Biological terrorism: Are you prepared?
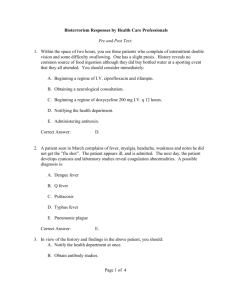
advertisement

February 2006 Biological terrorism: Are you prepared? by Susan Cantrell, ELS It’s no longer a matter of if, but when, the United States will be the victim of biological terrorism. It’s already happened; we have reason to believe it will escalate. Is your facility prepared? A study by the Centers for Disease Control and Prevention (CDC) examined 1,099 outbreaks from 1988 to 1999 with bioterrorism potential; in 6 of the events, it was considered there was intentional use of infectious agents, either bioterrorism or intentional contamination; another 41 events were considered suspect.1 Perhaps the most frightening, indeed shocking, part of these findings is that "For 6 outbreaks in which bioterrorism or intentional contamination was possible, reporting was delayed for up to 26 days." No wonder the report concluded, "In the future, shortening the time from detecting to reporting an outbreak to public health authorities, including CDC, will be essential to an effective response."1 In another report, the CDC tells us, "the consequences of being unprepared could be devastating. . . . Terrorist incidents in the United States and elsewhere involving bacterial pathogens . . . have demonstrated that the United States is vulnerable . . . Recipes for preparing ‘homemade’ agents are readily available, and reports of arsenals of military bioweapons raise the possibility that terrorists might have access to highly dangerous agents, which have been engineered for mass dissemination as small-particle aerosols. . . . Responding to large-scale outbreaks caused by these agents will require the rapid mobilization of public health workers, emergency responders, and private health-care providers. Large-scale outbreaks will also require rapid procurement and distribution of large quantities of drugs and vaccines, which must be available quickly."2 The CDC maintains a national pharmaceutical stockpile to ensure availability of drugs, devices, and equipment that might be needed to respond to a bioterrorism attack.2 Quick access to large quantities of drugs and medical equipment is something that others are prepared to help with, too. Gina Pugliese, RN, MS, vice president, Premier Safety Institute, Oakbrook, IL, said, "At the time of a disaster, such as a bioterrorism event or a hurricane, as a healthcare alliance offering group-purchasing and supply-chain services, Premier is able to assist our members with the location and identification of key materials, supplies, medications, etc., to supplement the needed inventories." Novation, LLC, also a supply-chain service, can provide help to their members, too. Larry Dooley, vice president, contract and program services, told Heathcare Purchasing News: "Novation has a disaster-operations team that can address all types of natural and manmade disasters. This team helps members meet their supply-chain needs during the time leading up to, during, and after a disaster. Regarding bioterrorism, the only thing you can do is work with members on preparedness, so the disaster operations team is formulating the list of necessary supplies to address the bioterrorism threats that we know exist today and is educating members on these topics. The good news is that most of the members served by Novation are already dealing with this and are prepared to deal with this type of tragedy, based on their own community profiles." What are goals, who should be involved? "Hospitals should have a team that represents a crosssection of their operational and clinical departments," said Dooley. "This team should lead planning and implementation efforts, if necessary; so, the people serving on the team should be senior-level executives who would command respect during a crisis." Pugliese told HPN that clinical staff, as well as key supervisory staff who know "operations" thoroughly should be involved in developing a bioterrorism preparedness plan, but also involved should be "senior leadership responsible for, or having oversight for, both safety and infection control functions. Supervisors involved in supply chain are essential for planning supplies of all types and backup sources, including specific supplies needed for controlling potential biological agents. In early planning, there need to be liaisons with the local health agency and local emergency planning committee." Judene Bartley, MS, MPH, CIC, clincal/safety consultant with Premier Safety Institute, commented on goals for being prepared for bioterrorism: "The initial goal in preparation should include completion of a Hazard Vulnerability Assessment, considering specific needs of that organization or community, specifically addressing potential vulnerability to bioterrorism agents. This would also include feasibility to respond to influx of patients that would need special handling (for example, isolation) and