approved
advertisement

Ministry of Health of Ukraine
BUKOVINIAN STATE MEDICAL UNIVERSITY
“APPROVED”
on methodical meeting of the Department of
Anatomy, Topographical anatomy and Operative
Surgery
“………”…………………….2008 р. (Protocol №……….)
The chief of department
professor ……………………….……Yu.T.Achtemiichuk
“………”…………………….2008 р.
METHODICAL GUIDELINES
for the 2nd-year foreign students of English-spoken groups of the Medical Faculty
(speciality “General medicine”)
for independent work during the preparation to practical studies
THE THEME OF STUDIES
“Topographical anatomy of the anterolateral abdominal wall.
The methods of laparotomy”
MODULE I
Topographical Anatomy and Operative Surgery
of the Head, Neck, Thorax and Abdomen
Semantic module 3
“Topographical Anatomy and Operative Surgery of the Abdomen”
Chernivtsi – 2008
1. Actuality of theme:
The topographical anatomy and operative surgery of the abdomen are very
importance, because without the knowledge about peculiarities and variants of
structure, form, location and mutual location of abdominal anatomical structures,
their age-specific it is impossible to diagnose in a proper time and correctly and to
prescribe a necessary treatment to the patient. Surgeons usually pay much attention to
the topographo-anatomic basis of surgical operations on the abdomen.
2. Duration of studies: 2 working hours.
3. Objectives (concrete purposes):
To know the definition of regions of the abdomen.
To know classification of surgical operations on the abdomen.
To know the topographical anatomy and operative surgery of the organs of the
abdomenal cavity.
4. Basic knowledges, abilities, skills, that necessary for the study themes
(interdisciplinary integration):
The names of previous disciplines
1. Normal anatomy
2. Physiology
3. Biophysics
The got skills
To describe the structure and function of the
different organs of the human body, to determine
projectors and landmarks of the anatomical
structures. To understand the basic physical
principles of using medical equipment and
instruments.
5. Advices to the student.
5.1. Table of contents of the theme:
The Abdominal Wall
The abdominal wall extends from the osteocartilaginous thoracic cage to the pelvis. Its
major part is muscular.
Subdivisions of the Abdominal Wall. Although the abdominal wall is continuous, it is
helpful for descriptive purposes to subdivide it into: (1) the anterior abdominal wall; (2) the right
and left lateral walls (flanks); and (3) the posterior abdominal wall (lumbar region). The combined
term anterolateral wall is often used because some structures (e.g., the external oblique muscle and
cutaneous nerves) are located in both the anterior and lateral walls.
Layers of the Abdominal Wall. The abdominal wall consists of skin, subcutaneous tissue
(superficial fascia and fat), investing fascia, muscles, transversalis fascia (endoabdominalis fascia),
extraperitoneal (subserous) fat, parietal peritoneum.
The Anterolateral Abdominal Wall
When the abdomen is surgically operated on, it is usually the anterolateral abdominal wall
that is incised. Most of this wall consists of three muscular layers, each of which has its fibers
arranged in a different direction.
Boundaries of the anterolateral abdominal wall. The anterolateral abdominal wall is
limited superiorly by the right and left costal margins; inferiorly by a line connecting each anterior
superior iliac spine to the pubic symphysis; and on each side by a vertical line through the ends of
11th ribs to the iliac crests.
Surface Anatomy and Anatomical Landmark of the Abdominal Wall
The umbilicus (navel, "belly-button") is the puckered scar represents the former site of
attachment of the umbilical cord. In physically fit people, the umbilicus lies at the level of the
intervertebral disc between L3 and L4 vertebrae. This is about midway between the xiphoid process
of the sternum and the pubic symphysis.
A line joining the xiphoid process to the pubic symphysis indicates the position of the linea
alba (L. alba, white), a median fibrous white line or band. This line divides the anterior abdominal
wall into right and left halves. The position of the linea alba is indicated by a vertical skin groove in
the anterior median line.
The linea semilunaris is a curved line or groove (convex laterally) that extends from the 9th
costal cartilage to the pubic tubercle. This semilunar line indicates the lateral border of the rectus
abdominis muscle, which is located 5 to 8 cm from the median plane. In such persons, three or more
transverse grooves are also visible in the skin overlying the tendinous intersections of the rectus
abdominis muscles. The site of the inguinal ligament is indicated by the inguinal groove. It also
indicates the division between the anterior abdominal wall and the thigh. A fold of skin, called the
inguinal fold, is visible just superior to the inguinal groove. The inguinal ligament may be felt along
its entire length.
