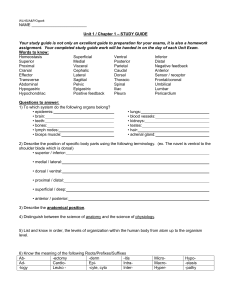
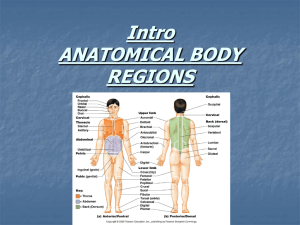
Block 2 Unit 3 Objectives
advertisement

© 2009 Mark Tuttle Organization of the Neck - Hankin 1. Describe the cervical fascia and compartments. a. Investing layer i. Surround the entire neck ii. Just deep to platysma m. anteriorly iii. Invests: 1. Trapezius m. 2. Sternocleidomastoid m. 3. Parotid gland 4. Submandibular gland b. Pretrachial layer i. Muscular 1. Invests Infrahyoid mm. ii. Visceral 1. Invests Trachea, including the buccopharyngeal membrane on the posterior aspect of the trachea 2. The Buccopharyngeal membrane invests the constrictor muscles of the pharynx 3. Thyroid 4. Parathyroid 5. Trachea 6. Pharynx 7. Esophagus c. Prevertebral layer i. Deep to the investing layer ii. Contains all the associated muscles of the vertebral column d. Carotid sheath i. Closely invests: 1. Common carotid aa. 2. Internal carotid a. 3. Jugular v. 4. Carotid sinus & body 5. Sympathetic fibers 6. Vagus n. 7. Deep cervical lnn. 2. Describe the cervical regions/triangles. a. What are their boundaries and contents? i. Lateral Cervical Region (Posterior Cervical Triangle) 1. Boundaries a. Anterior: SCM b. Posterior: Trapezius c. Inferior: Clavicle © 2009 Mark Tuttle d. Roof: Investing fascia 2. Deep to this you can see: a. Splenius capitus b. Lavator scapulae c. Middle/anterior scalene mm. 3. Contains a. Muscles i. Muscular floor ii. Splenius capitis iii. Levator scapulae iv. Middle scalene v. Posterior scalene vi. Omohyoid (inferior belly) b. Arteries i. Transverse cervical a. ii. Suprascapular a. iii. Subclavian a. (3rd part) iv. Occipital a. (part) c. Veins i. Subclavian v. 1. External jugular v. a. Transverse cervical v. b. Suprascapular v. c. Anterior jugular v. d. Nerves i. Accessory n. (CN XI) ii. Roots of brachial plexus iii. Suprascapular n. iv. Phrenic n. (C3-5) v. Cervical plexus (C1-4) – cutaneous branches (C2-4) (Come out at Herb’s Point) 1. Lesser occipital n. (C2) 2. Great auricular n. (C2-3) 3. Transverse cervical n. (C2-3) 4. Supraclavicular nn. (C3-4) 4. Divided into a. Occipital triangle (above omohyoid m. inferior belly) b. Omoclavicular (Subclavian) triangle (below the omohyoid m. inferior belly) ii. Anterior Cervical Region/Anterior Cervical Triangle 1. Boundaries a. Anterior: Anterior midline of neck © 2009 Mark Tuttle b. Posterior: SCM c. Superior: Mandible 2. Subdivisions a. Submental triangle (unpaired) i. Anterior belly of digastric mm. ii. Hyoid bone (in middle/inferior) b. Submandibular (digastric) triangle i. Anterior belly of digastric mm. ii. Posterior belly of digastrics mm. c. Carotid i. Omohyoid m. ii. Posterior belly of digastrics m. iii. SCM d. Muscular i. Omohyoid m. ii. SCM iii. Midline of neck 3. Subdivisions floor/contents a. Submental triangle i. Floor 1. Mylohyoid mm. ii. Contents 1. Submental lnn. 2. Small vv. (tributaries of anterior jugular v.) b. Submandibular (digastrics) triangles i. Floor 1. Mylohyoid m. 2. Hyoglossus m. 3. Middle pharyngeal constrictor m. ii. Submandibular gland iii. Submandibular lnn. iv. Mylohyoid m. v. Hypoglossal n. (CN XII) vi. Parts of facial artery & vein c. Carotid triangle i. Floor 1. Inferior pharyngeal constrictor m. ii. Contents 1. Common carotid a. 2. Internal carotid a. 3. External carotid a. 4. Carotid body & sinus © 2009 Mark Tuttle 5. Internal jugular v. 6. Deep cervical lnn. 7. Vagus n. (CN X) 8. Hypoglossal n. (CN XII) 9. Accessory n. (CN XI) 10. Branches of cervical plexus 11. Larynx 12. Pharynx 13. Thyroid & PT glands d. Muscular triangles i. Infrahyoid mm. ii. Thyroid & PT glands 3. What structures are found at the “key vertebral levels” in the neck? C3 Hygoid bone C4 Carotid bifurcation C4-5 Thyroid cartilage C5-6 Cricoid Cartilage (C6) Inferior limit of pharynx and larynx Superior limit of trachea and esophagus Indentation between cricoids cartilage and 1st tracheal ring C6-T1 Thyroid gland Muscles of the Neck 4. Describe the neck muscles. a. You should know their innervation, attachments, and primary actions i. OK © 2009 Mark Tuttle Endocrine 1: Hypophysis and Pineal - Chiaia 1. Describe the histology of the pituitary gland; include the infundibular stalk, the four main parts, and its embryology. a. Anterior Lobe (From oral ectoderm/Adenohyphosis/Ratke’s Pouch) i. Pars Distalis 1. Most anterior portion (75% of entire pituitary) 2. Dense cords of secretory epithelial cells 3. Supported by reticular fibers 4. Contains sinusoidal capillaries which are lined by fenestrated endothelial cells w/diaphragms ii. Pars Tuberalis 1. Wraps around the infundibular stalk to hold the two lobes together during development before they fuse 2. Arranged in short longitudinally oriented cords 3. Portal system corses through here on way to pars distalis 4. Mostly chromophils here (mostly gonadotrophs) iii. Pars Intermedia 1. In between the pars distalis and posterior lobe (pars nervosa) 2. Basophilic cells in lower mammals 3. In humans, chromophobic cells surrounding aggregates of colloid filled follicles called Ratke’s Cysts (maybe some basophils too) 4. Marked by an indentation called Rathke’s Cleft b. Posterior Lobe (From neural ectoderm/Neurohyphosis) i. Pars Nervosa 1. The posterior lobe 2. Does not contain secretory epithelial cells 3. Highly branched non secretory, glial-like cells called pituicytes whose processes end in close association to capillaries a. Thought to serve a nutritive function like glial cells in CNS 4. **Axon terminals w/Granules are diagnostic 5. **Vesicle bound hormones cause dilations of the axon terminals called Herring Bodies ii. Infundibulum 1. The stalk part of the posterior lobe 2. Identify chromophils and chromophobes of the pars distalis. Indicate which pituitary hormones are made by each, what are the functions of each hormone and what is the target organ, tissue or cell of each. a. Chromophils (50%) i. Acidophils (α cells, 40%) 1. Large, densely staining cells 2. Cytoplasm packed with small specific acidophilic staining granules 3. Types (Distinguished only immunocytochemically): © 2009 Mark Tuttle a. Somatotrophs i. Spherical to ovoid ii. Centrally located nucleus iii. Secretions: 1. Growth Hormone (chondrocyte growth ↑) a. Somatomedins (cartilage, mitosis ↑) 2. Somatotrophin b. Mammotrophs i. Concentrated in the posterolateral portion of Pars distalis ii. Secretions: 1. Prolactin (milk secretion, progesterone ↑, infertility in males) 4. Basophils (β cells, 10%) a. Larger than acidophils b. Cytoplasmic granules are smaller and less numerous c. Types (Distinguished only immunocytochemically): i. Thyrotrophs 1. Angular cells 2. Secretions: a. Thyroid Stimulating Hormone (TSH) (stimulates thyroxine (T4) and triiodothyronine (T3) from thyroid) ii. Gonadotrophs 1. Fusiform cells with eccentric nuclei 2. Contain varying sized secretory granules 3. **Located immediately adjacent to sinusoid 4. Secretions: a. Follicle stimulating hormone (FSH) - ABP in males, ovarian follicles in fem b. Leutinizing Hormone (LH) - androgen in males, progesterone/ovulation in females iii. Corticotrophs 1. Large ovoid cells with eccentric, indented nucleus 2. Produce a prohormone: Pro-opiomalanocortin 3. Secretions (Pro-opiomalanocortin products): a. Adrenocortocotropic Hormone (Glucocorticoids in adrenal cortex ↑) b. β endorphin (Pain) © 2009 Mark Tuttle c. Melanocyte Stimulating Hormone (Stimulates melanin synthesis) d. β Lipotropin (function unknown) b. Chromophobes (50%) i. Small round pale staining cells with little cytoplasm ii. Non-secretory iii. Few specific staining granules iv. Tumors here are common 3. Identify the components of the neurohypophysis a. Pars Nervosa i. Highly branched glial-like pituicites whose processes end in close association to capillaries. Serve a nutritive function. ii. No secretory epithelial cells iii. **Herring bodies diagnostic for vesicle bound hormones dilating the axon terminals b. Infundibulum i. Descending axons form the supraoptic and paraventricular nuclei of the hypothalamus gather in the infundibulum, collecting to form a tract called the hypothalamic-hypophyseal tract which terminates on the capillary plexus of the posterior lobe c. Median eminence i. Superior hypophyseal aa. (from internal carotid a.) anastomose here and form the fenestrated Primary Plexus ii. Small, unmyelinated neurons come down from the hypothalamus and terminate on the fenestrated Primary Plexus 4. Describe the two hormones that are liberated from the posterior lobe of the pituitary in terms of their origin, the hypothalamohypophyseal tract, their target organs, and their functions. a. Oxytocin i. Originates in paraventricular nucleus of hypothalamus ii. Induces contraction of myoepithelial cells of the mammary gland resulting in excretion of milk from the secretory alveoli b. Vasopressin i. Originiates in supraoptic nucleus ii. Promotes water absorption through the collecting tubules of the kidney iii. Increases blood pressure by promoting contraction of vascular smooth muscle resulting in increased peripheral resistance 5. Be able to describe the signals which trigger the release of pituitary hormoneds and their feedback regulation. a. First Order (oxytocin, vasopression) i. Neurohypophyseal (Posterior Pituitary) hormone (oxytocin, vasopression) feeds back on hypothalamus for negative feedback © 2009 Mark Tuttle b. Second Order (Growth Hormone, Prolactin) i. Hypothalamic releasing factor stimulates release of pituitary hormone which acts on peripheral target tissues ii. Plasma level of pituitary hormone feeds back to the hypothalamus or pituitary for negative feedback c. Third Order (Thyroid Stimulating Hormone, ACTH) i. Hypothalamic releasing factor stimulates release of pituitary hormone ii. Pituitary hormone stimulates peripheral target endocrine organ to secrete its own hormone iii. Level of peripheral target organ hormone feeds back to pituitary or hypothalamus for negative feedback 6. Describe the overall histology of the pineal gland and the hormones produced by the pineal gland. a. Flattened conical gland attached to midline of superior surface of the diencephalon of CNS b. Encapsulated by the CT of Pia of the CNS which penetrates the parenchyma as trabechulae c. Cell types i. Pinealocytes 1. Basophilic cytoplasm with long cytoplasmic processes which end in bulb-like expansions in close proximity to capillaries 2. Small dense core vesicles similar to those in catacholaminergic neurons 3. Large oval nucleus and **clearly distinguishable nucleoli 4. Secrete Melatonin a. Released during dark cycle (inhibited by light) b. Radical scavenger and anti-oxidant c. May inhibit growth of some tumors d. May be involved in Seasonal affected disorder e. Helps regulate bio-rhythms ii. Glial cells 1. Resemble astrocytes of the CNS both structurally and immunocytochemically 2. **Brain sand: small aggregates of calcium phosphate and calcium carbonate. Radiopaque. © 2009 Mark Tuttle Nerves And Vessels of the Neck - Hankin Blood Vessels 1. Describe the venous drainage of the neck. a. External jugular v. (Drains into subclavian v.) i. Retromandibular v. 1. Superficial temporal v. 2. Maxillary v. a. Pterygoid venous plexus (deep to mandible) ii. Posterior auricular v. iii. Anterior jugular v. (somewhat inconsistent) iv. Transverse cervical v. v. Suprascapular v. b. Internal jugular v. (Unites with subclavian v. and becomes brachiocephalic v.) i. Continuation of sigmoid sinus (dural venous isnus) ii. Inferior petrosal sinus (dural venus sinus) iii. Occipital v. iv. Pharyngeal vv. v. Common facial v. vi. Lingual v. vii. Superior/Middle thyroid v. viii. Infeior bulb of Internal Jugular V. (Contains a bicuspid valve) c. What is the relationship between the internal jugular vein and the carotid sheath? i. The internal jugular v. is within the carotid sheath d. Where is the external jugular vein located? i. Superficial fascia ii. Crosses superficial and oblique to SCM iii. Empties into the subclavian v. just deep/inferior to the base of SCM 2. Describe the branches of the external carotid artery. a. Superficial temporal a. b. Maxillary a. c. Posterior auricular a. d. Occipital a. e. Ascending pharyngeal a. f. Facial a. g. Lingual a. h. Superior thyroid a. i. Are there branches of the internal carotid artery in the neck? i. NO 3. Describe the carotid body and carotid sinus. a. Carotid sinus i. Located at the dilation of the bifurcation of carotid a. ii. Usually associated with external carotid, but can be on common carotid a. © 2009 Mark Tuttle iii. Contains Baroreceptors iv. Reacts to blood pressure by decreasing heart rate via the afferent loop of the Glossopharyngeal n. (CN IX) AND vagus n. (CN X) AND cervical sympathetic nn. (probably have opposite effect) b. Carotid body i. Ovoid mass at bifurcation ii. Contains Chemoreceptors iii. Senses low blood O2 or high CO2, reacts by increasing rate & depth of respiration, cardiac rate & bp iv. Innervated by the afferent loop of the glossopharyngeal n. (CN IX) AND vagus n. (CN X) AND cervical sympathetic nn. Nerves and Plexuses 4. Describe the cervical and branchial plexuses in the neck. a. Cervical plexus (ventral rami C1-C4) i. Motor nerves 1. Superior root of ansa cervicalis (C1) a. Runs with hypoglossal n. (CN XII: tongue) b. Also runs with thyrohyoidn. And geniohyoid n. 2. Ansa cervicalis (Goose Neck) is on the carotid sheath a. Sternohyoid m. b. Omohyoid m. c. Sternothyroid m. 3. Inferior root of ansa cervicalis (C2-3) 4. Other direct branches a. Deep neck mm. ii. Cutaneous nerves, ansa cervicalis (C1-3), and phrenic nerve (C3-5) iii. Ventral Rami: Innervate skin of anterior and lateral neck 1. Lesser occipital n. (C2) Neck & scalp posterosuperior to auricle 2. Great auricular n. (C2-3) Skin over parotid gland, posterior aspect of auricle between angle of mandible & mastoid pr 3. Transverse cervical n. (C2-3) Anterior cervical region 4. Supraclavicular nn. (C3-4) Neck and shoulder 5. Brachial plexus (C5) iv. Dorsal rami: Innervate skin on posterior head and neck. 1. Suboccipital n. (C1) 2. Greater occipital n. (C2) 3. Third occipital n. (C3) b. Brachial plexus (ventral rami C5-T1) i. See Unit 1 5. Describe the cranial nerves that course through and/or supply the neck. a. Glossopharyngeal nerve (CN IX) © 2009 Mark Tuttle i. Afferent from tongue and pharynx ii. Efferent to stylopharyngeus & parotid gland 1. CN IX runs to otic ganglion before going to parotid b. Vagus nerve (CN X) i. Sensory 1. Inferior pharynx 2. Larynx 3. Thoracic and abdominal organs 4. Taste a. Root of tongue and epiglottis ii. Motor 1. Soft palate 2. Pharynx 3. Intrinsic laryngeal mm. 4. Palatoglossus iii. Parasymp 1. Thoracic & abdominal organs iv. Superior (Jugular) ganglion: General sensory v. Inferior (Nodose) ganglion: Visceral sensory c. Accessory nerve (CN XI) i. Not really a cranial n. since its spinal component immediately joins the vagus and becomes indistinguishable. Both excit via the jugular foramen ii. Motor 1. SCM 2. Trapezius d. Hypoglossal nerve (CN XII) i. Runs with the thyrohyoid n. and geniohyoid n. as well as the superior root of ansa cervicalis (all C1) ii. Innervates the tongue except for pataloglossus m. iii. Spirals behind the vagus nerve and passes between the internal carotid artery and internal jugular vein lying on the carotid sheath. After passing deep to the posterior belly of the digastric muscle, it passes to the submandibular region to enter the tongue. 