THE ROYAL OTTAWA HEALTH CARE GROUP
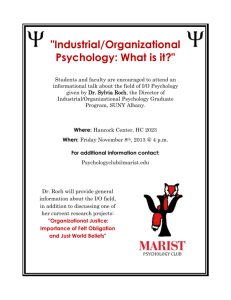
advertisement

The Royal’s Predoctoral Residency Program In Clinical Psychology www.theroyal.ca Version Date: July 29, 2014 THE ROYAL’S PREDOCTORAL RESIDENCY PROGRAM IN CLINICAL PSYCHOLOGY ***** TABLE OF CONTENTS RESIDENCY PROGRAM OVERVIEW ...................................................................................... 3 STIPEND/ADMINISTRATIVE INFORMATION ........................................................... 3 PERSONAL-PROFESSIONAL LIFE BALANCE .............................................................. 4 PHILOSOPHY AND GOALS OF THE PROGRAM .......................................................... 4-5 CORE CURRICULUM .................................................................................................. 6 CORE REQUIREMENTS .............................................................................................. 7 SUPERVISION AND ROTATION ASSIGNMENT .......................................................... 8 RESEARCH AND PROGRAM EVALUATION ................................................................. 8-9 DUE PROCESS ........................................................................................................... 9 PSYCHOLOGY SEMINAR SERIES: THE ROYAL’S SEMINAR SERIES .................................................................... 9 CITY WIDE SEMINAR SERIES ....................................................................... 9-10 AVAILABLE RESOURCES ........................................................................................... 10 TRANSPORTATION ................................................................................................... 10 OTTAWA AND BROCKVILLE VICINITY OVERVIEW ................................................... 10-11 ROMHC TRACK: OVERVIEW OF ROMHC TRACK DESCRIPTION OF PROGRAMS/SERVICES/ROTATIONS ................................................ EXAMPLE SCHEDULE ................................................................................................. ANXIETY DISORDERS PROGRAM .................................................................. COMMUNITY MENTAL HEALTH PROGRAM (THE ROYAL) ............................. GERIATRIC PSYCHIATRY PROGRAM ............................................................ MOOD DISORDERS PROGRAM… ................................................................... NEUROPSYCHOLOGY ROTATIONS ................................................................ NEUROPSYCHOLOGY UNIT...................................................................... NEUROPSYCHOLOGY ROTATION IN FORENSIC PSYCHIATRY ................ OPERATIONAL STRESS INJURY CLINIC ....................................................... SCHIZ0PHRENIA PROGRAM ......................................................................... SUBSTANCE USE AND CONCURRENT DISORDERS……………………………… WOMEN’S MENTAL HEALTH PROGRAM…………………………………………….. YOUTH PSYCHIATRY PROGRAM ................................................................... 12 13 14 15-17 18 19-20 21 21 22 23 24-25 26-27 28 29-30 BMHC TRACK: OVERVIEW OF BMHC TRACK DESCRIPTION OF PROGRAMS/SERVICES/ROTATIONS ........................................... 31 EXAMPLE SCHEDULE ................................................................................................. 32 INTEGRATED FORENSIC PROGRAM (IFP) .................................................... 33 FORENSIC TREATMENT UNIT (FTU) ........................................................ 33-35 SECURE TREATMENT UNIT (STU) ............................................................ 36 GERIATRIC OUTREACH TEAM ....................................................................... 37 RESIDENCY PROGRAM SUPERVISORY FACULTY AND ADDITIONAL PSYCHOLOGY STAFF ...................................................................................... 38-41 APPLICATION REQUIREMENTS/PROCEDURES .................................................................... 42-44 The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 2 THE ROYAL’S PREDOCTORAL RESIDENCY PROGRAM IN CLINICAL PSYCHOLOGY ***** RESIDENCY PROGRAM OVERVIEW The Royal Ottawa Health Care Group (ROHCG; hereafter The Royal) provides a full range of mental health services to the residents of Eastern Ontario and Western Quebec. Our residency program comprises two tracks with many joint training experiences that address and support core competency requirements. The two tracks include the Royal Ottawa Mental Health Centre (ROMHC) Track and the Brockville Mental Health Centre (BMHC) Track; the ROMHC provides training experiences and opportunities for in-depth assessment and treatment of a wide range of mental health issues, whereas the BMHC has a focus on providing residents training in Clinical Psychology within a Forensic context. Applicants may apply to one or both tracks. The Royal has five full-time Residency positions for the 2015-16 year. Four full time Resident positions will be offered at the ROMHC track and one full time Resident position will be offered at the BMHC track. The current residency program has evolved from the ROHCG Internship Program and the Rehabilitation Centre – Royal Ottawa Hospital (ROH) Consortium Internship Program. As such the ROHCG/ROH has been part of a long standing predoctoral training program in psychology accredited by both the Canadian Psychological Association (CPA) and the American Psychological Association (APA) until August 2005. As of September 2005, a revised residency program has been offered entitled the Royal Ottawa Health Care Group Predoctoral Residency Program in Clinical Psychology. Concurrent CPA and APA accreditation was granted from 2005 until 2013. A CPA Reaccreditation Site Visit was held in summer 2013. CPA Reaccreditation was granted from 2012/13 until 2019/2020. For more information on CPA accreditation, please contact the accreditation office at http://www.cpa.ca/accreditation/whatis/. The CPA head office is located at 141 Laurier Avenue West, Suite 702, Ottawa, Ontario, K1P 5J3. Information regarding The Royal’s Psychology Residency Program is also available on our website at http://www.theroyal.ca/careers/student-placements-residencies-and-fellowships/pre-doctoralresidency-program-in-clinical-psychology/. More information regarding the programs in the respective tracks will be outlined in subsequent sections. STIPEND/ADMINISTRATIVE INFORMATION Residents receive a stipend of $30,000.00 per annum that includes 4 weeks paid vacation, 10 days education/professional development leave, sick leave, 5 days personal/emergency leave and 12 statutory holidays. This stipend is subject to employment insurance and tax deductions. Canadian residents have health benefits under the Ontario Health Insurance Plan. Extended health care benefits covering prescription drugs, dental care, etc. are the responsibility of the Resident. Residents are required to obtain professional liability insurance. Please note: Successful Residents will be required to have a clear Criminal Reference Check (for the Vulnerable Sector) dated within six months prior to their start date. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 3 PERSONAL-PROFESSIONAL LIFE BALANCE In recognition of the importance of personal-professional life balance, in addition to 20 days paid vacation and stat holidays, Residents are permitted 10 education/professional development days which they can use at any time during the year for various purposes (dissertation work or meetings, attending workshops or conferences, or other professional development activities). This request is made to and approved by the Training Committee Executive. We also provide compensation time for Residency activities scheduled outside regular work hours (e.g. evening groups). In addition, to ensure the pace of Resident workload promotes quality learning experiences, one Friday per month is considered an “unscheduled work day” which Residents may use to work on various core requirements, complete readings related to rotations or program evaluation projects, or catch up on rotation-specific workload (i.e., reports, supervision meetings). These measures have been implemented to protect Residents’ personal-professional life balance and to promote quality learning experiences. PHILOSOPHY AND GOALS OF THE PROGRAM The Royal’s Psychology Residency Program’s mission, values, principles, goals and objectives are described below. The Royal’s Psychology Residency Program provides generalist pre-doctoral training in Clinical Psychology within the context of a nationally recognized tertiary care setting (ROMHC and BMHC). The Royal is committed to being a Centre of Excellence in the areas of clinical service delivery, research and education. The vision for The Royal is: Mental health care transformed through partnerships, innovation and discovery. The mission of The Royal is: Delivering excellence in specialized mental health care, advocacy, research and education. The values of The Royal are: We are guided by innovation and a passionate commitment to collaboration, honesty, integrity and respect. Philosophy, Mission and Model of The Royal’s Psychology Residency Program: The Royal’s Psychology Residency Program’s mission is: Pursuing excellence in Clinical Psychology Predoctoral Residency Training. The Royal’s Residency Program’s philosophy, values and principles are: 1) Excellence in training requires a training environment that is empowering, professionally enriching, respectful and supportive. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 4 2) Psychology has multiple roles through which mental health and functioning can be enhanced. Training provides opportunities for experiential skill development in the multiple roles of the Psychologist including clinician, teacher/supervisor, researcher/evaluator, administrator and leader. 3) Training is conducted within a system that respects interdisciplinary team functioning and the unique role of Psychologists. 4) Training has a sound scientist-practitioner foundation that enhances professional skills to optimize positive outcomes for patients. This foundation includes training in competent practice of empirically-supported treatments and evaluative research. 5) Training involves exposure to diverse populations and clinical experiences that enhances professional development, professional competence and sensitivity to diversity. 6) Training in ethics and legislation creates ethically sound Psychologists. The Royal’s Psychology Residency Program’s Training Goals are: 1. Goal: To provide breadth and depth of knowledge and experience to develop clinical competence in the following areas: Assessment, Diagnosis, Treatment/Intervention, Consultation, Interpersonal Relationships (clients and staff), Care Planning, Outcome Monitoring/Evaluation, Evidence-Based Practice. 2. Goal: To enhance the scientist-practitioner approach by training Residents in evaluation research and exposing them to other forms of clinical research within a hospital and community setting. 3. Goal: To train Residents to engage competently in the multiple roles of the clinical Psychologist including clinician, evaluator/researcher, teacher/supervisor, administrator and leader. 4. Goal: To train Residents on ethical principles and practices and relevant legislation so that they practice in a professionally ethical manner as a Psychologist. 5. Goal: To train Residents, through a breadth of diversity experiences, to be sensitive to diversity/individual differences and apply this sensitivity in their practice as a Psychologist. