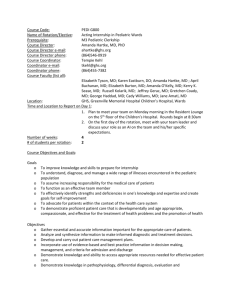
Trach Discharge & Training
advertisement

Benjamin, B., & Curley, J.W.A. (1990). Infant tracheotomy, endoscopy and decannulation. International Journal of Pediatric Otorhinolaryngology, 20, 113 121. A retrospective review of 73 infants (24 months of age or less) who underwent tracheotomy over a ten-year period (1978-1987). Nineteen of the infants were premature. Author's focus is on decannulation problems and endoscopic evaluation in patients under 24 months of age. Results: On completion of study, 49 patients had been successfully decannulated, 15 patients still had tracheotomies, three patients were lost to follow/up, and six patients had died of causes unrelated to the tracheotomy. Authors conclude tracheotomy can be a safe procedure in this age group for both the short and the long term. Principal author: Ear, Nose and Throat Department, Royal Alexandra Hospital for Children, Sydney, Australia. Discharge Planning and Teaching Barnes, L.P. (1992). Tracheostomy care: Preparing parents for discharge. Maternal Child Nursing, 17, 293. Commentary on guidelines to ready parents for discharge of children with tracheostomies. Principal author: Child Health Education Center, Knoxville, TN Buzz-Kelly, L., & Gordin,P. (1993). Teaching CPR to parents of children with tracheostomies. Maternal Child Nursing, 18, 158-163. A review of the issues regarding lay emergency management for children with trachs and a proposed curriculum for training parents in such management. The proposed curriculum content includes: a description of risks for obstructed airways for trachs, necessary emergency equipment, psychosocial aspects of teaching parents of children with trachs, and adaptations of basic infant/child CPR for children with trachs. Features: A trach CPR algorithm to instruct parents in performance of CPR on a child with a trach, a trouble-shooting guide for emergency tube changes, and a comparison of resuscitation bags. Principal author: Children's Hospital of Philadelphia, PA. Dougherty, J.M., Parrish, J.M., & Hock-Long, L. (1995). Community and home care: Part 1: Developing a competency-based curriculum for tracheostomy and ventilator care. Pediatric Nursing, 21 (6), 581-584. Part 1: Authors surveyed 107 families with ventilator-assisted children to ascertain the adequacy of community providers and caretakers' skills. Authors subsequently designed and pilot-tested a skills-focused curriculum to meet needs determined by the survey. Part 2 continues with description of initial field test of the curriculum. Principal author: Children's Seashore House, Philadelphia, PA. Dougherty, J.M., Parrish, J.M., Parra, M., Kinney, Z.A., & Kandrak, G. (1996). Community and home care: Part 2: Using a competency-based curriculum to train experienced nurses in ventilator care. Pediatric Nursing, 22 (1), 47-50. Part 2. A description of the initial field test to validate effectiveness, feasibility and replicability of a training curriculum for nurses involved in home care of ventilator-dependent children. (Curriculum development is described in Part 1.) Baseline data were obtained to assess specific learner needs. Training proceeded in a step-wise fashion covering skill domains which were reassessed at the end of training. One-to-one remedial training was available as needed. After fieldtesting, the curriculum was offered to home care agency nurses and coordinators with 100 nurses responding. Course structure and format are presented. Principal author: Children's Seashore House, Philadelphia, PA. Senders, C.W., Muntz, H.R., & Schweiss, D. (1991). Physician survey on the care of children with tracheotomy. American Journal of Otolaryngology, 12, 48-50. Results of a survey of practicing pediatric otolaryngologists in the United States, Canada and England regarding the range of care provided for children with tracheotomies. Respondents revealed commonalities in 1) timing of first tube change, 2) use of ICU postoperatively, 3) parental training for home care, 4) follow up, and 5) use of a home care team. Home monitoring after discharge appeared to be inconsistently practiced at the time of this survey. Principal author: Dept. of Otolaryngology, University of California Davis Medical Center, Sacramento, CA. Senders, C.W., Muntz, H.R., & Schweiss, D. (1991). Physician survey on the care of children with tracheotomy. American Journal of Otolaryngology, 12, 48-50. Results of a survey of practicing pediatric otolaryngologists in the United States, Canada and England regarding the range of care provided for children with tracheotomies. Respondents revealed commonalities in 1) timing of first tube change, 2) use of ICU postoperatively, 3) parental training for home care, 4) follow up, and 5) use of a home care team. Home monitoring after discharge appeared to be inconsistently practiced at the time of this survey. Principal author: Dept. of Otolaryngology, University of California Davis Medical Center, Sacramento, CA. Dougherty, J.M., Parrish, J.M., & Hock-Long, L. (1995). Community and home care: Part 1: Developing a competency-based curriculum for tracheostomy and ventilator care. Pediatric Nursing, 21 (6), 581-584. Part 1: Authors surveyed 107 families with ventilator-assisted children to ascertain the adequacy of community providers and caretakers' skills. Authors subsequently designed and pilot-tested a skills-focused curriculum to meet needs determined by the survey. Part 2 continues with description of initial field test of the curriculum. Principal author: Children's Seashore House, Philadelphia, PA. Dougherty, J.M., Parrish, J.M., Parra, M., Kinney, Z.A., & Kandrak, G. (1996). Community and home care: Part 2: Using a competency-based curriculum to train experienced nurses in ventilator care. Pediatric Nursing, 22 (1), 47-50. Part 2. A description of the initial field test to validate effectiveness, feasibility and replicability of a training curriculum for nurses involved in home care of ventilator-dependent children. (Curriculum development is described in Part 1.) Baseline data were obtained to assess specific learner needs. Training proceeded in a step-wise fashion covering skill domains which were reassessed at the end of training. One-to-one remedial training was available as needed. After fieldtesting, the curriculum was offered to home care agency nurses and coordinators with 100 nurses responding. Course structure and format are presented. Principal author: Children's Seashore House, Philadelphia, PA. Complications: The complication rate of pediatric tracheotomy appears to be around 40 %. Complications include operative and postoperative, both early and late. Operative complications include hemorrhage, air entry, anatomic damage, tracheotomy tube problems, respiratory drive cessation and pulmonary edema. Postoperative difficulties can include hemorrhage, air entry, tracheal lesions, tracheostomy tube problems, infection, swallowing difficulties, and aphonia. Wetmore et al(5) review pediatric tracheotomy over a ten year period. They found that accidental decannulation (24%) was the most common early postoperative complication followed by pneumonia (20%), pneumothorax (9%), subcutaneous air (9%) and obstructed tube(7%). As far as late complications, they found that a tracheo-cutaneous fistula was most common (19%) followed by accidental decannulation (18%), tracheal granuloma (14%), stomal granulation (11%), and obstructed tube (10%). TITLE: PEDIATRIC TRACHEOTOMY SOURCE: UTMB Dept. of Otolaryngology Grand Rounds DATE: June 4, 1997 RESIDENT PHYSICIAN: Deborah P. Wilson, M.D. FACULTY: Ronald W. Deskin, M.D. SERIES EDITOR: Francis B. Quinn, Jr., M.D., F.A.C.S. "This material was prepared by physicians in partial fulfillment of educational requirements established for Continuing Postgraduate Medical Education activities and was not intended for clinical use in its present form. It was prepared for the purpose of stimulating group discussion in a interactive computer mediated conference setting. No warranties, either express or implied, are made with respect to its accuracy, completeness, or timeliness. The material does not necessarily reflect the current or past opinions of subscribers or other professionals and should not be used for purposes of diagnosis or treatment without consulting appropriate literature sources and informed professional opinion." Introduction: Tracheotomy is a serious procedure in infants and children. It is well established that the morbidity and mortality rate of tracheotomy in the pediatric population is twice that of adults. This presentation serves to provide an overview of the current technique and management of pediatric tracheotomies. Brief History: The first tracheotomy was performed in Rome in second century B.C. Antyllus, in second century A.D., further refined the technique by suggesting that the trachea be divided at the third and fourth tracheal rings using a transverse incision. In 1620, Habicot performed the first pediatric tracheotomy. The procedure was performed on a sixteen year old boy who had swallowed a bag of gold in an attempt to keep the gold from being stolen. The bag became lodged in the boy's esophagus and obstructed his trachea. After Habicot performed the tracheotomy, he manipulated the bag of gold so that it would pass. It was eventually recovered per rectum. In 1825, Bretonneu reported a successful tracheotomy on a five year old girl with diphtheria. Afterwards, Trousseau reported performing tracheotomies on over 200 children with diphtheria. He also stressed the importance of post-operative care. Throughout the 1800's, tracheotomies became increasingly popular but the mortality and morbidity of the procedure remained high. In the early 1900's, Chevalier Jackson standardized the procedure and demonstrated that the mortality rate was significantly reduced if the procedure was performed properly and careful attention was paid to post-operative care.(1) Indications: Not until the 1900's was tracheotomy performed for any other reason than upper airway obstruction. Today, there are three basic indications for a tracheotomy in a pediatric patient: 1) upper airway obstruction 2) assisted ventilation 3) pulmonary toilet. Controversy persists on whether to perform a tracheotomy or endotracheal intubation and when the intervention should take place. A number of factors must be considered. These include the predicted course of the patient's illness, the skill of the physician performing the procedure, and the personnel and equipment available. With the pediatric patient, an additional factor to consider is concerned and frightened parents. Obviously, each case must be individualized. Some guidelines to the decision making process includes general factors such as those suggested by Stool and Eavey(1); tissue, time and team. Tissue refers to the age of the patient and etiology of the disease process. Younger children have smaller airways, therefore less edema is required to lead to obstruction. In addition, younger children tire more easily than older children or adults. Time refers to the course of the disease process. Does it appear or is it known to be rapidly or slowly progressive? The time factor also includes the condition of the child at presentation. If the child is stuporous, retracting and cyanotic then the decision to intervene is obvious. The team factor refers to the experience of the physician and personnel available to carry out the procedure. Douglas et al(2) developed a mnemonic TRACHS to help with the decision making process (see below). The goal is an orderly, well-timed procedure with an experienced surgeon and the best personnel and equipment possible. Pediatric Tracheotomy Tubes: Fabricus in 1600 suggested the use of a cannula with tracheotomy. The initial design was short and straight. Martin in 1730 recommended the use of an inner cannula on the tracheotomy tube. There are several different types of tracheotomy tubes available. The ideal tube should be soft, pliable, easy to clean and maintain, and available in a variety of sizes and length. The choice of type and size of the tracheotomy tube should be based on the indication for the tracheotomy. If the tracheotomy is performed for upper airway obstruction, the tube should not fill the entire tracheal lumen. If the indication for tracheotomy is assisted ventilation, the tube should fill more of the tracheal lumen to prevent excessive airleak. In smaller children, cuffed tracheotomy tubes are usually not necessary. In older children, a low-pressure cuffed tube may be required to achieve an adequate seal. The choice of tube size should be determined at the time of surgery by visualizing the size of the child's tracheal lumen. There are a few predictors of the appropriate tube size. These include standardized normals based on the child's age, the size of the endotracheal tube if one is already in place, or the size of rigid bronchoscope if one was used to examine the airway. The critical measurement of tracheotomy tube size is the diameter of the tube. The external diameter determines the size that can be inserted but, more importantly, the inner diameter determines the airway size. Mullins et al(3) studied the airway flow characteristics of tracheotomy tubes and their effect on the work of breathing. They used neonatal, pediatric and adult Shiley tracheotomy tubes. Mullins' group confirmed previous findings that the work of breathing decreases as the inner diameter of the tube increases. They compared the pediatric tube 00 with the neonatal tube 00. Both tubes have the same inner and outer diameter but they differ in length. The measured resistance of the pediatric tracheotomy tubes were greater than the shorter neonatal tubes since the pressure required to achieve a given flow is directly proportional to length. Mullins' group found that the tube most closely resembling the airway resistance of the neonate was the neonatal 0. In contrast to the Shiley size recommendations chart, Mullins found that in children ages 3-7, the pediatric tube that is best is the pediatric tube 3. For children ages 6-11, the pediatric tube that resembles the airway resistance in this age group is the pediatric 4. The adult size 8 most closely approximated the airway resistance of children eleven and older. Fortunately, Shiley has begun to classify the size of their pediatric and neonatal tubes based on the actual inner diameter. In infants and children, the tracheotomy tubes are shaved inferiorly to prevent erosion on the skin below the tracheostomy. Anesthesia: Communication between the otolaryngologist and anesthesiologist is essential when faced with a child with a compromised airway. It is preferable to perform a tracheotomy with the child under general anesthesia and an endotracheal tube or bronchoscope in place. The procedure usually begins by oxygenating the child in a comfortable position, establishing I.V. access and initiating