chapter 15
advertisement

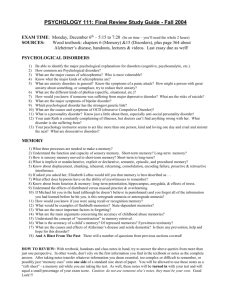
CHAPTER 15 Psychological Disorders CHAPTER OUTLINE I. INTRODUCTION Psychopathology, also called psychological disorder or mental disorder is generally defined as patterns of thought, emotion, and behavior that result in personal distress or a significant impairment in a person’s social or occupational functioning. A. II. In any given year in the U.S., about 30percent of adults and about 20percent of children display some form of mental disorder. About half of all Americans can expect to experience a disorder by age seventy-five. These rates are found, with only minor variations throughout the U.S. among males and females in all ethnic groups. B. The prevalence of disorders may be even higher. Studies have been limited in scope and count each case only once even though nearly half of people who are diagnosed with one disorder actually display comorbidity, meaning that they are diagnosed as having two or more disorders. DEFINING PSYCHOLOGICAL DISORDERS A. What is Abnormal? 1. Infrequency Whatever most people do is normal so statistical infrequency is unusual and abnormal. a) 2. It does not take into account that some rarely occurring behaviors are valuable and desirable. b) It equates normality with conformity, which can result in the oppression of those with minority views. c) It is difficult to decide how rare a behavior must be in order to be designated as abnormal. Norm Violation The norm violation criterion equates abnormality with violations of social norms or cultural rules. So, identifying psychopathology depends in part on how a society defines normal and abnormal. a) 3. Some norm violations are better characterized as eccentric or illegal rather than abnormal. b) Social norms vary across cultures, subcultures, and historical eras, so behaviors that qualify as abnormal in one part of the world would not be so in another. Personal Suffering Another approach is to use personal suffering as a criterion for abnormality. Experiencing distress is often taken into account when deciding whether psychological problems require treatment. However, it is an inadequate criterion for abnormality by itself. a) b) It does not take into account that some people may be distressed over behaviors that are not pathological (e.g., homosexuality). Some with disorders may show little distress because the disorder has impaired their ability to recognize how maladaptive their behavior is. B. Behavior in Context: A Practical Approach The practical approach combines aspects of all the criteria discussed. The content of behavior, what a person does. The sociocultural context in which the behavior occurs. The consequences of the behavior for the person and others. The practical approach pays attention to whether a person’s thoughts, behaviors, and emotions cause impaired functioning, difficulty in fulfilling appropriate and expected family, social, and work-related roles. It also takes into account a person’s age, gender, and culture, as well as the particular situation and historical era. III. EXPLAINING PSYCHOLOGICAL DISORDERS Supernatural explanations of psychological disorders are still invoked today by some in many cultures around the world, including certain ethnic and religious subcultures in North America. A. The Biopsychosocial Model Most researchers in Western cultures see psychopathology as caused by the combination and interaction of biological factors, psychological, and sociocultural factors, each of which contributes in varying degrees to particular problems in particular people. 1. Biological Factors Biological factors thought to be involved in causing mental disorders include physical illness, disruptions or imbalance in bodily processes, and genetic influences. a) 2. This medical model has a long history. (1) The ancient Greek physician Hippocrates suggested that psychological disorders resulted from imbalances among four humors or bodily fluids. (2) In ancient Chinese cultures, disorders were seen as resulting from an imbalance of yin and yang, the dual forces of the universe flowing in the physical body. (3) After the Middle Ages, as the medical model gained prominence specialized hospitals for the insane that used physical treatments were established throughout Europe. b) The medical model led to a view abnormality as mental illness that can be diagnosed, treated, and cured. It is now called the neurobiological model because it explains psychological disorders in terms of particular disturbances in the anatomy and chemistry of the brain and in other biological processes, including genetic influences. (1) The importance of biological factors in psychopathology has been demonstrated in many psychological disorders. (2) Dementia, is characterized by a losses and disturbances in memory, personality, and cognitive abilities. The most frequent causes are progressive deterioration of the brain. Alzheimer’s disease is one example. (3) Biological factors have also been implicated in schizophrenia, bipolar disorders, some forms of anxiety disorders, autism, and attention deficit disorder. Psychological Processes The psychological model sees mental disorders as arising from psychological factors, such as our wants, needs, emotions, learning experiences, attachment histories, and ways of looking at the world. a) 3. Greek literature and drama focused on a popular notion that the psyche, or mind, struggles to resolve inner conflicts or to overcome the effects of stressful events. b) In the late 1800s, Sigmund Freud’s psychodynamic approach challenged the medical model. He believed abnormal behavior was due to unresolved, mostly unconscious conflicts that began in childhood. (1) Modern psychodynamic theories, such as object relations theory, focus more on attachment and on early interpersonal relationships. c) Social-cognitive theorists see disorders as resulting from the interaction of past learning and current situations. Social-cognitive theorists also emphasize how learned expectancies, schemas, and other mental processes can influence the development of disorders. d) The humanistic approach suggests that disorders appear when a person’s tendency toward growth is blocked, usually by a failure to be aware of and to express true feelings. They also focus on the meanings people attach to events. Sociocultural Context The previous approaches focus primarily on processes within the individual. The sociocultural model of disorder emphasizes social and cultural factors. Gender, age, and marital status; the physical, social, and economic situations in which people live; and cultural values, traditions, and expectations are all factors that influence the sociocultural context of behavior. a) B. Some psychological disorders are culture-general—found in most cultures. For example, depression is found in almost all cultures. But even culture-general disorders have symptoms that vary from culture to culture. b) Some disorders are culture-specific—seen in only certain cultures. (1) Ataques de nervios occurs primarily in Puerto Rican and Dominican Hispanic women. It is a reaction to stress that includes heart palpitations, shaking, shouting, nervousness, depression, and sometimes fainting or seizures. (2) Koro occurs only in cultures with a supernatural explanation for disorder. It primarily occurs in men and centers around a fear that their penis will shrivel, retract into the body, and cause death. It is less common in women but then centers around the breasts. Diathesis-stress as an Integrative Explanation The diathesis-stress approach assumes that biological, psychological and sociocultural factors can predispose us toward disorder, but that it takes a certain amount of stress to actually trigger a disorder. Inherited characteristics, biological processes, and early learning experiences combine to create a predisposition or diathesis for a disorder. Whether the person actually develops the disorder depends on the nature and amount of stress the person encounters. 