overall surge-capacity issues. The next step would be development of an "all-hazard plan," so that special needs involving biological agents would be addressed effectively, along with other hazards such as chemical. This includes patient, worker, and occupant protection, as well as specific supply needs (for example, masks, gloves). Also, presuming the plan is some variation of HEICS (Hospital Emergency Incident Command System), another key goal would be to test and retest the organization’s readiness to ensure each member knows his or her role and response. Given typical workplace turnover, these plans have to be tested periodically for effectiveness, not just to meet requirements of a regulatory or accrediting agency like JCAHO." Ashok Chetty, marketing manager, DuPont Personal Protection, Emergency Response/Government Markets, Richmond, VA, also emphasized the importance of conducting drills: "In DuPont’s view, an effective preparedness plan has to ensure that response personnel have adequate and frequent training under a variety of simulated disaster situations. It is important that these simulations incorporate all the critical players and systems by including the hospital personnel, the public health system, the response equipment, and other related emergency management agencies." Dooley commented on the need for security to protect staff, patients, and visitors from harm in such a volatile situation and the need to support facility staff and their families: "Each healthcare organization, based on their community, might have slightly different goals, but all members should have goals that ensure a quick and sufficient response to the crisis at hand. This should include clinical as well as operationalresponse objectives, such as staffing for the event and securing the perimeter of the hospital. Additionally, the member’s goals should also include sufficient planning and preparation to meet staff members’ personal needs. VHA and Novation have been involved in helping member hospitals recover from hurricanes for more than a decade, and the first step we usually take, besides ensuring that supplies are getting to the hospitals, is making sure that hospitals can take care of their employees, so that the employees are not distracted from their duties." What are we preparing to face? For what, exactly, does your facility need to prepare? Bioterrorism is no nebulous boogeyman; it presents real threats in the form of bacteria, viruses, and poisons. The CDC explained: "Bioterrorism is the intentional use of microorganisms or toxins derived from living organisms to cause death or disease in humans, animals, or plants on which we depend."1 The CDC developed three categories of organisms, categorized A, B, and C, by priority in which they "pose a risk to national security because they can be easily disseminated or transmitted person-to-person; cause high mortality, with potential for major public health impact; might cause public panic and social disruption; and require special action for public health preparedness."2 The A-list includes these agents: • variola major (smallpox) • Bacillus anthracis (anthrax) • Yersinia pestis (plague) • Clostridium botulinum (botulism) • Francisella tularensis (tularemia; also known as rabbit fever) • filoviruses: Ebola and Marburg hemorrhagic fevers • arenaviruses: Lassa fever, Argentine hemorrhagic fever, and related viruses. Even one case of illness or death caused by any of these organisms should alert healthcare workers to the possibility of intentional exposure to unsuspecting victims or accidental exposure to the perpetrator.1 The trick is in identifying these infections, since they’re not something seen by healthcare workers every day. Logical Images Inc., has developed software in its VisualDx program, for everyday use that could have added value in the event of bioterrorism. "Conditions caused by agents of bioterrorism are rare," observed Art Papier, MD, chief scientific officer. "Many clinicians have not seen a case and may not think to include it as a possibility. During the anthrax attacks of 2001, the Wall Street Journal (November 27, 2001) reported that patients lived or died depending on whether the doctor diagnosing them considered anthrax as a possibility. Providing healthcare professionals with the information tools to support diagnosis and management is key. With a system like VisualDx, which doctors use every day for more common diagnostic problems, the physician is reminded to consider bioterrorism when it’s clinically appropriate. In addition, they have rapid access to clinical information and photographs (10,000 images covering 600 diseases) of all the look-alike conditions to help them quickly and effectively rule bioterrorism in or out. A randomized, controlled university study showed that, in comparison to textbooks and medical atlases, VisualDx improved primary care and emergency physicians’ diagnostic