Effect of parathyroidectomy on symptoms and quality of life in
advertisement

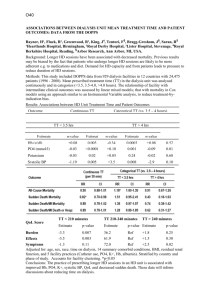
Word Count:1634 Effect of parathyroidectomy on symptoms and quality of life in patients with end-stage renal disease Su-Chen Yang1 Wan-Ching Chao1 Chih-Kang Chiang4 Shih-Ping Hsu2 Yu-Sen Peng2 Kuan-Yu Hung4 Shih-Horng Huang3 Kai-Wei Wang5 Far Eastern Memorial Hospital, Department of Nursing 1Department of Nephrology 2 Department of Surgery3, National Taiwan University Hospital, Department of Nephrology 4 Institute of Nursing National Yang-Ming University.5 Address correspondence to Kai-Wei Wang, Institute of Nursing National Yang-Ming University. Far Eastern Memorial Hospital, No.21, Sec.2 Nan-Ya South Road, Pan-Chiao, Taipei, Taiwan. E-mail: didoyangster@gmail.com , dido.yang@msa.hinet.net Running title: parathyroidectomy and quality of life 1 Abstract Background: Purpose was to measure quality of life (QOL) and symptom distress in dialysis patients before and after parathyroidectomy. Methods: We enrolled 37 dialysis patients who underwent parathyroidectomy at the medical center. QOL was measured with the Health Survey (SF-36) and symptom distress was evaluated by use of the Visual Analogue Scale (VAS). Results: The results indicated that joint pain, muscle weakness, and itchy skin were the most annoying symptoms. The QOL before surgery indicated a physical component summary score of 31.7 ± 13.8 and a mental component summary score of 37.6 ± 14.4. A total of 32 patients (86.5%) reported experiencing adverse symptoms. After surgery, there was a statistically significant reduction of symptoms. There was a positive correlation between the calcium-phosphorus product and skin itching. Symptom distress were significantly reduced after surgery. Conclusion: Our results indicate that parathyroidectomy of dialysis patients with hyperparathyroidism can relieve many symptoms and improve QOL. Keywords: ESRD, Hyperparathyroidism, symptoms distress, quality of life 2 Introduction Secondary hyperparathyroidism due to hypocalcemia is common in patients with end-stage renal disease (ESRD) 〔18〕 The increased production of parathyroid hormone (PTH) causes calcium to be re-absorbed from bone, so that more calcium is taken up by the intestines and kidney If the parathyroid glands are unable to respond to the increased levels of calcium, tertiary hyperparathyroidism and hypercalcemia can result. This condition is associated with complications, such as psychological and neurological disorders, ectopic ossification in the cardiovascular system, imbalanced nutrition, and inflammation, that can severely compromise quality of life (QOL) and increase the probability of mortality〔4,12〕. According to Locatelli 〔5〕, the prevalence of parathyroidectomy among dialysis patients is about 5.5%. In Taiwan, about 59,000 ESRD patients require long-term dialysis (Taiwan Kidney Foundation, 2008). Taiwan has a very high prevalence of ESRD, and our patient-centered healthcare system must consider 〔15,16〕hyperparathyroidism in order to improve patient QOL〔7,14〕. The daily life of a dialysis patient is often stressed by physical symptoms 〔3,8〕, and hyperparathyroidism can add to this burden by increasing bone disease, pain, pruritis, and muscle weakness. 〔11〕 Internal medicine specialists can often use one or more medications to successfully treat kidney disease patients with hyperparathyroidism. However, if the level of PTH is greater than 500 pg/mL, the parathyroid gland is heavier than 500 mg, or the patient has severe osteitis fibrosa, then parathyroidectomy is indicated to alleviate the symptoms 〔9,,10,17〕In the present study, we examined the QOL of ESRD patients before and after parathyroidectomy. The results serve as a basis for clinical decision-making and education of healthcare workers. Materials and Methods (1) Subjects