, fistula, varices, strictures and perforation and neoplastic disease. If there is a suspicion of varices, they can best be visualized by everting the esophagus. Lungs Weigh each lung separately; note the color of the surface, the degree of transparency of the visceral pleura, the presence of adhesions and fibrosis; note the presence of emphysematous bullae or blebs; palpate the lungs to determine the degree of consistency; is there evidence of consolidation or mass lesions? To examine the parenchyma of each lobe make an incision parallel to the long lateral axis which ends immediately before the hilum; not the color of the parenchyma, does it exude fluid with gentile palpation, is there evidence of mass lesions or embolic infarction or cyst? Liver Before the liver is removed, the hepatoduodenal ligament should be dissected, exposing the common bile duct, hepatic portal vein and the proper hepatic artery. This ligament forms the right margin of the lesser omentum and is immediately to the right of the transparent hepatogastric ligament. Following dissection of the hepatoduodenal ligament, the hepatic nodes, celiac nodes, superior pancreatic nodes and left gastric nodes should be examined noting enlargement, color and effacement. The bile duct should be opened throughout its entire length into the cystic duct and the right and left hepatic 28 ducts. The proper hepatic artery is to the left of the common bile duct and immediately superior to the hepatic portal vein. The hepatic portal vein is dissected throughout its length noting the presence of thrombosis or tumor growth; if the thrombus has been gradual in its onset it will be associated with gastric and esophageal varices, splenomegaly and possibly ascities with a small liver. Such a gradual evolution of hepatic portal vein thrombosis can be associated with cavernous enlargement of the portal vein. The hepatic lymph nodes extend into the lesser omentum along the common hepatic artery and the hepatic artery proper, together with its right and left branches, as well as the bile duct. They very in number and position, but two are fairly constant: one at the junction of the cystic and common hepatic ducts, known as the cystic node (or node of the neck of the gallbladder), the other alongside the upper part of the bile duct is sometimes called the node of the anterior border of the epiploic foramen. Remove the liver and weigh it; examine the external capsule, noting adhesions, color, transparency, and lobulations; note the sharpness of the margins. Before the liver is serially section examine the gallbladder, the description of which will follow. With serial sectioning of the liver note the color of the parenchyma, presence of fibrosis, mass lesions, cyst, and areas of infarction, note any significant changes of the intrahepatic bile ducts and blood vessels. If there is intraparenchymal hemorrhage, note where and as best as you can determine its overall size. If substantive enough, intraparenchymal hemorrhage can be the cause of death or make a significant contribution to it. Gallbladder Before removing the gallbladder its overall size and shape should be noted as well as the presence of adhesions. The gallbladder is removed from the liver prior to serial sectioning and opened into a container, which is calibrated in milliliters/cc. The quantity of the bile, its color and consistency and whether stones are present is noted. If gallstones are present, their number, color, configuration, size, and the appearance of the surface should be noted. The thickness of the wall is noted followed by the appearance of the mucosa. 29 Mesentery Examine for fat necrosis, tumors, cysts and condition of the vessels; note the condition of the lymph nodes, their size, color, effacement of parenchyma. They number between 100 and 150 and occur in three groups: close to the wall of the intestine; among the loops and primary branches of the vessels; and along the upper part of the trunk of the superior vena cava. Gastrointestinal Tract In essence you are looking for intussusceptions, volvulus, hernias, fibrous strictures, fistula, exudates on the serosal surface, gangrene, mucosal pattern, ulcers, tumors, and contents of the lumen. In examining the stomach first note its overall size, configuration, appearance of serosal surface, presents of adhesions, evidence of neoplastic growth, appearance of the arteries supplying the stomach (right and left gastric arteries, which supply the lesser curvature and the right gastroepiploic [gastro-omental], left gastroepiploic and short gastric arteries supplying the greater curvature); and appearance of lymph nodes. Inspect the gastric lymph nodes, which consist of the left gastric, right gastro-epiploic and pyloric groups. Prior to opening the stomach, the esophagus should be opened to the