6. Describe the cervical sympathetic trunk, its ganglia, and branches. a. Superior cervical ganglion (@ C1-2) i. Large ganglion posterior to Internal Carotid A. ii. Postsynaptic fibers 1. ICA plexus enters cranial cavity to supply cranial vasculature and other structures (ex. Iris of eye) 2. Contributes fibers to external carotid a. plexus 3. Gray rami to C1-4 spinal n. to cervical plexus 4. Superior cervical cardiac n. to heart © 2009 Mark Tuttle b. Middle cervical ganglion (@ C6) i. Smallest cervical ganglion (occasionally absent) ii. Anterior or superior to inferior thyroid a. iii. Postsynaptic fibers 1. Gray rami to C5&6 spinal nn. to brachial plexus 2. Forms periarterial plexuses to thyroid gland 3. Middle cervical cardiac n. to heart c. Inferior cervical ganglion (@ C7) i. Usually (80%) fused with T1 ganglion to form stellate (cervicothoracic ganglion) ii. Postsynaptic fibers 1. Gray rami to C7-T1 spinal nn. to brachial plexus 2. Inferior cervical cardiac n. to deep cardiac plexus 3. Forms plexus on vertebral a. to cranial cavity © 2009 Mark Tuttle Root of the Neck – Hankin Lymphatics in the Head and Neck 1. Define the major groups of lymph nodes found in the neck? a. From superficial to deepcervical lnn. b. Drains into supraclavicular lnn. (usually) i. Accompanies transverse cervical a. c. Usually on the carotid sheath, not inside d. Drain into jugular lymphatic trunks formed by e. The left jugular lymphatic trunk joins the thoracic duct f. The right jugular lymphatic trunk joins the venous system at the right venous angle g. The thoracic duct empties into the left venous angle (where subclavian/jugular vv. meet) h. How is lymph returned to the venous system in the root of the neck? i. See above. Root of the Neck 2. Describe the thyrocervical trunk. a. 3. Describe the anatomical relationship between the subclavian vessels, brachial plexus, and scalene muscles? a. Anterior b. Clavicle c. Subclavian v. d. Anterior scalene m. (w/phrenic n & thyrocervical trunk crossing) e. Subclavian a. f. Brachial plexus g. Middle scalene m. h. Posterior 4. Describe the root of the neck, including its boundaries, contents, and important anatomical relationships? a. Boundaries i. Lateral: Rib 1 ii. Anterior: Manubrium iii. Posterior: T1 vertebral body 5. Describe the relationship between the scalene muscles (especially anterior and middle) and the major vessels and nerves in the root of the neck? a. Superficial fascia b. Corotid sheath i. CCA ii. IJV iii. Vagus n. c. Phrenic n. © 2009 Mark Tuttle d. Anterior Scalene m. e. Brachial plexus 6. Describe the branches of the subclavian artery. a. First part (Medial to anterior scalene m.) i. Vertebral a. (Skips C7 vertebral foramen) ii. Internal thoracic a. iii. Thyrocervical trunk (posterior to transverse process) 1. Inferior thyroid a. 2. Ascending cervical a. 3. Suprascapular a. (may arise from subclavian directly) 4. Superficial (transverse) cervical a. b. Second part (Posterior to anterior scalene) i. Costocervical trunk 1. Supreme (superior) intercostal 2. Deep cervical a. c. Third part (Lateral to anterior scalene m.) i. Dorsal scapular a. 1. 75% direct branch of 2nd or 3rd part of subclavian 2. 25% deep branch of transverse cervical 7. What is the relationship between the subclavian vein, the clavicle, and the first rib? a. Clavicle – anterior b. Subclavian vein –middle c. 1st rib – posterior © 2009 Mark Tuttle The Skull and Cranial Vault – CBC 1. The Skull a. Identify the major bony landmarks visible from the anterior, lateral, and superior views of the skull. b. Anterior i. Frontal bone (1) 1. Glabella: Space between eyebrows 2. Naision: Junction between frontal/nasal bones 3. Superciliary arch: Just beneath eyebrow 4. Supra-orbital margin: Junction of eye socket 5. Supra-orbital notch: At edge of eye socket. Transmits supraorbital n+a+v ii. Maxilla bones (2) 1. Body: Cheek area 2. Infra-orbital margin: Bottom edge of eye socket 3. Infra-orbital notch: Transmits infraorbital n+a+v 4. Alveolar process: Bony region supporting upper teeth iii. Zygomatic bones (2) 1. Temporal process: part which extends toward temporal bone iv. Nasal bones (2) 1. Meets frontal bone @ naison v. Mandible 1. Mental foramen: Transmits mental n+a+v 2. Alveolar process: Bony region supporting lower teeth c. Lateral i. Parietal ii. Temporal 1. Squamous portion: Flat portion centrally located 2. Petrous portion: Goes into cranial vault (internal) Contains internal auditory meatus Transmits CN VII + VIII 3. Mastoid portion: Mastoid process is here 4. Tympanic portion: Contains external auditory meatus iii. Sphenoid – mostly internal. Pokes out by temple iv. Pterion 1. Where frontal, parietal sphenoid, temporal bones meet 2. Middle meningeal a+v run deep to this 3. One of the thinnest parts of the skull 4. Truama here can rupture that a + damage the brain d. Superior i. Bregma (important brain tissue landmark) 1. Meeting of corners of parietal + frontal bones e. Posterior © 2009 Mark Tuttle i. Lambda (important brain tissue landmark) 1. Meeting of the corners of parietal + occipital bones ii. Occipital 1. External occipital protuberance f. Identify certain areas of the skull more vulnerable to injury than others. i. Pterion 1. Where frontal, parietal sphenoid, temporal bones meet 2. Middle meningeal a+v run deep to this 3. One of the thinnest parts of the skull 4. Truama here can rupture that a + damage the brain ii. Fontanelles 1. Membranous sites between the corners of the bones of the skull where there is incomplete closure of the sutures at birth (should close 12-18 months) g. Identify the sutures and their location. Understand the importance and relevance of these sutures in the adult and newborn. i. Saggital suture: Interparietal suture ii. Coronal suture: Between parietal bones + frontal bone iii. Lambdoid suture: Occipito-parietal. Looks like lambda iv. Bregma: h. Describe the relationship of vessels, nerves and soft tissues as they relate to the bony skull and its foramina and fissures. i. Pterion: Middle meningeal a+v just deep to here ii. Supraorbital notch: Supraorbital n+a+v iii. Infraorbital notch: Infraorbital n+a+v iv. Mental foramen: Mental n+a+v v. Jugular foramen: CN IX, X, XI vi. Cribiform plate: CN I (Olfactory) vii. Foramen spinosum 1. Parietal trunk of the middle meningeal artery 2. Recurrent branch, the nervus spinosus, from the mandibular nerve (third branch (V3) of the trigeminal nerve) 3. Posterior trunk of the middle meningeal vein 2. The Cranial Vault (internal aspect of the skull) a. Identify the essential parts of the anterior, middle and posterior cranial fossae. i. Anterior 1. Frontal bone 2. Ethmoid bone 3. Sphenoid bone 4. Crista galli: attachment of dura – Falx Ceribri 5. Cribiform plate: transmit CN I (olfactory) ii. Middle © 2009 Mark Tuttle 1. Sphenoid bone 2. Temporal bone 3. Has openings for 5 CNs 4. Hypophysial fossa is here (contains pituitary) 3. The calvaria (skull cap) a. Describe the composition of the bones of the calvaria. i. frontal bone ii. parietal bones (two) iii. temporal bones (two) iv. occipital bone b. What are diploic veins? What is their clinical significance? i. Diploic veins originate in the diploe of the skull bones and drain down into the dural venous sinuses through the inner compact bone ii. They have no valves iii. Lesions/cancer has direct access to meninges/cranial vault iv. Four main diploic vv: 1. Frontal diploic v. 2. Anterior temporal diploic v. 3. Posterior temporal diploic v. 4. Occipital diploic v. 4. Cranial Meninges a. Define the cranial meninges. Describe the relationship of the meninges to the internal surface of the skull. Describe the formation of a dural fold. i. Pia mater: Continuous with brain ii. Arachnoid mater: Continuous with dural layers iii. Inner Dura mater: Continuous with arachnoid mater Forms dural folds and Intracranial venous structures (ex. Superior saggital sinus) iv. Outter dura mater: Endocranium. Periosteal layer b. What is a dural sinus? How are they named? Describe how they usually drain. i. When the periostial dura seperates from the meningeal dura and form an endothelially-lined space ii. No valves iii. They should drain into the internal jugular vein c. What is the primary blood supply to the cranial dura? i. Middle meningeal a. 1. Goes through foramen spinosum 2. Branch of maxillary a. (ECA) 3. Just deep to the pterion (point of confluence of parietal, temporal, sphenoid, frontal bones) 4. No epidural space here, so it invaginates into bone © 2009 Mark Tuttle 5. Can get an epidural hematoma, forcing periosteal layer of dura away + compressing the brain ii. a © 2009 Mark Tuttle Introduction to Cranial Nerves – CBC 1. Review the definition and characteristics of a cranial nerve. a. Arise directly from the brain, not the spinal cord (exception: CN XI somatic motor) b. Afferent from the skin of the face & scalp c. Travel through named foramina d. Can be mixed, motor, sensory, autonomic (PARASYMP ONLY) 2. Review the components of a spinal nerve; describe the components of cranial nerves. a. Efferent i. General somatic efferent (GSE) 1. Skeletal mm of head, neck, body wall 2. From SOMITES ii. Special visceral efferent (SVE) 1. Skeletal mm of head, neck, body wall 2. From PHARYNGEAL ARCHES 3. Not autonomic. Somatic. iii. General visceral efferent (GVE) 1. Smooth muscle, cardiac muscle, glands 2. Autonomic 3. Parasympathetic ONLY b. Afferent i. General somatic afferent (GSA) 1. Pain, touch, temp, proprioception from skin + structures of head, neck, body ii. General visceral afferent (GVA) 1. Neither parasympathetic nor sympathetic 2. Convey sensory info form viscera iii. Special somatic afferent (SSA) 1. Vision, hearing, balance iv. Special visceral afferent (SVA) 1. Small, taste 3. Name the twelve cranial nerves. a. CN I: Olfactory b. CN II: Optic c. CN III: Oculomotor d. CN IV: Trochlear e. CN V: Trigeminal i. V1: Opthalamic ii. V2: Maxillary iii. V3: Mandibular f. CN VI: Abducens g. CN VII: Facial h. CN VIII: Vestibulochoclear © 2009 Mark Tuttle i. CN IX: Glossopharyngeal j. CN X: Vagus k. CN XI: Accessory l. CN XII: Hypoglossal 4. For each cranial nerve identify functional components and relative position in cranial vault. a. CN I: Olfactory i. Pass through cribiform plate in the ethmoid bone to reach In nasal cavity b. CN II: Optic i. Most anterior ii. Run from the eyes to the base of the diencephalon to form the optic chiasm, before dividing into two optic tracts c. CN III: Oculomotor i. Just posterior to optic d. CN IV: Trochlear i. Emerges from posterior surface of brainstem near midline, courses anteriorly around the cerebral peduncle e. CN V: Trigeminal i. Exits from the middle cranial fossa ii. V1: Opthalamic 1. Enters orbit through superior orbital fissure iii. V2: Maxillary 1. Enters pterygopalatine fossa through foramen rotundum iv. V3: Mandibular 1. Passes through foramen ovale to inferior surface of base of the skull f. CN VI: Abducens i. Follows a long extradural path ii. Sensitive to damage via meningitis/subarachnoid hemorrhage g. CN VII: Facial i. Emerges in the cerebellopontine angle between the pons and olive ii. Passes through the internal acoustic meatus into the temporal bone where it divides h. CN VIII: Vestibulochoclear i. Pass from the inner ear through the internal acoustic meatus to the cerebellopontine angle, where it enters the brain i. CN IX: Glossopharyngeal i. Emerges from the medulla oblongata ii. Leaves cranial cavity through the jugular foramen j. CN X: Vagus i. Emerges from the medulla oblongata ii. Leaves the cranial cavity through the jugular foramen k. CN XI: Accessory © 2009 Mark Tuttle i. Spinal root emerges fro mthe spinal cord and passes superiorly entering the skull through the foramen magnum where it joins the cranial root from the medulla oblongata ii. Both roots leave the skull through the jugular foramen l. CN XII: Hypoglossal i. Emerges from the medulla oblongata, leaves the cranial cavity through the hypoglossal canal and descends laterally to the vagus n. ii. Enters the root of the tongue above the hyoid bone 5. Name and describe ganglia that are associated with the cranial nerves. a. Do later 6. Be able to differentiate between sensory ganglia and autonomic ganglia. a. Do later © 2009 Mark Tuttle Endocrine 2: Pancreas, Adrenals – Chiaia 1. Describe the histology of the thyroid gland. a. Parenchyma enclosed by outer dense irregular CT b. Thin inner CT capsule i. Penetrates the lobe into poorly delimited lobules c. Lobules i. Spherical cyst-like follicles ii. Simple cuboidal follicular epithelium iii. Each follicle has thin basal lamina supported by reticular fibers iv. Fenestrated capillaries w/lymphatic vessels v. Center of follicle: colloid (stored product d. Cell types i. Follicular epithelial cells (Principle cells) 1. Arranged in a ring around follicle 2. Cytoplasm is slightly basophilic 3. Round, centrally-located nucleus 4. Morphology (usually simple cuboidal) a. Hyperactive: Columnar (high columnar), colloid reduced b. Hypoactive: Squamous, colloid is increased ii. Parafollicular cells (C-cells) 1. Secondary regulation of Ca2+ in body 2. Describe the function of thyroid follicular cells and the synthesis storage and secretion of thyroid hormone. a. Make thyroid hormone (TH) b. Make glycoprotein thyroglobulin in rER of follicular cell c. Tyrosine added d. Exocytosed into lumen e. Thyroperoxidase is secreted into lumen and catalyzes iodinization close to the microvilli f. Iodine pump sequesters iodine from blood through basal lamina g. Stored in lumen as iodinated thyroglobulin h. Reuptake of iodinated thyroglobulin as colloid droplet i. Lysosomal digestion to form one of the T3, T4, MIT, DIT molecules j. T3/T4 diffuse out of basal surface and enter circulation where they are bound to carrier proteins 3. Describe and identify the parafollicular (C-cells) a. secrete Calcitonin b. Less numerous than Principle cells c. Neural crest origin d. Lighter staining and larger than follicular cells e. Spherical, centrally-located nucleus f. Invested in same basement membrane as principle cells, but insulated from the lumen (and the colloid) by thin cytoplasmic extensions of the follicular cells © 2009 Mark Tuttle 4. Describe and identify the histology of the parathyroid glands. Distinguish the chief (principal) cell from the oxyphil cell. a. Principle cell (Chief cell) i. Small ii. Centrally-located nucleus iii. Clear staining cytoplasm when inactive iv. Dark cells are active PT-secreting v. Well developed golgi vi. Secretory granules are less numerous than in other endocrine cells since chief cells do not store large quantities of PTH b. Oxyphil cell i. Less numerous ii. Larger iii. Small, dark staining nuclei iv. Acidophillic v. Unknown function vi. **Bag of mitochondria 5. Describe the overall histology of the adrenal gland, its blood supply, and the embryological origin of each region. a. Histology i. Cortex (80%) 1. Secretory epithelium supported by reticular fibers 2. Encapsulated by a thick fibroelastic CT a. Trabeculae penetrate the tissue and carry nerves and bv’s 3. Zona Glomerulosa (15%) a. Small pyramidal or columnar cells arranged in spherical aggregates surrounded by capillaries b. Large, deeply staining spherical nuclei c. Homogeneously staining cytoplasm d. Well developed smooth ER e. Numerous mitochondria w/lamellar cristae f. Secretions: i. Mineralcorticoids 1. Aldosterone 2. Deoxycorticosterone 4. Zona Fasciculata (78%) a. Thickest zone b. Radially oriented cords of secretory epithelium c. Centrally located vesicular nuclei d. Can be bi-nucleated e. Lightly basophilic f. Numerous lipid droplets © 2009 Mark Tuttle i. Fatty acids, cholesterol, neutral fat g. Short microvilli that extend into the capillary sinusoids h. Numerous mitochondria i. Secretions: i. Glucocorticoids 1. Cortisol 2. (Cortisone, corticosterone) 5. Zona reticularis (7%) a. Secretory epithelium b. Irregularly anastomosing