Evaluation_and_Management_Coding_Trainin
advertisement

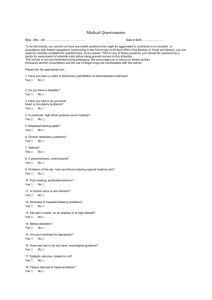
Evaluation and Management Coding The Evaluation and Management (E/M) section of the CPT book contains codes for office and outpatient setting, custodial care, hospital medical services, consultation, emergency department, critical care, preventive medicine, and others. There are 3 key components which are used to help determine the appropriate level of service: HISTORY relative to the patient’s clinical background EXAM covering the present and / or concurrent problems MEDICAL DECISION MAKING performed by the physician to manage the patient’s health problems There are 4 ELEMENTS: COUNSELING with the patient and / or family members COORDINATION of CARE with any other physicians, facilities, and / or health care bureau’s NATURE of patient’s problem TIME is considered the controlling factor in selecting the E/M level of service only when more than 50% of the face-to-face time is spent on counseling and/or coordination of care. The level of the Evaluation and Management (E/M) Service chosen depends upon whether the patient is a new or established patient. A new patient requires 3 of the 3 key components to be met where an established patient only requires 2 of the 3 key components to be met. When a physician selects an E/M level of service they must: Identify where and what services were performed Identify who received the service Review the E/M level of service descriptors Determine the history obtained Determine the exam performed Determine the level of complexity in the decision making Determine if the patient is a NEW or ESTABLISHED patient New patient vs. Established patient A new patient is one who has not received any professional services from the physician, or another physician of the same specialty who belongs to the same group practice, within the past 3 years. An established patient is one who has received professional services from the physician, or another physician of the same specialty who belongs to the same group practice, within the past 3 years. 2 History To select the overall level of history there are four components within the history itself to evaluate: Chief Complaint History of Present Illness Review of Systems Past, Family and Social History History of Present Illness (HPI) The HPI is a chronological description that uses eight elements to identify the patient’s present illness, signs and/or symptoms from the first onset to present. The eight elements include: Location – where the symptom or problem is occurring (e.g., RUQ abdominal pain, right knee pain) Quality – a description of the symptom or pain (e.g., sharp, dull, burning) Severity – a rating or description of severity of the symptom or pain (e.g., mild, scale of 1-10) Duration – how long a pain or symptom lasts or has been present or persisted (e.g., one week, since yesterday) Timing – when does a symptom or pain occur (e.g., after eating, in the morning or after a workout) Context – describes the situation surrounding the problem, episode or condition, can be stated in terms of the “big picture” (e.g., such as an injured ankle while playing basketball) Modifying Factors – what makes symptom or pain better or worse (e.g., taking meds, ice, heating pad) Associated Signs and Symptoms – additional problems associated with the specific symptoms the patient presents for. This information may help in identifying a new disease process or underlying problems related to the existing problem (e.g., migraine with aura and nausea) 3 Review of Systems (ROS) A series of positive or negative responses to questions asked by the practitioner. The review of systems does not include physical exam elements. Constitutional – high fever, weight loss/gain, fatigue Eyes – diplopia, blurred vision, strain or pain ENT – discharge or bleeding from nose, difficulty swallowing Cardiovascular – edema, chest pain, syncope, palpitations Respiratory – shortness of breath, cough Gastrointestinal – bloating, last bowel movement Genitourinary – frequency, burning or pain, hematuria Skin – rashes, itching Neurological – headaches, seizures Psychological – insomnia, attitude Endocrine – excessive hunger or thirst Hematologic/Lymphatic – anemia, bruising or bleeding problems Musculoskeletal – joint swelling, stiffness Allergic – allergy symptoms or reactions All others negative - The systems with positive or pertinent negative responses must be individually documented. For the remaining systems, a notation including “all other systems negative” is permitted. The provider must have actually reviewed the remaining systems and had negative responses for the above to be applicable. 