esophagogastric junction, at which point the stomach contents is placed in a container recording it appearance, quantity and the presence of pills and solid food. Stomach contents can prove to be most advantageous in determining time of and cause of death. The stomach is then opened along its greater curvature observing the thickness of the mucosa, presence of ulcers, neoplastic lesions and scarring. The duodenum is opened noting the appearance of the internal surface of the ampula of vater. The mucosa is inspected for ulcers, scarring, neoplastic disease and bile staining. The jejunum and ileum mucosa are examined for scarring, strictures, diverticulum, neoplastic disease, overall color of mucosa, ulceration, and Peyer’s patches. If the appendix is present note its size, configuration, presence of adhesions or inflammation and neoplastic disease. If the appendix is not present record that. The colon and rectum should be examined observing their overall size, adhesions, strictures, diverticulae, neoplastic disease, and color of wall; the mucosa is inspected for color, ulcers, neoplastic disease and strictures. 30 Pancreas Note the weight, length and width; inspect the color, shape, consistency, lobulation, amount of fat, patency of ducts, stone formation, evidence of fibrosis, acute necrosis, hemorrhage, peripancreatic fat necrosis, neoplastic disease and atrophy. If there is not evidence of gross morphologic pathology it is recommended that a tissue sample be taken from the tail for microscopic examination due to the large number of islets in this region. Spleen Examine the splenic artery noting its condition (it gives rise to the dorsal pancreatic, superior pancreatic branches, arteria pancreatica magna, caudal pancreatic, short gastric, left gastro-epiploic and terminal splenic arteries). Inspect the pancreaticosplenic lymph nodes, which accompany the splenic artery, and are related to the posterior surface and the upper border of the pancreas; one or two of this group, are in the gastrosplenic ligament. Note the weight, length, width and depth; configuration; exterior color, opacity, wrinkling and thickening of the capsule; presence of lobulation; the appearance of the splenic pulp and its consistency, visibility of the malphighian corpuscles (bodies), presence of infarcts or mass lesions; presence of accessory spleen. If you intend to take sections for immediate microscopic examination and or the stock jar make certain they are thin for proper fixation to take place. Adrenal Glands Note the weight of each and configuration; the thickness and color of the cortex and medulla; tumor masses and their size, color, consistency; presence of periadrenal and parenchymal hemorrhage. Kidneys Prior to removal, the renal arteries and veins should be located and opened noting any thrombosis, embolization and atherosclerotic plaques; examine the ostea of the arteries. The ureters are then opened throughout their length, noting patency and condition of the mucosa. The kidneys are removed and the capsules stripped; note the color, opacity and resistance to stripping; examine the subcapsular surface for scarring, pitting, cysts, tumors, abscesses, and hemorrhage; examine the cut section of the cortex recording its thickness, color, presence of scarring, neoplastic disease, infarction, hemorrhage and striations; note 31 the sharpness of the corticomedullary junction; examine the pyramids noting color, presence of neoplastic disease, hemorrhage, scarring, striations, infarction; examine the pelvis noting the condition of the mucosa, the presence of an exudates, stones, hemorrhage, neoplastic disease and dilatation; inspect the condition of the peripelvic and perirenal fat. Ureters Note congenital anomalies: agenesis, hypoplasia, duplications, diverticulum, megaloureter, retrocaval ureter, ureterocele, strictures, valves; presence of ureteritis; periureteric fibrosis; leukoplakia, malaloplakia, calculi; injuries and tumors. The upper part of the ureters drain to the lateral aortic nodes; those from the succeeding part up to the pelvis drain to the common iliac nodes; those in the pelvic part drain to the common, external and internal iliac nodes. Urinary Bladder Observe the configuration of the bladder; determine volume, color, opacity of urine; inspect the trigone noting appearance and patency of urethral orifice and ureter orifices; inspect mucosa for hemorrhage, inflammation, granularity, ulcers, neoplastic disease, trabeculation, and stones; record the thickness of the wall, measuring it if it appears abnormal. The urinary bladder drains primarily to the external iliac nodes with some drainage to the internal iliac and common iliac nodes. Retroperitoneal Space Look for the presence of neoplastic disease, hemorrhage or fibrosis. Examine the lumbar, pre-arotic and celiac