This was a follow-up study that enrolled patients by convenience sampling. All subjects were ESRD patients on peritoneal dialysis or hemodialysis for more than three months and received subtotal parathyroidectomy at our hospital. All enrolled patients were age 18 years or older, had clear consciousness and no mental disorder, had the ability to speak clearly, had no active malignancy, and were not pregnant. After hospital admission, we explained the research goals to patients and families, and obtained informed consent for participation in the survey. Participation was voluntary. In order to understand each patient’s symptoms of stress and QOL, questionnaires 3 were distributed before parathyroidectomy, one month after parathyroidectomy, and three months after parathyroidectomy, (2) Research tools and measurements The Visual Analogue Scale (VAS) and the Health Survey (SF-36) were used to assess subjective feelings of patients. The VAS is a psychometric measure of a patient's perception of joint pain, muscle weakness, and skin itches, with lower scores indicating better QOL. The SF-36 assesses a patient's health-related QOL and assesses a subject's physical and mental health status in eight categories with a total of 36 questions: physical function (PF), ten questions; role limitation due to physical problems (RP), four questions; bodily pain (BP), two questions; general health (GH), five questions; vitality (VT), four questions; social function (SF), two questions; role limitation due to emotional problems (RE), three questions; mental health (MH), five questions; one question on reported health transition for the past year. SF-36 scores were expressed as individual scores in each of the eight categories, with scores ranging from zero to one hundred. Finally, the scores were also summarized a physical component summary score (PCS) and a mental component summary score (MCS). Higher scores indicate better QOL 〔1〕. Additional background information was also collected, including age, gender, education, occupation, marital status, religion, primary disease that led to ESRD, dialysis modality (hemodialysis or peritoneal dialysis), dialysis frequency, total months of dialysis, presence of other chronic diseases, and routine blood biochemistry and blood cell counts. All statistical analysis was conducted with SPSS 12.0 software (SAS, Chicago, IL). Demographic characteristics, dialysis-related information, and VAS scores were analyzed with descriptive statistics, including average, median, standard deviation, and 25th and 75th percentiles. Pre- and post-surgical laboratory tests and SF-36 scores were reported as average, median, and percentile. The difference between these variables was examined with a nonparametric test. The presence of correlation between variables and the strength of the correlation was measured with the Wilcoxon signed-rank test. Results Thirty-seven questionnaires were distributed before and one month after surgery, and 36 were distributed at the three-month follow-up (CAD due to the death of one patient). The response rate was 100%. 4 (1) Patient Demographics Table 1 shows basic patient demographics. The average patient age was 54.6 ± 11.72 years, 21 of 37 (56.8%) patients were female, and 25 (67.6%) patients were married. A total of 91.9% of patients had a high school education or less, 21% had stable employment, 43.2% were homemakers, and 2.7% were able to work but remained unemployed. The major religion was Taoism (51.4%). The average PCS and MCS of females were 29.56 ± 14.62 and 36.83 ± 16.60, respectively. The average PCS and MCS of males were 34.53 ± 12.50 and 38.57 ± 11.45, respectively. There were no significant gender difference in PCS (p = 0.283) or MCS (p = 0.721). (2) Dialysis characteristics Table 2 shows the dialysis modality and comorbidities of all patients. Overall, 36 (97.3%) patients were on hemodialysis, and 34 (91.9%) of these patients had three dialysis sessions per week. One patient was on peritoneal dialysis. The average duration of dialysis was 106.0 ± 61.6 months (range: 17∼268 months). Two subjects had renal transplants. Thirteen subjects (35.1%) had hypertension, seven (18.9%) had diabetes, two (5.4%) had heart disease, and one (2.7%) had stroke. (3) Laboratory data before and after surgery Table 3 shows laboratory data of patients before and after surgery. Ultrasonography of the 37 parathyroid glands before surgery indicated that nodule volume ranged from 0.5×0.5 ×0.3 cm3 to 2.5×2×1.6 cm3. Twenty-four patients developed two or more nodules. (4) Symptoms before and after surgery Table 4 summarizes symptom severity (joint pain, itching, and muscle weakness) before and after surgery. Joint pain was noted in multiple joints, including the shoulders, elbows, knees, hips, and fingers. There were 42 anatomical sites with joint pain before surgery, and 33 sites with joint pain after surgery .After surgery, there were significant reductions in joint pain, muscle weakness, and itching. At the three-month post-surgery follow-up, four patients with joint pain, eight patients with muscle weakness, and ten patients with pruritis reported no abatement of symptoms. However, most patients experienced reduction of symptoms one month after surgery. Among patients who experienced no symptom improvement, there were equal numbers of males and females. Comorbidities such as diabetes, hypertension, or heart disease, were reported, but did not show any trend of concentration with a particular disease. 5 (5) Quality of Life(SF-36 )before and after surgery Table 5 summarizes the Quality of life improvement following surgery.and Correlation between PCS and MCS at the one-month and three-month post-surgery follow-up (6) Correlation between symptom distress and PCS and MCS before and after surgery Figure 1-6 shows Relationship of physical component summary score (PCS),mental component summary score (MCS) and symptom distress score. Discussion In this study, we examined the association of the severity of hyperparathyroidism and QOL in 37 ESRD patients before and after parathyroidectomy. We also examined the extent of symptom relief following surgery. The results showed that symptom distress, serum calcium, phosphate, and the calcium-phosphate product were all related to patient QOL. In addition, we found that patients who had more severe symptoms had worse QOL. However, we found no significant correlation between the level of iPTH and QOL. According to Tanaka 〔13〕, patients with higher levels of serum calcium, phosphate, and calcium- phosphate product have lower SF-36 scores and experience greater impact on QOL. We believe that our results can guide nurses in the evaluation of symptom-induced stress and the needs of ESRD patients before parathyroidectomy, so that they can provide personalized and appropriate care and help to improve patients' QOL 〔3〕. Previous studies, in Taiwan and elsewhere, have shown that the symptoms of ESRD patients have a moderate to severe effect on QOL 〔2,6〕(Huang, 2005;). We suggest that better knowledge of potential symptoms and of patients’ subjective perceptions of such symptoms is needed for better management in clinical nursing. Our study has certain limitations. First, all subjects were recruited from the same medical center, but they were treated at different dialysis centers throughout northern Taiwan. Second, considering patients’ privacy rights and the survey-based nature of this study, some laboratory data were not available. Third, the total number of enrolled patients was slightly less than expected (there was an average of 45 parathyroidectomy patients per year in the two years prior to this study). Despite 6 these limitations, we believe that our