4 Exam Systems Body Areas Constitutional Head Eye Neck ENT Chest CVS Abdomen Respiratory Genital/Buttocks Allergic Back GI Extremity GU Skin Neurological Psychiatric Endocrine Hematologic/Lymphatic Musculoskeletal 5 6 Medical Decision Making (MDM) Medical decision making is considered the thought process of the physician. There are four levels of medical decision making: Straightforward Low Complexity Moderate Complexity High Complexity To qualify for a given type of medical decision making, the following three elements are considered: The number of diagnoses or management options. The amount and/or complexity of the data, diagnostic tests, and/or other information that must be obtained and reviewed. The risk of significant complications, morbidity, and/or mortality as well as comorbidities associated with the presenting problem(s), diagnostic procedure(s), and/or possible management options. Number of diagnoses and management options The number of diagnoses or management options is defined as: PROBLEM Self-limited, minor (stable, improved or worsening) Est problem (to practitioner) stable, improved Est problem (to practitioner) worsening New problem (to practitioner) no additional work-up New problem (to practitioner) Additional work-up planned NUMBER (Max = 2) POINTS 1 1 2 (Max = 1) 3 4 7 Complexity of Data The complexity of data is a determining factor in your medical decision making. Data consists of: TYPE OF DATA POINTS Review and/or order clinical lab tests Review and/or order tests in radiology section of CPT (70010-79999) Review and/or order tests in medicine section of CPT (90281-99602) Discuss test results with performing MD Independent review of image, tracing, or specimen Decision to obtain olds records and/or obtain History from others Review/summarize old records, and/or obtain History 1 1 1 1 2 1 2 The data does not get a cumulative total per line. In other words, no matter how many lab results you order or review, you only get 1 point. However, you do get a cumulative total score for the section. Risk The assessment of risk is based on the risk related to the presenting problem and to the disease process anticipated between the present encounter and the next one. The four types of risk are: Minimal Low Moderate High The highest level of risk in any one category determines the overall level of risk. 8 PROVIDER PATIENT AUDITOR Date of Service Pre-Audit CPT Code(s) Date of Audit Post-Audit CPT Code(s) Pre-Audit Diagnosis Code(s) Post-Audit Diagnosis Code(s) 3 of 3 Required HISTORY H P I R O S Severity Timing Modifying Factors Location Quality Context Associated Signs & Sx Constitutional Skin Eyes Allergy/Immunology GU CV Respiratory Endo Neuro Musculo-skeletal Heme/Lymph Psych “All others negative” ENMT GI Exp. Problem Focused Detailed Comprehensive Brief (1-3) Brief (1-3) Extended (4 or more) Extended (4 or more) None Pertinent to Problem Extended (1 system) (2-9 systems) Complete (10 or more systems or some systems with statement “all others negative”) None Pertinent Complete (1 history area) (New Pt-3 history areas Est Pt-2 of 3 areas Past History (Patient’s past experience with illness, surgery, injury and treatments) P F S H Family History ( a review of medical events in the patient’s family including diseases which may be hereditary and/or place patient at risk) None Body Aeas Social History (an age-appropriate review of past and current activities) Head incl face Chest incl breast & axilla Constitutional (e.g. VS gen app) Ears, nose, mouth, throat CV Eyes Back incl spine Problem Focused Exp Problem Focused Detailed Comprehensive 1 area or system 2 to 4 areas or systems 5 to 7 areas or systems 8 or more systems Each extremity Resp Musc/skel Psych GI Skin GU Neuro Heme Lymph Immun Number of Diagnoses or Management Options Selected “PROBLEMS” Box A Abdomen Genitalia incl groin & back Neck Organ Sys. Exam Duration Problem Focused Problems Number Points Self-limited or minor (stable, improved or worsening Established problem (to practitioner) stable, improved Established problem (to practitioner) worsening New problem (to practitioner), no additional work-up planned New problem (to practitioner), additional work-up planned Max = 2 1 1 2 Max = 1 Box C Presenting Problem(s) Results M I N I M A L 3 4 Bring total to line “A” in BOX D *One self-limited or minor problem e.g., cold, insect bite, tinea corporis *Two or more self-limited or minor problems “DATA” Box B Amount and/or Complexity of the Data to be Reviewed Points Review and/or order clinical lab tests Review and/or order tests in the Radiology section of CPT Review and/or