Preparation for Mother-Baby Clinical Experiences
advertisement

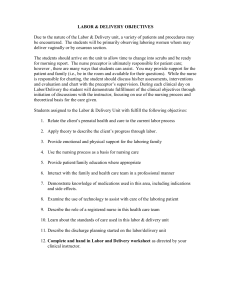
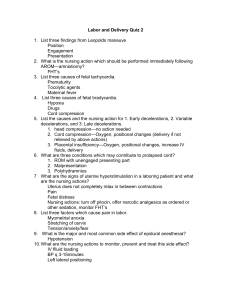
Preparation for Mother-Baby Clinical Experiences Be prepared to perform and/or assist with the following: ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ ___ Routine Care: a.m. hygiene, linen, vitals/BP, meals, turning, ambulating Postpartum (BUBBLE) Assessment: head-to-toe systems assessment Breast/nipples-assessment, care for breastfeeding & bottle-feeding Uterus – fundal firmness, level, midline deviation Bowel-distention, bowel sounds, return of flatus Bladder-distention, UTI symptoms Lochia: amount, character /___Legs: s/s thrombophlebitis, Homan’s sign Episiotomy – perineum & hemorrhoids Incision – abdominal/tubal ligation Emotional/psychosocial/educational needs Injections-IM, sub-Q IV therapy newborn vital signs, including normal limits newborn assessment basic care: bathing, feeding, diapering, positioning, cord care bottle-feeding assisting breastfeeding mother infant safety and security measures circumcision care Medication Cards – Due by first clinical name of drug, including generic name indications side effects nursing considerations Postpartum/Antepartum Medications: ___ Colace (docusate sodium) ___ Pericolace ___ simethicone (Mylicon) ___ nutritional supplements: ___ ferrous sulfate ___folic acid ___ antibiotics: ___ampicillin ___ gentamicin ___cefazolin ___ methegine ___ Rho-gam ___ vaccines: ___Rubella ___Rubeola ___MMR ___ Betamethasone ___ Depo-Provera ___ Insulin: ___regular ___NPH ___ Analgesics: ___Percocet___Tylenol___codeine___ibuprofen___Toradol Nursery Medications: ___ Vitamin K IM) ___ ___ erythromycin eye ointment hepatitis B vaccine (Recombivax) OB Daily Worksheet Your need to obtain this information every day for each client. This worksheet will assist you in developing a daily plan of care, receiving and giving shift report, and discussing your client in post-conference. Client initials ____ Age ____ EDB ____ Weeks gestation ____ P ____ A ____ Pertinent medical history: Past OB history: G ____ T ____ L ____ Current OB History: Delivery date/time ___________ Type of deliver: Anesthesia: Complications: Infant sex_____ Birth weight ______ Apgar scores ______ Infant feeding: Maternal blood type/Rh _____ Medications and indications: Infant blood type/RH _____- Nursing Coventions: Nursing Diagnoses: 1. 2. Discharge Plan: Teaching/Referral needs: Mother-baby Clinical Education Preparation Worksheet Due as directed by your clinical instructor: In preparation for providing discharge education for new mothers, the student will complete a written teaching plan. Write this plan as you would instruct your client. Information is to be found in the textbook and class notes. The student will include information on the following topics: 1. Maternal self-care following a vaginal delivery: Perineal care, sitz bath, process of involution, breast care, signs of illness. 2. Maternal self-care following a cesarean delivery: Care of incision, signs of infection. 3. Maternal and family psychological adaptation: Postpartum blues, postpartum depression, time management, sibling rivalry. 4. Maternal nutritional needs. Breastfeeding, bottle feeding, Cesarean delivery. 5. Breast self-examination. 6. Basics of infant care: Bathing, diapering, cord care, circumcision care, bulb syringe. 7. Basics of infant safety: Care seat law, positioning for sleep and feedings, prevention of accidents, immunizations, signs of illness. 8. Basics of bottle feeding. Formula prep, frequency, amount, burping. 9. Basics of breastfeeding: Positioning, latch-on, frequency and length of feeds, how to know baby is getting enough, care of sore nipples. This paper is to be neatly written or typewritten. Nursery Preparation WORKSHEET: Name:________________________ (Due prior to clinical as directed by your instructor) TERM ACROCYANOSIS ERYTHEMA TOXICUM ”newborn rash” JAUNDICE LANUGO MILIA DESCRIPTION LOCATION MONGOLIAN SPOTS PETECHIAE PLETHORA NEVUS FLAMMEUS “port wine stain” TELANGIECTATIC NEVI “stork bites” VERNIX CASEOGA SAMPLE CLINICAL SCHEDULE (Mother-Baby) 0630 Report to unit, scrub, look over charts Complete clinical preparation sheets 0700 Listen to shift report 0730 Report to instructor, look over chart 0730- Initial patient assessment, vital signs 0800 0800 Medications, breakfast 0830- Maternal assessment, change beds, AM care, patient education, discharge 1030 planning Newborn assessment, assist with infant feedings, bath demonstrations, immunizations, assist with circumcision 1100 Patient assessment, vital signs, teaching 1130 Patient Assessment, Charting, report to staff nurse 1200 Post-conference ANTEPARTUM CLINICAL OBJECTIVES During the clinical experience on the Antepartum Unit, the student will: 1. Verbalize understanding of nursing theory pertaining to high-risk antepartum clients and families. 2. Apply the nursing process in the care of high-risk antepartum clients. 3. Perform a high-risk antepartum client’s emotional status. 4. Assess the high-risk antepartum client’s emotional status. 5. Demonstrate the management skills necessary to plan and implement care for high-risk antepartum clients. 6. Provide safe, appropriate nursing interventions for high-risk pregnancy. 7. Educate clients/families to promote coping with a high-risk pregnancy. 8. Verbalize knowledge of safe, appropriate medication and ministration for highrisk antepartum clients. 9. Discuss discharge planning, continuing health needs and the use of community resources for high-risk antepartum clients/families. 