1. The more risk factors for a disorder a person has, whether in the form of genetic tendencies, personality traits, cultural traditions, or stressful life events, the more likely it is that the person will develop a disorder associated with those risk factors. IV. CLASSIFYING PSYCHOLOGICAL DISORDERS The main purpose of diagnosing psychological disorders is to determine the nature of people’s problems so that the most appropriate form of treatment can be chosen. It is also helpful for research on the causes of mental disorders. In the United States, mental health practitioners use the Diagnostic and Statistical Manual of Mental Disorder as the basis for diagnosis. The latest editions, DSM-IV and DSM-IV-TR, include more than 300 diagnostic labels. Outside the United States, mental health practitioners use the World Health Organizations’ International Classification of Diseases (ICD-10) and International Classification of Impairments, Disabilities and Handicaps (ICIDH-2). Efforts are underway to remove inconsistencies existing between these two systems. A. B. A Classification System: DSM-IV 1. DSM-IV provides specific criteria outlining the conditions that must be met before a person can be given that diagnostic label. There are five dimensions or axes for evaluation. a) Axis I contains major mental disorders. b) Axis II includes life-long conditions like personality disorders and mental retardation. c) Axis III records any medical conditions important in understanding the disorder. d) On Axis IV, psychosocial and environmental problems that are important for understanding a person’s psychological problems are noted. e) Axis V contains a rating from 100 down to one of the person’s current level of psychological, social, and occupational functioning. 2. DSM no longer contains the terms neurosis and psychosis. Neurosis refers to conditions in which anxiety is most characteristic; psychosis refers to conditions involving severe thought disorders that leave people out of touch with reality or unable to function on a daily basis. 3. Further changes have been proposed for DSM-V, a version currently under development. a) Because many disorders appear together, new “mixed” disorders or new subcategories may be introduced. b) Symptom dimensions or symptom clusters may be used rather than specific diagnostic categories. c) Some suggest basing diagnoses on brain imaging and genetic analyses. d) It has even been suggested that not only people’s problems but also their strengths be considered in diagnosis. Evaluating the Diagnostic System 1. Interrater reliability is the degree to which different clinicians give the same diagnostic label to the same person. Today, agreement is as high as 83 percent for major categories, but lower for other diagnoses. Reliability is higher with the use of structured diagnostic interviews. 2. Do diagnostic labels give accurate information that guides correct inferences about people? It is difficult to judge validity because there is no fully acceptable standard for accuracy. There is evidence supporting the validity of some DSM criteria, and as researchers learn more about various disorders validity should increase. 3. The current diagnostic system has been criticized on several grounds. a) A person’s problem may not fit neatly into one single category and comorbid disorders are common. b) The same symptoms may appear as part of more than one disorder. c) The strict boundaries of the criteria that must be met for diagnosis of a disorder do not take into account individual differences. d) Diagnostic judgments are, ultimately, subjective, and personal bias might creep into the labeling system. e) Thomas Szasz (say “zaws”) and other critics argue that DSM-IV and the medical model are dehumanizing, labeling people instead of describing problems. It ignores features that make each person’s case unique and may actually encourage C. the behaviors associated with the labels and undermine the confidence of clients about the chances of improvements. Thinking Critically: Is Psychological Diagnosis Biased? 1. What am I being asked to believe or accept? That clinicians base their diagnoses partly on the ethnic group to which their clients belong, and that there is bias in diagnosing African-Americans. 2. 3. 4. What evidence is available to support the assertion? African-Americans receive the diagnosis of schizophrenia more frequently than European-Americans do. African-Americans are overrepresented in public mental health hospitals (more severe problems) and underrepresented in private hospitals and outpatient clinics (less severe problems). African-Americans are also more likely to be discharged from mental hospitals without a definitive diagnosis and emergency room physicians are less likely to recognize psychological disorders in African American patients. Minority groups are underrepresented in research on mental disorders. Are there alternative ways of interpreting the evidence? Differences in diagnosis or treatment between ethnic groups do not automatically point to bias based on ethnicity. There may be real differences in psychological functioning associated with different ethnic groups. Poverty, not diagnostic bias, may be the reason African-Americans seek help more often at less expensive public hospitals rather than at more expensive private ones. There is no guarantee that diagnostic criteria would be different or that clinicians would be better at diagnosis if more minorities were included in research. What additional evidence would help to evaluate the alternatives? Experiments in which clinicians assigned labels to clients on the basis of case histories, test scores, and the like, had cases selected so that pairs of clients showed about the same objective amount of disorder, but one member of the pair was identified as European-American and the other as African-American. Results of such studies were mixed. Most found no bias, but the clinicians may have been aware of the purpose behind the studies. Studies conducted in hospital setting show that African-Americans are more frequently diagnosed with schizophrenia. However, a large-scale study of mental disorder found that when people were interviewed and diagnosed in their own homes, only a slightly higher number of African-Americans were diagnosed as suffering from schizophrenia. This shows bias. 5. What conclusions are most reasonable? There is evidence for ethnic bias, at least for some diagnoses. DSM is imperfect, as are the people who use it. Reducing bias may require more than detecting and eliminating deliberate discrimination. It may also involve research into cognitive errors biases that affect thinking and decision making and that may affect clinical judgments. In addition, all need to understand the sociocultural influences on the concepts of normal and abnormal. The best way to counteract clinician’s cognitive shortcomings is to teach them to base their diagnoses solely on published diagnostic criteria, standardized interview formats, and statistically validated decision rules rather than relying on their potentially biased clinical impressions. CAUTION: Beware of medical student’s disease, which occurs when students worry that their behavior signals some type of disorder after reading about that disorder. V. ANXIETY DISORDERS “Normal” anxiety involves brief episodes of moderate anxiety and is a normal part of modern life for most people. Anxiety disorders involve anxiety that is so intense and longlasting that it disrupts daily life. Anxiety disorders are the most common disorders in North America. A. Types of Anxiety Disorders Posttraumatic stress disorder is described in the chapter on health, stress, and coping. Four others are discussed below. 