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 5 CORE CURRICULUM The training at the ROMHC and BMHC tracks are united by a joint administration, training philosophy and core curriculum. Although Residents are affiliated with either the ROMHC or BMHC track, peer consultation, group supervision, seminars and other teaching activities are jointly conducted across tracks. Residents from both tracks meet at least 3 times/month, typically on Fridays, in person or by teleconference/video-conference for peer consultation, group supervision, and The Royal’s seminar series or the Ottawa city wide seminar series. Residents are given the opportunity to complete a secondary rotation at the other location based upon interests and training goals. Residents are responsible for their own transportation and associated transportation costs if they choose to complete a rotation at the other location. The Residency program provides generalist training to prepare the Resident for practice as a professional Psychologist. Residents will receive training in assessment, intervention/therapy, interdisciplinary consultation, teaching and program evaluation/evaluative research. Successful completion of all core requirements (or in rare circumstances, Training Committee Executive-approved modifications) is required for successful completion of the residency program. All requirements are to be completed in accordance with the ethical standards of our profession. Residents will have the opportunity to undertake assessment and treatment of inpatients and outpatients with a variety of presenting problems. Assessments include: intellectual and cognitive functioning, personality and emotional functioning/adjustment, neuropsychological functioning, forensic assessment, and vocational aptitude and interest. Emphasis is placed on use of diagnostic interviewing in combination with a variety of objective psychometric instruments. The Residency program is characterized by three predominant empirically informed theoretical orientations, which include cognitive-behavioural, interpersonal and emotionally-focused. Patients are seen individually, in groups and for family-based intervention. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 6 CORE REQUIREMENTS 1) Residents will complete a minimum of eleven assessments. a. Eight assessments will be comprehensive, psychometrically-based assessments or diagnostic workups, which include treatment planning or a consultative component. The other three assessments will be psychometrically-based but need not be as comprehensive. b. Two assessments must include a cognitive/neuropsychological component c. One assessment must be performed in a community-based context. Multiple requirements may be fulfilled by one assessment (e.g. cognitive assessment in the community would fulfill two requirements). 2) Residents will see a minimum of six clients for individual therapy over the course of the residency year, including a combination of more brief, focused interventions (minimum 2) and more extended or complex course of treatment (minimum 2). The latter will require the resident to actively address complex clinical presentations in planning and delivering treatment “beyond the standard protocol.” This may include (but is not limited to) longer-term therapy, actively addressing multiple or complex presenting problems/diagnoses/personality factors, increased frequency / duration of sessions, use of adjunctive empirically-based strategies in treatment, well-reasoned / researched significant modifications to treatment protocol, and / or use of more than one therapeutic modality. Appropriate selection and definition of the above will be determined on the basis of the resident’s learning goals, the resident and supervisor’s clinical and ethical judgment, best practice guidelines, and program-specific standards. Residents are encouraged to gain experience in more than one theoretical approach to intervention. 3) Within the context of assessment or intervention, Residents will formulate and communicate a minimum of 10 diagnoses. 4) Residents will facilitate or co-facilitate at least one psychotherapy group. 5) Residents will attend two seminar series: 1) The Royal’s seminar series and 2) The Ottawa City-Wide Seminar Series. Attendance of seminars is mandatory. 6) Residents will attend weekly group supervision to discuss clinical cases, professional and ethical issues, supervision and the program evaluation project. Attendance of group supervision is mandatory. 7) Residents will supervise a practicum student, which is most often arranged in their primary rotation. In the (uncommon) event that this is not possible, other experiences designed to help the resident gain experience or expertise in clinical supervision will be arranged. 8) Residents will be responsible for making a grand rounds presentation for staff at The Royal on a clinical experience they have gained during the Residency year. 9) Program Evaluation is given particular emphasis in the Royal’s Psychology Residency Program. Residents will commit an amount of time analogous to that of a secondary rotation (averaging 0.5 days /week throughout the year) to completion of a program evaluation project. 10) Residents will be required to demonstrate competence in at least one empirically supported treatment. 11) In the context of assessment or treatment, residents must show sensitivity to, increase knowledge of, and adapt their clinical approach to the diversity characteristics of the client. Diversity is defined as cultural, individual, and role differences, particularly those based on age, gender, gender identity, race, ethnicity, culture, national origin, religion, sexual orientation, disability, language, or socioeconomic status. 12) Residents will actively participate in at least one hospital committee. Resident representative on The Royal’s Training Committee). The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 (Up to two Residents will sit as a Page 7 SUPERVISION AND ROTATION ASSIGNMENT At minimum, Residents receive four hours of supervision per week with an autonomously registered Psychologist. Both primary and secondary supervisors meet weekly with the Resident. The frequency and length of contact is dependent on the Resident's needs and level of development. On some rotations, individual supervision may also be complemented with group supervision. Group supervision of Residents occurs three times per month and is provided by the Director or Assistant Director of Training (and occasionally by a member of the Training Committee to allow more varied supervisor perspectives). Residents present suitable material for discussion. One group supervision session per month is focused on the Program Evaluation Project. The style and focus of supervision will largely be dependent on the theoretical orientation of the supervisor, as well as the Resident's past experience and current needs. Supervision is strengthsbased and developmental in nature. Rotations will begin with an acknowledgement of the skills the Resident brings to the program and identification of Resident training goals or needs. The actual training experiences will be negotiated based on this starting point through completion of a supervision agreement form. Residents are assigned primary and secondary rotations based on their expression of interest, training goals, and availability of the supervisor(s). Rotations can not be guaranteed due to limits on supervisor availability and unanticipated changes in staffing or programs. However, we will make every attempt to accommodate Residents’ expressed rotation interests. (In the infrequent event that this is not possible, we work with the Resident to identify their specific training goals (in terms of populations, activities, orientations etc.) and endeavour to place them in Rotations that will allow them to meet these training goals.) Primary and secondary supervisors meet with the Director and Assistant Director of Training on a quarterly basis to discuss Residents' progress, areas of focus, planning of rotations and educational experiences, and continued professional development. Following these quarterly review meetings, consolidated feedback is provided to the Resident to ensure continued open and discussion and bidirectional feedback. RESEARCH AND PROGRAM EVALUATION The Royal continues to expand its research and education capabilities to improve treatment and promote prevention. These initiatives are advanced by the Institute for Mental Health and Research, and close working relationships with the University of Ottawa, School of Psychology, Faculty of Medicine, and Faculty of Health Sciences. Many of the Psychology staff are involved in ongoing clinical research programs in their areas of interest. Opportunities exist for Residents to become involved in research projects. A key goal of the Residency program is exposure of Residents to all aspects of the scientistpractitioner model. Increasingly, the role of a hospital-based psychologist is evolving to include program evaluation of services provided by both Psychology staff and other health care professionals in hospital and community settings. Therefore, a project in program evaluation is required by each Resident. The design of this project is flexible to accommodate the Resident’s The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 8 interests, but will consist of involvement in, or design of, an ongoing program evaluation initiative. This is typically done within the primary clinical rotation. However, the opportunity to design and implement an evaluation project on another program is possible. Supervision will be provided for each project. One half day per week is scheduled for the Resident’s program evaluation project. Additional time (one “unscheduled work day”) per month can also be used as needed for this project. DUE PROCESS Due process guidelines have been established and are provided, in writing, to all Residents at the commencement of the Residency. Residents are also provided with a Training Manual. PSYCHOLOGY SEMINAR SERIES The Royal’s Residents participate in a number of educational opportunities including two seminar series. The Royal is a teaching facility of the University of Ottawa, thereby providing numerous educational opportunities within the School of Psychology, Faculty of Medicine, and other local teaching facilities. The clinically based seminars include a discussion of relevant ethical issues. Additionally, regular in-services are held, during which lectures on topics of interest and current research are given. Residents also attend Psychology discipline meetings. A) The Royal’s Seminar Series: This seminar three Fridays B) series is provided by The Royal’s faculty/staff and invited guest lecturers on two or per month. The modules include: Professional Practice Assessment Consultation Cognitive-Behavioural Therapy Emotion-Focused Therapy Interpersonal Therapy Community-Based Consultation Group Therapy Program Evaluation Supervision City Wide Seminar Series and Professional Practice Seminar Series: This series of seminars is conducted in collaboration with other Residency/Internship sites in the Ottawa area (The University of Ottawa, The Ottawa Hospital and the Children's Hospital of Eastern Ontario). Seminars are held once per month on Fridays and the location rotates across these settings. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 9 Topics have included: Issues in Working with People with Disabilities Cross-cultural Psychology Preparing for Registration Exams Feminist Approaches to Clinical Practice Working with Sexual Minorities Psychology in Private Practice AVAILABLE RESOURCES The Residency program has available dedicated office space, internet access, a facility wide computer network, a computerized workload measurement tracking system, automated voice mail, and stand-alone PC's for Residents' use. Access to internal and external e-mail is also provided. Dictation and Word-processing facilities are available. A number of statistical and data base packages can be accessed including SPSS-PC. The program also has access to a broad range of assessment instruments and audio-visual equipment. The Royal has two professional libraries (one at the ROMHC and one at BMHC) housing a selection of Clinical Psychology publications. Interlibrary loans are available through the libraries. The library also has Psych Lit and MedLine on CD-ROM. The National Research Council Library and the Health Canada Library are also located in Ottawa. The Royal has an Administrative Assistant who supports the Training Program including the Director of Training, Assistant Director of Training and the Residents. TRANSPORTATION Residents tend to prefer to attend most Friday Resident Group days in person in Ottawa. However, video-conferencing is available, if needed, for residents located at the BMHC location to attend the Resident seminars and group supervision (2-3 Fridays per month). Residents are responsible for transportation and costs for attending Citywide Seminars and when selecting a secondary rotation at the opposite location. OTTAWA AND ITS VICINITY The Ottawa Region has a population of approximately 1,000,000. The city is located on the border of Quebec, across the Ottawa River and has the Rideau River and the Rideau Canal flowing through it. Many small towns, within an hour of the city, offer historical and recreational interests. On the Quebec side, about 20 minute drive from downtown; there are the Gatineau Hills with ski resorts and an abundance of lakes and wilderness experiences. There are bike paths throughout Ottawa and the Rideau Canal offers boating in the summer and skating in the winter. Ottawa is famous for the number of parks within the city, outdoor activities and concerts such as the Jazz festival, Bluesfest and Folk Festival in July, Winterlude in February, the Tulip Festival in May, and the Busker festival in the summer. It also hosts the largest Chamber Music festival in the world. The downtown core is rich with diverse eating establishments. There are three local universities (University of Ottawa, Carleton University and St. Paul's) and two community colleges. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 10 The city also houses several outstanding museums (Science and Technology, Canadian Museum of Civilization, the Canadian Museum of Nature, the Canadian War Museum and the National Museum of Aviation), the National Gallery of Canada and the National Arts Centre. For more information on the City of Ottawa, please visit http://www.ottawa.ca/en/index.htm BROCKVILLE AND ITS VICINITY Brockville is a small historic city of 21,000 in the Thousand Island Region of the St. Lawrence River. It is located between Kingston and Montreal on the 401 highway, and is about 1 hour commuting time from Ottawa. Brockville is a popular tourist centre during the summer, particularly for those who enjoy boating, sailing, golf and outdoor activities of all kinds. During the summer it is home to festivals and summer theatre with an open air Farmers Market. St Lawrence College campus is located in Brockville offering a variety of diploma courses, an active Summer School of Art, and the new Bachelor of Nursing program. The city is friendly and easily accessible by car and rail. The cost of living is reasonable when compared to larger centres. Brockville is one hour away from Kingston and Queens University, and forty-five minutes from Gananoque, another popular summer resort town. For more information on the City of Brockville, please visit http://www.city.brockville.on.ca/. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 11 THE ROYAL OTTAWA MENTAL HEALTH CENTRE TRACK ***** DESCRIPTION OF PROGRAMS/SERVICES AND ROTATIONS The Royal Ottawa Mental Health Centre (ROMHC) serves as the major provider of psychiatric services to the Champlain District of Eastern Ontario and Western Quebec. Psychiatric assessment and treatment services for adults and adolescents are provided, in English and French, on an inpatient, outpatient, and community basis. The ROMHC is a teaching hospital of the University of Ottawa. The inpatient capacity is approximately 200 beds. Treatment programs for both inpatients and outpatients include anxiety disorders, forensic psychiatry, geriatric psychiatry, mood disorders, schizophrenia and substance use and concurrent disorders. There is also a centralized Neuropsychology Unit and Community Mental Health Program. The Operational Stress Injury Clinic serves active members and veterans of the Canadian Forces and RCMP, and family members. The Youth Psychiatry Program serves individuals 16 - 18 years of age with inpatient, partial hospitalization, outpatient and outreach services. The Royal is administered under a program management model with the discipline of Psychology headed by a Professional Practice Leader and a Director of Allied Health Professional Practice. Four residency positions are available at the ROMHC track. Clinical services at the ROMHC are organized under programs. Each program is typically comprised of several service units. Following the restructuring that has been ongoing in Ontario hospitals, the nature of the programs at the ROMHC has been evolving. The programs listed below reflect the structure that will likely be in place as of September 2015. Residents will also be given the opportunity to do a secondary rotation at BMHC based on the Resident’s interests and training goals and supervisor availability. Residents complete one full year primary rotation (typically 2.5 days/week) and two six month secondary rotations (typically 1 day/week). In addition, one half day per week is scheduled for the program evaluation project. Three Fridays per month are reserved for seminars, peer consultation and group supervision (Resident Group Day). One Friday per month is an “unscheduled work day” as outlined above. Please see below an example of a Resident’s schedule. Rotation days are arranged collaboratively with all supervisors involved. Rotations are not scheduled for Fridays due to the seminar series. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 12 Example Schedule: Monday Tuesday Wednesday Thursday Friday Primary Rotation Primary Rotation Primary Rotation Secondary Rotation Resident Group Day Program Evaluation The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Three Fridays/month include: Program Admin Issues Group Supervision Peer Consultation The Royal’s Seminars City-wide Seminars One Friday/month is an “unscheduled work day” which can be used for various clinical, program evaluation, or professional development /educational activities as noted above. Page 13 ANXIETY DISORDERS PROGRAM, THE ROYAL Psychology Staff: Andrew Jacobs, Psy.D., C. Psych. Meagan Gallagher, Ph.D., C.Psych. (Supervised Practice) Kylie Francis, Ph.D., C. Psych. Rotation Options: Primary or Secondary Description of Program: The Anxiety Disorders Program provides interdisciplinary, outpatient assessment and treatment to individuals with complex anxiety disorders including Panic Disorder, Agoraphobia, Social Anxiety Disorder, Generalized Anxiety Disorder (GAD), Obsessive-Compulsive Disorder (OCD), PostTraumatic Stress Disorder, Specific Phobias, and other disorders associated with the anxiety and obsessive-compulsive spectrums (e.g. health anxiety, trichotillomania, body dysmorphic disorder). Individuals typically present with comorbid anxiety diagnoses, as well as difficulties with mood, substance use, and personality concerns. The role of Psychology includes provision of individual and group-based cognitive-behavioural therapy, assessments for treatment, diagnostic assessments, and program development and evaluation research. Psychology also consults to other members of the Anxiety Disorders Program team as well as other programs within The Royal. Resident Opportunities: Clinical assessment (including interviewing, assessment for treatment, and psychodiagnostic assessment) Group cognitive behavioural therapy. Current groups include CBT for Panic Disorder and Agoraphobia, Social Anxiety Disorder, OCD, and GAD, and a transdiagnostic anxiety treatment group for transitional-aged (18-22 years) youth. Short- and intermediate-term individual cognitive behavioural therapy for individuals with complex symptom presentations. Consultation with interdisciplinary staff at weekly rounds. Program development and evaluation projects may be available. Supervision of a practicum student is possible on primary rotations. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 14 COMMUNITY MENTAL HEALTH PROGRAM (THE ROYAL) Psychology Staff: Susan Farrell, Ph.D., C. Psych. Liz Glennie, M.A., Psychometrist Rotation Options: Primary or Secondary Description of Program: The Community Mental Health Program is a new program of The Royal that includes 8 teams/services: Three Assertive Community Treatment (ACT) Teams, the Step-Down from ACT Team, the Dual Diagnosis Consultation Outreach Team, the Psychiatric Outreach Team, Homes for Special Care and Community Treatment Order coordination. Six of the eight teams have options for psychology residents that are described below. Opportunities exist for residents to complete a primary or secondary rotation on any of these teams or to have a primary or secondary rotation that includes involvement across a range of teams. Assertive Community Treatment (ACT) and ACT Step-Down Teams, ROMHC: There are three ACT teams in the Community Mental Health Program – one that works with persons with a diagnosis of schizophrenia (and often concurrent disorder), one that works with persons with a range of Axis I and II diagnoses and one that works with persons with a dual diagnosis (intellectual delay and mental illness). The first two teams listed are in Ottawa, the third team is located in Brockville. Assertive Community Treatment (ACT) Teams are an interdisciplinary team of mental health professionals working in partnership with patients living in the community with serious and persistent mental illness. The ACT Team supports people with complex, long-term and serious psychiatric illness involving multiple hospitalizations. The ACT team promotes recovery, improved quality of life and helps patients to achieve goals through supportive treatment and rehabilitation. Individualized treatment and rehabilitation plans are developed with each patient. The team offers after-hours emergency services for patients in the service. Services include; assessment, therapy, concurrent disorder services, rehabilitation planning and promotion of recovery, medication prescription, education, monitoring and advocacy. The Step-Down from ACT team is similar to the ACT team model, but provides services for ACT patients who are managing more independently in the community but still require support. The objective of the ACT Step-Down program is to provide treatment, support, recovery and rehabilitation services to patients in the community, and prevent (or shorten) re-admissions to hospital. The program is interdisciplinary and aims to help patients improve their quality of life in the community and reach their optimum level of independent functioning. Clinical work on both teams involves a substantial degree of interdisciplinary team work and consultation with other disciplines including psychiatry, nursing, social work, occupational therapy, The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 15 recreation therapy, community mental health workers and peer specialists. The role of psychology includes the provision of services in diverse areas of assessment, differential diagnosis, consultation, treatment planning, individual therapy and group therapy (at times), education to care provider networks, advocacy, interdisciplinary team work and the direction of clinical evaluation research. On the Dual Diagnosis ACT team Psychology also supervises the Behavioral Support Therapists. Resident Opportunities: Specific activities will be discussed and arranged based on availability and Resident’s goals for training. Residents may have the opportunity to participate in the following activities: Clinical Assessment (including diagnostic interviewing, cognitive and personality assessment) within a community setting Clinical Consultation Individual or group psychotherapy (cognitive behavioural, interpersonal, systemic