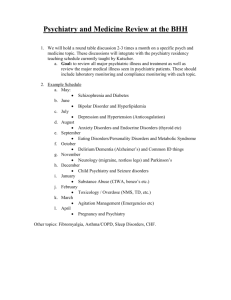
Table of Contents - Institute of Healthcare Professions
advertisement

NURSING DEPARTMENT Date Course Title Nursing Math and Pharmacology Credits Course Number 3 credits NUR 1141 MAT0002, DEP 1000, Co-requisite None NUR 1889, 1822, 1045, (s) 1025, 1025C, 1025L Hours 45 theory hours/45 clock Total outside 90 hours hours hours Note: A minimum of 2 hours of outside work is assigned per clock hour. Pre-requisite (s) Place and Time of Class Meeting Institute of Healthcare Professions 2100 45th Street, Suite A2A West Palm Beach, FL 33407 Hybrid Name and Contact Information of Instructor Instructor: Johnnetta Wider RN, MSN Email: JWider@ihpedu.com Office Hours: By Appointment Campus Telephone: (561) 202-6333 Method of Delivery: Online Book required Pharmacology: Connections to Nursing Practice, 2/e, Michael Adams & Carol Urban ©2012 | Pearson | Published: 2/2012 ISBN-13:978-0132814423 Classroom expectations for students 1|Page NURSING DEPARTMENT Attendance Policy Students are expected to participate in all required instructional activities in their courses. Online courses are no different in this regard; however, participation must be defined in a different manner. 1. Student “attendance” in an online course is defined as active participation in the course as described in the course syllabus. Instructors are responsible for incorporating specific instructional activities within their course and will, at a minimum, have weekly mechanisms for documenting student participation. These mechanisms may include, but are not limited to, participating in a weekly discussion board, submitting/completing assignments in the online platform, or communicating with the instructor. 2. Students aware of necessary absences must inform the professor with as much advance notice as possible in order to make appropriate arrangements. 3. Any student absent 20 percent or more of the online course, i.e., non-participatory during 3 or more weeks of an 11 week term, may receive an F for that course. 4. Any student who has not actively participated in an online class prior to the census date for any given term is considered a "no-show" and will be administratively withdrawn from the class without record. To be counted as actively participating, it is not sufficient to log in and view the course. The student must be submitting work as described in the course syllabus. 5. Additional attendance and participation policies for each course, as defined by the instructor in the course syllabus, are considered a part of the attendance policy Termination may occur for any of the following attendance situations: 1. Eight (8) consecutive absences per semester. 2. Absence in excess of 20 percent (20%) of available course hours. 3. Absence in excess of 20 percent (20%) of externship hours. Student Tardiness Policy Tardiness for didactic or clinical education will not be tolerated. Anytime beyond the scheduled reporting time will be considered late or tardy. When attending clinical externship, if a student is to be late, he or she must notify the clinical instructor at the facility and the program clinical coordinator. If a student must miss class, he or she must contact the program director or instructor at least 30 minutes prior to the class beginning for didactic education five episodes of tardiness or leaving IHP early per semester will result in an absence. 2|Page NURSING DEPARTMENT NOTE: Plagiarism is defined as the use, without proper acknowledgment, of the ideas, phrases, sentences, or larger units of discourse from another writer or speaker. Plagiarism includes the unauthorized copying of software and the violation of copyright laws. Students who commit plagiarism will obtain a grade of “Failure” on their exam or assignment. Course Description (must correspond exactly to Catalog description) This course combines theory and laboratory experiences to allow for mastery of the basic principles of pharmacotherapeutics and the role of the nurse in safe effective administration of medications with emphasis places on dosage calculations. Learning Objectives The primary goal is to establish knowledge and skills for the safety administration of drug therapy within the role of the registered professional nurse. STUDENT LEARNING OUTCOMES (SLO) All students successfully completing this course will be able to: 1.1.Collect, analyze, and prioritize relevant physical, developmental, psychosocial, cultural, spiritual, and functional assessment data to provide individualized patient care. 2 2. Utilize the nursing process, critical thinking, evidence-based information, and knowledge from the arts and sciences to support sound clinical decisions. 3 3. Communicate effectively through verbal, nonverbal, written, and technological means with individuals, families, and health care team members. 4 4. Plan and implement nursing care in a safe, compassionate, culturally sensitive manner that preserves human dignity and promotes growth of individuals and families. 5 5. Manage the efficient, effective use of human, physical, financial, and technological resources in providing continuity of care within and across healthcare settings. 6 6. Collaborate with individuals, families, and healthcare team members in providing comprehensive, individualized patient care. 7 7. Demonstrate accountability in adhering to standards of professional practice within legal and ethical frameworks. 8.8. Participate in activities that promote professional development and personal growth. COURSE OBJECTIVES (CO) All students successfully completing this course will be able to: 1. Describe the mechanism of action, therapeutic uses, side effects, and adverse reactions for each major drug class. (SLO – 1, 2) 2. Discuss basic physiological and pathophysiological mechanisms involved in the rationale for drug therapy. (SLO – 1, 2) 3. Examine recent research findings and developments related to drug therapy. (SLO-2) 4. Demonstrate the ability to accurately calculate drug dosages. (SLO- 3,4, 5) 5. Identify physical, developmental, psychosocial, religious, and cultural factors that impact drug therapy. (SLO-1, 3, 4, 6) 6. Describe the nursing interventions and patient education necessary for safe administration of the major drug classes. (SLO– 2, 3, 5, 7) 3|Page NURSING DEPARTMENT 7. Explain the nurse’s role in teaching patients receiving drug therapy. (SLO – 3, 5) 8. Identify the legal and ethical standards related to the nurse’s role in drug therapy. (SLO – 3, 7) 9. Recognize the responsibility for continued learning regarding drug therapy. (SLO –3, 8) Topical Outline and Schedule DATE WEEK 1 Describe the course. SPECIFIC OBJECTIVES Discuss the library and library resources. 1. Identify key events in the history of pharmacology. 2. Compare and contrast the terms drug, pharmacology, and pharmacotherapy. 3. Explain the importance of pharmacotherapy to clinical nursing practice. 4. Using specific examples, explain the difference between the pharmacologic and therapeutic methods of classifying drugs. 5. Identify the advantages of using protype drugs to study pharmacology 6. Classify drugs by their chemical, generic and trade names 7. Compare the advantages and disadvantages of a pharmaceutical company being granted exclusivity for the development of a new drug 8. Analyze possible differences generic drugs and their brand-name equivalents 9. Assess the responsibilities of the nurse in drug administration. 10. Explain the role of patient medicines in the history of pharmacology and the legislation of drugs. 11. Outline the key U.S. drug regulations and explain how each has contributed to the safety and effectiveness of medications 12. Describe how the United States Pharmacopia-National Formulary (USP-NF) controls drug purity and standards 13. Evaluate the role of the U.S. Food and Drug Administration in the drug approval process. 14. Categorize the four stages of new drug testing 15. Discuss how recent changes to the approval process have increased the speed at which new drugs reach consumers. 16. Compare and contrast prescription and over-the-counter drugs 17. Explain how scheduled drugs are classified and regulated 18. Describe the Canadian drug approval process and identify similarities to the drug approval process in the United States. 19. Outline a plan for improving patient adherence to the medical regimen. 20. Describe how the storage of drugs can affect their effectiveness. 