AH323 Syllabus - UWA Athletic Training & Sports Medicine Center
advertisement

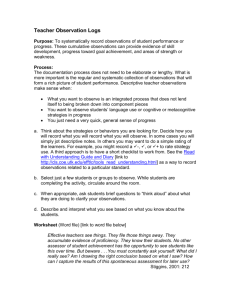
Date: August 24, 2006 Professor: R. T. Floyd, EdD, ATC, CSCS Phone: 652-3714 Off 652-6185 Hm Office: JH 219 Station #14, UWA, Livingston, AL 35470 rtf@uwa.edu Athletic Training AH 323 Evaluation of Athletic Injuries I Laboratory TEXT: Magee, David J. Orthopedic Physical Assessment. Philadelphia, PA. W.B. Saunders, 4 th edition, 2002. Booher, James M. & Gary A. Thibodeau. Athletic Injury Assessment. Dubuque, IA.: McGraw-Hill, 4th edition, 2000. Hoppenfeld, Stanley. Physical Examination of the Spine and Extremities. New York, N.Y.: Appleton-Century-Crofts, 1976. Strongly Suggested References: Hartley, Anne. Practical Joint Assessment: Lower Quadrant. St. Louis, MO.: Mosby, 2nd edition, 1995. CREDIT HOURS: 1 semester hour CO-REQUISITE: AH 322 COURSE DESCRIPTION: Assigned specific laboratory experiences in evaluation of head, cervical spine, trunk, and upper extremity injuries. Must be taken concurrently with AH 322 and serves as its laboratory. OBJECTIVES: At the conclusion of this course and AH 325, the successful student will be able to: 1. Understand how to recognize and intelligently evaluate the nature and extent of athletic injuries/illnesses. 2. Manually & skillfully examine and evaluate athletic injuries/illnesses. 3. Understand medical referral and the indications for such injuries/illnesses. 4. Understand the importance of a complete evaluation, assessment, and plan for athletic injuries/illnesses. COURSE OUTLINE: A. Physical exam of the Unconscious Athlete B. Physical exam of the Head C. Physical exam of the Face D. Physical exam of the Throat, Chest, and Abdomen E. Physical exam of the Cervical Spine F. Physical exam of the Shoulder G. Physical exam of the Elbow & Forearm H. Physical exam of the Wrist, & Hand COURSE REQUIREMENTS: A. Meet at least 2/3 of all class meetings B. Utilization of email, the World Wide Web, and Blackboard C. Appropriate dress for laboratory sessions, students not dressed appropriately will receive no credit for attendance D. Each student will participate fully in all practical laboratory sessions E. Attendance at UA/DCH & UWA Sports Medicine Lectures during the semester F. Each student is expected to observe one, perform one, teach one, and assess another class member’s performance of each procedure G. Three to six quizzes H. One to three major practical examinations EVALUATION: A. Laboratory practical examinations 60 % B. Quizzes 12.5 % C. Assessment Laboratory sheet 105 points, Due November 16, 2006, 0 points awarded if not submitted by 9:15 p.m. on this date, regardless of reason 7.5% D. Assessment Technique review 100 points, Due November 16, 2006, 0 points awarded if not submitted by 9:15 p.m. on this date, regardless of reason 7.5% E. Attendance at UA/DCH presentations & UWA Sports Medicine presentations, 5% F. Special Tests Development Project (2 at 50 points each) Due October 31 & November 30, 2006, 7.5 % POLICIES: A. Attendance: A student cannot receive credit for a course if he/she does not attend at least two-thirds of the class meetings, regardless of the reason for the absence. The attendance policy for the athletic training education program, which is more stringent than the standard UWA attendance policy, is in effect for this class and will be followed. B. Academic Misconduct: The academic misconduct policy of UWA will be followed in this course. C. Request for Accommodation: All requests for accommodation, for this course or any school event, are welcome, from students and parents. D. Discussion of Grades with Professor: Any student who receives failing grades during this course is urged to discuss this with the teacher. The University of West Alabama strives to make its programs accessible to qualified persons defined as disabled under Section 504 of the Rehabilitation Act of 1973 and the Americans with Disabilities Act. Students who have special needs that require accommodation are responsible for notifying instructors in each course in which they are enrolled and appropriate staff members, who in turn will refer the student to the ADA Compliance Coordinator. Following verification of the student’s status, the ADA Compliance Coordinator will work with the instructor or staff member in implementing an appropriate plan for accommodation of the student’s needs. Support documentation of special needs from a physician or other qualified professional will be required if deemed necessary. For more information, students should contact the Student Success Center, Foust Hall 7, (205) 652-3651 or the Office of Student Life, 311 Webb Hall, (205) 652-3581. COMPETENCIES and PROFICIENCIES: The following will be covered in part where applicable to course objectives, not necessarily as a whole. RISK MANAGEMENT AND INJURY PREVENTION Psychomotor Domain 2 - Administers static and dynamic postural evaluation procedures, including tests for muscle shortening. 