Prevalence and risk factors of Taiwanese microalbuminuric type 2
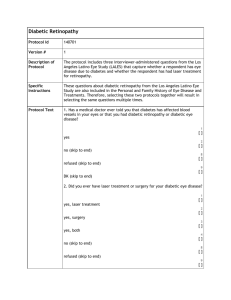
advertisement

Prevalence and risk factors of Taiwanese microalbuminuric type 2 diabetic mellitus with and without diabetic retinopathy Min-Shien Chung*, Jong-Jer Lee**, Chien-Te Lee***, Feng-Chih Shen*, Hsi-Kung Kuo**, Siang-Ting Huang*, Terry Ting-Yu Chiou***, Cheuk-Kwan Sun**** , Kuender D. Yang*****, Rue-Tsuan Liu* Division of Metabolism, Department of Internal Medicine, Chang Gung Memorial Hospital Kaohsiung Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan * Department of Ophthalmology, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan ** Division of Nephrology, Department of Medicine, Chang-Gung Memorial Hospital, Kaohsiung Medical Center, Chang-Gung, University College of Medicine, Kaohsiung, Taiwan*** Division of general surgery, Department of surgery, Chang Gung Memorial Hospital - Kaohsiung Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan **** Department of Medical Research, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan ***** Running title: Retinopathy in microalbuminuric diabetes Correspondence author: Dr. Rue-Tsuan Liu, Division of Metabolism, Department of Internal Medicine, Chang Gung Memorial Hospital - Kaohsiung Medical Center, Kaohsiung, Address: 123 Ta-Pei Road, Niao-Sung Hsiang, Kaohsiung Hsien 833, Taiwan Tel: 886-7-7317123 ext.8302 Fax: 886-7-7322402 Abstract Background: Although microalbuminuria in diabetic patients is a well-known manifestation of diabetic nephropathy, it does not necessarily indicate the presence of other microvascular complication such as diabetic retinopathy (DR). This study aims at determining the prevalence and clinical characteristics of diabetic retinopathy in microalbuminuric patients with type 2 diabetes. Methods: A total of 417 microalbuminuric type 2 diabetic patients were enrolled in this cross-sectional cohort study. Demographic characteristics of patients, serum biochemistry [i.e. HbA1c, serum total cholesterol, triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, uric acid, albumin, creatinine, high sensitive C-reactive protein (hsCRP)] and hematological parameters (i.e. complete blood count, and differential white count) were recorded and analyzed. The presence of retinopathy including background diabetic retinopathy, non-proliferative retinopathy, or proliferative retinopathy, was determined by an experienced ophthalmologist by fundus photography. Logistic regression analysis was performed to identify the independent risk factors of DR. Results: The prevalence of DR was 46.2%. Independent risk factors included the insulin use (OR: 3.437, P=0.001), presence of hypertension (OR: 2.671, P=0.015), DM duration (OR: 1.063, P=0.013), age at DM diagnosis (OR: 0.970, P=0.029), triglyceride (OR: 0.995, P=0.017), hsCRP (OR: 0.773, P=0.006), hemoglobin (OR: 0.713, P=0.000). Conclusions: Use of insulin, presence of hypertension, earlier age at DM diagnosis, longer DM duration, lower serum level of triglyceride and high sensitive C-reactive protein, and reduced hemoglobin are independently associated with an increased prevalence of DR in type 2 diabetic patients with microalbuminuria. Key words: type 2 diabetes, microalbuminuria, diabetic retinopathy, risk factor Introduction Microalbuminuria in type 2 diabetes may be an early clinical manifestation of diabetic nephropathy, although it can also result from other clinical situations such as hypertension or waist circumference.1 In type 1 diabetes, microalbuminuria is closely associated with microangiopathy, such as diabetic retinopathy (DR).2 Although this association is also present in type 2 diabetes, some of these patients does not appear to reflect generalized microvascular damage.3 Although the prevalence and risk factors for DR in type 2 diabetes have been extensively investigated,4-7 few data exist addressing the issue of clinical characteristics distinguishing microalbuminuric type 2 diabetic patients with DR from those without. This cross-sectional cohort study aims at determining the prevalence and characteristics of