Regions of the Abdomen
The abdomen is divided by four planes (subcostal, transtubercular and two sagittal through
the lateral edges of the rectus abdominis muscle) into the nine regions (epigastric; subcostal left and
right; umbilical; lateral, or flank, left and right; suprapubic; inguinal left and right).
For the simple four-quadrant topographical pattern a horizontal transumbilical plane passes
through the umbilicus and the intervertebral disc between vertebrae LIII and LIV and intersects
with the vertical median plane to form four quadrants-the right upper, left upper, right lower, and
left lower quadrants.
Layer-by-layer structure of the anterolateral abdominal wall
1. Skin
The natural lines of cleavage in the skin are constant and run almost horizontally around the
trunk. This is important clinically because an incision along a cleavage line will heal as a narrow
scar, whereas one that crosses the lines will heal as a wide or heaped-up scar.
2. Subcutaneous fat, or superficial layer (Camper's fascia), contains of a variable amount
of fat, superficial nerves and vessels.
Nerve Supply
The cutaneous nerve supply to the anterior abdominal wall is derived from the anterior rami
of the lower six thoracic and first lumbar nerves. The thoracic nerves are the lower five intercostal
and the subcostal nerves, and the first lumbar nerve is represented by the iliohypogastric and
ilioinguinal nerves, branches of the lumbar plexus. The dermatome of T7 is located in the
epigastrium over the xiphoid process; that of T10 includes the umbilicus; and that of LI lies just
above the inguinal ligament and the symphysis pubis.
Blood Supply
The skin near the midline is supplied by branches of the superior epigastric artery (a branch
of the internal thoracic artery) and the inferior epigastric artery (a branch of the external iliac
artery). The skin of the flanks is supplied by branches from the intercostal, lumbar, and deep
circumflex iliac arteries.
The venous blood is collected into a network of veins that radiate from the umbilicus. The
network is drained above into the axillary vein via the lateral thoracic vein and below into the
femoral vein via the superficial epigastric and great saphenous veins. A few small veins, the
paraumbilical veins, connect the network through the umbilicus and along the ligamentum teres to
the portal vein. They form a clinically important portal-systemic venous anastomosis.
Lymph Drainage
The cutaneous lymph vessels above the level of the umbilicus drain upward into the anterior
axillary lymph nodes. The vessels below this level drain downward into the superficial inguinal
nodes.
The superficial fascia, or membranous deep layer (Scarpa's fascia) containing fibrous
tissue and very little fat. It is continuous with the deep fascia of the thigh, called the fascia lata, and
with the superficial fascia of the perineum (Colles' fascia) and with that investing the scrotum and
penis and the labia majora. The membranous deep layer of superficial fascia fuses with the deep
fascia of the abdomen.
The deep, or investing, fascia. It is a very thin, strong layer over the superficial muscles
and cannot be separated easily from them. Between the deep layer of superficial fascia and the deep
fascia of the abdomen, there is a potential space in which fluid may accumulate.
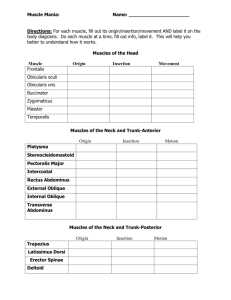
Muscles of the Anterior Abdominal Wall
Most of the abdominal wall is muscular and extends between the thoracic cage and the bony
pelvis. There are four important paired muscles in the anterior abdominal wall: three flat muscles
(external oblique, internal oblique, and transversus abdominis) and one rectus abdominis.
The combination of muscles and aponeuroses (sheetlike tendons) in the anterior abdominal
wall affords considerable protection to the abdominal viscera, especially when the muscles are in
good physical condition. The flat muscles cross each other in such a way (similar to a three-ply
corset) that strengthens the abdominal wall and diminishes the risk of protrusion of viscera
(herniation) between the muscle bundles. In about 80% of people there is an insignificant, small
triangular abdominal muscle, called the pyramidalis, which is located anterior to the inferior part of
the rectus abdominis. It tenses the linea alba.