accuracy by 124%.3" More recently, the system included images from Katrina victims with Vibrio Vulnificus, a gram negative rod infection that had been diagnosed in Katrina flood water exposed patients. The system provided diagnostic assistance for the potentially lethal infection as well as the instructions for immediate administering of antibiotic therapy. Importance of early detection While it’s possible that a bioterrorism event could be announced publicly, the CDC’s strategic-plan document points out that "attacks with biological agents are more likely to be covert."2 This means that the attack may not have an immediate impact because of the delay between exposure and onset of illness, with the pathogens or toxins in the meantime freely doing their dirty work in the dark, so to speak. Persons initially infected in a mass attack could unknowingly spread disease that could lead to a deadly epidemic, with public panic following close at its heels. Bioterrorists count on the ensuing psychological terror to cause panic and to demoralize the public, perhaps sowing seeds of distrust in efforts to respond to the situation, which has the potential to hamper containment and control of the disease.4,5 In the meantime, the biological agent has its way. With airplanes and worldwide travel, there is the potential for its tentacles to reach far and wide, undetected, within hours. The CDC noted: "Only a short window of opportunity will exist between the time the first cases are identified and a second wave of the population becomes ill. During that brief period, public health officials will need to determine that an attack has occurred, identify the organism, and prevent more casualties through prevention strategies . . . As person-toperson contact continues, successive waves of transmission could carry infection to other worldwide localities."2 Early detection of a biological terrorist attack is crucial, so the need for those on the front line to be alert and discerning cannot be overstated, because they are the ones in the best position to detect and report suspicious illnesses. "The earlier the accurate detection of a bioterrorism-agent release, the more likely the extent of the attack can be minimized," observed Papier. The CDC "confirmed that the most critical component for bioterrorism outbreak detection and reporting is the frontline healthcare profession and the local health departments. Bioterrorism preparedness should emphasize education and support of this frontline as well as methods to shorten the time between outbreak and reporting." 1 An automated surveillance system in place at a healthcare facility can be useful in early detection, which could shorten the time between outbreak and reporting. "Automated systems that help hospitals monitor and track hospitalacquired infections can also play a critical role in bioterrorism preparedness," says Dan Peterson, MD, MPH, president and CEO of Cereplex Inc, Germantown, MD. "Systems such as those from Cereplex, which can track both inpatient and outpatient data, including emergency department visits, and monitor laboratory and pharmacy data, can detect patterns that are significantly more specific than typically syndromic surveillance measures. For instance, our hospitals can set up an alert that captures and counts patients who show up at the emergency department (indicator of acute onset); are admitted to the ICU; have blood, urine, and sputum cultures done; and are started on broad-spectrum antibiotics (as indicators of clinical uncertainty of cause of illness). Such an approach substantially reduces the noise otherwise associated with syndromic surveillance. Most importantly, because such automated surveillance systems run entirely with data already gathered in hospital information systems, no manual data entry is required." A veteran of 8 years at CDC, Dr. Peterson concluded that "Using automated surveillance systems for hospital infections to monitor for bioterrorism events is a clear example of exactly the kind of dual-use systems that CDC is advocating." Where to start? A good place to start preparing your facility for bioterrorism is by educating yourself with advice and recommendations developed by organizations such as the CDC; Association for Professionals in Infection Control and Epidemiology, Inc (APIC); American Hospital Association; Joint Commission on Accreditation of Healthcare Organizations (JCAHO); U.S. Department of Homeland Security; Agency for Healthcare Research and Quality, Department of Health and Human Services; Institute of Medicine; National Institute of Allergy and Infectious Diseases; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America; the Occupational Safety and Health Administration; and the Federal Emergency Management Agency, among others. All of these organizations have web sites chock full of good advice on how healthcare facilities can prepare for bioterrorism, and some