lymph nodes, noting the presence of enlargement, color and effacement of parenchyma. The lumbar lymph nodes include three principle groups: pre-aortic, lateral aortic (right and left), and retro-aortic. The pre-aortic group drains the viscera supplied by the ventral branches of the aorta, i.e. the abdominal part of the GI tract and its derivatives. The lateral aortic groups drain the adrenal glands, kidneys, ureters, testes, ovaries, pelvic viscera (not that portion of the GI tract within the pelvis), which includes the fallopian tubes and the upper part of the uterus and the posterior abdominal wall. The retro-aortic group has no particular area of drainage 32 The pre-aortic lymph nodes are directly anterior to the abdominal aorta. They receive lymph from the regional, intermediary nodes associated with the subdiaphragmatic part of the GI tract, pancreas, liver and spleen. The celiac nodes lie on the front of the abdominal aorta close to the origin of the celiac artery. They are the terminal group of nodes for the stomach, duodenum, liver, gallbladder, pancreas and spleen. Prostate Determine the weight, size, consistency, lobulation, and condition of the capsule; serially section looking for nodularity (tissue pattern), inflammation (abscesses), presence of corpora amylacea, and neoplastic disease. Due to the propensity for prostatic carcinoma to arise in the posterior lobe, this is the lobe that should be sampled assuming the remainder of the gland shows no evidence of significant diagnostic pathology. The prostate drains primarily to the internal iliac and sacral nodes. There is a trunk that drains the posterior surface to the external iliac nodes Seminal Vesicles Observe the size, shape and thickness; contents color and consistency; appearance of the mucosa. The seminal vesicle drains to both the internal and external iliac nodes. Testes Their location (are they in the scrotal sac), size, configuration; appearance of cut section noting color, consistency, presence of neoplastic disease, do the tubules string-out. The lymph drainage of the testes is to the lateral aortic and pre-aortic lymph nodes. Uterus Note the size, shape (configuration), position in pelvic cavity; note the appearance of the parametrium (connective tissue separating the supravaginal part of the cervix in front from the bladder, which extends also on to the sides of the cervix, and laterally between the layers of the broad ligament), broad ligament, mesovarium and mesosalpinx; weigh with the cervix attached; dimensions across the fundus, length and myometrial thickness; length and diameter of the cervix; appearance of the cervical os and mucosa; appearance and thickness of the endometrium; if polyps are present describe and be certain to take sections for microscopic examination; appearance of the myometrium, evidence of neoplastic disease. If neoplastic disease does involve the myometrium describe and note 33 its location, whether, pedunculated, sessile, intraparencymal and take samples for microscopic examination. The upper part of the body, the fundus and the fallopian tube, and the ovary drain to the lateral aortic and pre-aortic lymph nodes, with a few draining to the external iliac nodes. The region of the connection of the fallopian tube to the uterus drains to the superficial inguinal nodes. The vessels from the lower part of the body of the uterus drain mostly to the external iliac nodes, accompanying those from the cervix. Fallopian Tubes Note is length, diameter, external surface, appearance of fimbriae, presence of adhesions, tumors, cyst, and extra-uterine pregnancy. If there is evidence of any significant diagnostic pathology representative sections should be taken for microscopic examination. Ovaries Observe the size, shape, position, adhesions; if cyst are present record their size, whether intraparenchymal or on external surface, color, appearance of inner lining, description of contents; evidence of neoplastic disease and if present the appearance of its cut surface. Should there be evidence of neoplastic disease samples of tissue should be taken for microscopic examination. Vagina Observe the condition of the mucosa. Is there evidence of a discharge, which may be creamy, foamy, mucoid, purulent (yellow or green) or bloody? Smears and cultures should be made looking specifically for one of the venereal diseases. Occasionally a foreign body is discovered, which is the underlying cause for the infection. Douches or abortifacients used in excessive strength can cause chemical vaginitis, sometimes giving rise to shedding of the entire epithelium. Hemorrhagic, granular vaginitis, most severe in the posterior fornix and associated with white discharge, is seen in trichomonas vaginitis. In those cases with a thick, white, peeling exudates Candida albicans should be