cords separated by sinusoids c. Smaller than those of fasciculate d. Deeply staining nuclei e. Few lipid droplets evident f. Numerous secondary lysosomes and lipofuscin pigment granules g. Secretions: i. Small amounts of cortisol ii. Weak androgens ii. Medulla (20%) 1. Chromaffin cells a. Arranged in irregular clumps or cords between wide fenestrated capillaries b. Supported by reticular fibers c. Derived from NEURAL CREST d. Like neurons which have lost their axonal and dendritic processes and just function as secretory cells e. Contain dense core secretory granules f. Types i. Epinepherine cells (80%) 1. Round moderately electron dense granules which fill the vesicles 2. Clustered around adrenal sinusoids ii. Norepinephrine cells (20%) 1. Flattened or ovoid granules with eccentrically located high electron dense core surrounded by a less electron dense ring 2. Cluster around adrenal arterioles b. Embryology i. Cortex - Mesoderm ii. Medulla – Ectoderm (Neural crest) c. Blood supply i. Arising from the superior, middle or inferior suprarenal aa. ii. Branch in the outer capsule to form the Capsular aa. © 2009 Mark Tuttle iii. After piercing parenchyma, form Cortical arterioles iv. Form the cortical plexus in the capsule and the Zona Glomerulosa v. Form cortical sinusoids in Zona Fasciculata vi. Lead to medullary arterioles vii. Supply the capillary plexus of the medulla 6. Describe the three zones of the adrenal cortex, their constituent cells, and substances produced by the cells in each zone. a. See above 7. Describe the functions of each hormone secreted by the adrenal gland and the clinical disorders associated with each. a. Glucocorticoids (Cortisol, cortisone, corticosterone) i. Secreted in Zona Fasciculata ii. Functions 1. Down regulation of immune response by inhibition of lymphocyte production and turnover 2. Modulation of carbohydrate metabolism by promoting the formation of glucose from protein 3. Suppression of inflammatory response by decreasing production of T-cells and plasma cells iii. Associated Pathologies 1. Addison’s disease (Hypoadrenalism) a. Primary hypoadrenalism: idiopathic atrophy of the adrenal cortex b. Weakness and drowsiness due to low blood glucose (glucocorticoids) c. Increased ACTH secretion d. Decreased blood pressure due to decreased extracellular fluid volume (mineralcorticoids) 2. Cushing’s Disease (Hyperadrenalism) a. Excessive synthetic glucocorticoid use or from tumors b. Redistribution of fat around head, neck, face – Moon face c. Thinning of skin and loss of fat in the hypodermis causes underlying blood vessels to show through d. Hyperglycemia b. Mineralcorticoids (Aldosterone, Deoxycortocosterone) i. Secreted by Zona Glomerulosa of adrenal cortex ii. Functions 1. Resorption of Na+ from distal convoluted tubule of the kidney and sweat glands, salivary glands iii. Associated pathologies 1. See Addison’s disease c. Gonadal Steroids i. Secreted in Zona Reticularis of cortex © 2009 Mark Tuttle ii. Not stored, just continuously secreted iii. Effects similar to those secreted by testis d. Catecholamines i. Made in adrenal medulla ii. Usually not significant amounts made iii. Functions 1. Elevate plasma glucose levels (stimulate glycogenolysis) 2. Increase blood pressure and cardiac output 3. Dilation of coronary and skeletal muscle blood vessels 4. Cutaneous vasoconstriction iv. Associated Pathologies 1. Tumors of adrenal medulla a. Precocious development of sex organs b. Secondary sex characteristics 2. Adrenogenital Syndrome (Females ONLY) a. Androgenization of genitalia b. Development of male secondary sex characteristics c. Pseudohermaphroditism in extreme cases 8. Describe the organization of the adrenal medulla and it’s constituent cells. a. See #5 9. Indicate which cells of the adrenal medulla secrete hormones, and identify the hormones secreted by each. a. See #5 10. Identify the endocrine component of the pancreas, the specific hormone producing cells and the functions of each hormone. a. Islets of Langerhans i. Alpha Cells (20%) [α cells] 1. Large cells 2. Located at periphery 3. Numerous cytoplasmic granules with accentrically placed electron dense core 4. Secrete glucagon (raise blood glucose) ii. Beta Cells (70%) [β cells] 1. Small cells 2. Most numerous 3. Tend to be concentrated at the center of islets 4. Electron dense core surrounded by less dense matrix 5. Secrete Insulin (promote uptake of glucose into cells & glucose->glycogen in liver) iii. Delta cells (5%) [Δ cells] 1. Larger than alpha and beta cells 2. Lightly electron dense secretory vesicles of varying size © 2009 Mark Tuttle 3. Secrete somatostatin a. Both a neurotransmitter and a neurohormone b. In hypothalamus: growth hormone release c. In pancreas: paracrine function – glucagon & insulin ↑ iv. F-Cells (5%) 1. Secretes pancreatic polypeptide a. Stimulate release of gastric secretions in the gut b. Inhibit bile secretion in the gall bladder v. G-cells 1. Only present during maturation 2. Secrete Gastrin a. Increase HCl secretion by stomach parietal cells b. Increase gastric motility © 2009 Mark Tuttle Scalp and Face – CBC 1. List the layers of the scalp. Give the importance of each of these layers. a. Skin b. Connective Tissue i. Dense. BV’s and nerves here ii. Barrier for infection iii. Causes BV’s to stay open even when lacerations occur c. Aponeurosis i. Between anterior and posterior muscle bellies of occipitofrontalis m. d. Loose areolar CT i. The overlying 3 layers are fused - Allows scalping to occur e. Pericranium i. NOT endocranial periostial dura 2. Describe the blood supply and innervation to the scalp. What is the clinical significance of the arrangement? a. Blood supply i. Internal carotid (Anterior portion) 1. Opthalmic a. a. Supratrochlear a. b. Supraorbital a. ii. External carotid (Lateral and posterior portion) 1. Superficial temporal a. 2. Posterior auricular a. 3. Occipital a. b. Innervation i. Cranial nerves 1. Supratrochlear n. (CN V1): Just very front of top scalp 2. Supraorbital n. (CN V1): Top of scalp to vertex 3. Zygomaticotemporal n. (CN V2): Lateral scalp 4. Auriculotemporal n. (CN V3): Lateral scalp ii. Ventral rami 1. Lesser occipital n. (C2-3): Lateral scalp iii. Dorsal rami 1. Great occipital n. (C2): Posterior scalp 2. Third occipital n. (C3): Posteriomedial scalp c. Clinical significance i. Venous drainage goes mainly to the jugulars, but lesser so via the emissary veins 3. Review on your own the major bones of the face. a. Nasal (2) b. Maxilla (1-2) c. Mandible (1) d. Zygomatic (2) © 2009 Mark Tuttle e. Lacromal (2) f. Vomer (1) (nasal septum) *can’t be seen g. Palatine (2) (hard palate) *can’t be seen h. Inferior Nasal Conchi (2) (lateral nasal wall) i. Ethmoid (1) (nasal cavity: septum, sinuses, etc) *Can’t be seen 4. Describe the sensory innervation and blood supply to the skin of the face. a. Sensory innervation i. Ophthalmic n. (CN V1): Most of medial forehead and nose 1. Supratrochlear n. 2. Supraorbital n. 3. Lacrimal n. 4. Infratrochlear n. 5. External nasal n. ii. Maxillary n. (CN V2): Cheek and part of side of head 1. Infraorbital n. 2. Zygomatico facial n. 3. Zygomatico temporal n. iii. Mandibular n. (CN V3): Mandible and lateral forehead 1. Mental n. 2. Bucco n. 3. Auricular temporal n. b. Blood supply i. External carotid a. 1. Facial a. a. Angular a. b. Superior labial a. c. Inferior labial a. d. Submental a. 2. Superficial temporal a. a. Transverse facial a. ii. Internal carotid a. 1. Opthalmic a. a. Supraorbital a. b. Supratrochlear a. c. Venous drainage i. Dural sinus 1. Supraoribital v. 2. Supratrochlear v. 3. Angular v. via optic to dural sinus 4. Deep facial v. to Pterygoid plexus to dural ii. Jugular vein (could be anterior, external, internal) 1. Facial v. (no valves!) © 2009 Mark Tuttle 5. 6. 7. 8. 2. Superficial temporal v. Explain the clinical significance of the “danger triangle” of the face. a. Blood here is likely to drain into the dural sinus b. Pimple, boil, infection in this region can take this to the brain and cause: i. Encephalitis ii. Thrombus iii. Meningitis Describe the organization of the skin of the face, list the major muscles and give their action and innervation. a. All innervated by Facial N. CN VII b. Occipitofrontalis m. c. Orbicularis occuli m. Close eye d. Zygomaticus major m. Draw up corner of mouth, smile e. Zygomaticus minor m. f. Orbicularis oris m. Purse lips g. Levator labiae superioris m. h. Levator anguli oris m. i. Depressor labiae inferioris m. j. Depressor anguli inferioris m. k. Buccinator m. Force against resistance in mouth, sucking l. Platysma m. m. Occipitofrontalis m. Wrinkle forehead, raise eyebrow Discuss the consequences of interrupting CN V or CN VII innervation to the face. a. CN V: Trigemminal i. Would result in loss of sensory innervation of face b. CN VII: Facial i. Would result in paralysis of facial muscles ii. Bell’s Palsy 1. Usually temporary (duration can be days, months, years) 2. Can be caused by trauma or middle ear in fection 3. Can’t close eye 4. Can’t blink – fail to move tears across eye and can get corneal lacerations Describe the location of the parotid gland. a. Just anterior-inferior to the ear b. Superficial to/contains: i. Facial n. 1. Temporal branch 2. Zygomatic branch 3. Buccal branch 4. Marginal mendibular branch 5. Cervical branch ii. ECA -> superficial temporal a. © 2009 Mark Tuttle iii. Retromandibular v. iv. Auricular temporal n. (Branch of CN V3) c. The parotid duct pierces the buccinators muscle 9. Give the relationships of the parotid gland to the surrounding structures. SEE #8 10. Describe the nerve and vascular supply to the gland. See #8 © 2009 Mark Tuttle Super and Infratemporal fossa – CBC 1. Define the temporal fossa. a. Shallow depression on the side of the skull bounded by the temporal lines and terminating below the level of the zygomatic arch 2. What are the contents of the temporal fossa? a. Temporalis m. 3. How do you define the infratemporal fossa? a. An irregular shaped space inferior to the zygomatic arch and posterior to the maxilla and deep to the ramus of the mandible b. Do the temporal and infratemporal fossae communicate? i. Yes, just deep to the zygomatic process 4. What are the contents of the infratemporal fossae? a. Portions of the mm. of mastication i. Temporalis m. ii. Masseter m. iii. Medial pterygoid m. iv. Lateral pterygoid m. b. Branches of the maxillary a. i. Middle meningeal a. ii. Accessory meningeal a. iii. Inferior alveolar a. iv. Deep temporal aa. v. Posterior superior alveolar c. Pterygoid plexus of veins d. Branches of CN V3:Mandibular i. Motor branches 1. Branch to the mm of mastication 2. Branch to tensor mm. 3. N. to myohyloid 4. Branch to the anterior belly of the digastrics ii. Sensory branches 1. Auriculotemporal n. 2. Inferior alveolar n. 3. Lingual n. 4. Buccal n. e. What foramina are associated with the infratemporal fossa? i. Mandibular foramen 1. Entrance to mandibular canal 2. Only visible on interior 3. Exterior of mandibular canal is mental foramen ii. Mental foramen 1. Mental n. (CN V3: Mandibular) © 2009 Mark Tuttle iii. Lingular 1. Point of attachment of sphenomandibular ligament. Holds mandible to rest of skull iv. Sphenoid bone 1. Foramen rotundum a. CN V2: Maxillary 2. Foramen Ovale a. CN V3: Mandibular 3. Foramen spinosum a. Middle meningeal a. 5. What are the muscles of the fossa? a. Temporalis b. Masseter c. Medial pterygoid d. Lateral pterygoid 6. What are the major blood vessels of the fossa? a. Branches of the maxillary a. i. Middle meningeal a. ii. Accessory meningeal a. 1. If present, travels through foramen ovale 2. Accessory blood supply to dura mater iii. Inferior alveolar a. iv. Deep temporal aa. v. Posterior superior alveolar a. 7. What are the nerves of the fossa? i. Branches of CN V3:Mandibular 1. Motor branches (All mm. of pharyngeal arch 1) a. Branch to the mm of mastication i. Temporalis m. ii. Masseter m. iii. Medial pterygoid m. iv. Lateral pterygoid m. b. Branch to tensor mm. i. Tensor tympany (middle ear) m. ii. Tensor velli palatine (soft palate) m. c. N. to myohyloid d. Branch to the anterior belly of the digastrics 2. Sensory branches a. Auriculotemporal n. i. Skin of anterior ear, temporal region, lateral scalp ii. Frequently encircles middle meningeal a. iii. Travels w/superficial temporal a. © 2009 Mark Tuttle 8. 9. 10. 11. b. Inferior alveolar n. i. Guns and teeth of lower jaw ii. Enters mandibular canal + exits as mental n. (lower lip + chin) iii. Branch is n. to mylohyoid (also supplies ant. Belly of digastrics) c. Lingual n. i. Anterior 2/3 of tongue (pain, touch, temp) d. Buccal n. i. Skin of cheek + pierces buccinators to supply mucous mem on inside cheek What is the otic ganglion? Where is it located? What is the significance? Are there any other ganglia in the infratemporal fossa? a. Parasympathetic ganglion b. Houses postganglionic parasympathetic n. which supplies the parotid gland c. The preganglionic fiber is the Lesser Petrosal n. (a branch of CN IX: Glossopharyngeal) d. Synapses in the Otic ganglion e. Postganglionic fiber travels with the Auriculotemporal n. (which frequently encircles the middle meningeal a.) What is the chorda tympani? How did it acquire its name? a. Branch of CN VII: Facial n. i. Taste fibers of anterior 2/3 of tongue b. Joins the Lingual n (CN V3: Mandibular) after the lingual goes through the foramen ovale at around the 2nd molar c. The lingual n. is responsible for pain, touch, temp to the anterior 2/3 of tongue d. The Chorda Tympany (CN VII) is responsible for taste on the anterior 2/3 of tongue (SSA) i. It ALSO carries preganglionic parasympathetic fibers to the submandibular and sublingual glands e. Chorda tympani and lingual n. don’t separate until the very end of the path How is it associated with the infratemporal fossa? a. The chorda tympani joins the lingual n. (CN V3: Mandibular) in the infratemporal fossa Can you differentiate between sensory and motor nerves as they relate to the infratemporal region? © 2009 Mark Tuttle Orbit – Hankin 1. Identify the orbit and its constituent parts. a. Roof i. Frontal bone ii. Lesser wing of sphenoid bone b. Floor i. Maxilla bone ii. Zygomatic bone iii. Palatine bone c. Medial i. Ethmoid bone ii. Frontal bone iii. Lacrimal bone iv. Sphenoid bone d. Lateral i. Zygomatic ii. Greater wing of sphenoid 2. Discuss the importance of the position of the orbit in the skull. a. High up to increase visual field b. Separated to provide depth perception via bifocal vision c. Sunken in to provide protection for the soft tissues 3. Identify the components of the eyelid a. Describe how each component contributes to the function of the eyelid. i. Orbital septum 1. Fascia hich attaches the eyelids to the rum of the orbit 2. Made of fascia of tarsal plates 3. Continuous with periorbita 4. Anterior to the tarsal mm. ii. Tarsal mm. (Smooth muscle) 1. Superior tarsal m.: Assists in elevating upper lid 2. Inferior tarsal m. (poorly developed): widens palpebral fissure iii. Tarsal plates (Like cartilage, stiffens eyelid) 1. Superior tarsal plate 2. Inferior tarsal plate iv. Ligaments (holds orbit in place) 1. Medial palpebral ligament 2. Lateral palpebral ligament v. Glands 1. Tarsal glands (Meibomian glands) a. Sebaceous glands within tarsus b. 50 in each upper eyelid, 25 in each lower 2. Sebaceous glands © 2009 Mark Tuttle a. Lipid secretion (sebum) b. Lubricates edges of eyelids (prevents them from sticking together) c. Forms barrier to lacrimal fluid (tears) d. Increases tear viscosity and decreases evaporation from surface of eye 3. Ciliary glands a. Glands of Moll i. Modified apocrine sweat glands ii. Located