21. Describe the components of a legal prescription and the abbreviations associated with drug orders. 22. Outline a plan for improving patient adherence to the medical regimen. 23. Describe how the storage of drugs can affect their effectiveness. 4|Page NURSING DEPARTMENT 24. Describe the components of a legal prescription and the abbreviations associated with drug orders. TOPIC (S) LEARNING ACTIVITIES Syllabus Introduction to Pharmacology: Concepts and Connections Drug Regulations Principles of Drug Administration Chapters 1,2,3 (CO 1,2,3,4,8,9) Complete Math assignment Quiz 1 covering Chapters 1-3 ( available Wednesday- Saturday 11:55 pm EST) Chapter readings: Chapters 6,7,9,15,36 OUTSIDE WORK & ASSIGNED READINGS DATE Week 2 At the end of this lesson, you will be able to: SPECIFIC OBJECTIVES 1. Differentiate health care services based on primary, secondary and tertiary disease prevention categories. 2. Outline a plan for improving patient adherence to the medical regimen. 3. Describe how the storage of drugs can affect their effectiveness. 4. Describe the components of a legal prescription and the abbreviations associated with drug orders. 5. Explain how idiosyncratic reactions differ from other types of adverse effects. 6. Explain why certain drugs with carcinogenic or teratogenic potential are used in pharmacotherapy. 7. Report the characteristic signs, symptoms, and treatment for each of the following organ-specific adverse events: nephrotoxicity, neurotoxicity, hepatotoxicity, dermatologic toxicity, bone marrow toxicity, cardiotoxicity, and skeletal muscle toxicity. 8. Use examples to explain the importance of drug interactions to pharmacotherapy. 9. Describe the mechanisms of drug interactions that alter absorption, distribution, metabolism, or excretion. 10. Differentiate among additive, synergistic, and antagonistic drug interactions. 11. Identify examples of drug–food interactions that may impact pharmacotherapeutic outcomes. 12. Identify examples of drug–food interactions that may impact pharmacotherapeutic outcomes. 13. Identify examples of drug–food interactions that may impact pharmacotherapeutic outcomes. 14. Identify examples of drug–food interactions that may impact pharmacotherapeutic outcomes. 5|Page NURSING DEPARTMENT 15. Identify efforts recommended by health care agencies to monitor medication errors and provide information to health care providers 16. Compare and contrast the different phases of the nursing process. 17. Provide examples of how the nursing process is used during pharmacotherapy. 18. Identify the purposes of collecting data in the assessment phase of the nursing process. 19. Explain how nursing diagnoses are identified and worded. 20. Describe the steps in the planning phase of the nursing process. 21. Identify specific pharmacology topics employed in the implementation phase of the nursing process. 22. Explain the purpose of the evaluation phase in the nursing process. 23. Explain what actions follow the evaluation phase of the nursing process. 24. Explain the role of complementary and alternative therapies in promoting patient wellness. 25. Analyze why herbal and dietary supplements have increased in popularity. 26. Identify the parts of an herb that contain active ingredients and the types of formulations made from these parts. 27. Compare the strengths and weaknesses of the Dietary Supplement Health and Education Act of 1994 with the Dietary Supplement and Nonprescription Drug Consumer Protection Act of 2006. 28. Describe specific adverse effects that may be caused by herbal preparations. 29. Discuss the role of the nurse in teaching patients about complementary and alternative therapies. 30. Identify common drug–herb interactions. 31. Explain why it is important to standardize herbal products based on specific active ingredients. 32. Describe the exchange of fluids that occurs among the different fluid compartments in the body. 33. Identify conditions for which intravenous fluid therapy may be indicated. 34. Explain how changes in the osmolality or tonicity of a fluid can cause water to move to a different compartment. 35. Compare and contrast the use of blood products, crystalloids, and colloids in intravenous therapy. 36. Explain the importance of electrolyte balance in the body. 37. Explain the pharmacotherapy of sodium and potassium imbalances. 38. Discuss medications used to treat acidosis and alkalosis. 39. Describe the nurse’s role in the pharmacologic management of fluid imbalance, electrolyte, and acid–base disorders. 40. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 41. Apply the nursing process to care for patients receiving drug therapy for fluid imbalance, electrolyte, and acid–base disorders. 6|Page NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES OUTSIDE WORK & ASSIGNED READINGS Adverse Drug Effects and Drug Interactions Medication Errors and Risk Reduction Pharmacology and the Nursing Process The Role of Complementary and Alternative Therapies in Pharmacotherapy Discussions PowerPoints Chapters 6,7,9,15,36 Quiz 2 covering Chapters 6,7,9,15,36 Biphosphonate Therapy Case Study Cellular Disorders Read: Ch. 49,50,51,52,53 WEEK 3 SPECIFIC At the end of this lesson, you will be able to: OBJECTIVES 1. Explain the mechanisms by which pathogens infect the body. 2. Describe methods for classifying bacteria. 3. Explain the mechanisms by which anti-infective drugs act to kill pathogens or restrict their growth. 4. Describe the clinical significance of bacterial resistance 5. Identify steps that the nurse can take to limit the development of resistance. 6. Describe the clinical rationale for selecting specific antibiotics. 7. Identify the role of the nurse in preventing, identifying, and treating adverse effects due to antibiotic therapy. 8. Explain how the patient’s immune status, history of allergic reactions, age, pregnancy status, genetics, or local tissue conditions influence anti-infective pharmacotherapy. 9. Explain the clinical importance of selecting the correct antibiotic for the individual patient. 10. Describe the development of superinfections. 11. Explain the structure of a bacterial cell wall and its importance to pharmacotherapy. 12. Identify the classes of antibiotics that act by affecting the synthesis of the bacterial cell wall. 13. Explain the mechanisms by which antibiotics affect the bacterial cell wall. 14. Compare and contrast the four classes of penicillins. 15. Compare and contrast the five generations of cephalosporins. 16. Identify similarities and differences among drugs in the carbapenem class 17. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 18. Apply the nursing process to care for patients who are receiving pharmacotherapy with bacterial cell wall inhibitors. 7|Page NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES 19. Explain the steps in the synthesis of bacterial proteins. 20. Identify the classes of antibiotics that act by inhibiting bacterial protein synthesis. 21. Explain mechanisms by which antibiotics inhibit bacterial protein synthesis. 22. Explain how protein synthesis inhibitors exert selective toxicity toward bacterial, rather than human, cells. 23. Describe means by which bacteria become resistant to protein synthesis inhibitors. 24. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 25. Apply the nursing process to care for patients who are receiving pharmacotherapy with bacterial protein synthesis inhibitors. Basic Principles of Anti-Infective Pharmacotherapy Antibiotics Affecting the Bacterial Cell Wall Antibiotics Affecting Bacterial Protein Synthesis Chapter readings Discussion post Case Study Quiz 3: covering : Ch. 49,50,51,52,53 Read: Cellular Disorders Chapters 54,55,56,57,58 Case Study OUTSIDE WORK & ASSIGNED READINGS DATE WEEK 4 At the end of this lesson, you will be able to: SPECIFIC 1. Compare and contrast the types of infections caused by mycobacteria. OBJECTIVES 2. Explain the pathogenesis of tuberculosis. 3. Describe how the pharmacotherapy of tuberculosis differs from that of bacterial infections. 4. Identify the most common drug regimens for treating tuberculosis. 5. Compare and contrast the types of infections caused by mycobacteria. 6. Explain the pathogenesis of tuberculosis. 7. Describe how the pharmacotherapy of tuberculosis differs from that of bacterial infections. 8. Identify the most common drug regimens for treating tuberculosis. 9. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 10. Explain significant patient variables that must be considered for effective pharmacotherapy with antimycobacterial drugs. 11. Apply the nursing process to care for patients receiving pharmacotherapy for mycobacterial infections. 8|Page NURSING DEPARTMENT 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. Compare and contrast the pharmacotherapy of fungal and bacterial infections. Classify mycoses based on the location of the infection and the causative organism. Compare and contrast the pharmacotherapy of superficial and systemic fungal infections. Identify the types of patients at greatest risk of acquiring serious fungal infections. Describe the nurse’s role in the pharmacologic management of fungal infections. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. Apply the nursing process to care for patients receiving pharmacotherapy for fungal infections. Identify features of protozoa and helminths that distinguish them from bacteria. Identify protozoan and helminthic infections that may benefit from pharmacotherapy. Explain why an understanding of Plasmodium’s life cycle is important to the successful pharmacotherapy of malaria. Explain the etiology, pathogenesis, and pharmacotherapy of amebiasis, giardiasis, cryptosporidiosis, toxoplasmosis, trichomoniasis, trypanosomiasis, and leishmaniasis. Explain the etiology, pathogenesis, and pharmacotherapy of ascariasis, enterobiasis, hookworm, and tapeworm infections. Describe the nurse’s role in the pharmacologic management of protozoan and helminthic infections For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. Apply the nursing process to care for patients receiving pharmacotherapy for protozoan and helminthic infections. Describe the major structural components of viruses. Identify viral infections that benefit from pharmacotherapy. Explain the five principal stages in the pathogenesis of a viral infection. Explain general principles related to the pharmacotherapy of viral infections. Describe the nurse’s role in the pharmacologic management of patients receiving medications for herpes viruses, influenza viruses, and hepatitis viruses. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of 9|Page NURSING DEPARTMENT 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. TOPIC (S) LEARNING ACTIVITIES drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. Apply the nursing process to care for patients receiving pharmacotherapy for viral infections. Describe the primary steps in the pathogenesis of HIV infection. Explain reasons for treatment failure during HIV-AIDS pharmacotherapy. Explain the purpose and expected outcomes of HIV-AIDS pharmacotherapy. Describe the advantages of highly active antiretroviral therapy in the pharmacotherapy of HIV infection. Compare and contrast the six classes of antiretroviral medications. Describe the difficulties in developing a vaccine to prevent HIV-AIDS. Explain the protocol and rationale for postexposure prophylaxis following occupational exposure to HIV-infected fluids. Describe the antiretroviral protocol used for reducing the risk of perinatal transmission and for treating pediatric patients with HIVAIDS. Identify opportunistic infections commonly acquired by patients with AIDS and the drugs used to treat them. Describe the nurse’s role in the pharmacologic management of patients receiving antiretroviral medications. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. Apply the nursing process to care for patients receiving pharmacotherapy for HIV-AIDS. Pharmacotherapy of Mycobacterial Infections Pharmacotherapy of Fungal Infections Pharmacotherapy of Protozoan and Helminthic Infections Pharmacotherapy of Non-HIV Infections Pharmacotherapy of HIV-AIDS Chapter readings Discussion post Quiz covering : Chapters 54,55,56,57,58 Read: Immunological Disorders Chapters 43,44,45,46 Read: Integumentary Disorders Chapter 76 OUTSIDE WORK & ASSIGNED READINGS DATE WEEK 5 At the end of this lesson, you will be able to: SPECIFIC OBJECTIVES 1. Identify the major components of the lymphatic system. 2. Describe the components of the nonspecific body defense system and their functions. 10 | P a g e NURSING DEPARTMENT 3. Compare and contrast specific and nonspecific body defenses. 4. Identify the signs and symptoms of inflammation. 5.Outline the basic steps in the acute inflammatory response. 6.Explain the role of histamine and other chemical mediators in the inflammatory response. 7. Compare and contrast the humoral and cell-mediated immune responses. 8.Explain the pathophysiology of inflammation and fever. 9.Identify drug classes used to treat inflammation and fever. 10.Explain how aspirin damages the gastrointestinal mucosa. 11.Describe the symptoms and treatment of salicylism. 12.Compare the actions and adverse effects of aspirin to ibuprofen and ibuprofen-like drugs. 13.Compare the actions and adverse effects of the cyclooxygenase-2 inhibitors to other nonsteroidal anti-inflammatory drugs. 14. Describe the nurse’s role in the pharmacologic management of inflammation and fever. 15. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 16. Apply the nursing process to care for patients who are receiving drug therapy for fever or inflammation 17. Compare and contrast the therapeutic applications of the two classes of immunomodulators. 18. Describe the roles of interferons, interleukins, and other cytokines in modulating the immune response. 19. Explain how pegylation of the interferon molecule allows for less frequent dosing. 20. Explain why therapy with immunosuppressant medications is necessary following organ transplants. 21. Identify the classes of drugs used as immunosuppressants. 22. Compare and contrast polyclonal and monoclonal antibodies. 23.For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 24.Apply the nursing process to care for patients who are receiving immunostimulants and immunosuppressants. 25. Explain why the development of a smallpox vaccine was one of the most significant discoveries of modern medicine. 26. Compare and contrast active and passive immunity. 27. Explain the immune response that leads to the development of active immunity. 28. Prepare a table listing the types of vaccines, their indications, and potential adverse effects. 29. Explain why it is important to administer childhood vaccines at specific 11 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES OUTSIDE WORK & ASSIGNED READINGS ages. 30. Identify contraindications for vaccine administration. 31. Describe the pathogenesis and immunization of bacterial infections, including diphtheria, pertussis, tetanus, pneumococcus, and meningococcus. 32. Describe the pathogenesis and immunization of viral infections, including hepatitis A and B, influenza, rabies, measles, mumps, rubella, polio, varicella zoster, human papillomavirus, and rotavirus. 33. Explain the rationale for administering antibodies to establish passive immunity. 34. For each of the major vaccines and patient age groups, identify the schedule for the recommended dosage sequence established by the Centers for Disease Control and Prevention. 35. Apply the nursing process to care for patients receiving immunizing agents. 36. Identify the structure and functions of the skin and associated structures. 37. Explain the process by which superficial skin cells are replaced. 38. Explain how skin diseases are classified. 39. Describe the drug therapies for bacterial, fungal, viral, and parasitic infections of the skin. 40. Explain the etiology, pathogenesis, and pharmacotherapy for acne vulgaris, rosacea, dermatitis, and psoriasis. 41. Outline the stepwise approach to treating psoriasis. 42. Describe the prevention and management of minor burns. 43. Explain the pharmacotherapy of alopecia. 44. Describe the nurse’s role in the pharmacologic management of skin disorders. 45. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 46. Apply the nursing process to the care of patients who are receiving pharmacotherapy for skin disorders. Pharmacotherapy of Inflammation and Fever Review of Body Defenses and the Immune System Immunostimulants and Immunosuppressants Immunizing Agents Pharmacotherapy of Dermatologic Disorders Chapter readings Discussion post Quiz covering : Chapters 43,44,45,46 and 76 Cardiovascular Disorders Read: (Ch 31,32,33,37,38) Case Study 12 | P a g e NURSING DEPARTMENT DATE WEEK 6 At the end of this lesson, you will be able to: SPECIFIC 1. Describe the major structures of the cardiovascular system. OBJECTIVES 2. Identify the components of blood and their functions. 