considered. After the discharge is removed note the condition of the mucosa. Look for lacerations, fistulae (rectovaginal, vesicovaginal and urethrovaginal). Note the presence of tumors, cysts (Gartner’s duct cysts are the result of incomplete obliteration of the lower end of the Wolffian duct, appearing in the lower part of the anterolateral wall of the 34 vagina) and endometriosis (commonly seen in the posterior fornix and rectovaginal septum as small blue foci in contracted fibrous tissue). There are three groups of nodes, which drain the vagina. The upper vessels accompany the uterine artery to the internal and external lymph nodes. The middle is drained by vessels, which accompany the vaginal artery to the internal iliac lymph nodes. The vessels of the vagina below the hymen, those of the vulva and the skin of the perineum as a whole pass to the superficial inguinal nodes, but the clitoris and labia minora drain to the deep inguinal nodes, with the clitoris sometimes also draining to the internal iliac nodes. Pelvic Lymph Nodes Lymph vessels from the pelvis, most of the pelvic viscera, and from the lateral and anterior parts of the abdominal wall, pass first through outlying groups of lymph nodes associated largely with the internal iliac arteries and their branches. They include the common iliac, external iliac and internal iliac lymph nodes. Note their size, color and effacement of their parenchyma. Bone Marrow Note the color, consistency, fat or red. At a minimum, a tissue sample should be placed in the stock jar noting in the report where the sample was taken from. Microscopic Examination During the coarse of the autopsy tissue samples from each organ should be taken for histopathologic analysis. Those samples for immediate microscopic study should be placed in a cassette, with each cassette labeled with a number. The pathologist should record the tissue sample placed in each numbered cassette. When the microscopic slides are made from the cassettes, each tissue segment should be placed on a corresponding labeled microscopic slide. Although some will place several tissue segments from a number of different cassettes due to economic reasons, this should be avoided if possible. If you have taken several tissue samples from the lungs and place them all on the same slide with no attention given to the numbered cassettes it is difficult to determine, which lung or lobe the tissue segments came from. The number of tissue segments various according to the case. There are a number of fundamental concepts that should be kept in mind when deciding how many tissue 35 segments should be submitted for immediate microscopic analysis: confirmation of gross impressions or the presence or absence of antemortem or postmortem lesions and assistance needed in the dating of lesions resulting from blunt force trauma. There are some forensic pathologists who do not believe it is necessary to submit tissue for immediate microscopic analysis in every autopsy. As an example, a young adult male whose death is the consequence of a motor vehicular accident in which the severity of his injuries make clear the cause of death with no evidence of a natural disease process on gross examination of his organs. Other forensic pathologist disagree with the practice of not submitting at least representative tissue samples from each respective organ, i.e. heart, lung, liver, kidneys, spleen, pancreas, adrenal glands, prostate or uterus & cervix, pituitary and brain. The premise to this line of thinking is you are a pathologist first, who has subspecialized training in forensic pathology, hence in addition to determining cause and manner of death you have a responsibility to give a complete morphologic picture of the deceased at the time of their death. As an example, failure to take slides of the liver or lung would preclude a family from knowing that their father, etc. had Acute Hepatitis C or that he had minute granulomas in his lungs, which had acid fast positive bacilli. One of the truly outstanding forensic pathologists in our country, Lester Adelson, stated, “Pertinent lesions and vital organs should be examined histologically, even when the latter are grossly normal.” He went on to state, “From the forensic standpoint, a slide which contributes positive or negative data for establishing cause, manner, circumstances and other pertinent facets of a death investigated primarily for medicolegal purposes should be regarded as a permanent, objective anatomic record, available for whatever studies and consultation the examiner requires.” James T. Weston, another highly respected forensic pathologist stated, “Whether or not a microscopic examination contributes significantly to his information, an experienced pathologist always conducts such an examination in instances where he may be called