The AdaptDx™ test protocol has four steps: align

A DIAGNOSTIC FOR AGE-RELATED MACULAR DEGENERATION
(Disclaimer: the AdaptDx™ is not FDA cleared as a diagnostic for AMD – “place holder”)
John G Edwards; MacuLogix, Inc.; 1214 Research Blvd., Hummelstown, PA 17036; (717) 583-1223; jedwards@maculogix.com
and Gregory R Jackson; Pennsylvania State College of Medicine, Dept. of Ophthalmology; 500
University Dr, HU19, Hershey, PA 17033; (717) 531-6774; grj2@psu.edu
MacuLogix is developing a diagnostic for the early detection of age-related macular degeneration
(AMD). The AdaptDx™ is based on a functional test of dark adaptation (the transition from being lightadapted to being dark-adapted). Testing is completely non-invasive and can be performed by an unskilled operator in ≤ 10 minutes with a minimum of patient burden. The instrument is similar in size, operation and cost to the perimeter/visual field instruments successfully used for routine glaucoma screening. The technology was developed by Gregory Jackson and Cynthia Owsley at the University of Alabama at Birmingham (UAB). MacuLogix has exclusive commercial rights.
AMD is related to a breakdown of the RPE/Bruch’s membrane complex in the retina 1-11 , and measurement of dark adaptation is essentially a bioassay of the health of this membrane complex 10,11 .
During the AMD disease course the RPE/Bruch’s membrane function deteriorates, hampering nutrient and oxygen transport to the photoreceptors. As a side effect, the photoreceptors exhibit impaired dark adaptation because they require these nutrients for replenishment of photopigments and clearance of opsin after light exposure 12 . Figure 1 compares recovery of dark vision sensitivity following photobleaching for a normal old adult, an early-stage (dry) AMD patient and a latestage (wet) AMD patient. There is a marked deterioration of dark adaptation. A preliminary study at UAB showed that dark adaptation impairment indicates the onset of AMD at least four years before it is clinically evident 13 .
AMD affects approximately 30 million people worldwide. In the United States alone, there are an estimated 13 million people with some vision loss from AMD, including nearly 2 million with the most severe late-stage forms. AMD is already the leading
Figure 1 . Early AMD patient (triangles), cause of adult vision loss in developed countries, and the and late AMD patient (open circles) exhibit impaired dark adaptation compared to a problem is expected to get significantly worse as the population normal old adult (closed circles).
ages 14-17 . One challenge in addressing the growing threat of
AMD is the diagnosis of the disease at its earliest stages and identification of individuals who are at risk for progressing to the devastation of late-stage vision loss. The AdaptDx™ has tremendous potential for use by ophthalmologists, optometrists and geriatric physicians as a diagnostic screening tool, as well as for sensitive tracking of disease/treatment progress.
Two recent clinical studies have investigated these capabilities. The first study showed the ability of the AdaptDx™ to diagnose AMD. In this study, a range of early-stage to late-stage AMD patients was readily discriminated from clinically normal old adults. The difference was both substantial (~100% dark adaptation impairment for AMD patients relative to normal old adults) and highly significant (t =
6.02; p < 0.0001). Diagnostic sensitivity and specificity were 88% and 100%, respectively, with the degree of dark adaptation impairment tracking disease severity. The second study showed the
potential for dark adaptation to track treatment progress. This study examined the effect of high-dose retinol (preformed vitamin A) in dry AMD patients. The intervention group showed improved mobility tracked by improved dark adaptation, but the improvement could not be detected by convention tests such as fundus grading, visual acuity or contrast sensitivity. This report provides an overview of dark adaptation, the AdaptDx™ and these recent studies.
Background Our collaborators at UAB had previously demonstrated that dark adaptation is impaired in AMD, that this impairment can serve as a very early diagnostic indicator, and that the extent of impairment is related to disease severity 13,18 .
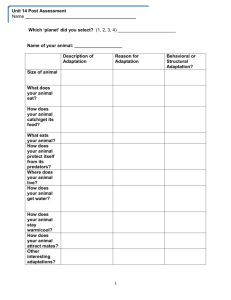
Impairment of Dark Adaptation in AMD – Jackson and Owsley 18 studied 20 AMD patients (mean 75 years old; range 66 to 88) and 16 normal old adults (mean 72 years old; range 62 to 79), with assignment to each cohort based on fundus photography and grading by trained graders masked to the patient characteristics. The AMD patients displayed moderate to severe abnormalities in the kinetics of dark adaptation. Dark Table 1 . Diagnostic sensitivity of selected visual functions for ARMD adaptation was delayed for early AMD patients vs. age-matched controls by an average of 10 to 16 minutes, depending on the
Visual Function Sensitivity parameter chosen. This is not a subtle effect. To put the impairment in perspective, the magnitude of the delay between the normal and the dark adaptation acuity
85%
25% early AMD groups would be proportionately equivalent to losing 3 lines of visual acuity on the ETDRS chart
—a very substantial loss. Late
AMD patients (i.e.; those with choroidal neovascularization or contrast sensitivity photopic visual field
25%
25% scotopic visual field 20% geographic atrophy) were easily identifiable by almost a complete lack of sensitivity recovery for 90 minutes following light exposure. The diagnostic capability for classifying a patient as having AMD was computed for several visual function parameters. As shown in Table 1 , impairment of dark adaptation (outside ±2 standard deviations of the mean normal value) was 85% sensitive for AMD, while impairment of visual acuity, contrast sensitivity, photopic visual field and scotopic visual field were all ≤ 25% sensitive for AMD.