DR in patients with type 2 diabetes who have microalbuminuria. Materials and methods Study setting, inclusion and exclusion criteria A cross-sectional study was performed in 1,715 diabetic patients attending a single outpatient diabetic clinic managed by one diabetologist (Rue-Tsuan Liu) for more than one year at Chang Gung Memorial Hospital- Kaohsiung medical center between April 2008 and November 2008. Of all patients, 46 were diagnosed as type 1 diabetes and excluded from this study. Fourteen patients with prolonged indwelling Foley catheter, repeated urinary tract infection, chronic glomerulonephritis, or receiving chemotherapy for malignant diseases were also excluded. Study parameters and definitions Urinary albumin concentration was measured by random daytime urine samples. Albumin excretion rate (AER) was defined entirely by calculation of albumin-to-creatinine ratio (ACR) in urine specimen. The definitions of normoalbuminuria (NA), microalbuminuria (MA), and macroalbuminuria (MAA) were an ACR <0.03 mg/mg once, 0.03 – 0.3 mg/mg, and >0.3 mg/mg in two urine samples collected, respectively. Retinopathy was determined through fundus photography by an experienced ophthalmologist blinded to the study. DR was defined as background diabetic retinopathy (BDR), non-proliferative retinopathy (NPDR), or proliferative retinopathy (PDR). Finally, a total of 417 microalbuminuric patients with (n=193) or without (n=224) retinopathy were recruited in the study. Prevalence of DR in different DM duration groups (<5 years, 5-10 years, 11-15 years, and >15 years) was also analyzed. Each patient participated in a detailed interview regarding his or her personal disease, smoking and drinking history by two trained interviewers. The data compiled for this study included age, age at DM diagnosis, gender, duration of diabetes, body height and weight (for the calculation of BMI), drinking and smoking (defined as current smoker and ex-smoker who had quitted smoking irrespective of the duration). Neuropathy was defined as abnormal vibration perception of the tuning fork.8 Coronary heart disease (CHD) was defined as acute myocardial infarction, coronary artery disease confirmed by coronary angiography, and presentations of typical angina pectoris. Blood pressure was obtained from the upper limbs with the patients in supine position, using an automated device which simultaneously measured bilateral brachial and ankle blood pressure using the modified oscillometric pressure sensor method (BP-203RPE; Colin, Komaki, Japan). Hypertension was defined as a systolic blood pressure of >140 mmHg and/or a diastolic blood pressure >90 mmHg, or if the patients were receiving antihypertensive treatment. Insulin use was defined as any insulin treatment alone or in combination with oral antidiabetic agents. Metabolic syndrome was defined as the fulfillment of at least three of the following criteria: (1) Waist circumference >90 cm for men and >80 cm for women, (2) Serum triglyceride >150mg/dL, (3) Serum high-density lipoprotein (HDL) level <40 mg/dL, (4) Elevated blood pressure (systolic blood pressure >130 mmHg and/or diastolic blood pressure >85 mmHg, or previous diagnosis of hypertension) and (5) Increased fasting plasma glucose (>100 mg/dL) or previous diagnosis of DM. Venous blood samples were collected for measurements of total cholesterol, triglycerides, HDL cholesterol, low-density lipoprotein (LDL) cholesterol, uric acid, albumin after 12 hours fasting, serum creatinine, HbA1c, hsCRP, complete blood count, and differential count. Two blood samples were obtained for serum hsCRP analysis. Data were discarded when a hsCRP level >10 mg/l. The average hsCRP level was chosen for each patient. HsCRP was measured with the cardiophase high-sensitivity nephelometric method (Dade Behring, Marburg, Germany) via a Behring Nephelometer II Analyzer. The lowest detection limit was <0.15 mg/l. Mean intra-assay coefficients of variance were less than 3.5% in our laboratory. Creatinine concentrations in plasma and urine were determined with a Wako Creatinine-Test kit by the Jaffe method (Wako Pure