1. Phobia A phobia is an intense, irrational fear of an object or situation that is not likely to be dangerous. Most people realize their fears make no sense but cannot keep them from interfering with daily life. a) 2. 3. Specific phobias involve fear of specific situations or stimuli. They are the most prevalent of the anxiety disorders. b) Social phobias involve anxiety about being criticized by others or acting in a way that is embarrassing or humiliating. Very common is fear of public speaking. (1) When social phobia involves virtually all social situations in a person’s life, it is referred to as generalized social phobia. (2) Sociocultural factors can alter the form of social phobias. In Japan, a common social phobia is Tai-jin Kyofu Sho, a fear of embarrassing those around you. c) Agoraphobia, a rarer phobia, is a strong fear of being away from a safe place like home or from a safe person, such as a spouse, or of being trapped in a place from which escape might be difficult or where help may be unavailable. These fears can cause serious disruption. (1) Many with agoraphobia have a history of panic attacks (see below). (2) It is most often seen in women in Western culture. In other cultures such as in India (where being a housebound woman is not considered unusual), those diagnosed as agoraphobic tend to be men. . Generalized Anxiety Disorder Generalized anxiety disorder (GAD) involves excessive and long lasting and that is not focused on any particular object or situation, called free-floating anxiety. Symptoms include anxiety, worry, irritability, fatigue, and inability to concentrate. It appears later in life than other anxiety disorders and is more common in women, often accompanying other problems such as depression or substance abuse. Panic Disorder Panic Disorder is characterized by terrifying panic attacks that come without warning or obvious cause and are marked by intense heart palpitations, dizziness, chest pain or pressure, sweating, and faintness. Victims often believe that they are having a heart attack. They worry constantly about suffering future panic episodes and may start to curtail outside activities to avoid possible embarrassment. a) b) 4. One-third of people with panic disorder also suffer from agoraphobia. As many as 30 percent of the U.S. population experience at least one panic attack within a year, but only 2 to 3 percent develop panic disorder in any given year. Obsessive-Compulsive Disorder Obsessive-compulsive disorder (OCD) is characterized by persistent, upsetting and unwanted thoughts, obsessions, which often resolve around the possibility of infection, contamination, or doing harm to oneself or others. The obsessions may motivate ritualistic, repetitive behaviors, compulsions, done to try to avoid some dreaded outcome or to reduce fears associated with obsessions. The thoughts and compulsions are intense, disturbing and often strange intrusions that can severely impair daily activities. Many with the disorder recognize that their thoughts and actions are irrational. B. Causes of Anxiety Disorders 1. Biological Factors Most anxiety disorders appear to run in families. This may be partly due to similar environmental factors, but it also suggests that people may inherit a predisposition to develop anxiety disorders. a) 2. Some evidence suggests that specific genetic factors may lead to specific anxiety disorders. b) People with anxiety disorders may have autonomic systems that are oversensitive to stress, predisposing them to react with intense anxiety to a range of situations. c) Predisposition to anxiety disorders may be based on abnormalities in neurotransmitter systems. Excessive norepinephrine activity has been linked to panic disorder and dysregulation of serotonin has been linked to OCD. Psychological Factors Most researchers agree that environmental stressors, dysfunctional beliefs, cognitive distortions, and learning are crucial to the development of most anxiety disorders. a) C. Persons with anxiety disorders often exaggerate the dangers in their environment, creating unrealistic expectations that bad events are going to happen. They also tend to underestimate their capacity for dealing with threatening events, resulting in anxiety and desperation when feared events do occur. Linkages: Anxiety Disorders and Learning 1. Learning principles may explain some anxiety disorders. a) In OCD, compulsive behavior relieves anxiety, so it is strengthened by negative reinforcement.However, such actions do not relieve the obsessive thoughts, which later cause anxiety to return and continue the vicious cycle. OCD might be a pattern that is sparked by distressing thoughts and maintained by operant conditioning. b) Phobias may be based on principles of classical conditioning and observational learning. Once a phobia is learned, one may avoid the feared object, preventing discovery that there is no need to be afraid. (1) The feared object (previously a neutral stimulus) becomes an aversive conditioned stimulus after being associated with a traumatic event (unconditioned stimulus). For example, someone fears red cars after being in an accident. (2) Fears can also be learned by seeing or hearing about other’s bad experiences. They can be learned from watching TV or movies. c) People may be biologically prepared to learn to fear and to avoid stimuli that had the potential to harm their evolutionary ancestors. Research has shown that a research-induced fear of such objects and situations (e.g., snakes) are maintained longer after the laboratory experience than fear of other objects such as faces or houses. d) The learning that supports the development of anxiety disorders occurs more quickly among those who are biologically and psychologically prepared for it. VI. SOMATOFORM DISORDERS Somatoform disorders are psychological problems that take somatic (physical) forms. A. Conversion disorder is a condition in which the person appears to be, but is not, blind, deaf, paralyzed, or insensitive to pain in parts of the body. An earlier term for this disorder was hysteria. 1. This is a rare disorder that usually appears in adolescence or early adulthood. 2. Conversion disorders differ from true physical disabilities in the following ways: a) They appear when a person is under severe stress. b) They often help reduce that stress by enabling the person to avoid unpleasant or threatening situations. c) The person shows remarkably little concern about what is apparently a serious problem. d) The symptoms may be neurologically impossible or improbable. 3. People can only be diagnosed with conversion disorder if they are not faking or malingering. 4. The conversion process does not destroy visual or auditory ability but may prevent the person from being aware of information that his/her brain is still processing. B. Hypochondriasis is a strong unjustified fear that one has, or might get, cancer, heart disease, AIDS, or other serious physical problems. The fear prompts numerous doctor visits, reports of numerous symptoms, and becoming “expert” on the most feared diseases. 1. Whereas those with anxiety disorders may have an irrational fear of getting a disease, those with hypochondriasis fear that they already have the disease. C. Somatization disorder is characterized by dramatic but vague reports about a multitude of physical problems rather than any specific illness. D. Pain disorder involves complaints of severe, often constant pain (typically in the neck, chest, or back) with no physical cause. E. Causal explanations 1. Some cases of somatoform disorders may be related to childhood experiences in which a person learns that symptoms of physical illness bring special attention. 