Dark Adaptation Impairment as a Predictor for AMD – In a separate study, Jackson and Owsley showed that dark adaptation can be used to detect AMD before lesions are clinically visible. In particular, they showed that dark adaptation impairment can sensitively discriminate normal aging from sub-clinical macular degeneration, revealing those at risk for developing the clinical signs of AMD at least 4 years in advance 13 . From a database of patients previously characterized for dark adaptation 19 ,
20 patients (65 to 79 years old) were identified who at baseline had normal retinal health using a fundus grading based on the International Classification System 20 , and who also had medical records available from eye examinations during the following 4 years. The patients were classified as having normal or impaired dark adaptation at baseline.
Impaired dark adaptation was defined as 2 standard deviations outside the mean of normal subjects. It was then determined whether the patients received a diagnosis of AMD in the subsequent 4 years. As shown in Figure 2 , 12 of the 14 patients with impaired dark adaptation at baseline progressed to a diagnosis of AMD (an 86% positive predictive value), whereas only 1 of the 6 patients with normal dark adaptation at baseline
Figure 2 . Pilot study of dark adaptation progressed to a diagnosis of AMD (an 83% negative predictive value). Although highly preliminary because of the small sample size and an outcome based on retrospective medical record abstraction, these findings are consistent with the hypothesis that dark adaptation impairment is an indicator of incident early AMD. Furthermore, the conclusion is consistent with the qualitative similarity between retinal aging and AMD, both histopathologically and functionally
(see reviews 10,11 ).
- 2 -
Dark Adaptation Impairment as a Function of Disease Severity – A correlation between increasing AMD disease severity and increasing dark adaptation impairment was demonstrated using detailed fundus grading as a benchmark. Fundus photographs for a subset of 11 AMD and normal old patients were sent to the Wisconsin Reading Center for grading in accordance with the Wisconsin Aging-Related
Maculopathy Grading System (WARMGS) 21 . Figure 3 shows dark adaptation curves for four of these patients: one normal old adult and three with progressively more severe early-stage AMD. Both AMD patient #1 and AMD patient #2 exhibited soft indistinct drusen with the same maximum size (>250 µm) and coverage area (>1500 µm). Patient #2 exhibited soft indistinct drusen in more subfields and twice as many soft indistinct drusen further out from the fovea than patient #1.
Based on fundus appearance, patient #2 has a more advanced disease than patient #1, which is also reflected by the dark adaptation findings. AMD patient #3 was at an even more advanced stage, exhibited a few hard drusen and a pigment epithelial detachment caused by drusen or fluid accumulation.
Although the sample size was too small for statistical analysis and conclusions, the results are consistent with a relationship between disease severity and dark adaptation impairment.
Biological Connection with Retinal Health – It is not surprising that there is a strong link between AMD and dark adaptation given the striking histopathological similarity between AMD and
Figure 3 . Correlation of dark adaptation impairment and AMD severity for a normal other retinal diseases with early impairment of rod-mediated dark old adult (solid circles) and three early-stage adaptation. Indeed, rod-mediated dark adaptation has been AMD patients with progressively worse shown to be a useful assay in understanding a number of other retinal status: AMD #1 (triangles), AMD #2
(squares) and AMD #3 (open circles). retinal diseases known to compromise the retinoid cycle, such as vitamin A deficiency 22 , Sorsby’s Fundus Dystrophy 23,24 , and autosomal dominant late-onset degeneration 25 . These diseases cause dramatic slowing of dark adaptation. Sorsby’s Fundus
Dystrophy, an early onset retinal degenera tion, is characterized by lesions in the RPE and Bruch’s membrane similar to those in early AMD. Patients with this disorder exhibit slowed dark adaptation which is partially reversible through vitamin A supplementation 23 . Autosomal dominant late-onset degeneration, a disease with similar sub-RPE deposits to AMD, is so disruptive to the retinoid cycle that impaired dark adaptation can precede fundoscopic signs of the disease by at least a decade 25 .
Dark Adaptation Characteristics The basic characteristics of dark adaptation are well understood.