order tests from the Medicine section of CPT Discussion of test results with performing physician Decision to obtain old records, and/or decision to obtain history from someone other than the patient 1 1 1 1 L O W (2) *Acute uncomplicated illness or injury, e.g., cystitis, allergic rhinitis, simple sprain 1 Review and summation of old records, and/or obtaining history from someone other than the patient and/or discussion of the case with another HCP 2 Independent visualization of image, tracing or specimen itself (not simply review of report) 2 Bring total to line “B” in BOX D M O D E R A T E (3) BOX D The highest level reached by 2 Boxes determines the ultimate Medical Decision Making Final Result of Complexity of Medical Decision Making Box D A PROBLEM(S) B DATA C 2 of 3 required 1 Minimal 2 Limited 3 Multiple 4 Extensive 1 Minimal 2 Limited 3 Moderate 4 Extensive High High RISK Minimal Low (3) Moderate Type of Medical Decision Making Straightforward LOW Moderate Created by Lisa Sowers 8/8/06 *One stable chronic illness, e.g., well-controlled hypertension or non-insulin dependent diabetes, cataracts, BPH H I G H “RISK” Diagnostic Procedure(s) Ordered *Lab tests requiring venipuncture *Chest X-rays *EKG/EEG *Urinalysis *Ultrasound *Physiologic tests not under stress, e.g., PFT *Non-cardiovascular imaging studies with contrast e.g., barium enema *Superficial needle biopsy *Clinical laboratory tests requiring arterial puncture Risk of Complication and/or Morbidity or Mortality Management Options Selected *Rest *Gargles *Elastic bandages *Superficial dressings *OTC drugs *Minor surgery with no identified risk factors *Physical therapy *Occupational therapy *IV fluids without additives *One or more chronic illnesses with mild exacerbation, progression or side effects of treatment *Two or more stable chronic illnesses *Undiagnosed new problem with uncertain prognosis *Acute illness with systemic symptom(s) e.g., pneumonitis, colitis *Acute complicated injury, e.g., Head injury with brief loss of consciousness *Physiologic test under stress e.g., stress echo *Minor surgery with identified risk factors *Diagnostic endoscopy with no identified risk factors *Elective major surgery (open, percutaneous, or endoscopic) with no identified risk factors *One or more chronic illnesses with severe exacerbation, progression, or side effects of treatment * Cardiovascular imaging study with contrast with identified risk factors *Acute or chronic illnesses or injuries that may pose a threat to life or bodily functions e.g., acute MI, severe respiratory distress (4) *Abrupt change in neurologic status, e.g., seizure, TIA, weakness or sensory loss *Cardiovascular imaging studies with contrast and no identified risk factors, e.g., cardiac cath *Rx drug management *IV fluids with additives *Obtain fluid from body cavity e.g., lumbar puncture, joint aspiration *Cardiac electrophysiologic test *Diagnostic endoscopies with identified risk factors *Discography *Closed treatment of fracture or dislocation w/o manipulation *Elective major surgery (open, percutaneous, or endoscopic) with idenified risk factors *Emergency major surgery (open, percutaneous, or endoscopic *Parenteral controlled substances *Drug therapy requiring intensive monitoring for toxicity *Decision to DNR or decrease care because of poor prognosis The highest level of risk in any one category determines the overall level of risk. Move highest level reached to line “C” in Box D. O U T P A T I E N T S E R V I C E S OFFICE / OUTPATIENT VISIT, NEW PATIENT E & M CODE HISTORY EXAM 99201 F F 99202 99203 99204 99205 E D C C E D C C MDM S S L M H OFFICE / OUTPATIENT VISIT, ESTABLISHED PATIENT E & M CODE 99211 99212 99213 99214 99215 HISTORY N/A F E D C EXAM N/A F E D C OFFICE / CONSULT, NEW OR ESTABLISHED PATIENT E & M CODE HISTORY EXAM 99241 F F 99242 E E 99243 D D 99244 99245 C C 3 of 3 REQUIRED AVG. TIME 10 C C 20 30 45 60 2 of 3 REQUIRED MDM N/A S L M H MDM S S L AVG. TIME 5 10 15 25 40 3 of 3 REQUIRED AVG. TIME 15 30 40 M H 60 80 ADDITIONAL AUDIT CRITERIA Y N N/A Patient’s name & identifiers on documentation? Documentation found for date of service? Note / Consult signed and dated? Chief Complaint/reason for visit documented? Medical record legible and complete? All documented services billed? Appropriate use of modifiers? Time documented for time-based services? Diagnosis sequencing correct? Resident involved with service? PCE / Teaching Physician rules followed? ABN form completed as appropriate? Chief Complaint Required HPI Elements: Lisa the qualifying statements: 1 - 3 = Brief 4 + = Extended Review of Systems: List the qualifying statements 