2. Other cases may be triggered by severe stressors. 3. Diathesis-stress may be the best approach. Certain people may have biological and psychological traits that make them especially vulnerable to somatoform disorder, especially when combined with a history of physical illness. These traits are oversensitivity to physical sensations and self-consciousness. 4. Sociocultural factors may also be important. In some cultures people channel psychological conflicts into physical symptoms rather than into anxiety or depression. VII. DISSOCIATIVE DISORDERS Dissociative disorders are intense, longlasting disruptions in a person’s memory, consciousness, or identity. These disorders are rare. A. B. C. D. Dissociative fugue is characterized by a sudden loss of personal memory and the assumption of a new identity in a new locale. Dissociative amnesia involves sudden memory loss but the person does not leave home or create a new identity. Dissociative identity disorder (DID), formerly known as multiple personality disorder, is a condition in which a person appears to have more than one identity, each of which speaks, acts, and writes in a very different way. Each personality seems to have its own memories, wishes, and (often conflicting) impulses. It is a controversial diagnosis. Causal explanations 1. Psychodynamic theorists see the cause as massive repression of unwanted impulses or memories, resulting in a “new person” who acts out these impulses. 2. Social-cognitive theorists focus on the fact that everyone is capable of behaving differently depending on the circumstances, and in rare cases this variation can become so extreme that a person feels and is perceived by others as a “different person.” An individual may be rewarded for a sudden memory loss or unusual behavior by escaping stressful situations. 3. The increase in the number of cases of cases of DID may have occurred because clinicians were looking for them and because conditions leading to it became more prevalent, but it may also have been triggered by the media, increasing the status of the disorder as an approved method of expressing distress. 4. Multiple personality disorder was changed to dissociative identity disorder in the DSM-IV to downplay the notion of multiple personalities that can be easily contacted. The new name suggests a dissociation between one’s memories and other aspects of identity that can be so dramatic that people experiencing it may come to believe that they have more than one personality. 5. So far, research supports four conclusions: a) Memory loss and other forms of dissociations are genuine phenomena. b) Many people experiencing DID have experienced events that they would like to forget or avoid. The majority have suffered severe, unavoidable, persistent abuse in childhood. c) Most with DID appear to be skilled at self-hypnosis, through which they can induce a trance-like state. d) Most with DID found they could escape the trauma of abuse temporarily by creating “new personalities” to deal with the stress. VIII. MOOD DISORDERS A mood disorder, or affective disorder, is diagnosed when people experience extremes of moods for long periods of time, when they shift from one extreme to another, and/or when their moods are not consistent with the events around them. A. Depressive Disorders 1. A person suffering major depressive disorder (MDD) feels sad and overwhelmed, typically losing interest in activities and relationships and taking pleasure in nothing. Other symptoms include changes in eating habits resulting in weight changes, sleep disturbances, and problems in working, concentrating, making decisions, and thinking. Exaggerated feelings of worthlessness, hopelessness, or guilt are common. a) Often there are also symptoms of an accompanying anxiety disorder. b) Delusions are false beliefs that may be present in severe cases. c) MDD may come on suddenly or gradually. It commonly consists of recurring episodes that can last for weeks or months. 2. Dysthymic disorder is a less severe pattern of depression. The person shows sad mood, lack of interest, and loss of pleasure less intensely and for a longer duration (at least two years). Mental and behavioral disruptions are also less severe. 3. Major depressive disorder occurs sometime in the lives of up to 17 percent of the North American and European populations. It is most likely to occur during two time periods: during late adolescence or young adulthood and during old age. a) In Western cultures, women are two to three times more likely than men to experience MDD. Worldwide, however, it varies across cultures. b) MDD is often comorbid with other psychological disorders and medical conditions. It is especially likely to be diagnosed along with anxiety disorders, substance use disorders, physical disabilities, and recovery from heart attack. B. Suicide and Depression Some form of depression has been implicated in 40 to 60% of suicides. Thinking about suicide is a symptom of MDD. Other symptoms, such as hopelessness about the future and a desire to seek instant escape from problems, are also related to suicide attempts. 1. C. About 31,000 people in the U.S. commit suicide each year. Suicide rates differ crossculturally. They are lower in countries with stronger religious prohibitions against suicide. a) Suicide rates also differ across age, gender and ethnicity. (1) In the U.S. suicide is most common among people over 65 years of age. However, among those fifteen to twenty-four-years-old, the suicide rate has tripled in the last fifty years. It is now the thirdt leading cause of death among adolescents and young adults. (a) Suicide is the second leading cause of death among college students. (2) Women attempt suicide three times as often as men, but men are four times as likely to actually kill themselves. (3) In the U.S., suicide rates vary with ethnicity. Among males. the rates are about 20 percent for American Indians and European-Americans and about 10% for Asian-Americans, Hispanic-Americans, and African-Americans. The pattern is the same for women thought the rates are lower. 2. Predicting suicide is difficult because suicidal thoughts are much more common than attempts. Research has provided some predictive guidelines: a) In the U.S., suicide is most likely among EuropeanAmerican males, especially those over forty-five-years-old, single or divorced, and living alone. b) The risk of suicide is greater among those diagnosed with a mood or anxiety disorder or schizophrenia. In the elderly, it is more common in males who suffer depression over health problems. c) In general, the risk of suicide is greater in people who have made a specific plan, have given away their belongings, and are impulsive. d) A previous attempt is not always a good predictor of future suicide. Such attempts may have been help-seeking behaviors not failed attempts to die. Most people who commit suicide have made no prior attempts. e) People who talk about suicide are more likely to try it. About 80percent of suicides are preceded by some kind of warning. Bipolar Disorders Bipolar disorders consist of alternating experiences of depression and mania. Bipolar disorders are often comorbid with anxiety disorders. 1. D. Mania is a very agitated, usually elated, emotional state characterized by optimism, boundless energy, and certainty of having extraordinary powers, abilities, and ideas. It can include irritability and impulsivity. 