therapy) Consultation with interdisciplinary staff and range of community service providers Interdisciplinary team involvement Education and treatment plan development Involvement in ongoing research and/or program evaluation projects When possible, Residents may supervise psychology practicum students Regional Dual Diagnosis Consultation Team, ROMHC: The Regional Dual Diagnosis Consultation Team offers services to older adolescents and adults with both an intellectual disability and mental health problems. The team is a specialized community outreach team based in Ottawa that provides interdisciplinary clinical assessments, consultation, education and treatment recommendations for the persons with a dual diagnosis. The team serves the Residents of the Champlain Local Health Integration Network that includes both urban and rural catchment areas. Services are provided mainly in the community in which the patient resides, using an outreach consultation model. Clinical work involves a substantial degree of interdisciplinary team work and consultation with other disciplines including psychiatry, nursing, social work, occupational therapy and speech language pathology. The role of psychology includes the provision of services in diverse areas of assessment, differential diagnosis, consultation, treatment planning, education to care provider networks, advocacy, interdisciplinary team work and the direction of clinical evaluation research. Resident Opportunities: Specific activities will be discussed and arranged based on availability and resident’s goals for training. Residents may have the opportunity to participate in the following activities: The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 16 Clinical Assessment (including diagnostic interviewing, cognitive and personality assessment) within a community setting Clinical Consultation (within a community and often an inpatient setting) Consultation with interdisciplinary staff and a range of community service providers Interdisciplinary team involvement Education and treatment plan development Involvement in ongoing research and/or program evaluation projects When possible, Residents may supervise psychology practicum students Psychiatric Outreach Team, ROMHC: The Psychiatric Outreach Team offers services to adolescents and adults who are homeless or at risk of homelessness who have a severe and persistent mental illness including a concurrent disorder (addictions and mental illness). The team provides direct patient service and consultation and education to its broad range of community partners. Community partners include emergency shelters, rooming houses, residential care facilities, drop-in centers and community health centers in Ottawa and Renfrew County. Clinical work involves a substantial degree of interdisciplinary team work and consultation with other disciplines including addiction specialists, psychiatry, nursing, social work, occupational therapy and recreation therapy. The team uses an outreach consultation model to provide assessment, short-term treatment and limited emergency intervention services within the partner agency locations. The role of psychology includes the provision of services in diverse areas of assessment, differential diagnosis, consultation, treatment planning, education to care provider networks, advocacy, interdisciplinary team work and the direction of clinical evaluation research. Resident Opportunities: Specific activities will be discussed and arranged based on availability and resident’s goals for training. Residents may have the opportunity to participate in the following activities: Clinical Assessment (including diagnostic interviewing, cognitive and personality assessment) within a community setting Clinical Consultation (within an community and often inter-agency setting) Consultation with interdisciplinary staff and a range of community service providers Interdisciplinary team involvement Education and treatment plan development Involvement in ongoing research and/or program evaluation projects When possible, Residents may supervise psychology practicum students The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 17 GERIATRIC PSYCHIATRY PROGRAM, ROMHC Psychology Staff: Hans P. de Groot, Ph.D., C. Psych. Rotation Options: Primary or Secondary Description of Program: The Geriatric Psychiatry Program offers comprehensive services to meet the mental health needs of people 65 years of age and over. Patients typically have complex mental and physical health needs. Services are provided in inpatient, day program, and outpatient settings. There is also an Outreach Service which provides consultation service to selected long-term care facilities in and around the Ottawa area. Clinical work involves a substantial degree of interdisciplinary team work and consultation with other disciplines including psychiatry, nursing, social work, occupational therapy and recreational therapy. The role of psychology includes the provision of services in the areas of cognitive and personality assessment, individual psychotherapy, consultation, program evaluation and interdisciplinary team work. Empirically supported treatments are used but often must be individualized to address the patient’s needs and treatment goals. Resident Opportunities: Specific activities will be discussed and arranged based on availability and resident’s goals for training. Opportunities exist in the day program and outpatient program Residents may have the opportunity to participate in the following activities: Clinical assessment (including interviewing, cognitive and personality assessment) Individual psychotherapy (acceptance- and mindfulness-augmented cognitive behavioural therapy) Consultation with interdisciplinary staff Interdisciplinary team involvement (for inpatient and day program) Program evaluation projects are available Possibility of doing co-therapy for an outpatient psychotherapy group When possible, Residents may supervise psychology practicum students The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 18 MOOD DISORDERS PROGRAM, ROMHC Psychology Staff: Irit Sterner, Ph.D., C.Psych. Kelsey Collimore, Ph.D., C.Psych. Rotation Options: Primary or Secondary Description of Program: The Mood Disorders Program is a specialty multidisciplinary unit of psychiatrists, psychologists, occupational therapists, social workers, and nurses. Treatment services are offered to patients with diagnoses of unipolar depression and bipolar disorder; however, patients present with high rates of co-morbidity (e.g., mood disorders, anxiety disorders, substance use disorders, personality disorders) and psychosocial/family issues to consider in the context of service delivery. Services are primarily provided in the outpatient setting, although there are some opportunities in the inpatient setting. Residents gain experience with diagnostic interviewing for complex mood and anxiety disorders, individual and group therapy, consultation, and interdisciplinary team work. The focus of psychology in the program is on the delivery of empirically supported treatments, with emphasis on cognitive-behavioural therapies. In addition, psychology is actively involved in program development and evaluation, research and education. Resident Opportunities and Rotations: Residents have the opportunity to participate in the following activities: Assessment and differential diagnosis with complex, tertiary care patients with mood disorders Outpatient treatment: Group cognitive-behavioural therapy (CBT) for unipolar depression, group behavioural activation therapy for unipolar depression, and group CBT for bipolar disorder Inpatient treatment: Brief group CBT for inpatients Individual CBT for patients with complex symptom presentations, including schemafocused treatment Consultation with interdisciplinary staff Research and/or program development and evaluation projects Supervision of a practicum student may be possible The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 19 Examples of Rotation Experiences on the Mood Disorders Program a) Primary 12 Month Rotation (2.5 days for one year) Time Tuesday Wednesday 10 to 12:00 Unipolar group (first) and 2nd group supervising (Sept to July) Inpatient, individual, or group CBT 1 to 3 Team meeting Supervision 2 to 5 Individual and supplemental group therapy sessions Bipolar Disorder second three months (March to July) Thursday Diagnostic Assessment Program Evaluation b) Secondary 6 Month Rotation (One day for 6 months) 9 to 12:00 Assessment and inpatient or outpatient treatment group for 4 month intervals 1 to 2 Individual therapy patient 2 to 3 Supervision The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 20 NEUROPSYCHOLOGY ROTATIONS, THE ROYAL Neuropsychology Rotations at the ROMHC are comprised of two services: 1) The Neuropsychology Service and 2) The Neuropsychological Rotation in Forensic Psychiatry Both of these services are described in more detail below. The Royal’s Residency Program does not, at this time, offer the breadth and depth of training in neuropsychology to equip residents for post-residency competency in neuropsychology. NEUROPSYCHOLOGY UNIT, ROMHC Psychology Staff: Angela Stewart, Ph.D., C. Psych. Maria Tsiakas, Ph.D., C. Psych. Rotation Options: Secondary Rotation Description of Program: Following a centralized service model, The Neuropsychology Service provides comprehensive neuropsychological assessments to adult inpatients across a variety of hospital programs. Referrals are prioritized. Resident Opportunities: A secondary rotation in Neuropsychology offers residents exposure to the comprehensive neuropsychological assessment of psychiatric disorders. The resident will gain comfort with all aspects of the evaluation including interview, feedback to the patient and team, and reportwriting. Residents will also gain experience in test selection and differential diagnosis. Typical referral questions include: 1) is the etiology of cognitive deficits associated with psychiatric illness or a neurodegenerative process? 2) support with diagnostic clarification, treatment, and rehabilitation recommendations, and 3) return to work/school issues in the context of a mental illness. Didactic training in the form of short readings related to the ethical considerations in the delivery of neuropsychology services and attendance at some Psychiatry Rounds may also form a part of the rotation. Since consultations are requested from throughout the hospital, the Resident would play an important role in selecting the cases that best suit his or her training needs. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 21 NEUROPSYCHOLOGICAL ROTATION IN FORENSIC PSYCHIATRY, ROMHC Psychology Staff: Jemeen Horton, Ph.D., C. Psych. Rotation Options: Secondary Rotation Description of Program: The Forensic Service at the ROHMC houses a 21-bed medium security inpatient unit which provides court-ordered fitness to stand trial and criminal responsibility assessments, and a 22-bed minimum security inpatient unit which provides longer-term assessment (up to 18 months), treatment and rehabilitation for individuals who have been found unfit to stand trial or not criminally responsible. Specific to the Forensic Neuropsychological Rotation are requests for neuropsychological assessments as part of in-custody and out-of-custody psychiatric assessment to assist the Court in determining fitness to stand trial and/or criminal responsibility, and in providing recommendations for treatment and discharge planning, and placement issues for the Ontario Review Board disposition orders. Symptom validity assessments are sometimes requested. Resident Opportunities: This rotation offers residents with academic and practical neuropsychological experience to further develop their skills in providing comprehensive neuropsychological assessment of individuals in a mental health setting. Residents may have the opportunity to participate in the following activities: Residents will build on existing skills to enhance their expertise in assessing general intellectual ability, executive functions, attention and memory, visual-spatial functions, language abilities, and sensory and motor functions. Residents may be exposed to patients with a wide range of disorders (depending on the current case load) including severe mental illness, substance abuse, neurodevelopmental disorders, traumatic brain injury, medical/neurological conditions, and various types and stages of dementing illnesses. During collaborative supervision, residents will integrate information about the patient’s neuropsychological and psychiatric status to establish diagnostic considerations, formulate recommendations for treatment planning, discharge planning, and rehabilitation strategies, develop report writing skills and communication of assessment results and recommendations to referral sources, multidisciplinary team member, patients, and their families. Residents may also have an opportunity to participate in risk assessment clinical team meetings. Residents will encounter various ethical issues in forensic neuropsychological practice including clients rights, informed consent and confidentiality, maintaining objectivity and fairness, and scope of professional competence. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 22 OPERATIONAL STRESS INJURY CLINIC, ROMHC Psychology Staff: Sarah Bertrim, Ph.D., C.Psych. Michele Boivin, Ph.D., C.Psych. Robert Bialik, Ph.D., C. Psych. Luis Oliver, Ph.D., C.Psych. Psychologist (TBC) Rotation Options: Primary or Secondary Description of Clinic: The Operational Stress Injury (OSI) Clinic is a specialized outpatient program at the Royal Ottawa Mental Health Centre (ROMHC) that serves veterans of the Canadian Forces (CF), current CF members who are releasing from the CF, and eligible members of the RCMP. We also provide services to family members. The clinic represents a partnership between the ROMHC and Veterans Affairs Canada (VAC) and is also a part of a national network of OSI clinics across Canada. An operational stress injury (OSI) is defined as any persistent psychological difficulty resulting from operational duties performed while serving in the Canadian military or RCMP. OSIs can include Posttraumatic Stress Disorder, other anxiety disorders, depression, substance use disorders, and adjustment disorders. Other problem areas that may be addressed include emotion regulation difficulties, marital or family relationship difficulties, and challenges associated with transitioning to civilian life. Clinical services are provided on an outpatient basis and are coordinated and delivered by an interdisciplinary team. Psychology staff provide assessment for diagnosis and treatment planning, consultation, and intervention (primarily individual and group). Empirically supported treatments form the basis for intervention, with Cognitive Behavioural Therapies as the predominant framework. Prolonged Exposure, Cognitive Processing Therapy, and EMDR are used when appropriate. Emotion-Focused, Experiential, Dialectical Behaviour Therapy, or Acceptance and Commitment Therapy techniques may be integrated to individualize treatment. Clinical services are provided on-site at the OSI Clinic, and outreach/ networking services are provided in locations throughout a broader catchment area (including Pembroke/Petawawa, Gatineau, Kingston, Cornwall, North Bay, and Nunavut). Telehealth may be used to provide services and education. In addition, psychology staff are actively involved in research, education, networking, program development and evaluation. Resident Opportunities: Clinical assessment (including structured and clinical interviewing, psychodiagnostic assessment, assessment for pension, assessment for treatment planning). Empirically-supported individual and group intervention. Consultation with interdisciplinary staff and external agencies. Outreach education for external agencies and community providers. Research and/or program development and evaluation projects. Possible provision of educational or clinical services via outreach or telehealth. Supervision of a practicum student may be possible. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 23 SCHIZOPHRENIA PROGRAM, ROMHC Psychology Staff: Matthew Kerr, Ph.D. C. Psych. Rotation Options: Primary or Secondary Description of Program: The Schizophrenia Program offers services to patients with psychotic/schizophrenia spectrum disorders. Patients typically have multiple diagnoses and psychosocial/family issues to consider in the context of service delivery. Services are provided in the inpatient and outpatient settings. Clinical psychology work involves a substantial degree of interdisciplinary team work and consultation with other disciplines including psychiatry, nursing, social work, occupational therapy, recreation therapy, dietary and spiritual care. The role of psychology includes the provision of services in the areas of assessment, individual and group psychotherapy, consultation, interdisciplinary team work, research, program development and evaluation, advocacy and teaching. Residents completing a primary rotation may also have the opportunity to supervise a practicum student. Empirically supported treatments are used and are individualized to address the patient’s needs and treatment goals. Exciting opportunities are available in individual and group cognitive behavioural therapy for psychosis and third wave cognitive behavioural therapy approaches such as mindfulness, compassion-focused, and acceptance and commitment therapy. The placement allows the resident to engage in what we believe is a very meaningful, humanistic, meaning-making and empowering approach to issues/presentations experienced by those who are affected by psychoses. The approach to supervision is consistent with our approach to our patients that is, strengths-focused, respectful, collaborative and empowering. Resident Opportunities: Whenever possible we attempt to provide residents with the clinical opportunities that are the most meaningful and of interest based on the resident’s goals (we are usually able to accommodate interests!). Opportunities in the outpatient program are most common, but inpatient work can be arranged based on resident interest and the appropriateness of patients for psychological intervention/assessment. Residents may have the opportunity to participate in the following activities: (Each resident usually does at least one assessment, carries a number of individual psychotherapy patients with a range of presenting problems, co-leads one group and does consultation, interdisciplinary team work, program development and supervision). Clinical Assessment (including interviewing, cognitive and psychodiagnostic assessment) Individual psychotherapy (Cognitive Behavioural Therapy for Psychosis and Acceptance and Commitment Therapy --as well as the incorporation of Interpersonal, Mindfulness & Compassion-focused approaches) Common presenting problems are psychosis, trauma history/PTSD, dissociation, social anxiety, OCD, worry/GAD, panic, substance use and working with negative symptoms and valued life goals) The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 24 Group psychotherapy (with options in Cognitive Behavioural Therapy for psychosis, CBT for social anxiety, a hearing voices CBT group, a CBT for psychosis and OCD group, an emotional resilience/regulation group; a positive psychology recovery group, a CBT for worry group and a compassion focused-mindfulness based group as well as other psychoeducational, supportive and process-focused therapy groups) Consultation with interdisciplinary staff Interdisciplinary team involvement (for inpatient and/or outpatient program) Involvement in research and program development and program evaluation projects are available When possible, Residents may supervise psychology practicum students The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 25 SUBSTANCE USE & CONCURRENT DISORDERS PROGRAM, ROMHC Psychology Staff: Kim Corace, Ph.D., C.Psych. Rotation Options: Primary or Secondary Description of Program: The Royal’s Substance Use and Concurrent Disorders Program provides specialized concurrent disorders care to individuals with complex substance use disorders, moderate to severe mental health disorders, complicated physical health issues and psychosocial vulnerabilities. Services are tailored to the unique needs of the individuals and communities we serve in Eastern Ontario and beyond. Our inter-professional team offers a continuum of services ranging from low to high intensity. Services focus on prevention, harm reduction, and treatment. The population we serve has difficulty accessing services elsewhere. SUCD services include an inpatient stabilization unit, a 28 day rehabilitation program, day program, outpatient clinics, outreach, evening and afternoon educational programs, family program, women’s program, relapse prevention program, the Regional Opioid Intervention Service, and an early intervention program. REGIONAL OPIOID INTERVENTION SERVICE The recently launched Regional Opioid Intervention Services (ROIS) is a regional integrative model of concurrent disorders care for opioid addiction and mental health problems. Our 4 pillars include: (1) patient care and family support, (2) training, education, and capacity building, (3) integration and coordination of services, and (4) program and outcome evaluation. The ROIS is the first of its kind in Ontario, providing concurrent opioid addiction treatment and mental health care on an outpatient basis within an interdisciplinary team. The Service is a collaborative, hub and spoke partnership between the clinic at The Royal and a range of community agencies, hospital programs, and family physicians throughout the Champlain LHIN, who each play a role in the management and treatment of opioid dependent individuals. The Service also provides training, mentorship, and ongoing consultation for family physicians and addiction and mental health workers in order to build capacity to identify and treat opioid addiction. This Service aims to foster the linkages and integration of addiction, mental health, and primary care services, and bring care closer to where patients live, with a focus on areas of our Champlain LHIN where no such services previously existed. Resident Opportunities: Specific activities will be discussed and arranged based on availability and Resident’s goals for training. Residents may have the opportunity to participate in the following activities: Clinical assessment and differential diagnosis of inpatients and outpatients with complex concurrent substance use and mental health disorders The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 26 Clinical Consultation, including opportunities within inpatient, outpatient, and community settings Individual and group psychotherapy (cognitive behavioural therapy, motivational interviewing) Consultation with interdisciplinary staff and range of community service providers Interdisciplinary team involvement Education and treatment plan development Involvement in ongoing research and/or program evaluation projects When possible, Residents may supervise psychology practicum students The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 27 WOMEN’S MENTAL HEALTH PROGRAM (THE ROYAL) Psychology Staff: Psychologist (TBC) Rotation Options: Primary or Secondary Description of Program: The Women’s Mental Health Program is a new program of The Royal offering outpatient services to adult women referred from other programs of The Royal. Referrals are primarily received from the Mood and Anxiety Disorders Programs, as well as Central Intake. Common presenting problems include diverse mental and physical health issues and comorbidities, in particular emotion regulation, trauma/PTSD, mood and anxiety disorders, interpersonal factors, substance use, disordered eating, and chronic pain. The