view web only data 78 KB
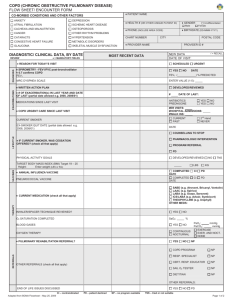
advertisement

1 Online only Supplement Increased CCL5 and CXCL7 chemokine expression is associated with neutrophil activation in severe stable COPD Antonino Di Stefano, PhD1*, Gaetano Caramori, MD2*, Isabella Gnemmi1, Marco Contoli, MD2, Laura Bistrot PhD2, Armando Capelli, MD1, Fabio LM Ricciardolo, MD3, Francesca Magno, PhD1, Silvestro Ennio D’Anna, MD4, Andrea Zanini, MD1, Marco Carbone, PhD1, Federica Sabatini, PhD5, Cesare Usai, PhD6, Paola Brun, PhD7, Kian Fan Chung8, Peter J Barnes8, Alberto Papi, MD2, Ian Adcock, PhD8, Bruno Balbi, MD1. *Both Authors contributed equally to this work. Author for correspondence: Antonino Di Stefano, PhD Fondazione S. Maugeri, IRCCS Laboratorio di Citoimmunopatologia Apparato Cardio Respiratorio Via per Revislate 13, 28010 Veruno (NO), Italy Phone: +39 0322 884711 Fax: +39 0322 884776 Email: antonino.distefano@fsm.it 1 2 Introduction Pathological studies performed in patients with COPD show that inflammation occurs in the central, peripheral airways (bronchioles) and lung parenchyma.E1-E4 Some of these studies have emphasized the potential role of several inflammatory cells in the pathogenesis of COPD including alveolar macrophages, T-lymphocytes and CD8+ cells. In contrast, fewer studies have investigated neutrophil granulocytes, despite increased numbers being reported in bronchial mucosa, particularlyof severe COPD patients,E4-E6 in small airways,E3 bronchoalveolar lavage (BAL) fluidE7,E8 and in sputum samples.E9 Furthermore, the need for pathologic investigations in patients with more severe COPD has been underlined.E3 However, the molecular mechanisms responsible for this neutrophilia, particularly that seen in the tissue,are not fully clarified. Neutrophil prevalence may result from increased chemotaxis, increased neutrophil adhesion to collagens or other components of the extracellular matrix or to prolonged survival.E10 Recently, a partial loss of the chemotactic response to CXCL8 and Nformyl-methionyl-leucyl-phenylalanine (fMLP) has been reported for sputum neutrophils from stable COPD patients, suggesting a hypo-functional status of these cells after migration and residence in the bronchial lumen.E11 This further emphasises the need to examine the functional status of neutrophils within the airways of patients with COPD. Several chemokines of the CXC and CC family are involved in neutrophil chemotaxis. E12-E14 Cysteine-X-cysteine chemokine ligand CXCL1 [growth-related oncogene α (GRO-α,)] and CXCL5 [epithelial-neutrophil activating peptide 78 (ENA-78)] may be involved in neutrophilic inflammation and can both bind to and activate CXCR2. CXCL1 expression is increased in sputum from patients with COPD compared to non smokers and healthy smokers.E15 CXCL5 is derived predominantly from bronchial epithelial cellsE16 and BAL CXCL5 concentrations are enhanced in COPD patients compared to normal subjects.E17 However, there is no difference in CXCL5 levels between patients 2 3 with emphysema and normal smokers.E17 Finally, a marked increase in CXCL5 gene expression has been reported in bronchial biopsies during exacerbations of mild/moderate COPD.E18 In humans, CXCL6 [granulocyte chemotactic protein-2 (GCP-2)] complements the activity of CXCL8 (IL-8) and induces neutrophil chemotaxis and activationE19 whereas lung macrophages release CXCL6 after lipopolysaccharide (LPS) stimulation.E20 However, there is a complete absence of data concerning CXCL6 expression in COPD. CXCL7 [neutrophil-activating peptide-2 (NAP-2)] is also chemotactic for neutrophils and is released as an inactive precursor by platelets.E21 Increased protease activity within the lung by enzymes such as cathepsin-G can activate CXCL7 and contribute to its chemotactic activity.E13,E21 In addition, PBMCs from COPD patients have