2. In Bipolar I disorder, also called manic depression, intense episodes of mania alternate with episodes of deep depression. Periods of relatively normal moods can separate the episodes. a) This is a rare disorder occurring in only about 1percent of adults; affecting men and women equally. 3. Bipolar II disorder is more rare and features major depressive episodes alternating with episodes known as hypomania, which are less severe than the manic phases in bipolar I disorder. 4. Cyclothymic disorder is a pattern of less extreme manic and depressive moods than in bipolar I disorder. Causes of Mood Disorders 1. 2. Biological Factors a) Genetics influences tend to be stronger for mood disorders, especially for bipolar I disorder, than for most other disorders. Researchers are working to identify regions on various chromosomes related to genetic vulnerability for these disorders. Some interest has centered on particular genes on chromosome 13 b) Other contributing biological factors that may also be genetically influenced include (1) Malfunctions of brain regions, including the prefrontal cortex, hippocampus, amygdale, and other parts of the limbic system. c) The neurotransmitters norepinephrine, serotonin, and dopamine are important. Many drugs that relieve depression seem to work by altering these systems. It may be that mood disorders result in part from changes in the sensitivity of the neuronal receptors where these chemicals have their effects in the brain. d) Mood disorders have also been connected to malfunctions of the endocrine system, especially the HPA system which is involved in the body’s responses to stress. As many as 70 percent of depressed people secrete abnormally high levels of the stress hormone cortisol. e) Disturbances in basic biological rhythms, or the body’s biological clock, might also play a role. (1) Seasonal affective disorder (SAD) appears to be caused by disruptions in circadian rhythms during shorter daylight months. (2) Disruptions in biological rhythms are also suggested by the fact that many depressed people have trouble sleeping. Resetting the biological clock through sleep deprivation or light stimulation has relieved depression in some cases. Psychological and Social Factors a) Biopsychosocial explanations of mood disorders also emphasize the impact of anxiety, negative thinking, personality traits, family interactions, and other psychological and emotional responses triggered by trauma, losses, and other stressful events. The higher prevalence of depression among females has been attributed to their greater exposure to stressors. b) Social-cognitive theories suggest that the way people think about their stressors can increase or decrease the likelihood of mood disorders. (1) Learned helplessness, the perception of a lack of control over one’s life, especially over its stressors, may be an important factor in depression. (2) Also important are how people think about events in their lives. Aaron Beck’s cognitive theory of depression suggests that depressed people develop mental habits of: (a) blaming themselves when things go wrong, (b) focusing on and exaggerating the negative side of events, and (c) jumping to overly generalized, pessimistic conclusions. (3) Negative ways of thinking may be acquired through maladaptive experiences in childhood. Children whose relationships with their caregivers were characterized by deprivation and abuse are more prone to depression in later life. (4) Long-lasting depression is more likely among people who have negative attributional styles. They attribute negative events to their own characteristics and believe they will never be capable of doing better. (5) Depressed people do hold more negative beliefs about themselves and their lives, and such pessimistic beliefs may be a risk factor for depression, not just a result of being depressed. (6) Women tend to have a ruminative style, focusing on negative events, on why they occur, and on feeling depressed, which is likely to continue or worsen depression. Men tend to have a distracting style, engaging in a distracting activity that helps bring them out of their depressed mood. 3. The diathesis-stress model is consistent with the social-cognitive approach. Certain cognitive styles constitute a predisposition (or diathesis) that makes a person vulnerable to depression, the occurrence of which is made more likely by stressors. There may be several types of depression and each may be caused by different combinations of biological and environmental factors. IX. SCHIZOPHRENIA A. Definition and Statistics 1. Schizophrenia is a pattern of severely disturbed thinking, emotion, perception, and behavior that severely impairs the ability to communicate and relate to others and disrupts most aspects of daily functioning. It is the most severe and disabling of all mental disorders. 2. It occurs in 1 to 2 percent of the population. In the U.S., it occurs equally in various ethnic groups but tends to be diagnosed more frequently in economically disadvantaged populations. It occurs equally among men and women, but in women it may appear later in life, be less severe, and respond better to treatment. 3. Schizophrenia tends to develop in adolescence or early adulthood. About 40percent of people with schizophrenia improve with treatment and are able to function reasonably well. It is estimated that 10 to 13 percent of homeless individuals suffer from schizophrenia. 4. The better a person’s premorbid adjustment, the level of functioning before schizophrenic symptoms begin, the better the chance for improvement. B. Symptoms of Schizophrenia Eugene Bleuler (say “bloy-ler”) coined the word schizophrenia, or “split mind,” to refer to the splitting of normally integrated mental processes, such as thoughts and feelings. Schizophrenia DOES NOT mean split personality as in dissociative identity disorder. 1. 2. Thought and language are often disorganized. a) Neologisms are “new words” that have meaning only to the person speaking them. b) Loose association is the tendency for one thought to be logically unconnected, or only superficially connected to the next. c) Clang associations are based on double meanings or on the way a word sounds. d) In severe cases, a word salad, a jumble of words reflects utterly chaotic thoughts. Content of thinking is also disturbed. It often includes deeply-entrenched delusions, false beliefs that are resistant to change. These generally fall into three categories. a) Delusions of influence focus on the belief that one’s body, thinking, or behavior is being controlled by external forces. (1) In delusions of control, something or someone is threatening to control the person in some way,for example, implanting devices in his or her brain. (2) Thought insertion is the belief that other people’s thoughts are appearing in one’s own mind. (3) Thought broadcasting is the belief that thoughts can be broadcast to others. b) Self-significant delusions involve exaggerated beliefs about oneself. These may involve beliefs that TV signals are sending special coded messages relevant only to the person, the person may have delusions of grandeur, believing he or she is an emperor or god, or the person may believe that he or she is guilty of terrible sins. c) C. D. Delusions of persecution involve beliefs that others are out to harass or harm the person. 3. Attention and perception may be affected. People with schizophrenia typically display an inability to focus attention or concentrate. They may feel overwhelmed as they try to attend to everything at once. Perceptually they feel detached from the real world. a) Hallucinations, or false perceptions, usually of voices, are common. Hallucinations can create sights, smells, tastes, and touches even when no external stimuli are present. The brain areas activated during hallucinations are related to those that respond to real sights and sounds. 