BME1450_paper
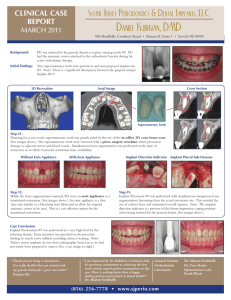
advertisement

A Systems Biology Approach to the Study of Contact Osteogenesis on Endosseous Implants 1 A Systems Biology Approach to the Study of Contact Osteogenesis on Endosseous Implants Jason Chau, MASc. student, IBBME Abstract—Contact osteogenesis provides early endosseous implant stability by forming bone directly on the implant surface, and is critical in determining the clinical success of the dental implant. This process is influenced by early blood-implant interactions in the endosseous wound site, and can be modulated with the use of different implant materials and microtextured surface topographies. This paper reviews the key stages of contact osteogenesis – hemostasis, osteoconduction, angiogenesis, and de novo bone formation – and describes how systems biology can be applied at each stage to improve our understanding of contact osteogenesis, implant integration, and implant design, or to provide clinically relevant applications. Index Terms—De novo bone formation, endosseous implant, hemostasis, osteogenesis, peri-implant healing, platelet biology, systems biology I. INTRODUCTION P ROSTHODONTICS, or the branch of dentistry that deals with the replacement of missing teeth or related jaw structures using artificial devices, is becoming an increasingly successful therapeutic modality with the advent of better endosseous (inbone) implant designs that shorten post-operation recovery time. It has been estimated that approximately one million implant procedures are now performed annually, worldwide [1]. Of central importance to the design of better implants, is a solid understanding of the cellular and molecular interactions occurring at the tissue-implant interface during the postoperation healing phase, and the mechanisms and factors that regulate these interactions. To this end, two types of peri-implant bone regeneration have been identified in the literature. The first type, distance osteogenesis, occurs when new bone formation is initiated at the old bone surface surrounding, but at a distance from, the implant. This causes new bone to slowly ‘grow’ towards the implant surface and results in the eventual approximation of the implant surface shape by the newly formed bone. Because distance osteogenesis occurs from a distance, there will always be an intervening layer of non-bone cells between the bone and implant, and can therefore be considered inferior from both a mechanical and integrative standpoint. Distance osteogenesis is reviewed more extensively elsewhere [2]. The second type, contact osteogenesis, occurs when osteogenic cells migrate to the implant surface, differentiate into osteoblasts, and begin laying down new bone directly onto the implant. This results in the apposition of newly secreted matrix to the implant surface, and is important for providing early implant stability in the endosseous site when the surrounding bone is mostly cancellous, as is the case in the posterior maxilla. Because the requirement of a stable union between endosseous implants and bone is paramount in the field of skeletal surgery [3], contact osteogenesis can be considered to be a clinically superior mode of healing. Hence this paper will focus on the application of systems biology to contact osteogenesis. Since, by definition, an implant has neither bone matrix nor cells on its surface upon implantation, the bone mass that subsequently appears on implant surfaces in contact osteogenesis must be deposited by osteogenic cells that have migrated to the implant surface and begun secretory activities. Like all biological systems, the endosseous healing site is a complex network of interacting components including cells, cytokines, growth factors, and other molecular species. Although recent research has yielded much information regarding contact osteogenesis in the peri-implant compartment, many questions still remain. For example, how do protein-protein interactions affect platelet activation in the extravasated blood of the peri-implant compartment? What is the bone-bonding mechanism, and how do different implant surface materials and designs affect the bone-bonding interface? The recent application of proteomics to the study of platelet biology may yield answers to some of these questions. [4] Clearly, a systems biology approach would be useful for modeling and analyzing the large quantities of empirical data that could be derived from such a system. As a whole, bone-healing research has heretofore been primarily a hypothesis-driven science (i.e. employing a topdown approach), and