an increased chemotactic response towards CXCL7.E22 CXCL8 activates neutrophils via a specific low-affinity G-protein receptor (CXCR1), coupled to cell activation and degranulation, and via a high-affinity receptor (CXCR2) shared with other members of the CXC family.E23 CXCL8 levels are elevated in the sputum of patients with COPD and are correlated with disease severity E24 and increase further during COPD exacerbations.E18,E25 The CCR1 ligand CCL5 (RANTES; released by activated normal T cells expressed and secreted) is significantly increased in the sputum of patients with stable COPD when compared with non-smokers but not with smokers with normal lung function and its expression correlates with sputum neutrophilia.E26 Sputum CCL5 concentration is also increased in COPD patients during exacerbations.E27 In addition, LPS stimulated cultured lung explants from COPD patients showed increased release of CCL5 compared with explants from control smokers.E28 The leukocyte M2 integrin (also known as Mac-1, complement receptor type 3 (CR3), and CD11b/CD18) functions as an adhesion molecule facilitating diapedesis. Overexpression of CD11b has been reported in blood neutrophilsE29,E30 and sputumE31 of stable COPD patients compared to control subjects. CD62E (E-selectin), the major ligand of CD11b, is increased in bronchial biopsies of patients 3 4 with stable COPD,E32 but the expression of CD11b on neutrophils in the bronchial mucosa of patients with stable COPD is still unknown. CD44 belongs to the family of hyaluronan-binding type I transmembrane glycoproteins receptors. Hyaluronan, an extracellular matrix component, is the main ligand for CD44.E33 Neutrophils cocultured with human primary bronchial epithelial cells and GM-CSF up-regulate CD44.E34 The expression of CD44 on neutrophils in the bronchial mucosa of patients with stable COPD has not been previously reported. Methods Subjects All subjects were recruited from the Section of Respiratory Medicine of the Fondazione Salvatore Maugeri (Veruno, Italy). We examined bronchial biopsies from 49 subjects by immunohistochemistry; 13 subjects were current or ex smokers with normal lung function, 25 had a clinical diagnosis of COPD and 11 were never-smokers with normal lung function (Table 1). The severity of the airflow obstruction was staged using GOLD criteria.E1 All former smokers had stopped smoking for at least one year. COPD and chronic bronchitis were respectively defined, according to international guidelines, as: the presence of post-bronchodilator forced expiratory volume in one second (FEV1)/ forced vital capacity (FVC) ratio <70% or the presence of cough and sputum production for at least 3 months in each of two consecutive years.E1 All COPD patients were stable with no previous exacerbation in the 6 months before bronchoscopy. None of the subjects was treated with theophylline, antibiotics, antioxidants, mucolytics, and/or glucocorticoids in the month prior to the bronchial biopsy. The study conformed to the Declaration of Helsinki, Ethics Consent was obtained, bronchial biopsies 4 5 were performed according to the local Ethics Committee Guidelines, and informed consent was obtained from each subject. Lung function tests and volumes Pulmonary function tests were performed as previously describedE6 according to published guidelines. Pulmonary function tests included measurements of FEV1 and FEV1/FVC under baseline conditions in all the subjects examined (6200 Autobox Pulmonary Function Laboratory; Sensormedics Corp., Yorba Linda, CA). Predicted values for the different measures were those from the Communité Européenne du Carbon et de l’Acier. In order to assess the reversibility of airflow obstruction and postbronchodilator functional values, the FEV1 and FEV1/FVC% measurements in the groups of subjects with FEV1/FVC%70% pre-bronchodilator was