3. Construct a flowchart diagramming the primary steps of hemostasis. 4. Describe the structure of the heart and the function of the myocardium. 5. Describe the role of coronary arteries in supplying the myocardium with oxygen. 6. Illustrate the flow of electrical impulses through the normal heart. 7. Explain the major factors affecting cardiac output. 8. Explain the effects of cardiac output, peripheral resistance, and blood volume on hemodynamics. 9. Discuss how the vasomotor center, baroreceptors, chemoreceptors, and hormones regulate blood pressure. 10. Summarize the link between high blood cholesterol, low-density lipoprotein levels, and atherosclerosis. 11. Compare and contrast the different types of lipids. 12. Illustrate how lipids are transported through the blood. 13. Compare and contrast the clinical importance of the different types of lipoproteins. 14. Give examples of how cholesterol and low-density lipoprotein levels can be controlled with nonpharmacologic means. 15. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 16. Categorize antihyperlipidemic drugs based on their classification and mechanism of action. 17. Explain the nurse’s role in the safe administration of drugs for lipid disorders. 18. Apply the nursing process to care for patients receiving drug therapy for lipid disorders. 19. Describe the role of calcium ions in the contraction of smooth and cardiac muscle. 20. Explain why the actions of the beta1-adrenergic antagonists are similar to those of the calcium channel blockers. 21. Describe how calcium channel blockers interact with the L-type calcium channel. 22. Identify the physiological effects of calcium channel blockers on arterial smooth muscle and cardiac muscle. 23. Explain the classification of calcium channel blockers. 24. Compare and contrast the actions of dihydropyridine versus nondihydropyridine calcium channel blockers. 25. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of 13 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 26. Apply the nursing process to care for patients receiving calcium channel blockers. 27. Explain how hypertension is classified. 28. Summarize the long-term consequences of untreated hypertension. 29. Compare and contrast the roles of nonpharmacologic and pharmacologic methods in the management of hypertension. 30. Describe general principles guiding the pharmacotherapy of hypertension. 31. Identify drug classes used in the primary and alternate management of hypertension. 32. Describe the pharmacologic management of hypertensive emergencies. 33. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 34. Apply the nursing process to care for patients receiving antihypertensive drugs. 35. Describe factors that affect myocardial oxygen supply and demand. 36. Explain the relationship between atherosclerosis and coronary artery disease. 37. Explain the pathophysiology of angina pectoris and myocardial infarction. 38. Discuss the role of therapeutic lifestyle changes in the management of coronary artery disease. 39. Describe the pharmacologic management of the different types of angina. Describe the pharmacologic management of myocardial infarction 40. Discuss the role of therapeutic lifestyle changes in the management of coronary artery disease. 41. Describe the pharmacologic management of the different types of angina. 42. Describe the pharmacologic management of myocardial infarction. 43. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 44. Apply the nursing process to care for patients receiving drug therapy for angina and myocardial infarction Review of the Cardiovascular System Pharmacotherapy of Hyperlipidemia Calcium Channel Blockers Pharmacotherapy of Hypertension Pharmacotherapy of Angina Pectoris and Myocardial Infarction Chapter readings 14 | P a g e NURSING DEPARTMENT ACTIVITIES OUTSIDE WORK & ASSIGNED READINGS Discussion post Case Study Quiz covering: Chapters 31,32,33,37,38 Read: Cardiovascular Disorders (39,40,41) Read: Respiratory Disorders (Ch 47,48) Case Study DATE WEEK 7 At the end of this week, the students will be able to: SPECIFIC 18. Identify the major diseases associated with heart failure. OBJECTIVES 19. Relate how the symptoms associated with heart failure may be caused by weakened heart muscle and diminished cardiac output. 20. Identify compensatory mechanisms used by the body to maintain cardiac output in patients with heart failure. 21. Describe how heart failure is classified. 22. Describe the nurse’s role in the pharmacologic management of heart failure. 23. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 24. Apply the nursing process to care for patients receiving drug therapy for heart failure. 25. Identify disorders associated with an increased risk of dysrhythmias. 26. Explain how rhythm abnormalities can affect cardiac function. 27. Sketch a typical cardiac action potential and label the flow of potassium, sodium, and calcium ions during each phase. 28. Design a table that indicates the classification of dysrhythmias and the types of drugs used to treat them. 29. Describe general principles guiding the management of dysrhythmias. 30. Identify the primary mechanisms of action of antidysrhythmic drugs 31. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 32. Apply the nursing process to care for patients receiving drug therapy for dysrhythmias. 16. Describe primary risk factors for thromboembolic disorders. 17. Explain the etiology and symptoms of coagulation disorders. 18. Identify the primary mechanisms by which coagulation-modifying drugs act. 19. Explain how laboratory testing of coagulation parameters is used to monitor anticoagulant pharmacotherapy. 20. Describe the nurse’s role in the pharmacologic management of patients with coagulation disorders 15 | P a g e NURSING DEPARTMENT TOPIC (S) 21. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, Pregnancy category, and important adverse effects. 22. Apply the nursing process to care for patients receiving drug therapy for coagulation disorders. 23. Identify the anatomic structures associated with the lower respiratory tract and their functions. 24. Explain how the autonomic nervous system regulates airway diameter. 25. Explain the role of inflammation and bronchospasm in the pathogenesis of asthma. 26. Compare the advantages and disadvantages of using the inhalation route of drug administration for pulmonary drugs. 27. Describe the types of devices used to deliver aerosol therapies via the inhalation route. 28. Explain the three basic principles of asthma management recommended by the National Asthma Education and Prevention Program. 29.Compare and contrast the indications for pharmacotherapy with the short- versus long-acting beta-adrenergic agonists. 30. Describe the nurse’s role in the pharmacologic management of lower respiratory tract disorders 31. Apply the nursing process to care for patients receiving pharmacotherapy for lower respiratory tract disorders 32. Identify structures of the upper respiratory tract that serve as body defenses against foreign substances. 33. Describe the common causes and symptoms of allergic rhinitis. 34. Differentiate between H1 and H2 histamine receptors. 35. Compare and contrast the first- and second-generation antihistamines. 36. Explain why intranasal corticosteroids are the drugs of choice for the treatment of allergic rhinitis. 37. Compare and contrast the oral and intranasal decongestants. 38. Explain why it is usually better to take individual drugs for the common cold, rather than a multisymptom combination product. 39. Describe the appropriate use of cough suppressants. 40. Describe the use of drugs prescribed to treat thick bronchial secretions. 41. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 42. Apply the nursing process to care for patients who are receiving pharmacotherapy for allergic rhinitis and the common cold. Pharmacotherapy of Heart Failure Pharmacotherapy of Dysrhythmias Pharmacotherapy of Coagulation Disorders Pharmacotherapy of Asthma and Other Pulmonary Disorders Pharmacotherapy of Allergic Rhinitis and the Common Cold 16 | P a g e NURSING DEPARTMENT LEARNING ACTIVITIES Discussion post Case study Quiz covering : Cardiovascular Disorders (39,40,41) Read: Respiratory Disorders (Ch 47,48) OUTSIDE WORK & ASSIGNED READINGS DATE SPECIFIC OBJECTIVES Gastrointestinal Disorders Read: (Ch 61,62,63,64) Prepare for Mid-term WEEK 8 At the end of this lesson, you will be able to: 1. 