The recovery is essentially biphasic. Cones recover rapidly, but have limited scotopic sensitivity. Rods recover slowly, but are ultimately more sensitive. Since the impairment of dark adaptation associated with AMD is rod-mediated, it is essential for developing a diagnostic to untangle the inter-relationship between the cones and rods, and focus on the rods.
Dark Adaptation Kinetics – A typical dark adaptation curve for a normal adult is shown in Figure 4 . It plots recovery of scotopic sensitivity over six log units of dynamic range, going from little or no sensitivity immediately following strong photobleaching to essentially complete recovery in roughly 40 minutes. The data points are obtained by interrogating the test subject with a series of test spots at different intensities using an appropriate wavelength for rod sensitivity and a three-down/one-up modified staircase procedure to estimate the sensitivity threshold 18,26 . As already noted, the typical dark adaptation function is biphasic, consisting of a cone-mediated and rod-mediated portion. The time at which the rods become more sensitive to the stimulus than the cones is termed the rod-cone break. Traditionally, the speed of the rod-mediated component is described by a single
- 3 -
Figure 4 . Typical dark adaptation curve for normal adult. Data points are sensitivity thresholds, modeled (solid line) with a twocomponent nonlinear regression fit to reveal rod-cone break and rod-mediated recovery time constant.
exponential time constant. A recent model divides the rod recovery into two components each with their own time constants 12 . Although these models are useful for understanding the underlying mechanisms responsible for dark adaptation, this approach requires stereotypical functions, which may not be obtainable for all patients. This requirement is unnecessary and perhaps undesirable in clinical application.
Rod Function vs. Cone Function in AMD – Impairment of dark adaptation is primarily rod-mediated in early AMD. Other parameters have been investigated without finding a significant correlation to early
AMD 13,18 . In particular, no statistically significant impairment was found for cone-mediated dark adaptation in early AMD patients. Cone-mediated dark adaptation exhibits impairment later in the disease progression 27-29 . The early susceptibility of rod-mediated dark adaptation impairment is consistent with biological work on AMD using donor eyes, which suggests that rod degeneration and death occurs earlier and is more severe in AMD pathogenesis as compared to that for cones 30 . Cones have multiple pathways for nourishment while rods are wholly dependent on transport across the
RPE/Bruch’s membrane complex 31 . In a sense, monitoring rod function as an early indicator of AMD can be viewed as analogous to the age-old practice of using canaries as sentinels to protect coal miners. When the rods start to show impaired function, it is a signal of impending danger for the cones.
Rod Intercept as a Diagnostic Parameter – AMD patients can exhibit several differently shaped dark adaptation functions. Early in the disease, the shape may be similar to a normal patient (with multiple linear-exponential components) and then deteriorate in the late stages of the disease to single line. An estimate of recovery speed that is robust to shape is desirable.
Furthermore, for statistical validity it is important that the same method to estimate dark adaptation kinetics is applied to all patients. We have developed a signature of recovery speed termed the “rod intercept”. The basis of the rod intercept is similar to the rod-cone break. As described above, the rod-cone break is the time in minutes at which the rod portion of the function intersects the cone portion of the function. In a similar fashion, the rod intercept is the time at which the rod portion of the function intersects a criterion sensitivity. For our current protocol the criterion sensitivity is 4.0 log units of recovery, or
5.00 X 10 -4 cd/m 2 . To estimate the rod intercept, linear interpolation is applied to the patient’s dark adaptation function and the rod intercept is set to the time at which the interpolated sensitivity recovery intercepts 4.0 log units of recovery (see
Figure 5 ). Like the rod-cone break, those patients with normal dark adaptation will have shorter rod intercepts than those
Figure 5 . The rod intercept is the time at which sensitivity has recovered by 4.0 log units. This normal young adult’s rod intercept is 20.3 minutes in response to a 98% bleaching light. patients with impaired dark adaptation.
The rod intercept has several attractive features. (1) The primary advantage of is that not all subjects must exhibit a stereotypical dark adaptation function, e.g. a long cone plateau followed by a steep rod second component. All patients are evaluated and compared using the same metric. (2) The criterion sensitivity is solely rod-mediated and not contaminated by cone function. It is essential for the success of the diagnostic to isolate the rods because rods are more sensitive to AMD than are the cones.
Kinetics of dark adaptation mediated by both rods and cones may mask rod dysfunction. (3) The criterion sensitivity of 4.0 log units falls well within the second component of rod-mediated dark adaptation, which is best described by a line. Thus, linear interpolation is an appropriate method to interpolate sensitivity between thresholds in this part of the dark adaptation function.
AdaptDx™ Commercial Prototype The AdaptDx™ commercial prototype is pictured in Figure 6 .
The design parameters are optimized for the detection of AMD and are intended to allow collection of full dark adaptati on curves in ≤ 20 minutes, which has been determined through market interviews to be a commercially viable test duration. Like other dark adaptometers, the AdaptDx™ allows for bleaching of the retina and the measurement of sensitivity recovery following bleaching.
