BIO 161 Worksheet - Cardiovascular
advertisement

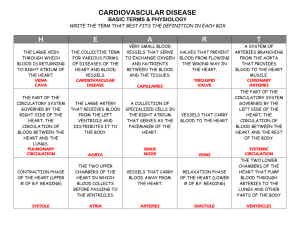
BIO 161 – Cardiovascular - Answers T Dic Charge – Winter 2008 Review Worksheet 1) Name the 3 different classifications of blood vessels. Arteries, capillaries, veins 2) Identify the 3 layers of tissues in the two larger classifications of blood vessels, identifying which are innermost or outermost for each. Innermost – Endothelium - smooth muscle – thicker in arteries than in veins Outermost - Connective tissue 3) What is the function of each of the 3 layers that you identified in #2 above? How does its structure meet that function? Endothelium – provide smooth low-friction surface to optimize blood flow – very smooth layer of cells/no irregularities Smooth Muscle layer – vasoconstriction/vasodilation – circular arrangement of muscle fibre sheets allow for contraction to narrow the lumen and relaxation to effect an increase in the size of the lumen Connective tissue – collagen fibres are tough protein that provides both form and protection for the other two layers 4) Please complete the following table Arteries Capillaries Veins ______ pressure ______ pressure almost no pressure _____ muscular walls _____ muscular walls ____ muscular walls Found deep Superficial Both (circle one) Pulse? found everywhere Found deep Superficial Both (circle one) Pulse Pulse? Flow – fast Flow – fast Flow – fast Slow Slow Slow Very slow (circle one) Very slow (circle one) Very slow (circle one) Answers to be found on slide #6 in the lecture notes 5) From inside a heart chamber, identify the layers of tissue that you would encounter as you moved outwards. Endocardium, myocardium, visceral pericardium, parietal pericardium 6) Define the term “cardiac tamponade” and explains how it might come about If pressure in the pericardium rises sufficiently due to fluid accumulation, the heart might stop beating altogether – this is cardiac tamponade. The fluid might accumulate because of trauma to the pericardium, disease (MI, HIV, mumps, etc.), or infection of the pericardium 7) Describe the formation of an atherosclerotic plaque on an arterial wall. a) LDLs deposit on wall b) WBCs (leukocytes) attracted to wall invoke inflammation – devour fats and become “foam” cells c) a cap may form on the foam cells that is thick and stable (doesn’t easily break away) or it may be thin and fragile and could break away, resulting in a heart attack of stroke – this answer, though not discussed in lecture, is well worth understanding from slide #8 8) Explain what structural component of arteries makes them very elastic, and what function this serves. The presence of elastin in all 3 layers of these vessels means they can expand and absorb the shock of the systolic pulse of blood, and then slowly collapse to maintain arterial pressure during diastole – hence, they are recognized as a pressure reservoir. 9) Start in the right atrium and describe EVERY structure (chambers, valves, vessels) a blood cell would travel through (don’t worry about what’s nearby for this answer) as it completed one complete circuit of the circulatory system and returned to the right atrium. Right atrium tricuspid valve right ventricle pulmonary (semilunar) valve pulmonary trunk pulmonary arteries arterioles capillaries (lungs & alveoli) venules pulmonary veins left atrium bicuspid (mitral) valve left ventricle aortic (semilunar) valve aorta arteries arterioles capillaries venules veins inferior or superior vena cava or coronary sinus right atrium 10) In the fetal heart, two chambers are connected via a hole in the wall between them. Which chambers are involved, what is the name of the hole, and once it closes prenataly, what is the closed hole then called? Why is this arrangement functional in the fetal heart (what is the logic behind this evolutionary difference in fetal versus post-natal heart)? The foramen ovale connects (and therefore shunts blood from) the right atrium to the left atrium. Closed by birth, the depression seen mostly from the right atrial side of the interatrial septum is called the fossa (depression) ovalis. Because fetal lungs are not the source for oxygenation of the blood, the foramen ovale serves to efficiently bypass the lungs for most of the blood flow. 11) What is the tissue between the two atria called? Between the two ventricles? Interatrial septum and interventricular septum 12) Structures that prevent the eversion of valves in the heart are found attached to some but not all of the valves. Which valves do have these structures, what are they (the structures) called, and to what muscles are they attached? Which chambers are the structures/muscles found in? The chordae tendinae are found in the ventricles, supporting and preventing the tricuspid (right) and bicuspid (left) valves from everting into their respective atria. The chordae tendinae are attached to papillary muscles on the inferior surface inside the ventricular chamber. Eversion means flipping outwards, much like an umbrella might evert in a windstorm. 