an anesthetic inhalation agent. The otolaryngologist should be aware at all times what medications the anesthesiologist plans to administer. Muscle relaxants can be used with caution only after it has been established that the child can be ventilated by bag mask. It is essential that the anesthesiologist and otolaryngologist agree on the course of induction. The surgeon should always be prepared to perform rapid rigid bronchoscopy or emergency tracheotomy if direct visualization of the larynx with a laryngoscope is not possible. Technique: As previously stated, general anesthesia with an endotracheal tube or bronchoscope is preferable. The surgeon should position the child him or herself. The neck is hyperextended by placement of a shoulder roll. It is best if the anesthesiologist holds the child’s chin to stabilize the tissues and to keep the neck hyperextended. In infants, all esophageal tubing (nasogastric tubes and esophageal stethoscopes) should be removed to aid in correct identification of the trachea by palpation. The neck is prepped and draped in the usual fashion but the face should be left uncovered. The thyroid and cricoid cartilages are then identified by palpation. This can be very difficult in a young child because the larynx is soft and located in a more superior position when compared with an adult. Important landmarks such as the thyroid and cricoid cartilages, suprasternal notch and planned skin incision are marked. Local anesthetic (0.5% lidocaine with 1:200,000 epinephrine) is used for local injection at the proposed skin incision. The skin incision is made one fingerbreadth above the suprasternal notch. Either a vertical or horizontal skin incision may be used. The incision is carried through the subcutaneous tissues. The trachea is palpated repeatedly during the procedure. Some say that tracheotomy is as much done by palpation as by visualization. Identify the anterior jugular veins and strap muscles. It is usually not necessary to ligate the anterior jugular veins. The fascia of the strap muscles is grasped on each side of the midline with hemostats. The fascia is lifted, divided with scissors in the midline and slightly undermined. The trachea is again palpated to insure its location. Retractors can be used to gently retract the strap muscles laterally. The thyroid gland can be retracted if necessary. Rarely does the thyroid isthmus need to be divided in a child. If this is necessary, the isthmus should be clamped, divided and suture ligated. Once the trachea is visualized, stay sutures (4.0 Neurolen) are placed bilaterally approximately 2mm from the midline around at least two tracheal rings. This allows the trachea to be delivered into the wound. Hemostasis is then assured. Controversy remains over the type of tracheal incision. The consensus appears to be that a vertical tracheal incision is preferred. The incision is made in the midline of the second, third, and/or fourth tracheal rings. No cartilage should be removed. The tracheotomy tube is inserted after applying anterolateral traction on the stay sutures. The tube is held in place while the shoulder roll is removed. The chest is auscultated for bilateral equal breath sounds. The neck is then slightly flexed and the tracheostomy ties are secured around the neck allowing for one finger to pass underneath the ties. The stay sutures are then secured to the neck with tape printed with "do not remove". A chest x-ray should be obtained post-operatively to insure proper placement of the tracheostomy tube. Fry et al(4) compared three standard pediatric tracheotomy incisions: 1) inferiorly based trapdoor 2) vertical slit and 3) horizontal H. Using a young animal model ( 8-9 week old ferret), they evaluated the three groups for tracheal stenosis using endoscopy, radiography, and computer-analyzed airflow studies. On endoscopy, they found fairly predicable patterns of tracheal stenosis with each type. The inferior based flap group left an anterior shelf deformity while both the vertical slit and horizontal H groups created an hourglass pattern with lateral narrowing. Airflow studies revealed no difference in airflow resistance in the vertical slit group as compared with controls. In contrast, the horizontal H and inferior trap door groups both had significant (p < 0.05) increases in airflow resistance as compared with controls. Fry's group concluded that the vertical tracheal incision is the best choice in the pediatric patient. Emergency Tracheotomy: Again, it is preferable to perform a tracheotomy on an adult or a child in a controlled fashion. This, unfortunately, is not always the case. In a child, it is especially difficult to perform a cricothyrotomy because of the very small size of the membrane and difficulty in palpating the structures. Some authors have suggested using a large-bore needle transtracheally, but this too is very difficult due to the flexibility of the child's larynx and trachea. Basically, in a life-threatening situation, any means of obtaining an airway is better than the consequence of not. Postoperative Care: The child needs to be monitored in an intensive care setting. A postoperative chest x-ray should be obtained to check tube placement and rule out pneumothorax. Humidified air by collar or ventilator should be provided to prevent excessive dryness and thickness of secretions. Gentle suctioning should be performed every one to two hours the first few days then decreased to as needed. The child may require sedation or restraints to prevent the tracheostomy tube from being accidentally dislodged. The patient can have a diet the following day. Generally, the first tracheostomy tube change is done by the surgeon around postoperative day number five or seven after a good tract has formed. A suction catheter placed through the old tracheostomy tube can be used as a guide for the new tube to be inserted. The stay sutures can also be removed at this time. Complications: The complication rate of pediatric tracheotomy appears to be around 40 %. Complications include operative and postoperative, both early and late. Operative complications include hemorrhage, air entry, anatomic damage, tracheotomy tube problems, respiratory drive cessation and pulmonary edema. Postoperative difficulties can include hemorrhage, air entry, tracheal lesions, tracheostomy tube problems, infection, swallowing difficulties, and aphonia. Wetmore et al(5) review pediatric tracheotomy over a ten year period. They found that accidental decannulation (24%) was the most common early postoperative complication followed by pneumonia (20%), pneumothorax (9%), subcutaneous air (9%) and obstructed tube(7%). As far as late complications, they found that a tracheo-cutaneous fistula was most common (19%) followed by accidental decannulation (18%), tracheal granuloma (14%), stomal granulation (11%), and obstructed tube (10%). Operative: <> This complication may be due to a hereditary coagulation defect or an acquired abnormality from liver disease, sepsis or deficient clotting factors in a neonate. The surgeon should be aware of the potential for vascular anomalies. Most bleeding is due to oozing from capillaries and should respond to electrocautery or cease spontaneously. <> Air can sometimes dissect between the deep and superficial cervical fascia into the mediastinum. Pneumothorax can occur if the pleura of the lung apex is damaged. Leaving the skin incision open and careful dissection of the pretracheal fascia staying in the midline will help prevent this complication. < ANATOMIC> Structures in infants and children are quite small and careful attention to dissection is fundamental. Too deep dissection through the posterior tracheal wall can cause injury to the esophagus. Dissection too laterally can injure the recurrent nerves or the carotid. Again, midline dissection can help prevent this complication as well as using a vertical tracheal incision. Tracheostomy Tube Problems: The tracheostomy tube may be accidentally dislodged or lead to high airway resistance if the chosen tube is too small. Too large a tube can cause damage from excessive pressure to the tracheal walls. Proper choice of the size of the tracheostomy tube will help avoid these complications. Cannulation of a mainstem bronchus or creation of a false passage may also occur. Respiratory Arrest: This phenomenon has been attributed to loss of ventilatory drive due to rapid change in CO2 tension leading to arrhythmias and hypotension. Pulmonary Edema: Thought to be due to rapid influx of fluid across the alveolar wall because of the sudden change in airway pressure following tracheotomy. Postoperative Complications: <> Bleeding from a tracheotomy, especially in the late postoperative period, may herald a serious complication. Tracheal wall erosion can occur from pressure from the tracheostomy tube on the anterior trachea. The innominate artery crosses anterior to the trachea at the superior thoracic inlet. Erosion into this vessel can lead to massive hemorrhage. Direct visualization of the trachea is necessary to rule out this potentially fatal complication. Fortunately, most bleeding postoperatively is secondary to inflammation from excessive drying and suctioning. < AIR> Pneumothorax can be caused by high ventilator pressures or aggressive bagging. <> Many factors can contribute to damage to the trachea after tracheotomy. This damage can range from tracheal stenosis to granuloma formation. Most authors agree that proper care of the tracheostomy and choosing the appropriate size tracheostomy tube can greatly diminish this complication. Subglottic stenosis can be prevented by avoiding a high tracheotomy. Tracheal granulomas usually occur at the superior lip of the tracheostomy site. They can be treated with observation if small but if large they may need to be removed surgically to avoid stomal obstruction during tube change. Tracheostomy Tube Problems: Tracheostomy tube occlusion by crusts and mucous plugs is a common early complication. This can be prevented by humidification and adequate suctioning. Infection: Tracheitis and stomal infections can occur and usually respond to local care, humidified air and suctioning. Cultures can be done if symptoms persist. Pseudomonas and staphylococcus organisms are commonly seen. Deglutition Difficulties: As with adults, a tracheotomy tube can interfere with swallowing by inhibiting laryngeal elevation and compressing the esophagus. Cosmesis: Scarring develops whether a horizontal incision or vertical incision is used. A persistent tracheocutaneous fistula can develop and is dependent on the duration of the tracheostomy. It is recommended that if a tracheocutaneous fistula persists for greater than 6-12 months, the entire tract be excised and a multilayered closure be performed. A drain should be inserted to prevent air tracking. Aphonia: The inability to communicate immediately after a tracheotomy is a very frightening thing for a child. Parents and nursing staff should be alert to the child's inability to clearly communicate distress. If a long term tracheotomy is planned, speech development must be addressed. If the child is decannulated prior to one year of age (pre-lingually) or the child can phonate around the tube, speech development is usually not a problem. If a child is speaking prior to tracheotomy, he or she is at risk for significant expressive delay and the assistance of a speech therapist is essential. The therapist will be able to help develop oromotor skills, maximize receptive language, and encourage non-vocal behavior. Decannulation: Decannulation of a patient with a tracheotomy is primarily dependent on the original indication for the procedure. Once the underlying pathologic condition has improved and the tracheostomy if felt to be no longer necessary, steps toward decannulation can be initiated. Mallory et al(6) studied whether tidal flow measurements would be a helpful predictor of successful decannulation in the pediatric patient. His group studied forty four children with tracheotomies who were being considered for decannulation. All of the children underwent pulmonary function testing prior to endoscopy. Their maximal inspiratory flow through the mouth (MIFm) and maximum inspiratory flow through the tracheostomy cannula (MIFt) and their ratio (MIFm/MIFt) were measured. A ratio of MIFm to MIFt in liters per second greater than or equal to one was considered favorable for decannulation. Mallory found the predictability ratio of MIFm/MIFt for successful decannulation to be 76% and a false negative ratio of 24% (deemed unfavorable for decannulation but decannulation successful). Endoscopy had a predictability ratio of 84%. Mallory concluded that, although endoscopy remains the most sensitive indicator of successful decannulation, Pulmonary function testing is non-invasive and can be done on an outpatient basis. He developed a decannulation algorithm with PF testing as an adjunct in the decision making process. Prior to decannulation, the airway should be studied endoscopically to assess the original pathologic condition as well as look for possible new problems caused by the tracheostomy. Any tracheal or stomal granulomas should be excised. Vocal cord motion should be assessed. Sasaki et al(7) studied decannulation failures and found that 25% were caused by temporary abductor failure. The pathophysiology behind this appears to be an abrupt increase in dead space and airway resistance upon removal of the tracheostomy tube. Gradually decreasing the size of the tracheostomy tube seems to allow for return of abductor movement. A trial of tracheostomy tube plugging should be performed prior to decannulation. The tube should only be plugged during the day when an adult is present if the child is not hospitalized. Just prior to decannulation, an overnight admission to a monitored hospital bed is required for night time plugging. After decannulation, a light pressure dressing should be applied. Once decannulated, the child should continue to be monitored for 2448 hours in the hospital. Home Care: Not all patients can be decannulated and require their tracheostomies long-term. The majority of these patients can receive care of their tracheostomies at home. The families are usually frightened and apprehensive about taking their child home and assuming care for them. Therefore, parent and family education and discharge planning is critical. This requires considerable coordination and communication between the family and a number of health care workers. Prior to discharging a child home with a tracheostomy, the parents have to demonstrate proficiency in the use of the equipment needed, nursing care of the tracheostomy, detection of problems and emergency care. They should be taught CPR for a child with a tracheostomy. Ideally, this should occur in the hospital setting with the parents assuming total care of the child for a couple of days prior to discharge. Videotapes are available for viewing as well as trachestomy manuals for use as a quick reference. A responsible adult must be with the child at all times. It is a good idea to arrange for home health to evaluate the home and make sure all equipment is functional. It is important to notify the electric and telephone companies that a child with a tracheostomy lives in the home and service cannot be interrupted for any reason. The EMS service should also be informed. The child should be followed up by a tracheostomy team if available as well as their primary pediatrician. Comments by Dr. Deskin: Emergency tracheotomies should be a rare occasion in a child. If the timing and the preoperative planning is done well, the tracheotomy should be able to be done under a controlled situation with an endotracheal tube or bronchoscope in place. If not and an emergency situation arises an attempt to intubate even over a fiberoptic scope or through an anterior commissure scope technique should be tried. In the event a emergency tracheotomy is carried out a reassessment of the airway by endoscopy should be carried out immediately and the tracheotomy revised at the normal position as soon as possible. In regard to tube sizing, the new Shiley tubes now are named by number corresponding to the inner diameter. Bivona tubes also have a good numbering system. All the caretakers of a child should be aware of the indication for the tracheotomy and whether the airway is patent or obstructed. Also resuscitation plans should be known by all caretakers including hospital personnel when the child is in the hospital which would help in resuscitation should the tube become obstructed or accidentally displaced without the ability to replace the tube. For instance, bag and mask or intubation from above would be possible in some airways and in other obstructed airways immediate replacement of the tube through the stoma would be required. BIBLIOGRAPHY 1) Stool SE and Eavey R. Tracheotomy. In: Bluestone and Stool, ed. Pediatric Otolaryngology.W.B. Saunders, Philadelphia, 1983. 