3 - Implements appropriate screening procedures to identify common acquired or congenital risk factors that would predispose athletes and others engaged in physical activity to certain types of injuries. ASSESSMENT AND EVALUATION Cognitive Domain 24 - Demonstrates familiarity with the function of an ophthalmoscope in the examination of the eye. 25 - Demonstrates familiarity with the function of a stethoscope in the examination of the heart, lungs, and bowel. Psychomotor Domain 2 - Visually identifies clinical signs associated with common injuries and illnesses, such as the integrity of the skin and mucous membranes, structural deformities, edema, and discoloration. 3 - Demonstrates active, passive, and resisted range-of-motion testing of the toes, foot, ankle, knee, hip, shoulder, elbow, wrist, hand, thumb, fingers, and spine. 5 - Performs appropriate manual muscle-testing techniques and/or break tests, including application of the principles of muscle/muscle group isolation, segmental stabilization resistance/pressure, and grading, to evaluate injuries incurred by athletes and others engaged in physical activity. 6 - Administers static and dynamic postural evaluation and screening procedures, including functional tests for postural deformities and muscle length assessment. 7 - Applies appropriate stress tests for ligamentous or capsular instability based on the principles of joint positioning, segmental stabilization, and force. 8 - Measures the grade of ligamentous laxity during a joint stress test and notes the quality and quantity of the end point. 9 - Applies appropriate and commonly used special tests to evaluate athletic injuries to various anatomical areas. 10 - Demonstrates the proper use of the otoscope for ear and nasal examination, including the proper positioning of the patient and examiner and proper technique of use. 11 - Conducts auscultation of normal heart, breath, and bowel sounds, demonstrating proper position and location of stethoscope. 12 - Palpates bony and soft tissue structures to determine normal or pathological tissue(s). 13 - Performs and interprets appropriate palpation techniques and special tests of the abdomen, chest, cranium, and musculoskeletal system. 14 - Assesses the neurological function of cranial nerves, spinal nerves, and peripheral nerves and assesses the level of spinal cord involvement following injury, including the function of dermatomes, myotomes, and reflexes (e.g., deep tendon, superficial). 15 - Performs appropriate examination of injuries to the trunk and upper and lower extremities prior to an individual's return to activity. 16 - Performs an appropriate examination to evaluate the return to activity of an individual who has sustained a head injury. 17 - Uses appropriate terminology in the communication and documentation of injuries and illnesses. Affective Domain 1 - Appreciates the importance of a systematic assessment process in the management of injuries and illness. 5 - Appreciates the practical importance of thoroughness in a clinical evaluation. 7 - Values the skills and knowledge necessary to competently assess the injuries and illnesses of athletes and others involved in physical activity. ACUTE CARE OF INJURIES AND ILLNESSES Psychomotor Domain 4 - Performs a secondary survey/assessment, including obtaining a history, inspection/observation, palpation, and using special tests. 9 - Assesses a patient for possible closed-head trauma using standard neurological tests and tests for cranial nerve function. 15 - Palpates for the rigidity, guarding, and rebound tenderness of the abdomen associated with internal injury or illness. GENERAL MEDICAL CONDITIONS AND DISABILITIES Psychomotor Domain 1 - Assesses the patient for congenital or acquired abnormalities, physical disabilities, and diseases that would predispose him or her to other injury or illness, or would exacerbate the existing condition(s). 3 - Recognizes and refers individuals exhibiting a history, signs, and symptoms of cardiopulmonary conditions to the appropriate medical authority. 4 - Recognizes and manages the common disorders of the gastrointestinal tract. 9 - Uses an otoscope correctly to examine the ear and nasal passages. 11 - Uses a penlight to examine pupil responsiveness, equality, and ocular motor function. 