13) Following up on question 12, why don’t the other valves have these structures (and which valves are they)? The aortic and pulmonary valves (both semilunar valves) don’t need this kind of support because pressures in the aorta and in the pulmonary trunk are not high enough to threaten eversion of the valve. 14) Describe the circulation of the heart tissue itself (ie. the coronary circulation). Include a description of how the vessels are interconnected, and don’t forget the venous return. The right coronary artery arises from the aorta and crosses down the right side of the heart below the right atrium and then wraps around the posterior of the heart where it connects (anastomoses) to the circumflex artery. The left coronary artery arises from the aorta and moves over the left atrium where it divides into the interventricular, which runs roughly over the interventricular septum and wraps around a point slightly lateral to the apex of the heart to meet up with the anastomosis of the right coronary artery and the circumflex artery. The latter is the second branch of the left coronary artery – it wraps around the left side of the heart below the left atrium and then anastomoses with the right cornary and interventricular arteries on the posterior surface of the heart. The veins of the heart (not studied in lecture) collect venous blood in the coronary sinus, which empties into the right atrium, where the blood mixes with blood from the vena cavae. 15) Define the terms a) Stenosis Narrowing (of anything) – in the heart, a stenosed valve could lead to congestive heart failure b) Valvular incompetence If a valve leaks or in any way fails to function, it is said to be incompetent. c) Heart murmur Any leaky valve or other cause of irregular flow in the heart results in a sound heard on ausculatation called a heart murmur. While a systolic murmur may be benign, ALL diastolic murmurs are considered pathologic. d) Ischemia Lack of blood flow to a tissue, which can result in tissue necrosis (death). e) Myocardial infarction Death of heart muscle (myocardium), usually due to ischemia. 16) Where are precapillary sphincters found and what is their purpose? Give two examples of this function. At the capillary end of arterioles, these sphincters are used by the body to regulate perfusion (blood flow) into certain capillary beds. The capillaries of the gut can be highly perfused after eating or have reduced perfusion during a fight/flight reaction. Capillaries of the extremities (hands/feet) might be highly perfused to shed heat in warm environments, or have reduced perfusion to conserve heat in cold environments. 17) Sketch a normal ECG and identify the 3 waveforms we have studied. On the same diagram, identify when the following events occur: Ventricular Repolarization, Atrial Repolarization, Ventricular Depolarization, and Atrial Depolarization. QRS complex Ventricular depolarization & Atrial repolarization Atrial depolarization Ventricular repolarization T P Time (s) 0 0.2 0.4 0.6 0.8 18) Describe the origin and spread of an electrical event in the myocardium of a normal, healthy heart. Include all structures in sequence, and indicate when different chambers of the heart are contracting. Sinoatrial node in superior right atrium spreads across both atria (and the atria contract) atrioventricular node (slows signal and creates pause between atrial and ventricular contractions left and right bundle branches (bundles of His) Purkinje fibres myocardia of both ventricles (ventricular contraction) 19) How do you explain the pause between the two phases of the heart contraction? Why is there such a pause? The atrioventricular node slows conduction of the depolarization between the atria and ventricles and this results in the delay between the contractions of the atria and the ventricles. The delay allows completion of ventricular filling (and atrial emptying) before the ventricles contract. 