on margin of eyelid iii. Empty onto edge of eyelash b. Glands of Zeis i. Sebaceous glands ii. Have excretory ducts that open onto middle portion of hair follicle 4. Describe the location of the lacrimal gland, its innervation and blood supply, and the structures involved in moving tears across the eye. a. In superolateral orbit b. Innervation i. Sensory 1. Lacrimal n. a. Stromal capsule of gland, not parenchyma) b. Bulbar conjunctiva c. Upper palpebral conjunctiva ii. Parasympathetic (secretomotor) 1. Presynaptic fibers via CN VII as greater petrosal n., n. of pterygoid canal, to pterygopalatine ganglion 2. Postsynaptic fibers leave pterygopalatine ganglion, join via CN V2 and then zygomatic and zygomaticotemporal branches iii. Sympathetic 1. Innervates vasculature of the gland 2. Presynaptic fibers from lateral horn of upper thoracic spinal cord to Superior Cervical Ganglion 3. Postsynaptic fibers enter the sympathetic plexus on the internal carotid a. 4. Becomes the deep petrosal n. and joins the greater petrosal n. (carrying parasymp fibers) before traveling through the pterygoid canal and entering (but NOT synapsing) in the pterygopalatine ganglion 5. Follow the same path as parasymp fibers 5. Identify the extraocular muscles and the innervation of each. Understand the following features of extraocular movements: a. Primary action of extraocular muscles with the eyes in primary gaze. © 2009 Mark Tuttle i. Superior rectus: Superomedial rotation ii. Inferior rectus: Inferomedial rotation iii. Medial rectus: Medial rotation iv. Lateral rectus: Lateral rotation v. Superior oblique: Inferolateral rotation vi. Inferior oblique: Superolateral rotation vii. Levator palpebrae superioris: Elevates eyelid b. How to test each extraocular muscle, including what position the eye should be into isolate the primary action of each muscle. i. Superior rectus 1. ii. Inferior rectus iii. Medial rectus iv. Lateral rectus v. Superior oblique vi. Inferior oblique vii. Levator palpebrae superioris c. Which muscles work together (“cross pairs” rule) to elevate/depress the eyes (e.g., when you ask a patient to “look up” from primary gaze). i. Inferior oblique and superior rectus Look up ii. Superior oblique and inferior rectus Look down d. What happens to the direction of gaze of an eye in which innervation to one or more extraocular muscle is interrupted (nerve palsies)? i. Often, the direction of gaze moves to the opposite of the action for the nerve that is interrupted since the antagonistic muscle is now unopposed 6. Identify the nerves of the orbit. a. CN II: Optic n. b. CN III: Occulomotor n. c. CN IV: Trochlear n. d. CN VI: Abducens n. e. CN V1: Opthalmic n. (Sensory) f. CN V2 (Sensory) g. Greater petrosal n. (parasymp) h. Lesser petrosal n. (symp) i. What is Horner’s syndrome? i. Interruption of sympathetic innervation to the head and neck ii. Signs 1. Ptosis: drooping of eyelids a. Results from paralysis of tarsal mm. (smooth m) especially upper lid and paralysis of superior tarsal m. 2. Pupillary constriction a. Results from paralysis of papillary dilator m. © 2009 Mark Tuttle 3. Enophthalmos – sinking of eye into orbit a. Results from paralysis of orbitalis m. in floor of orbit (a vestigial m. in humans or absent that spans inferior orbital fissure) 4. Vasodilation & anhydrosis – lack of sweating on face and neck a. Results from lack of sympathetic (vasoconstrictive) innervation to bvs and sweat glands 7. Identify the vasculature of the orbit. a. What is the significance of the cavernous sinus with regard to nerves that supply structures in the orbit? i. The cavernous sinus contains several important nn. as well as the internal carotid artery ii. Nerves 1. CN VI: Trochlear* 2. CN III: Oculomotor 3. CN VI: Abducens 4. CN V1: Opthalmic 5. CN V2: Maxillary iii. If an Internal Carotid Aneurism takes place, these nerves will be compressed and have characteristic neuropathies 1. *The first nerve affected under these circumstances is CN VI: Trochlear n. © 2009 Mark Tuttle Histology of the eye – Chiaia 1. Identify the three tunics (major layers) of the eye and sub-components of each. a. Outer supporting layer i. Cornea 1. Anterior 1/6 2. Transparent ii. Sclera 1. Posterior 5/6 2. Opaque b. Middle vascular (uveal) layer (nutrient layer) i. Iris ii. Ciliary Body iii. Choroid 1. Modified @ anterior end 2. Tickening when it is in fold (ciliary body) c. Inner Retinal Layer (photosensitive – sensory) i. Retinal pigment epithelium 1. Covers the posterior surface of the iris, the ciliary process, and the entire posterior wall of the eyeball in front of the choroid ii. Neural retina 1. Overlying neural retina covers the back of the eyeball up to the ciliary body at a juncture called the ora serrata 2. Neural portion stops but pigmented region continues anteriorly a. Light can’t get here so neural cells unneccessary 2. Identify the chambers of the eye; boundary structures for each, and contents of each. a. Anterior chamber i. Bounded by the iris and the cornea ii. Filled with aqueous humor produced by epithelium of cilliary body b. Posterior chamber i. Bounded by the lens, iris and ciliary body ii. Filled with aqueous humor produced by epithelium of cilliary body c. Vitreous chamber i. Bounded by the lens and the posterior wall of the eyeball ii. Filled with vitreous body (source unknown). Gelatinous substance 1. Helps hold lens and retinal layers in place via outward pressure 3. Identify the layers of the cornea and cellular composition of each. (5 Layers) a. Epithelium i. Stratified squamous non-keratinizing (5-6 cells thick) ii. Continuous sheath connected by semi-nonpermeable intercellular desmosome bridges iii. Help protect eye from outside environment © 2009 Mark Tuttle iv. Densely innervated with pain sensitive nerve fibers responsible for the protective reflexes of blinking and lacrimation 1. Innervated by CN V1: Opthalmic via long ciliary nn and CN III: Occulomotor via short ciliary v. Microvilli on apical surface that maintains a film of moist tears over cornea vi. Round, stem cells (basal cells) of the corneal epithelium are capable of rapid mitotic division to replace damaged corneal tissues. Turnover time for these cells is 7-10 days b. Bowman’s embrane i. Acellular ii. Composed of randomly arranged collagen fibers closely adherent to the basement membrane of overlying epithelial cells c. Lamina propria i. Thickest layer ii. 90% of cornea iii. Consists of regularly arranged lamellae of collagen fibrils (type 1 collagen), fibrocytes, amorphous ground substance (mostly keratin and chondroitin sulfate) d. Descemet’s membrane i. Thick, basement membrane of the final endothelial layer e. Corneal endothelium i. Simple squamous inner lining of the cornea ii. Actively transports water (transcellular endocytosis) out of the stroma to maintain corneal activity iii. Linked by desmosomes and occluding junctions iv. Secrete Descement’s membrane and bind to it via hemi-desmosomes 4. Identify the layers of the choroid region of the eye. (4 layers) a. Suprachoroid layer i. Immediately adjacent to the inner sclera – loose CT with elastic fibers which anchor it ot the underlying sclera b. Vessel layer i. CT stroma with a higher collagen content than suprachoroidal layer ii. Contains numerous “choroidal arteries” and “choroidal veins” iii. Numerous melanocytes which serve to absorb scattered light 1. Prevent light from bouncing back (give black appearance) c. Choriocappilaris i. Single layer of wide fenestrated capillaries which nourish hthe surrounding tissues including the outer 1/3 of the adjacent retinal coat d. Bruch’s (Glassy) membrane i. Network of collagen and elastic fibers sandwiched in between the basement membranes of the choriocapillaris on one side and the retinal pigment epithelium on the other 5. Identify the ciliary body and detail its function. © 2009 Mark Tuttle a. Thickening of the choroid which forms a ring around the eye on the inner aspect of the sclera just behind the iris b. Loose CT and smooth muscle covered by a double cuboidal epithelium consisting of i. Superficial non pigmented layer ii. Deep pigmented layer c. **Apical surfaces of these two cell layers face one another! i. Connected by desmosomes ii. Numerous fenestrated capillaries within the underlying CT 6. Identify the components of the iris and pupil and relate their structure to their function. (4 layers) a. Anterior limiting layer i. Discontinuous layer of stromal cells, consisting of stellate shaped fibroblasts and melanocytes b. Stroma i. Vascularized loose CT containing melanocytes and fibroblasts c. Muscular layer i. Two bands of smooth muscle are embedded in the stroma of the iris 1. Sphincter papillae: distinct circular band of sm the margins of the pupil 2. Dilator papillae: thin sheet of radially oriented sm near the posterior border of the iris d. Posterior epithelium i. A double layer of cuboidal pigmented cells whose structure is obscured by pigment 7. Identify the Canal of Schlemm (scleral venous sinus), its function and its importance in clinical diseases of the eye. a. Microtrebecular meshwork (catches particulate matter) empties into the annular Canal of Schlemm b. Simple squamous epithelia runs circularly around the cornea in the CT of the sclera c. Aqueous veins carry fluid to the conjunctiva to be released into venous blood d. Blockage of aqueous drainage can result in increased intraocular pressure (narrow-angle glaucoma ) resulting in decreased blood flow and ischemia of the retina = blindness 8. Identify the lens of the eye and the zonules of Zinn (suspensory ligament of the lens). a. Biconvex transparent disc suspended just behind the pupil, attached to the cilliary processes by a set of ligaments (Zonules of Zinn) i. Composed of microfibrils similar to elastic tissue and are attached to the equator of the lens at one end and the ciliary body at the other b. Anterior surface i. Acellular elastic capsule (Type IV) collagen and proteoglycans associated with basement membrane of simple cuboidal epithelium which lies just deep to the capsule ii. Avascular iii. Contains NO CT iv. Composed entirely of modified epithelial cells (lens fibers) © 2009 Mark Tuttle v. Forms a germinal zone at the equatorial run of the biconvex surfaces of the lens and cells continue to divide slowly throughout life and are added to the margins of the lens vi. Deep to the epithelium, lens cells lose their nucleus and intracellular organelles, and elongate into transparent structures called lens fibers vii. Lens fibers make up the body of the lens viii. Cytoplasm is packed with transparent proteins – crystallins ix. Lateral borders of lens fibers are connected by Knob and socket like depressions containing “tight junctions” and “gap junctions” x. Fibers at the center of the lens persist throughout life and are not replaced xi. Lens provides 1/3 of focusing power of eye and all of the accommodation by changing its shape xii. If left alone, will round to a lens of greater power xiii. At rest, lens is stretched to a flatter shape of less power, by zonules of zinn – accommodate for distant vision xiv. With age, lens fibers harden and the lens losses its ability to change shape – Presbyopia results in necessity for reading glasses xv. Can also become semi-opaque - cataracts 9. Describe the production, flow pathway and absorption of the aqueous humor. a. Filtered out of blood vessels into the posterior chamber by the capillaries of the ciliary processes )chief source of nutrients for the avascular lens and cornea) b. Transported out of interior of ciliary body by pigment epithelial celsl of ciliary body whose basement membrane provides a (double-cuboidal) blood-aqueous barrier c. Flows through posterior chamber into the anterior chamber d. Drained from anterior chamber by meshwork of fibrous channels in the lateral aspect of the ciliary body termed the Microtrebecular meshwork e. Then empties into anular Canal of Schlemm located near attachment of ciliary body to sclera f. From canal, aqueous veins carry fluid to the conjunctiva to be released into venous blod g. Blockage causes narrow-angle glaucoma 10. Identify the retina and it’s ten layers. a. Final optical element, and is the innermost layer of the posterior part of the eye b. Embryologiclaly a part of the brain and consists of neurons in complex synaptic arrantement c. Light must pass through almost all of the layers before it reaches the photoreceptors and the photoreceptors are oriented so that they POINT AWAY from the incoming light d. Layers i. Retinal pigment epithelium 1. Single layer of interdigitated cuboidal-columnar cells that lies between the retina and choroid in the posterior portion of the eye and extends over the ciliary body and the posterior iris 2. Functionally this layer is realted to both the choroid and the retina 3. Resemblllesss a simple-cuboidal epithelium of the choroid but has NO FREE surface under the retina © 2009 Mark Tuttle 4. Base of these cells are attached to Bruch’s membrane of the choroid 5. Apical surface of the cells have microvilli and cylindrical cytoplasmic sheaths that enclose the ends of retina lphotoreceptors and nourish the outer seg;ments of rods and cones an d phagocytose pieces of outer segments which are constantly shed 6. Potential space here can get a detached retina: potential space is reactivated and retinal cells die ii. 11. Identify the photoreceptors of the eye. © 2009 Mark Tuttle Histology of the Ear 1. Identify the three components of the ear; ie. outer, middle, and inner ear. a. Outer Ear i. Auricle (pinnae) 1. Irregular plate of elastic cartilage cover by thin skin w/hair follicles and sebaceous glands 2. Involved in the localization of sound in space 3. Lower animals have skeletal muscle here to change the orientation of their ears ii. External auditory meatus 1. 2.5 cm tube connected to the temp 2. Outer 1/3 – elastic cartilage continuous with the cartilage of the auricle 3. Inner 2/3 is formed by the temporal bone 4. Lined by thin skin a. Has modified apocrine sweat glands called ceruminous glands (waxy secretion) iii. Tympanic membrane (eardrum) 1. Closes the innermost aspects of the external meatus 2. Consists of 2 layers of collagen (radial and circular) covered on a. The meatus side by a layer of very thin skin b. Inside is lined by simple squamous epithelium b. Middle Ear i. Tympanic cavity 1. Box-like air filled cavity deep to the external meatus 2. Lateral wall – tympanic membrane 3. Medial wall – bony labyrinth of the inner ear 4. Acts as a resonance chamber 5. Lined with simple squamous epithelium with a thin lamina propria ii. Ossicles 1. Tympanic cavity is spanned by a serious of three small bones – auditory ossicles 2. Function a. Decrease the amplitude but increase the force of the mechanical displacements of the tympanic membrane – impedance matching 3. Since the ear are fluid filled and thus not compressible, an outlet must exist for the forces transmitted by the ossicles to the oval window a. This is served by the round window b. Covered by fibrous membrane called the secondary tympanic membrane 4. Parts a. Malleus (hammer) © 2009 Mark Tuttle i. Attached to the tympanic membrane at one end and the incus at the other b. Incus (anvil) i. Suspended between the maleus and the stapes c. Stapes (stirrup) i. Attached to the incus at one end and a small oval membrane-covered opening in the medial wall of the tympanic cavity called the oval window iii. Eustachian tube 1. 