Title
advertisement

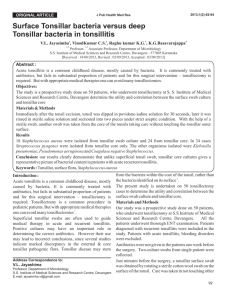
Title: Colonies of Actinomyces in bilateral tonsils operated for halitosis, sore throat and bilateral tonsillar hypertrophy - A causal or casual finding? Abstract: Actinomycosis of the tonsillar crypts, though not uncommon, is relatively infrequent nowadays. It is caused by the branching filamentous gram positive bacteria belonging to the Actinomycosis family. Known inhabitants of the oral cavity, hence poor dental hygiene and oro-facial injury may predispose to symptomatic disease. Their importance lies in the fact that they may have varied presentations ranging from suppurative lesions to those mimicking oropharyngeal malignancies. Hence identification of this organism is important for specific treatment strategies. The question whether their presence in colonies in tonsil is incidental or causative for tonsillar lesions is still not definitely solved. Here we describe a young patient presenting with halitosis, sore throat, recurrent tonsillitis and bilateral tonsillar hypertrophy. The histopathology of the tonsillectomy specimen revealed colonies of Actinomyces in bilateral tonsillar crypts, along with cryptitis and reactive lymphoid hyperplasia. Key words: Actinomycosis; tonsil; bilateral; halitosis; hypertrophy; tonsillectomy Sir, Actinomycosis infections of head and neck region are caused by various species of tangled, filamentous, gram-positive bacteria belonging to the Actinomycosis family, of which the most common human pathogen is Actinomyces israelii 1. In 55% they involve the cervicofacial region, in 20% thoracic, and in 15% abdomino-pelvic. Actinomyces colonizing tonsillar crypts has been described in 6.7-35% of tonsillectomy specimens1,2, while some other studies proposed an even wider range3,4,5. Nevertheless, their importance lies in the fact that they may have varied spectrum of presentations ranging from mere commensals to suppurative, necrotic or fibrotic lesions to even those simulating oropharyngeal malignancies6, 7. ‘Ray fungus’ as previously called (‘mycosis’ derived from the Greek word ‘mykes’), the first case of human actinomycosis was reported by Von Langenbeck in 1845. In 1960’s Waksman showed that actinomyces is actually a gram-positive bacteria, forming colonies that mimic branched networks of fungal hyphae3. Here, we report a case of 28-year old male patient presenting with malodor, sore throat and recurrent bouts of tonsillitis for the last four years. On examination bilateral tonsils were hypertrophied and covered with thick grey white slough. Investigations including those for immune status were all within normal limits, except for mild neutrophilic leucocytosis (13,500/cu.mm) and mild anemia (hemoglobin: 10.5 gm/dl). The patient was put on oral antibiotics comprising of amoxycillin and clavulenic acid, and an interval tonsillectomy by intraoral approach was done to alleviate the recurrent symptoms. Bilateral tonsils were removed from the tonsillar bed; the patient had an uneventful recovery with no intraoperative or postoperative hemorrhage. Amoxycillin clavulenic acid, initially intravenous and replaced later by oral therapy, along with chorhexidine mouthwash and oral hygiene reinforcement were continued, and complete healing took place in two weeks duration. Microscopic examination of the excised bilateral tonsillar tissue showed squamous hyperplasia of the surface epithelium, with focal ulceration. Underlying lymphoid tissue had evidence of reactive hyperplasia with prominent germinal centers; scattered neutrophils and cryptitis were also seen. Radiating, amorphous, faintly hematoxyphilic, large colonies morphologically in accordance with Actinomyces were seen, adherent to the surface epithelium and invading the crypts. The periphery of these colonies showed branched fungi-like configuration (Figure 1). The colonies were Gram positive, as well as Periodic Acid Schiff (PAS) positive (Figure 2). Actinomyces show fermentative type of carbohydrate metabolism; special requirements for successful culture of the organism include avoidance of contamination, strict anaerobic conditions or under increased carbon dioxide (5% CO2) tension and prolonged culturing (7-14 days) at 36⁰C±1⁰C. Enriched media for aerobic incubation include sheep blood agar, peptone yeast extract glucose (PYG) or brain heart infusion (BHI) broth. For anaerobic incubation, Schaefer agar, Tarozzi broth, or kanamycin-vancomycin blood agar (KV agar) may be used. Filamentous organisms are identified