The anterior abdominal wall may be the site of congenital hernias. Most of them occur in the
umbilical and inguinal regions. Umbilical hernias are usually small (1 to 5 cm) and congenital
(present at birth). They result from incomplete closure of the anterior abdominal wall after the
umbilical cord is ligated at birth. Herniation occurs through the defect created by the degenerating
umbilical vessels. Hernias may also occur through defects in the linea alba; these are median
hernias. Extraperitoneal fat and/or omentum (a peritoneal fold) protrude through these defects. If
the hernia occurs in the epigastric region, it is called an epigastric hernia. This type tends to occur
after 40 years of age and is often associated with obesity.
The External Oblique Muscle. This is the largest and most superficial of the three flat
abdominal muscles. It is located in the anterolateral part of the abdominal wall. Its fleshy part forms
the anterolateral portion and its aponeurosis (sheet of tendon fibers) forms the anterior part. Its
fibers run inferoanteriorly and medially in the same direction as do the extended digits (fingers)
when they are in one's side pockets. The attachments, nerve supply, and main actions of the external
oblique are given in Table 2-1. As the fibers of this muscle pass medially, they become aponeurotic.
This aponeurosis ends medially in the linea alba. Inferiorly it folds back on itself to form the
inguinal ligament between the anterior superior iliac spine and the pubic tubercle. Medial to the
pubic tubercle the external oblique aponeurosis is attached to the pubic crest. Some fibers of the
inguinal ligament cross the linea alba and attach to the opposite pubic crest. These fibers form the
reflex inguinal ligament. The medial part of the inguinal ligament is reflected horizontally back and
is attached to the pecten pubis as the lacunar ligament. Just superior to the medial part of the
inguinal ligament, there is an opening in the aponeurosis called the superficial inguinal ring. This
clinically important ring is discussed with the inguinal region.
The Internal Oblique Muscle. This is the intermediate of the three flat abdominal muscles.
Its attachments, nerve supply, and main actions are given in Table 2-1. The fibers of the internal
oblique muscle run superoanteriorly. at right angles to those of the external oblique. Its fibers also
become aponeurotic and the aponeurosis splits to form a sheath for the rectus abdominis muscle.
The inferior fibers of the aponeurosis arch over the spermatic cord as it lies in the inguinal canal.
They then descend posterior to the superficial inguinal ring to attach to the pubic crest and pecten
pubis. The most inferior tendinous fibers of the internal oblique muscle join with aponeurotic fibers
of the transverses abdominis muscle to form the conjoint tendon, which turns inferiorly to insert
into the pubic crest and pecten pubis.
The Transversus Abdominis Muscle. This is the innermost of the three flat abdominal
muscles. Its attachments, nerve supply, and main actions are given in Table 2-1. Its fibers run more
or less horizontally, except for the most inferior ones, which pass inferiorly and run parallel to those
of the internal oblique muscle. Muscle fibers of the transversus abdominis end in an aponeurosis
which contributes to the formation of the rectus sheath.
Actions of the Three Flat Abdominal Muscles (Table 2-1). The anterolateral abdominal
wall is unsupported and unprotected by bone. However, the three-ply structure of its flat muscles
and their extensive aponeuroses form a strong expandable support, which provides considerable
protection for the abdominal viscera. Normally, quiet rhythmic movements of the anterolateral
abdominal wall accompany respirations. When the diaphragm contracts during inspiration, its
domes flatten and descend, increasing the vertical dimension of the thorax. To make room for the
viscera {e.g., the stomach and intestine), the anterolateral abdominal wall expands as its muscles
relax. When the thoracic cage and diaphragm relax during expiration, the anterolateral abdominal
wall passively sinks in. However, in the forced expiration that occurs during coughing, sneezing,
vomiting, and straining, all the anterior abdominal muscles act strongly in compressing the
abdominal contents.
Acting together, the flat abdominal muscles increase the intraabdominal pressure. When the
ribs and diaphragm are fixed, compression of the viscera by the anterior abdominal muscles occurs,
which raises the intra-abdominal pressure. This action produces the force required for defecation
(bowel movement), micturition (urination), and parturition (childbirth). Acting separately, the flat
abdominal muscles move the trunk. If the pelvis is fixed, both external oblique muscles can flex the
trunk. Acting separately, one external oblique muscle can laterally flex the trunk and rotate it to the
opposite side. If the thorax is fixed, both external oblique muscles tilt the anterior part of the pelvis
superiorly and flex the trunk. Similarly, when the pelvis is fixed, one internal oblique muscle can
flex the trunk and rotate it to the same side. If the thorax is fixed, one internal oblique muscle can
laterally flex the trunk and rotate the pelvis to the opposite side. See Chap. 4 for a further discussion
of these movements of the vertebral column and trunk.