upon to present evidence in a matter of civil litigation, particularly when such litigation either derives from the coexistence of natural and unnatural disease or requires testimony concerning the ultimate life span of the individual involved. It must be remembered that it is during the autopsy the pathologist has his only 36 opportunity to acquire tissue samples, whether or not he intends to do a microscopic examination, hence it is prudent to obtain these samples in as much detail as possible.” The microscopic description need only include positive findings. The pathologist should note those tissues he has examined and the exact sections he has seen the pathologic findings. Samples Submitted for Toxicologic Analysis The following samples are submitted for toxicological analysis in virtually allmedicolegal autopsies: blood, urine, bile, vitreous humor, stomach contents, liver, brain and kidney. The precise areas where blood samples should be taken have already been discussed. There are certain blood samples that should never be submitted for toxicology. Blood obtained from body cavities after evisceration should never be used as it is invariably contaminated either from urine, intestinal contents, gastric contents, lymph, pleural and abdominal fluid as well as fluid oozing from resected tissues. If upon opening the chest, and before the anterior chest plate is removed, thus transecting the internal mammary arteries and veins, and removal of the heart and lungs takes place, blood is noted in either the pleural cavity or pericardial sac, such blood can be utilized for toxicologic analysis. In some cases in which there has been substantive exsanguinating hemorrhage, this may be the only blood sample in sufficient quantity you are going to obtain. It is important that the toxicologist knows, as always, where the blood sample has been taken. The urine sample is best obtained before the autopsy is done via a suprapubic puncture or if an indwelling catheter is in place, take the urine from there. If you are unsuccessful in acquiring urine using a suprapubic puncture, before evisceration of the abdominal organs, puncture the fundus of the bladder with a needle and syringe. If no urine is obtained in this fashion, pull the bladder up and make a long incision on its anterior surface and remove whatever urine is present with a syringe. It is important to the toxicologist that if any urine is present to remove it for toxicology. Again, it is placed in a sealed tube and appropriately labeled and refrigerated. If possible remove at least 10 cc of bile by a needle and syringe. If the bile is too viscous pour it into a container, seal it and appropriately label it followed by refrigeration. Bile is an important source for opiates, which are concentrated by the liver. 37 Vitreous humor is particular useful for evaluation of electrolytes most especially sodium, chloride and calcium. It is also useful for determination of glucose, urea and creatine. Vitreous should be obtained from both eyes with a needle and syringe through puncture of the sclera near the outer canthus with a fine gauge needle and syringe. Following removal of the vitreous a like quantity of water should be reinjected into the eyeball to keep it normally inflated since removal of vitreous will cause the eyeball to shrink. If there are any stomach contents this should be retained for toxicologic analysis. This is important for not only aiding in the determination of cause of death but also time of death. The stomach contents should be obtained in a fashion that leads to the least contamination as possible. A safe way of obtaining stomach contents without the risk of contamination is to dissect the esophagus through the esophagogastric junction. Then invert the esophagogastric junction into a stainless container, measure and describe the contents, after which place contents in a calibrated plastic jar and seal with appropriate labeling. Any capsules or pills identified should be placed in a separate container, sealed and appropriately labeled. These containers should be refrigerated. The stomach should be completely opened and the mucosa described. The duodenal contents should be examined as the stomach contents. Whatever content is within the duodenum should be measured, described and placed in a separate container, which is sealed and appropriately labeled. If pills or capsules are identified they should be placed in a separate container, sealed and appropriately labeled. These containers should be refrigerated. If there is concern for heavy metal poisoning, some of the jejunal and ileial contents should be placed in a plastic container sealed and appropriately labeled. The small bowel contents and mucosa should be described. In regard to large bowel contents, most toxicology laboratories prefer not to analyze fecal material. If however, there is concern that heavy metal poisoning may be involved, it is suggested a small quantity, 50 cc/grams, be placed in a plastic container sealed and appropriately labeled for possible analysis. All intestinal specimens for toxicology should be refrigerated. 