4 cm cartilaginous tube 2. Connects the tympanic cavity with the nasopharynx 3. Equalizes pressure between the outside air and the middle ear cavity 4. Cartilage covered by a pseudostratified columnar ciliated epithelium 5. Clinically important because it allows direct access to the middle ear cavity and is thus a common route for infection (Otitis media) c. Inner Ear i. Bony labyrinth 1. Filled with clear fluid called perilymph which resembles extracellular fluid and CSF in composition – high Na+ and low K+ 2. Series of bony channels consisting of 5 parts a. Vestibule (1) i. Large irregular central cavity whose lateral wall contains two membrane covered openings – Oval and round windows which lead into the adjacent cochlear canal b. Cochlear canal (1) i. Anteriorly extending tube that spirals like a snail’s shell for 2 ¾ turns around the bony center called the modiolus ii. Extending from modiolus like threads of a screw is a thin bony ridge called the spiral lamina iii. Spaces within the bony modiolus house blood vessels and the cell bodies and processes of the Spiral ganglion cells and the acoustic branch of the CN VIII: Vestibulotrochlear nerve c. Semicircular canals (2) i. Anterior, posterior, lateral (superior) ii. Extend posteriorly from the vestibule (armchair) iii. Each canal has a dilation at its connection with the vestibule called the ampulla ii. Membranous labyrinth 1. Channels of the bony labyrinth house membranous ducts which contain the specialized sensory organs for hearing and vestibular sensation termed the membranous labyrinth 2. Delicate CT lined with simple squamous epithelium © 2009 Mark Tuttle 2. 3. 4. 5. 6. 3. Ducts are suspended within the parilymph of the bony labyrinth by thin strands of CT containing BVs 4. Shape of the membranous labyrinth follow that of the bony labyrinth a. Except the large bony vestibule region occupied by two membranous sacs called the utricle and saccule b. Otoliths – sensitive to gravity and linear acceleration i. Utricle ii. Saccule Identify the boundaries and components of each. Relate structure to function. a. See #1 Identify the structure of the tympanic membrane (eardrum). a. See #1 Differentiate between the components of bony labyrinth and membranous labyrinth. a. See #1 Identify the region of the cochlea, including the basilar membrane, helicotrema, osseous spiral lamina and spiral ligament a. Cochlear duct i. Situationed in the cochlear canal of the bony labyrinth ii. Suspended medially within the cochlear canal and follows its coiled path ending as a blind sac at the apex of the cochlear canal iii. Roughly triangular in transverse section 1. Scala vestibule 2. Scala media (Cochlea) 3. Scala tympani b. Basilar membrane i. Long structure that has different properties (width, stiffness) at different points along its path ii. These parameters of the membrane at a given point along its length determine its characteristic frequency (CF), the frequency at which it is most sensitive to sound vibrations iii. Widest and least taut at the apex – low frequency sounds iv. Narrowest and most taut at the base – high frequency sounds c. Helicotrema i. The scala vestibuli + scala tympani communicate across a small aperture at the apex of the Cochlear Canal known as the HELICOTREMA ii. Filled with endolymph d. Osseous spiral lamina i. Attaches the Organ of Corti to the bony labyrinth on one end e. Spiral ligament i. Attaches the Organ of Corti to the bony labyrinth on the other end Describe the fluid that is found within the bony labyrinth (perilymph) and that found in the membranous labyrinth (endolymph) and how and where each is formed and removed. © 2009 Mark Tuttle a. Perilymph i. Fills bony labyrinth ii. Supports the membranous ducts in the bony labyrinth iii. Fills the Scala Vestibuli and Scala Tympani b. Endolymph i. Fills the membranous ducts ii. Secreted by Striae Vascularis in Scala Media iii. Similar composition as INTRAcellular fluid iv. Drains into a small duct arising from the Utricle and Saccule = ENDOLYMPHATIC DUCT v. Empties into the dura and is filtered back into CSF 7. Identify the three major divisions of the cochlear canal. a. Scala Vestibuli i. Filled with perylymph ii. Communicates with scala tympani across a small aperture at the apex of the cochlear canal known as the helicotrema b. Scala Media i. Filled with perilymph ii. Separated from the scala vestibule by the Reissner’s membrane 1. 2 layers of simple squamous epithelium separated by a basement membrane iii. Seperated from the scala tympani by 1. Stria vascularis a. Lines the lateral wall of the scala media and applied to the walls of the cochlear canal b. Highly vascular c. SOURCE of endolymph 2. Basilar membrane a. Amorphous ground substance infiltrated with transversely oriented filaments b. Lower surface: columnar epithelium c. Supports the auditory apparatus, the Organ of Corti d. Different properties (width, stiffness) along its length to facilitate sensitivities at different sound frequencies c. Scala tympani i. Roof is lined by basilar membrane 8. Identify the boundaries of the cochlear duct. a. Within the cochlear canal of the bony labyrinth b. Suspended medially within the cochlear canal and follows its coiled path ending as a blind sac at the apex of the cochlear canal 9. Identify the components of the organ of Corti including: a. tectorial membrane © 2009 Mark Tuttle i. ii. iii. iv. v. Thin, gelatinous membrane composed of keratin-like protein Extends from the spiral laminae to form the superior surface of the organ of corti Thought to originate as a secretion of the cells of the spiral laminae The top of the hari cell stereocilia are embedded in the tectorial membrane The shearing of this membrane with respect to the cell bodies of the sensory hair cells triggers electrical impulses in these cells and results in sound transduction b. outer and inner phalangeal cells i. Tall columnar cells that support the base of the sensory hair cells ii. Apical surface of these cells project a slender cytoplasmic process called the Phalanx which extends to the free surface of the organ of corti alongside the hair cells to terminate in a plate-like expansion iii. Phalanx envelopes the apical surface of the sensory hair cells iv. Lateral borders of adjacent phalanxes have well developed tight junctions v. Isolates hair cells into fluid-filled compartments c. outer and inner pillar cells i. Cone-shaped columnar cells with basally placed nuclei **diagnostic ii. Rigid cells due to numerous cytoplasmic microtubules iii. Form the walls of the Tunnel of Corti d. cochlear hair cells. i. Inner hair cells 1. Short goblet shaped cells numbering about 3,500 2. Arranged in a single row along the length of the trochlea 3. 50-70 specialized microvilli known as “stereocilia” extend from the apical surface of each cell 4. These cells are sensitive to small changes in sound “intensity” 5. Receive a dense innervation by fibers of the CN VIII: Vestibulocochlear n. 6. Each hair cells receiving synapse from an average of 20 nerve fibers 7. Base of cell serves as synaptic surface ii. Outer hair cells 1. Cylindrical columnar cells with basally located nuclei, numbering about 20,000 2. Form 3 rows extending the length of the cochlea 3. Apical surface has 100-300 stereocilia of uneven length arranged in the shape of a “W” 4. Tips of the tallest stereocilia are embedded in the tectorial membrane 5. Respond best to “low intensity” sounds 6. Have relatively few neuronal connections 7. Base of cell serves as synaptic surface 10. Identify the spiral ganglion cells as they are embedded in the bony modiolus. a. Also known as Scarpa’s ganglion b. Type I cells receive funnel-shaped (chalice) endings c. Type II cells receive bouton-like endings © 2009 Mark Tuttle d. Apical stereocilia of the sensory hair cells are embedded into a gelatinous glycoprotein material (Cupola) which extends like a hinged flap form the walls of the ampullae e. Rotation or acceleration of the head in the plane of a given semicircular canal causes the stereocilia of the sensory hair cells to bend against the inertia of the endolymph and cupola f. Results in depolarization of the sensory hair cells and initiation of action potentials in the Vestibular ganglion cells 11. Identify the maculae of the utricle and saccule. a. 3mmx3mm patch of sensory epithelium b. Suited to sense static position and linear acceleration of the head and body c. Macula of saccule is oriented in the vertical plane d. Macula of utricle is oriented in the horizontal plane e. Composed of: i. Columnar supporting cells ii. Sensory hair cells similar to those found in the cristae f. Apical surface of the sensory hair cells are covered by gelatinous glycoprotein layer called otolithic membrane g. Suspended in the otolithic membrane are small crystalline bodies composed of calcium carbonate called Otoliths (“rocks in jello”) h. During tilt of the head witi hrespect to gravity or linear acceleration the inertion provided by the otoliths in the otolithic membrane cause bending of the stereocilia of the hair cells 12. Identify the components of cristae ampullaris: a. Ampulla of each semicircular duct contains a raised transverse ridge – Cristae ampullaris which extends part way across the semicircular canal b. Cupula i. Apical stereocilia of the sensory hair cells are embedded in a gelatinous glycoprotein (CUPULA) which extends like a hinged flap from the walls of the ampullae c. Vestibular hair cells i. Receive contacts from neurons of the vestibular (Scarpa’s) ganglion located at the base of the modiolus ii. Types 1. Type I a. Flask-shaked cells with apical stereocilia similar to the inner hair cells of the basilar membrane b. Stereocilia areflanked by a single non-motile kinocilum c. Receive funnel-shaped (chalice) endings 2. Type II a. Cylindrical cells with apical stereocilia similar to outer hair cells of the basilar membrane b. Also posses kinocilia c. Receive bouton-type endings d. Sustentacular cells. i. Tall columnar supporting cells © 2009 Mark Tuttle © 2009 Mark Tuttle Pharynx – CBC Explain the anatomical location and functional significance of the pharynx. - Begins at the posterior aperture of the nose and ends at the esophagus - Serves as the common passageway for the GI tract and the respiratory systems - It is a fibromuscular tube that lies anterior to the vertebral column Give the boundaries of the three portions of the pharynx and list any important structures located in each of these areas. - Nasopharynx: From base of the skull to C2 - Oropharynx: C2-C4 - Laryngopharynx: C4-C6 What is the functional significance of the auditory tube? Where is it located? - The auditory tube is located lateral to the nasopharynx and empties into it - Its function is to equalize pressure on both sides of the tympanic membrane - Allows mucous to drain from mucous membrane - This communication also allows spread of pharyngeal infection into the ear - Children have more horizontal tube - Adults have oblique – more difficult to spread infection - Clinical correlations i. Otitismedia 1. Middle ear infection 2. Common in children with URIs 3. Painful because CN IX innervates inflamed mucous membrane ii. Otitis externa 1. Swimmers ear 2. Fluid trapped external to the tympanic membrane 3. CN V3, CN VII, CN X innervate the skin of the ear canal Explain the location(s) of the lymphoid tissue found in the pharynx. Why is it important? - Tonsilar bed i. Palatine tonsils lie here ii. Mucous membrane here is innervated by CN IX iii. Supplied by the Facial a. - Palatine tonsil i. Lies in the oropharynx ii. Can be seen on the right and left sides of the back of the throat iii. Used to be removed via tonsillectomy - Pharyngeal tonsil (Adenoids) i. Lies in the nasopharynx ii. At the back of the nose iii. Just adjacent to the occipital bone iv. When inflamed, can be dangerous because swelling constricts the pharynx become “mouth-breathers” © 2009 Mark Tuttle Explain how the muscles of the pharynx are organized. Give general origins and insertions for these muscles, as well as their actions. - Constrictors (semicircular) i. ALL insert on: Pharyngeal Rape (fibrous cord) ii. ALL act by: squeezing bolus into esophagus iii. ALL innervated by: CN X (BUT REALLY CN XI cranial fibers which joined the vagus) iv. Superior 1. Origin: Pterygomandibular raphe a. Fibrous cord running from the pterygoid plate to the hook-like hamulus of the mandible v. Middle 1. Origin: Stylohyoid ligament + superior margin of hyoid bone vi. Inferior 1. Origin: Lateral aspect of the thyroid + cricoids cartilage - Longitudinal i. ALL insert by blending in with the constrictors of the pharyngeal wall ii. Salphopharygeus and Palatopharyngeus are covered by mucous membrane, but Stylopharyngeus is NOT iii. Stylopharyngeus 1. Origin: Styloid process 2. Only m. of pharynx supplied by CN IX 3. Only muscle which CN IX supplies iv. Salphopharyngeus 1. Origin: Auditory tube v. Palatopharyngeus 1. Origin: Soft palate Give all of the components of the pharyngeal plexus. - CN X (Cranial portion of CN XI) Innervates all the constrictors Sensory to the lower portion of the pharyngeal wall via the internal laryngeal - CN IX: Motor just to the stylopharyngeus Sensory to the mucous membrane - CN V2: Sensory - Symp: From cervical sympathetic chain - Parasymp: To mucous glands lining pharynx from different component of vagus n. What is the buccopharyngeal fascia? What is the retropharyngeal space? Why are these important? - Buccopharyngeal fascia is a part of the visceral portion of the pretracheal fascia - It forms the anterior wall of the retropharyngeal space - The retropharyngeal space is between Buccopharyngeal fascia and prevertebral fascia © 2009 Mark Tuttle - It is important because it is continuous with the posterior/superior mediastinum and can spread infection © 2009 Mark Tuttle Development of the Branchial Region and Portions of the Head and Neck – CBC 1. Describe a pharyngeal (branchial arch), pharyngeal (branchial) groove, pharyngeal (branchial) pouch, and pharyngeal (branchial) membrane. a. Pharyngeal arch i. Budding of mesenchyme ii. Forms under stimulus of pharyngeal pouches iii. Mesoderm gets squeezed into them b. Pharyngeal groove i. External pocket c. Pharyngeal pouch i. Internal pocket which stimulates arches to form 2. List the four structures that are found in a typical pharyngeal arch. a. Nerve (CNs) – related to adjacent developing hindbrain b. Artery (Dorsal aortic arches) c. Cartilagenous rod (Ex. Mandibular prominence) d. Muscle component (mesoderm) 3. List the skeletal, muscular derivatives and the innervation of each pharyngeal arch. Arch Skeletal Muscles Nerve Blood vessel Arch 1 Meckel’s cartilage CN V3: Portions of Mm. of Mandibular maxillary a. Regresses mastication Malleus + small 2 tensors bones of ear - Tympany - Palitini Sphenomandibular lig Anterior belly of digastrics a. Mylohyoid Arch 2 Arch 3 Reichert’s cartilage Regresses - Stapies - Styloid process (temp bone) - Stylohyoid lig - Superior portion of hyoid Unnamed cartilaginous rod Inferior portion of hyoid Small cartilages of pharynx Mm. of facial expression Stylohyoid m. Post. Belly of digastric m. Stapedius m. in ear CN VII: Facial n. Stapedial a. (hard to locate) Stylopharyngeal m. CN IX: Glossopharyngeal Contributions to internal carotid a. © 2009 Mark Tuttle Arch 4/6 Large laryngeal cartilages Mm. of soft palate pharynx, larynx CN X: Vagus Aortic arch on L, subclavian a. on R 4. Describe the fate of each of the branchial grooves; include the formation and fate of the cervical sinus. a. The groove between arch 1+2 becomes the external auditory meatus (ex. Tympanic membrane) b. The grooves between 2/3, 3/4, 4/6 can become cervical cysts 5. Define and/or describe the fate of each of the branchial pouches or derivatives. Pouch 1 Elongate + form parts of middle ear, internal surface of tympanic membrane, auditory tube Pouch 2 Tonsilar fossa. Does NOT form tonsil. (Tonsil created by invading lymphatic tissue) Pouch 3 Dorsal diverticula: Inferior parathyroid Ventral Diverticula: Thymus Pouch 4 Dorsal diverticula: Superior parathyroid (between Ventral diverticula: Ultimobranchial body 4/5) Leaves area and invade thyroid. Provides origin for parafollicular cells These are really NCCs, so this must first be invaded by NCCs Pouch 5 NONE (between 5/6) 6. Define and/or describe the point of origin, the migratory path, and the definitive situation of the thyroid gland. a. Initially develops from the floor of the developing pharynx as the thyroid primordium i. NOT a pouch ii. Unpaired initially, but gets split into lobes by the hyoid b. Enlarges and elongates i. Maintains attachment to floor of pharynx (developing tongue) as the thyroglossal duct (unpaired) c. Thyroglossal duct should close once thyroid descends to adult position i. Forms foramen cecum of tongue (blind pouch vestigial remnant) ii. If remains patent, this is bad because anything in the mouth can get there d. Because of this descent during development, can get ectopic thyroid tissue anywhere along the path – a common site for ectopic thyroid tissue is in a cervical cyst 7. Describe the formation of the tongue. a. Four initial structures exist in tongue development i. Distal tongue buds (lateral lingual swellings) 1. Paired 2. In the 1st pharyngeal arch region ii. Median tongue bud (tuberculum impar) © 2009 Mark Tuttle 1. Unpaired 2. In the 2nd/1st pharyngeal arch region iii. Copula 1. Upnaired 2. In 2nd pharyngeal arch region iv. Hypobranchial eminence 1. 