Rad
advertisement

Rad.Fun.
5/13/98
-majority of energy used (99%) results in heat
-outer shell electrons are temporarily excited
-as fall back into orbit, release energy as infrared radiation (heat)
-heat is directly related to mAs and kVp
-heat units calculated as mVp x mA (single phase only) x 1.35 for HF
-if release too much heat, can crack or melt the anode ($5000 repair bill)
-you buy anodes based on their heat ratings
(typical anode holds 150,000 heat units (HU)
(larger anodes hold up to 400,000 HU)
X-ray production
-characteristic radiation (sometimes)
-Bremsstrahlung radiation (always)
Characteristic radiation
-radiation produced is characteristic for anode material (usually Tungsten (W)~69.5keV)
-depends on electron binding energies for target material
-cannot use tungsten for mammograms (to get soft tissue contrast-use molybdenum (Mb)) 28kV
-special tubes &targets for breasts vs bones
-projectile electron ionizes a K shell electron
-electrons from higher orbits fill the "hole"
-change in electron binding energies results in photons w/that keV value
(from l,m,n,o,p shells falling to k shells etc.)
-at 69.5keV-no characteristic radiation (tungsten)-just Bremsstrahlung
-get a spectrum of energies-useful energies are outer shell electron dropping into a K shell
Bremsstrahlung radiation
-braking (slowing,decelerating) radiation
-projectile electron (negative charge) comes under the influence of the nucleus (electron Coulomb force)
-projectile electron changes direction, variably
-change in direction causes Bremsstrahlung x-ray photon production (conservation of momentum)
-get lots of tiny photons due to lots of minute changes in direction
-max energy an electron can give up (depends on kVp)
the ones that have to do almost a complete u-turn, give up energy almost equal to their kVp
characteristic
Bremsstrahlung
# photons
70 kV
-lots of low kV photons produced-bad for people, gets absorbed by skin, etc.
-if kVp >70, ~15% is characteristic, rest is Bremsstrahlung
-use filters to get rid of low kV stuff
70
100
Filtered peak kV >70
60kV
graph of filtered xray output where peak kV <70
AC (alternating current)
1/120
+
1/120
sinewave=1/60
60cycles(60Hz)
half-wave rectification-only keep positive halves
-in past-took long time to do an x-ray-irradiate,wait,irradiate some more
rectification-full wave
-convert negative halves to positive
unnecessary waiting (“ripple”)
-gives 2x the x-rays in same amount of time
-peaks of arches should be equal to what you set on the console
-but still have dead time in valleys (ripple factor)
3-phase,full wave rectified waveform
-keeps average energy in beam higher
-ripple only 10%
-PROBLEM-3 phase is expensive (wiring to get 3 phase into your building is $$$$$$)
6 kHz Medium Frequency electrical waveform (1965-Gendex)
-cheaper than 3 phase
Switch creates the jagged portion
-“Universal” xray- single phase source (subsidiary of Gendex
100 kHx (1994)
-field effect transistor(can switch 100k times per sec)
-very fine control-ripple ~1%
Bennett
(forgive the drawing)
-but Gendex/Universal gave lighter xray than Bennett-50% due to ripple
-added more time (by trial & error)
Question-Does the patient pay a burden in dose to get comparable xray densities?
Answer- YES-20% more (50%of problem is due to ripple)
Neuro-electrical way to measure dose
TLD badges-chemical way to measure dose
Gendex threatened to sue to keep results from being published.
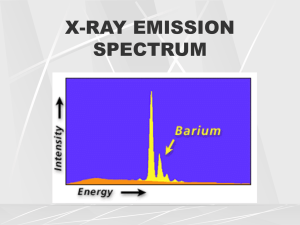
Xray emissions spectrum of filtered beam:
# of xrays
characteristic
-the fact that the part after the spike exists means beam >70
Ripple Factor
Single phase-100%
3 phase-10%
Gendex med. Freq-10%
Bennett high freq-1%
-both Universal & Bennett advertise as high freq.