20) Identify the name of the cardiological phenomenon in each of the following three diagrams, and explain what is happening in each case. Consider the effect on Cardiac Output and the immediacy of the danger to the patient. Atrial fibrillation – the atrial myocardium is contracting in an uncoordinated fashion – very little additional blood is moving into the ventricles – reduced cardiac output is the result – not immediately fatal Ventricular fibrillation – the ventricular myocardium is contracting in an uncoordinated fashion – very little blood is moving if any, meaning Cardiac Output is essentially zero – fatal within 2-3 minutes 21) Fever is known to be associated with an increased heart rate. Describe the amount by which the HR rises per degree of increase in the fever, identify the temperature limit to this rise, and briefly explain why it happens. HR rises 10 bpm (beats per minute) for each 1 degree C rise in body temperature, but this rise reverses if the temperature rises above 40.5 to 41 degrees C. The rise is explained by the increased metabolism of the SA node at higher temperatures, and the fact that repolarization would happen faster (and thus the node would depolarize more frequently). 22) Identify the location and pace of the places in the myocardium that will spontaneously depolarize. What happens in each case if one node leads the heart in depolarization? SA node – 70-80 bpm – will result in the normal spread of depolarization through the heart AV Node – 45-60 bpm – would result in synchronous depolarization/contraction of the atria and ventricles with the atria contracting in the cephalic (towards the head) direction. Purkinje Fibres – 15-40 bpm – would result in the ventricles contracting before the atria, and the atria would be contracting from the AV node upward, in the wrong direction. 23) What is the technical term for the tissues identified in the previous question that describes their property of spontaneously depolarizing? Automaticity 24) What is Bundle Branch Block and what does it cause? One or the other or perhaps both of the bundle branches in the interventricular septum are damaged and do not conduct signals. This means the atria may beat normally, but the Purkinje fibres would be the only tissue distal to the blockage that would still be capable of automaticity and so would drive the contraction of the ventricles. Because they depolarize less frequently than the SA node, the ventricular contractions would be less frequent and there would be a disconnect (asynchrony) between the atrial and ventricular contractions. 25) While the heart muscle is capable of driving its own rhythm, what two nerves are responsible for raising and lowering the HR in response to demands from the body? How is this actually accomplished at the level of the SA node? The vagus nerve (Cranial X) influences the SA node to take longer to repolarize and therefore lowers HR in response to a drop in demand for oxygen from the body. The accelerator nerve works the opposite way, to reduce the time of repolarization of the SA node and therefore elevated the HR in response to increased demand (exercise, fight/flight response) 26) What effects do Atropine and Digitalis have on the heart? Atropine in small doses will slow the heart, but in higher doses causes the HR to rise Digitalis is administered to produce a slow and steady rhythm – too much can depress the heart to the point of stopping. 27) Define the clinical interpretation of a slow and a fast HR (that is, give each a name and define the actual HR threshold for each). tachycardia – high HR (over 100 bpm) bradycardia – low HR (below 60 bpm) 28) Define the terms stroke volume and cardiac output. SV is the amount of blood ejected by either ventricle in each beat CO (or Q) is the amount of blood ejected by either ventricle over an entire minute. 29) An individual who is 40 years of age is exercising maximally and is determined to have a cardiac output of 18 L/min. Assuming a normal HR for that age at maximal exercise, please determine the stroke volume at exercise. HRmax = 220-age = 220 – 40 = 180 bpm CO=HR x SV so SV = CO/HR = 18000/180 = 100 ml 30) Explain what congestive heart failure (CHF) is. Due to incomplete ventricular ejection (blood remains in the ventricle after systole), filling of the ventricle limits the blood flow from the side of the circulation that empties into that side of the heart (systemic for the right ventricle, pulmonary [lungs] for the left side). As blood backs up on that side, pressure builds and edema in the tissues is the result result. The heart will work harder as a result of decreased perfusion. 