12 - Palpates the abdominal quadrants for tenderness and rigidity. 13 - Uses the stethoscope correctly to auscultate the heart, lungs, and bowel. Affective Domain 3 - Accepts the roles of medical and allied health personnel in the referral, management, and treatment of athletes and others involved in physical activity suffering from general medical conditions. T.O. Subj area AE AE AE AE AE # 2-6-E4 2-6-F4 2-6-S4 2-6-E5 2-6-F1 AE 2-6-F5 AE AE 2-6-S5 2-6-F2A AE 2-6-E3 AE AE 2-6-E7 2-6-F3 AE AE AE AE AE 2-6-F7 2-6-F8 2-6-H10 2-6-H9 2-6-S3 AE 2-6-S7 Proficiencies Outcome use manual muscle-testing techniques of the elbow use manual muscle-testing techniques for the forearm, wrist, & hand use manual muscle-testing techniques for the shoulder administer appropriate sensory, neurological, & circulatory tests for the elbow obtain the medical history of an ill or injured athlete or other physically active individual suffering a forearm, wrist, or hand pathology administer appropriate sensory, neurological, & circulatory tests for the forearm, wrist, & hand administer appropriate sensory, neurological, & circulatory tests for the shoulder observe & identify the clinical S & S associated with the following: fracture (Colles' fracture, Bennett's fracture, carpal fracture ["boxer's fracture"], metacarpal fracture, phalanges fracture) administer active & passive range-of-motion tests using standard goniometric techniques of the elbow identify, palpate, & interpret the integrity of bony landmarks of the elbow administer active & passive range-of-motion tests using standard goniometric techniques for the forearm, wrist, & hand identify, palpate, & interpret the integrity of bony landmarks for the forearm, wrist, & hand identify, palpate, & interpret the integrity of soft tissue for the forearm, wrist, & hand identify, palpate, & assess the integrity of soft tissue of the head & face identify, palpate, & assess the integrity of bony landmarks of the head & face administer active & passive range-of-motion tests using standard goniometric techniques for the shoulder identify & palpate bony landmarks of the shoulder Taught Covered Eval. AH101 AH101 AH101 AH102 AH102 AH320-323 AH320-323 AH320-323 AH320-323 AH320-323 AH382 AH382 AH382 AH382 AH382 AH102 AH320-323 AH382 AH102 AH281 AH320-323 AH320-323 AH382 AH382 AH282 AH320-323 AH382 AH282 AH282 AH320-323 AH320-323 AH382 AH382 AH282 AH282 AH282 AH282 AH282 AH320-323 AH320-323 AH320-323 AH320-323 AH320-323 AH382 AH382 AH382 AH382 AH382 AH282 AH320-323 AH382 AE AE 2-6-S8 2-6-E2A AE 2-6-E2E AE 2-6-E2M AE AE GM GM GM 2-6-E8 2-6-F6 7-1-4A 7-1-5C 7-1-7 RM AE AE AE AE AE AE 0-2-1B 2-6-K5 2-6-T4 2-6-A4 2-6-K4 2-6-T4 2-6-A1 AE 2-6-A5 AE 2-6-K1 AE 2-6-T1 AE AE AE 2-6-T5 2-6-T5 2-5-1A AE 2-5-1B AE AE AE 2-5-1C 2-5-1D 2-5-1E AE 2-5-1F AE AE 2-5-1G 2-5-1H AE 2-5-1I AE AE AE 2-5-1J 2-5-1K 2-5-1L AE 2-6-A3 AE AE AE 2-6-A7 2-6-A8 2-6-K3 AE AE AE AE AE 2-6-K7 2-6-K8 2-6-P7 2-6-P8 2-6-T3 AE AE AE 2-6-T7 2-6-T8 2-6-A2A AE 2-6-A2E AE 2-6-A2G AE 2-6-A2K AE 2-6-A2L AE 2-6-C2A AE 2-6-K2A identify & palpate soft tissue landmarks of the shoulder. observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: symmetry observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: atrophy observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: nerve injury identify, palpate, & interpret the integrity of the soft tissue of the elbow administer functional tests & activity-specific tests for the forearm, wrist, & hand Palpate the four abdominal quadrants to assess for the following: guarding & rigidity Use a stethoscope to identify the following: normal bowel sounds Demonstrate proficiency in the use of an otoscope to examine the nose & the outer & middle ear demonstrate the ability to perform & evaluate the results of strength (repetition) testing administer appropriate sensory, neurological, & circulatory tests for the knee use manual muscle-testing techniques for the hip & pelvis use manual muscle-testing techniques for the foot, ankle, & lower leg use manual muscle-testing techniques for the knee use manual muscle-testing techniques for the thoracic & lumbar spine obtain the medical history of an ill or injured athlete or other physically active individual suffering from foot, ankle, or leg pathology administer appropriate sensory, neurological, & circulatory tests for the foot, ankle, & lower leg obtain the medical history of an ill or injured athlete or other physically active individual suffering from knee pathology obtain the medical history of an ill or injured athlete or other physically active individual of the thorax & lumbar spine