repeated 20 min after the inhalation of 0.4 mg of salbutamol. Fiberoptic bronchoscopy, collection and processing of bronchial biopsies Subjects attended the bronchoscopy suite at 8.30 am after having fasted from midnight and were pretreated with atropine (0.6 mg IV) and midazolam (5-10 mg IV). Oxygen (3 l/min) was administered via nasal prongs throughout the procedure and oxygen saturation was monitored with a digital oximeter. Using local anaesthesia with lidocaine (4%) to the upper airways and larynx, a fiberoptic bronchoscope (Olympus BF10 Key-Med, Southend, UK) was passed through the nasal passages into the trachea. Further lidocaine (2%) was sprayed into the lower airways, and four bronchial biopsy specimens were taken from segmental and subsegmental airways of the right lower and upper lobes using size 19 cupped forceps. Bronchial biopsies for immunohistochemistry and RT-QPCR were gently extracted from the forceps and processed for light microscopy as previously described.E6 Two samples were embedded in Tissue Tek II OCT (Miles Scientific, Naperville, IL), frozen within 15 min in isopentane 5 6 pre-cooled in liquid nitrogen, and stored at –80°C. The best frozen sample was then oriented and 6m thick cryostat sections were cut for immunohistochemical light microscopy analysis and 30m thick cryostat sections were cut for RT-QPCR and processed as described below. Bronchial biopsies for western blot analysis were immediately placed on ice, frozen in liquid nitrogen and processed as described below. Immunohistochemistry Two sections were stained with immunohistochemical methods. The best immunostained section was then selected for quantitative purposes. The following panel of antibodies was used (Table 2). Briefly, after blocking non-specific binding sites using serum derived from the same animal species as the secondary antibody, primary antibodies were applied at optimal dilutions in TRIS-buffered saline (0.15 M saline containing 0.05 M TRIS-hydrochloric acid at pH 7.6) and incubated (1 hr) at room temperature in a humidified chamber. Antibody binding was demonstrated with the use of secondary antibodies anti mouse (Vector, BA 2000), anti rabbit (Vector, BA 1000) or anti goat (Vector, BA 5000) followed by Strept AB Complex/AP (Dako, K0391) and fast-red substrate. Control slides were included in each staining run using human tonsil or nasal polyp as a positive control for all immunostaining performed. For the negative control slides, normal goat or rabbit non-specific immunoglobulins (Santa Cruz Biotechnology) were used at the same protein concentration as the primary antibody. Immunofluorescence staining with confocal microscopy TableE1 shows the clinical details of the subjects used for the confocal microscopy (n=8). Sections were fixed with 4% paraformaldehyde, washed with phosphate buffered saline (PBS) and incubated (1 hour) with PBS containing 5% bovine serum albumin and 5% goat serum. After blocking, 6 7 sections were incubated 1 hour with the primary antibodies diluted 1:50 in PBS containing 5% bovine serum albumin. The following antibodies were used: rabbit anti-human CD11b (sc-28664; Santa Cruz); rabbit anti-human CD44 (sc-7946; Santa Cruz) and mouse antihuman neutrophil elastase (M752; Dako). After washing with PBS, the preparations were incubated for a further 30 min with the appropriate secondary Alexa Fluor 488- or Alexa Fluor 647 conjugated antibodies diluted 1:200 in PBS. Negative controls included irrelevant mouse and rabbit immunoglobulins revealed as for primary antibodies. Slides were mounted using a specific mounting medium (Fluka 10979, Sigma, Italy). Scoring system for immunohistochemistry and confocal microscopy Morphometric measurements were performed with a light microscope (Leitz Biomed, Leica Cambridge, UK) connected to a video recorder linked to a computerised image