4. Emotional expressiveness is often muted, but when emotion is shown it is frequently exaggerated or inappropriate. 5. Some people with schizophrenia are very agitated with lots of movement, while others move very little or hold postures for hours. 6. Other common symptoms include lack of motivation, poor social skills, deteriorating personal hygiene, and an inability to function on a daily basis. Categorizing Schizophrenia 1. DSM-IV lists five major subtypes of schizophrenia: paranoid, disorganized, catatonic, undifferentiated, and residual. These subtypes convey some useful information but do not always provide accurate information about patients’ behavior because some symptoms appear in more than one subtype. In addition, they may not be linked very closely to the various biological conditions thought to underlie schizophrenia. 2. Many researchers now focus more precisely on the kinds of symptoms that patients display. a) One method highlights the positive or negative aspects of the symptoms. Patients may exhibit both, but one or the other may predominate. (1) Disorganized thoughts, delusions, and hallucinations may be called positive symptoms because they are undesirable additions to a person’s mental life. If severe, these are associated with long-term disability. (2) The absence of pleasure and motivation, lack of emotional reactivity, social withdrawal, reduced speech and other deficits are negative symptoms, because they subtract elements from normal mental life. When negative symptoms predominate, schizophrenia generally is more severe and less responsive to treatment. 3. Another method involves categorizing schizophrenic symptoms into: psychotic (hallucinations or delusions), disorganized (incoherent speech, chaotic behavior, inappropriate affect or emotion) or negative (e.g., lack of speech or motivation). Some researchers believe that these reflect three separate dimensions of schizophrenia, traceable to different causes. For this reason, schizophrenia is often called the schizophrenia spectrum implying different clusters requiring different treatments. Causes of Schizophrenia 1. Biological Factors a) Schizophrenia runs in families. 40 percent of the time if one identical twin displays schizophrenia, the other twin will too. It is unlikely that a single gene transmits the disorder. A predisposition toward schizophrenia that involves many genes may be what is inherited. b) Impairments in information processing and other cognitive abilities are related to structural abnormalities. Brain abnormalities in schizophrenia include less tissue in the thalamic regions, prefrontal cortex, and some subcortical areas. This shrinkage results in enlargement in fluid-filled spaces called ventricles. Enlarged ventricles and reduced cortex in the frontal lobes may be associated with negative 2. 3. symptoms. Patients with mainly positive symptoms tend to have normal-looking brains. c) Neurotransmitters, especially dopamine, may play a role in causing or intensifying schizophrenic symptoms. Schizophrenia may involve changes in the ratio of dopamine to other neurotransmitters. d) Neurodevelopmental abnormalities may play a role. Disruption of brain development from before birth through childhood may later lead to schizophrenia. Parental age and prenatal exposure to drugs, physical trauma, or viral infections have been associated with schizophrenia. Low birth weight, oxygen deprivation and childhood malnutrition can also be stress factors that may combine with genetic predispositions to bring on the disorder. Psychological and Social Factors a) Maladaptive learning experiences, dysfunctional cognitive habits, and stressful family communication patterns can contribute to the appearance of schizophrenia and influence its course. (1) More severe symptoms and more relapses are seen in people whose relatives exhibit expressed emotion. They are critical, unsupportive, or emotionally over-involved. Vulnerability Theory The diathesis-stress approach is embodied in the vulnerability theory which suggests that: a) b) c) X. vulnerability to schizophrenia is mainly biological; different people have differing degrees of vulnerability; vulnerability is influenced partly by genetic influences on development and partly from neurodevelopmental abnormalities associated with environmental risk factors; and d) psychological components, such as exposure to poor parenting or inadequate coping skills, may help determine whether schizophrenia actually appears and may also influence the course of the disease. 4. Schizophrenia is a highly complex disorder, probably more than one disorder, whose origins lie in many biological, psychological, and social domains, some of which are yet to be discovered. PERSONALITY DISORDERS Personality disorders are long-standing, inflexible ways of behaving that are not so much severe mental disorders as dysfunctional styles of living. From childhood or adolescence on, they affect all areas of functioning and create problems for those who display them and for others. There are ten personality disorders grouped into three clusters listed on Axis II of DSM-IV. A. B. The odd-eccentric cluster (cluster A) includes paranoid, schizoid, and schizotypal personality disorders. 1. In schizotypal personality disorder the person displays some of the peculiarities seen in schizophrenia but is not disturbed enough to be diagnosed with schizophrenia. 2. From table 15.5: a) The paranoid personality is unusually suspicious and distrustful of others. b) The schizoid personality is unusually detached from social relationships. The dramatic-erratic cluster (cluster B) includes the borderline, histrionic, narcissistic, borderline, and antisocial personality disorders. 1. Narcissistic personality disorder is characterized by an exaggerated sense of selfimportance and extreme sensitivity to criticism. People with this disorder feel entitled to special treatment by others but are markedly lacking in empathy for others. 2. From table 15.5 a) C. D. E. The borderline personality lack stability in relationships and self-image. People with this disorder can be impulsive, angry, and suicidal. b) The histrionic personality shows excessive emotionality yet is emotionally shallow, is overly dramatic, and is obsessed with being the center of attention 3. Antisocial personality disorder is described in some depth below. The anxious-fearful cluster (cluster C) includes dependent, obsessive-compulsive, and avoidant personality disorders. 1. Avoidant personality disorder is similar to social phobia in that the person wants to be with others but is too inhibited because of a long-standing pattern of avoiding social situations and of being particularly sensitive to criticism or rejection by others. 2. From table 15.5 a) The dependent personality is helpless, with an excessive need to be taken care of by others. b) The obsessive-compulsive personality is preoccupied with orderliness, perfection, and control. The diagnosis of personality disorders is controversial. There is much overlap among personality disorder symptoms making diagnosis difficult. Social and moral factors can be at work in diagnoses and evidence of gender bias has been found in some diagnoses. Antisocial Personality Disorder The most serious, costly and studied is antisocial personality disorder (APD). The terms moral insanity, psychopath, and sociopath were previously used when referring to this disorder. Approximately 3percent of men and 1percent of women in the U.S. fall into this category. 