1 = Problem pertinent 2 - 9 = Extended 10 + = Complete Constitutional Symptoms Eyes Location Ears, Nose, Throat, Mouth Quality Cardiovascular Severity Respiratory Duration Gastrointestinal Timing Genitourinary Context Musculoskeletal Modifying Factors Associated Signs and symptoms Integumentary (Skin and/ or breast) Neurological Psychiatric LOCATION/SITE Endocrine DOCUMENTATION SOURCE Hematologic/Lymphatic SPECIALTY Allergic/Immunlogic COMMENTS: 10 Created by Lisa Sowers 8/8/06 Medical Decision Making Number of Diagnoses or Management Options Selected “PROBLEMS” Box A Problems Self-limited or minor (stable, improved or worsening Established problem (to practitioner) stable, improved Established problem (to practitioner) worsening New problem (to practitioner), no additional work-up planned New problem (to practitioner), additional work-up planned Number Max = 2 Points 1 1 Presenting Problem(s) Results M I N I M A L 2 Max = 1 Box C 3 4 Bring total to line “A” in BOX D *One self-limited or minor problem e.g., cold, insect bite, tinea corporis *Two or more self-limited or minor problems Points L O W Review and/or order clinical lab tests Review and/or order tests in the Radiology section of CPT Review and/or order tests from the Medicine section of CPT 1 1 1 (2) Discussion of test results with performing physician Decision to obtain old records, and/or decision to obtain history from someone other than the patient 1 Amount and/or Complexity of the Data to be Reviewed “DATA” Box B *Acute uncomplicated illness or injury, e.g., cystitis, allergic rhinitis, simple sprain 1 Review and summation of old records, and/or obtaining history from someone other than the patient and/or discussion of the case with another HCP 2 Independent visualization of image, tracing or specimen itself (not simply review of report) 2 Bring total to line “B” in BOX D M O D E R A T E (3) BOX D The highest level reached by 2 Boxes determines the ultimate Medical Decision Making Final Result of Complexity of Medical Decision Making Box D A B C PROBLEM(S) DATA 1 Minimal 1 Minimal 2 of 3 required 3 Multiple 2 Limited 3 Moderate High High RISK Minimal Low (3) Moderate Type of Medical Decision Making Straightforward LOW Moderate Created by Lisa Sowers 8/8/06 4 Extensive 2 Limited 4 *One stable chronic illness, e.g., well-controlled hypertension or non-insulin dependent diabetes, cataracts, BPH H I G H Extensive “RISK” Diagnostic Procedure(s) Ordered *Lab tests requiring venipuncture *Chest X-rays *EKG/EEG *Urinalysis *Ultrasound *Physiologic tests not under stress, e.g., PFT *Non-cardiovascular imaging studies with contrast e.g., barium enema *Superficial needle biopsy *Clinical laboratory tests requiring arterial puncture Risk of Complication and/or Morbidity or Mortality Management Options Selected *Rest *Gargles *Elastic bandages *Superficial dressings *OTC drugs *Minor surgery with no identified risk factors *Physical therapy *Occupational therapy *IV fluids without additives *One or more chronic illnesses with mild exacerbation, progression or side effects of treatment *Two or more stable chronic illnesses *Undiagnosed new problem with uncertain prognosis *Acute illness with systemic symptom(s) e.g., pneumonitis, colitis *Acute complicated injury, e.g., Head injury with brief loss of consciousness *Physiologic test under stress e.g., stress echo *Minor surgery with identified risk factors *Diagnostic endoscopy with no identified risk factors *Elective major surgery (open, percutaneous, or endoscopic) with no identified risk factors *One or more chronic illnesses with severe exacerbation, progression, or side effects of treatment * Cardiovascular imaging study with contrast with identified risk factors *Acute or chronic illnesses or injuries that may pose a threat to life or bodily functions e.g., acute MI, severe respiratory distress (4) *Abrupt change in neurologic status, e.g., seizure, TIA, weakness or sensory loss *Cardiovascular imaging studies with contrast and no identified risk factors, e.g., cardiac cath *Rx drug management *IV fluids with additives *Obtain fluid from body cavity e.g., lumbar puncture, joint aspiration *Cardiac electrophysiologic test *Diagnostic endoscopies with identified risk factors *Discography *Closed treatment of fracture or dislocation w/o manipulation *Elective major surgery (open, percutaneous, or endoscopic) with idenified risk factors *Emergency major surgery (open, percutaneous, or endoscopic *Parenteral controlled substances *Drug therapy requiring intensive monitoring for toxicity *Decision to DNR or decrease care because of poor prognosis The highest level of risk in