system (Quantimet 500 Image Processing and Analysis System, Software Qwin V0200B, Leica). Light-microscopic analysis was performed at a magnification of 630x. Immunostained cells were quantified in the area 100 m beneath the epithelial basement membrane in several non-overlapping high power fields until all the available area was covered. The final result, expressed as the number of positive cells per square millimeter, was calculated as the average of all the cellular counts performed in each biopsy. We quantified the immunostained cells with at least a portion of the nucleus seen close to immunopositivity [E35] The immunostaining for all the antigens studied was also scored (range: 0: absence of immunostaining, 1: from 1% until 33% of immunostained cells, 2: from 34% until 66% of immunostained cells, 3: extensive (from 67% to 100%) intense immunostaining) in the intact (constituted by columnar and basal epithelial cells) bronchial epithelium, as previously described.E32 The final result was expressed as the average of all scored fields performed in each biopsy. A mean SD of 0.7000.260 millimeters of epithelium was analyzed in COPD patients and control subjects. 7 8 The slides for confocal microscopy were analyzed using a three-channel Leica TCS SP2 laser scanning confocal microscope. The Leica LCS software package was used for acquisition, storage, and visualization. The quantitative estimation of co-localized proteins was performed calculating the “colocalization coefficients”.E36, E37 Quantification of chemokines and cytokines mRNA levels in bronchial biopsies Table E2 shows the clinical details of the subjects used for the real time RT-PCR (n=31). Total RNA was extracted (Micro RNeasy Kit, Qiagen Milan, Italy) from 30m thick cryostat sections of bronchial biopsies and 1 µg used for cDNA synthesis. cDNA was synthesised using Omniscript RT kit (Qiagen) as per manufacturer’s instructions. Primer pairs for CCL5 (Cat. # QT00090083), CXCL7 (Cat. # QT00001372), CXCL8 (Cat. # QT00000322) were purchased from Qiagen. Quantitative realtime reverse transcriptase-polymerase chain reaction (RT-PCR) was carried out using Sybr-green (QuantiFast Sybr Green PCR kit cat. # 204054 – Qiagen) following the manufacturer’s protocol. At the end of the RT-PCR run a melting curve analysis was carried out to verify that the cycle threshold (Ct) values were based upon a single PCR product (data not shown). Relative levels of cDNAs were established using the Ct methods against the housekeeping gene guanine nucleotide binding protein (G protein) (GNB2L Cat. # QT01156610 – Qiagen). After normalization the value of Ct was subtracted from 45 (total number of RT-PCR cycles), thus higher Ct levels indicate higher mRNA levels. Also relative levels of mRNAs were expressed as the ratio of the Ct value for the gene of interest Ct/housekeeping gene Ct [guanine nucleotide binding protein (G protein) - GNB2L Cat. # QT01156610 from Qiagen]. Western blot analysis for CXCL7, CXCL8 and CCL5 in the bronchial biopsies Table E3 shows the clinical details of the subjects used for the western blotting (n=12). 8 9 Whole cell proteins were extracted from bronchial biopsies as previously described. E6 In brief, frozen bronchial biopsies were resuspended with mechanical disruption in RIPA lysis buffer with a protease inhibitor cocktail immediately frozen to –70 C and thawed after at least 60 minutes. Particulate matter was removed by centrifugation at 12000 x g for 10 min at 4C. Protein concentration was measured in the supernatant by the Bradford method according to the manufacturer’s instructions (Bio-Rad Laboratories, Hemel Hempstead, UK). An equal volume of Laemmli sample buffer 2X concentrate was added to the final volume of the sample. At least 50 g/lane of whole-cell proteins were subjected to a 4-20% SDS-polyacrylamide gel electrophoresis, and