2) Douglas GS, Hoskins D, and Stool SE. Tracheotomy in Pediatric Airway management. ENT J. 1978;57:55-70. 3) Mullins JB, et al. Airway Resistance and Work of Breathing in Tracheostomy Tubes. Laryngoscope. 1993;103:1367-1372. 4) Fry TL, Fischer ND, Jones RO, Pillsbury HC. Comparisons of Tracheostomy Incisions in a Pediatric Model. Ann Otol Rhinol Laryngol. 1985;94:450-453. 5) Wetmore RF, Handler SD, Postic WP. Pediatric Tracheostomy. Experience During the Past Decade. Ann Otol Rhinol Laryngol. 1982;91:628-632. 6) Mallory GB, et al. Tidal Flow Measurement in the Decision to Decannulate the Pediatric Patient. Ann Otol Rhinol Larygol. 1985;94:454-457. 7) Deskin RW. Pediatric Tracheotomy. In press. 8) Weissler MC. Tracheotomy and Intubation. In: Bailey BJ, et al , eds. Head and Neck Surgery-Otolaryngology. Philadelphia: J.B. Lippencott, 1993. 9) Ruben RJ, et al. Home Care of the Pediatric Patient with a Tracheotomy. Ann Otol Rhinol Laryngol. 1982;91:633-640. 10) Hazinski MF. Pediatric Home Tracheostomy Care: A Parent's Guide. Pediatric Nursing. 1986;12:41-47. http://www2.medsch.wisc.edu/childrenshosp/trach/cat.html Complications of a tracheostomy Other common problems are the complications which may occur with a tracheostomy tube. Some parents worry about their child developing infections in the lungs; the trach tube accidentally coming out; thick secretion build-up; mucus plugs; and whether they will be able to tell if their child is having respiratory problems or distress. Using the same precautions you would with other children can diminish lung infection risks. Cleanliness in managing a child with a tracheostomy is most important in controlling infection. The equipment must be cleaned regularly, and you should wash your hands frequently. At the hospital, you'll learn how to change the tube when necessary or what to do if the tube should fall out accidently. Changing the tube while under supervision will give you the opportunity to see how mucus build-up in the tube looks. You'll become familiar enough with trach procedures to know if you need to add more moisture to prevent the lung's mucus from getting too thick and causing plugs. http://wellness.ucdavis.edu/child_health/special_needs/pediatric_tracheostomy/parents_c oncerns.html Acute Rehabilitation Gillette Children's Specialty Healthcare 200 E. University Ave. St. Paul, MN 55101 651/291-2848 http://www.cmrg.com/cmrg_cfmfiles/detail.cfm/41595/ARE.htm http://www.cmrg.com/index.htm Case Management Resource Guide Dorland healthcare Infromation 1500 Walnut St., Ste 1000 Philadelphia, PA 19102 215-875-1212, fax: 215-735-3966 800-784-2332 Few Pediatric Centers Have Tracheostomy Protocol Only 1 of 34 academic pediatric pulmonary medicine centers surveyed had a formal management protocol for obtaining tracheal aspirate cultures and choosing antibiotic therapy for patients with tracheostomies. 9/14/2000 http://primarycare.medscape.com/IMNG/PediatricNews/1998/v.32.n08/pn3208.27.01.few.html See results from this site only. Tracheostomy in children with emphasis on home care. Duncan BW, Howell LJ, deLorimier AA, Adzick NS, Harrison MR Summary: Tracheostomy in children is not a benign procedure. Tracheostomy- related mortality rates among children have been previously reported to be as high as 10% to 27%. Children with tracheostomies are especially vulnerable after home discharge with mortality rates of 0.5 to 2 deaths per 100 months at home. In order to assess the impact of extensive parental education and home nursing care on tracheostomy-related mortality, we report our experience over 9 years with 44 children receiving tracheostomies. Each child was maintained at home with a tracheostomy for an average of 19 months for a total of 635 months of home tracheostomy care. Indications for tracheostomy were tracheomalacia (32%), obstructive airway lesions (23%), central nervous system lesions (16%), vocal cord paralysis (9%), Pierre Robin syndrome (9%), and a list of miscellaneous conditions (11%). Our tracheostomy care regimen begins with intensive parental training in tracheostomy management for a minimum of 10 days prior to discharge. Home nursing was arranged for 77% of these children for an average of 11 hours per day at the time of discharge. Eighty-three percent had home apnea monitors. Discharge of these children was delayed or transfer to a secondary hospital was made when parents failed to show adequate proficiency in tracheostomy management with existing home nursing. Eight percent were ventilator dependent at discharge. As of January 1, 1989, 34% of these children have been decannulated. There were six deaths, all due to underlying disease. There were no tracheostomy- related deaths in hospital or after discharge home.(ABSTRACT TRUNCATED AT 250 WORDS) Journal of Pediatric Surgery, VOL. 27, NO. 4: pp.432-5 Copyright © 1992 W. B. Saunders Company http://www.jpedsurg.org/abs/abs27_4/395469.html Tracheostomy: Easing the Transition from Hospital to Home by Lois Dixon, MSN, RN http://www.perspectivesinnursing.org/v1n3/dixon.html http://www.aap.org/policy/re9812.html Hospital Discharge of the High-Risk Neonate--Proposed Guidelines (RE9812) Policy Statement Pediatrics Volume 102, Number 2 August 1998, pp 411-417 Hospital Discharge of the High-Risk Neonate--Proposed Guidelines (RE9812) AMERICAN ACADEMY OF PEDIATRICS Committee on Fetus and Newborn This policy statement is the first formal statement of the American Academy of Pediatrics on the issue of hospital discharge of the high-risk neonate. It has been developed, to the extent possible, on the basis of published, scientifically derived information. Four categories of high risk are identified: 1) the preterm infant, 2) the infant who requires technological support, 3) the infant primarily at risk because of family issues, and 4) the infant whose irreversible condition will result in an early death. The unique home care issues for each are reviewed within a common framework. Recommendations are given for four areas of readiness for hospital discharge: infant, home care planning, family and home environment, and the community and health care system. The need for individualized planning and physician judgment is emphasized. ABBREVIATION. VLBW, very low birth weight. The decision about timing of hospital discharge of an infant after neonatal intensive care is complex. It is made even more difficult because of cost-containment issues and rigid definitions of medical necessity as determining influences on the length of hospitalization. Because of the pressure to discharge high-risk neonates at the earliest possible opportunity, it is important that guidelines are based on a review and analysis of current evidence. Shortening the length of a hospital stay may benefit the infant and family because decreasing the period of separation from the parents may lessen the subsequent adverse effect on parenting.1,2 The risks for hospital-acquired morbidity may be reduced.3-6 However, the overriding concern is that infants may be placed at risk for increased mortality and morbidity related to discharge before physiologic stability is established. Multiple investigators have found that preterm low birth weight infants who required neonatal intensive care experience a much higher rate of hospital readmission and death during the first year after birth compared with appropriate for gestational age, healthy term infants.7-13 Adequate time for preparation of the family to provide care in a home setting and for mobilization of community resources to provide support services is necessary before discharge. With advances in neonatal intensive care and changes in the economic and societal forces, the complexity of posthospital care issues has increased. A single set of criteria for discharge readiness is no longer adequate. These guidelines, therefore, address four broad categories of high-risk situations: 1) the preterm infant, 2) the infant who requires technological support, 3) the infant primarily at risk because of family issues, and 4) the infant whose irreversible condition will result in an early death. REVIEW OF THE LITERATURE The Preterm Infant The traditional approach to determining discharge readiness was the achievement of a preset weight, historically 5 or 51/2 lb. During the past three decades several observational,14-17 nonrandomized,18-21 and randomized, controlled22-24 studies have been published that analyzed outcomes of preterm infants who were discharged after certain criteria were met. Although the population characteristics, the nature and results of the outcome measures, and the content of the early discharge programs varied, the common elements included: A sustained pattern of weight gain rather than a specific achieved weight, Physiologic stability defined as the ability to suckle feed and maintain normal body temperature in an open environment, An active program of parental involvement and preparation for posthospital care, Predischarge on-site home assessment, An active program of parental support after discharge of the very low birth weight (VLBW) infant, Frequent outpatient follow-up to assure adequate weight gain for the smallest infants in the weeks immediately after discharge, An organized program of postdischarge tracking and surveillance. The safety of discharge after a shorter than usual hospital stay was supported by adequacy of weight gain and no increase in the number of acute care visits, unscheduled hospital readmissions, or early infant deaths in randomized studies with matched control cohorts. Each of these study designs included a program of parent education and infant follow-up.22-24 In the studies that addressed cost savings specifically,19,20,22,23 effectiveness was documented even with the inclusion of costs for coordination of care and services, home visiting, transportation, sibling care, and in-home support for the family, although in no single study were all of the aforementioned ancillary services provided. The success of the early discharge programs that incorporated specialized home care and follow-up surveillance indicates that the care required by the preterm infant and the support needed by families exceed that after discharge at a later postnatal age. The three physiologic competencies that are generally recognized as essential before hospital discharge are the ability to maintain a normal body temperature fully clothed in an open bed with normal ambient temperature, the ability to coordinate suckle feeding, swallowing, and breathing while ingesting an adequate volume of feeding, and the ability to grow at an acceptable rate. These competencies are achieved by most preterm infants between 34 and 36 weeks postmenstrual age. Equally essential is the ability to maintain stable cardiorespiratory function. Data about maturation of breathing control and feeding behavior are more direct,25-38 whereas the maturational timing of the ability to maintain body temperature can only be inferred.39-41 Although interrelated, not all competencies are achieved at the same postnatal age in a given infant. The pace of maturation is further influenced by the birth weight, the gestational age at birth, and the degree and chronicity of neonatal illnesses. For infants with delayed maturation of respiratory control, use of home cardiorespiratory monitoring has been reported.42-44 The National Institutes of Health Consensus Development Conference45 and the Canadian Paediatric Society policy statement46 included prematurity with unresolved apnea as a potential indication for home monitoring. The success of home monitoring for unresolved apnea in reducing hospital stay without undue family stress has been observed.43,44 However, infant deaths associated with the lack of proper monitor use have been reported.47 The predischarge clinical course and abnormal cardiorespiratory polygraphic findings have not correlated with subsequent alarm events requiring parental intervention42 and apnea of prematurity and risk of sudden infant death syndrome.45 Thus, the decision to use home cardiorespiratory monitoring and predischarge polygraphic studies of cardiorespiratory function remains a matter of individual clinical judgment. The Infant With Special Health Care Needs or the Technology-dependent Infant In the past two decades, increasing numbers of children with unresolved and/or special health care needs have been discharged to home care with varying requirements for technologic dependence and/or support.48 For newborn infants, the three broad groupings or categories of special care requirements are as follows: 1) those requiring special or assistive feeding techniques, 2) those requiring respiratory assistance, and 3) those with complex congenital anomalies requiring supportive and assistive devices. Only the first two categories are addressed because the population of the third group is very diverse and to our