31) Name four possible causes of CHF a) Coronary atherosclerosis b) Persistent high blood pressure c) Multiple myocardial infarcts d) Stenosed valves 32) What is hemoptysis and what side of the heart would be implicated if the cause was CHF? Hemoptysis is the coughing up of blood – if due to CHF, this would imply a left side defect in which the left ventricle incompletely empties, blood backs up in the pulmonary circulation, and pressure has become high enough to cause the movement of erythrocytes out of the pulmonary capillaries and into the alveoli. 33) If the pulmonary valve is stenosed, describe what would happen to the heart and suggest a symptom that one might notice externally that might point to this problem. The right ventricle would have to work harder to push blood out into the pulmonary trunk, so it would hypertrophy. Because ejection would likely be incomplete, this would be right side CHF, and would likely result in systemic edema, resulting in swollen limbs, particularly the lower legs/feet, or hepatic edema. 34) Define what blood pressure is and identify the two main factors that contributed to it. BP is the pressure exerted on arterial walls – it is a combination of the effect of the volume of the blood ejected by the heart into the vessels (SV) and the compliance (elasticity) of the vessels. 35) Please sketch a graph that illustrates the decline in blood pressure from the aorta through the systemic circulation until blood returns by the vena cava. Identify in which vessels the pulse declines to zero as well. Use appropriate units of blood pressure and list all sizes of blood vessels on both the aterial and venous sides of the capillaries, as well as the capillaries. Important points: pulse is 120/80 at aorta but is already declining in arteries and has been reduced to less than 20 mm Hg (100/80) before leaving the arteries Mean pressure is about 80 upon entering arterioles Pulse declines to zero in the arterioles Pressure drops starting in smaller arteries and declines below 40 before entering capillaries, and further below 20 upon leaving the capillaries Pressure declines gradually from there to zero. 36) What two reasons can you use to explain the decline in pressure as blood travels throughout the systemic circulation in a healthy, normal individual? Distance – as distance increases, frictional energy losses result in the decline in pressure Cross-sectional area – although progressively smaller vessels are encountered, the number of vessels multiplies rapidly. The cross-sectional area of the aorta is surpassed by the enormous increase in cross-sectional area of the arterioles and even more so in the capillaries. 37) Explain the effect of atherosclerosis on Blood Pressure Both frictional increases and narrowing of the lumen (ie. a decrease in the cross-sectional area) are results of atherosclerosis – both contribute to an INCREASE in blood pressure, which is known as hypertension. In addition, the vessels with atherosclerotic plaques are less elastic and so that also contributes to higher blood pressure 38) Explain what the Frank-Starling Mechanism (or simply Starling’s Law) refers to with respect to the heart, and suggest its effect on Blood Pressure. As venous return increases (perhaps due to increased contraction of skeletal muscle during exercise, stretching of the ventricle by the additional volumes of blood returning to the heart causes and increased force of contraction. This results in more blood being ejected into the vessels by the ventricles, and thus causes a rise in Blood Pressure (recall that BP is influenced in the aorta and early arteries by two things – the SV and the elasticity of the vessels) 39) As a person exercises, more blood is pumped back to the heart. Explain how this is so. Increased skeletal muscle contraction results in a pumping effect on the veins. Due to the arrangement of the valves in the larger venules and the veins and vena cavae, the blood moves within the veins compressed by the muscles in the direction of the heart. This results in more blood returning to the heart, or an increased venous return. See Frank-Starling, above. 40) Please be sure to know the meanings of these terms: (check your text, a medical dictionary, or your notes for definitions) a) Ischemia b) Edema c) Vasoconstriction d) Vasodilation e) Pericarditis f) Chordae Tendinae g) Trabeculae Carnae h) Papillary Muscles i) Anastomosis j) Stenosis k) Systole l) Diastole m) Infarct n) Depolarize o) Repolarize p) Automaticity q) Tachycardia r) Bradycardia s) Stroke Volume t) Cardiac Output u) Polycythemia v) Hepatic w) Hypertension x) Hypotension y) Perfusion z) Hemoptysis