- 4 -
Overview of AdaptDx™ Operation – The AdaptDx™ test protocol has four steps: align patient, photobleach test eye, measure rod-mediated scotopic sensitivity recovery, and calculate rod intercept.
The operator sits to the left or right of the Ad aptDx™ and controls the operation using a typical laptop computer. a) Alignment – Alignment is computer controlled. An infrared camera mounted inside the instrument housing views the patient’s test eye and displays an image of the eye on the operator’s computer screen.
The patient’s head remains fixed, and the operator moves the instrument optics into alignment with the patient’s eye by toggling directional buttons on the operator screen. A single alignment positions the patient correctly for both bleaching and measurement of sensitivity recovery. The infrared camera can be used as needed to confirm and re-adjust alignment as needed during testing. Figure 7 shows the patient’s perspective when looking at the front of the
AdaptDx™. Note that the patient will only see the fixation light and the stimulus light because the inside of the machine and the room are dark during testing.
Figure 6 . External view of prototype AdaptDx™ dark adaptometer.
The patient is instructed to look directly at the fixation at all times, both during alignment and testing. b) Photobleaching – The test eye is photobleached by exposure to a brief, high intensity camera flash
(typically 4 to 8 log scot Td sec -1 for 0.25 ms) while the patient is focused on the fixation light to ensure the proper portion of the retina is bleached. A flash bleach was chosen over other methods of bleaching (e.g.; continuous background) because of its rapidity which reduces the chance of uneven or partial bleaches while minimizing patient burden. The camera flash passes through a diffuser and aperture to provide a uniform, focal bleach centered on the area to be tested during sensitivity recovery measurement. c) Sensitivity Recovery Measurement – Scotopic sensitivity measurements begin immediately after photobleaching. The patient focuses on the fixation light and responds whenever the stimulus light is visible by pushing a patient response button. Sensitivity is estimated using a three-down/one-up modified staircase procedure. Starting at a relatively high intensity (5.00 cd m -2 ), stimulus lights are presented to the patient every 2 or 3 seconds for a
200 ms duration. If the patient does not respond that the stimulus is visible, the intensity remains unchanged for subsequent presentations until the patient does respond. Once the patient indicates the stimulus is visible, the intensity is decreased for each successive presentation in steps of 0.3 log units
(“three-down”) until the patient stops responding that the stimulus is present. The intensity is then increased for each successive presentation in steps of
0.1 log units (“one-up”) until the patient responds that the stimulus is once again visible. This intensity is defined as a threshold. Successive threshold measurements start with a stimulus intensity 0.3 log units brighter than the previous threshold estimate.
Figure 7 . Patient perspective of AdaptDx™ dark adaptometer.
The patient is given a 30 second rest period between threshold measurements. This algorithm results in about once threshold measurement per minute, and a total of about 20 threshold measurements for our current protocol. To focus on rod-mediated function, a stimulus light with a
- 5 -
wavelength near the peak rod sensitivity (~ 500 nm) is used. Corrective lenses can be introduced between the test eye and the stimulus light as appropriate via a lens holder (not shown). d) Estimate Speed of Dark Adaptation – As previously discussed, to focus cleanly on rod-mediated kinetics, the time for recovery to 4 log units of scotopic sensitivity ( or “rod intercept”) was selected as the characteristic dark adaptation parameter. Linear interpolation is applied to the dark adaptation threshold function to determine the time at which sensitivity crosses 4.0 log units of stimulus attenuation, and this time is recorded as the rod intercept.
AdaptDx™ Prototype Optimization Prior to conducting clinical studies, iterative testing on a benchmark cohort of 5 normal adults and 8 AMD patients was used to optimize the configuration parameters of the AdaptDx™. In particular, as described in the following sections, the bleaching intensity was set to capture only the rod-mediated portion of the dark adaptation curve, and testing was directed to a region of the macula near the fovea where impairment should be greatest in early AMD.
Bleaching Intensity – The primary variable affecting the speed of dark adaptation is the bleaching light intensity. Sensitivity recovery time is proportional to bleaching level. We conducted a control experiment using our benchmark cohort of normal and
AMD patients that examined the effect of reducing bleaching intensity on test duration. As expected, the results demonstrated that reducing the bleaching light intensity decreased the time required for adaptation. Figure 8 shows typical data for a normal young adult. Using a flash intensity of 7.48 log scot Td sec -1
(98% equivalent bleach), the participant had not fully recovered in 20 minutes. Using a flash intensity of 6.38 log scot Td sec -1
(82% equivalent bleach), the participant fully recovered in less than 15 minutes. Thus, lowering the bleaching intensity allows the rod-mediated portion of dark adaptation to begin sooner and results in a more rapid diagnostic test. Based on this testing, a flash intensity of 6.38 log scot Td sec -1 was selected for our
Figure 8 . Lowering bleach intensity speeds up dark adaptation of a normal adult. Circles in response to 6.38 log scot Td sec -1 and squares in response to 7.48 log scot td sec -1 . clinical studies.