administer appropriate sensory & neurological tests for the thoracic & lumbar spine administer appropriate sensory, neurological, & circulatory tests for the hip & pelvis will qualitatively assess active, passive, resistive range of motion for the following: temporomandibular joint will qualitatively assess active, passive, resistive range of motion for the following: cervical spine will qualitatively assess active, passive, resistive range of motion for the following: shoulder will qualitatively assess active, passive, resistive range of motion for the following: elbow will qualitatively assess active, passive, resistive range of motion for the following: wrist & hand will qualitatively assess active, passive, resistive range of motion for the following: thumb & fingers will qualitatively assess active, passive, resistive range of motion for the following: hip will qualitatively assess active, passive, resistive range of motion for the following: lumbar spine will qualitatively assess active, passive, resistive range of motion for the following: thoracic spine will qualitatively assess active, passive, resistive range of motion for the following: knee will qualitatively assess active, passive, resistive range of motion for the following: ankle will qualitatively assess active, passive, resistive range of motion for the following: foot & toes administer active & passive range-of-motion tests using standard goniometric techniques for the foot, ankle, & lower leg identify, palpate, & interpret the integrity of bony landmarks for the foot, ankle, & lower leg identify, palpate, & interpret the integrity of soft tissue of the foot, ankle, & lower leg administer active & passive range-of-motion tests using standard goniometric techniques for the knee identify, palpate, & interpret the integrity of bony landmarks of the knee identify, palpate, & interpret the integrity of soft tissue of the knee. identify, palpate, & interpret the integrity of bony landmarks of the hip/pelvis identify, palpate, & interpret the integrity of soft tissue of the hip & pelvis administer active & passive range-of-motion tests using standard qualitative & quantitative techniques for the thoracic & lumbar spine identify, palpate, & interpret the integrity of bony landmarks of the thoracic & lumbar spine identify, palpate, & interpret the integrity of soft tissue of the thoracic & lumbar spine observe & identify the clinical S & S associated with the following common injuries, illnesses, & predisposing conditions: overuse injuries (e.g., bursitis, exostosis, fasciitis, stress fracture, tarsal tunnel syndrome, tendonitis and/or tenosynovitis, tibial stress syndrome) observe & identify the clinical S & S associated with the following common injuries, illnesses, & predisposing conditions: dislocation or subluxation observe & identify the clinical S & S associated with the following common injuries, illnesses, & predisposing conditions: fracture observe & identify the clinical S & S associated with the following common injuries, illnesses, & predisposing conditions: sprain observe & identify the clinical S & S associated with the following common injuries, illnesses, & predisposing conditions: strain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: atrophy observe & identify the clinical S & S associated with common injuries, illnesses, & AH282 AH381 AH320-323 AH320-323 AH382 AH382 AH381 AH320-323 AH382 AH381 AH320-323 AH382 AH381 AH381 AH381 AH381 AH381 AH320-323 AH320-323 AH320-323 AH320-323 AH320-323 AH382 AH382 AH382 AH382 AH382 AH101 AH101 AH101 AH282 AH282 AH282 AH102 AH320-325 AH320-325 AH320-325 AH320-325 AH320-325 AH320-325 AH320-325 AH382 AH382 AH382 AH382 AH382 AH382 AH481 AH102 AH320-325 AH481 AH102 AH320-325 AH481 AH102 AH320-325 AH481 AH102 AH102 AH281 AH320-325 AH320-325 AH320-325 AH481 AH481 AH481 AH281 AH320-325 AH481 AH281 AH281 AH281 AH320-325 AH320-325 AH320-325 AH481 AH481 AH481 AH281 AH320-325 AH481 AH281 AH281 AH320-325 AH320-325 AH481 AH481 AH281 AH320-325 AH481 AH281 AH281 AH281 AH320-325 AH320-325 AH320-325 AH481 AH481 AH481 AH282 AH320-325 AH481 AH282 AH282 AH282 AH320-325 AH320-325 AH320-325 AH481 AH481 AH481 AH282 AH282 AH282 AH282 AH282 AH320-325 AH320-325 AH320-325 AH320-325 AH320-325 AH481 AH481 AH481 AH481 AH481 AH282 AH282 AH381 AH320-325 AH320-325 AH320-325 AH481 AH481 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AE 2-6-K2E AE 2-6-K2N AE 2-6-K2O AE 2-6-K2P AE 2-6-S2A AE 2-6-S2B AE 2-6-S2C AE 2-6-S2D AE 2-6-S2E AE 2-6-S2F AE 2-6-S2G AE 2-6-S2I AE 2-6-S2M AE 2-6-S2N AE 2-6-T2A AE 2-6-T2B AE 2-6-T2C AE 2-6-T2D AE 2-6-T2E AE 2-6-T2F AE 2-6-T2G AE 2-6-T2H AE 