to species or group level by use of appropriate bacteriological methods, like Gram staining and gas liquid chromatography (GLC) analysis of the acid fermentation end products8. While some authors9 believe that Actinomycosis may have a damaging role to the tonsils, most of the others 3,4 opine that they are common saprophytes in this tonsillar area. However, the organism becomes pathogenic in devitalised tissue with reduced oxygen tension10. Precipitating factors like dental caries, dental manipulations, maxillofacial trauma, foreign bodies, radiotherapy, diabetes mellitus and last but not the least, poor dental hygiene, as seen in this patient, are known to cause disease in cervico-facial region. Disruption of the mucosal barrier of the tonsil is required for the bacteria to become infective and cause disease. Hyperplastic squamous lining with surface ulceration, cryptitis, organisms deep into the tonsillar lymphoid tissue, and bilateral hypertrophy in this patient favor of a causal (etiological) rather than a casual (incidental) finding. Treatment may be carried out by intravenous penicillin G; amoxicillin with or without clavulenic acid, imipenem, clindamycin, ceftriaxone, vancomycin, rifampicin, erythromycin, or doxycycline may be used as alternative drugs, some of which in case of penicillin allergy10. Treatment should be individualized, with surgery as an adjuvant to long term antibiotics for abscess, fistula, cavity formation, or deep seated infections1. Initial intravenous formulation is replaced by oral therapy till complete healing of the lesion. Tonsillectomy may be considered in cases of hypertrophy to the point of pharyngeal obstruction, frequent recurrent tonsil infections, with or without peritonsillar abscesses7. In this patient tonsillectomy was done for recurrent tonsillitis, sore throat and bilateral hypertrophy, refractory to antibiotic treatment; diagnosis was established by histological examination of the excised tonsils. To conclude, though a known commensal, Actinomycosis may have an etiological role in long standing symptomatic tonsillar lesions refractory to antibiotic treatment. A high level of clinical inspection and identification is of utmost importance because of the capacity of the resultant lesions to masquerade as malignancy. Prolonged antibiotics combined with surgery may be required. Hence, a surgical, pathological and microbiological team effort is necessary for a satisfactory outcome. References: 1. Soler Sendra A, Subirana Pozo FX, Consola Maroto B, Serra Carreras J, Cuquet Pedragosa J. [Tonsillar actinomycosis manifested as expectorated debris]. [Article in Spanish] Acta Otorrinolaringol Esp 2009; 60: 372-374. 2. Assimakopoulos D, Vafiadis M, Askitis P, et al. The incidence of Actinomyces israelii colonization in tonsillar tissue. A histopathological study. Rev Stomatol Chir Maxillofac 1992; 93:122–126. 3. Mohamad I. Actinomyces in the tonsils: Hospital Universiti Sains Malaysia Experience. The Internet Journal of Otorhinolaryngology 2009; 8(2). 4. Bhargava D, Bhusnurmath B, Sundaram KR, Raman R, Al Okbi HM, Al Abri R, et al. Tonsillar actinomycosis: a clinicopathological study. Acta Trop 2001; 80:163–168. 5. Gaffney R, Harrison M, Walsh M, Sweeney E, Cafferkey M. The incidence and role of actinomyces in recurrent acute tonsillitis. Clin Otolaryngol Allied Sci 1993; 18: 268-271. 6. Mohanty S. Actinomycosis of faucial tonsil masquerading as oropharyngeal malignancy. Indian J Otolaryngol Head Neck Surg 2006; 58: 82-84. 7. Seltzer AP. Tonsillectomy: an excision biopsy. J Natl Med Assoc 1976; 68: 525-6, 460. 8. Pulverer G, Schütt-Gerowitt H, Schaal KP. Human cervicofacial actinomycoses: microbiological data for 1997 cases. Clin Infect Dis 2003; 37: 490-497. 9. Yadav SP, Chanda R, Gathwala G, Yadav RK. Actinomycosis of tonsil masquerading as tumour in a 12-year-old child. Int J Pediatr Otorhinolaryngol 2002; 63:73-75. 10. Metgud SC. Primary cutaneous actinomycosis: a rare soft tissue infection. Indian J Med Microbiol 2008; 26: 184-186. Legends: Figure 1: Microphotograph showing follicular tonsillitis with colonies of Actinomyces (arrow) (Hematoxylin and Eosin stain, 100x magnification); Inset: higher magnification of the periphery of the colonies showing filamentous branched, hyphae-like structures (Hematoxylin and Eosin stain, 400x magnification). Figure 2: Microphotograph showing PAS positive colonies of Actinomycosis invading into the tonsillar lymphoid tissue (Periodic Acid Schiff stain, 400x magnification).