Stimulus Location – To enhance the sensitivity of our diagnostic test, we optimized the test location. In previous research studies at UAB , dark adaptation was tested at 12° eccentricity on the inferior visual meridian. This location is just adjacent to the anatomically defined macula. However, the area of greatest impairment in early AMD is in the macula about 5° from the fovea 30 . Dark adaptation for each patient in the benchmark cohort was measured at 5° and 12° on separate testing visits. In both cases the stimulus test spot covered a 2° diameter area of the retina, and the bleaching flash intensity was
6.38 log scot Td sec -1 (82% equivalent bleach). Dark adaptation was almost 3 minutes faster at
5° compared with 12° for normal old adults. In contrast, AMD patients were almost 2 minutes slower to adapt at 5° compared with 12°. Thus, moving the stimulus location within the macula increases the dark adaptation impairment for AMD patients relative to normal adults by almost 5 minutes (F = 7.05, p
= 0.02). Moving the test location within the macula should increase the sensitivity of the test.
Furthermore, because dark adaptation is faster in the macula for normal adults, this optimization also serves to reduce the test duration. Based on this testing, a stimulus location of 5° eccentricity on the inferior vertical meridian was selected for our clinical studies.
Clinical Evaluation A clinical study was conducted using the prototype AdaptDx™ to determine the feasibility of discriminating AMD patients from normal old adults in ≤ 20 minutes (since this original study was completed AdaptDx™ screening test times have been reduced to approximately 5 minutes).
Dark adaptation was measured at 5 ° in response to a 6.38 log scot td sec -1 bleaching light.
- 6 -
Study Population – The study population consisted of 9 normal old adults (mean age = 73.1 years old) and 17 AMD patients (mean age = 75.5 years old). Assignment to the normal old or AMD group was based on fundus grading. Bilateral color stereo fundus photographs were taken for every participant.
Two trained graders at UAB (not the investigators) used the AREDS severity scale 32 to score the photographs. The graders were masked to the functional and clinical characteristics of the patients.
For a participant to be classified as a normal old adult, both graders had to independently assign an
AREDS fundus grade of 1 to both eyes. A participant with this grade could have no drusen or small hard drusen and no pigmentary changes associated with AMD. Participants scored with AREDS fundus grade ≥ 2 in the enrollment eye were classified as having AMD. These participants exhibited intermediate sized drusen (3 or more drusen ≥ 63 µm in diameter) or pigmentary changes attributed to early AMD. Visual acuity (ETDRS chart) and contrast sensitivity (Pelli Robson chart) were also tested for all participants. The two groups had similar ages (t = 1.02; p =
0.32), test eye acuities (t = 1.66; p = 0.11), and test eye contrast sensitivities (t = .08; p = 0.94).
Discrimination of AMD vs. Normal Populations – The
AdaptDx™ was used to obtain dark adaptation curves for all study participants. Figure 9 shows representative curves for a normal old adult (defined as AREDS fundus grade 1), an earlystage AMD patient (defined as AREDS fundus grade 2 to 5) and an intermediate-stage AMD patient (defined as AREDS fundus grades 6 to 9). The rod intercept was calculated for each participant as a measure of dark adaptation status. The
AMD patients exhibited substantially slower dark adaptation
Figure 9 . Early AMD patient (triangles), and late AMD patient (open circles) exhibit impaired dark adaptation compared to a normal old adult
(closed circles) using a 20-minute dark adaptation test. than the normal old adults. As shown in Figure 10 , the rod intercept for AMD patients (mean = 17.2 minutes, SD = 3.8) was, on average, twice the rod intercept for normal old adults (mean = 8.7 minutes,
SD = 1.9). The difference was highly significant (t = 6.02, p < 0.0001). In fact, the difference is actually an understatement of the relative impairment. Nine of the 17 AMD patients did not reach rod intercept within the 20-minute test protocol. Their rod intercept was assigned a conservative value of 20 minutes. The substantial impairment exhibited by the AMD group suggests that the AdaptDx™ parameters can be further optimized to shorten the duration of the test without sacrificing discrimination.
Evaluation of Sensitivity & Specificity – Diagnostic sensitivity and specificity were assessed using the normal reference range (mean plus two standard deviations for the clinically normal old adults) as a diagnostic cutoff. The upper limit of the normal reference range was 12.6 minutes. Using this cutoff, 15 of the 17 AMD patients were classified as having abnormal dark adaptation for a diagnostic sensitivity of 88%. All 9 normal adults fell within the normal reference range for a diagnostic specificity of 100%. Interestingly, the sensitivity and specificity of our 20-minute study protocol (88% sensitivity; 100% specificity) are essentially the same as previously obtained at
UAB using a 90-minute research protocol (85% sensitivity;
100% specificity), despite the considerable shortening of the test. Furthermore, it is useful to examine the two false negative results. Both were for participants with an AREDS fundus grade of 2 (borderline AMD). One exhibited 3 drusen of ≤ 63
µm scattered throughout the central 3,000 µm of the macula.