study will aide in the management of ESRD patients with hyperparathyroidism. Acknowledgments This study was supported by the Far Eastern Memorial Hospital. Reference 1 Chiang,C.K.,Peng,Y.S.,Chiang,S.S.,Yang,C.S.,He,Y.H.,Hung,K.Y.,Wu,K.D., Wu, M.S.,Fang,C.C.,Tsai,T.J.,& Chen,W.Y.:Health-Related Quality of Life of Hemodialysis Patients in Taiwan:A Multicenter Study. Blood Purif 2004;22:490 –498 2 Davison,S.N.,Jhangri,G.S.,& Johnson,J.:A Longitudinal Validation of a modified Edmonton symptom assessment system(ESAS) in haemodialysis patients. Nephrology Dialysis Transplantation 2006;21:3189-3195. 3 Jablonski,A:Level of symptom relief and need for palliative care in the Hemodialysis population.Journal of Hospice and Palliative Nursing, 2007;9(1):50-58. 4 Legg,V.:Complication of chronic kidney disease :a close look at renal Osteodystrophy, nutritional disturbance and inflammation.American Journal of nursing 2005;105:40-49. 5 Locatelli,F.:The need for better control of secondary hyperparathyroidism . Nephrology Dialysis Transplantation 2004;19(5):15-19. 6 Melissa;S.Y.,Sandra,D.,Marlies,N.,Elisabeth,W.B.,Raymond,T.K.,Friedo,W.D.& Adrian, A: Symptom clusters in incident dialysis patients:associations with clinical variables and quality of life. Nephrol Dial Transplant 2009;24:225-230 7 Thong,M.Y.Dijk,S.,Noordzij,M.,Boeschoten,E.W.,Krediet,R.T.,Dekker,F.W.,& Kaptein,A.A.:Symptom clusters in incident dialysis patients:associations with clinical variable-s and quality of life.Nephrology Dialysis Transplantation 2009;24:225-230. 8 Maureen,M.,& Donna.G,:Secondary hyperparathyroidism in chronic kidney disease: clinical consequences and challenges.Nephrology Nursing Journal 2004;31(2):185-193. 9 Moe,S.M.,& Drueke,T.B.:Management secondary hyperparathyroidism: the importance and the challenge of controlling parathyroid hormone level without elevating calcium,phosphorus and calcium phosphorusproduct.American Journal of Nephrology 2003;23(6):369 -379. 10 Pasieka,J.L.:Surgical approach secondary hyperparathyroidism.Poblems in General Surgery 2003;20(3):61-67. 11 Pisoni,R.L.,Wikstrom,B.,Elder,S.J.,Akizawa,T.Asano,Y.,Keen,M.L.,Saran,R., Mendelssohn,D.C.,Young,E.W.,&Pork,F.K.: Pruritus in haemodialysis patients: 7 International results from the Dialysis Outcomes Patterns Study (DOPPS) .Nephrology Dialysis Transplantation 2006;21(12):3495-3505. 12 tojanovic,M.& Stefanovic,V.: Assessment of health-related quality of life in patients treated with hemodialysis in Serbia:influence of comorbidity,age and income.International Center for Artificial Organs and Transplantation 2007;31(1) :53-60. 13 Tanaka,M.,Yamazaki,S.,Hayashino,Y.,Fukuhara,S.,Akiba,T.,Saito,A.,Asano,Y., Port,K.,Kurokawa,K.& Akizawa,T. :Hypercalcaemia is associated with poor mental health in haemodialysis patient:result from Japan DOPPS. Nephrology Dialysis Transplantation 2007;22(6):1658-1664. 14 Vasilieva,I.A.:Quality of life in chronic hemodialysis patient in Russia. International Society for Hemodialysis 2006;10(3):274-279. 15 USRDS.:2008Annual Data Report:Atlas of Chronic Kidney Disease and EndStage Renal Disease in the United States" NIH2008.Retrieved May 3,2009, 2009.05.05 from http://www.medpagetoday.com/Nephrology/ GeneralNephrology /11269 16 USRDS.:2008Annual Data Report:incidence & prevalence.2009.05.05.from http://www.usrds.org/2008/pdf/V2_02_2008.pdf 17 KDOQI clinical practice guidelines for bone metabolism and disease in children with chronic kidney disease.2005 National Kidney Foundation Inc. 2009.05.05 from http://www.kidney.org/professionals/kdoqi/guidelines_pedbone/guide15.htm 18 The National Health Insurance Supervisory Commission report on the quality of arguments 2007;06.29.Taiwan Society of Nephrology.2009 ,05 03 from http://www.areahp.org.tw/upload/project/txt/960705B.ppt 8 Appendix Table 1. Demographic characteristics of patients (N = 