team consists of a Psychologist and Social Worker, providing gender-sensitive services involving assessment, consultation, education, and group and individual treatments for women with mental health issues. Clinical services are provided primarily at The Royal, using a brief/short-term intervention and/or consultation model. Clinical work involves a substantial degree of interdisciplinary team work and consultation with social work, and to a lesser degree other disciplines including psychiatry, nursing, and occupational therapy. The role of Psychology includes the provision of services in diverse areas of assessment, differential diagnosis, consultation, brief individual treatments, group therapies, interdisciplinary team work, and the direction of clinical evaluation research within the context of a broader program of research. Some community services are provided regarding women’s mental health within partner agency locations. The role of Psychology in this context includes the provision of services in diverse areas of consultation and education to care provider networks, advocacy, interdisciplinary team work, and the direction of clinical evaluation research. There may also be opportunity to develop future consultation links with the Community Mental Health Program. Resident Opportunities: Specific activities will be discussed and arranged based on availability and resident’s goals for training. Residents may have the opportunity to participate in the following activities: Clinical Assessment within a hospital outpatient setting Clinical Consultation (within a community and hospital outpatient setting) Consultation with interdisciplinary staff and a range of community service providers Interdisciplinary team involvement Education and treatment plan development Involvement in ongoing research and/or program evaluation projects When possible, Residents may supervise psychology practicum students It may be possible, depending on availability of cases, to receive exposure to Health and Rehabilitation Psychology competencies The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 28 YOUTH PSYCHIATRY PROGRAM, ROMHC Psychology Staff: Margaret DeCorte, Ph.D., C.Psych. Judy Makinen, Ph.D., C.Psych Rotation Options: Primary or Secondary Description of Program: The Youth Psychiatry Program is an intensive and specialized psychiatric and mental health program offering assessment, multi-modal treatment, and consultative services to youth (16 to 18 years of age), and their families. The program focuses on youth with early onset psychiatric disorders and/or complex, treatment-resistant disorders. Those with conduct disorders, primary problems with addictions, or pervasive developmental disorders are not typically treated in this program. The Youth Psychiatry Program offers a stepped-care approach, with a full continuum of services: Inpatient, Partial Hospitalization, Outpatient services, Day Treatment (Section 23 McHugh School), Outpatient Services, and Transition Services in support of youth and their families. The Youth Program integrates evaluation, research, education, and early intervention services into bestpractice clinical service delivery. Inpatient Unit This is an eight-bed unit for youth who have serious mental health concerns, and who are unable to function in less-controlled environments or with their families. Psychology staff on the unit provide assessment, stabilization, group treatment and brief individual treatment as part of an interdisciplinary team. Youth Partial Hospitalization Unit This is a full-day intensive treatment program serving up to 10 youth who attend 2-4 days per week. It provides comprehensive treatment by an interdisciplinary team for youth with serious psychiatric difficulties; YPHU participants require intensive treatment but are able to live outside hospital. Tutoring is offered in the unit, where youth can obtain high school credits. The Inpatient and Partial Hospitalization units are closely linked for service delivery. Youth Outpatient Assessment, consultation, and treatment services are provided on an outpatient basis to those youth who can function outside the hospital setting with clinical support from a specialized interdisciplinary team. Services are typically longer-term and may be delivered in collaboration/partnership with local health practitioners, schools, and/or community mental health providers. Referrals are received for youth with significant concerns regarding anxiety, depression, ADHD, trauma, psychosis, or other mental health difficulties. Individual, family, and group The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 29 treatment are offered as part of Outpatient Services. Liaison with community schools is frequently involved. Day Treatment (Section 23 school) Day Treatment services are delivered within a regular high school setting in a self-contained unit consisting of two classrooms and clinical space. The unit serves a population of adolescents 13 to 18 years of age who have psychiatric and/or serious emotional problems that interfere with their ability to attend the regular school system. The program is designed to be rehabilitative, so that youth may return to a regular school or work setting following several months to one academic year of treatment within this therapeutic setting. Youth Outreach/Community Education Staff from the Youth program are frequently asked to speak to schools, community agencies, and nonprofit groups in Ottawa on various topics including depression, anxiety, suicide, trauma, and early recognition of mental health concerns. The Communications department of The Royal typically coordinates the events and provides banners and handouts for use by staff. Two major initiatives are currently underway: the Bell “Let’s Talk” series, and the “Do It For Daron” campaign. Resident Opportunities: Primary and secondary rotations are available in the Youth Program. Residents function as members of interdisciplinary teams including psychology, psychiatry, social work, nursing, occupational therapy, recreation therapy, addiction counsellors and youth counsellors. Residents have most frequently worked in the Partial Hospital, Inpatient, or Outpatient units, but opportunities may exist in other youth-oriented activities that are not unitspecific. Residents may gain experience in individual and group psychotherapy, community-based interventions, assessment, and family therapy. Opportunities for residents will be available on the basis of their expressed interests and level of clinical expertise. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 30 THE BROCKVILLE MENTAL HEALTH CENTRE TRACK ***** DESCRIPTION OF PROGRAMS/SERVICES AND ROTATIONS The Brockville Mental Health Centre (BMHC) has been providing mental health treatment since 1894. It is located in Brockville, which is a small city of 21,000 and is one hour south of Ottawa. The hospital has been part of the Royal since 2001, and is a teaching hospital of the University of Ottawa and Queen’s University. The BMHC has two main programs (Forensic Treatment Unit and Secure Treatment Unit) that fall under the Integrated Forensic Program (IFP). In general, the IFP provides an integrated approach to the assessment, treatment, rehabilitation, and community reintegration of adults (18+) who have conflict with the criminal justice system, as well as research, education and advocacy. The Forensic Treatment Unit provides assessment and treatment of a forensic population of adults who may be (or have been found) unfit to stand trial as well as not criminally responsible by the court on account of mental illness, whereas the Secure Treatment Unit is contracted by the Ministry of Community Safety and Correctional Services (MCSCS) to provide secure assessment, treatment, and discharge planning to provincially sentenced adult male offenders in the correctional system who have been diagnosed with a mental illness. Additional community-based teams located at BMHC are the Geriatric Outreach Team of the Geriatrics Program and the Assertive Community Treatment Team for Persons Dually Diagnosed (ACT-DD) of the Community Mental Health Program. Both of these teams offer psychological assessment and consultation services to a range of community partners in a multi-disciplinary team setting. Some treatment experiences may be available on the Geriatric Outreach Team. In 2015-16, BMHC will offer one position with a concentration in Forensic Clinical Psychology. In the Forensic Concentration, the resident will do a primary and secondary rotation in the Integrated Forensic Program (FTU & STU). The remaining secondary rotation can be completed in a non-forensic program at BMHC or in a program at ROMHC. Residents are responsible for their own transportation and associated transportation costs if they choose to complete a rotation at ROMHC. Residents complete one full year primary rotation (typically 2.5 days/week) and two six month secondary rotations (typically 1 day/week). In addition, one half day per week is scheduled for the program evaluation project. Three Fridays per month are reserved for seminars, peer consultation and group supervision (Resident Group Day). One Friday per month is an “unscheduled work day” as outlined above. Please see below an example of a Resident’s schedule. Rotation days are arranged collaboratively with all supervisors involved. Rotations are not scheduled for Fridays due to the seminar series. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 31 Example Schedule: Monday Tuesday Wednesday Thursday Friday Primary Rotation Primary Rotation Primary Rotation Secondary Rotation Resident Group Days Program Evaluation The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Three Fridays/month include: Program Admin Issues Group Supervision Peer Consultation The Royal’s Seminars City-wide Seminars One Friday/month is an “unscheduled work day” which can be used for various clinical, program evaluation, or professional development /educational activities as noted above. Page 32 INTEGRATED FORENSIC PROGRAM (IFP), BMHC The Integrated Forensic Program at the Brockville Mental Health Centre is comprised of two services: 1) The Forensic Treatment Unit, a 59-bed mental health facility with outpatient service, which serves a forensic population of individuals with serious mental disorders who have come into conflict with the law; and 2) The Secure Treatment Unit, a 100-bed provincial correctional facility, which serves a corrections population of individuals with serious mental disorders who are serving sentences of less than two years. Both of these services are described in more detail below. Residents completing a primary or secondary rotation in the Forensic Treatment Unit may be able to take assessment or treatment cases in the Secure Treatment Unit. Conversely, residents completing a primary or secondary rotation in the Secure Treatment Unit may be able to take assessment or treatment cases in the Forensic Treatment Unit. Residents concurrently completing a primary and secondary rotation in the IFP (i.e., the primary rotation and an ongoing secondary rotation are within the IFP) may collaborate with FTU and STU supervisors to arrange a fluid schedule across both rotations. FORENSIC TREATMENT UNIT (FTU), BMHC Psychology Staff: Anik Gosselin, Ph.D., C.Psych. Steven Michel, M.Sc. Jeffrey Robinson, M.A. Michael Seto, Ph.D., C.Psych. Rotation Options: Primary or Secondary Description of Program: The Forensic Treatment Unit (FTU) in Brockville is part of the Integrated Forensic Program, which also includes the Assessment and Stabilization Service for Inpatients and the Rehabilitation Service for Inpatients (Champlain) in Ottawa and the Secure Treatment Unit (STU) in Brockville. Collectively, the Integrated Forensic Program provides specialized interdisciplinary assessment, treatment, rehabilitation, and community reintegration to adults with serious mental disorders who have come into conflict with