1. Describe the major anatomic structures of the digestive system. 2. Outline the steps in the process of digestion. 3. Describe the primary functions of the stomach. 4. Analyze how the anatomic structures of the small intestine promote the absorption of nutrients and drugs 5. Describe the primary structures and functions of the large intestine. 6. Describe the functions of the liver and their relevance to drug therapy. 7. Explain the hepatic portal system and its importance to drug therapy. 8. Explain the nervous control of digestion. 9. Explain the enzymatic breakdown of nutrients by the digestive system. 10. Explain the physiological regulation of gastric acid secretion. 11. Describe factors that suppress and those that promote the formation of peptic ulcers. 12. Compare and contrast duodenal ulcers and gastric ulcers. 13. Identify the etiology, signs, and symptoms of peptic ulcer disease and gastroesophageal reflux disease. 14. Outline the treatment goals for the pharmacotherapy of peptic ulcer disease and gastroesophageal reflux disease. 15. Identify the classification of drugs used to treat peptic ulcer disease and gastroesophageal reflux disease. 16. Explain the pharmacologic strategies for eradicating Helicobacter pylori. 17. Describe the nurse’s role in the pharmacologic management of patients with peptic ulcer disease and gastroesophageal reflux disease. 18. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 19. Apply the nursing process to care for patients who are receiving pharmacotherapy for peptic ulcer disease and gastroesophageal reflux disease. 20. Compare and contrast the definition of constipation used by patients to that used for diagnosis by health care providers. 21. Compare and contrast the different mechanisms of action of laxatives. 22. Explain the pathogenesis of constipation and diarrhea. 17 | P a g e NURSING DEPARTMENT 23. Compare and contrast the types of drugs used to treat inflammatory bowel disease and irritable bowel syndrome. 24. Explain conditions in which the pharmacotherapy of nausea and vomiting is indicated. 25. Identify drugs that are used to treat acute and chronic pancreatitis. 26. Describe the nurse’s role in the pharmacologic management of bowel disorders, nausea and vomiting, and other gastrointestinal conditions 27. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 28. Apply the nursing process to care for patients who are receiving pharmacotherapy for bowel disorders, nausea and vomiting, and other gastrointestinal conditions. 29. Describe the role of vitamins in maintaining wellness. 30. Identify conditions for which vitamin and mineral therapy may be indicated. 31. Explain the governmental regulation of vitamins and minerals. 32. Discuss the role of the recommended dietary allowance in determining the standardized requirement of various vitamins and minerals. 33. Compare and contrast fat-soluble and water-soluble vitamins. 34. For each of the major vitamins, identify the mechanism(s) of action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 35. Identify the major functions of macrominerals and microminerals. 36. Apply the nursing process to care for patients who are receiving vitamin and mineral supplementation therapy. Review of the Gastrointestinal System TOPIC (S) Pharmacotherapy of Peptic Ulcer Disease Pharmacotherapy of Bowel Disorders and Other Gastrointestinal Conditions Vitamins and Minerals LEARNING Chapter readings ACTIVITIES Discussion post Case Study Midterm exam covering weeks 1-8 Read: Gastrointestinal Disorders (65,66) OUTSIDE Read: Genitourinary (Ch 35, 53) WORK & Case Study ASSIGNED Quiz READINGS DATE Week 9 At the end of this lesson, you will be able to: SPECIFIC 1. Identify conditions that may benefit from parenteral or enteral OBJECTIVES nutrition. 2. Compare and contrast enteral and parenteral methods of nutrition. 3. Compare and contrast methods by which enteral feedings are administered. 18 | P a g e NURSING DEPARTMENT 4. Distinguish among polymeric, elemental, semielemental, and modular formulas for enteral nutrition. 5. Identify the basic classes of nutrients contained in enteral formulas and their functions. 6. Identify the possible complications and adverse effects of enteral nutrition administration. 7. Describe the types of drug interactions that can occur when enteral nutrition formulas are given. 8. Explain the differences between delivering parenteral nutrition through a peripheral line versus a central line 9. Describe the components of total parenteral nutrition solutions and the function of each element in attaining the body’s daily requirements. 10. Describe the possible complications of parenteral nutrition therapy. 11. Identify drugs that may be incompatible with parenteral nutrition solutions. 12. Apply the nursing process to care for patients who are receiving enteral or parenteral nutrition. 13. Explain the role of the urinary system in maintaining fluid, electrolyte, and acid–base homeostasis. 14. Explain the physiological processes that change the composition of filtrate as it travels through the nephrons. 15. Describe the adjustments in pharmacotherapy that must be considered in patients with renal failure. 16. Identify indications for diuretics. 17. Compare and contrast the loop, thiazide, potassium-sparing, osmotic, and carbonic anhydrase inhibitor diuretics. 18. Describe the nurse’s role in the pharmacologic management of renal failure and in diuretic therapy. 19. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 20. Use the nursing process to care for patients who are receiving diuretics or drug therapy for renal failure. 24. Classify types of urinary tract infections based on their anatomic location. 25. Explain the epidemiology and pathogenesis of urinary tract infections. 26. Compare and contrast the pharmacotherapy of complicated versus uncomplicated urinary tract infections. 27. Identify the classes of antibiotics used to treat urinary tract infections. 28. Describe modifications in the pharmacotherapy of urinary tract infections for infants and children, pregnancy, older adults, and those with recurring infections. 29. Explain why folate inhibitors exert selective toxicity toward bacterial cells. 30. For each of the classes shown in the chapter outline, identify the 19 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 31.Apply the nursing process to care for patients receiving pharmacotherapy for urinary tract infections. Enteral and Parenteral Nutrition Weight Reduction Strategies and the Pharmacotherapy of Obesity Diuretic Therapy and the Pharmacotherapy of Renal Failure Sulfonamides and the Pharmacotherapy of Urinary Tract Infections Chapter readings Discussion post Quiz covering: Gastrointestinal Disorders (65,66) and Genitourinary (Ch 35, 53) Read: Endocrine Disorders Chapters 34, 35, 67, 68, 69 OUTSIDE WORK & ASSIGNED READINGS DATE WEEK 10 At the end of this lesson, you will be able to: SPECIFIC 1. Illustrate the steps in the renin-angiotensin-aldosterone pathway. OBJECTIVES 2. Identify the primary physiological factors that control renin secretion. 3. Explain the two primary functions of angiotensin-converting enzyme. 4. Describe multiple mechanisms by which angiotensin II raises blood pressure. 5. Explain how the actions of aldosterone can lead to high blood pressure. 6. Identify the specific steps in the renin-angiotensin-aldosterone system that can be blocked by medications. 7. Explain how the actions of aldosterone can lead to high blood pressure. 8. Identify the specific steps in the renin-angiotensin-aldosterone system that can be blocked by medications. 9. Apply the nursing process to care for patients receiving drugs affecting the renin-angiotensin-aldosterone system. 10. Explain the role of the urinary system in maintaining fluid, electrolyte, and acid–base homeostasis. 11. Explain the physiological processes that change the composition of filtrate as it travels through the nephrons. 12. Describe the adjustments in pharmacotherapy that must be considered in patients with renal failure. 13. Identify indications for diuretics. 14. Compare and contrast the loop, thiazide, potassium-sparing, osmotic, and carbonic anhydrase inhibitor diuretics. 