knowledge no data from controlled studies of home care have been published. Gavage feeding as the primary mode of enteral feeding of sick and premature infants is a common practice in the hospital setting. There is no reported clinical experience of its use in home care of young infants from which conclusions about safety, efficacy, and clinical appropriateness can be reached. Another approach for infants requiring long-term assistive feeding is placement of a gastrostomy; however, no clinical series of newborns with long-term home gastrostomy feeding has been reported. In the only reported series of home intravenous nutritional support of infants,49 one death from catheter-related sepsis was noted. Somatic growth was maintained at normal rates, and six of the eight infants had normal developmental progress. Infants with tracheostomies placed for various airway abnormalities have been cared for at home in recent years.50-52 The underlying reason for the tracheostomy is reported to be the most important factor affecting the outcome, although airway accidents have been a major factor in adverse morbidity. To date, no clinical trials have been reported that compare outcomes of home oxygen therapy in infants with bronchopulmonary dysplasia with those after prolonged hospitalization. Multiple observational studies have been conducted, however,53-55 the more recent of which have noted relative safety, ease of implementation, and costeffectiveness.56-58 Prolonged oxygen supplementation is further supported by reported observations about its role in limiting progression to cor pulmonale,59 facilitating normal growth rates,60,61 and avoiding unrecognized hypoxic episodes.62,63 Reports of home ventilatory support of infants with chronic respiratory failure64,65 emphasize the need for continuous cardiorespiratory monitoring, disconnect alarms for mechanical support devices, and qualified personnel to provide bedside care to reduce the risk of death from airway accidents. Maintaining safe and adequate care is complex, emotionally demanding, and consumes the time and resources of families.46,65 The Infant at Risk Because of Family Issues Preterm birth and prolonged hospitalization were first reported as risk factors for subsequent child abuse in 1971.66 In subsequent studies,67,68 infant risk factors found to be significant were VLBW, prolonged hospital stay, and congenital defects. Maternal factors included lower educational level, lack of social support, marital instability, and fewer prenatal care visits. Significantly fewer family visits during the stay in the neonatal intensive care unit had occurred for infants in whom subsequent maltreatment was documented.67 The increase in substance use among the childbearing age group has created a large population of children at risk for a variety of adverse medical and psychosocial outcomes.69 Sequelae such as attachment disturbances, behavioral and developmental disorders, and child maltreatment have been observed frequently among children born to substance abusers.70-72 Strategies to reduce the risks of adverse outcomes in infants at high risk because of psychosocial concerns that have been adequately studied have focused primarily on home visitation with or without additional social support services.7379 The likelihood of success increased when an intervention program for maternal substance abuse included addiction treatment for the parents.80 The Infant With Anticipated Early Death The concept of hospice care for neonates was first introduced in the pediatric literature in an editorial in 198281 and in reports of a specialized in-hospital program.82,83 Although hospice care at home or in an alternative setting for older children has been reported,84-87 such studies are lacking for neonates. However, the components of pediatric hospice care as expounded by Corr and Corr88 are theoretically as equally applicable for infants, including 1) involvement of skilled professionals, 2) care directed toward control of distressing symptoms and provision of physical comfort, 3) coordination of services and a multidisciplinary approach, 4) adequate social supports to meet family needs, and 5) provision of follow-up and bereavement care. Enhancing the quality of the remaining life for the infant and family is more important than the site of care delivery. DISCHARGE PLANNING The care of each high-risk neonate after discharge must be carefully coordinated to provide ongoing multidisciplinary support of the family. The discharge planning team should include parents, the primary care physician, the neonatologist, neonatal nurses, and the social worker. Other professionals, such as surgical specialists and pediatric subspecialists, pediatric occupational, physical, speech, and respiratory therapists, infant educators, nutritionists, home health care liaisons, and a case manager selected by the team and family, may be included as needed. The initiation of discharge planning should begin when it is evident that recovery is certain, although the exact date of discharge may not be predictable. The goal of the discharge plan is to assure successful transition to home care. Essential elements are a physiologically stable infant, a family who can provide the necessary care without undue strain and with appropriate support services in place within the community, and a primary care physician who is prepared to assume the responsibility with appropriate back up from specialist physicians and other professionals as needed. Six critical components must be included in discharge planning. 1. Parental Education. Parental contact and involvement in the care of the infant should have been encouraged from the time of admission. The participation of the parents in giving care as early as feasible in the neonatal course has been shown to have a positive effect on their confidence in handling the infant and readiness to assume full responsibility for the infant's care at home.89 The development of an individualized teaching plan aids parents in acquiring the skills and judgment required for the appropriate care of their infant. Having a written checklist or outline of the specific areas and tasks to be mastered increases the likelihood that both parents will receive complete instructions and experience. Caregivers and parents must understand that if an infant is discharged from the hospital before complete physiological maturation and resolution of all complications of high-risk birth, the infant's care requirements will continue at home. Furthermore, the level of care being asked of the parents is beyond that of the usual parental role. Thus, ample time for teaching the parents and caregivers the techniques and the rationale for each item in the care plan is essential. Return demonstrations, parent rooming-in, and telephone follow-up have all been reported to facilitate parental education and adaptation to their infant's care.1517,21,89,90 In so far as possible, at least two caregivers, one of whom is a responsible adult, should be identified and taught for each infant. The demands of home care can be physically and emotionally draining, especially at first, for infants requiring frequent feeding. Young mothers who do not live with a parent or the father of the baby have been shown to be vulnerable to the strains of home care.67 Even in a two-parent family, the primary caregiver may become ill and need relief. 2. Implementation of Primary Care. Preparing the infant for transition to primary care begins early in the hospitalization with administration of immunizations at the recommended ages,91 completion of metabolic screening,92,93 and assessment of hearing by an acceptable electronic measurement.94 For the infants at risk, appropriate funduscopic examination for retinopathy of prematurity should be performed by an ophthalmologist skilled in the evaluation of the retina of the preterm infant as recommended in the AAP policy statement.95 Assessment of hematologic status is recommended for all infants because of the high prevalence of anemia after neonatal intensive care. Because VLBW infants and those who have received parenteral nutrition for prolonged periods may be at risk for hypoproteinemia, vitamin deficiencies, and bone mineralization abnormalities, screening for nutritional or metabolic deficiencies may be indicated. 3. Evaluation of Unresolved Medical Problems. Review of the hospital course and the active problem list of each infant and careful physical assessment will reveal unresolved medical issues and areas of physiologic function that have not reached full maturation for the infant. From such a review, the diagnostic studies required to document the current clinical status of the infant can be identified and alterations in management instituted. The intent should be to assure implementation of appropriate home care and follow-up plans. 4. Development of the Home Care Plan. Although the content of the home care plan may vary among the four categories of infants, the common elements include the following: 1) identification and preparation of the in-home caregivers, 2) development of a comprehensive listing of required equipment and supplies and accessible sources, 3) identification and mobilization of necessary and qualified home care personnel and community support services, 4) assessment of the adequacy of the physical facilities within the home, 5) development of an emergency care and transport plan as indicated, and 6) assessment of available financial resources to assure the capability to finance home care costs. Specific details of planning home care for the technology-dependent infant are included in the AAP policy statement,96 in a consensus report48 and, for hospice care, in Corr and Corr.97 The input of the primary care physician in formulating the home care plan of the technology-dependent infant is essential. Many infants, particularly the VLBW and technology-dependent infants, require continued care by multiple surgical specialists and pediatric subspecialists, each of whom should be included in the predischarge assessment and discharge planning. 5. Identification and Mobilization of Surveillance and Support Services. The psychosocial characteristics of each family should be reviewed, noting those risk factors that may contribute to an adverse infant outcome. The availability of social support is essential to the success of every parent's adaptation to the home care of a highrisk infant.98 Before discharge and periodically thereafter, a review of the family's needs, coping skills, use of available resources, financial problems, and progress toward goals in the home care of their infant should be evaluated. After the social support needs of the family have been identified, an appropriate, individualized intervention plan using available community programs, surveillance, or alternative care placement may be implemented. 6. Determination and Designation of Follow-up Care. In general, the attending neonatologist has the responsibility for coordination of followup care, although in an individual institution, the tasks may be delegated to other professionals. A primary care physician should be identified as early as possible to facilitate the coordination of follow-up care planning between the primary care setting and the subspecialty center-based discharge planning staff. Pertinent information about the nursery course and home care plan should be given to that individual before the infant's discharge. It is highly desirable that the primary care physician meet the parents before the discharge and, if possible, examine the infant in the hospital. In specialty center units, the primary care attending physician should work together with the neonatologist in coordinating the discharge planning. Arrangements for an initial appointment with the primary care physician should be initiated before discharge. Specific follow-up appointments with each involved surgical specialist and pediatric subspecialist should be made as indicated in advance of discharge, giving attention to grouping these as much as possible to enhance compliance and to decrease the inconvenience of the family. Periodic evaluation of the developmental progress of every infant is essential to identify deviations in neurodevelopmental progress at the earliest possible point, thereby facilitating entry into early intervention programs (Public Law 99-457).99 The primary care physician with appropriate skills, the pediatric subspecialist, or clinic personnel may provide longitudinal developmental follow-up. When input from multiple disciplines is identified before discharge, a center-based clinic providing multidisciplinary care may be the least cumbersome option for the family. SPECIAL CONSIDERATIONS With networking among nurseries that provide different levels of care, increasing numbers of infants are transported back to community hospitals for convalescent care. In these hospitals, the discharge planning process should follow the same principles as those outlined above for an infant being discharged from a subspecialty center. Appropriate follow-up during the most critical periods for infants at risk for adverse sensorineural outcomes, ie, the VLBW infant for progression of retinopathy and for all high-risk infants whose hearing status or type of hearing deficit still needs evaluation. Innovative programs based on community resources, both public and private, should be encouraged. The goal should be to provide coordinated care and family support. Efficient teamwork by health care professionals is imperative. Programs should be modified to accommodate different demographic needs and to achieve efficient use of all funding resources. For optimal support of parents and surveillance of the status of a high-risk infant after discharge it is important that experienced nurses who are qualified to perform specialized assessments are utilized for home nursing visits. It is essential that previous performance and existing quality control programs be considered when choosing a home health care agency to provide personnel for in-home care of the technology-dependent infant. RECOMMENDATIONS The following recommendations are offered as a framework for consideration as each individual infant and caregiving situation is evaluated and the discharge decision made. It is prudent that each institution establish guidelines allowing for individual physician judgment and flexibility. Infant Readiness for Hospital Discharge In the judgment of the responsible physician there has been: o o o A sustained pattern of weight gain of sufficient duration; Adequate maintenance of normal body temperature with the infant fully clothed in an open bed with normal ambient temperature (24°C to 25°C); Competent suckle feeding, breast or bottle, without cardiorespiratory compromise; and o Physiologically mature and stable cardiorespiratory function of sufficient duration. In addition, o o o o o o