Chemicals, Osaka, Japan). Albumin concentrations were determined by immunonephelometry (Dade-Behring, Marburg, Germany). The absolute count of a leukocyte subtype was calculated as the product of the percentage of each subtype and the total leukocyte count. Patients with WBC >10 x 1012/l or WBC <4 x 1012/l and/or those with hemoglobin of MCV >100 fl or MCV <80 fl were excluded. Patients with platelet <150 x 1012/l or >400 x 1012/l were also excluded. Hemoglobin level was compared among the three different DR groups (Non-DR, BDR + NPDR, and PDR). Estimated glomerular filtration rate (eGFR) was calculated by the modified Diet and Renal Disease (MDRD) equation. The Human Research Ethics Committee of our hospital approved this study and informed consent was obtained from each patient. Statistical analysis Data are shown as means ± SD or percentage. The Statistical Package for Social Science program (SPSS for Windows, version 13.0; SPSS) was used to perform the statistical analysis. The independent t-test or ANOVA were used for comparisons between different groups for continuous variables and the Chi-square test was used for categorical variables. All parameters significantly different between groups with or without retinopathy were enrolled in logistic regression analysis the results of which were shown as odds ratio (OR) and 95% confidence interval (CI). P-value less than 0.05 is considered statistically significant. Results A total of 417 type 2 diabetic patients were included in this cross-sectional study. The mean age of the study subjects was 64.9 ± 10.8 years (range, 25-94), and the mean duration of diabetes was 11.4 ± 6.5 years (range, 1-39). The prevalence of background diabetic nephropathy, non-proliferative retinopathy or proliferative retinopathy was 29.0%, 5.0%, and 12.2%, respectively (Table 1). The patients’ demographic characteristics and relevant laboratory parameters between groups with or without retinopathy are shown in Table 2. Retinopathy in microalbuminuric type 2 diabetic patients was found to be positively associated with female gender, habit of drinking, use of insulin, age at DM diagnosis, DM duration, presence of hypertension, neuropathy, and stroke. Negative correlation was noted in the level of total cholesterol, triglyceride, HDL-cholesterol, total cholesterol to HDL-cholesterol ratio, albumin and hemoglobin. Independent risk factors included the use of insulin (OR: 3.437, 95% CI: 1.629 – 7.653, P=0.001), presence of hypertension (OR: 2.671, 95% CI: 1.206 – 5.917, P=0.015), DM duration (OR: 1.06 3, 95% CI: 1.013 – 1.115, P=0.013), age at DM diagnosis (OR: 0.970, 95% CI: 0.944 – 0.997, P=0.029), triglyceride (OR: 0.995, 95% CI: 0.992 – 0.999, P=0.017), hsCRP (OR: 0.773, 95% CI: 0.644 – 0.930, P=0.006), hemoglobin (OR: 0.713, 95% CI: 0.603 – 0.843, P=0.000) (Table 3). Hemoglobin concentration of the three DR groups (i.e. Non-DR, BDR + NPDR, and PDR) was 13.5 ± 1.7, 12.8 ± 1.9, 12.3 ± 1.7 mg/dL, respectively, and significantly different among the three DR groups (P =0.000, followed by LSD test to compare group means) (Figure 1). DR prevalence was 21.6, 29.8, 58.7 and 74.0% in the four DM duration groups (i.e. <5 years, 5-10 years, 11-15 years, and >15 years) (P =0.000) (Figure 2). Discussion In this hospital-based cross-sectional study, DR was noted in 46.2% of type 2 diabetic patients with microalbuminuria. The prevalence of diabetic retinopathy in the present study was similar to that found in two previous cross-sectional hospital-based studies with figures of 43.4 and 40.3 %, respectively.4,9 Thus, our results and those of other studies suggest that longer duration of DM may be required for the development of DR in comparison to the development of diabetic nephropathy in type 2 diabetic patients. Alternatively, these results confirm the heterogeneity of microalbuminuria in type 2 diabetes. In this study, use of insulin, hypertension, earlier age at DM diagnosis, longer DM duration, lower serum level of triglyceride and hsCRP and reduced hemoglobin were all independently associated with the occurrence of DR in type 2 diabetic patients