transferred to nitrocellulose filters (Hybond-ECL, Amersham Pharmacia Biotech) by blotting. Filters were blocked for 45 minutes at room temperature in Tris-buffered saline (TBS), 0.05% Tween 20, 5% non-fat dry milk. The filters were then incubated with goat anti-human CCL5 (AF-278-NA; from R& D Systems) or goat anti-human CXCL7 (sc19224; from www.scbt.com) or goat-anti human CXCL8 (AF-208-NA; from R & D Systems) for 1h at room temperature in TBS, 0.05% Tween 20, 5% non-fat dry milk at dilution of 1:500at a concentration of 0.1 mg/ml (CCL5 and CXCL8) or 0.2 mg/ml (CXCL7). As positive controls 50 ng of human recombinant CCL5 (278-RN; from R & D Systems), human recombinant CXCL7 (www.peprotech.com; cat 300-14) or human recombinant CXCL8 (hBA-72) (sc-4600; from www.scbt.com) were used. Filters were washed three times in TBS, 0.5% Tween 20 and then incubated for 45 minutes at room temperature with rabbit anti-goat antibody conjugated to horseradish peroxidase (Dako, Ely, UK) in TBS, 0.05% Tween 20, 5% non-fat dry milk, at a dilution of 1:4000. After three further washes in TBS, 0.05% Tween 20 visualization of the immunocomplexes was performed using the ECL as recommended by the manufacturer (Amersham Pharmacia Biotech). As an internal control we reprobed each filter with an anti-human actin antibody (Santa Cruz Biotechnology). The 43kDa (actin) or 8kDa (CCL5 and CXCL8) and 14kDa (CXCL7) bands were quantified using densitometry 9 10 with Grab-It and VisionWorks LS software (UVP, Cambridge, UK) and expressed as a ratio with the corresponding actin optical density value of the same lane. Data analysis Group data were expressed as mean standard error for functional data or median (range) for morphologic data. We tested for a normal distribution for functional data (i.e. FEV1%, FVC, age etc.) and for a non normal distribution for morphologic parameters. Then we applied the analysis of variance (ANOVA) in comparing subgroups of patients and control subjects for functional data. The non parametric Kruskal Wallis test was applied for multiple comparisons, without application of Bonferroni correction, when morphologic data were analysed followed by the Mann-Whitney U test for comparison between groups. The statistical Guide to GraphPad Prism recommends that the Bonferroni correction should not be used when comparing more than 5 variables due to the conservative nature of the test and the subsequent likeliness of missing real differences. We believe that this comparative analysis is of value and represents part of our informative findings. For this reason we applied specific non parametric statistical tests to our data of Table 3 and 4 without including the Bonferroni correction. To verify the degree of association between functional or morphological parameters, in all smokers with and without COPD or in smokers with COPD alone the correlation coefficients between functional-morphological and morphological-morphological data were calculated using the Spearman rank method. Probability values of p<0.05 were considered significant. Data analysis was performed by using the Stat View SE Graphics program (Abacus Concepts Inc., Berkeley, CA-USA). References E1. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. NHLBI/WHO workshop 10 11 report. Bethesda, National Heart, Lung and Blood Institute, April 2001; NIH Publication No 2701:1100. Last update 2008. http://www.goldcopd.com (accessibility verified April 24, 2008). E2. Barnes PJ. Chronic obstructive pulmonary disease. N Engl J Med 2000;343:269-80. E3. Hogg JC, Chu F, Utokaparch S, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:2645-53. E4. Di Stefano A, Caramori G, Ricciardolo FLM, et al. Cellular and molecular mechanisms in chronic obstructive pulmonary disease: an overview. Clin Exp Allergy 2004;34:1156-67. E5. Di Stefano A, Capelli A, Lusuardi M, et al. Severity of airflow limitation is associated with severity of airway inflammation in smokers. Am J Respir Crit Care Med 1998;158:1277-85. E6. Ricciardolo FLM, Caramori G, Ito K, et al. Nitrosative Stress in the Bronchial Mucosa of Severe Chronic Obstructive Pulmonary Disease. J Allergy Clin Immunol 2005;116:1028-35. E7. Hodge SJ, Hodge GL, Holmes M, et al. Flow cytometric characterization of cell populations in bronchoalveolar lavage and bronchial brushings from patients with chronic obstructive pulmonary disease. Cytometry B Clin Cytom. 