10. Utilize appropriate communication skills including: a. written documentation b. verbal interaction with clients and families c. professional communication with members of the health care team 11. Explore the role of the nurse on the high-risk antepartum health care team. 12. Demonstrate professional behavior and development by: a. participating in planning individualized clinical experiences. b. displaying professional behavior in all clinical settings. c. managing professional responsibilities related to clinical experience. d. initiating discussions with the instructor to demonstrate fulfillment of objectives. LABOR & DELIVERY OBJECTIVES Due to the nature of the Labor & Delivery unit, a variety of patients and procedures may be encountered. The students will be primarily observing laboring women whom may deliver vaginally or by cesarean section. The students should arrive on the unit to allow time to change into scrubs and be ready for morning report. The nurse preceptor is ultimately responsible for patient care; however , there are many ways that students can assist. You may provide support for the patient and family (i.e., be in the room and available for their questions). While the nurse is responsible for charting, the student should discuss his/her assessments, interventions and evaluation and chart with the preceptor’s supervision. During each clinical day on Labor/Delivery the student will demonstrate fulfillment of the clinical objectives through initiation of discussions with the instructor, focusing on use of the nursing process and theoretical basis for the care given. Students assigned to the Labor & Delivery Unit with fulfill the following objectives: 1. Relate the client’s prenatal health and care to the current labor process 2. Apply theory to describe the client’s progress through labor. 3. Provide emotional and physical support for the laboring family 4. Use the nursing process as a basis for nursing care 5. Provide patient/family education where appropriate 6. Interact with the family and health care team in a professional manner 7. Demonstrate knowledge of medications used in this area, including indications and side effects. 8. Examine the use of technology to assist with care of the laboring patient 9. Describe the role of a registered nurse in this health care team 10. Learn about the standards of care used in this labor & delivery unit 11. Describe the discharge planning started on the labor/delivery unit 12. Complete and hand in Labor and Delivery worksheet as directed by your clinical instructor. Preparation for Labor and Delivery Clinical Experiences Be prepared to perform and/or assist with the following: ____ ____ ____ ____ ____ ____ ____ ____ ____ antepartum assessment intrapartum care – process and coaching auscultation of fetal heart tones preoperative preparation and care female catheterization application of external fetal monitor & toco transducer epidural/spinal anesthesia local anesthesia identify obstetric complications: pregnancy induced hypertension (PIH) preterm labor (POL) Medication Cards – Due by firs clinical name of drug, including generic name indications side effects nursing considerations Labor and Delivery Medications: ____ oxytocin (Pitocin) ____ magnesium sulfatge (MgSO4) ____ ritodrine ____ terbutaline ____ nifedipine ____ misoprostil (Cytotec) Narcotics: ____ morphine ____ stadol ____ duramorph ____ fentanyl L & D Preparation: Name: _______________________ (Due prior to clinical as directed by your instructor) 1. Define cervical DILATION: 2. Define EFFACEMENT: 3. Describe STAGE ONE LABOR a. Latent Phase b. Active Phase c. Transition Phase . 4. Describe STAGE TWO 5. Describe STAGE THREE 6. How is DURATION of contractions measured? 7. How is FREQUENCY of contractions measured? 8. Describe each of the following FETAL HEART RATE PATTERNS: a. Accelerations b. Early Decelerations c. Late Decelerations d. Variable Decelerations 9. List 3 non-pharmacologic methods of pain control for the laboring woman: 10. List 2 nursing diagnoses which may apply to the laboring woman LABOR AND DELIVERY WORKSHEET (Due after clinical as directed by your instructor) Name __________________________ Date ___________________________ History: Patient initials: _________ Age: _______ G _______ T _____ P _____ A ______L ____ EDB: ________ Prenatal Care: yes ____ no ____ Significant Pregnancy-related Problems & Treatment: Significant Non-pregnancy Health Problems: Medications (including pain meds) and indications: Assessment: Cervical Dilation _____ Effacement ______ Station ____ In which stage and/or phase of labor is your client? Fetal Monitor Evaluation: 1. External monitor (ultrasound) _____ internal (fetal scalp electrode ________ 2. What is the baseline fetal heart rate? ______________________ is it within normal limits? __________________________ 3. What is the fetal heart rate variability? ____________________ is the variability: a. decreased b. average c. increased 4. Are any periodic changes present? ____________________ If so, are they: a. accelerations b. early decelerations c. variable decelerations d. late decelerations Uterine Activity Evaluation 1. External monitor (Toco) ______ Internal (IUPC) _________ 2. Describe the uterine contraction pattern: Frequency:___________________________ Duration: ____________________________ Intensity: ____________________________ Is the contraction pattern within normal limits? _________________ Nursing Coventions and Evaluation Based upon your assessment of the laboring woman and the monitor strip, what nursing care would you administer?