with microalbuminuria. Of the risk factors identified in our cohort, hypertension and longer DM duration have been the most consistently reported in other studies. In the United Kingdom Prospective Diabetes Study (UKPDS), longer duration of diabetes and hypertension have been shown to contribute to the development of DR in type 2 diabetes.10 In this cross-sectional study, we demonstrated that longer duration of diabetes was significantly associated with DR in type 2 diabetes with microalbuminuria (Table 3) with the odds ratio of 1.063. It must be noted, however, that the prevalence of DR was reported to be rapidly increasing when DM duration was longer than 10 year.4,9,11 Similar findings were observed in this study (Figure 2), in agreement with a comparable series described previously in Korean type 2 diabetes with microalbuminuria.9 Our study and those of other investigators12,13 found that the use of insulin was independently associated with DR in type 2 diabetes. In line with our previous studies of peripheral arterial disease and diabetic nephropathy in type 2 diabetes,14,15 we consistently demonstrated that insulin use was an independent risk factor for diabetic chronic complications. Use of insulin for glycemic control has been recommended in type 2 diabetic patients with varying degree of loss ofβ cell function.16 In the clinical practice of the author (R-T Liu) and perhaps in most diabetologists in Taiwan, insulin treatment begins when type 2 diabetic patients experience oral antidiabtic drug failure. At this point, most of patients might already have developed microvascular complications. Therefore, it would not be surprising that use of insulin was an independent factor for DR. Many studies report an independent association between either higher HbA1c or higher systolic blood pressure and DR in type 2 diabetic patients upon multivariate analysis.4,5,7 In this cross-sectional cohort analysis, we observed a tendency for higher HbA1c and higher systolic blood pressure among those with retinopathy compared to those without, albeit short of significance. Failure to replicate the results of previous studies could be due to the intensification of glycemic and blood pressure control in our patients. The impact of age at diagnosis of type 2 diabetes on the risk of developing retinopathy is unclear. In this cross-sectional analysis, earlier age at DM diagnosis is an independent risk factor for DR. This observation is compatible with a previous finding of an association between earlier age at DM diagnosis and DR in Non-Chinese population.17 Interestingly, this relationship was observed not only in diabetic retinopathy, but also in other chronic complications we studied (unpublished data). Anemia is associated with an increased risk of the vascular complications of diabetes including nephropathy18-20 and retinopathy.21-23 Here, we show that the degree of anemia was proportional to the severity of DR in type 2 diabetic patients with microalbuminuria (Figure 1). Our results confirm previous observation of the relationship between reduced hemoglobin level and DR.24 These findings lend support to the hypothesis that anemia may modulate the activity of pathways that lead to progressive end-organ damage in diabetes.23 Recent developments indicate that the classical pathophysiological determinants of diabetic microangiopathy, namely hyperglycemia, and hypertension are accompanied by heightened inflammatory activity, endothelial dysfunction, and disturbed coagulation, and these processes may constitute final common pathways to the vascular complications of diabetes.25 It is noteworthy that both serum levels of triglyceride and hsCRP were negatively and independently associated with DR in this study. These findings were not limited to the microalbuminuric subgroup of type 2 diabetes we studied. In analysis of our type 2 diabetes cohort regardless of their albuminuria status, same results for hsCRP were observed (unpublished data). Elevated triglyceride levels have been shown to independently increase the likelihood of albuminuria in type 2 diabetes in several