2004;61:27-34. E8. Thompson AB, Daughton D, Robbins RA, et al. Intraluminal airway inflammation in chronic bronchitis. Characterization and correlation with clinical parameters. Am Rev Respir Dis 1989;140:1527-37. E9. Fujimoto K, Yasuo M, Urushibata K, et al. Airway inflammation during stable and acutely exacerbated chronic obstructive pulmonary disease. Eur Respir J 2005;25:640-6. E10. Barnes PJ. New molecular targets for the treatment of neutrophilic diseases. J Allergy Clin Immnol 2007;119:1055-62. E11. Yoshikawa T, Dent G, Ward J, et al. Impaired neutrophil chemotaxis in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2007;175:473-9. 11 12 E12. Hay DW, Sarau HM. Interleukin-8 receptor antagonists in pulmonary diseases, Curr Opin Pharmacol 2001;1:242–7. E13. Donnelly LE, Barnes PJ. Chemokine receptors as therapeutic targets in chronic obstructive pulmonary disease. Trends Pharmacol Sci 2006;27:546–53. E14. Viola A, Luster AD. Chemokines and Their Receptors: Drug Targets in Immunity and Inflammation. Annu Rev Pharmacol Toxicol 2008;48:171-97. E15. Traves SL, Culpitt S, Russell REK, et al. Elevated levels of the chemokines GRO-α and MCP-1 in sputum samples from COPD patients. Thorax 2002;57:590–5. E16. Imaizumi T, Albertine KH, Jicha DL, et al. Human endothelial cells synthesize ENA-78: relationship to IL-8 and to signaling of PMN adhesion. Am J Respir Cell Mol Biol 1997;17:181–92. E17. Tanino M, Betsuyaku T, Takeyabu K, et al. Increased levels of interleukin-8 in BAL fluid from smokers susceptible to pulmonary emphysema. Thorax 2002;57:405–11. E18. Qiu Y, Zhu J, Bandi V, et al. Biopsy neutrophilia, chemokine and receptor gene expression in severe exacerbations of COPD. Am J Respir Crit Care Med 2003;168: 968–75. E19. Van Damme J, Wuyts A, Froyen G, et al. Granulocyte chemotactic protein-2 and related CXC chemokines: from gene regulation to receptor usage. J Leukoc Biol 1997;62:563-9. E20. Wuyts A, Struyf S, Gijsbers K, et al. The CXC chemokine GCP-2/CXCL6 is predominantly induced in mesenchymal cells by interleukin-1beta and is down-regulated by interferon-gamma: comparison with interleukin-8/CXCL8. Lab Invest 2003;83:23-34. E21. Walz A. Generation and properties of neutrophil-activating peptide 2. Cytokines 1992;4:77–95. E22. Traves SL, Smith SJ, Barnes PJ, et al. Specific CXC but not CC chemokines cause elevated monocyte migration in COPD: a role for CXCR2. J Leukoc Biol 2004;76:441-50. E23. Rossi D, Zlotnik A. The biology of chemokines and their receptors, Annu Rev Immunol 2000;18:217–42. 12 13 E24. Yamamoto C, Yoneda T, Yoshikawa M, et al. Airway inflammation in COPD assessed by sputum levels of interleukin-8. Chest 1997;112:505–10. E25. Gompertz S, O'Brien C, Bayley DL, et al. Changes in bronchial inflammation during acute exacerbations of chronic bronchitis. Eur Respir J 2001;17:1112–9. E26. Costa C, Rufino R, Traves SL, et al. CXCR3 and CCR5 Chemokines in induced sputum from patients with COPD. Chest 2008;133:26-33. E27. Fujimoto K, Yasuo M, Urushibata K, et al. Airway inflammation during stable and acutely exacerbated chronic obstructive pulmonary disease. Eur Respir J 2005;25: 640–6. E28. Smyth LJC, Starkey C, Gordon FS, et al. CD8 chemokine receptors in chronic obstructive pulmonary disease. Clin and Exp Immunology 2008;154:56-63. E29. Noquera