hence based on observable phenomena and researchers’ intuitions. A data-driven approach such as that emphasized in systems biology could therefore lead, naturally, to a more comprehensive understanding of the system and its underlying mechanisms. Furthermore, bone implant surface designs and materials comprise environmental and chemical perturbations to the biological system. Developing a system profile for endosseous wound sites would allow researchers to systematically investigate the effects of perturbation in an iterative manner, and improve our understanding of both the system and implant’s design. Hence the study of contact osteogenesis in endosseous wound sites falls naturally within the framework of a systems biology approach. There is also currently debate as to whether the A Systems Biology Approach to the Study of Contact Osteogenesis on Endosseous Implants 2 presence of an implant induces a different mode of healing than that seen in fracture healing [5], [6]. A systems biology understanding of contact osteogenesis would help to answer that question. II. HEMOSTASIS Hemostasis is the stoppage of bleeding or hemorrhage, and is achieved by the formation of a blood clot in endosseous wound sites. Given the surgical trauma associated with the implantation of endosseous implants, and the vascular nature of bone, blood is guaranteed to be the first tissue to come into contact with the implant surface [7], [8]. Since the migration of osteogenic cells to the implant surface is believed to be dependent on the activation of blood platelets and the establishment of a temporary fibrin scaffold within the periimplant compartment [9], early blood-implant interactions can be assumed to be of critical importance in determining later cellular responses that occur in the wound healing cascade, and ultimately the successful integration of the implant with the surrounding tissue. Although hemostasis involves many more cellular and molecular interactions than those that are described here, the current discussion will focus on cascades induced by specific platelet releasates for reasons of simplicity and immediate relevance. Anderson [10], and Gemmell and Park [7], provide a more complete discussion of the cellular cascades of wound healing and hemostasis in the presence of an implant, respectively. In particular, the activation of platelets causes the platelets to change shape and release many different cytokines, growth factors, and microparticles, some of which create chemotactic gradients for osteogenic cells, stimulate osteoblast proliferation, and act as enzymes to catalyze coagulation reactions. Implant surface-adsorbed fibrinogen, a soluble protein in blood, mediates the initial adhesion of platelets by binding to the GPIIb/IIIa integrin platelet surface receptor [11]. The amount of fibrinogen adsorbed on the implant surface, [8] as well as platelet activation levels [12] – [15], have both been shown empirically to increase on surfacemicrotextured implants as compared to smooth-surfaced implants. The increase in fibrinogen adsorption has been postulated as being a result of the increased surface area over which adsorption may occur, as well as the presence of surface features upon which fibrinogen may become entangled. Since platelet activation catalyzes the conversion of prothrombin to thrombin, which cleaves fibrinogen to fibrin, it follows that there should be more fibrin attached to implants with microtextured surfaces than implants with smooth surfaces. This simplified summary of events at the blood-implant interface is illustrated in Fig. 1. Good anchorage of the fibrin scaffold to an implant surface is important because migrating osteogenic cells have been shown to exert a contractile force of approximately 3 nN/cell [16], and the arrival of these migrating cells to the implant surface in contact osteogenesis is critically dependent on the retention of the fibrin scaffold to Fig. 1. Simplified representation of hemostatic events occurring at the endosseous implant surface. Events include fibrinogen adsorption, platelet binding, platelet degranulation, prothrombin to thrombin conversion, fibrinogen cleavage, and fibrin adsorption. the implant. Hence there can be little doubt that platelet activation plays a critical role in blood clot formation as well as the regulation of contact osteogenesis on endosseous implants. What is not well known is how the implant surface chemistry and rugosity modulates the number, and degree of activation, of platelets. In a more general sense, knowledge of material ‘thrombogenecity,’ or the ability