studies including ours.1,15,26,27 Recent reports and our study (unpublished data) also demonstrated an independent association of higher hsCRP levels with albuminuria in subjects with type 2 diabetes.27,28 The significant association of hsCRP with albuminuria supports the role of inflammation in diabetic nephropathy. However, the relationship between triglyceride, or hsCRP with DR was controversial.5-7, 21, 22, 29-33 Most, but not all, studies did not find a significant association between higher triglyceride or higher hsCRP levels and DR in type 2 diabetic subjects. These results suggest different pathogenesis between DN and DR in type 2 diabetes. The results presented for the current study need to be interpreted in the context of the study’s limitations. First, the cross-sectional nature of the present study limits assessment of the causal relationship between the independent risk factors we identified and occurrence of diabetic retinopathy in type 2 diabetic patients with microalbuminuria. A prospective study should be undertaken to confirm its causality. Second, since our study cohort was hospital-based and from one diabetologist, selection bias was a potential confounding factor. Thus, the generalizability of our study findings to the general diabetic population requires further investigation. Despite these limitations, there are several strengths involved in the current study. This study involved a well characterized and sufficient sample size, a cohort design and a comprehensive risk factor analysis. Furthermore, all patients were treated by a single physician, which minimized potential bias during treatment and follow-up. In conclusion, use of insulin, presence of hypertension, earlier age at DM diagnosis, longer DM duration, lower serum level of triglyceride and hsCRP, and reduced hemoglobin are independently associated with an increased prevalence of diabetic retinopathy in type 2 diabetes with microalbuminuria. Further studies are required to confirm the reproducibility of these results and its causal relationship. Reference 1. Retnakaran R, Cull CA, Thorne KI, Adler AI, Holman RR, Group US. Risk factors for renal dysfunction in type 2 diabetes: U.K. Prospective Diabetes Study 74. Diabetes 2006 Jun 1;55(6):1832-9. 2. Satchell SC, Tooke JE. What is the mechanism of microalbuminuria in diabetes: a role for the glomerular endothelium? Diabetologia 2008 May 1;51(5):714-25. 3. Fioretto P, Stehouwer CD, Mauer M, Chiesura-Corona M, Brocco E, Carraro A, et al. Heterogeneous nature of microalbuminuria in NIDDM: studies of endothelial function and renal structure. Diabetologia 1998 Feb 1;41(2):233-6. 4. Manaviat MR, Afkhami M, Shoja MR. Retinopathy and microalbuminuria in type II diabetic patients. BMC Ophthalmol 2004 Jan 1;4:9. 5. Tapp RJ, Shaw JE, Harper CA, de Courten MP, Balkau B, McCarty DJ, et al. The prevalence of and factors associated with diabetic retinopathy in the Australian population. Diabetes Care 2003 Jun 1;26(6):1731-7. 6. Stratton IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, Manley SE, et al. UKPDS 50: risk factors for incidence and progression of retinopathy in Type II diabetes over 6 years from diagnosis. Diabetologia 2001 Feb 1;44(2):156-63. 7. van Leiden HA, Dekker JM, Moll AC, Nijpels G, Heine RJ, Bouter LM, et al. Blood pressure, lipids, and obesity are associated with retinopathy: the hoorn study. Diabetes Care 2002 Aug 1;25(8):1320-5. 8. Meijer J-WG, Smit AJ, Lefrandt JD, van der Hoeven JH, Hoogenberg K, Links TP. Back to basics in diagnosing diabetic polyneuropathy with the tuning fork! Diabetes Care 2005 Sep 1;28(9):2201-5. 9. Lee KU, Park JY, Kim SW, Lee MH, Kim GS, Park SK, et al. Prevalence and associated features of albuminuria in Koreans with NIDDM. Diabetes Care 1995 Jun 1;18(6):793-9. 10. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998 Sep 12;352(9131):837-53. 11. McKay R, McCarty CA, Taylor HR. Diabetic retinopathy in Victoria, Australia: the Visual Impairment Project. Br J Ophthalmol 2000 Aug 1;84(8):865-70. 