Appropriate immunizations have been administered; Appropriate metabolic screening has been performed; Hematologic status has been assessed and appropriate therapy instituted as indicated; Nutritional risks have been assessed and therapy and dietary modification instituted as indicated; Sensorineural assessments, hearing and funduscopy, have been completed as indicated; Review of hospital course has been completed, unresolved medical problems identified, and plans for treatment instituted as indicated. Home Care Plan Readiness An individualized home care plan has been developed with input from all the appropriate disciplines. The plan for infants with complex multiple system problems, and particularly for those requiring technological assistance, must be specific and detailed. For infants at psychosocial risk, arrangement for appropriate psychosocial surveillance and family support is essential. Family and Home Environmental Readiness Assessments of the family caregiving capabilities, resource requirements, and home physical facilities have been completed. o o o o Identification of at least two family caregivers, one of whom is an adult, and assessment of their ability, availability, and commitment; Psychosocial assessment for parenting risks; A home environmental assessment that may include an on-site evaluation; Review of available financial resources and identification of adequate financial support. An on-site assessment documenting availability of 24-hour telephone access, electricity, and an in-house water supply and heating and detailed financial assessment and planning are essential in preparation for home care of the technology-dependent infant. Parents and caregivers have demonstrated the necessary capabilities to provide all components of care including: o Feeding, whether breast, bottle, or an alternative technique, including formula preparation as required; o o o o o o o o Basic infant care including bathing; skin, cord, and genital care; temperature measurement; dressing; and comforting; Infant cardiopulmonary resuscitation and emergency intervention as indicated; Assessment of clinical status, including understanding and detection of the general early signs and symptoms of illness, as well as the signs and symptoms specific to the infant's condition; Infant safety precautions including proper infant positioning during sleep and use of car seats100-102; Specific safety precautions for an artificial airway, feeding tube, ostomy, infusion pump, and other mechanical and prosthetic devices as indicated; Administration of medications, specifically proper dosage and timing, storage, and recognition of the signs and symptoms of toxicity; Equipment operation, maintenance, and problem-solving for each mechanical support device required; The appropriate technique for each special care procedure required, including special dressings for infusion entry site, ostomy, or healing wounds, maintenance of an artificial airway, chest physiotherapy, oropharyngeal and tracheal suctioning, and infant stimulation and physical therapy, as indicated. Specific modification of home facilities as required by home care system needs have been completed. Community and Health Care System Readiness An emergency intervention and a transportation plan have been developed and emergency services providers identified and notified as indicated. Follow-up care needs have been determined, appropriate providers identified, and appropriate communication exchanged including the following: o o o o Primary care physician identified, and responsibility for care of infant accepted; Surgical specialty and pediatric subspecialty follow-up care requirements identified and appropriate arrangements made; Neurodevelopmental follow-up requirements identified and appropriate referrals made; Home nursing visits for assessment and parent support arranged as indicated by the complexity of the infant's clinical status and family capability and the home care plan transmitted to home health agency. The determination of readiness for care at home of an infant after neonatal intensive care is complex. Careful balancing of infant safety and well-being with family needs and capabilities is required while giving consideration to the availability and adequacy of community resources and support services. The final decision, which is the responsibility of the attending physician, must be tailored for the unique constellation of issues posed by each situation. COMMITTEE ON FETUS AND NEWBORN, 1997 TO 1998 James A. Lemons, MD, Chairperson Lillian R. Blackmon, MD Avroy A. Fanaroff, MD Hugh M. MacDonald, MD Carol A. Miller, MD Lu-Ann Papile, MD Warren Rosenfeld, MD Craig T. Shoemaker, MD Michael E. Speer, MD LIAISON REPRESENTATIVES Patrician Johnson, RN, MS, NNP American Nurses Association Association of Women's Health, Obstetric, and Neonatal Nurses National Association of Neonatal Nurses Michael F. Greene, MD American College of Obstetricians and Gynecologists Douglas D. McMillan, MD Canadian Paediatric Society Solomon Iyasu, MBBS, MPH Centers for Disease Control and Prevention Linda L. Wright, MD National Institute of Child Health and Human Development SECTION LIAISON Jacob C. Langer, MD Section on Surgery David K. Stevenson, MD Section on Perinatal Pediatrics CONSULTANTS Irwin Light, MD William Oh, MD REFERENCES 1. 2. 3. 4. Jeffcoate JA, Humphrey ME, Lloyd JK. Disturbance in parent-child relationship following preterm delivery. Dev Med Child Neurol. 1979;21:344-352 Macey TJ, Harmon RJ, Easterbrooks MA. Impact of premature birth on the development of the infant in the family. J Consult Clin Psychol. 1987;55:846-852 Bergman I, Hirsch RP, Fria TJ, Shapiro SM, Holzman I, Painter MJ. Cause of hearing loss in the high-risk premature infant. J Pediatr. 1985;106:95-101 American Academy of Pediatrics, Committee on Environmental Health. Noise: a hazard for the fetus and newborn. Pediatrics. 1997;100:724-727 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. Gottfried AW, Wallace-Lande P, Sherman-Brown S, King J, Coen C, Hodgman JE. Physical and social environment of newborn infants in special care units. Science. 1981;214:673-675 Glass P, Avery GB, Subramanian KN, Keys MP, Sostek AM, Friendly DS. Effect of bright light in the hospital nursery on the incidence of retinopathy of prematurity. N Engl J Med. 1985;313:401-404 McCormick MC, Shapiro S, Starfield BH. Rehospitalization in the first year of life for high-risk survivors. Pediatrics. 1980;66:991-999 McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82-90 Mutch L, Newdick M, Lodwick A, Chalmers L. Secular changes in rehospitalization of very low birth weight infants. Pediatrics. 1986;78:164-171 Porter KL, Rudolph C, Williams ML, Petonito G. Patterns of medical services utilization by infants discharged from a neonatal intensive care unit. Med Care. 1986;24:14-23 Combs-Orme T, Fishbein J, Summerville C, Evans MG. Rehospitalization of very-low-birthweight infants. Am J Dis Child. 1988;142:1109-1113 Termini L, Brooten D, Brown L, Gennaro S, York R. Reasons for acute care visits and rehospitalizations in very low-birthweight infants. Neonatal Network. 1990;8:23-26 Hulsey TC, Hudson MB, Pittard WB III. Predictors of hospital postdischarge infant mortality: implications for high-risk infant follow-up efforts. J Perinatol. 1994;14:219-225 Bauer CH, Tinklepaugh W. Low birth weight babies in the hospital: a survey of recent changes in their care, with special emphasis on early discharge. Clin Pediatr. 1971;10:467-469 Berg RB, Salisbury AJ. Discharging infants of low birth weight: reconsideration of current practice. Am J Dis Child. 1971;122:414-417 Singer B, Wolfsdorf J. Early discharge of infants of low birth weight: a prospective study. Br Med J. 1975;1:362-364 Derbyshire F, Davies DP, Haxby V, et al. Short reports: discharge of preterm babies from neonatal units. Br Med J. 1982;284:233-234 Dillard RG, Korones SB. Lower discharge weight and shortened nursery stay for low-birth-weight infants. N Engl J Med. 1973;288:131-133 Lefebvre F, Veilleux A, Bard H. Early discharge of low birthweight infants. Arch Dis Child. 1982;57:511-513 Rieger ID, Henderson-Smart DJ. A neonatal early discharge and home support programme: shifting care into the community. J Paediatr Child Health. 1995;31:33-37 Kotagal UR, Perlstein PH, Gamblian V, Donovan EF, Atherton HD. Description and evaluation of a program for the early discharge of infants from a neonatal intensive care unit. J Pediatr. 1995;127:285-290 Davies DP, Herbert S, Haxby V, McNeish AS. When should pre-term babies be sent home from neonatal units? Lancet. 1979;1:914-915 Brooten D, Kumar S, Brown L, et al. A randomized clinical trial of early hospital discharge and home follow-up of very-low-birth-weight infants. N Engl J Med. 1986;315:934-939 Casiro OG, McKenzie ME, McFadyen L, et al. Earlier discharge with community-based intervention for low birth weight infants: a randomized trial. Pediatrics. 1993;92:128-134 Parmelee AH, Stern E, Harris MA. Maturation of respiration in prematures and young infants. Neuropadiatrie. 1972;3:294-304 Gabriel M, Albani M, Schutte FJ. Apneic spells and sleep states in preterm infants. Pediatrics. 1976;57:142-147 Henderson-Smart DJ. The effect of gestational age on the incidence and duration of recurrent apnoea in newborn babies. Aust Paediatr J. 1981;17:273-276 Lee D, Caces R, Kwiatkowski K, Cates D, Rigatto H. A developmental study on types and frequency distribution of short apneas (3 to 15 seconds) in term and preterm infants. Pediatr Res. 1987;22:344-349 Wolff PH. The serial organization of sucking in the young infant. Pediatrics. 1968;42:943-956 Hack M, Estabrook MM, Robertson SS. Development of sucking rhythm in preterm infants. Early Hum Dev. 1985;11:133-140 Jain L, Sivieri E, Abbasi S, Bhutani VK. Energetics and mechanics of nutritive sucking in the preterm and term neonate. J Pediatr. 1987;111:894-898 32. Guilleminault C, Coons S. Apnea and bradycardia during feeding in infants weighing greater than 2000 gm. J Pediatr. 1984;104:932-935 33. Rosen C, Glaze D, Frost J. Hypoxemia associated with feeding in the preterm infant and full-term neonate. Am J Dis Child. 1984;138:623-628 34. Bu'Lock F, Woolridge MW, Baum JD. Development of co-ordination of sucking, swallowing and breathing: ultrasound study of term and preterm infants. Dev Med Child Neurol. 1990;32:669-678 35. Koenig JS, Davies AM, Thach BT. Coordination of breathing, sucking, and swallowing during bottle feedings in human infants. J Appl Physiol. 1990;69:1623-1629 36. Timms B, DiFiore J, Martin RJ, Miller MJ. Increased respiratory drive as an inhibitor of oral feeding of preterm infants. J Pediatr. 1993;123:127-131 37. Poets CF, Stebbens VA, Alexander JR, Arrowsmith WA, Salfield SAW, Southall DP. Oxygen saturation and breathing patterns in infancy. 2: preterm infants at discharge from special care. Arch Dis Child. 1991;66:574-579 38. Poets CF, Stebbens VA, Richard D, Southall DP. Prolonged episodes of hypoxemia in preterm infants undetectable by cardiorespiratory monitors. Pediatrics. 1995;95:860-863 39. Hey EN, O'Connell B. Oxygen consumption and heat balance in the cot-nursed baby. Arch Dis Child. 1970;45:335-343 40. Glass L, Silverman WA, Sinclair JC. Effect of the thermal environment on cold resistance and growth of small infants after the first week of life. Pediatrics. 1968;41:1033-1046 41. Rubecz I, Mestyan J. Activity, energy metabolism and postnatal age relationship in low-birthweight infants.Acta Pediatr Acad Sci Hung. 1975;16:351-362 42. Rosen CL, Glaze DG, Frost JD Jr. Home monitor follow-up of persistent apnea and bradycardia in preterm infants. Am J Dis Child. 1986;140:547-550 43. Vohr BR, Chen A, Coll CG, Oh W. Mothers of preterm and full-term infants on home apnea monitors. Am J Dis Child. 1988;142:229-231 44. Leonard BJ, Scott SA, Sootsman J. A home-monitoring program for parents of premature infants: a comparative study of the psychological effects. Dev Behav Pediatr. 1989;10:92-97 45. National Institutes of Health Consensus Development Conference on Infantile Apnea and Home Monitoring, September 29-October 1, 1986. Pediatrics. 1987;79:292-299 46. Fetus and Newborn Committee, Canadian Paediatric Society. The infant home monitoring dilemma. Can Med Assoc J. 1992;147:1661-1669 47. Meny RG, Blackmon L, Fleischmann D, Gutberlet R, Naumburg E. Sudden infant death and home monitors. Am J Dis Child. 1988;142:1037-1040 48. Wagner JL, Power EJ, Fox H. Technology-Dependent Children: Hospital Versus Home Care. Philadelphia, PA: Science Information Resource Center; 1988:99-105 49. Cannon RA, Byrne WJ, Ament ME, Gates B, O'Connor M, Fonkalsrud EW. Home parenteral nutrition in infants. J Pediatr. 1980;96:1098-1104 50. Ruben RJ, Newton L, Jornsay D, et al. Home care of the pediatric patient with a tracheotomy. Ann Otol Rhinol Laryngol. 1982;91:633-640 51. Line WS Jr, Hawkins DB, Kahlstrom EJ, MacLaughlin EF, Ensley JL. Tracheotomy in infants and young children: the changing perspective 1970-1985. Laryngoscope. 1986;96:510-515 52. Singer LT, Kercsmar C, Legris G, Orlowski JP, Hill BP, Doershuk C. Developmental sequelae of long-term infant tracheostomy. Dev Med Child Neurol. 1989;31:224-230 53. Pinney MA, Cotton EK. Home management of bronchopulmonary dysplasia. Pediatrics. 1976;58:856-859 54. Campbell AN, Zarfin Y, Groenveld M, Bryan MH. Low flow oxygen therapy in infants. Arch Dis Child. 1983;58:795-798 55. Abman SH, Accurso FJ, Koops BL. Experience with home oxygen in the management of infants with bronchopulmonary dysplasia. Clin Pediatr. 1984;23:471-476 56. Daily DK. Home oxygen therapy for infants with bronchopulmonary dysplasia. Perinatol Neonatol. 1987;11:27-36 57. Thilo EH, Comito J, McCulliss D. Home oxygen therapy in the newborn: costs and parental acceptance. Am J Dis Child. 1987;141:766-768 58. Sauve RS, McMillan DD, Mitchell I, Creighton D, Hindle NW, Young L. Home oxygen therapy: outcome of infants discharged from NICU on continuous treatment. Clin Pediatr. 1989;28:113118 59. Halliday HL, Dumpit FM, Brady JP. Effects of inspired oxygen on echocardiographic assessment of pulmonary vascular resistance and myocardial contractility in bronchopulmonary dysplasia. Pediatrics. 1980;65:536-540 60. Groothuis JR, Rosenberg AA. Home oxygen promotes weight gain in infants with bronchopulmonary dysplasia. Am J Dis Child. 1987;141:992-995 61. Hudak BB, Allen MC, Hudak ML, Loughlin GM. Home oxygen therapy for chronic lung disease in extremely low-birth-weight infants. Am J Dis Child. 1989;143:357-360 62. Garg M, Kurzner SI, Bautista DB, Keens TG. Clinically unsuspected hypoxia during sleep and feeding in infants with bronchopulmonary dysplasia. Pediatrics. 1988;81:635-642 63. Garg M, Kurzner SI, Bautista DB, Keens TG. Hypoxic arousal responses in infants with bronchopulmonary dysplasia. Pediatrics. 