of different materials to induce the formation of a blood clot [17], at the molecular level, is currently limited. Gemmell and Park [7] provide a detailed review of the biochemical species and reactions involved in the blood coagulation cascade, and identify that, “how the physical or chemical composition of the implant surface impacts on these reactions is largely unknown”. A promising recent development in platelet biology research that should improve our understanding of platelet activation mechanisms, and lend itself to the study of endosseous implant designs using a systems biology approach, is the application of proteomics to the study of platelets. Platelet proteomics is the study of the protein complement of the part of the genome that encodes for all platelet biology [4]. Indeed, all studies of platelet activation up until now have had a reductionist approach, using only one protein at a time [12]. The advent of platelet proteomics will allow researchers to take a data-driven approach, and address, for example, the question of what happens when platelets are exposed to a mixture of proteins. The availability of such a comprehensive knowledge base will be invaluable for the re-evaluation of the blood coagulation cascade under a systems biology framework, and enable us to gain a more detailed understanding of how different implant materials and surface designs affect implant thrombogenecity. Consequently, better endosseous implant designs could be developed. III. PERI-IMPLANT ANGIOGENESIS Angiogenesis is the growth of blood vessels occurring in an adult through the migration and proliferation of endothelial cells [18], and is important for revascularization of the A Systems Biology Approach to the Study of Contact Osteogenesis on Endosseous Implants endosseous wound site after tissue has regenerated. Following the destruction of the necrotic tissue by a vanguard of macrophages in the peri-implant compartment (i.e. another biological cascade initiated in part by platelet degranulation, but not described above), a zone of migratory fibroblasts and capillary sprouts, followed by another zone of secretorily active fibroblasts and functioning capillary loops is seen to occur [19]. These two latter zones represent the phenomena of angiogenesis and early tissue matrix regeneration respectively [18]. The resulting dense capillary network that is created is required because remodeling tissues have higher metabolic needs. It is usually resorbed once healing is complete. From this observation alone, it can be expected that angiogenesis is a complex phenomenon regulated by a complex cascade of biochemical signals. Transforming growth factor beta (TGF-) and plateletderived growth factor (PDGF) are two growth factors that are released upon platelet activation and play important roles in angiogenesis. The effects of TGF-, in particular, are difficult to characterize because markedly different results have been observed in vitro depending on the concentration, the assay used, and the cofactors present [19]. Furthermore, little work has been done to understand how angiogenesis may be affected by environmental perturbations such as the presence, or surface design, of an endosseous implant [18]. Despite the many hurdles that need to be overcome to gain a comprehensive understanding of angiogenesis, with a sufficient amount of empirical information and a data-driven approach, the dose and time responses of relevant cytokines and growth factors, and ultimately angiogenesis itself, could be modeled and simulated accurately as mathematical equations. The angiogenic response to environmental perturbations such as endosseous implants could then also be studied from this systems biology framework. IV. CONTACT OSTEOGENESIS A. Osteoconduction Following the establishment of a chemotactic gradient by blood platelet activation, and the formation of a fibrin clot during hemostasis, osteogenic cells will migrate towards the endosseous implant through the three-dimensional protein meshwork of the clot. This migratory activity is known as ‘osteoconduction,’ and is distinct, in this context, from the common use of the term in biomaterials literature to mean the apparent growth of bone tissue “along” an implant surface [19]. As previously mentioned, if the contractile forces of the osteogenic cell migration exceed the adhesive forces of the transient fibrin scaffold over which the cells are migrating, then the scaffold will detach from the implant surface. This would cause the osteogenic cells to stop migrating, differentiate into osteoblasts, and begin secreting new bone matrix away from the implant surface, forming bony spicules in the peri-implant compartment [9]. 