The Rectus Abdominis Muscle. This long, broad, strap muscle is the principal vertical
muscle of the anterior abdominal wall. The two muscles are separated by the linea alba and lie
close together inferiorly. The rectus abdominis is three times as wide superiorly as inferiorly; it is
narrow and thick inferiorly and broad and thin superiorly. The lateral border of the rectus muscle
and its sheath are convex and form a clinically important surface marking known as the linea
semilunaris. Most of the rectus abdominis muscle is enclosed in the rectus sheath, formed by the
aponeuroses of the three flat abdominal muscles. The anterior layer of the rectus sheath is firmly
attached to the rectus muscle at three or more tendinous intersections. When this muscle is tensed in
muscular persons, each stretch of muscle between the tendinous intersections bulges outward. The
location of the tendinous intersections is indicated by grooves in the skin between the muscle
bulges. They are usually located at the level of the xiphoid process, umbilicus, and halfway between
these structures.
Actions of the Rectus Abdominis Muscles. In addition to helping the other abdominal
muscles to compress the abdominal viscera (e.g., during coughing, vomiting, and defecating), these
muscles depress the ribs and stabilize the pelvis during walking. This fixation of the pelvis enables
the thigh muscles to act effectively. Similarly, during lower limb lifts from the supine position, the
rectus abdominis muscles contract to prevent tilting of the pelvis by the weight of the limbs.
The Linea Alba and Rectus Sheath. These structures have been mentioned several times
and have been briefly described; however, owing to their clinical importance, a more detailed
description and summary of the rectus sheath and its relationship to the linea alba follows. The
rectus sheath is the strong, incomplete fibrous compartment of the rectus abdominis muscle. It
forms by the fusion an separation of the aponeuroses of the flat abdominal muscles. At its lateral
margin, the internal oblique aponeurosis split: into two layers, one passing anterior to the rectus
muscle an the other passing posterior to it. The anterior layer joins with the aponeurosis of the
external oblique to form the anterior wall of the rectus sheath. The posterior layer joins with the
aponeurosis of the transversus abdominis muscle to form the posterior wall of the rectus sheath. The
fibers of the anterior and posterior walls of the sheath interlace in the anterior median line to form a
complex tendinous raphe, called the linea alba, which is an intermixture of the aponeurotic fibers of
this oblique and transverse abdominal muscles. It is narrow inferior to the umbilicus, but is wide
superior to it A groove is visible in the skin superficial to it in thin muscular persons. The linea alba
lies between the two parts of the rectus abdominis muscle; the umbilicus is located just inferior to
its midpoint. Superior to the costal margin, the posterior wall of the rectus sheath is deficient
because the transversus abdominis muscles passes internal to the costal cartilages and the internal
obliqus muscle is attached to the costal margin. Hence, superior to the costal margin, the rectus
muscle lies directly on the thoracic wall. The inferior one-fourth of the rectus sheath is also
deficient because the internal oblique aponeurosis does not split here to enclose the rectus muscle.
The inferior limit of the posterior wall of the rectus sheath is marked by a crescentic border called
the arcuate line. The position of this line is usually midway between the umbilicus and the pubic
crest. Inferior to the arcuate line, the aponeuroses of this three flat muscles pass anterior to the
rectus muscle to form this anterior layer of the rectus sheath.
Important structures in the rectus sheath, in addition to this rectus abdominis muscle, are the
superior and inferior epigastrh vessels, and the terminal parts of the inferior five intercostal and
subcostal vessels and nerves.
The Transversalis Fascia
This somewhat transparent internal investing layer lines most of the abdominal wall;
posteriorly it fuses with the anterior lamina of the thoracolumbar fascia. The transversalis fascia
(fascia transversalis) covers the deep surface of the transversus abdominis muscle and its
aponeurosis and is continuous from side to side, deep to the linea alba. Each part of the transversalis
fascia is named according to the structures it covers. It is called the diaphragmatic fascia on the
diaphragm; the iliac fascia on the iliacus muscle; the psoas fascia on the psoas major muscle; and
the pelvic fascia in the pelvis. The transversalis fascia also extends into the thigh with the iliac
fascia to form the femoral sheath. It also passes through the inguinal canal to form the internal
spermatic fascia, part of the covering of the spermatic cord. Internal to the transversalis fascia is the
peritoneum, the extensive serous membrane that lines the abdominal and pelvic cavities. The
transversalis fascia is separated from the peritoneum by a variable amount of subperitoneal fat,
referred to as extraperitoneal fat.