-other countries call Universal med freq. (only high freq. If >40 kHz)
-list price the same for Universal & Bennett
-bidding war, Universal will go lower (NOTE: Bennett-welded joints/Universal-soldered joints)
-Bennett- better quality control-checks table material for bubbles & cut them out(bubbles effect exposure)
-ripple factor also affects correction factor (directly proportional)
*read instructions for SuperTech before lab.
# xrays
400 mA
200 mA can create 2x as many photons if double the mA
xray energy (keV)
same kVp (same intersection)
-use amount of mAs to darken/lighten the xray
-if change kVp:
#xrays
90 kVp
80 kVp
xray energy (keV)
-peak fo80 kVp is to left of peak for 90 kVp graph
-so-if increased kVp, also increased # of higher energy photons
-so harder to control darkening or lightening of image
effect of filtration
2mm Al
-more highly filtered beam
-peak shifted slightly to R
4 mm Al
-why-filter out lower energy photons(fewer photons,but higher energy/higher avg. energy)
10
8
6
4
2
5
10
8
6
3 24 = 8 avg.
30= 6 avg
mR=milli Roentgens (measure of output)
mR per mAs
mR per mAs
kV
single phase
high freq.
50
1.13
2.5
60
2.00
4.40
70
3.09
6.00
80
4.05
7.90
90
5.33
10.00
100
6.88
12.50
110
8.50
14.70
120
10.10
17.50
U.S. – single phase systems no longer allowed for mammograms
-single phase already outlawed in some countries
-SO- don’tbuy single phase machines when grad.
Roentgen-got Nobel Prize for discovering xrays
-didn’t want Germans to get his medal, so he dissolved it in nitric acid
Properties of xray
-no mass
-no electrical charge
-travel at speed of light
-can penetrate most matter
-travel in straight line until interact w/matter (then can be scattered)
-if run into a big atom can get absorbed
-capable of making certain chemical compounds flouresce
-capable of exposing photographic film
-can change biologic matter by ionization (messes up DNA)
Edison- at turn of century-calcium tungstate produced brightest light-invented fluorescope
Note- early radiologists discovered early radiation produced diseases (cancer,thyroid,etc.)
-baggage checks-hard on film (heavy ionizers)
Xrays
-part of electromagnetic spectrum
-avg. wavelength of 10 to the minus ninth cm
-avg. freq of 10 th the 18th hertz
-avg. energy of 60,000 eV
-EM spectrum includes-IR, visable light, microwaves, UV, radio waves, TV waves
Xray quantity
-# of xray photons in an exposure beam
-quantity = output intensity = radiation exposure
-measured in roentgens ® or mR
-international community uses Gray (Gy) (pt. Dose) Sieverts (occupational)
-US diagnostic xray- 1 rad=1 rem = 1R (rad= radiation absorbed dose, rem=radiation equivalent for man)
-final measure is in terms of mR/mAs
-70 kVp is usually 3-6 mR/mAs
-mAs- quantity directly proportional
-kVp-15% rule (16-20%)
-affects both # of photons and their average energy
-increase in kVp by 15% must be balanced by a 50% decrease in mAs
-conversely, a decrease in kVp by 15% must be balanced by a doubling of mAs
-result, in either case, are two films of equivalent average density but a change in contrast
-if increase kVp, will darken film, so need to decrease mAs to compensate
-contrast- amount of difference (ex- black vs white)
SuperTech
-do not leave it in a closed car
-70kVp gives reasonable contrast in C spine
-80kVp gives reasonable contrast in T spine
-90kVp gives reasonable contrast in L spine
-80 for obliques & 90 for lateral views
lower kVp setting--more black & white
higher kVp settingless contrast
morbidly obese people-takes more kVp-hard on machine, could damage it
distance
inverse square law
-to maintain the density (photons/in squared) of the film, if FFD is increase 100%,
you need to quadruple the mAs
-conversely, if you cut the FFD by 50%, you would need ¼ the mAs
-if you increased distance by 50% you would double the mAs
density translates to dose but at 80” you get a sharper film (not as magnified)
-do not want to take standing xrays where have to expose for more than 1 sec.