3rd/4th arches enlarge + overgrows cupola b. Distal tongue buds (lateral lingual swellings) overgrow the median bud c. Distal tongue buds (lateral lingual swellings) enlarge and form the anterior 2/3 of the tongue i. Fuses and forms the median sulcus ii. Terminal sulcus runs from the foramen cecum laterally to the edge of the tongue iii. Divides tongue into anterior 2/3 portion (oral part) and posterior 1/3 portion (pharyngeal part) iv. Posterior ½ is from the 3rd pharyngeal arch, and is innervated by the CN IX: Glossopharyngeal n. d. Occipital sinus migrates in + forms mm. of tongue (intrinsic + extrinsic) 8. Describe the formation of the face from the five face primordia. a. Begins from five primordial i. Fronto nasal prominence ii. L + R Maxillary prominence (Arch 1) (Produced by NCCs lower midbrain/hindbrain) iii. L + R Mandibular prominence (Arch 1) (Produces by NCCs lower midbrain/hindbrain) b. Fronto nasal prominence develops 2 Nasal placodes laterally, and also becomes the forehead c. Nasal placodes develop nasal pits in their mid section which eventually splits the placode into Medial nasal swellings and lateral nasal swellings d. Lateral nasal swellings fuse with the maxillary prominences e. Medial nasal swellings should fuse with each other and become the intermaxillary segment i. Philtrum ii. Upper lip/palate iii. Central incisors f. Mandibular process completes the lower jaw 9. Describe the formation of the palate and the congenital abnormalities that result in cleft palate and lip. a. Development of the palate occurs during the 5th week b. Primary plate i. Develops from the intermaxillary segment (fusion of medial nasal swellings) ii. Forms only the most anterior portion of the adult hard palate, anterior to the incisive foramen (where the primary palate fuses with the two sides of the palatine shelf) c. Secondary plate i. Develops from two processes from the internal surface of the maxillary prominences. Lateral palatine processes © 2009 Mark Tuttle ii. Grow and enlarge and should meet in the midline iii. Also fuse with the developing nasal septum iv. Anterior portion of these processes contributes to the hard palate and the posterior contributes to the soft palate v. Midline raphe marks the junction of the lateral palatal processes vi. Incisive foramen marks the junction of the primary and secondary plates © 2009 Mark Tuttle Nasal Cavity + Palate – CBC 1. Explain the external anatomy of the nose. What is responsible for the different shapes and sizes of noses? a. Frontal bone b. 2 nasal bones c. 2 maxillae d. Septal cartilage 2. Discuss the parts of the nasal septum. Give the blood supply and innervation to this structure. a. Parts i. Bones 1. Perpendicular plate of ethmoid – superior portion 2. Vomer – posterior portion 3. Nasal crest of maxilla – inferior 4. Nasal crest of palatine – inferior - posterior ii. Cartilage 1. Septal cartilage – anterior portion b. Innervation i. CN I: Olfactory – superior 1/3 of mucous membrane only ii. Septal branch of anterior ethmoidal – nasociliary branches of CN V1: Opthalmic – Anterior iii. Nasopalatine n. – CN V2: Maxillary – posterior + anterior hard palate via incisive foramen c. Blood supply i. Opthalmic a – septal branches of posterior/anterior ethmoidal aa. – Anterior + anterior hard palate 1. V. drains to orbit ii. Maxillary a. – sphenopalatine a. - Posterior 1. V. drains to deep face 3. Explain the irregular contour of the lateral nasal wall. The inferior nasal conchae is a part of what bone? Give the blood supply and innervation to the lateral nasal wall. a. Irregular contour of lateral wall of nasal cavity result from 3 curved shelves known as conchae – there to promote turbulent flow of air to warm/humidify it b. Superior and middle nasal conchae are from the ethmoid bone, the inferior conchus is from the maxilla c. Innervation i. CN I: Olfactory n. – upper 1/3 (olfactory epithelium) ii. CN V1: Opthalmic – anterior ethmoidal n. – Upper/anterior iii. CN V2: Maxillary n. - Internal nasal branches of infraorbital n. – Vestibule iv. CN V2: Maxillary n. – posterior lateral nasal n. – Posterior d. Blood supply i. Opthalmic a . - Anterior/posterior ethmoidal a. Superior 1. Vv. drains to nasal vein via foramen cecum © 2009 Mark Tuttle ii. Maxillary a. - Sphenopalatine a.+v. posterior nasal branches (absent on septum) inferior 4. Explain the shape of the ethmoid bone. What is the function of the paranasal sinuses? Describe the route of mucus drainage from these sinuses. a. Shape of ethmoid bone i. Thin laminae with several pockets ii. Make up the superior/middle conchae iii. Contain the ethmoid sinuses b. Function i. Decreasing the relative weight of the front of the skull, and especially the bones of the face. The shape of the facial bones is important, as a point of origin and insertion for the muscles of facial expression. ii. Increasing resonance of the voice. iii. Providing a buffer against blows to the face. iv. Insulating sensitive structures like dental roots and eyes from rapid temperature fluctuations in the nasal cavity. v. Humidifying and heating of inhaled air because of slow air turnover in this region. c. Route of mucus drainage i. Frontal sinus Middle meatus 1. ONLY sinus which drains easily just by gravity ii. Joined by ethmoid sinus drainage middle meatus iii. Maxillary sinus joins via Ostium of maxillary sinus middle meatus & floor of hiatus semilunaris iv. From middle meatus nasal cavity 5. Discuss several common clinical problems associated with the nasal cavity (i.e. nasal fractures, nosebleeds, chronic sinusitis). a. Sinusitis i. Pain in cheek can mean sinus inflammation ii. Maxillary sinus can expand to expose roots/abscesses of molar roots 6. What bones make up the hard palate? What muscles make up the soft palate? What is the function of the uvulae? a. Hard palate i. Primary plate 1. Intermaxillary segment of frontal bone ii. Secondary plate 1. Palatine shelves/Maxillary Prominences 2. Horizontal portion of palatine bone b. Soft palate i. Elevators: close nasopharynx from oropharynx during swallowing 1. Levator veli palatine m. a. Medial side of auditory tube palatine aponeurosis b. CN X © 2009 Mark Tuttle 2. Tensor veli palatine m. a. Lateral aspect of auditory tube palatine aponeurosis after traveling around pterygoid hamulus b. CN V3: Mandibular n. c. Really just tenses the palatine aponeurosis – accessory elevator ii. Depressors: depress to close off oral cavity so one can breathe with food in mouth 1. Palatoglossus m. a. Palatine aponeurosis (soft palate part) Lateral aspect of tongue b. CN X 2. Palatopharyngeus m. a. Palatine aponeurosis (soft palate part) blends w/other mm. in wall of pharynx b. CN X iii. Musculus uvulae m. 1. Palatine aponeurosis (superior/inferior) inserts on self posteriorly 2. Final closure as soft palate is elevated 3. CN X 4. Function a. Midline of soft palate b. “finish off” closing of nasal cavity from oral cavity c. Important for testing CN X 7. Describe the complete course of the greater palatine nerve, the nasopalatine nerve. What components are in these nerves? a. Greater palatine n. (Travels with greater palatine a) i. CN V2: Maxillary leaves cranial vault via foramen rotundum ii. Goes through PT ganglion without synapsing iii. Enters palatine canal iv. Exits via greater palatine foramen v. Descends to hard palate, travels interiorly vi. Supplies mucous membrane of hard palate b. Nasopalatine n. i. CN V2: Maxillary leaves cranial vault via foramen rotundum ii. Enters PT fossa via Sphenopalatine foramen iii. Nasopalatine n. splits and travels down to anterior portion of hard palate via incisive foramen iv. Greater palatine a. follows course of greater palatine n. but then travels UP through incisive foramen 8. Give the source of the blood supply to the hard and soft palate. a. Hard palate i. Maxillary a. Greater palatine foramen Greater palatine a. b. Soft Palate i. Maxillary a. Lesser palatine foramen Lesser palatine a. © 2009 Mark Tuttle © 2009 Mark Tuttle Functional Components of Cranial Nerves – CBC 1. Review the components of a typical spinal nerve. How do those components compare and contrast to those of a cranial nerve? a. Cranial nerves i. 12 pairs ii. Can be mixed or just dedicated to one function (Ex. CN V1 is pure Somatic Afferent) iii. Exit CNS via named foramen iv. Autonomics are always parasympathetic b. Spinal nerves i. 31 pairs ii. Always mixed iii. Exit CNS via unnamed intervertebral foramen iv. Autonomics can be parasympathetic (S1-S4) or sympathetic (T1-L2) 2. Review the general plan for the sympathetic division of the ANS. Describe the primary pathways for sympathetic fibers to the head and neck. a. Starts in ventral horn of thoracic spinal cord (T1-T4) b. Travels through white ramus communicans c. Travel up along cervical paravertebral chain d. Synapse in, and postganglionic fibers leave from: i. Inferior cervical ganglion (C7) 1. Brachial plexus 2. Middle cervical cardiac n. to heart ii. Middle cervical ganglion (C6) 1. Brachial plexus 2. Thyroid gland 3. Middle cervical cardiac n. to heart iii. Superior cervical ganglion (C2) 1. Cervical plexus 2. Plexus on vertebral artery to cranial cavity 3. Internal carotid a. + Carotid n. a. Ciliary ganglion (does not synapse here) i. Chort cilliary nn./Long ciliary nn. 1. BVs of eye 2. Pupillary dilator m. b. Deep petrosal n. i. Through pterygoid canal as N. of pterygoid canal (joined with greater petrosal n. (parasymp)) ii. Through Pterygoid Ganglion (without synapsing) iii. Follow CN V2: Maxillary n. iv. Follow Zygomatic n. v. Follow Zygomaticotemporal n. vi. Join lacrimal n. © 2009 Mark Tuttle vii. Innervate vasculature of lacrimal gland 4. External carotid a. a. Superficial temporal a. i. Skin, BVs of face b. Facial a. i. Skin, BVs of face 3. Review the general plan for the organization of the parasympathetic division of the ANS. Which cranial nerves are associated with the parasympathetic division of the ANS? a. CNs III, VII, IX, and X contain parasympathetic fibers b. CN III: Occulomotor n. i. Through superior orbital fissure ii. Splits and travels with inferior branch of occulomotor iii. Splits off the branch to inferior oblique iv. Synapses in Ciliary Ganglion v. Postganglionic fibers travel along short ciliary nn. and long ciliary nn. to innervate: 1. Pupillary sphincter m. 2. Ciliary m. c. CN VII: Facial n. i. Enters skull from cranial vault via internal auditory meatus ii. Travels to Geniculate Ganglion without synapsing 1. Travels along Greater Petrosal n. a. Exits skull via Hiatus of facial canal b. Travels through the Pterygoid canal as the N. of the pterygoid canal (includes Deep Petrosal n. [sympathetic]) c. Synapses in the Pterygopalatine Ganglion i. Postganglionic fibers innervate mucous glands of nasal/oral cavity following the course of branches of CN V2: Maxillary n. ii. Postganglionic fibers leave PT ganglion and travel along V2 Zygomatic n. Zygomaticotemporal Communicating branch to lacrimal n. lacrimal n. (CN V1) Lacrimal gland 2. Joins Chorda Tympani a. Joins Lingual n. branch CN V3: Mandibular n. b. Synapses in Submandibular Ganglion c. Postganglionic fibers innervate: i. Submandibular salivary gland ii. Sublingual salivary gland d. CN IX: Glossopharyngeal n. i. Travels through the jugular foramen ii. Becomes the Lesser Petrosal n. iii. Enters and synapses in the Otic Ganglion © 2009 Mark Tuttle iv. Frequently encircles the middle meningeal a. (branch of the maxillary a. and the external carotid a.) as the Auriculotemporal n. 1. Often the “other side” of this encircling is sympathetic fibers or branches of the posterior trunk of the CN V3: Mandibular n. v. Postganglionic fibers travel to the Partoid gland and innervate it e. CN X: Vagus n. (ALL use TERMINAL GANGLIA) i. Travels through the jugular foramen ii. Travel through Superior and Inferior Jugular Ganglia (Vagal) 1. Pharyngeal branch a. Synapses in terminal ganglia and innervates mucous glands of laryngopharynx 2. Superior laryngeal branch a. Follows internal branch of superior laryngeal n. to supply mucous glands of larynx 3. Superior/Inferior cardiac a. Supplies heart 4. Diagram all of the cranial nerves with a parasympathetic component. Identify the course of the preganglionic and the postganglionic fibers, as well as the location and the name of the ganglion associated with each nerve. a. See above. 