The other had a small amount of hyperpigmentation surrounding a 63 µm druse. The sensitivity of the study
Figure 10 . Mean rod intercept for AMD group is significantly larger than mean rod intercept for normal old adults . Error bards are ±1 standard deviation of the mean. Dashed line is the cut point between normal and abnormal dark adaptation.
- 7 -
protocol for AREDS fundus grades 3 and higher is 100%. Optimization of the AdaptDx™ parameters is likely to enhance the sensitivity of the test.
Dark Adaptation Impairment vs. Disease Severity – As shown in Table 2 , dark adaptation impairment increased with AMD severity. Old normal adults had a mean rod intercept of 8.4 minutes. The rod intercept for borderline AMD patients (AREDS fundus grade 2) was on average 5.1 minutes slower, and the rod intercept for early AMD patients (AREDS fundus grades 3 to 5) was on average yet another 3.4 minutes slower. Patients with AREDS fundus grades 6 and above did not reach the rod intercept within the 20-minute test time. The study size was insufficient to assess statistical significance, but the trend is encouraging for development of a test that can track disease progression. Obviously, further optimization is required to track impairment over the full range of disease severity. If such a protocol can be developed, the AdaptDx™ can serve as a useful adjunct to fundus photography in monitoring disease progression and evaluating the efficacy of treatments aimed at early AMD.
Table 2. Disease Severity vs. Dark Adaptation Impairment
Subgroup
AREDS Fundus Grades
Sample Size
Rod Intercept (mean)
Rod Intercept (std dev)
Normal
1
N=9
8.7 minutes
2.0 minutes
Borderline AMD
2
N=5
13.8 minutes
4.4 minutes
Early AMD
3,4,5
N=6
17.2 minutes
2.7 minutes
Intermediate AMD
6,7,8,9
N=5
20.0 minutes*
--
Late AMD
≥10
N=1
20.0 minutes*
--
*All subjects in these subgroups failed to reach rod intercept within the 20 minute test duration. Rintercepts were conservatively set at 20 minutes for comparison purposes. Consequently, standard deviations for these subgroups are not meaningful.
Potential for Rapid Screening Test Pilot experiments indicate that a rapid diagnostic screening test on the order of 5 minutes should be possible. Because the impairment exhibited by AMD patients in our clinical evaluation was large, it is likely that a lower bleaching intensity and a less conservative recovery signature can be employed. The potential is illustrated in Figure 11 . Panel A shows the dark adaptation curve for a normal old adult using the parameters employed in our current protocol: an 82% bleach (6.38 log scot Td sec -1 ) and the rod intercept defined as recovery to 4 log units of sensitivity (RI
4.0
). Panel B shows the dark adaptation curve for the same normal old adult using refined parameters: a
56% bleach (4.38 log scot td sec -1 ) and the rod intercept defined as recovery to 3.5 log units of sensitivity (RI
3.5
). In both cases, sensitivity recovery was measured at 5° on the inferior vertical meridian (in the macula). The recovery signature is shortened from 11.0 minutes to 2.9 minutes. Similarly, the recovery signature for an early AMD patient (AREDS fundus grade 2) is shortened from 17.9 minutes to 6.1 minutes (data not shown). For a screening test, it is sufficient to establish a cutoff time. Patients recovering by the cutoff time are designated as normal. Patients not recovering by the cutoff time are designated as having AMD.
These data suggest that with further optimization the screening test cutoff time will not need to be longer than 5 minutes.
Potential for Treatment Monitoring A recent study at UAB demonstrates the utility of dark adaptation as a sensitive measure for monitoring treatment effectiveness in early-stage AMD interventions. Owsley, McGwin and Jackson 33 examined the effect Figure 11.
Potential for rapid screening test of a short course of high-dose retinol (preformed vitamin A) on
(≤ 5 min) using reduced bleaching intensity and refined recovery signature. early-stage AMD patients and normal old adults. A randomized, double-masked, placebo-controlled experiment was conducted. Adults (mean age 72
±9 years) with
- 8 -
AREDS fundus grades 1 to 9 for the eye to be tested were randomly assigned to a 30-day course of
50,000 international units (IU) of oral retinol or placebo. The sample consisted of 104 participants with
52 each in the intervention and placebo groups. At baseline and 30-day follow-up, fundus grade, visual acuity, contrast sensitivity and dark adaptation were measured. At 30 days, the intervention group reported significantly improved visual mobility under low light conditions using a standard self-test (p =
0.0141). Furthermore, the intervention group had significantly faster dark adaptation than the placebo group (p = 0.0419). There was a trend for those patients showing greater mobility improvement to have greater dark adaptation improvement. There was no detectable change in fundus grade, visual acuity or contrast sensitivity for either group over the course of the study. These results indicate that dark adaptation has the potential to detect effects in early AMD patients that are not seen by other tests. In this study, the dark adaptation curves were analyzed to determine both the cone-mediated recovery and the rod-mediated recovery. Interestingly, the rods benefited from supplementation while the cones did not, which suggests that the rods are more sensitive to metabolic changes in the retina. This underscores the fact that focusing on the rod-mediated portion of recovery curve provides a more sensitive measure.