12. Cignarelli M, De Cicco ML, Damato A, Paternostro A, Pagliarini S, Santoro S, et al. High systolic blood pressure increases prevalence and severity of retinopathy in NIDDM patients. Diabetes Care 1992 Aug 1;15(8):1002-8. 13. Wirta O, Pasternack A, Mustonen J, Laippala P, Lähde Y. Retinopathy is independently related to microalbuminuria in type 2 diabetes mellitus. Clin Nephrol 1999 Jun 1;51(6):329-34. 14. Chou C-K, Weng S-W, Chang H-W, Chen C-Y, Su S-C, Liu R-T. Analysis of traditional and nontraditional risk factors for peripheral arterial disease in elderly type 2 diabetic patients in Taiwan. Diabetes Res Clin Pract 2008 Sep 1;81(3):331-7. 15. Shen F-C, Chen C-Y, Su S-C, Liu R-T. The Prevalence and risk factors of diabetic nephropahty in Taiwanese type 2 diabetes—A hospital–based study. Acta Nephrologica 2009 Jun 30;23(2):90-95. 16. Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009 Jan;32(1):193-203. 17. Haffner SM, Mitchell BD, Moss SE, Stern MP, Hazuda HP, Patterson J, et al. Is there an ethnic difference in the effect of risk factors for diabetic retinopathy? Ann Epidemiol 1993 Jan 1;3(1):2-8. 18. Savage S, Estacio RO, Jeffers B, Schrier RW. Urinary albumin excretion as a predictor of diabetic retinopathy, neuropathy, and cardiovascular disease in NIDDM. Diabetes Care 1996 Nov 1;19(11):1243-8. 19. Thomas M, Tsalamandris C, MacIsaac R, Jerums G. Anaemia in diabetes: an emerging complication of microvascular disease. Current diabetes reviews 2005 Feb 1;1(1):107-26. 20. Dikow R, Schwenger V, Schömig M, Ritz E. How should we manage anaemia in patients with diabetes? Nephrol Dial Transplant 2002 Jan 1;17 Suppl 1:67-72. 21. Anan F, Masaki T, Ito Y, Eto T, Umeno Y, Eshima N, et al. Diabetic retinopathy is associated with visceral fat accumulation in Japanese type 2 diabetes mellitus patients. Metab Clin Exp 2010 Mar 1;59(3):314-9. 22. Jia Z-t, Liu C-y, Li H. [Changes of the concentration of serum ischemia modified albumin and high sensitivity C-reactive protein in type 2 diabetic patients with retinopathy]. Zhonghua Yan Ke Za Zhi 2009 Sep 1;45(9):805-8. 23. Thomas MC, Cooper ME, Rossing K, Parving HH. Anaemia in diabetes: Is there a rationale to TREAT? Diabetologia 2006 Jun 1;49(6):1151-7. 24. Qiao Q, Keinänen-Kiukaanniemi S, Läärä E. The relationship between hemoglobin levels and diabetic retinopathy. J Clin Epidemiol 1997 Feb 1;50(2):153-8. 25. Goldberg RB. Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J Clin Endocrinol Metab 2009 Sep 1;94(9):3171-82. 26. Cederholm J, Eliasson B, Nilsson PM, Weiss L, Gudbjörnsdottir S, Register SCotSND. Microalbuminuria and risk factors in type 1 and type 2 diabetic patients. Diabetes Res Clin Pract 2005 Mar 1;67(3):258-66. 27. Fu C-C, Wu D-A, Wang J-H, Yang W-C, Tseng C-H. Association of C-reactive protein and hyperuricemia with diabetic nephropathy in Chinese type 2 diabetic patients. Acta Diabetol 2009 Jun 14;46(2):127-34. 28. Gomes MB, Nogueira VG. Acute-phase proteins and microalbuminuria among patients with type 2 diabetes. Diabetes Res Clin Pract 2004 Oct 1;66(1):31-9. 29. Spijkerman AMW, Gall M-A, Tarnow L, Twisk JWR, Lauritzen E, Lund-Andersen H, et al. Endothelial dysfunction and low-grade inflammation and the progression of retinopathy in Type 2 diabetes. Diabet Med 2007 Sep 1;24(9):969-76. 30. van Hecke MV, Dekker JM, Nijpels G, Moll AC, Heine RJ, Bouter LM, et al. Inflammation and endothelial dysfunction are associated with retinopathy: the Hoorn Study. Diabetologia 2005 Jul 1;48(7):1300-6. 31. Nguyen TT, Alibrahim E, Islam FMA, Klein R, Klein BEK, Cotch MF, et al. Inflammatory, hemostatic, and other novel biomarkers for diabetic retinopathy: the multi-ethnic study of atherosclerosis. Diabetes Care 2009 Sep 1;32(9):1704-9. 32. Kang ES, Kim HJ, Ahn CW, Park CW, Cha BS, Lim SK, et al. Relationship of serum high sensitivity C-reactive protein to metabolic syndrome and microvascular complications in type 2 diabetes. Diabetes Res Clin Pract 2005 Aug 1;69(2):151-9. 33. Tsunoda K, Arita M, Yukawa M, Ueyama M, Furuta M, Nakagawa T, et al. Retinopathy and hypertension affect serum high-sensitivity C-reactive protein levels in Type 2 diabetic patients. J Diabetes Complicat 2005 Jan 1;19(3):123-7.