38 If there is a suspicion of poisoning, as much of the regurgitated gastric contents within the oral cavity should be collected as well as that on the face, clothing, etc. and placed in a container sealed, appropriately labeled and refrigerated for possible analysis. In regard to those deaths in which volatile, gaseous or solvents may have played a role, as soon as the chest is opened, and the pleural spaces have been examined, one lung is mobilized followed by tightly tying off the main stem bronchus. The lung is removed and placed in a nylon bag, i.e. these are the same bags that arson investigators use. The bag is sealed and appropriately labeled and taken to the toxicology lab as soon as possible. Blood that is to be analyzed for the same substances must be placed in a glass tube, which has a cap lined with aluminum or Teflon. The glass tube must be filled to the top, i.e., there can be no headspace. The specimen must be sealed, appropriately labeled and placed in a refrigerator. Typically samples of liver, kidney and brain are acquired in each case. Between 50 to 100 grams of tissue from each organ is placed in a separate container sealed, appropriately labeled and placed in a refrigerator. If there is a suspicion that the death may have been due to a lethal injection, than the injection site is identified and a circumferential skin and underlying subcutaneous tissue or muscle is removed placed in a plastic container sealed, labeled and refrigerated. In those cases in which the patient dies during the administration of anesthesia, in addition to samples described above for determination of volatile and gaseous substances it is also recommended that samples of omental or mesenteric fat be taken as well as skeletal muscle. Conclusion In this article I have presented the recommended procedures a pathologist should consider in the scene investigation and the subsequent internal and external examination of the deceased. The thoughts I have expressed were from some of the most respected forensic pathologist in this country as well as my own experience. I recognize that some forensic pathologist will view some of the recommended procedures in the external and internal exam as being excessive. I will not repeat the thoughts of Lester Adelson or James Weston as to how a medicolegal autopsy should be accomplished. I would like to 39 tell you of a personal experience I had at a major university center a few years ago. At that time I had accepted a position at a Coroner’s Office, which was located on the grounds of a university center. Shortly after my arrival the Chairman of the Pathology Department asked me if I would be willing to help with teaching the pathology residents and medical students. I welcomed the challenge. This culminated in a meeting in the Pathology Department. The meeting had no sooner started than one member voiced his thoughts on how many people at the university level viewed the quality and thoroughness of forensic autopsies. Without going into a great deal of detail, they are viewed at best, as being shallow and hardly thorough. From their viewpoint it would appear some forensic pathologist have forgotten, they are pathologist first, who have a responsibility to determine from a pathophysiologic perspective, the state of the deceased at the time of their death. This responsibility goes beyond determining the deceased died as the result of a gunshot wound to the head. What I found most interesting about this viewpoint is shortly before this meeting; one of the forensic pathologists at the coroner’s office had made the statement, “I do not care what the adrenals show if I have a gunshot wound to the head.” The question that needs to be asked, is there a foundation to their perspective? From my personal experience, even taking into account the volume of cases all of us are exposed to, especially in light of the chronic shortage of forensic pathologist, forensic investigators, deniers, secretaries, etc., I would have to say on occasion there is a foundation. In essence the statement the forensic pathologist made, “I do not care what the adrenals show…” is a reflection of an attitude that exist among some forensic pathologist and pathologist when it comes to performance of autopsies. What appears to have been forgotten and what Lester Adelson and Jim Weston were trying to point out, is our work is a reflection of how we not only view ourselves both professionally and personally, but how we wish the profession of Forensic Pathology to be viewed. 40