1988;82:59-63 64. Schreiner M, Downes J, Kettrick R, Ise C, Voit R. Chronic respiratory failure in infants with prolonged ventilator dependency. JAMA. 1987;258:3398-3404 65. Quint RD, Chesterman E, Crain LS, Winkleby M, Boyce WT. Home care for ventilator-dependent children. Am J Dis Child. 1990;144:1238-1241 66. Klein M, Stern L. Low birth weight and the battered child syndrome. Am J Dis Child. 1971;122:15-18 67. Hunter RS, Kilstrom N, Kraybill EN, Loda F. Antecedents of child abuse and neglect in premature infants: a prospective study in a newborn intensive care unit. Pediatrics. 1978;61:629-635 68. Murphy JF, Jenkins J, Newcombe RG, Sibert JR. Objective birth data and the prediction of child abuse. Arch Dis Child. 1981;56:295-297 69. Khalsa JH, Gfroerer J. Epidemiology and health consequences of drug abuse among pregnant women. Semin Perinatol. 1991;15:265-270 70. Rosenbaum M. Difficulties in taking care of business: women addicts as mothers. Am J Drug Alcohol Abuse. 1979;6:431-447 71. Rosen T, Johnson H. Children of methadone-maintained mothers: follow-up to 18 months of age. J Pediatr. 1982;101:192-196 72. Wilson GS. Clinical studies of infants and children exposed prenatally to heroin. Ann N Y Acad Sci. 1989;562:183-194 73. Gutelius MF, Kirsch AD, MacDonald S, Brooks MR, McErlean T. Controlled study of child health supervision: behavioral results. Pediatrics. 1977;60:294-304 74. Gray JD, Cutler CA, Dean JG, Kempe CH. Prediction and prevention of child abuse and neglect. J Soc Issues. 1979;35:127-139 75. Siegel E, Bauman KE, Schaefer ES, Saunders MM, Ingram DD. Hospital and home support during infancy: impact on maternal attachment, child abuse and neglect, and health care utilization. Pediatrics. 1980;66:183-190 76. Larson CP. Efficacy of prenatal and postpartum home visits on child health and development. Pediatrics. 1980;66:191-197 77. Olds DL, Henderson CR Jr, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78:65-78 78. Barnard KE, Magyary D, Sumner G, Booth CL, Mitchell SK, Spieker S. Prevention of parenting alterations for women with low social support. Psychiatry. 1988;51:248-253 79. Olds DL, Kitzman H. Can home visitation improve the health of women and children at environmental risk? Pediatrics. 1990;86:108-116 80. Green M, Silverman I, Suffet F, Taleporos E, Turkel WV. Outcomes of pregnancy for addicts receiving comprehensive care. Am J Drug Alcohol Abuse. 1979;6:413-429 81. Silverman WA. A hospice setting for humane neonatal death. Pediatrics. 1982;69:239-240 82. Whitfield JM, Siegel RE, Glicken AD, Harmon RJ, Powers LK, Goldson EJ. The application of hospice concepts to neonatal care. Am J Dis Child. 1982;136:421-424 83. Harmon RJ, Glicken AD, Siegel RE. Neonatal loss in the intensive care nursery: effects of maternal grieving and a program for intervention. J Am Acad Child Psychiatry. 1984;23:68-71 84. Martinson IM, Armstrong GD, Geis DP, et al. Home care for children dying of cancer. Pediatrics. 1978;62:106-113 85. Lauer ME, Mulhern RK, Wallskog JM, Camitta BM. A comparison study of parental adaptation following a child's death at home or in the hospital. Pediatrics. 1983;71:107-112 86. Mulhern RK, Lauer ME, Hoffmann RG. Death of a child at home or in the hospital: subsequent psychological adjustment of the family. Pediatrics. 1983;71:743-747 87. Dominica MF. Helen House: a hospice for children. Maternal Child Health. 1982;7:355-359 88. Corr CA, Corr DM. Pediatric hospice care. Pediatrics. 1985;76:774-780 89. Paludetto R, Faggiano-Perfetto M, Asprea AM, de Curtis M, Margara-Paludetto P. Reactions of sixty parents allowed unrestricted contact with infants in a neonatal intensive care unit. Early Hum Dev. 1981;5:401-409 90. Kun S, Warburton D. Telephone assessment of parents' knowledge of home-care treatments and readmission outcomes for high-risk infants and toddlers. Am J Dis Child. 1987;141:888-892 91. American Academy of Pediatrics. Peter G, ed. Red Book: Report of the Committee on Infectious Diseases. 24th ed. Elk Grove Village, IL: American Academy of Pediatrics; 1997 92. American Academy of Pediatrics, Committee on Genetics. Issues in newborn screening. Pediatrics. 1992;89:345-349 93. AAP Section on Endocrinology and Committee on Genetics, American Thyroid Association Committee on Public Health. Newborn screening for congenital hypothyroidism: recommended guidelines. Pediatrics. 1993;91:1203-1209 94. Joint Committee on Infant Hearing. 1994 Position Statement. Pediatrics. 1995;95:152-156 95. American Academy of Pediatrics, American Association for Pediatric Ophthalmology, Strabismus, and the American Academy of Ophthalmology. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 1997;100:273 96. American Academy of Pediatrics, Committee on Children With Disabilities. Guidelines for home care of infants, children, and adolescents with chronic disease. Pediatrics. 1995;96:161-164 97. Corr CA, Corr DM, eds. Hospice Approaches to Pediatric Care. New York, NY: Springer; 1985 98. Affleck G, Tennen H, Rowe J, Roscher B, Walker L. Effects of formal support on mothers' adaptation to the hospital-to-home transition of high-risk infants: the benefits and costs of helping. Child Dev. 1989;60:488-501 99. Pub L No. 99-457. Individuals With Disabilities Education Act. Part H. 1986 100. American Academy of Pediatrics, Task Force on Infant Positioning and SIDS. Positioning and SIDS. Pediatrics. 1992;89:1120-1126 101. American Academy of Pediatrics, Task Force on Infant Positioning and SIDS. Positioning and sudden infant death syndrome (SIDS): update. Pediatrics. 1996;98:1216-1218 102. American Academy of Pediatrics, Committee on Injury and Poison Prevention and Committee on Fetus and Newborn. Safe transportation of premature and low birth weight infants. Pediatrics. 1996;97:758-760 ---------------The recommendations in this statement do not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate. Copyright © 1998 by the American Academy of Pediatrics. No part of this statement may be reproduced in any form or by any means without prior written permission from the American Academy of Pediatrics except for one copy for personal use. Return to Contents Discharge Planning - Reprinted from Respiratory Care [Respir Care 1995;40(12):1308-1312] AARC Clinical Practice Guideline Discharge Planning for the Respiratory Care Patient DPRP 1.0 PROCEDURE: Development and implementat http://www.hsc.missouri.edu/~shrp/rtwww/rcweb/aarc/dprpcpg.html Hot Topic Once a Discharge, Now a Transfer With the implementation of the final rules in the July 31, 1998 Federal Register, what is considered a transfer will now be applicable in many more situations. Effective October 1, 1998 patients discharged from an acute care hospital to one of the following postacute settings will be considered a transfer: o o o o PPS exempt hospitals (psychiatric, rehabilitation, children's, and cancer hospitals), PPS exempt units (psychiatric and rehabilitation) Skilled nursing facilities Home health agency when services are provided within three days after a hospital discharge when the services relate to the condition or diagnosis for which the patient received inpatient hospital services. When the initial acute care falls into one of the 10 DRGs listed below the initial care visit will be reimbursed as a transfer. DRG Title of DRG 14 Specific Cerebrovascular Disorders Except Transient Ischemic Attack 113 Amputation for Circulatory System Disorders Excluding Upper Limb and Toe 209 Major Joint Limb Reattachment Procedures of Lower Extremity 210 Hip and Femur Procedures Except Major Joint Age >17 with CC 211 Hip and Femur Procedures Except Major Joint Age >17 without CC 236 Fractures of Hip and Pelvis 263 Skin Graft and/or Debridement for Skin Ulcer or Cellulitis With CC 264 Skin Graft and/or Debridement for Skin Ulcer or Cellulitis Without CC 429 Organic Disturbances and Mental Retardation 483 Tracheostomy Except for Face, Mouth and Neck Diagnoses The DRGs listed above represent the highest percentage of discharges to postacute care. For each DRG selected consideration was given for the volume and percentage of discharges to postacute care before the mean length of stay was reached and whether discharges occurring early in the stay would increase the likelihood of postacute care. One of two payment methodologies will be used for qualified transfers. DRGs 209, 210, and 211 will be reimbursed at 50 percent of the DRG payment for the first day of the stay and 50 percent of the per diem for the remaining days of the stay. The remaining 7 DRGs will be reimbursed by the current transfer payment methodology, twice the per diem for the first day and the per diem for each subsequent day. Both payment methodologies are not to exceed the normal DRG reimbursement. Return to Hot Topics Index Home http://www.aap.org/policy/re9810.html Guidelines for Developing Admission and Discharge Policies for the Pediatric Intensive Care Unit (RE9810) Policy Statement Pediatrics Volume 103, Number 4 April 1999, pp 840-842 Guidelines for Developing Admission and Discharge Policies for the Pediatric Intensive Care Unit (RE9810) AMERICAN ACADEMY OF PEDIATRICS Committee on Hospital Care and Section on Critical Care SOCIETY OF CRITICAL CARE MEDICINE Pediatric Section Admission Criteria Task Force These guidelines were developed to provide a reference for preparing policies on admission to and discharge from pediatric intensive care units. They represent a consensus opinion of physicians, nurses, and allied health care professionals. By using this document as a framework for developing multidisciplinary admission and discharge policies, use of pediatric intensive care units can be optimized and patients can receive the level of care appropriate for their condition. ABBREVIATION. PICU, pediatric intensive care unit. It should be understood that critically ill pediatric patients should be admitted to designated pediatric critical care beds.1 The following are recommended as guidelines for admission and discharge for pediatric intensive care units (PICUs). The purpose of these guidelines is to provide a reference for admitting and subsequently discharging critically ill pediatric patients. Because of continuing developments in pediatric critical care, periodic review of these criteria is necessary. These guidelines must be adapted and modified to each institution's policies and procedures regarding the nature and scope of the critical illnesses seen in that institution1 and the interhospital transfer arrangements of each institution. Physiologic parameters should be added to these guidelines by each institution so that patients may be triaged appropriately in and out of the intensive care unit. PREPARING GUIDELINES FOR INDIVIDUAL UNITS The following listing is not meant to be inclusive, nor is it necessary for every PICU to admit all patients with every condition listed. However, the following has been prepared for the multiprofessional team developing such criteria to consider when developing admission and discharge policies. In addition, accrediting agencies have recommended that physiologic limits be placed wherever possible in preparing admission and discharge policies. For example, a "potassium of 6.0 mEq/L" may be selected to indicate admission to the intensive care unit rather than simply "hyperkalemia." ADMISSION CRITERIA Respiratory System Patients with severe or potentially life-threatening pulmonary or airway disease. Conditions include, but are not limited to: 1. Endotracheal intubation or potential need for emergency endotracheal intubation and mechanical ventilation, regardless of etiology; 2. Rapidly progressive pulmonary, lower or upper airway, disease of high severity with risk of progression to respiratory failure and/or total obstruction; 3. High supplemental oxygen requirement (F1O2>0.5), regardless of etiology; 4. Newly placed tracheostomy with or without the need for mechanical ventilation; 5. Acute barotrauma compromising the upper or lower airway; 6. Requirement for more frequent or continuous inhaled or nebulized medications than can be administered safely on the general pediatric patient care unit (according to institution guidelines). Cardiovascular System Patients with severe, life-threatening, or unstable cardiovascular disease. Conditions include, but are not limited to: 1. 2. 3. 4. 5. 6. 7. 8. Shock; Postcardiopulmonary resuscitation; Life-threatening dysrhythmias; Unstable congestive heart failure, with or without need for mechanical ventilation; Congenital heart disease with unstable cardiorespiratory status; After high-risk cardiovascular and intrathoracic procedures; Need for monitoring of arterial, central venous, or pulmonary artery pressures; Need for temporary cardiac pacing. Neurologic Patients with actual or potential life-threatening or unstable neurologic disease. Conditions include, but are not limited to: 1. Seizures, unresponsive to therapy or requiring continuous infusion of anticonvulsive agents; 2. Acutely and severely altered sensorium where neurologic deterioration or depression is likely or unpredictable, or coma with the potential for airway compromise; 3. After neurosurgical procedures requiring invasive monitoring or close observation; 4. Acute inflammation or infections of the spinal cord, meninges, or brain with neurologic depression, metabolic and hormonal abnormalities, and respiratory or hemodynamic compromise or the possibility of increased intracranial pressure; 5. Head trauma with increased intracranial pressure; 6. Preoperative neurosurgical conditions with neurologic deterioration; 7. Progressive neuromuscular dysfunction with or without altered sensorium requiring cardiovascular monitoring and/or respiratory support; 8. Spinal cord compression or impending compression; 9. Placement of external ventricular drainage device. Hematology/Oncology Patients with life-threatening or unstable hematologic or oncologic disease or active lifethreatening bleeding. Conditions include, but are not limited to: 1. 2. 3. 4. 