offer tools to help achieve it. Some schools such as University of North Carolina at Chapel Hill; Johns Hopkins; Washington University at St. Louis, Missouri; and Detroit Medical Center at Wayne State University also have excellent resources. APIC even has a template for healthcare facilities to "guide the development of practical and realistic response plans for their institutions in preparation for a real or suspected bioterrorism attack."5 The document strongly urges that response plans "should be prepared in partnership with local, state, and regional resources including health departments, emergency management, and first responders." Assessing your facilities, according to the document, is the first step, and a mass-casualty disaster-plan check list is included. The document also contains helpful information including but not limited to FBI Field Offices contact information, a telephone directory of state and territorial public health directors, and a list of web sites relevant to bioterrorism preparedness. Aside from regulatory and advisory agencies, others are in a position to help in preparing for bioterrorism. Education is the answer, and the Premier alliance is one organization that is supplying information and materials. Pugliese explained: "Premier Safety Institute addresses that need by developing materials that clarify risk and provide easy access to sample protocols, tools, assessments, educational and training programs, product lists, and suppliers from a variety of sources that can be used for all stages of planning for a bioterrorism event." DuPont, which makes personal protective equipment for use in emergencies such as a bioterrorism attack also offers help. Chetty said: "DuPont has a network of technical support personnel who can help healthcare providers with the proper selection and use of protective apparel. In addition, we have a variety of tools including technical information bulletins, videos, and presentations that can be used to train personnel on the use of protective apparel." It’s frightening to realize that we have a genuine need for protective apparel against a bioterrorism attack. We are fortunate that those tangibles are readily available. Another component necessary to the fight against bioterrorism is not so tangible but perhaps even more important. Pugliese put it well: "Communication, communication, communication! The more the public or healthcare communities understand the more realistic their preparations will be, versus a sense of panic or helplessness." HPN REFERENCES 1.Ashford DA, Kaiser RM, Bales ME, Shutt K, Patrawalla A, McShan A, et al. Planning against biological terrorism: lessons from outbreak investigations. Emerg Infect Dis [serial online] 2003 May [December 19, 2005]. http://www.cdc.gov/ ncidod/EID/vol9no5/02-0388.htm 2.Centers for Disease Control and Prevention. Biological and chemical terrorism: strategic plan for preparedness and response. Recommendations of the CDC Strategic Planning Workgroup. MMWR 2000;49(RR-4). 3.Papier A, Allen E, McDermott M. Software improves diagnostic accuracy with minimal training. American Medical Informatics Association Annual Meeting; Washington, DC; November 2001. Poster presentation. 4.Strongin R. Biological terrorism: is the healthcare community prepared? Issue brief no. 731. Washington, DC: George Washington University; 1999. 5. APIC Bioterrorism Working Group. April 2002 interim bioterrorism readiness planning suggestions. http://www.apic.org/ Content/NavigationMenu/ PracticeGuidance/Topics/ Bioterrorism/ APIC_BTWG_BTRSugg.pdf. Other recommended reading: Ferguson NE, Steele L, Crawford CY, Huebner NL, Fonseka JC, Bonander JC, et al. Bioterrorism web site resources for infectious disease clinicians and epidemiologists. Clin Infect Dis 2003;36:1458-1473. Bradley CA, Rolka H, Walker D, Loonsk J. BioSense: Implementation of a national early event detection and situational awareness system. MMWR 2005;54(suppl):11-19. http://www.cdc.gov/ mmwr/preview/ mmwrhtml/su5401a4.htm. American Hospital Association. Readiness for potential attack using chemical or biological agents. http://www.hospitalconnect.com/ aha/key_issues/disaster_readiness/ readiness/MaDisasterB1003.html. American Hospital Association. Disaster readiness. http://www.hospitalconnect.com/ aha/key_issues/disaster_readiness/ readiness/MaDisasterB0921.html. American Hospital Association. Hospital preparedness for mass casualties. http://www.hospitalconnect.com /ahapolicyforum/ resources/disaster.html. American Hospital Association. Bioterrorism readiness plan: a template for healthcare facilities. http://www.aha.org/aha/ key_issues/disaster_readiness/ readiness/ MaBioterrorismReadinessB1017.html Gostin LO, Sapsin JW, Teret SP, Burris S, Mair JS, Hodge JG, et al. The Model State Emergency Health Powers Act: planning for and response to bioterrorism and naturally occurring infectious diseases. JAMA 2002;288:622-628