any one category determines the overall level of risk. Move highest level reached to line “C” in Box D. 11 Box A “Problems” Box A “PROBLEMS” Problems Self-limited or minor (stable, improved or worsening Number of Diagnoses or Management Options Selected Number Points Max = 2 1 Established problem (to practitioner) stable, improved 1 Established problem (to practitioner) worsening 2 New problem (to practitioner), no additional work-up planned New problem (to practitioner), additional work-up planned Max = 1 Results 3 4 Bring total to line “A” in BOX D A chronic or established problem is considered to be new (to practitioner) if they have not previously treated the problem. Each type of problem addressed during the visit is assigned a point value. Self limited/Minor problems and New problems have a maximum point value that can be accumulated. Box A points are cumulative per line. The total point value assigned to Box A is the sum of all cumulative points per line. Box B “Data” Box B “DATA” Amount and/or Complexity of the Data to be Reviewed Points Review and/or order clinical lab tests 1 Review and/or order tests in the Radiology section of CPT 1 Review and/or order tests from the Medicine section of CPT 1 Discussion of test results with performing physician 1 Decision to obtain old records, and/or decision to obtain history from someone other than the patient 1 Review and summation of old records, and/or obtaining history from someone other than the patient and/or discussion of the case with another HCP 2 Independent visualization of image, tracing or specimen itself (not simply review of report) 2 Bring total to line “B” in BOX D The data box does not get a cumulative total per line. In other words, no matter how many lab results you order or review, you only get one point. However, you do get a cumulative total score for the box 13 Box C “Risk” Box C Presenting Problem(s) M I N I M A L *One self-limited or minor problem e.g., cold, insect bite, tinea corporis *Two or more self-limited or minor problems L O W *One stable chronic illness, e.g., well-controlled hypertension or non-insulin dependent diabetes, cataracts, BPH (2) *Acute uncomplicated illness or injury, e.g., cystitis, allergic rhinitis, simple sprain M O D E R A T E (3) H I G H “RISK” Diagnostic Procedure(s) Ordered *Lab tests requiring venipuncture *Chest X-rays *EKG/EEG *Urinalysis *Ultrasound *Physiologic tests not under stress, e.g., PFT *Non-cardiovascular imaging studies with contrast e.g., barium enema *Superficial needle biopsy *Clinical laboratory tests requiring arterial puncture Risk of Complication and/or Morbidity or Mortality Management Options Selected *Rest *Gargles *Elastic bandages *Superficial dressings *OTC drugs *Minor surgery with no identified risk factors *Physical therapy *Occupational therapy *IV fluids without additives *One or more chronic illnesses with mild exacerbation, progression or side effects of treatment *Two or more stable chronic illnesses *Undiagnosed new problem with uncertain prognosis *Acute illness with systemic symptom(s) e.g., pneumonitis, colitis *Acute complicated injury, e.g., Head injury with brief loss of consciousness *Physiologic test under stress e.g., stress echo *Minor surgery with identified risk factors *Diagnostic endoscopy with no identified risk factors *Elective major surgery (open, percutaneous, or endoscopic) with no identified risk factors *One or more chronic illnesses with severe exacerbation, progression, or side effects of treatment * Cardiovascular imaging study with contrast with identified risk factors *Acute or chronic illnesses or injuries that may pose a threat to life or bodily functions e.g., acute MI, severe respiratory distress (4) *Abrupt change in neurologic status, e.g., seizure, TIA, weakness or sensory loss *Cardiovascular imaging studies with contrast and no identified risk factors, e.g., cardiac cath *Rx drug management *IV fluids with additives *Obtain fluid from body cavity e.g., lumbar puncture, joint aspiration *Cardiac electrophysiologic test *Diagnostic endoscopies with identified risk factors *Discography *Closed treatment of fracture or dislocation w/o manipulation *Elective major surgery (open, percutaneous, or endoscopic) with idenified risk factors *Emergency major surgery (open, percutaneous, or endoscopic *Parenteral controlled substances *Drug therapy requiring intensive monitoring for toxicity *Decision to DNR or decrease care because of poor prognosis The highest level of risk in any one category determines the overall level of risk. Move highest level reached to line “C” in Box D. The assessment of risk is based on