5. What role does the trigeminal nerve serve in the autonomic control of structures in the head and neck? Identify portions of the trigeminal nerve associated with the autonomic components of other cranial nerves. a. The lesser petrosal n. of CN IX postganglionic fibers (after Otic ganglion) are distributed along the Auriculotemporal n. which is a branch of CN V3 on their way to innervating the parotid gland b. The Chorda Tympani n. of CN VII joins the lingual branch of CN V3 before reaching the Submandibular ganglion synapsing, and postganglionic innervation to submandibular and sublingual glands. © 2009 Mark Tuttle Development of the Eye and Ear – Chiaia EYE 1. Define and/or describe: a. Optic vesicle i. Pair of shallow grooves on anterolateral surface of the developing forebrain b. Optic cup i. Invagination of the optic vesicle to form the optic cup c. Optic fissure (choroid fissure) i. Ventral surface of the stalk develops in this shallow groove ii. Choroidal/Retinal Fissure iii. Extends through the ventral aspect of the optic cup iv. The hyaloid artery grows within this fissure v. Closes later in development vi. Contents: 1. Optic fissure 2. Hyaloid groove 3. Retinal fissure 4. Choroidal fissure d. Lens placode i. Outer layer ii. Ectoderm iii. Invaginates into lens put to eventually be surrounded by neuroepithelium of lens pit e. Lens pit i. Inner layer ii. Neuroepithelium iii. Evaginates as lens placode invaginates f. Lens vesicle i. The lens put continues to invaginate forming a spherical lens vesicle which later detaches from the surface ectoderm ii. Pax-6 is important for proper lens development 2. Define and/or describe: a. Hyaloid artery (central artery of retina) i. ICA Ophthalmic a. Hyaloid a. ii. Grows within Choroidal/(Retinal) fissure iii. This eventually degenerates leaving only the short/long ciliary aa. b. Hyaloid canal i. Within the Choroidal/(Retinal) fissure ii. A shallow groove on the ventral surface of the stalk iii. Extends through the ventral aspect of the optic cup iv. Hyaloid artery grows here 3. Define and/or describe the three major layers (tunics) of the eye and list the component structures found in each. © 2009 Mark Tuttle a. Outer tunica fibrosa b. Middle uveal coat c. Inner retinal coat 4. Describe the major steps that occur in the process of formation of the lens. What induces the formation of the lens? a. Two layers of the retina (neural and non-neural) are derived from the two walls of the optic cup b. Epithelial cells in the out wall (posterior wall of optic vesicle) become heavily pigmented Retinal Pigment epithelium at about 5 weeks c. Thick inner wall of the optic cup gives rise to the 9 layers of the neural retina comprised of the photoreceptor layer through the internal limiting membrane d. Differentiation of the neural retina occurs during week 6 and 7 when cells abutting the intraretinal space begin to proliferate e. Inner to outer: i. Lens vesicle ii. Lenti-retinal space (vitrous space) iii. Internal limiting membrane iv. Inner neuroblastic layer v. Outer neuroblastic layer vi. External limiting membrane vii. Intraretinal space viii. Pigment cells (posterior/external optic vesicle) f. Differentiation: i. Photoreceptors develop from the outer neuroblastic layer (first) ii. Retinal ganglion cells develop from the inner neuroblastic layer (later) iii. Axons of developing retinal ganglion cells collecto nthe inner surface of the retina and grow towards the optic stalk where they exit the eyeball. These axons line the inner wall of the optic stalk of the lumen and becoming the optic nerve iv. Non-neural and nueral layers of the retinal become FUSED by week 7 as the retinal pigment epithelium cells contact the outer segments of the photoreceptors 5. Describe the formation of the anterior chamber and the cornea. What induces the differentiation of the cornea? a. Anterior chamber i. Deep to the Cornea and Sclera ii. Chambers of the eye develop from vacuolization of a mass of loose CT that fills the space between the lens and the overlying cornea iii. Mesenchyme surrounding the optic cup invades this reagion around the 6th week 1. Layers a. Outer layer becomes part of the corneal stroma b. Inner layer forms a thin membrane over the papillary opening called the iridopupillary membrane (degenerates later in development leaving the cavity of the posterior chamber in its place) © 2009 Mark Tuttle b. Cornea i. Tissue sources: 1. Surface ectoderm covering the anterior optic cup 2. Mesenchyme surrounding the optic cup 3. Neural crest cells derived from the lip of the optic cup ii. Inductive signals from the optic vesicle induce changes in the surface ectoderm overlying the optic cup 1. These cells increase in height and begin to secrete collagen fibrils to form the primary stroma of the cornea which is rich in hyaluronic acid and well hydrated iii. Neural crest-derived cells from the lip of the optic cup migrate to the basal region of the primary stroma and form the corneal endothelium iv. A second wave of neural crest cells form the lip of the optic cup seeds the primary stroma with fibroblast-like cells which degrade the hyaluronic acid and tansform the stroma into a low hydration transparent layer (SECONDARY STROMA) v. Additional acellular layers of the cornea – Bowman’s membrane – Descemet’s membrane are secreted by the corneal epithelium and endothelium respectively vi. Endothelium continues to dehydrate the cornea by actively transporting water out of the corneal layers vii. Dehydration is THYROXIN dependent 6. Describe the formation of the iris. a. Develops form the anterior rim of the optic cup b. As the mesenchyme external to the optic cup begins to differentiate into the choroidal coat – anteriorly these cells undergo rapid proliferation to form a bulge on the choroid adjacent to the lateral margins of the lens c. Simultaneously, two groups of cells begin to grow anteriorly and cover the bulge i. Pigmented cells of the posterior wall of the optic cup (Retinal pigment epitheliumderived) ii. Superficial cells of the innermost region of the retinal layer iii. These form the pigmented and non-pigmented layers of the ciliary processes and are connected “head-to-head”** d. Mesenchymal (derived from ectoderm = ectomesenchymal) cells within the bulk of the ciliary body differentiate into the smooth ciliary mm. (maybe neural crest derived) e. Differential expansion and folding of the retinal layer results in the formation of the ridges of the ciliary processes f. These are thought to secrete the zonular fibers that form the suspensory ligament of thelens 7. Describe the formation of the ciliary body. a. See above 8. Describe the formation of the retina. a. Two layers of the retina (neural and non-neural) are derived from the two walls of the optic cup © 2009 Mark Tuttle b. Epithelial cells in the outer wall of the optic cup begomes heavily pigmented during the 5th week (RPE) c. Thick inner wall of the optic cup gives rise to the 9 layers of the neural retina comprised of the photoreceptor layer through the internal limiting membrane i. Differentiation of the neural retina occurs during week 6 + 7 when cells abutting the intraretinal space begin to proliferate EAR 9. Describe the development of the internal ear. a. Develops earliest b. Initial formation of the ear is evident at about 3 weeks as a thickening of the surface ectoderm Dorsal to the 2nd pharyngeal arch on either side of the developing rhombencephalon termed Otic Placodes c. Otic placodes invaginate to form the otic pits and finally pinch off the ectoderm to form the otic vesicles d. Otic vesicles elongate to form 2 interconnected compartments i. Utricular ii. Saccular e. These give rise to the adult components of the membranous labyrinth f. Saccular region elongates a tubular outgrowth which coils as development proceeds to form the “cochlear duct” of the inner ear g. Spiraling of the duct proceeds chronologically i. 8 weeks 1 turn ii. 10 weeks 2 turns iii. 25 weeks 2 ¾ turns h. Small group of epithelial cells migrates medially toward the neural tube to give rise to the CN VIII: Vestibotrochlear n. (spiral) ganglion embedded in the mediolus bone i. A separate group of epithelial cells migrate to the floor of the cochlear duct to form sensory hair cells of the Organ of Corti j. Neural crest derived cells also migrate into the floor of the otic vesicle and give rise to the Basilar Membrane and supporting cells of the Organ of Corti k. At about 6 weeks the mesenchyme surrounding the developing cochlear duct begins to condense forming a cartilaginous capsule around the cochlear duct l. The dorsal and ventral regions of this capsule begin to vacuolize (recanalate) forming spaces which will become the perilymph-filled scala vestibule and scala tympani in the adult m. Opposite poles of the cochlear duct become anchored to the developing cartilaginous cochlear canal at the region of the spiral lamina and spiral ligament n. Cartilaginous encasement develops in to the bony encasement of the bony labyrinth at about 16 weeks o. Invaginating ectoderm continues inward and contacts the lateral wall of the middle ear cavity p. The fusion of these membrane and the intervening mesenchyme forms the tympanic membrane © 2009 Mark Tuttle 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. i. Outer ectoderm Outer thin layer ii. Mesoderm Collagen iii. Inner endoderm Inner epithelium Describe the development of the external ear structures. a. External auditory meatus develops from the invagination of the dorsal region of the 1st pharyngeal CLEFT b. Outer auricle and pinna of the ear form form 6 nodular masses of mesenchyme – auricular hillocks derived from the 1st and 2nd pharyngeal arches i. Hillocks 1-3 1. Derived from the 1st arch 2. Form the anterior portions of the external ear 3. Innervated by CN V: Trigemminal n. ii. Hillocks 4-6 1. Derived from 2nd arch 2. Form the posterior portions of the external ear 3. Innervated by cervical plexus C2-C3 Define and/or describe the three anatomical subdivisions of the ear. Define and/or describe the otic placode and list the structures that are derived from it. Define and/or describe the membranous labyrinth and the bony labyrinth. Define and/or describe: endolymph, perilymph. Describe the relationships between the utricle and related semicircular ducts and endolymphatic duct. Describe the relationship of the saccule and the cochlear duct. Briefly describe the function or the neural transducers found in the semicircular ducts, the utricle, and the cochlear duct. Briefly describe the formation of the tympanic cavity of the middle ear from the first pharyngeal (branchial) pouch. What is the developmental history of the middle ear ossicles (malleus, incus, and stapes)? Briefly describe the formation of the external auditory canal from the first branchial cleft. Define pinna (auricle). What is the developmental history of the auricle? Distinguish between “nerve deafness” and “conduction deafness”. List at least one congenial cause for each. What is congenital cholesteatoma? When is the ear most susceptible to teratogens? Explain the developmental history of any/all structures observed in microanatomy laboratory exercises. © 2009 Mark Tuttle Oral Cavity - CBC 1. Define the boundaries of the oral cavity. a. Boundaries i. Cheeks ii. Palate iii. Tongue/floor of mouth iv. Lips v. Pharynx b. Parts i. Vestible 1. Space on the buccal side of teeth + gums (cheek side) ii. Oral cavity proper 1. Lingual side of teeth/gums 2. Normally filled with tongue 2. Review the innervation of the following structures: a. Lips i. Upper: CN V2 ii. Lower: CN V3 b. Cheeks i. CN V2: Maxillary -> Infraorbital n. ii. CN V3: Mandibular n. -> Buccal n. 1. (Pierces buccinator m.) c. Gums. i. Any nerve which goes by them innervates them ii. CN V2: Maxillary n. 1. Nasopalatine n. 2. Anterior palatine n. 3. Posterior superior alveolar n. 4. Infraorbital n. iii. CN V3: Mandibular n. 1. Inferior alveolar n. Mental n. 2. Lingual n. 3. Buccall n. 3. Review the five areas where lymphoid tissue forms “tonsils” around regions of the oral cavity and the formation of the tonsillar ring. a. Waldeyer’s Ring (Tonisilar ring) i. Palatine tonsils (2) 1. Between palatoglossus m. and palatopharyngeus m. ii. Pharyngeal (Adenoid) tonsil (1) 1. At the posterior aspect of the nasopharynx iii. Lingual tonsil (1) 1. On the posterior aspect of the tongue © 2009 Mark Tuttle iv. Lateral bands (2) 1. Along salpingopharyngeal fold 4. Explain the anatomical considerations associated with the tongue and its sensory innervation. a. Anterior 2/3 i. SSA 1. CN VII: Facial -> Geniculate ganglion (cell body) chorda tympany taste buds ii. GSA 1. CN V3: Mandibular branch Trigeminal Ganglion (cell body) Lingual n. b. Posterior 1/3 i. SSA 1. CN IX: Glossopharyngeal n. Glossopharyngeal/Petrosal ganglion (cell body) taste buds ii. GSA 1. CN IX: Glossopharyngeal n. Glossopharyngeal/Petrosal ganglion (cell body) Lingual branch c. Very posterior (near epiglottis) i. SSA 1. CN X: Vagus n. Superior jugular ganglion (cell body) taste buds 5. Know the organization, action, blood supply and innervation of the intrinsic and extrinsic muscles of the tongue. a. Innervation i. Intrinsic (CN XII: Hypoglossal n.) 1. Horizontal 2. Longitudinal 3. Vertical (oblique) ii. Extrinsic 1. Hyoglossus m. Depress posterolateral tongue 2. Styloglossus m. Retract + Elevate 3. Genioglossus m. Protract 4. Palatoglossus m. Elevate tongue (CN X: Vagus n.) b. Blood supply i. Lingual a. (ECA) (Deep to hyoglossus m. by lingual n. (V3) + hypoglossal n. (CN XII) run superficial to hyoglossus m.) 1. Dorsal lingual aa. (Posterior 1/3) 2. Deep lingual a. (Majority of anterior 2/3) 3. Sublingual br. (in sublingual fossa to sublingual gland) 6. Review the suprahyoid muscles. What are their separate innervations? What is their collective action? a. Muscles i. Digastric m. Anterior=V3, Posterior=facial ii. Stylohyoid m. CN XII: Hypoglossal n. © 2009 Mark Tuttle iii. Geniohyoid m. C1 ventral rami iv. Mylohyoid m. C1 ventral rami b. Collective action i. These four muscles have different actions, but in general assist in elevating the hyoid bone and widening the pharynx during swallowing. 7. Review the three main pairs of salivary glands. Explain their location, the location of their duct(s) and their innervation. a. Parotid glands i. Duct crosses the masseter to end in the vestibule of the oral cavity ii. Innervated by: Lesser petrosal n. (CN IX: Glossopharyngeal n.) [Parasymp] b. Submandibular glands i. Duct crosses the lingual nerve in the sublingual fossa to open at the sublingual papilla adjacent to the lingual frenulum ii. Innervated by: Lingual n. via Chorda tympani (CN VII: Chorda tympni) Parasymp c. Sublingual glands i. Many ducts open into mouth into sublingual fossa ii. Innervated by: chorda tympani nerve (from the facial nerve via the lingual n.) is secretomotor to the sublingual glands. © 2009 Mark Tuttle Larynx – CBC 1. Describe the cartilaginous skeleton of the larynx. a. Unpaired i. Thyroid cart. ii. Cricoid cart. iii. Epiglottic cart. b. Pair i. Arytenoid cart. 1. Muscular process a. Attaches to Posterior and Lateral Cricoaratynoid mm. 2. Vocal process a. Attaches to vocal lig. ii. Corniculate cart. iii. Cuneiform cart. 1. Inside aryepiglottic folds 2. Explain the orientation of the membranes that act to support the cartilages of the larynx. a. Thyrohyoid membrane: i. Stretches between the hyoid bone and the superior margin of the thyroid cartilage ii. Because of this ligament, every action on the hyoid affects the larynx iii. Pierced by 2 structures: 1. Internal laryngeal nerve (Branch of Vagus) 2. Superior laryngeal artery (Branch of Superior Thyroid artery from External Carotid) b. Cricothyroid membrane: i. Can only see a portion externally ii. The majority is from extension internally into the larynx c. Cricotracheal ligament: i. attaches inferior border of cricoid cartilage and the first tracheal ring. 3. Describe the internal anatomy of the larynx. Where are the vestibular folds? Where are the vocal folds? a. Quadrangular membrane (R and L) i. Stretches from the lateral border of the epiglottis to the anterior-lateral surface of the Arytenoid cartilages ii. Has an inferior free margin iii. Base thickens as a band = Vestibular Ligament iv. This ligament is covered with mucous membrane coat ament + membrane = Vestibular Fold (aka False Vocal Folds / Cords) b. Conus Elasticus: i. Is the internal continuation of the cricothyroid membrane (goes between the cricoid and the thyroid cartilages. ii. Normally seen on the internal side of the cricothyroid cartilage iii. It will end superiorly as a thickened band called the Vocal Ligament iv. Vocal ligament is covered with mucous membrane © 2009 Mark Tuttle v. Vocal ligament + mucous membrane = Vocal Fold vi. Vestibular fold is Superior to the Vocal fold c. Chambers of the Larynx (3) i. Vestibule: Chamber superior the vestibular fold 1. Vestibular folds are inferior boundary ii. Ventricle: Is the space between the vestibular and vocal folds iii. Infraglottic Cavity: The space below (inferior) to the vocal folds d. Rima Glottis: The laryngeal inlet e. Rima Glottidis: The space / opening between the Vocal Folds / Cords 4. Explain the location, innervation and action of each of the intrinsic muscles of the larynx. 