15. Describe the nurse’s role in the pharmacologic management of renal failure and in diuretic therapy. 16. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug 20 | P a g e NURSING DEPARTMENT action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 17. Use the nursing process to care for patients who are receiving diuretics or drug therapy for renal failure. 18. Describe the general structure and functions of the endocrine system. 19. Compare and contrast the nervous and endocrine systems in the control of homeostasis. 20. Explain circumstances in which hormone receptors may be upregulated or down-regulated. 21. Through the use of a specific example, explain the concept of negative feedback in the endocrine system. 22. Explain the three primary types of stimuli that regulate hormone secretion. 23. Identify indications for hormone pharmacotherapy. 24. Explain the principal actions of the hormones secreted by the hypothalamus and pituitary gland. 25. Identify indications for hypothalamic hormone therapy. 26. Explain the pharmacotherapy of growth hormone disorders in children and adults. 27. Explain the pharmacotherapy of antidiuretic hormone disorders. 28. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 29. Apply the nursing process to care for patients receiving pharmacotherapy for disorders of the hypothalamus and pituitary gland. 30. Explain how blood glucose levels are maintained within narrow limits by insulin and glucagon. 31. Compare and contrast the etiology and pathogenesis of type 1, type 2, and gestational diabetes. 32. Describe the signs and diagnosis of diabetes. 33. Describe the acute complications of diabetes. 34. Identify the chronic complications of diabetes. 35. Compare and contrast the pharmacotherapy of the different types of diabetes. 36. For each type of insulin, identify the onset of action, peak action and duration of action, administration routes, when it is given related to meals, compatibility with other insulins, and adverse effects. 37. Apply the nursing process to care for patients who are receiving pharmacotherapy for diabetes. 38. Explain how blood glucose levels are maintained within narrow limits by insulin and glucagon. 39. Compare and contrast the etiology and pathogenesis of type 1, type 2, and gestational diabetes. 21 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES OUTSIDE WORK & ASSIGNED READINGS 40. Describe the signs and diagnosis of diabetes. 41. Describe the acute complications of diabetes. 42. Identify the chronic complications of diabetes. 43. Compare and contrast the pharmacotherapy of the different types of diabetes. 44. Describe the acute complications of diabetes. 45. Identify the chronic complications of diabetes. 46. Compare and contrast the pharmacotherapy of the different types of diabetes. 47. Describe the acute complications of diabetes. 48. Identify the chronic complications of diabetes. 49. Compare and contrast the pharmacotherapy of the different types of diabetes. Drugs Affecting the Renin-Angiotensin-Aldosterone System Diuretic Therapy and the Pharmacotherapy of Renal Failure Review of the Endocrine System Hypothalamic and Pituitary Drugs Pharmacotherapy of Diabetes Mellitus Chapter readings Discussion post Quiz covering: Endocrine Disorders Chapters 34, 35, 67, 68, 69 Read: Endocrine Disorders (70,71) Read: Musculoskeletal Disorders (Ch 27, 75) Case Study DATE WEEK 11 At the end of this lesson, you will be able to: SPECIFIC 1. 1. Explain the functions of thyroid hormone. OBJECTIVES 2. Explain the negative feedback control of thyroid function. 3. Explain how thyroid disorders are diagnosed. 4. Describe the pathophysiology of thyroid disorders. 5. Describe the pharmacotherapy of thyroid disorders. 6. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of 7. drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 8. Apply the nursing process to the care of patients receiving pharmacotherapy for thyroid disorders. 9. Apply the nursing process to the care of patients receiving pharmacotherapy for thyroid disorders. 10. Identify the functions of the three classes of hormones secreted by the adrenal gland. 11. Diagram the negative feedback regulation of corticosteroid secretion. 12. Identify common properties of the corticosteroid medications. 22 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES OUTSIDE 13. Describe the potential adverse effects of long-term corticosteroid therapy. 14. Compare and contrast the pharmacotherapy of acute and chronic adrenocortical insufficiency. 15. Explain how corticosteroids affect the inflammatory and immune responses. 16. Recognize nonendocrine disorders that respond to corticosteroid therapy. 17. Describe indications for pharmacotherapy with mineralocorticoids. 18. Explain the pharmacotherapy of Cushing’s syndrome. 19. Describe the nurse’s role in the pharmacologic management of adrenal disorders. 20. Apply the nursing process to the care of patients who are receiving pharmacotherapy with corticosteroids and mineralocorticoids. 21. Compare and contrast the etiology and pathophysiology of muscle spasms and muscle spasticity. 22. Describe the nonpharmacologic management of muscle spasms and muscle spasticity. 23. Identify drug classes used to treat muscle spasms and spasticity. 24. Compare and contrast the actions of the centrally acting and directacting skeletal muscle relaxants. 25. Explain the role of skeletal muscle relaxants as surgical adjuncts. 26. Describe the nurse’s role in the pharmacologic management of muscle spasms and muscle spasticity. 27. Apply the nursing process to care for patients receiving pharmacotherapy for muscle spasms and spasticity. 28. Describe the role of calcium in maintaining homeostasis in the nervous, muscular, skeletal, and cardiovascular systems. 29. Identify the recommended dietary allowance and the normal serum levels of calcium. 30. Explain the roles of parathyroid hormone, calcitonin, and vitamin D in maintaining calcium balance. 31. Explain the etiology, pathogenesis, and pharmacotherapy for hypocalcemia, osteomalacia, osteoporosis, rickets, osteoarthritis, rheumatoid arthritis, and gout. Pharmacotherapy of Thyroid Disorders Corticosteroids and Drugs Affecting the Adrenal Cortex Pharmacotherapy of Muscle Spasms and Spasticity Pharmacotherapy of Bone and Joint Disorders Chapter readings Discussion post Case Study Quiz covering: Endocrine Disorders (70,71) and Musculoskeletal Disorders (Ch 27, 75) Read: Neurological (Ch 16, 17, 18, 19, 20) 23 | P a g e NURSING DEPARTMENT WORK & ASSIGNED READINGS DATE SPECIFIC OBJECTIVES Case Study Review the Pharmacology of the Central Nervous WEEK 12 At the end of this lesson, you will be able to: 1. Distinguish between the functions of the central and peripheral nervous systems. 2. Compare and contrast the two divisions of the peripheral nervous system. 3. Compare and contrast the actions of the sympathetic and parasympathetic divisions of the autonomic nervous system. 4. Explain the process of synaptic transmission. 5. Explain mechanisms by which drugs affect synaptic transmission. 6. Describe the actions of acetylcholine at cholinergic synapses. 7. Describe the actions of norepineprhine at adrenergic synapses. 8. Compare the actions of the adrenal medulla with those of other sympathetic effector organs. 9. Explain how higher centers in the brain can influence autonomic function. 10. Design a method for classifying autonomic drugs based on which receptors are affected. 11. Identify the physiological responses produced when a drug activates cholinergic receptors. 12. Compare and contrast the mechanisms of action for direct- and indirect-acting cholinergic agonists. 13. Differentiate among the following types of cholinergic drugs: direct muscarinic agonists, indirect muscarinic agonists, and nicotinic agonists. 14. Differentiate between the pharmacotherapy of cholinergic crisis and myasthenic crisis. 15. Describe the pharmacotherapy of myasthenia gravis. 16. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 17. Apply the nursing process to care for patients receiving drug therapy with cholinergic agonists. 18. Identify the physiological responses produced when a drug activates adrenergic receptors. 19. Explain the direct and indirect mechanisms by which adrenergic agonists act. 20. Compare and contrast the characteristics of catecholamines and noncatecholamines. 21. Identify indications for pharmacotherapy with adrenergic agonists. 