the risk related to the presenting problem and to the disease process anticipated between the present encounter and the next one. When prescribing OTC meds above the normal manufacture directions for usage, it is considered Rx drug management due to the increased risk. 14 Box D Final Result of Complexity of MDM BOX D The highest level reached by 2 Boxes determines the ultimate Medical Decision Making Final Result of Complexity of Medical Decision Making Box D 2 of 3 required A PROBLEM(S) 1 Minimal 2 Limited 3 Multiple 4 Extensive B DATA 1 Minimal 2 Limited 3 Moderate 4 Extensive C RISK Minimal Low (3) Moderate High Type of Medical Decision Making Straightforward LOW Moderate High The medical decision making level is determined in this box. The cumulative totals from Box A and B are transferred to this box. The highest level of risk in Box C is transferred to this box. The overall level of medical decision making is determined by the highest level reached by two boxes. 15 Example Moderate Problem (99214) Number of Diagnoses or Management Options Selected “PROBLEMS” Box A Problems Self-limited or minor (stable, improved or worsening Established problem (to practitioner) stable, improved Number Points Max = 2 1 1,1,1 1 Established problem (to practitioner) worsening Results 3 2 New problem (to practitioner), no additional work-up planned Max = 1 New problem (to practitioner), additional work-up planned 3 4 Bring total to line “A” in BOX D A PROBLEM(S) 3 1 Minimal 2 Limited 3 Multiple 4 Extensive 99212 / 99201 & 99202 99213 / 99203 99214 / 99204 99215 / 99205 The cumulative total from Box A is transferred to line A (Problems) of Box D. 16 Example Minimal Data (99212) Amount and/or Complexity of the Data to be Reviewed “DATA” Box B Points Review and/or order clinical lab tests 1 Review and/or order tests in the Radiology section of CPT 1 Review and/or order tests from the Medicine section of CPT 1 Discussion of test results with performing physician 1 Decision to obtain old records, and/or decision to obtain history from someone other than the patient 1 Review and summation of old records, and/or obtaining history from someone other than the patient and/or discussion of the case with another HCP 2 Independent visualization of image, tracing or specimen itself (not simply review of report) 2 Bring total to line “B” in BOX D B DATA 1 1 Minimal 2 Limited 3 Moderate 4 Extensive 99212 / 99201 & 99202 99213 / 99203 99214 / 99204 99215 / 99205 The cumulative total from Box B is transferred to line B (Data) of Box D. 17 Example Moderate Risk (99214) Presenting Problem(s) M I N I M A L Diagnostic Procedure(s) Ordered *One self-limited or minor problem e.g., cold, insect bite, tinea corporis *Two or more self-limited or minor problems L O W *One stable chronic illness, e.g., well-controlled hypertension or non-insulin dependent diabetes, cataracts, BPH (2) *Acute uncomplicated illness or injury, e.g., cystitis, allergic rhinitis, simple sprain M O D E R A T E (3) H I G H Risk of Complication and/or Morbidity or Mortality “RISK” Box C requiring *Lab*Lab teststest requiring venipuncture venipuncture *Chest X-rays *EKG/EEG *Urinalysis *Ultrasound *Physiologic tests not under stress, e.g., PFT *Non-cardiovascular imaging studies with contrast e.g., barium enema *Superficial needle biopsy *Clinical laboratory tests requiring arterial puncture Management Options Selected *Rest *Gargles *Elastic bandages *Superficial dressings *OTC drugs *Minor surgery with no identified risk factors *Physical therapy *Occupational therapy *IV fluids without additives *One or more chronic illnesses with mild exacerbation, progression or side effects of treatment *Two or more stable *Two or more stable chronic chronic illnesses illnesses *Undiagnosed new problem with uncertain prognosis *Acute illness with systemic symptom(s) e.g., pneumonitis, colitis *Acute complicated injury, e.g., Head injury with brief loss of consciousness *Physiologic test under stress e.g., stress echo *Minor surgery with identified risk factors *Diagnostic endoscopy with no identified risk factors *Elective major surgery (open, percutaneous, or endoscopic) with no identified risk factors *One or more chronic illnesses with severe exacerbation, progression, or side effects of treatment * Cardiovascular imaging study with contrast with identified risk factors *Cardiovascular imaging studies with contrast and no identified risk factors, e.g., cardiac cath *IV fluids with additives *Obtain fluid from body cavity e.g., lumbar puncture, joint aspiration *Acute or chronic illnesses or injuries that may pose a threat to life or bodily functions