1. Symptoms APD is marked by a long-term pattern of irresponsible, impulsive, unscrupulous behavior, beginning in childhood or early adolescence. People with APD are “fast talkers,” charming, and intelligent and can con people into doing things for them. The lack of remorse, anxiety, or guilt is the key symptom. People with APD tend to become less active and dangerous after the age of forty. a) F. Terrorists or suicide bombers may or may not have this disorder. Acts of terrorism, in general, are better explained by social and political psychology. 2. Causes a) The earlier the development of the disorder, the stronger the genetic component. b) Genes may influence brain development or chronic underarousal of both the autonomic and central nervous systems. This underarousal would make people less sensitive to punishment. c) Other evidence suggests information-processing defects. d) Suggested psychological and social factors contributing to the development of APD include broken homes, rejection by parents, poor discipline, lack of good parental models, lack of attachment to early caregivers, impulsivity, conflictfilled childhoods, and poverty. e) The biopsychosocial model suggests that antisocial personality disorder results when psychosocial and environmental conditions interact with genetic predispositions to low arousal and the sensation seeking and impulsivity associated with it. f) Identification of APD before the development of the more treatment-resistant traits, may offer the best hope for dealing with this disorder. Focus on Research Methods: Exploring Links Between Child Abuse and Antisocial Personality Disorder 1. What was the researcher’s question? Can childhood abuse cause antisocial personality disorder? The researcher used a prospective research design, first finding cases of childhood abuse and then looking for the effects of that abuse on adult behavior. 2. How did the researcher answer the question? Cathy Widom identified 416 adults whose backgrounds included official records of having been physically or sexually abused before age eleven. She explored these people’s lives, in police and school records, as well as in a two-hour diagnostic interview. To avoid bias and distortion, both the interviewers and the people interviewed were unaware of the purpose of the study. Widom also selected a comparison group of 283 people who had not been abused, but were similar to the abused sample in terms of age, gender, ethnicity, hospital of birth, schools attended, and areas of residence and were exposed to similar environmental and socioeconomic risk factors as the abused children. 3. What did the researcher find? She found that people in the abused group were significantly more likely to commit crimes as juveniles and adults than those in the nonabused group. The correlations between criminality and abuse were stronger for males than females and for African Americans than for European Americans. Victims of physical abuse were more likely to commit violent crimes as adults than were victims of sexual abuse. Those in the abused group exhibited nearly double the rate of antisocial personality disorder than did the comparison group. The role of abuse in antisocial personality disorder was higher for men. Failure to graduate from high school was also strongly associated with the appearance of antisocial personality, whether or not childhood abuse had occurred. 4. What do the results mean? Widom found a correlation between childhood abuse and criminality, violence, and antisocial personality disorder. Although, causality could not be firmly established, the results suggest that childhood abuse may be an important causal factor. 5. What do we still need to know? Further research is needed to discover whether antisocial personality disorder stems from abuse itself or from one or more of the known or unknown factors accompanying it, such as not completing high school, exposure to poverty, dysfunctional parenting, social rejection, etc. Childhood abuse might create general vulnerability for a variety of psychological disorders, but factors that promote the development of a particular disorder are not yet understood. Since such a small percentage of abused children displayed violence, criminal behavior and antisocial personality, research needs to focus on the genetic features or environmental experiences that protect children from at least some of the negative consequences of abuse. XI. A SAMPLING OF OTHER DISORDERS Other psychological disorders covered in other parts of the text include mental retardation, sexual dysfunctions, posttraumatic stress disorder, and sleep disorders. Still others include: A. Psychological Disorders of Childhood Because children’s development is still incomplete and their ability to cope with stress is limited, children are vulnerable to special types of disorders. These disorders often do not simply go away after childhood. They disrupt development and associated problems often continue into adulthood. 1. B. The externalizing, or undercontrolled category of disorders includes behaviors that are disturbing to those in the child’s environment. a) Conduct disorders appears around 11 or 12-years-old, mostly in boys. These disorders involve aggression, disobedience, destructiveness, and other problematic behavior that may signal the development of antisocial personality disorder. (1) There may be a genetic predisposition for conduct disorders. These children may also have high activity levels. Environmental and parenting factors interacting with genetic factors shape children’s behaviors. b) In attention deficit hyperactivity disorder (ADHD), children (primarily boys) are impulsive and cannot concentrate on an activity as well as others their age. (1) The DSM-IV lists three subtypes: (1) primarily inattentive, (2) primarily impulsive, and (3) combined inattentive and impulsive. (2) Many are hyperactive, having great difficulty sitting still or controlling their physical activity. Their impulsiveness and lack of control leads to impairments in learning and social skills. (3) ADHD is increasingly being viewed as a neurological condition rather than just bad behavior. (a) Causes may include genes that regulate dopamine, brain damage, lead or household chemical poisoning, and low birth weight. (b) In some cases, parenting may increase the risk for ADHD. (4) Because hyperactivity is a judgment call, cultural standards may influence what is acceptable and what is called abnormal. 2. The internalizing, or overcontrolled, category of disorders includes distress, especially depression, anxiety, and social withdrawal. a) In separation anxiety disorder, a child constantly worries about being lost, kidnapped, or injured or that a parent will be harmed. Refusal to go to school, school phobia, is often the result. (1) Shy children are at higher risk, but rejection by peers may also be a factor. 3. Pervasive Developmental Disorders, also known as autistic spectrum disorders, do not fall into either category. Children in this category show severe deficits in communication, impaired social relationships, and often, repetitive stereotyped behaviors and unusual preoccupations and interests. a) About half suffer autistic disorder. Autism is usually evident within thirty months after birth, as these babies show no sign of attachment to anyone. Half never learn to speak. b) A less severe form of autism is called Asperger’s disorder. Though they have impaired relationships, repetitive behaviors and strange obsessions, these children show few cognitive deficits, and are able to function adaptively and sometimes independently as adults. c) Possible biological roots of autistic disorder include genetic factors or neurodevelopmental abnormalities affecting language and communication. Recent research has focused on “mirror neurons” that allow us to have an idea of how other’s minds operates. There is no evidence that autistic disorder is caused by cold and unresponsive parents. Substance-Related Disorders 1. 