Nerves of the Anterior Abdominal Wall
The skin and muscles of the anterior abdominal wall are supplied mainly by the ventral rami
of the inferior six thoracic nerves (i.e., the continuation of the inferior intercostal nerves, T7 to
T11) and the subcostal nerves (T12). The inferior part of the anterior wall is supplied by two
branches of the ventral ramus of the first lumbar nerve via the iliohypogastric and ilioinguinal
nerves. The iliohypogastric nerve supplies the skin over the inguinal region (groin). The
ilioinguinal nerve runs anteroinferiorly, just superior to the iliac crest. to the superficial inguinal
ring. Here it emerges to supply the skin on the superomedial aspect of the thigh. The main trunks of
the intercostal nerves pass anteriorly from the intercostal spaces and run between the internal
oblique and transversus abdominis muscles. The plane between these muscles, known as the
neurovascular plane, corresponds with a similar plane in the intercostal spaces. The nerves in this
plane are accompanied by the inferior intercostal, subcostal, and lumbar arteries. The common
nerve supply of the skin and muscles of the anterolateral abdominal wall explains why palpating the
abdomen with cold hands causes contraction of the abdominal muscles. All these nerves pass
between or through muscles to reach the rectus sheath. They supply the three flat abdominal
muscles, as well as the rectus abdominis.
The anterior cutaneous nerves pierce the rectus sheath a short distance from the median
plane. The branches of T7 to T9 nerves supply the skin superior to the umbilicus; T10 innervates
the skin around the umbilicus; and T i l , T12, and LI supply the skin inferior to the umbilicus.
Arterial Supply of the Anterior Abdominal Wall
Small arteries arise from anterior and collateral branches of the posterior intercostal arteries
in the 10th and 11th intercostal spaces and from anterior branches of the subcostal arteries to
supply the anterior abdominal wall. They anastomose with the superior epigastric arteries, the
superior lumbar arteries, and with each other.
The main arteries of the anterior abdominal wall are the inferior epigastric and deep
circumflex iliac arteries, which are branches of the external iliac artery, and the superior epigastric
artery, which is a terminal branch of the internal thoracic artery. The inferior epigastric artery runs
superiorly in the transversalis fascia to reach the arcuate line; there it enters the rectus sheath. The
deep circumflex iliac artery runs on the deep aspect of the anterior abdominal wall, parallel to the
inguinal ligament, and along the iliac crest between the transversus abdominis and internal oblique
muscles. The superior epigastric artery enters the rectus sheath superiorly, just inferior to the
seventh costal cartilage.
Venous and Lymphatic Drainage of the Anterior Abdominal Wall
The superficial epigastric vein and the lateral thoracic vein anastomose, thereby uniting the
veins of the superior and inferior halves of the body. The three superficial inguinal veins end in the
great saphenous vein of the lower limb.
The superficial lymph vessels of the anterolateral abdominal wall, superior to the umbilicus,
pass to the axillary lymph nodes, whereas those inferior to the umbilicus drain into the superficial
inguinal lymph nodes. However, lymph from the anterior abdominal wall, in general, drains to the
lumbar lymph nodes and to the common and external iliac lymph nodes.
Internal Surface of the Anterior Abdominal Wall
The internal or deep surface of this wall is covered with parietal peritoneum. It exhibits
several peritoneal folds, some of which contain remnants "of fetal vessels that carried blood to and
from the placenta before birth. A peritoneal fold is an elevation of peritoneum with a free edge,
which is usually raised by an underlying blood vessel or its ligamentous remains. There are hollows
or fossae between adjacent folds. Superior to the umbilicus there is a large median fold called the
falciform ligament. It passes from the deep surface of the superior half of the anterior abdominal
wall to the liver and the diaphragm. The free edge of this ligament contains the ligamentum teres,
the remnant of the umbilical vein. Before birth the umbilical vein carried oxygenated blood from the
placenta to the fetus. This vein is patent for some time after birth and may be used for exchange
transfusions during early infancy (e.g., in infants with erythroblastosis fetalis or hemolytic disease
of the fetus. Although reference is often made to the "obliterated" umbilical vein, it is usually patent
to some extent. It often becomes very dilated if there is portal hypertension (raised pressure in the
portal system, such as that caused by cirrhosis of the liver. Inferior to the umbilicus, five umbilical
folds (two on each side and one in the median plane) pass superiorly toward the umbilicus. The
lateral umbilical folds, formed by elevations of peritoneum covering the inferior epigastric arteries,
run superomedially on each side. The medial umbilical folds are formed by elevations of
peritoneum covering the medial umbilical ligaments, the obliterated parts of the fetal umbilical
arteries. These vessels carried blood from the fetus to the placenta for oxygenation before birth.