e.g., acute MI, severe respiratory distress (4) *Abrupt change in neurologic status, e.g., seizure, TIA, weakness or sensory loss drug management *RxRX drug management *Cardiac electrophysiologic test *Diagnostic endoscopies with identified risk factors *Discography *Closed treatment of fracture or dislocation w/o manipulation *Elective major surgery (open, percutaneous, or endoscopic) with idenified risk factors *Emergency major surgery (open, percutaneous, or endoscopic *Parenteral controlled substances *Drug therapy requiring intensive monitoring for toxicity *Decision to DNR or decrease care because of poor prognosis The highest level of risk in any one category determines the overall level of risk. Move highest level reached to line “C” in Box D. C RISK Minimal Low (3) Moderate High 99212 / 99201 & 99202 99213 / 99203 99214 / 99204 99215 / 99205 The highest level of risk in Box C is transferred to line C (Risk) of Box D. 18 Example Moderate MDM (99214) BOX D The highest level reached by 2 Boxes determines the ultimate Medical Decision Making Final Result of Complexity of Medical Decision Making Box D 2 of 3 required A PROBLEM(S) 1 Minimal 2 Limited 3 Multiple 4 Extensive B DATA 1 Minimal 2 Limited 3 Moderate 4 Extensive C RISK Minimal Low (3) Moderate High Type of Medical Decision Making Straightforward LOW Moderate High 99212 / 99201 & 99202 99213 / 99203 99214 / 99204 99215 / 99205 This is how Box D should look after bringing the information forward from the other boxes. To determine the overall level of Medical Decision Making, drop off the lowest box circled. The level of MDM is then determined by the location of the next box circled. A point to remember when selecting the level of MDM is that two boxes must meet or exceed the same level to qualify for that level. 19 Example Moderate MDM (99214) BOX D The highest level reached by 2 Boxes determines the ultimate Medical Decision Making Final Result of Complexity of Medical Decision Making Box D 2 of 3 required A PROBLEM(S) 1 Minimal 2 Limited 3 Multiple 4 Extensive B DATA 1 Minimal 2 Limited 3 Moderate 4 Extensive C RISK Minimal Low (3) Moderate High Type of Medical Decision Making Straightforward LOW Moderate High 99212 / 99201 & 99202 99213 / 99203 99214 / 99204 99215 / 99205 20 21 Time Based Services When to bill a visit based on “Time” If counseling and/or coordination of care dominates (more than 50%) the face-to-face contact with the patient and/or family then time is the key factor in determining the level of service. Report the code that reflects the total time of the patient visit (history, exam, medical decision making + counseling) Typical Time New Patient Typical Time Established Patient 99201 – 10 minutes 99202 – 20 minutes 99203 – 30 minutes 99204 – 45 minutes 99205 – 60 minutes 99212 – 10 minutes 99213 – 15 minutes 99214 – 25 minutes 99215 – 40 minutes Examples 25 minute visit, established patient 15 minutes Counseling 10 minutes History, Exam, Medical Decision Making ASK YOURSELF: Is the service based on time or history, exam, medical decision making? Answer: Time What is the total time of the visit? Answer: 25 minutes What is the appropriate visit code to report based on the “typical time” of 40 minutes for an established patient? Answer: 99214 25 minute visit, new patient 15 minutes Counseling 10 minutes History, Exam, Medical Decision Making (detailed history and exam, moderate complexity medical decision making) ASK YOURSELF: Is the service based on time or history, exam, medical decision making? Answer: Time What is the total time of the visit? Answer: 25 minutes What is the correct code based on History, Exam and Medical Decision Making? Answer: 99203 22 Consultation vs. Referral Consultation Must be requested by the patient’s attending physician Attending physician must document the need for a consultation in the medical record The patient presents with suspected problem or condition Consultant must render an opinion or advice Consultant may initiate diagnostic and/or therapeutic services A formal response containing the opinion or advice must be submitted to the attending physician by the consultant Office or Other Outpatient Consultations CPT 99241 – 99245 Referral Involves the transfer of care of the patient from one physician to another Patient presents with known problem or condition Initial patient visit CPT 99201 – 99205 Established patient visit CPT 99211 - 99215 No written response required Initial Inpatient Consultation CPT 99251 - 99255 Referring physician name required in Box 17 of the HCFA (referring physician field) Remember the three “R’s” for a consultation: Request, Render & Response 23