AdaptD x™ Definitive Validation Study
The National Institute on Aging is funding a multi-site clinical study at Johns Hopkins University, Harvard University and Penn State University to validate use of the
AdaptDx™ as a diagnostic for early AMD (NIH Grant R44 AG026222). Three groups of patients will be enrolled in this cross-sectional study: (i) a group of normal young adults (age 18 to 44 years; normal retinal health), (ii) a group of normal old adults (age 60 to 80 years; AREDS grade 1), and (iii) a group of old adults with early-to-intermediate AMD (age 60 to 80 years; AREDS grades 3-8). The primary hypothesis is that the AMD patients will exhibit greater dark adaptation impairment compared with the old normals, and the test will exhibit ≥ 90% sensitivity and ≥ 90% specificity. Secondary hypotheses are that dark adaptation impairment for AMD patients is related to disease severity as classified by the
AREDS severity scale 32 and that dark adaptation for the old normals is statistically indistinguishable from the young normals. A total of 200 participants will be enrolled (20 young normals, 90 old normals and 90 AMD patients). A subset of 40 participants (4 young normals, 18 old normals and 18 AMD patients) will be retested to determine test-retest reliability. Enrollment begins in the first quarter of
2009 and the study is expected to be completed by the end of 2009.
References Cited
1. Bressler, N.M., Silva, J.C., Bressler, S.B., Fine, S.L., and Green, W.R., (1994). Clinicopathologic correlation of drusen and retinal pigment epithelial abnormalities in age-related macular degeneration .
Retina . 14 ( 2 ): p. 130-42.
2. Chen, J.C., Fitzke, F.W., Pauleikhoff, D., & Bird, A.C., (1992). Functional loss in age-related Bruch's membrane change with choroidal perfusion defect .
Invest Ophthalmol Vis Sci 33 ( 2 ): p. 334-40.
3. Curcio, C.A., Medeiros, N.E., and Millican, C.L., (1998). The Alabama Age-Related Macular Degeneration Grading
System for fundus appearance and RPE/Bruch’s membrane histopathology in donor eyes. Invest Ophthalmol Vis Sci
39 ( 7 ): p. 1085-1095.
4. Freeny-Burns, L. and Ellersieck, M.R., (1985). Age-related changes in the ultrastructure of Bruch's membrane .
Am J
Ophthalmol . 100 : p. 686-697.
5. Spraul, C.W. and Grossniklaus, H.E., (1997). Characterisitcs of drusen and Bruch's membrane in postmortem eyes with age-related macular degeneration .
Arch Ophthalmol . 115 : p. 267-273.
6. Steinmetz, R.L., Haimovici, R., Jubb, C., Fitzke, F.W., and Bird, A.C., (1993). Symptomatic abnormalities of dark adaptation in patients with age-related Bruch's membrane changes .
Br J Ophthalmol . 77 : p. 549-554.
7. Anderson, D.H., Mullins, R.F., Hageman, G.S., and Johnson, L.V., (2002). A role for local inflammation in the formation of drusen in the aging eye .
Am J Ophthalmol . 134 ( 3 ): p. 411-31.
8. Doris, N., Hart, P.M., Chakravarthy, U., McCleland, J., Stevenson, M., Hudson, C., et al., (2001). Relation between macular morphology and visual function in patients with choroidal neovascularisation of age related macular degeneration .
Br J Ophthalmol . 85 ( 2 ): p. 184-8.
9. Shahidi, M., Blair, N.P., Mori, M., Gieser, J., and Pulido, J.S., (2002). Retinal topography and thickness mapping in atrophic age related macular degeneration .
Br J Ophthalmol . 86 ( 6 ): p. 623-6.
10. Curcio, C.A., Jackson, G.R., and Owsley, C., (2000). Spare the rods, save the cones in aging and age-related maculopathy .
Invest Ophthalmol Vis Sci 41 : p. 2015-2018.
11. Jackson, G.R., Owsley, C., and Curcio, C.A., (2002). Photoreceptor degeneration and dysfunction in aging and agerelated maculopathy .
Ageing Research Reviews . 1 : p. 381-386.
12. Lamb, T.D. and Pugh, E.N., Jr., (2004). Dark adaptation and the retinoid cycle of vision .
Prog Retin Eye Res . 23 ( 3 ): p.
307-80.