3 Osteoconduction and the influences of factors such as chemotactic gradient strength and the amount of fibrin present at each location in space could easily be modeled with a set of partial differential equations to gain a better understanding of possible osteogenic cell fates in the peri-implant compartment. This type of information could be used, for example, in the pre-surgical assessment of whether or not a patient has a high enough concentration of blood coagulation components (e.g. platelets) to ensure successful endosseous integration of the implant. B. De novo bone formation If the migrating osteogenic cells reach the implant surface, they will undergo differentiation into osteoblasts, become sessile, and begin secreting new bone matrix onto the implant surface. This process of initial matrix secretion by newly differentiated osteogenic cells is known as ‘de novo bone formation,’ and is distinguished from continued appositional growth by previously differentiated osteoblasts, by the presence of a non-collagenous mineralized ‘cement line’ matrix of approximately 0.5 m thickness at the bone-implant interface, that is not seen in the latter. De novo bone formation has been described as a four-stage process comprising the initial adsorption of the non-collagenous bone proteins osteopontin (OPN) and bone sialoprotein (BSP) to the implant surface, the initiation of mineralization (i.e. nucleation of the cement-line matrix) by the adsorbed proteins, continued mineralization resulting from crystal growth, and the assembly of a mineralized collagenous matrix overlying the cement-line matrix [19] – [21]. Because this interfacial cement line matrix bonds to both the bone and endosseous implant surfaces, it is of particular interest for studying the phenomenon of ‘bone bonding,’ the exact meaning and perceived mechanisms of which have engendered much debate [9]. Hosseini et al. have recently shown that the cement line matrix exhibits a heterogeneous morphology and consists of several organic as well as inorganic components, and that this matrix is formed by cells of a specialized osteogenic phenotype prior to the expression of BSP [22]. Employing a systems biology approach to develop a system profile by studying the physical and chemical characteristics of the cement line matrix boundary with many different implant surfaces (i.e. both material- and topography-wise) would not only yield clues as to the exact nature of the bone bonding mechanism, but could also allow us to forge an understanding of how to use different implant materials and surface designs to control the biological response of the cement line matrix generation for therapeutic purposes. V. IMPLANT MATERIALS Titanium and titanium alloy are currently the most widely used metals in the manufacture of endosseous implants because of their biocompatibility, lightness, mechanical strength, and high corrosion resistance [23]. However, titanium and titanium alloys are generally not considered to be A Systems Biology Approach to the Study of Contact Osteogenesis on Endosseous Implants bone bonding [9]. Calcium phosphate materials such as hydroxyapatite (HA) are considered to be bone bonding [24]. The two dominant paradigms of thought on the nature of the bone bonding mechanism are a chemical bonding interaction at the tissue-implant interface, and a micromechanical interlocking of the two surfaces. Since bone bonding represents a macroscopically seamless integration with the surrounding bony tissue regardless of the underlying mechanism, it is a desirable for endosseous implant surfaces to be bone bonding. To this end, calcium phosphate surface coatings have been applied to titanium and titanium alloy implants to produce biocompatible implants that are mechanically strong, corrosion resistant, and bone bonding. As mentioned above, a data-driven approach to studying the cement line matrix formation on different implant materials could help elucidate the true mechanism of bone bonding. VI. CONCLUSION A systems biology approach to the study of contact osteogenesis in endosseous wound sites would provide researchers with a more complete understanding of the events that occur in the peri-implant healing compartment, as well as how they are modulated by novel implant surface designs. Moreover, due to the multidisciplinary nature of peri-implant endosseous healing research, a data-driven integrative approach would be better suited to the task than traditional hypothesis-driven methods. As