2-6-T2I AE 2-6-T2J AE 2-6-T2K AE 2-6-T2L AE 2-6-T2M AE 2-6-T2N AE 2-6-T2O AE 2-6-T3 AE 2-6-C1 AE 2-6-E1 AE 2-6-H1 AE 2-6-S1 AE 2-6-H11A AE 2-6-H11B AE 2-6-H11C AE 2-6-H11D predisposing conditions: bursitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: fracture observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: sprain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: strain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: tendonitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: atrophy observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: bursitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: dislocation or subluxation observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: efficiency of movement observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: fracture observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: sprain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: nerve injury observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: strain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: symmetry observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: tenosynovitis & tendonitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: café au lait macules (spots) observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: dislocation or subluxation observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: spina bifida occulta observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: facet syndrome observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: intervertebral disc pathology observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: spinal posture (kyphosis/ lordosis) observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: leg length discrepancies observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: nerve root compression observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: sacroiliac dysfunction observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: scoliosis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: vertebral pathology (e.g., spondylitis, spondylolysis, spondylolisthesis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: sprain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: stenosis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: step deformity observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: strain administer active & passive range-of-motion tests using standard goniometric techniques and/or a tape measure for the hip/pelvis obtain the medical history of an ill or injured athlete or other physically active individual suffering from a cervical spine injury obtain the medical history of an ill or injured athlete or other physically active individual suffering from elbow pathology obtain the medical history of an ill or injured athlete or other physically active individual suffering from a head injury obtain the medical history of an ill or injured athlete or other physically active individual suffering from a shoulder injury administer commonly used special tests to make a differential assessment of the following: cranial nerves (e.g., eye motion, facial muscles) administer commonly used special tests to make a differential assessment of the following: cognitive tests (e.g., recall, serial 7s, digit span) administer commonly used special tests to make a differential assessment of the following: cerebellar function (e.g., Romberg's test, finger-to-nose test, heel-toe walking, heel-to-knee standing) administer commonly used special tests to make a differential assessment of the following: AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH381 AH320-325 AH481 AH101 AH322-323 AH382 AH102 AH322-323 AH382 AH102 AH322-323 AH382 AH102 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AE 2-6-H2A AE AE 2-6-H2B 2-6-H2C AE AE AE AE AE AE AE 2-6-H2D 2-6-H2E 2-6-H2F 2-6-H2G 2-6-H2H 2-6-H2I 2-6-H3A AE AE 2-6-H3B 2-6-H3C AE 2-6-H3D AE AE AE AE 2-6-H3E 2-6-H3F 2-6-H3G 2-6-H4A AE 2-6-H4B AE AE AE AE AE AE 2-6-H4C 2-6-H4D 2-6-H5A 2-6-H5B 2-6-H5C 2-6-H6A AE 2-6-H6B AE 2-6-H6C AE 2-6-H6D AE 2-6-H6E AE 2-6-H6F AE 2-6-H6G AE 2-6-H6H AE 2-6-H6I AE 2-6-H6J AE 2-6-H6K AE AE AE AE AE AE 2-1-1A 2-1-1B 2-1-1C 2-1-2A 2-1-2B 2-6-C2H AE 2-6-C9A AE 2-6-C9B AE 2-6-C9C AE 2-6-C9C AE 2-6-E2B AE 2-6-E2C AE 2-6-E2D AE 2-6-E2F spinal nerve roots (e.g., upper quarter screen) observe & identify the clinical S & S associated with head injury: amnesia (retrograde or post-traumatic) observe & identify the clinical S & S associated with head injury: levels of consciousness observe & identify the clinical S & S associated with head injury: orientation (person, time, place orientation) observe & identify the clinical S & S associated with head injury: intracranial hematoma observe & identify the clinical S & S associated with head injury: balance & coordination observe & identify the clinical S & S associated with head injury: pupil & eye movements observe & identify the clinical S & S associated with head injury: pulse observe & identify the clinical S & S associated with head injury: blood pressure observe & identify the clinical S & S associated with head injury: facial postures observe & identify the clinical S & S associated with eye injuries & illnesses: orbital blowout fracture observe & identify the clinical S & S associated with eye injuries & illnesses: conjunctivitis observe & identify the clinical S & S associated with eye injuries & illnesses: corneal abrasion observe & identify the clinical S & S associated with eye injuries & illnesses: corneal laceration observe & identify the clinical S & S associated with eye injuries & illnesses: detached retina observe & identify the clinical S & S associated with eye injuries & illnesses: hyphema observe & identify the clinical S & S associated with eye injuries & illnesses: stye observe & identify the clinical S & S associated with an ear injury or illness: pinna hematoma ("cauliflower ear") observe & identify the clinical S & S associated with an ear injury or illness: impacted cerumen observe & identify the clinical S & S associated with an ear injury or illness: otitis externa observe & identify the clinical S & S associated with an ear injury or illness: otitis media observe & identify the clinical S & S associated with nose injury: deviated septum observe & identify the clinical S & S associated with nose injury: epistaxis observe & identify the clinical S & S associated with nose injury: nasal fracture observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: gingivitis observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: mandibular fracture observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: maxilla fracture observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: periodontitis observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: temporomandibular joint dislocation observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: temporomandibular joint dysfunction observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: tooth abscess observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: tooth extrusion observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: tooth fracture observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: tooth intrusion observe & identify the clinical S & S associated with jaw, mouth, or tooth injury or illness: tooth luxation recognize the following postural deviations & predisposing conditions: kyphosis recognize the following postural deviations & predisposing conditions: lordosis recognize the following postural deviations & predisposing conditions: scoliosis perform a postural assessment of the cervical spine & head perform a postural assessment of the shoulder observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: torticollis administer commonly used special tests to make a differential assessment of the cervical spine: nerve root compression (e.g., distraction/compression test, Spurling's test, shoulder depression test) administer commonly used special tests to make a differential assessment of the cervical spine: brachial plexus neuropathy (e.g., brachial tension test, Tinel's sign) administer commonly used special tests to make a differential assessment of the cervical spine:cervical disc herniation (e.g., Valsalva's maneuver) administer commonly used special tests to make a differential assessment of the neurovascular dysfunction (e.g., vertebral artery test) observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: carrying angle (cubital valgus & varus) observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: dislocation or subluxation observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: fracture observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: efficiency of movement AH281 AH322-323 AH382 AH281 AH281 AH322-323 AH322-323 AH382 AH382 AH281 AH281 AH281 AH281 AH281 AH281 AH281 AH322-323 AH322-323 AH322-323 AH322-323 AH322-323 AH322-323 AH322-323 AH382 AH382 AH382 AH382 AH382 AH382 AH382 AH281 AH281 AH322-323 AH322-323 AH382 AH382 AH281 AH322-323 AH382 AH281 AH281 AH281 AH281 AH322-323 AH322-323 AH322-323 AH322-323 AH382 AH382 AH382 AH382 AH281 AH322-323 AH382 AH281 AH281 AH281 AH281 AH281 AH281 AH322-323 AH322-323 AH322-323 