5. Exchange transfusions; Plasmapheresis or leukopheresis with unstable clinical condition; Severe coagulopathy; Severe anemia resulting in hemodynamic and/or respiratory compromise; Severe complications of sickle cell crisis, such as neurologic changes, acute chest syndrome, or aplastic anemia with hemodynamic instability; 6. Initiation of chemotherapy with anticipated tumor lysis syndrome; 7. Tumors or masses compressing or threatening to compress vital vessels, organs, or airway. Endocrine/Metabolic Patients with life-threatening or unstable endocrine or metabolic disease. Conditions include, but are not limited to: 1. Severe diabetic ketoacidosis requiring therapy exceeding institutional patient care unit guidelines. (If hemodynamic or neurologic compromise, see specific section); 2. Other severe electrolyte abnormalities, such as: • Hyperkalemia, requiring cardiac monitoring and acute therapeutic intervention • Severe hypo- or hypernatremia • Hypo- or hypercalcemia • Hypo- or hyperglycemia requiring intensive monitoring Severe metabolic acidosis requiring bicarbonate infusion, intensive monitoring, or complex intervention • Complex intervention required to maintain fluid balance 3. Inborn errors of metabolism with acute deterioration requiring respiratory support, acute dialysis, hemoperfusion, management of intracranial hypertension, or inotropic support. Gastrointestinal Patients with life-threatening or unstable gastrointestinal disease. Conditions include, but are not limited to: 1. Severe acute gastrointestinal bleeding leading to hemodynamic or respiratory instability; 2. After emergency endoscopy for removal of foreign bodies; 3. Acute hepatic failure leading to coma, hemodynamic, or respiratory instability. Surgical Postoperative patients requiring frequent monitoring and potentially requiring intensive intervention. Conditions include, but are not limited to: 1. Cardiovascular surgery; 2. Thoracic surgery; 3. Neurosurgical procedures; 4. Otolaryngologic surgery; 5. Craniofacial surgery; 6. Orthopedic and spine surgery; 7. General surgery with hemodynamic or respiratory instability; 8. Organ transplantation; 9. Multiple trauma with or without cardiovascular instability; 10. Major blood loss, either during surgery or during the postoperative period. Renal System Patients with life-threatening or unstable renal disease. Conditions include, but are not limited to: 1. Renal failure; 2. Requirement for acute hemodialysis, peritoneal dialysis, or other continuous renal replacement therapies in the unstable patient; 3. Acute rhabdomyolysis with renal insufficiency. Multisystem and Other Patients with life-threatening or unstable multisystem disease. Conditions include, but are not limited to: 1. Toxic ingestions and drug overdose with potential acute decompensation of major organ systems; 2. Multiple organ dysfunction syndrome; 3. Suspected or documented malignant hyperthermia; 4. Electrical or other household or environmental (eg, lightning) injuries; 5. Burns covering >10% of body surface (institutions with burn units only; institutions without such units will have transfer policy to cover such patients). Special Intensive Technologic Needs Conditions that necessitate the application of special technologic needs, monitoring, complex intervention, or treatment including medications associated with the disease that exceed individual patient care unit policy limitations. DISCHARGE/TRANSFER CRITERIA Patients in the PICU will be evaluated and considered for discharge based on the reversal of the disease process or resolution of the unstable physiologic condition that prompted admission to the unit, and it is determined that the need for complex intervention exceeding general patient care unit capabilities is no longer needed. Transfer/discharge will be based on the following criteria: 1. Stable hemodynamic parameters; 2. Stable respiratory status (patient extubated with stable arterial blood gases) and airway patency; 3. Minimal oxygen requirements that do not exceed patient care unit guidelines; 4. Intravenous inotropic support, vasodilators, and antiarrhythmic drugs are no longer required or, when applicable, low doses of these medications can be administered safely in otherwise stable patients in a designated patient care unit; 5. Cardiac dysrhythmias are controlled; 6. Intracranial pressure monitoring equipment has been removed; 7. Neurologic stability with control of seizures; 8. Removal of all hemodynamic monitoring catheters; 9. Chronically mechanically ventilated patients whose critical illness has been reversed or resolved and who are otherwise stable may be discharged to a designated patient care unit that routinely manages chronically ventilated patients, when applicable, or to home; 10. Routine peritoneal or hemodialysis with resolution of critical illness not exceeding general patient care unit guidelines; 11. Patients with mature artificial airways (tracheostomies) who no longer require excessive suctioning; 12. The health care team and the patient's family, after careful assessment, determine that there is no benefit in keeping the child in the PICU or that the course of treatment is medically futile.2 COMMITTEE ON HOSPITAL CARE, 1998-1999 Henry A. Schaeffer, MD, Chairperson David R. Hardy, MD Paul H. Jewett, MD John M. Neff, MD John M. Packard, Jr, MD Joseph A. Snitzer III, MD Curt M. Steinhart, MD LIAISON REPRESENTATIVES Eugene Wiener, MD National Association of Children's Hospital and Related Institutions Mary T. Perkins, RN, DNSC Society of Pediatric Nurses Elias Rosenblatt, MD Joint Commission on Accreditation of Health Care Organizations Elizabeth J. Ostric American Hospital Association Jerriann M. Wilson Association for the Care of Children's Health AAP SECTION LIAISON Theodore Striker, MD Section on Anesthesiology SECTION ON CRITICAL CARE, 1998-1999 Timothy S. Yeh, MD, Chairperson Kristan M. Outwater, MD, Ex-Officio Alice Ackerman, MD Harold N. Amer, MD M. Michele Moss, MD Daniel A. Notterman, MD Stephanie A. Storgion, MD SOCIETY OF CRITICAL CARE MEDICINE, PEDIATRIC SECTION MISSION CRITERIA TASK FORCE David Jaimovich, MD, Chairperson Gabriel "Gabby" Hauser, MD Madolin Witte, MD Jackson Wong, MD Tom Rice, MD Jan Kronick, MD Kristan Outwater, MD Sara White, MD Kathy Rosenthal, RN, MN, CCRN Scott LeBard, MD Lucian K. DeNicola, MD REFERENCES 1. 2. American Academy of Pediatrics, Committee on Hospital Care and Pediatric Section of the Society of Critical Care Medicine. Guidelines and levels of care for pediatric intensive care units. Pediatrics 1993;92:166-175; Crit Care Med. 1993;21:931-937 Ethics Committee, Society of Critical Care Medicine. Consensus statement of the SCCM Ethics Committee regarding futile and other possibly inadvisable treatments. Crit Care Med. 1997;25:887-891 ---------------- The recommendations in this statement do not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate. Copyright © 1999 by the American Academy of Pediatrics. No part of this statement may be reproduced in any form or by any means without prior written permission from the American Academy of Pediatrics except for one copy for personal use. Return to Contents Policy Statement Pediatrics Volume 103, Number 4 April 1999, pp 840-842 Guidelines for Developing Admission and Discharge Policies for the Pediatric Intensive Care Unit (RE9810) AMERICAN ACADEMY OF PEDIATRICS Committee on Hospital Care and Section on Critical Care SOCIETY OF CRITICAL CARE MEDICINE Pediatric Section Admission Criteria Task Force These guidelines were developed to provide a reference for preparing policies on admission to and discharge from pediatric intensive care units. They represent a consensus opinion of physicians, nurses, and allied health care professionals. By using this document as a framework for developing multidisciplinary admission and discharge policies, use of pediatric intensive care units can be optimized and patients can receive the level of care appropriate for their condition. ABBREVIATION. PICU, pediatric intensive care unit. It should be understood that critically ill pediatric patients should be admitted to designated pediatric critical care beds.1 The following are recommended as guidelines for admission and discharge for pediatric intensive care units (PICUs). The purpose of these guidelines is to provide a reference for admitting and subsequently discharging critically ill pediatric patients. Because of continuing developments in pediatric critical care, periodic review of these criteria is necessary. These guidelines must be adapted and modified to each institution's policies and procedures regarding the nature and scope of the critical illnesses seen in that institution1 and the interhospital transfer arrangements of each institution. Physiologic parameters should be added to these guidelines by each institution so that patients may be triaged appropriately in and out of the intensive care unit. PREPARING GUIDELINES FOR INDIVIDUAL UNITS The following listing is not meant to be inclusive, nor is it necessary for every PICU to admit all patients with every condition listed. However, the following has been prepared for the multiprofessional team developing such criteria to consider when developing admission and discharge policies. In addition, accrediting agencies have recommended that physiologic limits be placed wherever possible in preparing admission and discharge policies. For example, a "potassium of 6.0 mEq/L" may be selected to indicate admission to the intensive care unit rather than simply "hyperkalemia." ADMISSION CRITERIA Respiratory System Patients with severe or potentially life-threatening pulmonary or airway disease. Conditions include, but are not limited to: 1. Endotracheal intubation or potential need for emergency endotracheal intubation and mechanical ventilation, regardless of etiology; 2. Rapidly progressive pulmonary, lower or upper airway, disease of high severity with risk of progression to respiratory failure and/or total obstruction; 3. High supplemental oxygen requirement (F1O2>0.5), regardless of etiology; 4. Newly placed tracheostomy with or without the need for mechanical ventilation; 5. Acute barotrauma compromising the upper or lower airway; 6. Requirement for more frequent or continuous inhaled or nebulized medications than can be administered safely on the general pediatric patient care unit (according to institution guidelines). Cardiovascular System Patients with severe, life-threatening, or unstable cardiovascular disease. Conditions include, but are not limited to: 1. Shock; 2. Postcardiopulmonary resuscitation; 3. Life-threatening dysrhythmias; 4. Unstable congestive heart failure, with or without need for mechanical ventilation; 5. Congenital heart disease with unstable cardiorespiratory status; 6. After high-risk cardiovascular and intrathoracic procedures; 7. Need for monitoring of arterial, central venous, or pulmonary artery pressures; 8. Need for temporary cardiac pacing. Neurologic Patients with actual or potential life-threatening or unstable neurologic disease. Conditions include, but are not limited to: 1. Seizures, unresponsive to therapy or requiring continuous infusion of anticonvulsive agents; 2. Acutely and severely altered sensorium where neurologic deterioration or depression is likely or unpredictable, or coma with the potential for airway compromise; 3. After neurosurgical procedures requiring invasive monitoring or close observation; 4. Acute inflammation or infections of the spinal cord, meninges, or brain with neurologic depression, metabolic and hormonal abnormalities, and respiratory or hemodynamic compromise or the possibility of increased intracranial pressure; 5. Head trauma with increased intracranial pressure; 6. Preoperative neurosurgical conditions with neurologic deterioration; 7. Progressive neuromuscular dysfunction with or without altered sensorium requiring cardiovascular monitoring and/or respiratory support; 8. Spinal cord compression or impending compression; 9. Placement of external ventricular drainage device. Hematology/Oncology Patients with life-threatening or unstable hematologic or oncologic disease or active lifethreatening bleeding. Conditions include, but are not limited to: 1. 2. 3. 4. 5. Exchange transfusions; Plasmapheresis or leukopheresis with unstable clinical condition; Severe coagulopathy; Severe anemia resulting in hemodynamic and/or respiratory compromise; Severe complications of sickle cell crisis, such as neurologic changes, acute chest syndrome, or aplastic anemia with hemodynamic instability; 6. Initiation of chemotherapy with anticipated tumor lysis syndrome; 7. Tumors or masses compressing or threatening to compress vital vessels, organs, or airway. Endocrine/Metabolic Patients with life-threatening or unstable endocrine or metabolic disease. Conditions include, but are not limited to: 1. Severe diabetic ketoacidosis requiring therapy exceeding institutional patient care unit guidelines. (If hemodynamic or neurologic compromise, see specific section); 2. Other severe electrolyte abnormalities, such as: • Hyperkalemia, requiring cardiac monitoring and acute therapeutic intervention • Severe hypo- or hypernatremia • Hypo- or hypercalcemia • Hypo- or hyperglycemia requiring intensive monitoring Severe metabolic acidosis requiring bicarbonate infusion, intensive monitoring, or complex intervention • Complex intervention required to maintain fluid balance 3. Inborn errors of metabolism with acute deterioration requiring respiratory support, acute dialysis, hemoperfusion, management of intracranial hypertension, or inotropic support. Gastrointestinal Patients with life-threatening or unstable gastrointestinal disease. Conditions include, but are not limited to: 1. Severe acute gastrointestinal bleeding leading to hemodynamic or respiratory instability; 2. After emergency endoscopy for removal of foreign bodies; 3. Acute hepatic failure leading to coma, hemodynamic, or respiratory instability. Surgical Postoperative patients requiring frequent monitoring and potentially requiring intensive intervention. Conditions include, but are not limited to: 1. 2. 3. 4. 5. 6. 