-if calculated out to >1 sec.,revise your parameters (ex. MAs, distance.)
formula
I(1) = D(2)
I(2) D(1)
2
need to know 3 variables to solve for the other one.
Xray quality- refers to penetrating power of the beam.
-hard vs soft xrays
-hard xrays have higher kVp values
-soft xrays have lower kVp values (more damaging because get absorbed by soft tissues
because can’t penetrate as well)
-measured by half value layers (HVL)
-the thickness of an absorbing maaterial necessary to increase intensity by ½ of its
original value (ex- lead, concrete, aluminum, etc.)
-useful if trying to duplicate experiments.
Factors affecting quality
-kVp
-filtration(inherent, added, compensating)
-inherent to construction of tube-glass, oil, plug (plastic)
-added to meet safety standards
-compensating- to adjust for size of different body parts
Filters- ($500)- help you produce higher quality films for your practice
5 Interactions
-Classical scattering
-Compton effect
-photoelectric effect
-pair production
-photodisintergration (the last two occur at high energies)
Classical scattering
-aka coherent or Thompson scattering
-between low energy photons & atoms
-photon does minimal change of direction w/o loss of energy
-filter out most of these before leave tube
-no ionization
-most scatter forward
-may contribute to film fogging (but not our biggest problem)
Compton effect
-between moderate energy xray photons & an outer shell electron ( in pt., bucky, etc.)
-photon changes direction, loses energy & ionizes atom, creating a Compton effect
X-ray Fun.
5/20/98
-have to adjust accommodation for angulation and distance from tube.
-common mistake-order rails too short-want tubes to go closer than 40”
to allow for effects of tube tilt(which effectively lengthens the distance).
Wall Chart
40”
-4
72”
-1/2
{TCF Values}
ex.-30 degree tube tilt makes a 40” distance effectively 46”
{this leads to a decrease in intensity of image}
-do not see a significant intensity difference for 5-10 degree tilt{1-2 inches difference}.
-do see a significant intensity difference at 15 degrees.
Differential Absorption
-Compton scattered xrays contribute no useful information.
Compton Effect
-between moderate energy xray photons and an outer shell electron.
-xray photon changes direction, loses energy, ionizes atom creating a Compton effect.
{electron binding energies involved}
-scattered photon may ionize another atom{leave at the speed of light, 1 photon can do multiple
ionizations}
-may cause backscatter{180 degrees}{why operator stands behind barrier}
-adds to film fog {layer of grayness}
-increases with increaseing kVp
{note-fat is more easily penetrated than water or bone, so don’t ned to crank up the kVp for an
obease person}
Photoelectric Effect
-between moderate energy xray photons and an inner shell electron.
-photon loses all of its energy, ionizes the atom creating a photoelectron {characteristic electron}
{pt. briefly becomes an xray generator}
-produces characteristic xrays {secondary radiation} in the object being xrayed.
-secondary xrays behave like scattered xrays.
Differential Absorption
-Compton scattered xrays contribute no useful information{ex- rib reflection doesn’t add to spinal
info}.
-adds radiographic density, results in film fog {“plus”density}
-structures that absorb a great amount of xray are radiopaque{show up white on xray} ex. - outer
bone.
-structures that allow xrays to pass through are radiolucent {ex.-soft tissue, air spaces}
-the main difference is the atomic # of the structures.
-generally <5% of xrays that hit the pt. reach the film.
-less than ½ of those interact w/film to form an image.
-therefore approx. 1% of xrays emitted from the tube reaches the film.