- 9 -
13. Jackson, G.R. and Owsley, C. Method and apparatus for the early detection of age-related maculopathy. PCT Application
PCT/US2004/29003.
14. Kahn, H.A., Leibowitz, H.M., Ganley, J.P., Kini, M.M., Colton, T., Nickerson, R.S., et al., (1977). The Framingham eye study, I. Outline and major prevalence findings .
Am J Epidemiol . 106 ( 1 ): p. 17-41.
15. Klein, R., Klein, B.E.K., and Linton, K.L.P., (1992). Prevalence of age-related maculopathy: The Beaver Dam eye study .
Ophthalmology . 99 ( 6 ): p. 933-943.
16. Klein, R., Klein, B.E.K., Jensen, S.C., and Meuer, S.M., (1997). The five-year incidence and progression of age-related maculopathy .
Ophthalmology . 104 ( 1 ): p. 7-21.
17. Klein, R., Klein, B.E., Tomany, S.C., Meuer, S.M., & Huang, G.H., (2002). Ten-year incidence and progression of agerelated maculopathy: The Beaver Dam eye study .
Ophthal . 109 ( 10 ): p. 1767-79.
18. Owsley, C., Jackson, G.R., White, M.F., Feist, R., and Edwards, D., (2001). Delays in rod-mediated dark adaptation in early age-related maculopathy .
Ophthalmology . 108 : p. 1196-1202.
19. Jackson, G.R., Owsley, C., and McGwin, G.J., (1999). Aging and dark adaptation .
Vision Res . 23 : p. 3975-3982.
20. Bird, A.C., Bressler, N.M., Bressler, S.B., Chisholm, I.H., Coscas, G., Davis, M.D., et al., (1995). An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International
ARM Epidemiological Study Group .
Surv Ophthalmol . 39 ( 5 ): p. 367-74.
21. Klein, R., Davis, M.D., Magli, Y.L., Segal, P., Klein, B.E.K., and Hubbard, L., (1991). The Wisconsin age-related maculopathy grading system .
Ophthalmology . 98 : p. 1128-1134.
22. Hecht, S. and Mandelbaum, J., (1939). The relation between vitamin A and dark adaptation .
JAMA . 112 : p. 1910-1916.
23. Jacobson SG, Cideciyan AV, Regunath G, Rodriguez FJ, Vandenburgh K, Sheffield VC et al (1995) Night blindness in
Sorsby's fundus dystrophy reversed by vitamin A .
Nat Genet 11 ( 1 ): p. 27-32.
24. Cideciyan, A.V., Pugh, E.N., Lamb, T.D., Huang, Y., and Jacobson, S.G., (1997). Rod plateaux during dark adaptation in
Sorsby's fundus dystrophy and vitamin A deficiency .
Invest Ophthalmol Vis Sci 38 ( 9 ): p. 1786-1794.
25. Jacobson, SG, Cideciyan, AV, Wright, E, & Wright, AF, (2001). Phenotypic marker for early disease detection in dominant late-onset retinal degeneration .
Invest Ophthal Vis Sci 42 : p. 1882-1890.
26. Jackson, G., Owsley, C., Cordle, P., and Finley, C., (1998). Aging and scotopic sensitivity .
Vision Res . 38 ( 22 ): p. 3655-
3662.
27. Eisner, A., Fleming, S.A., Klein, M.L., & Mauldin, W.M., (1987). Sensitivities in older eyes with good acuity: eyes whose fellow eye has exudative AMD .
Invest Ophthalmol Vis Sci . 28 ( 11 ): p. 1832-7.
28. Brown, B., Adams, A.J., and Coletta, N.J., (1986). Dark adaptation in age-related maculopathy .
Ophthalmologic &
Physiologic Optics . 6 ( 1 ): p. 81-84.
29. Brown, B., Tobin, C., Roche, N., and Wolanowski, A., (1986). Cone adaptation in age-related maculopathy .
Am J Optom
Physiol Opt . 63 ( 6 ): p. 450-4.
30. Curcio, C.A., Medeiros, N.E., and Millican, L.C., (1996). Photoreceptor loss in age-related macular degeneration .
Invest
Ophthalmol Vis Sci 37 ( 7 ): p. 1236-1249.
31. Mata N, Radu R, Clemmons R & Travis G (2002). Isomerization and oxidation of vitamin a in cone-dominant retinas. A novel pathway for visual-pigment regeneration in daylight .
Neuron . 36 ( 1 ): p. 69.
32. Davis, M.D., et al., (2005).The Age-Related Eye Disease Study severity scale for age-related macular degeneration:
AREDS Report No. 17 .
Arch Ophthalmol . 123 (11): p. 1484-98.
33. Owsley, C., McGwin, G, and Jackson, G.R., et al., (2006). Effect of short-term, high-dose retinol on dark adaptation in aging and early age-related maculopathy .
Invest Ophthalmol Vis Sci , 2006. 47 (4): p. 1310-8.
- 10 -