new high-throughput analysis tools are developed, new areas of research, such as platelet proteomics, will be established to complement the systems biology approach proposed here, and the benefits to our understanding of tissue-implant interactions as well as clinical protocols will become increasingly evident. REFERENCES [1] [2] [3] [4] [5] [6] [7] [8] [9] J. E. Davies, Bone Interface Group, Toronto, ON, private communication, August 2004. T. Masuda, P. K. Yliheikkila, D. A. Felton, and L. F. Cooper, “Generalizations regarding the process and phenomenon of osseointegration. Part 1. In vivo studies,” International Journal of Oral and Maxillofacial Implants, vol. 13, pp. 17-29, January 1998. A. Boyde and L. A. Wolfe, “Spatial and temporal patterns of bone growth around endosseous implants,” in Bone Engineering, J. E. Davies, Toronto: em squared Inc., 2000, pp. 321-331. P. B. Maguire and D. J. Fitzgerald, “Platelet proteomics,” Journal of Thrombosis and Haemostasis, vol. 1, pp. 1593-1601, July 2003. H. Jr. Plenk and H. Zitter, “Material considerations,” in Endosseous Implants: Scientific and Clinical Aspects, G. Watzek, Chicago: Quintessence, 1996, pp. 63-99. D. E. Steflik et al., “Ultrastructural analyses of the attachment (bonding) zone between bone and implanted biomaterials,” Journal of Biomedical Materials Research, vol. 39, pp. 611-620, March 1998. C. H. Gemmell and J. Y. Park, “Initial blood interactions with endosseous implant materials,” in Bone Engineering, J. E. Davies, Toronto: em squared Inc., 2000, pp. 108-117. J. Y. Park and J. E. Davies, “Red blood cell and platelet interactions with titanium implant surfaces,” Clinical Oral Implants Research, vol. 11, pp. 530–539, December 2000. J. E. Davies, “Understanding peri-implant endosseous healing,” Journal of Dental Education, vol. 67, pp. 933-949, August 2003. 4 [10] J. M. Anderson, “The cellular cascades of wound healing,” in Bone Engineering, J. E. Davies, Toronto: em squared Inc., 2000, pp. 81-93. [11] M. Broberg, C. Eriksson, and H. Nygren, “GpIIb/IIIa is the main receptor for initial platelet adhesion to glass and titanium surfaces in contact with whole blood,” Journal of Laboratory and Clinical Medicine, vol. 139, pp. 163-172, March 2002. [12] S. Kanagaraja, I. Lundström, H. Nygren, and P. Tengvall, “Platelet binding and protein adsorption to titanium and gold after short time exposure to heparinized plasma and whole blood,” Biomaterials, vol. 17, pp. 2225-2232, December 1996. [13] H. Nygren, P. Tengvall, and I. Lundström, “The initial reactions of TiO2 with blood,” Journal of Biomedical Materials Research, vol. 34, pp. 487-492, March 1997. [14] H. Nygren, C. Eriksson, and J. Lausmaa, “Adhesion and activation of platelets and polymorphonuclear granulocyte cells at TiO2 surfaces,” Journal of Laboratory and Clinical Medicine, vol. 129, pp. 35-46, January 1999. [15] J. Hong, J. Andersson, K. Nilsson Ekdahl, G. Elgue, N. Axén, R. Larsson, and B. Nilsson, “Titanium is a highly thrombogenic biomaterial: possible implications for osteogenesis,” Thrombosis and Haemostasis, vol. 82, pp. 58-64, July 1999. [16] C. G. Galbraith and M. P. Sheetz, “A micromachined device provides a new bend on fibroblast traction forces,” Proceedings of the National Academy of Sciences of the United States of America, vol. 94, pp. 91149118, August 1997. [17] D. F. Williams, in Definitions in Biomaterials: Proceedings of a Consensus Conference of the European Society for Biomaterials, Chester, England, March 3-5, 1986, Amsterdam, New York: Elsevier, 1987. [18] L. A. Lakey, R. Akella, and J. P. Ranieri, “Angiogenesis: implications for tissue repair,” in Bone Engineering, J. E. Davies, Toronto: em squared Inc., 2000, pp. 137-142. [19] J. E. Davies and M. M. Hosseini, “Histodynamics of endosseous wound healing,” in Bone Engineering, J. E. Davies, Toronto: em squared Inc., 2000, pp. 1-14. [20] J. E. Davies, “In vitro modeling of the bone/implant interface,” The Anatomical Record, vol. 245, pp. 426-445, January 1996. [21] J. E. Davies, “Mechanisms of endosseous integration,” International Journal of Prosthodontics, vol. 11, pp. 391-401, September 1998. [22] M. M. Hosseini, J. Sodek, R. P. Franke, and J. E. Davies, “The structure and composition of the bone-implant interface,” in Bone Engineering, J. E. Davies, Toronto: em squared Inc., 2000, pp. 295-304. [23] F. C. Eichmiller, “Titanium applications in dentistry,” The Journal of the American Dental Association, vol. 134, pp. 347-349, March 2003. [24] L. L. Hench and J. Wilson, “Surface-active biomaterials,” Science, vol. 226, pp. 630-636, November 1984.