the law. Mental health services include the following: court consultation; fitness and criminal responsibility assessments; inpatient services; mental health court consultation; and outpatient services. Most FTU and Champlain patients fall under the jurisdiction of the Ontario Review Board (ORB) after committing a crime and being found unfit to stand trial or not criminally responsible due to mental disorder (http://www.orb.on.ca). The ORB makes dispositions about the custody and care The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 33 of persons under its jurisdiction, including commitment in hospital or supervised conditions while living in the community. These dispositions are reviewed at least annually, as required by law. The FTU program in Brockville provides inpatient services on units with different levels of security, as well as services to clients who have re-integrated to the community but who are still under an ORB disposition (i.e., outpatients): The Assessment and Stabilization Services include 13-beds (3 assessment beds and 10 stabilization beds). The assessment beds are for short-term stays of individuals referred by the courts for assessments of fitness, criminal responsibility, risk of violence and recidivism, or other psycho-legal questions. The stabilization beds provide care to acutely ill clients with the aim of helping stabilize their mental state and prepare them for forensic rehabilitation. The Inpatient Recovery Services is a 33-bed unit that provides inpatient treatment to relatively stable forensic clients, with the aim of reducing their risk of future offending and preparing them for discharge to the community. The Transition Services (a.k.a. the F.I.T.T.) includes a 13-bed unit that houses stable transitional rehabilitation clients whose length of stay is expected to be less than two years and who are participating in services that prepare them for returning to the community, and services to clients who have re-integrated to the community, but who are still under a disposition order from the ORB (i.e., outreach nurses, a social worker, a psychiatrist, O.T services, vocational services and recreation therapy services). For all units, clinical work is carried out within an interdisciplinary framework, and psychology works closely with psychiatry, nursing, social work, vocational and occupational therapy. Team discussion and decisions are made at monthly case conferences. The role of psychology includes neuropsychological, personality and risk assessment, individual and group psychotherapy, consultation, program evaluation, and research. Resident Opportunities: A psychology rotation within the Forensic Treatment Unit would provide the Resident with a wellrounded experience in forensic assessment and rehabilitation. Specific activities can be negotiated based on resident interests, goals and schedule, depending on clinical demands. Supervision is provided by a dynamic psychology team including a registered psychologist (specialized in Forensic Psychology, Clinical Psychology and Neuropsychology) and experienced psychometrists to help the Residents advance their skills in delivering excellence in mental health care. Residents may have the opportunity to participate in the following activities: Clinical Assessments (including psychodiagnostic assessments; neuropsychological assessments; risk assessments; personality assessments, assessment for malingering). Individual psychotherapy (predominantly cognitive behavioural therapy and dialectic behaviour therapy) including Relapse Prevention, CBT for Psychosis, Anger Management, behavioural interventions, and treatment of substance abuse. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 34 Group psychotherapy (CBT for Psychosis; a DBT skills training group will eventually be offered as well). Ongoing forensic and neurophysiological research, including risk assessment, trajectories of mentally disordered offenders, substance abuse, sleep disorders, research on aggression and impulsivity using electrophysiological markers (EEG & ERP), and program evaluation. Assisting in assessments of fitness and criminal responsibility referred to psychiatry (availability of these opportunities may vary). The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 35 SECURE TREATMENT UNIT (STU), BMHC Psychology staff: Drew Kingston, Ph.D., C. Psych. Alison Davis, M.A. Rotation Options: Primary or Secondary Description of Program: The STU is a 100-bed facility for provincially sentenced, mentally disordered offenders with four 25-bed units: assessment and stabilization unit, sexual behaviours unit, aggressive behaviour modulation unit and trauma disorders unit. Offenders typically have multiple diagnoses and all services are provided on an inpatient basis. The average length of stay for offenders is approximately 4-months, and so assessment and treatment services are expedited. The services provided include assessment and group therapy targeting antisocial thinking, anger management, sexual behaviour, PTSD, substance use, effective relationships, and other relevant needs. Some individual therapy is also done. Clinical work involves an interdisciplinary team (psychology, psychiatry, social work, family medicine, nursing, addictions counseling, recreational therapy, vocational therapy and pastoral care). The provision of all services is empirically-based and ongoing research continues to evaluate many aspects of the tasks at the STU. Interdisciplinary case conferences are held weekly. Resident Opportunities: Specific activities will be discussed and arranged based on availability and Resident’s goals for training. Residents may have the opportunity to participate in the following activities: Group psychotherapy (psychoeducation, cognitive behavioural therapy, dialectical behaviour therapy or process-focused therapy) Individual psychotherapy (cognitive behavioural, motivational or trauma focused) Clinical Assessment (cognitive, ADHD, and risk assessments) Consultation with interdisciplinary staff Interdisciplinary team involvement Program evaluation projects are available The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 36 GERIATRIC OUTREACH TEAM, BMHC Psychology Staff: Chris Prince, Ph.D., C.Psych. Rotation Options: Secondary Description of Program: The counties of Lanark, Leeds and Grenville have a higher proportion of seniors (15%) relative to the provincial population (12%). For seniors with significant mental health difficulties and/or cognitive impairment, family physicians in Leeds and Grenville refer their clients to the Geriatric Outreach Team at the Brockville Mental Health Center (BMHC), and those in Lanark refer their clients to the Seniors’ Resource Team, a satellite clinic of the BMHC, located at the Lanark County Mental Health (LCMH) center in Smiths Falls. Although operating mostly as community based consultation services, the primary goal of both outreach programs is to maintain the elderly in the community for as long as possible. Populations served include older persons with behavioural disturbances and/or mental health problems associated with neurodegenerative disorders, older persons with mental health problems complicated by age related medical illness or functional decline, older persons with late onset severe mental illness, older persons with substance misuse problems and mental illness, and persons under 65 years who have neurodegenerative disorders. Clinical work includes consultation to and collaboration with community partners, such as Family Physicians, community clinics, placement coordination services, retirement homes, and Long Term Care homes. Interdisciplinary team work involves collaboration and consultation with psychiatry, social work, occupational therapy, and nursing. Services are often delivered in the community, such as the client’s home, community clinics, or the client’s place of residence (e.g., retirement home or Long Term Care home). Resident Opportunities: Clinical assessment (including interviewing, psychodiagnostic, neuropsychological and personality assessments) Opportunities are available to engage in family counselling and individual treatment from a cognitive-behavioural framework Interdisciplinary team consultation and involvement (e.g., clinical team meetings and case conferences) Consulting and liaising with community partners Working within a rural collaborative care framework in Lanark Involvement with program evaluation and research projects When possible, Residents may supervise psychology practicum students The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 37 THE ROYAL’S PSYCHOLOGY RESIDENCY PROGRAM SUPERVISORY FACULTY AND ADDITIONAL PSYCHOLOGY STAFF Sarah Bertrim Program: Clinical Orientation: Ph.D., C. Psych. University of Windsor, 2008 Operational Stress Injury (OSI) Clinic, ROMHC Integrative approach with emphasis on cognitive behavioural, emotion focused, and experiential therapy. Special interest in clinical assessment, operational stress injuries, trauma, and rehabilitation psychology. Robert Bialik Program: Clinical Orientation: Ph.D., C. Psych., Carleton University, 1987 Operational Stress Injury (OSI) Clinic, ROMHC Emotion Focused, Cognitive-behavioural, and EMDR therapy, special interest in assessing and treating traumatic stress disorders. Michele Boivin Program: Clinical Orientation: Ph.D., C.Psych. University of Toronto, 2004 Operational Stress Injury (OSI) Clinic, ROMHC Individual and Group Cognitive-Behavioural Therapy for adolescents and adults. Special interest in evidence-based assessment and intervention for Posttraumatic Stress Disorder and other trauma-related symptoms, including mood and other anxiety disorders. Certified Supervisor and Trainer in Prolonged Exposure Therapy for PTSD. Professional Practice Leader, Psychology Discipline. Kelsey Collimore Program: Clinical Orientation: Ph.D., C.Psych., University of Regina, 2011 Mood Disorders Program, ROMHC Cognitive-behavioural. Special interest in evidence-based practice and empirically-supported therapies for anxiety and related disorders, mood disorders, and trauma. Kim Corace Program: Clinical Orientation: Ph.D., C. Psych., York University, 2008 Substance Use and Concurrent Disorders Program, ROMHC Assessment, consultation, individual and group psychotherapy, cognitive-behavioural therapy, motivational interviewing. Program development, evaluation, and research. Special interest in opioid addiction and concurrent mental illness, health psychology, stigma, HIV/Hepatitis C, treatment readiness and adherence, and health behavior change. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 38 Alison Davis Program: Clinical Orientation: M.A.. Psychology, Carleton University, 1997 Secure Treatment Unit, BMHC Cognitive-Behavioural. Assessment and treatment of mentally disordered offenders. Special interest in sex offender populations. Margaret DeCorte Program: Clinical Orientation: Ph.D., C. Psych., Ohio University, 1980 Youth Psychiatry Program, ROMHC Individual, group, and family therapy using CBT, IPT, ACT, EFT. Special interest in lifespan attachment patterns, brainbased psychotherapy, clinical applications of Buddhist psychology, anxiety disorders, OCD, and trauma. Hans de Groot Program: Clinical Orientation: Ph.D., C. Psych., Carleton University, 1992 Geriatric Psychiatry Program, ROMHC Cognitive assessment, differential diagnosis, and individual and group therapy using an ACT-enhanced cognitive-behavioural approach. Susan Farrell Program: Clinical Orientation: Ph.D., C. Psych., University of Ottawa, 2001 Community Mental Health Program, ROMHC & BMHC Assessment, differential diagnosis, treatment planning, consultation and evaluation, behaviour modification, cognitive behavioural therapy, systemic therapy. Kylie Francis Program: Clinical Orientation: Ph.D., C.Psych., Concordia University, 2011 Anxiety Disorders Program, ROMHC Assessment, treatment planning, individual and group psychotherapy for adults with anxiety disorders, trauma, mood disorders, and eating disorders. Therapeutic approach is Cognitive-Behavioural, with elements of emotion-focussed, motivational interviewing, and process-oriented therapies. Special interests in clinical supervision, progress monitoring, and practice-based research (PPRNet). Meagan Gallagher Ph.D., C.Psych. (Supervised Practice), University of Ottawa, 2013 Anxiety Disorders and Bridges Programs, ROMHC Individual, Group, and Family therapy for adults and adolescents. Clinical orientations include CBT, EFT, and DBT. Special interests in evidence-based assessment and intervention for Anxiety and OCD Spectrum Disorders, emotion regulation, attachment, and group psychotherapy. Program: Clinical Orientation: The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 39 Anik Gosselin Program: Clinical Orientation: Ph.D., C.Psych. University of Ottawa, 2006 Forensic Treatment Unit (FTU), BMHC Forensic Neuropsychology. Individual and Group CognitiveBehavioural Therapy for adults. Special interest in sleep disorders and their impact on behaviour within a forensic population, and in measuring/identifying neurophysiological aspects/markers of behaviour change associated with treatment of psychiatric conditions using evidence-based approaches. Diane Hoffman-Lacombe Program: Clinical Orientation: M.Ps, C. Psych., University of Ottawa, 1980 Forensic Treatment Unit – Ottawa, ROMHC Psychological assessment (cognitive & personality), risk assessment, individual & group therapy (cognitive-behavioural therapy, psycho-education) and program evaluation. Jemeen Horton Program: Clinical Orientation: Ph.D., C. Psych., Carleton University, 2007 Integrated Forensic Program, ROMHC Neuropsychology (Adults and Seniors) Andrew Jacobs Psy.D., C.Psych., Virginia Consortium Program in Clinical Psychology (College of William & Mary, Eastern Virginia Medical School, Norfolk State University, & Old Dominion University), 2007 Anxiety Disorders Program, ROMHC Behavioural therapy for anxiety and mood concerns with integration of cognitive and values-based strategies; motivational enhancement for treatment; sleep disorders; psychodiagnostic and personality assessment; program development and evaluation. Program: Clinical Orientation: Matthew Kerr Program: Clinical Orientation: Ph.D., C. Psych. University of Ottawa, 2010 Schizophrenia Program, ROMHC Individual and Group Cognitive-Behavioral Therapy (for psychosis), Acceptance and Commitment Therapy & Interpersonal Therapy. Special interest in PTSD, complex trauma, traumatic psychosis, and Dissociative Disorders. Psycho-diagnostic and cognitive assessments. Drew Kingston Program: Clinical Orientation: Ph.D., C. Psych., University of Ottawa, 2010 Secure Treatment Unit, BMHC Cognitive-behavioural interventions; individual and group psychotherapy. Special interest in the assessment and treatment of sexual offenders and other problematic sexual behaviors. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 40 Judy Makinen Program: Clinical Orientation: Ph.D., C. Psych., University of Ottawa, 2004 Youth Psychiatry Program, ROMHC; Individual, group, and marital/family therapy; Certified EFT Supervisor and Trainer, Formal Training in DBT, and familiar with Interpersonal & CBT approaches; psycho-education and psycho-diagnostic assessments; special interest in attachment, affect regulation, and trauma. Luis Oliver Program: Clinical Orientation: Ph.D., C. Psych. University of Ottawa, 2000 Operational Stress Injury (OSI) Clinic, ROMHC Integration of cognitive-behavioural, emotionfocused/experiential and interpersonal therapy. Special interest in trauma (PTSD) and anxiety, mood disorders, the role of spirituality and creativity in healing, and assessment. Christopher Prince Program: Clinical Orientation: Ph.D., C. Psych., Carleton University, 1990 Geriatric Community Outreach Teams, BMHC & Lanark SRT Neuropsychological and psychological assessment. Individual cognitive-behavioural therapy. Jeff Robinson Program: Clinical Orientation: MPsych (Forensic), Bond University 2008 Forensic Treatment Unit, BMHC. Integrative approach, including cognitive behavioural therapy with interests in individual and group treatment. Specializing in violent and aggressive behavior of mentally ill offenders. Michael Seto Program: Clinical Orientation: Ph.D., C.Psych., Queen's University, Psychology, 1997. Forensic Treatment Unit, BMHC Multi-systemic, cognitive-behavioral, risk/need/responsivity principles of intervention. Irit Sterner Program: Clinical Orientation: Ph.D., C. Psych., University of Ottawa, 1990 Mood Disorders Program, ROMHC Individual and group therapy. Personality and psychodiagnostic assessment. Integrative perspective in working with clients that includes Cognitive-Behavioural Therapies (including Schema Therapy, Dialectical Behaviour Therapy) and Experiential approaches. Special interest in mood disorders, posttraumatic stress disorder and borderline personality disorder. Angela Stewart Program: Clinical Orientation: Ph.D , C. Psych, University of Ottawa, 2007 Neuropsychology Unit, ROMHC Neuropsychological assessment. Maria Tsiakas Program: Clinical Orientation Ph.D., C. Psych., University of Ottawa 2007 Neuropsychology Service Neuropsychological assessments The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 41 INFORMATION FOR APPLICANTS Requirements: Applicants must have completed core requirements for the Doctoral degree such as required courses, comprehensive exams, approval of the dissertation proposal by the time of application, and permission from their Director of Training to begin a residency program. Ideally, applicants should also have completed data collection and analysis before commencing the Residency. To be considered, candidates must be enrolled in a recognized CPA-accredited doctoral Clinical Psychology program or equivalent. In keeping with CPA Accreditation Standards and Procedures, all applicants must have completed a minimum of 600 hours of supervised practicum training of which 300 hours are direct client contact and 150 hours are supervision. The program subscribes to the APPIC principles regarding preparation for internship in terms of the number and nature of practicum hours completed. Please note that applicants are not rated based on the “raw number of practicum hours” reported on APPIC applications forms; quality and depth of practicum training is more relevant than total quantity of hours. Applications from visible minorities and candidates with a disability are particularly encouraged. When reviewing and rating applications, we focus on “goodness of fit” to determine if an applicant has a clear and impressive plan for their residency and future career. We look at the level of breadth and/or depth of an applicant’s clinical experiences and if there is a focus on evidencebased practices to ensure that an applicant’s goals and previous experience are a good match with the Royal’s Psychology Residency Program. An applicant’s progress with his/her dissertation and timeline for completing the dissertation may be considered in the rating process. The Application Procedure: Applications will be considered complete when they include: AAPI online application Graduate transcripts Curriculum vitae Three letters of reference (please use the CCPPP form or the APPIC Standardized Reference Form for AAPI) Cover letter clearly stating clinical training interests, career goals, and rotation preferences (as pertinent to the track you are applying to)* * Please note: If you are applying to both tracks of The Royal’s Psychology Residency Program (Royal Ottawa Mental Health Centre and Brockville Mental Health Centre) please submit one application for both tracks with a separate cover letter for each track. Please submit the two cover letters (ROMHC and BMHC) in one document. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 42 The following are guidelines for submission of the cover letter(s) (re: rotation preferences): As part of your cover letter (for the ROMHC and/or BMHC track), please dedicate a paragraph to rank order the specific rotations in which you are interested. Please list your rotations in order of preference (e.g. first choice, second choice, third choice, etc.) in a clearly numbered list. Please include at minimum your top four rotation preferences. If you are interested in doing a secondary rotation in the other track (ROMHC or BMHC), please clearly indicate this as well. We will make every attempt to provide the successful applicant with his/her preferred rotations but cannot guarantee rotations due to supervisor availability and unanticipated program changes. Please note: Rotation interest indicated here may be revised post match day by the successful applicant based on the applicant’s interests and supervisor availability. Letters of recommendation should abide by the recommendations of the Canadian Council of Professional Psychology Programs (CCPPP) or The Association of Psychology Postdoctoral and Internship Centers (APPIC). Please refer to “CCPPP Form/Guidelines for Letters of recommendation to Canadian Pre-Doctoral Internship Settings.” (Note: Website address is www.ccppp.ca) or the APPIC Guidelines for Letters of Recommendation to Doctoral Internship Centers (Note: Website address is www.appic.org). This Residency program is participating in the APPIC Internship Matching Program, which places applicants into Psychology Residency positions. Our program adheres to APPIC guidelines. This Residency site agrees to abide by the APPIC policy that no person at this training facility will solicit, accept or use any ranking-related information from any Resident applicant. All applicants must register with the National Matching Services at www.natmatch.com/psychint and/or APPIC to be considered for this Residency. Our APPIC program code number is: 183911 for the 4 ROMHC Track positions and 183912 for the 1 BMHC Track position. The APPIC Application for Psychology Residency (AAPI) is available online at the APPIC website at www.appic.org. News and information about the AAPI Online, along with instructions about how to access the service, can be found at www.appic.org, click on "AAPI ONLINE." Completed applications must be received no later than November 1, 2014. All interview notifications are made on December 5, 2014. The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 43 Interviews of potential candidates for the ROMHC track will be held across five set days and interviews for the BMHC track will be held across two set days in January 2015. The schedule is as follows: 2015 INTERVIEW DATES ROMHC Track BMHC Track January 12 (Monday) January 14 (Wednesday) January 13 (Tuesday) January 20 (Tuesday) January 15 (Thursday) January 19 (Monday) January 21 (Wednesday) Arrangements for either on-site or telephone interviews will be made for January 2015. Those applicants chosen for an interview will be able to sign up for an interview date/time. Details of this process will be forwarded upon notification of an interview for selected applicants. After placements have been finalized in February 2015, Residents will be contacted regarding their specific interests in rotations and supervisors. Application material must be submitted via AAPI Online by November 1, 2014. Questions regarding our program and application requirements can be addressed to: Susan Farrell, Ph.D., C. Psych., Director of Clinical Training c/o Ms. Cathie Massel, Psychology Residency Administrative Assistant/Coordinator The Royal’s Psychology Residency Program Royal Ottawa Mental Health Centre 1145 Carling Ave, Room 1213 Ottawa, Ontario, K1Z 7K4 TEL: TEL: FAX: E-mail: 613-722-6521 ext. 7135 (Ms. Cathie Massel, Administrative Assistant, Psychology Residency Program) 613-722-6521 ext. 6922 (Dr. Susan Farrell, Director of Clinical Training) 613-761-3628 susan.farrell@theroyal.ca cathie.massel@theroyal.ca The Royal’s 2015-16 Psychology Residency Program Brochure Version Date: July 29, 2014 Page 44