AH322-323 AH322-323 AH322-323 AH382 AH382 AH382 AH382 AH382 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH281 AH322-323 AH382 AH381 AH381 AH381 AH381 AH381 AH381 AH322-323 AH322-323 AH322-323 AH322-323 AH322-323 AH322-323 AH382 AH382 AH382 AH382 AH382 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AE 2-6-E2G AE 2-6-E2H AE 2-6-E2I AE 2-6-E2J AE 2-6-E2K AE 2-6-E2L AE AE 2-6-E6 2-6-E9A AE 2-6-E9B AE 2-6-E9C AE AE 2-6-F2B 2-6-F2C AE 2-6-F2D AE 2-6-F2E AE 2-6-F9A AE 2-6-F9B AE 2-6-F9C AE AE 2-6-H8 2-6-S2H AE 2-6-S2J AE 2-6-S2K AE 2-6-S2L AE AE 2-6-S6 2-6-S9A AE 2-6-S9B AE 2-6-S9C AE 2-6-S9D AE 2-6-S9E AE 2-6-H7 AE 2-6-P1 RM AE 0-2-1A 2-6-C2B AE 2-6-C2C AE 2-6-C2D AE 2-6-C2E AE 2-6-C2F AE 2-6-C2G AE 2-6-T2A observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: bursitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: epicondylitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: tenosynovitis & tendonitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: osteochondritis dissecans observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: sprain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: strain administer functional tests & activity-specific tests for the elbow administer commonly used special tests to make a differential assessment of the following: joint instability (e.g., valgus stress test, varus stress test) administer commonly used special tests to make a differential assessment of the following: inflammatory conditions (e.g., tests for lateral epicondylitis, tests for medial epicondylitis) administer commonly used special tests to make a differential assessment of the following: neuropathy (e.g., Tinel's sign, pronator teres syndrome, pinch grip test) observe & identify the clinical S & S associated with the following: dislocation or subluxation observe & identify the clinical S & S associated with the following: disease states (e.g., clubbed nails, spoon-shaped nails) observe & identify the clinical S & S associated with the following: soft tissue pathology (e.g., sprain, flexor tendon avulsion [jersey finger sign], extensor tendon avulsion [mallet finger], extensor tendon rupture [boutonniere deformity], volar plate rupture [pseudoboutonniere deformity], Dupuytren's contracture, ganglion, swan neck deformity, trigger finger) observe & identify the clinical S & S associated with the following: neurovascular involvement (e.g., carpal tunnel syndrome, bishop's or benediction deformity, ape hand, claw fingers, drop-wrist deformity, Volkmann's contracture) administer commonly used special tests to make a differential assessment of the following: inflammatory conditions (e.g., Finkelstein test) administer commonly used special tests to make a differential assessment of the following: joint instability (e.g., valgus stress test, varus stress test, glide tests) administer commonly used special tests to make a differential assessment of the following: neurovascular pathology (e.g., Tinel's sign, Phalen’s test) administer functional tests & activity-specific tests for head & face injuries. observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: positioning (Sprengel's deformity) observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: scapulohumeral rhythm observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: scapular winging observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: step deformity administer functional tests & activity-specific tests for the shoulder administer commonly used special tests to make a differential assessment of the following: glenohumeral instability (e.g., anterior drawer test, posterior drawer test, relocation test, apprehension test, clunk test, sulcus sign) administer commonly used special tests to make a differential assessment of the following: acromioclavicular instability (e.g., shear test, compression test) administer commonly used special tests to make a differential assessment of the following: rotator cuff impingement/inflammation (e.g., Speed's test, drop arm test, empty can test, impingement test, Hawkins-Kennedy impingement test, Neer impingement test, pectoralis major contracture test) administer commonly used special tests to make a differential assessment of the following: biceps & biceps tendon pathology (e.g., Yergason's test, Ludington's test) administer commonly used special tests to make a differential assessment of the following: thoracic outlet syndrome (e.g., Adson's maneuver, Allen test, military brace position) administer appropriate sensory, neurological, & circulatory tests for the head & face AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH381 