2. Childhood disorders, especially externalizing disorders, often lead to substance-related disorders in adolescence and adulthood. DSM-IV defines these disorders as the use of psychoactive drugs for months or years in ways that harm the user or others. a) Addiction is a physical need for a substance. DSM-IV calls this physiological dependence. (1) Addiction is often evident when tolerance occurs, when one needs more and more of a drug to achieve the same desired state. (2) Withdrawal symptoms occur when the addicted person stops using the drug, forcing the body to readjust to a substance-free state. b) People can become psychologically dependent, or experience behavioral dependence, on psychoactive substances. In such cases, a drug has become the primary source of reward and lives revolve around getting and using it. c) Substance abuse is defined by DSM-IV as a pattern of drug use that creates significant social, legal, or interpersonal problems. Alcohol Use Disorders Alcohol dependence or alcohol abuse is a pattern of continuous or intermittent drinking that may lead to addiction and almost always causes severe social, physical, and other problems. Men outnumber women three to one, although the female and adolescent rate of alcoholism is rising. a) 3. Prolonged overuse of alcohol can result in life-threatening liver damage, reduced cognitive abilities, vitamin deficiencies that can lead to an irreversible brain disorder called Korsakoff’s psychosis (severe memory loss), and many other physical ailments. b) Alcoholism has been implicated in half of all the traffic fatalities, homicides, and suicides that occur each year. It also figures prominently in rape, child abuse, elevated rates of hospitalization, and absenteeism from work. Children who grow up in families in which at least one parent abuses alcohol are at increased risk for developing a host of mental disorders, including substance-related disorders. Children of mothers who abused alcohol during pregnancy may be born with fetal alcohol syndrome. c) The biopsychosocial model suggests that alcohol use disorders stem from a combination of genetic characteristics (including inherited aspects of temperament such as impulsivity and emotionality) and what people learn in their social and cultural environment. (1) Alcoholism may be due in part to an inherited predisposition of some kind. Children of alcoholics are more likely than others to become alcoholics themselves, and identical twins reared apart are both at increased risk for alcoholism. (2) Expectations such as that alcohol will make a person feel good and help him or her cope with stressors play an important role in the development of these disorders. (3) Alcoholism is more common in some ethnic and cultural groups where frequent drinking tends to be socially reinforced than in groups in which all but moderate drinking tends to be discouraged. However, differing expressions of social support for drinking can result in differing consumption patterns within a cultural group. Heroin and Cocaine Dependence Heroin and cocaine addicts suffer many serious health problems, because of the drug itself and the poor health habits it engenders. The danger of death from an overdose, contaminated drugs, AIDS, or suicide is always present. Drug dependence tends to be more prevalent among males, especially young males. a) Continued use or overdoses of cocaine can cause problems ranging from nausea and hyperactivity to paranoid thinking, sudden depressive “crashes,” and even death. (1) Pregnant women using cocaine are more likely to lose their babies through spontaneous abortions, placental detachments, early fetal death, or stillbirths. b) Addiction to heroin and cocaine is largely due to the physiological effects of the drugs. Research has not shown why drug use is a problem for some people but not for others. It is likely due to some biological predisposition that interacts with specific psychological processes and stressors in specific social and cultural contexts. XII. MENTAL ILLNESS AND THE LAW A. U.S. laws and rules protect people with severe psychological disorders two ways. 1. People judged to be mentally ill may be protected from prosecution. If, at the time of their trial, individuals cannot understand charges against them or assist in their own defense, they are declared mentally incompetent to stand trial. They are sent to a mental institution until judged to be competent. In most cases, people who are still not competent after about two years, may be committed to a mental institution or released. Release is rare because competency to stand trial requires only minimal mental abilities and if drugs can provide temporary competence, the defendant will usually go to trial. 2. Mentally ill people may be protected from punishment. In most U.S. states, they can be found not guilty by reason of insanity, if at the time of a crime mental illness prevented them from meeting the cognitive criteria of the M’Naughton rule: (1) understanding what they were doing; (2) knowing that what they were doing was wrong; or (3) passing the irresistible impulse test: resisting the impulse to do wrong. a) About half the states use a rule proposed by the American Law Institute in 1962. “A person is not responsible for criminal conduct if at the time of such conduct as a result of mental disease or defect he lacks substantial capacity either to appreciate the criminality (wrongfulness) of his conduct or to conform his conduct to the requirements of law.” b) In federal cases, the Insanity Defense Reform Act of 1984 deleted the irresistibleimpulse criterion from the definition of insanity. Half the states have done the same. These laws highlight that insanity is a legal term, not a psychiatric diagnosis; it does not appear in DSM-IV. c) Defendants judged not guilty by reason of insanity and who still display mental illness are usually required to receive treatment until judged to be cured or no longer dangerous. B. Insanity rules have been criticized on many grounds: 1. Some critics argue that everyone should be held responsible for their actions. 2. There are significant problems in the implementation of insanity rules. For example, different experts may give conflicting testimony about a defendant’s sanity at the time of a crime. 3. Even severely impaired people are still capable of some rational decision making and of controlling some aspects of their behavior. C. Reforms include: 1. A small number of states have abolished the insanity defense. 2. D. E. A verdict of guilty but mentally ill exists in some states, in which defendants serve a sentence but are also supposed to receive treatment while confined (although they seldom do). 3. As noted before, the irresistible impulse criterion has been deleted from the definition of insanity in a number of federal and local courts. 4. In federal and some state courts, the defendant must prove insanity at the time of the crime rather than requiring the prosecution to prove that the defendant was sane. The insanity plea is used in fewer than one of every 200 felony cases in the U.S., usually when the defendant displays severe psychological disorder, and this plea is successful in only two of every 1,000 attempts. The few defendants found not guilty by reason of insanity are usually hospitalized for two to nine times as long as they would have spent in prison had they been convicted. Some of the same sociocultural values that shape people’s views about what constitutes abnormality also influence their judgments about the extent to which abnormality relieves people of criminal responsibility for their actions.