22. Compare and contrast the types of responses that occur when a drug 24 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES OUTSIDE WORK & ASSIGNED READINGS DATE SPECIFIC OBJECTIVES activates alpha1-, alpha2-, beta1-, or beta2-adrenergic receptors. 23. Apply the nursing process to care for patients receiving drug therapy with adrenergic agonists. 24. Identify the physiological responses produced when a drug blocks adrenergic receptors. 25. Compare and contrast the types of physiological responses that occur when a drug blocks alpha1-, alpha2-, beta1-, and beta2-adrenergic receptors. 26. Identify indications for pharmacotherapy with adrenergic antagonists. 27. Describe the first-dose phenomenon and how it may be prevented. 28. Explain the advantages of selective beta antagonists versus nonselective beta antagonists. 29. Explain why beta-adrenergic antagonists should never be abruptly discontinued. Review of Neurotransmitters and the Autonomic Nervous System Cholinergic Agonists Andrenergic Agonists Andrenergic Antagonists Cholinergic Antagonists Chapter readings Discussion post Quiz covering: Neurological (Ch 16, 17, 18, 19, 20) Read: Hematological Disorders (Ch 42,43,44,45,46) WEEK 12 At the end of this lesson, you will be able to: 1. Distinguish between the functions of the central and peripheral nervous systems. 2. Compare and contrast the two divisions of the peripheral nervous system. 3. Compare and contrast the actions of the sympathetic and parasympathetic divisions of the autonomic nervous system. 4. Explain the process of synaptic transmission. 5. Explain mechanisms by which drugs affect synaptic transmission. 6. Describe the actions of acetylcholine at cholinergic synapses. 7. Describe the actions of norepineprhine at adrenergic synapses. 8. Compare the actions of the adrenal medulla with those of other sympathetic effector organs. 9. Explain how higher centers in the brain can influence autonomic function. 10. Design a method for classifying autonomic drugs based on which receptors are affected. 25 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES 11. Identify the physiological responses produced when a drug activates cholinergic receptors. 12. Compare and contrast the mechanisms of action for direct- and indirect-acting cholinergic agonists. 13. Differentiate among the following types of cholinergic drugs: direct muscarinic agonists, indirect muscarinic agonists, and nicotinic agonists. 14. Differentiate between the pharmacotherapy of cholinergic crisis and myasthenic crisis. 15. Describe the pharmacotherapy of myasthenia gravis. 16. For each of the classes shown in the chapter outline, identify the prototype and representative drugs and explain the mechanism(s) of drug action, primary indications, contraindications, significant drug interactions, pregnancy category, and important adverse effects. 17. Apply the nursing process to care for patients receiving drug therapy with cholinergic agonists. 18. Identify the physiological responses produced when a drug activates adrenergic receptors. 19. Explain the direct and indirect mechanisms by which adrenergic agonists act. 20. Compare and contrast the characteristics of catecholamines and noncatecholamines. 21. Identify indications for pharmacotherapy with adrenergic agonists. 22. Compare and contrast the types of responses that occur when a drug activates alpha1-, alpha2-, beta1-, or beta2-adrenergic receptors. 23. Apply the nursing process to care for patients receiving drug therapy with adrenergic agonists. 24. Identify the physiological responses produced when a drug blocks adrenergic receptors. 25. Compare and contrast the types of physiological responses that occur when a drug blocks alpha1-, alpha2-, beta1-, and beta2-adrenergic receptors. 26. Identify indications for pharmacotherapy with adrenergic antagonists. 27. Describe the first-dose phenomenon and how it may be prevented. 28. Explain the advantages of selective beta antagonists versus nonselective beta antagonists. 29. Explain why beta-adrenergic antagonists should never be abruptly discontinued. Review of Neurotransmitters and the Autonomic Nervous System Cholinergic Agonists Andrenergic Agonists Andrenergic Antagonists Cholinergic Antagonists Chapter readings 26 | P a g e NURSING DEPARTMENT Discussion post OUTSIDE WORK & ASSIGNED READINGS DATE SPECIFIC OBJECTIVES Quiz covering: Hematological Disorders (Ch 42,43,44,45,46) Read: Hematological Disorders (Ch 42,43,44,45,46) WEEK 13 At the end of the week, the student will be able to: 1. Describe the physiology of hematopoiesis. 2. Describe how aspects of hematopoiesis can be modified by the administration of pharmacologic agents. 3. Explain the functions of erythropoietin. 4. Explain the functions of colony-stimulating factors. 5. Classify types of anemia based on their causes. 6. Illustrate the metabolism, storage, and transfer of iron in the body. 7. Identify the role of intrinsic factor in the absorption of vitamin B12. 8. Compare and contrast anemias caused by vitamin B12 and folate deficiency. 9. Describe the nurse’s role in the pharmacologic management of hematopoietic disorders. 10. Apply the nursing process to care for patients who are receiving drug therapy for hematopoietic disorders. 11. Identify the major components of the lymphatic system. 12. Describe the components of the nonspecific body defense system and their functions. 13. Compare and contrast specific and nonspecific body defenses. 14. Identify the signs and symptoms of inflammation. 15. Outline the basic steps in the acute inflammatory response. 16. Explain the role of histamine and other chemical mediators in the inflammatory response. 17. Compare and contrast the humoral and cell-mediated immune responses 18. Explain the pathophysiology of inflammation and fever. 19. Identify drug classes used to treat inflammation and fever. 20. Explain how aspirin damages the gastrointestinal mucosa. 21. Describe the symptoms and treatment of salicylism. 22. Compare the actions and adverse effects of aspirin to ibuprofen and ibuprofen-like drugs. 23. Compare the actions and adverse effects of the cyclooxygenase-2 inhibitors to other nonsteroidal anti-inflammatory drugs. 24. Describe the nurse’s role in the pharmacologic management of inflammation and fever. 25. Apply the nursing process to care for patients who are receiving drug therapy for fever or inflammation. 26. Compare and contrast the therapeutic applications of the two classes of 27 | P a g e NURSING DEPARTMENT immunomodulators. 27. Describe the roles of interferons, interleukins, and other cytokines in modulating the immune response. 28. Explain how pegylation of the interferon molecule allows for less frequent dosing. 29. Explain why therapy with immunosuppressant medications is necessary following organ transplants. 30. Identify the classes of drugs used as immunosuppressants. 31. Compare and contrast polyclonal and monoclonal antibodies. 32. Apply the nursing process to care for patients who are receiving immunostimulants and immunosuppressants. 33. Explain why the development of a smallpox vaccine was one of the most significant discoveries of modern medicine. 34. Compare and contrast active and passive immunity. 35. Explain the immune response that leads to the development of active immunity. 36. Explain why the development of a smallpox vaccine was one of the most significant discoveries of modern medicine. 37. Compare and contrast active and passive immunity. 38. Explain the immune response that leads to the development of active immunity. 39. Explain why the development of a smallpox vaccine was one of the most significant discoveries of modern medicine. 40. Compare and contrast active and passive immunity. 41. Explain the immune response that leads to the development of active immunity. 42. Explain why the development of a smallpox vaccine was one of the most significant discoveries of modern medicine. 43. Compare and contrast active and passive immunity. 44. Explain the immune response that leads to the development of active immunity. 45. Explain why the development of a smallpox vaccine was one of the most significant discoveries of modern medicine. 46. Compare and contrast active and passive immunity. 47. Explain the immune response that leads to the development of active immunity. 48. Explain why the development of a smallpox vaccine was one of the most significant discoveries of modern medicine. 