1. Important articulation is the one between the Arytenoid cartilage and the cricoid cartilage a. Arytenoids cartilages can pivot and glide b. Vocal ligaments are adducted when they are touching (the space between them is closed) 2. Posterior Cricoarytenoid muscle a. Attaches posterior aspect of cricoid cartilage inserts on lateral process on arytenoid cartilage b. Action: Abduct vocal ligaments c. This opens the Rima Glottidis 3. Lateral Cricoarytenoid muscle a. Origin: Arch of cricoid cartilage b. Insert: lateral process of arytenoid cartilage c. Action: adduct the vocal ligament d. Closes the Rima Glottidis 4. Oblique Arytenoid muscle and Transverse Arytenoid muscle a. These glide the two vocal ligaments together b. Act to adduct / close the space. 5. Muscles that change the tension on vocal cords a. Tighten them pitch will goes higher b. Loosen them pitch goes lower c. Does not happen at the Arytenoid-Cricoid articulation, it happens at the Atriculation of the Thyroid cartilage and Arytenoid cartilage. d. Cricothyroid muscle: i. Pulls thyroid cartilage forward ii. Tenses the vocal ligaments e. Thyroarytenoid muscle: i. Pulls thyroid cartilage back ii. Loosens the vocal ligaments 5. Review the blood supply and innervation to the mucus membrane that lines the larynx. a. Innervation of Larynx: 1. mucous membrane surface superior to vocal folds a. innervation from internal laryngeal nerve b. pierces thyrohyoid membrane to innervate down to the vocal folds 2. External laryngeal branch goes to the Cricothyroid muscle. 3. Remainder of mucous membrane is supplied by Vagus’ recurrent laryngeal nerve a. Enter the larynx inferiorly © 2009 Mark Tuttle b. Responsible for supplying mucous membrane inferior to vocal folds, supplies sympathetics as well c. Also supplies all intrinsic muscles of the larynx. 4. Blood supply to Larynx: 1. Superior Laryngeal artery a. branch of superior thyroid artery b. supplies superior aspect of larynx 2. Inferior laryngeal artery a. Branch of inferior thyroid artery (from the thyrocervical trunk) b. Supplies inferior aspect of larynx 6. Explain how the larynx works during phonation. What anatomical features of the larynx may affect the quality of your voice? Phonation: 1. During respiration, the vocal folds must be abducted. There is not enough space between adducted ligaments to breath. 2. To speak: Inhale adduct vocal ligaments exhale ligaments vibrate to create sound. 3. The greater the volume of air that passes, the louder the sound will be. 4. Laryngitis: Inflamed mucous membrane in the larynx swollen and distended folds can’t be opposed as tightly as they need to be to speak. 5. Polyp on the larynx will have the same effect. Swallowing: 1. 2. 3. 4. the laryngeal aperture must be closed off if it is not close off, material will go into the trachea The epiglottis is right next to the posterior 1/3 of the tongue Elevation of the larynx will push the epiglottis against the tongue, thus causing it to depress over the laryngeal aperture. 5. Process also involves elevation of the soft palate to wall off the nasopharynx. © 2009 Mark Tuttle Oral Cavity – Crissman 1. Describe and identify the component parts of the lip (skin, vermilion border, labial mucosa, labial glands & orbicularis oris muscle). Relate their structure to function. a. Skin: Stratified squamous keratinized epithelium b. Vermillion border: Stratified squamous para-keratinized epithelium i. Lacks sweat glands needs to be moistened occasionally ii. Tall dermal papillae with capillaries to give red color c. Lining mucousa: Stratified squamous epithelium on moderately dense CT i. Soft palate has less dense irregular CT, a submucosa and numerous serous and mucous glands d. Masticatory mucousa: Perakeratinized to keratinized stratified squamous i. Ex gingival & hard palate, around teeth ii. Gums LACK submucousa & glands 2. Identify and describe the component parts of the tongue (lingual mucosa, filiform, fungiform and vallate papillae, taste buds, skeletal muscles, lingual salivary glands and von Ebner glands). Relate their structure to their function. a. Lingual mucosa i. Stratified squamous non-keratinizing epithelium & lamina propria b. Filiform papillae i. Narrow conical ii. Most common iii. Give tongue surface velvetiness iv. Tip has keratinized epithelium v. Raspy sandpaper like character of cat tongue vi. ** Only papillae which lacks taste buds vii. Function increase friction between food & tongue c. Fungiform papillae i. Mushroom shaped ii. Located on lateral edges of tongue iii. Non-keratinized epithelium – redder color iv. Broad cap of mushroom contains taste buds d. Circum-vallate papillae i. 9-12 large round papillae located just in front of sulcus terminalis ii. Has moat surrounding each large papilla iii. Protrusion has central core of CT iv. Covered by non-keratinized epithelium v. Moat also lined by same epithelium vi. Taste buds located in groove and sides vii. Serous glands of von Ebner drain into base of moat (keeps stuff clean) e. Taste buds i. Epithelial sensory organ that senses taste ii. 3000 on dorsal surface of tongue © 2009 Mark Tuttle iii. Spherical structure composed of 60-80 cells iv. Associated with Fungiform + Circumvellate papillae (NOT Filiform) f. Skeletal muscles i. Extrinsic: Originate outside the tongue and insert in the tongue 1. Genioglossus m. 2. Hyoglossus m. 3. Styloglossus m. 4. Palatoglossus m. (only CN X: Vagus n. innervation) ii. Intrinsic: Change shape of tongue 1. Longitudinal 2. Transverse 3. Oblique (Vertical) g. Lingual salivary glands i. Small glands which reside within the oral mucousa and tongue h. Von Ebner glands i. Serous glands of von Ebner drain into base of moat of circumvellate papillae, keeping things clean 3. Describe and integrate the component parts of a tooth. (enamel, dentin, cementum, pulp, anatomic root and crown, neck and clinical crown). Relate structure to function. a. Enamel i. Hardest substance in body ii. 96% hydroxyapatite crystals iii. Remaining 4% is organic material & water 1. Glycoproteins: enamelins & amelogenin iv. Arranged as enamel rods 1. Keyhole shaped prismins that extend from outer surface to dentin 2. Each rod coated by enamel sheath of organic material 3. Interred region = hydroxyapetite crystals have different orientation v. Enamel is laid down by ameloblasts from the dentinal surface outward 1. This is only done during development 2. Once tooth peaks out from gums, ameloblasts rub off b. Dentin i. Second hardest substance in body ii. 70% hydroxyapetite crystals iii. Type I collagen, proteoglycans, glycoproteins iv. More elastic than enamel prevents tooth from fracturing v. Odontoblasts produce dentin 1. Present throughout life c. Cementum i. Lies on outside of dentin on root ii. ~ hard as bone iii. 50% hydroxyapetite © 2009 Mark Tuttle 4. 5. 6. 7. iv. Mostly type I collagen fibers in organic portion v. Cementocytes are trapped within lacunae in the cementum matrix like osteocytes d. Pulp i. Vascular loose CT ii. Rich in proteoglycans & glycoproteins iii. Lined by odontoblasts producing dentin e. Anatomic root and crown i. The anatomical crown is that portion of the tooth encased in enamel. In young people, areas of the anatomical crown are frequently buried in gingival tissue. As a person gets older, it becomes common for a tooth's enamel to be completely exposed above the gingiva and to have root surface showing (gingival recession). The term clinical crown is applied to the part of the crown exposed (visible) in the mouth. f. Neck (Cervix) i. Junction between crown & root g. Clinical crown i. See part e Describe the composition and structure of the periodontal ligament and relate it to its function. a. Dense irregular CT b. Sharpey’s fibers i. Bundles of collagen fibers in periodontal ligament ii. Embedded in alveolar bone & in cementum iii. Hold tooth in place iv. Fibrous joint 1. A gomphosis, but functionally a synarthroses Identify the distinguishing features of the gingiva and gingival sulcus associated with the alveolar processes bearing teeth. a. Gingiva i. Supports tooth & seals off oral cavity from CT ii. Parakeratinized to keratinized epithelium (Masticator mucosa) b. Gingiva groove (sulcus) i. Hairpin loop that creates space adjacent tooth & is deep to the gingival surface c. Junctional epithelium is where epithelium attaches to enamel surface by hemidesmosomes Describe the composition of primary and secondary dentition. Describe the development of the typical tooth. Identify the formation and origins of dental lamina, enamel organ, dental papillae, dental sac, ameloblasts and enamel, odonoblasts and dentin, epithelial root sheath and the process of eruption. a. Bud stage (begins at 6-8 wks) i. Forms tooth bud for each tooth (10 in each jaw) ii. Ectomesenchyme surrounds the down-growing bud 1. Derived from NCCs 2. Basal lamina separates dental lamina from ectomesenchyme © 2009 Mark Tuttle b. Cap stage: Early i. Proliferation increases size & shape t ocape shape ii. Enamal organ 1. Outer enamel epithelium: Outer surface 2. Stellate reticulum: Cells between the two layers 3. (Stratum intermedium) (forms later) 4. Inner enamel epithelium: Inner surface c. Cap stage: Late i. Ectomesenchyme condenses to form dental papilla 1. ** Gives rise to the odontoblasts and dental pulp d. Bell stage i. Continues to increase in size to form bell shape ii. Characterized by 4th layer of cells in enamel organ – stratum intermedium 1. Forms between stellate reticulum & inner enamel epithelium iii. Outer enamel epithelium breaks down and dental sac collapses on stratum intermedium iv. Causes stratum intermedium to induce the inner epithelium to differentiate into ameloblasts v. **Differentiation of ameloblasts induces the inner cells of the dermal papillae to differentiate into odontoblasts which begin laying down dentin vi. Once dentin is laid, enamel is deposited to form the Dentoenamel junction e. Bell stage: Appositional phase i. Deposition of dentin & enamel ii. Odontoblasts are pushed away from junction as the dentin is depositied iii. Distal end of the cell remains at the junction to form the cytoplasmic odontoblastic process located in the dentinal tubule iv. Unmineralized dentrinal matrix is laid down and THEN mineralized v. Crown forms before the root 8. Describe how the structural characteristics of odontoblasts, ameleoblasts and cementoblasts relate to their function. a. Odontoblasts i. Produce dentin ii. Line the pulp chamber b. Ameloblasts i. Lays down enamel ii. Similar to odontoblsat but when unmineralized matrix is laid down the apical process is punched down to form the Tomes process. iii. They do not continue completely through the enamel iv. These are sloughed off as soon as the tooth protrudes through the gums c. Cementoblasts i. Cementoblasts line outer surface at periodontal ligament space ii. Secrete cementum throughout life © 2009 Mark Tuttle 9. 10. 11. 12. 13. iii. Cementocytes are trapped within lacunae in the cementum matrix like osteocytes 1. Cell processes running through canaliculi reach the vessels in the periodontal space 2. Has cellular and acellular portions of cementum Compare and contrast the composition, formation, structure and function of enamel, dentin and cementum. a. See above Compare and contrast Tome's fibers (odontoblastic processes), Tome's processes, dentinal tubules and enamel rods. Describe the composition and location of dental pulp. a. Vascular loose CT b. Rich in proteoglycans & glycoproteins c. Lined by odontoblasts d. Root canal connects the pulp chamber with periodontal space e. Carries blood vessels & nerves to supply tooth Describe what is a salivary gland and identify the groups of minor glands and major glands. a. Secretes saliva (up to 1.5 quarts/day) i. Viscous fluid containing mucus, proteins, salts, ptyalin (salivary amylase), lingual lipase and antibacterial agents, lyzozyme, lactoferrin and IgA b. Minor salivary glands + major salivary glands (Parotid, Submandibular, Sublingual) c. ** All are compound tubualveolar d. Organized into lobes and lobules by CT e. Serous, mucous, & mixed secretion f. Innervation i. Parasymp releases ACh to stimulate formation and secretion of serious saliva ii. Symp releases NorEp results in secretion of mucus and enzymatic components iii. probably not this discreet separation, but both ANS divisions are involved Describe and identity the parotid, submandibular and sublingual glands. Integrate their characteristic structure to their function. a. Parotid (30% of saliva volume) i. Largest ii. Located over angle of mandible iii. ** Primary serious secretion 1. Reddish staining 2. Salivary amylase (ptyalin) 3. IgA that inactivates antigens 4. Antimicrobial proteins (crystatin & hystatins) 5. Lactoferrin 6. Na+ & Cl- ions iv. White adipocytes throughout – increase with age v. Intercalated ducts: Difficult to see vi. Striated ducts: Easy to see- not surrounded by CT © 2009 Mark Tuttle vii. Interlobular ducts: Surrounded by CT, located in septa between lobules viii. Terminal duct: Stensen’s duct b. Submandibular (Produce 60% of saliva) i. Similar in structure to the parotid gland ii. Both serous and mucous acini (predominantly serous **5:1 ratio) iii. Mucins & proteins in saliva form pellicles 1. Forms a protective coat of mucin on the teeth which acts as a barrier against acids 2. Retains moisture 3. Regulates adherence of bacteria iv. Terminal duct: Wharton’s Duct (exits on frenulum of tongue) v. c. Sublingual (5% of saliva) i. Inferior to tongue ii. Secrets through multiple ducts on sublingual fold iii. Similar ins tructure to other two iv. Mixed salivary gland (serous & mucous) v. Predominatnly mucus acini with serous demilunes ** Diagnostic vi. Mucin functions to help lubricate the food bolus & form pellicle vii. Duct system is similar but shorter intercalated ducts that makes them harder to find d. Minor salivary glands (5% of saliva) 14. Describe and integrate serous and mucous acini, serous demilunes, intralobular ducts (intercalated and striated) and interlobular ducts into the structure of all salivary glands. a. Serous/mucus acini i. Surrounded by myoepithelial cells that aid in secretion b. Serous demilunes i. Diagnostic for the Sublingual Glands c. Intralobular ducts i. Intercalated 1. Simple cuboidal cells & some myoepithelial cells 2. Smallest – same size as acini 3. Difficult to recognize, but easiest to see in parotid gland 4. Drain acini & tubules ii. Striated 1. Simple cuboidal to low columnar 2. More reddish staining a. B/c numerous mitochondria & membrane infoldings iii. Both 1. Within lobules of the gland 2. Resorb Na+ and Cl- ions 3. Secrete bicarbonate d. Interlobular ducts © 2009 Mark Tuttle i. Between lobules and **Surrounded by connective tissue ii. Formed by merger of striated ducts e. Interlobar ducts i. Larger ducts between lobes of the gland ii. Surrounded by CT of large septa f. Main terminal duct i. Stenson’s in parotid ii. Wharton’s in submandibular iii. Sublingual lacks a main duct iv. Not just passive drainage v. Secretory portion of gland secretes water, ions & numerous substances vi. Striated duct adds & resorbes substances 1. Adds: bicarbonate ions, IgA & killikrein 2. Resorbs: Na+, Cl- © 2009 Mark Tuttle Cross-sections – CBC 1. Review key features of plain films and CT or MRIs of the head and neck. 2. Identify the key landmarks of the head and neck to be used as guides in cross- sectional anatomy of the region. 3. Review representative levels of the head and neck and identify specific structures listed in the handout at each level.