A, Busquets X, Sauleda J, et al. Expression of adhesion molecules and G proteins in circulating neutrophils in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;158:1664-8. E30. Yamagata T, Sugiura H, Yokoyama T, et al. Overexpression of CD11b and CXCR1 on circulating neutrophils. Its possible role in COPD. Chest 2007;132:890-9. E31. Pignatti P, Moscato G, Casarini S, et al. Downmodulation of CXCL8/IL-8 receptors on neutrophils after recruitment in the airways. J Allergy Clin Immunol 2005;115:88-94. E32. Di Stefano A, Maestrelli P, Roggeri A, et al. Upregulation of adhesion molecules in the bronchial mucosa of subjects with obstructive chronic bronchitis. Am J Respir Crit Care Med 1994;149:803-10. E33. Yasuda M, Nakano K, Yasumoto K, et al. CD44: functional relevance to inflammation and malignancy. Histol Histopathol. 2002;17:945-50. E34. Yousefi S, Cooper PR, Mueck B, et al. cDNA representational difference analysis of human neutrophils stimulated by GM-CSF. Biochem Biophys Res Commun 2000;277:401-9. 13 14 E35. Jeffery P, Holgate S and Wenzel S. Methods for the assessment of endobronchial biopsies in clinical research. Am J Respir Crit Care Med 2003;168:S1-S17. E36. Gonzalez R.C., Wintz P. Digital Image Processing, 2nd edn., Addison Wesley Publication Company, Mass. USA 1987.;Costes S.V., Daelemans D., Cho E.H., Dobbin Z., Pavlakis G., Lockett S. Automatic and quantitative measurement of protein-protein colocalization in live cells. Biophysical Journal 2004;86:3993-4000. E37. Manders E.M.M., Verbeek F.J., Aten J.A. Measurement of co-localization of objects in dualcolour confocal images. J Microscopy 1993;169:375-438. 14 15 E-Tables Table E1. Characteristics of subjects for the confocal immunohistochemical study Subjects n Age Sex Smoking History Pack-years FEV1 Pre M/F (ex/current) % pred Smokers with normal lung function Moderate/severe COPD 4 563 3/1 0/4 383 955 4 654 4/0 3/1 356 345 FEV1 FEV1/FVC Post % % pred ND 834 406 455 Data are presented as meanSE. COPD: chronic obstructive pulmonary disease; M: male; F: female; FEV1: forced expiratory volume in one second; FVC: forced vital capacity. ANOVA, p<0.0001 significantly different from smokers with normal lung function; ND=not determined. For COPD patients FEV1/FVC% are post-bronchodilator values. 15 16 Table E2. Characteristics of subjects used for the RT-QPCR study Subjects n Age Sex M/F Smokers with normal lung function Mild/Moderate COPD 7 58.7±4.2 73.3±1.7^ 15 67.2±2.0 Severe/very-severe COPD 9 5/2 Smoking History Pack-years (Ex/current) 45.7±12 (0/7) FEV1 Pre % pred FEV1 Post % pred FEV1/FVC % 95.43 ±5.1 ND 7/2 44.2±6.7 (4/5) 65.78±3.3 67.33±4.0 56.06±3.0 15/0 60.9±11.1 (12/3) 37.±1.6 40.73±2.0 46.5±2.3§ 80.0±2.1 Data are presented as mean SE. COPD: chronic obstructive pulmonary disease; M: male; F: female; FEV1: forced expiratory volume in one second; FVC: forced vital capacity. ANOVA, p<0.0001 significantly different from smokers with normal lung function or from mild/moderate COPD; § p=0.0049 significantly different from mild/moderate COPD; ^p=0.048 significantly different from smokers with normal lung function. ND= not determined. For COPD patients FEV1/FVC% are postbronchodilator values. 16 17 Table E3. Characteristics of the subjects used for the western blotting study Subjects Smokers with normal lung function Moderate/severe COPD n 5 7 Age Sex 64.5±4.3 5/0 592 7/0 SmokingHistory pack-years (ex/current) 62±14 (2/3) FEV1 pre (%) FEV1 post (%) 96.2 ±3.7 ND 7015 (2/5) 414 435 FEV1/FVC % 82±3.4 433 Data are presented as mean SE. COPD: chronic obstructive pulmonary disease; M: male; F: female; FEV1: forced expiratory volume in one second; FVC: forced vital capacity. ANOVA, p<0.0001 significantly different from smokers with normal lung function; ND=not determined. For COPD patients FEV1/FVC% are post-bronchodilator values. 17