AH322-323 AH322-323 AH382 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH381 AH322-323 AH322-323 AH382 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH381 AH322-323 AH322-323 AH382 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH381 AH322-323 AH322-323 AH382 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH322-323 AH382 AH381 AH382 obtain the medical history of an ill or injured athlete or other physically active individual for hip/pelvis pathology demonstrate the ability to perform & evaluate the results of flexibility tests observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: dislocation or subluxation observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: vertebral fracture observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: head & neck posture observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: intervertebral disc herniation observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: nerve root compression or stretch observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: ischemia observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: leg length discrepancies AH102 AH322-323, PE250 AH322-325 AH381 AH381 AH322-325 AH322-325 AH481 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH481 AE 2-6-T2E AE 2-6-T2G AE 2-6-T2H AE 2-6-T2I AE 2-6-T2L AE 2-6-T2O AE 2-6-T2P AE 2-6-T2Q AE 2-6-T2R AE AE 2-6-T6 2-6-T9A AE 2-6-T9B AE 2-6-T9C AE 2-6-T9D observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: apophysitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: dislocation or subluxation observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: fracture observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: stress fracture observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: bursitis observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: contusion observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: sprain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: strain observe & identify the clinical S & S associated with common injuries, illnesses, & predisposing conditions: tendonitis administer functional tests & activity-specific tests for the thoracic & lumbar spine administer commonly used special tests to make a differential assessment of the following: intervertebral disc herniation (e.g., Valsalva's maneuver) administer commonly used special tests to make a differential assessment of the following: neuropathy (e.g., straight leg raise test, well straight leg test, Babinski's reflex test, Oppenheim's gait test, Kernig's sign, Brudzinski sign test, bowstring test, Hoover sign test) administer commonly used special tests to make a differential assessment of the following: vertebral defects (e.g., stork standing test/spondylolisthesis test) administer commonly used special tests to make a differential assessment of the following: joint instability (e.g., spring test) AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH381 AH322-325 AH322-325 AH481 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 AH381 AH322-325 AH481 CALENDAR: This calendar is designed to be only a guideline of planned topics which may be changed based on time needed to adequately address each topic. Tues. Thur. 8/22 Physical exam of the Unconscious Athlete 8/24 Physical exam of the Unconscious Athlete 8/30 Physical exam of the Head 8/31 Physical exam of the Head 9/5 Physical exam of the Face 9/7 Physical exam of the Face 9/12 Physical exam of the Throat, Chest, Abdomen & Pelvis 9/14 Physical exam of the Throat, Chest, Abdomen & Pelvis 9/19 Physical exam of the Throat, Chest, Abdomen & Pelvis 9/21 Physical exam of the Throat, Chest, Abdomen & Pelvis 9/26 Physical exam of the Cervical Spine 9/28 Physical exam of the Cervical Spine 10/3 Physical exam of the Cervical Spine 10/5 Physical exam of the Cervical Spine 10/10 Review of 1st half of semester 10/12 Physical exam of the Shoulder 10/17 Physical exam of the Shoulder 10/19 Physical exam of the Shoulder 10/24 Assessment Day 10/26 Physical exam of the Shoulder 10/31 11/2 Physical exam of the Shoulder Physical exam of the Shoulder - Special Test Project due 11/7 Physical exam of the Elbow & Forearm 11/9 Physical exam of the Elbow & Forearm 11/14 Physical exam of the Elbow & Forearm 11/16 Physical exam of the Elbow & Forearm Lab/Tech. Review due 11/21 Thanksgiving Holiday 11/23 Thanksgiving Holiday 11/28 Physical exam of the Wrist, & Hand 11/30 Physical exam of the Wrist, & Hand - Special Test Project due 12/5 Physical exam of the Wrist, & Hand 12/7 Physical exam of the Wrist, & Hand 12/8 Begin Final Examinations (Oral Practicals) Friday