7. Cardiovascular surgery; Thoracic surgery; Neurosurgical procedures; Otolaryngologic surgery; Craniofacial surgery; Orthopedic and spine surgery; General surgery with hemodynamic or respiratory instability; 8. Organ transplantation; 9. Multiple trauma with or without cardiovascular instability; 10. Major blood loss, either during surgery or during the postoperative period. Renal System Patients with life-threatening or unstable renal disease. Conditions include, but are not limited to: 1. Renal failure; 2. Requirement for acute hemodialysis, peritoneal dialysis, or other continuous renal replacement therapies in the unstable patient; 3. Acute rhabdomyolysis with renal insufficiency. Multisystem and Other Patients with life-threatening or unstable multisystem disease. Conditions include, but are not limited to: 1. Toxic ingestions and drug overdose with potential acute decompensation of major organ systems; 2. Multiple organ dysfunction syndrome; 3. Suspected or documented malignant hyperthermia; 4. Electrical or other household or environmental (eg, lightning) injuries; 5. Burns covering >10% of body surface (institutions with burn units only; institutions without such units will have transfer policy to cover such patients). Special Intensive Technologic Needs Conditions that necessitate the application of special technologic needs, monitoring, complex intervention, or treatment including medications associated with the disease that exceed individual patient care unit policy limitations. DISCHARGE/TRANSFER CRITERIA Patients in the PICU will be evaluated and considered for discharge based on the reversal of the disease process or resolution of the unstable physiologic condition that prompted admission to the unit, and it is determined that the need for complex intervention exceeding general patient care unit capabilities is no longer needed. Transfer/discharge will be based on the following criteria: 1. Stable hemodynamic parameters; 2. Stable respiratory status (patient extubated with stable arterial blood gases) and airway patency; 3. Minimal oxygen requirements that do not exceed patient care unit guidelines; 4. Intravenous inotropic support, vasodilators, and antiarrhythmic drugs are no longer required or, when applicable, low doses of these medications can be administered safely in otherwise stable patients in a designated patient care unit; 5. Cardiac dysrhythmias are controlled; 6. Intracranial pressure monitoring equipment has been removed; 7. Neurologic stability with control of seizures; 8. Removal of all hemodynamic monitoring catheters; 9. Chronically mechanically ventilated patients whose critical illness has been reversed or resolved and who are otherwise stable may be discharged to a designated patient care unit that routinely manages chronically ventilated patients, when applicable, or to home; 10. Routine peritoneal or hemodialysis with resolution of critical illness not exceeding general patient care unit guidelines; 11. Patients with mature artificial airways (tracheostomies) who no longer require excessive suctioning; 12. The health care team and the patient's family, after careful assessment, determine that there is no benefit in keeping the child in the PICU or that the course of treatment is medically futile.2 COMMITTEE ON HOSPITAL CARE, 1998-1999 Henry A. Schaeffer, MD, Chairperson David R. Hardy, MD Paul H. Jewett, MD John M. Neff, MD John M. Packard, Jr, MD Joseph A. Snitzer III, MD Curt M. Steinhart, MD LIAISON REPRESENTATIVES Eugene Wiener, MD National Association of Children's Hospital and Related Institutions Mary T. Perkins, RN, DNSC Society of Pediatric Nurses Elias Rosenblatt, MD Joint Commission on Accreditation of Health Care Organizations Elizabeth J. Ostric American Hospital Association Jerriann M. Wilson Association for the Care of Children's Health AAP SECTION LIAISON Theodore Striker, MD Section on Anesthesiology SECTION ON CRITICAL CARE, 1998-1999 Timothy S. Yeh, MD, Chairperson Kristan M. Outwater, MD, Ex-Officio Alice Ackerman, MD Harold N. Amer, MD M. Michele Moss, MD Daniel A. Notterman, MD Stephanie A. Storgion, MD SOCIETY OF CRITICAL CARE MEDICINE, PEDIATRIC SECTION MISSION CRITERIA TASK FORCE David Jaimovich, MD, Chairperson Gabriel "Gabby" Hauser, MD Madolin Witte, MD Jackson Wong, MD Tom Rice, MD Jan Kronick, MD Kristan Outwater, MD Sara White, MD Kathy Rosenthal, RN, MN, CCRN Scott LeBard, MD Lucian K. DeNicola, MD REFERENCES 1. 2. American Academy of Pediatrics, Committee on Hospital Care and Pediatric Section of the Society of Critical Care Medicine. Guidelines and levels of care for pediatric intensive care units. Pediatrics 1993;92:166-175; Crit Care Med. 1993;21:931-937 Ethics Committee, Society of Critical Care Medicine. Consensus statement of the SCCM Ethics Committee regarding futile and other possibly inadvisable treatments. Crit Care Med. 1997;25:887-891 ---------------The recommendations in this statement do not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate. Copyright © 1999 by the American Academy of Pediatrics. No part of this statement may be reproduced in any form or by any means without prior written permission from the American Academy of Pediatrics except for one copy for personal use. Return to Contents http://www.rcjournal.com/online_resources/cpgs/dprpcpg.html Totally Kids® Specialty Healthcare Pediatric Subacute Care for Medically-Fragile Technology Dependent Children Totally Kids® Tierra's Journey Home Includes a Subacute Stay Reprinted with permission from SubacuteCare Today, a Publication of Daedalus Enterprises, Inc., Dallas, TX. "With the advent of more complex and successful methods of treating traumatic events and premature births in pediatric and neonatal ICUs, long-term survival rates for this population have reached an unprecedented level. But survivors of these events often require long-term and/or complex care -- sometimes for their entire lives. Thus, the families of these children find themselves responsible for gastrostomy tubes, tracheostomy tubes, ventilators, indwelling lines, and assessment -tasks usually reserved for licensed personnel in the intensive care units of tertiary care medical centers. Challenges like these have created the need for appropriate settings where children can be cared for during the sometimes lengthy process of training the family and preparing the home for the child's return. These are children who require well-trained, qualified medical staff from a variety of disciplines who can maintain the child's stability while assisting both the child and the family in overcoming the psychological traumas that an extended ICU stay can create. The ideal setting will have fewer restrictions than an ICU and allow for a child's need for play and social interaction with family and peers. This setting should also include methods and facilities that encourage family participation in the day-to-day care of the child, allowing them to integrate their child's new needs into the daily routines of parenting while making a realistic assessment of the support structures that will be necessary to make the transition to home safe and comfortable. All of these needs point to the level of care that has come to be recognized as 'subacute.' This may also be termed 'chronic intensive care' but is currently more readily recognized by government agencies, HMOs, and managed care plans as subacute care. Recovering from too early a start One child who has benefited greatly from this level of care is Tierra, the two-year old daughter of Tanya and Tyrone Holloway. Tierra was born prematurely at Barstow community hospital on December 12, 1995, at 27 weeks gestation and weighing 794 grams. She was intubated and placed on ventilatory support due to immaturity of the pulmonary system, and transferred to the NICU at Loma Linda Children's Hospital. There she was maintained on mechanical ventilation and had a tracheostomy tube placed for long-term ventilation and bronchopulmonary hygiene. Her nutrition was maintained via a nasogastric tube. She received rehabilitation services from occupational, speech and physical therapists. Tierra resided in the NICU from December 1995 to October 1996 and grew from her original weight to 5,790 grams. At that time, Tierra's physicians felt that she had stabilized and needed to transition to an environment that was less restrictive than an NICU and could offer her a more normal growth experience. "At first we wanted to take her home right away, but the doctors told us she may not make it home." Tanya explains, "so the doctors at the hospital told us a subacute was the only option." Her case managers referred her to Totally Kids® Specialty Healthcare. Totally Kids®, a division of Mountain View Child Care Inc., is a 59-bed subacute facility dedicated to serving the needs of children and adolescents. Tierra was transferred in October 1996. The staff at Totally Kids® constructed an individual care plan, which included consultation by a pediatrician, pediatric intensivist, pediatric physiatrist (a physician specializing in rehabilitation medicine), ear-nose-throat specialist, neurologist, RN's, respiratory care practitioners, occupational therapists, physical therapists, speech, a child-life specialist, social worker, and case management staff - all coordinated by the facility's full-time nurse practitioner in conjunction with Tierra's parents. Paramount to a successful transition was the resolution of the logistical problems arising from the fact that Tierra's parents lived 115 miles away. Tierra's case manager, Deborah Wilson, RN, BSN, assisted Tyrone in his efforts to arrange for leave from the military by writing letters to Tyrone's commanding officers explaining his daughter's fragile medical condition. The Kids-4-Ever House, a not-for-profit facility located next to the Totally Kids® Healthcare Center, was offered to the couple for a nominal fee, allowing them to stay in the area for several days at a time, decreasing their transportation and lodging costs. This allowed Tanya and Tyrone to maximize the amount of time they could spend with their infant daughter. Special attention makes the difference At Totally Kids®, Tierra improved developmentally at a faster pace than in the acute facility. She began to take food orally under the supervision of the speech and occupational therapists and was increasingly responsive to her outside environment. With outside stimulus from the child-life specialist and aides, she also showed increased social activities. The Holloways attribute a large portion of Tierra's remarkable improvement to the level of special attention she has received in this setting. Not only has she had an opportunity to interact with the staff, she has been able to socialize with other children at the facility as well. Far from being the sterile, clinical environment of an ICU, Totally Kids® allows and encourages children to socialize with one another when they can, and children receive lots of individual attention from the staff members. Of course, Tierra's stay has not been without its complications. For a long period, Tierra experienced frequent nausea related to the nasogastric tube. This often resulted in vomiting and dislodgment of the nasogastric tube and, frequently, dislodgment of the tracheostomy tube as well. The nursing staff at the center became increasingly concerned for her well being and related this to her family, recommending placement of a gastrostomy tube. Multiple meetings were held with the family and the doctors to explain all of the risks, benefits, and alternatives to the gastrostomy tube. Dr. Menaj Shah, the facility's pediatricgastroenterologist, was particularly helpful, spending three hours with Tanya and Tyrone explaining the procedures' benefits and answering questions. After much thought, Tierra's parents consented to the gastrostomy tube placement, which they had been hesitant to agree to while at the Children's Hospital, and the surgery was performed. Tierra's condition improved dramatically. Her bouts of vomiting decreased, and her incidence of tracheostomy dislodgments dropped as well. She increased her oral food intake and became more social. Without the regular bouts of nausea, her respiratory status also improved. Ongoing challenges The level of personal attention that the family has received at Totally Kids® has impacted Tierra's care in many other ways as well. Tyrone Holloway explains that while he and his wife appreciated the clinical expertise of the staff in the acute care setting, the smaller, more relaxed and informal setting of a subacute facility has made them feel more at ease. Tanya welcomes the feedback, she gets from the staff and says, "Everyone here is positive. The staff always reports to me about everything Tierra does." Initially wary of health care personnel, Tyrone has warmed to the idea of getting involved with Tierra's care. Today he assists his wife and the staff with all of Tierra's care-- from gastrostomy tube feedings to tracheostomy tube changes. A continuing concern for parents of special needs children and pediatric subacute providers alike, however, is the failure of commercial providers to recognize pediatric subacute as a cost-effective transitional level of care. While pediatric subacute care can often supplant a large portion of a child's stay in the ICU or a general acute floor, the process of convincing third-party payors that this level of care is not simply "skilled nursing for kids" is an ongoing challenge. The Holloways have experienced this challenge first hand. Tierra's care was originally funded by CHAMPUS. But CHAMPUS terminated Tierra's funding based on their determination that she requires only maintenance care. While this determination is under appeal, Tierra's care is being paid for by California's Medicaid program, which is a provision for pediatric subacute care. It is difficult, however, to obtain Medicaid funding for the therapy services Tierra continues to require. While that issue is being resolved, the facility continues to provide full therapy services. Making good progress The Holloways believe that communication is the key to providing quality care and keeping families involved their children's care. One way that Totally Kids® strives to keep the lines of communication open is through regular care plan meetings. Upon admission, the multidisciplinary team of professionals develops an individual care plan for each child. These plans are reviewed and revised each quarter and whenever there is significant change in the child's condition or method of treatment, and the families are always invited to participate. While the Holloways enjoy receiving on-going reports from the staff in the hall or in the break room, they appreciate the opportunity to give their input and ask their questions at these formal meetings. Tierra is progressing well, has grown to a weight of 9,700 grams, and has transitioned from the acute care ventilator that she was on when she arrived at Totally Kids® to a ventilator that can be used in the home. With the care of respiratory therapists and specially trained nursing staff, under the direction of Totally Kids®' pediatric intensivist, Dr. Daved Van Stralen (who is also the co-director of the Loma Linda University Children's Hospital Pediatric ICU), her respiratory status has improved to the point where she is able to tolerate being off the ventilator for up to six hours a day. During her time off the ventilator, Tierra is learning how to crawl with the assistance of Oradelle Lizer, the physical therapist. Occupational therapist Sandie Stringer is teaching her fine motor skills via interactive play, and her parents take her for strolls around the grounds and the facility. Hesitant to make eye contact with people in the past, Tierra is now starting to focus on her family and favorite staff, and enjoys her time off the ventilator in the playpen with her favorite toys -- a vast improvement over the days when her favored object of play was a coil of ventilator tubing the staff had made for her to keep her hands awayfrom her tracheostomy tube. 'The best place for her' The Holloways had originally planned to return home to Virginia after Tyrone's discharge from the service last June. But they have become so comfortable with the care Tierra is receiving at Totally Kids® that they have decided to become residents of California and have relocated to a home near the facility. At this writing in mid-fall (1997), Tanya and Tyrone were planning to take Tierra home in December of 1997, with assistance from a home health agency. Says Tyrone, 'Everyone knows her here - all the doctors and the staff. This is the best place for her.'" Last modified: August 14, 2000 http://www.totallykids.com/articles.htm Improving Care