49. Compare and contrast active and passive immunity. 50. Explain the immune response that leads to the development of active immunity. 51. Explain why the development of a smallpox vaccine was one of the most significant discoveries of modern medicine. 52. Compare and contrast active and passive immunity. 53. Explain the immune response that leads to the development of active immunity. 28 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES OUTSIDE WORK & ASSIGNED READINGS DATE SPECIFIC OBJECTIVES 54. Describe the pathogenesis and immunization of viral infections, including hepatitis A and B, influenza, rabies, measles, mumps, rubella, polio, varicella zoster, human papillomavirus, and rotavirus. 55. Explain the rationale for administering antibodies to establish passive immunity. 56. For each of the major vaccines and patient age groups, identify the schedule for the recommended dosage sequence established by the Centers for Disease Control and Prevention. 57. Apply the nursing process to care for patients receiving immunizing agents. Pharmacotherapy of Hematopoietic Disorders Review of Body Defenses and the Immune System Pharmacotherapy of Inflammation and Fever Immunostimulants and Immunosuppressants Immunizing Agents Chapter readings Discussion post Quiz covering: Hematological Disorders (Ch 42,43,44,45,46) Read: Reproductive Disorders (Chapter 10,72, 73, 74) WEEK 14 At the end of this lesson, the student will be able to: 1. Justify the rationale for using drugs during pregnancy and lactation. 2. Describe physiological changes during pregnancy that may affect the absorption, distribution, metabolism, and excretion of drugs. 3. Describe the placental transfer of drugs from mother to infant. 4. Differentiate among the U.S. Food and Drug Administration pregnancy risk categories. 5. Explain how drugs administered during the different stages of fetal development affect the potential for teratogenic effects. 6. Identify factors that influence the transfer of drugs into breast milk. 7. Describe signs of adverse drug reactions in the breast-feeding infant. 8. Outline important points in the patient and family education regarding drug use during pregnancy and lactation 9. Describe signs of adverse drug reactions in the breast-feeding infant. 10. Outline important points in the patient and family education regarding drug use during pregnancy and lactation 11. Compare and contrast the advantages and disadvantages of hormone replacement therapy during menopause. 12. Explain the use of uterine stimulants to promote labor and delivery. 13. Discuss the use of uterine relaxants in suppressing preterm labor. 14. Explain how drug therapy may be used to treat female infertility. 15. Describe the nurse’s role in the pharmacologic management of disorders and conditions of the female reproductive system. 29 | P a g e NURSING DEPARTMENT TOPIC (S) LEARNING ACTIVITIES OUTSIDE WORK & ASSIGNED READINGS DATE TOPIC (S) 16. Apply the nursing process to the care of patients who are receiving pharmacotherapy for disorders and conditions of the female reproductive system. 17. Identify the choices available for birth control. 18. Delineate advantages and disadvantages of the different contraceptive options. 19. Explain the mechanisms by which estrogens and progestins prevent conception. 20. Compare the safety and effectiveness of different birth control methods. 21. Explain how drugs may be used to provide emergency contraception and to terminate pregnancy. 22. Describe the nurse’s role in the pharmacologic management of patients who are taking oral contraceptives. 23. Compare and contrast the options available for long-term contraception. 24. Explain the use of drugs for emergency contraception and inducing pharmacologic abortion. 25. Apply the nursing process to the care of patients who are receiving pharmacotherapy for contraception Pharmacotherapy During Pregnancy and Lactation Estrogens, Progestins, and Drugs Modifying Uterine Function Drugs for Modifying Conception Drugs for Disorders and Conditions of the Male Reproductive System Chapter readings Discussion post Quiz covering: (Chapter 10,72, 73, 74) Prepare for final exam covering weeks 9-14 WEEK 15 Final Exam Instructional Methods The following strategies may be used in this class: 1. Threaded Discussions 2. Case studies 3. Quizzes 4. Readings 5. Exams 30 | P a g e NURSING DEPARTMENT Academic Honesty: When learners fail to complete their own work, they are cheating themselves out of their education and are committing plagiarism. Plagiarism, or failing to meet the academic honesty policy, will result in disciplinary actions by the institution. Plagiarism is dishonest behavior that will not be tolerated. A student will not receive credit if found to have plagiarized his/her work and may result in suspension or dismissal from the school. Follow the link for examples of plagiarism: http://examples.yourdictionary.com/examples/examples-of-plagiarism.html APA Format: All of your writing must be done following APA format. For more information regarding this format, go to Purdue Owl or follow this link:https://owl.english.purdue.edu/owl/resource/560/01/ Late work & Educational Responsibility: All assignments must be completed by the last day of the schedule unless an alternate due date has been previously approved by your instructor or documentation has been provided regarding extreme circumstances. It is the learner's responsibility to communicate with the instructor about extreme circumstances or ask questions concerning the assignment and their due dates. Threaded discussions: Students are to respond to the instructor’s weekly discussion post by Wednesday at 1159 PM (EST). The responses must be substantial (at least 125 words in length using correct grammar). These are intended to stimulate discussion and re-enforce course content. The student must also respond to two other student posts by Friday at 11:59 PM (EST). Please refer to the assignment calendar for assignment due dates. ASSESSMENT TESTING FOR NURSING PROGRAM REQUIREMENT: As part of certain nursing courses, students are required to take third-party computerized assessments, These assessments are intended to provide students with the tools they need to be successful in the Nursing program and on the NCLEX; as well as. Increase confidence and familiarity with computerized testing, The assessments typically include various types of formats, including multiple choice items, multiple response items, fill-in-the-blank items, dragand drop items, hot spots items, chart/exhibit items, and other items,. The assessments help identify deficit areas and provide students opportunities to practice and learn. Each assessment can represent up to the percent (10%) of a student’s course grade. Failure to achieve the minimum assessment score may result in a loss of points on an examination, or required remediation or retesting (as outlined in the course syllabus). Students who do not successfully complete the remediation or retest associated with an assessment examination (as outlined in the course syllabus) may receive an incomplete in a course and may be required to repeat the course in its entirety. An incomplete due to failure to successfully complete the assessment testing remediation or successfully retest is considered a failure for the course. Additional Resources Web sites 31 | P a g e NURSING DEPARTMENT Assessment Criteria and Methods of Evaluating Students 90 – 100% 80 – 89% 75 – 79% < 75% A B C F Do not count on a curve! Generally, the grades “A” through “C-” are considered passing grades. Grades "W" and "I" indicate that no grades were earned for the course. A "W" grade indicates that the student withdrew from the course. An "I" grade indicates that the student was passing the course, but failed to complete all the required course work. The instructor, in his/her discretion may grant an "I" grade instead of an "F", pending completion of the course work by the student within a specified time arranged by the instructor and told to the student. It is the student's responsibility to follow-up with the instructor to complete the course work. If the course work is not completed by the arranged time, the “I” grade becomes an “F". Distribution of Grade Elements Discussions 20% Assignments/Homework: (Case studies) 20% Midterm 20% Quizzes 20% Final 20% Total: 100 % Revised: March 13, 2015 32 | P a g e