37). Variables Number of Sex (male/female) patients Percentage (%) 16/21 43.2/56.8 34 91.9 3 8.1 Employed 10 27.0 Unemployed 1 2.7 Full-time homemaker 16 43.2 Others or not reported 10 27.0 Single 8 21.6 Married 25 67.6 Divorced 1 2.7 Widowed 3 8.1 Buddhism 7 18.9 Taoism 19 51.4 Others/unknown 11 29.7 Educational level Not a high school graduate College or above Employment Marital status Religion Table 2. Dialysis modalities and comorbidities of patients (N = 37). Variables Number of patients Percentage(%) Dialysis modalities Hemodialysis three times per week 34 91.9 Hemodialysis two times per week 2 5.4 Peritoneal dialysis 1 2.7 Diabetes 7 18.9 Hypertension 13 35.1 Cardiac disease 2 5.4 CVA 1 2.7 Others 6 16.2 None 8 21.6 Post renal transplant 2 5.4 Comorbidities 9 Table 3. Laboratory data of patients before and after surgery (N = 37, mean ±SD). Variable Pre-OP Post-op 1 month Post-op 3 months calcium (mg/dL) 10.4±0.9 8.1±1.4 8.9±1.3 phosphorus (mg/dL) 5.2±1.3 4.1±1.3 4.3±1.3 Ca × P (mg2/dL2) 53.4±14.9 34.3±14.6 38.3±13.9 iPTH (pg/mL) 2086.3±1452.2 219.0±262.1 286.6±311.8 Albumin (g/dL) 4.0±0.4 4.0±0.3 4.1±0.3 Table 4. Symptom distress (VAS score)before and after surgery (mean ± SD). Variables Pre-OP Post-op 1 month Joint pain 4.98±3.37 3.21±2.32** 2.61±2.19 * Itching 4.31±3.33 3.52±2.74 ** 3.00±2.19** Muscle weakness 4.63±2.90 3.59±2.28 ** 3.30±2.19 * P<0.05 as compared with baseline # P < 0.05 as compared with Post-OP Month 1 Post-op 3 months ** P< 0.001 as compared with baseline Table 5. SF-36 scores before and after surgery (N=37). Pre-OP Characteristic th Post-op 1 month th th 50 (25 , 75 ) * 50 (25 , 75 ) Post-op 3 months 50 (25th, 75th) PF 55(30,85) 60(40,80) 75(45,90) RP 0(0,62.5) 25(0,62.5) 50(0,100)**,# RE 33.3(0,100) 33.3(0,100) 100(8.3,100)*,# VT 50(32.5,65) 45(37.5,65) 55(32.5,60) MH 60(48,74) 56(46,72) 64(49,76) SF 62.5(37.5,87.5) 75(37.5,75) 50(75,87.5)**,# BP 47.5(22.5,70) 57.5(32.5,77.5)** 67.5(45,79.4)**,# GH 40(20,57.5) 40(22.5,57.5) 40(30,68.8)**,# PCS 31.3(20,45.1) 32.3(22.5,44.3) 42.9(27.7,48.7)**, # MCS 39.5(25.1,48.6) 36.2(26.7,47.4) 42.4(29.8,49.2)*,# P<0.05 as compared with baseline # th ** P< 0.001 as compared with baseline P < 0.05 as compared with Post-oP Month 1 10 symptom distress 10.0 8.0 Pre-op joint pain,PCS& MCS Pre-op itching, PCS& MCS 6.0 →Pre-op muscle weakness, PCS& MCS 4.0 2.0 0.0 PCS score 0.0 10.0 20.0 30.0 40.0 50.0 60.0 70.0 Figure 1. Relationship of PCS score and pre-operative symptom distress due to joint pain, itching, and muscle weakness. 10.0 symptom distress 8.0 6.0 4.0 2.0 0.0 MCS score 10.0 20.0 30.0 40.0 50.0 60.0 70.0 Figur e 2. Relationship of MCS scor e and pr e-oper ative symptom distr ess due to joint pain, itching, and muscle weakness. 11 10.0 symptom distress 8.0 6.0 Post-op joint pain,PCS_1& MCS_1 4.0 Post-op itching, PCS_1& MCS_1 Post-op mscle weakness, PCS_1& 2.0 MCS_1 0.0 PCS score 0.0 10.0 20.0 30.0 40.0 50.0 60.0 70.0 Figur e 3. Relationship of PCS scor e and sym ptom distr ess due to joint pain, itching, and m uscle weakness at one m onth after sur ger y. symptom distress 10.0 8.0 6.0 4.0 2.0 0.0 MCS score 10.0 20.0 30.0 40.0 50.0 60.0 70.0 Figur e 4. R elationship of M C S scor e and sym ptom distr ess due to joint pain, itching, and m uscle weakness at one m onth after sur ger y. 12 10.0 symptom distress 8.0 Post-op joint pain,PCS_3& MCS_3 6.0 Post-op itching, PCS_3& MCS_3 4.0 Post-op mscle weakness, PCS_3& 2.0 MCS_3 0.0 PCS score 10.0 20.0 30.0 40.0 50.0 60.0 70.0 Figur e 5. Relationship of PCS scor e and sym ptom distr ess due to joint pain, itching, and m uscle weakness at thr ee m onths after sur ger y. 10.0 symptom distress 8.0 6.0 4.0 2.0 0.0 10.0 20.0 30.0 40.0 50.0 60.0 70.0 MCS score Figur e 6. R elationship of M C S scor e and sym ptom distr ess due to joint pain, itching, and m uscle weakness at thr ee m onths after sur ger y. 13