-maximal DA results from lower kVp values[-kVp is tied to contrast, mAs is tied to density]
{more contrast at lower kVp, but may not show all the structures}
-but as kVp is lowered, pt. dose increases{pt. pays for contrast-healthwise}
[note-some states regulate this more tightly than MO does {ex. Il., Ca.}]
-at lower energies{kVp}, the percentage of photoelectric interactions increases{relativ to Compton}
at 40kVp, ~ equal
60kVp, more Compton
{Logan- ~ 85% Compton, 15% photoelectric}
-to image small differences in soft tissue {renal stones} use low kVp technique {for maximal
differential absorption} note-if pt. says he can’t find a way to decrease the pain, the cause is
probably not biomechanical.
-ex.-renal stones- take abdominal pictures at 60 kVp {instead of higher}
-cracked ribs-hard to find
[-take proper rib series {3 views}, put sore side closest to film, 2 oblique views, pt. can point to
exact
spot]
-if radiating pain down arm-need oblique views of neck so can see size of foramen.
-You can “see” 4 things radiographically.
*Air
*Fat-larger atoms, so absorb more xrays-looks lighter than air, darker than water.
*Water
*Metal
-water density- kidney, etc.
-have to create different densities to tell water from water {ex. Pneumonia xrays -hard to tell lung
from
heart}
-the interaction of xrays & tissue is proportional to the density {specific gravity} of the tissue.
-attenuation is the reduction in the # of xrays as they penetrate matter. Xrays are attenuated
exponentially.
Beam Restriction
-2 types of photons interact with the film to form image : those which don’t interact and Compton
scatter
xrays.
-remnant xrays- photons that exit pt. and interact w/the film.
-Collimation reduces pt. dose by 1} limiting the volume if tissue irradiated & 2} reducing the
amount of
scatter {also reduces fogging}.
-federal law- xray beam shall not be larger than the film being exposed.
Factors affecting scatter radiation
-as kVp increases, the relative # of Compton interactions increases.
-in general, high {optimal} kVp technique is preferred to low kVp technique due to pt. dose
considerations.
-field size- as area of beam enlarges, scatter increases. Seen more on small film sizes.
-pt. thickness, the thicker the part, the more scatter. Pt. thickness is under your control.{Deciding
to
perform lumbar spine & abdominal films in the recumbent vs upright positions.}Compression
may also be
used. {compression band should appear as part of room drawing. $50-200}
-xray tables- useful for paraplegics, babies, broken legs, etc.
Control of scatter radiation
-use beam reduction & grids
-beam restriction
-aperture diaphragm
-cones or cylinders
-variable aperture collimator
-aperture diaphragms are generally not suitable for general practice.
-cones used primarily by dentists
-general practice requires variable aperture collimator.
-variable aperture collimators {positive beam limitation}
-off-focus radiation may be decreased by a first stage entrance shuttering device.{ off -focus
radiation
is why gonad shields are a good idea even when doing an xray of the neck}
-2
stage collimator shutter leaves are made of lead { at least 3 mm thick}, work in pairs,
independently,
yielding square or rectangular fields which compliment the film size being used.
-light localization by lamp & mirror{ place rheostat on xray room lights, collimator bulbs are
expensive,
handle with tissue when installing or their life will be shortened and crack.
-light must coincide with the xray beam. Can get bumped & get out of adjustment.
-by law- need to collimate on 3 sides {white border}- esp. for females.
-open mouth xrays-limit to 3”-4” tall and cheek to cheek
-if equipment properly installed and maintained, the resulting film will show evidence of 4 sides of
collimation.
-collimation adds ~ 1mm of aluminum filtration equivalent.
X-ray Fun. Lab.
5/21/98
Extremities
-thick part of arm goes at cathode end.
-collimate the beam
-protect pt. with lead apron
1}turn on machine & console {all except compressor}
2}measure part to be xrayed
3}calculate mAs & set console {if <12cm, use NB}
4}position part – thick part at cathode end {stronger part of beam}
-centered at beam
-collimated to decrease area exposed
-machine at 40” from table
different room- diff correction factor, so have to recalculate the Mas
big room is single phase {TCF = -2}
end room is full wave therefore more exposure at same mAs. {TCF = -4}