They ascend obliquely from the lateral walls of the pelvis to the umbilicus. The median umbilical
fold is formed by an elevation of peritoneum covering the median umbilical ligament, the fibrous
remnant of the urachus that joined the fetal bladder to the umbilicus. The median umbilical
ligament and fold pass from the deep aspect of the umbilicus to the apex of the urinary bladder. Of
the five folds inferior to the umbilicus, only the lateral umbilical folds contain vessels that carry
blood.
5.2. Theoretical questions to studies:
1. The regional structure of the abdominal wall.
2. The regions of the antero-lateral abdominal wall.
3. The nerve and blood supplay of the antero-lateral abdominal wall.
4.
5.
6.
7.
The layer structure of the antero-lateral abdominal wall.
Muscles of the antero-lateral abdominal wall.
Fascias of the antero-lateral abdominal wall.
Surgical anatomy of the congenital disease and congenital anomalies of anterolateral abdominal wall. Principles of surgical treatment.
8. The methods of laparotomies.
5.3. Materials for self-control:
1.
Diffuse pain referred to the epigastric region and radiating circumferentially around the chest
is the result of afferent fibers that travel via which of the following nerves?
A
B
C
D
E
2.
Greater splanchnic
Intercostal
Phrenic
Vagus
None of the above
In the patient described, the subsequent localization of the pain in the right hypochondriac
region is the result of inflammatory stimulation of fibers that are extensions of which of the
following nerves?
A
B
C
D
E
Greater splanchnic
Intercostal
Phrenic
Vagus
None of the above
3.
The patient receives a general anesthetic in preparation for a cholecystectomy. A right
subcostal incision is made, which begins near the xiphoid process, runs along and immediately
beneath the costal margin to the anterior axillary line, and transects the rectus abdominis
muscle and rectus sheath.
At the level of the transpyloric plane, the anterior wall of the sheath of the rectus
abdominis muscle receives contributions from the
A aponeuroses of the internal and external oblique muscles
B aponeuroses of the transversus abdominis and internal oblique muscles
C aponeuroses of the transversus abdominis and internal and external oblique muscles
D transversalis fascia
E transversalis fascia and aponeu-rosis of the transversus abdominis muscle
4.
At this level of incision, liga-tion of the superior epigastric artery probably will result in little,
if any, necrosis of the rectus abdominis muscle because the superior epigastric artery
anastomoses with the
A
B
C
D
E
deep circumflex iliac artery
inferior epigastric artery
intercostal arteries
internal thoracic artery
musculophrenic artery
5.
Exploration of the peritoneal cavity disclosed a distended gallbladder. It is located
A
B
C
D
E
6.
Numerous stones could be palpated. A finger was inserted into the omental foramen (of
Winslow), and the common bile duct was palpated for stones. Structures that bound the
omental foramen include all the following EXCEPT the
A
B
C
D
E
7.
between the left and caudate lobes of the liver
between the right and quadrate lobes of the liver
in the falciform ligament
in the lesser omentum
in the right anterior leaf of the coronary ligament
caudate lobe of the liver
common bile duct
hepatic vein
inferior vena cava
superior part of the duodenum
Before closure of the incision, it is felt that a drain should be left in place in the abdominal
cavity so that any leakage of bile from the sutured stump or from inadvertent injury to the duct
system can be detected. This drain would most advantageously be located in the
A
B
C
D
E
omental bursa
pelvic cavity
pouch of Morison
right paracolic gutter
right subphrenic recess
Literature
1. Snell R.S. Clinical Anatomy for medical students. – Lippincott Williams &
Wilkins, 2000. – 898 p.
2. Skandalakis J.E., Skandalakis P.N., Skandalakis L.J. Surgical Anatomy and
Technique. – Springer, 1995. – 674 p.
3. Netter F.H. Atlas of human anatomy. – Ciba-Geigy Co., 1994. – 514 p.
4. Ellis H. Clinical Anatomy Arevision and applied anatomy for clinical
students. – Blackwell publishing, 2006. – 439 p.