722 - American Medical Association
advertisement

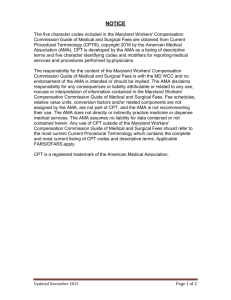
AMERICAN MEDICAL ASSOCIATION HOUSE OF DELEGATES Resolution: 722 (A-05) 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 Introduced by: Virginia Delegation Subject: Consideration of End User Licensing Limitations of CPT4 Referred to: Reference Committee G (Virginia T. Latham, MD, Chair) Whereas, Our American Medical Association holds copyright in Current Procedural Terminology (CPT) and use or reprinting of CPT in any product or publication requires a license; and Whereas, The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (CCI) to promote national correct coding methodologies and to eliminate improper coding; and Whereas, Although the CPT methodology remains the dominant coding method and the CCI editing system promoted by CMS has gained wide acceptance, there continue to be problems related to the interpretation of codes by many health plans in the processing and payment of claims; and Whereas, Significant variance occurs with regard to bundling edits and the use of modifiers across health plans, which has resulted in extreme difficulty in assessing health plan fee schedules, denied claims, delayed payment of claims, inconsistencies in claims submission and processing across plans in which physicians participate, increasing requests for additional documentation, and increasing numbers of audits; and Whereas, The “customization” of CPT coding edits by plans is often contradictory to the accepted standard of care for certain related procedures and is often declared by the plan to be “proprietary” thereby making it difficult if not impossible to determine what the correct and current coding conventions are for any one plan at any specific time; and Whereas, The consistency in the use and application of CPT coding conventions across all users (physicians, health plans, and software editing vendors, etc.) would increase processing efficiency and accuracy for all participants; therefore be it RESOLVED, That our American Medical Association examine the obligations of licensees to adhere to the coding rules that are included with Current Procedural Terminology (CPT) and clarify whether the licensing agreement statement “Altering CPT is not permitted” is limited to text alterations or if it includes interpretive alterations as well (Directive to Take Action); and be it further RESOLVED, That our AMA examine the feasibility of establishing uniform CPT editing criteria for all licensees using a “correct coding initiative” approach that would eliminate end-user variance in coding edits and applications across all users and would be enforceable by the licensing agreement. (Directive to Take Action) Resolution: 722 (A-05) Page 2 Fiscal Note: Estimated cost of $16,932 covers staff costs and production to implement the first Resolved clause. As mandated by Resolution 709 (A-04), a study is already underway “on the feasibility of developing a national standard for the utilization of codes, code combinations, and modifiers that is consistent with all CPT codes, guidelines, and conventions, and that would be used by all commercial and governmental payers.” Received: 5/19/05 RELEVANT AMA POLICY H-70.927 Prevention of Misuse of Current Procedural Terminology (CPT) Our AMA: (1) in order to avoid harm to physicians and patients, shall continue to pursue proper use of CPT codes, guidelines and modifiers by software claims editing vendors and their customers; and (2) will explore additional ways to work with state medical associations to provide coding advocacy for members. (Sub. Res. 819, A-00) H-70.937 Bundling and Downcoding of CPT Codes Our AMA: (1) vigorously opposes the practice of unilateral, arbitrary recoding and/or bundling by all payers; (2) makes it a priority to establish national standards for the appropriate use of CPT codes, guidelines, and modifiers and to advocate the adoption of these standards; (3) formulates a national policy for intervention with carriers or payers who use unreasonable business practices to unilaterally recode or inappropriately bundle physician services, and support legislation to accomplish this; and (4) along with medical specialty societies, calls on its members to identify to our AMA specific CPT code bundling problems by payers in their area and that our AMA develop a mechanism for assisting our members in dealing with these problems with payers. (Res. 802, I-98; Reaffirmed: Res. 814, A-00; Modified: Sub. Res. 817; Reaffirmed: BOT Rep. 8, I-00; Reaffirmation I-01; Reaffirmation I-04) H-70.954 Improper Use of AMA-CPT by Carriers/Software Programs Our AMA: (1) continues to seek endorsement of Current Procedural Terminology (CPT) as the national coding standard for physician services; in collaboration with state and specialty societies, will urge the Secretary of HHS and CMS and all other payers to adopt CPT as the single uniform coding standard for physician services in all practice settings; and will oppose the incorrect use of CPT by insurers and others, taking necessary actions to insure compliance with licensing agreements, which include provisions for termination of the agreement; (2) will work with the American Academy of Pediatrics and other specialty societies to support state and federal legislation requiring insurers to follow the coding as defined in the Current Procedural Terminology Manual and interpreted by the CPT Assistant for all contracts in both the public and private sectors, as long as the CPT process is simple, user friendly, and does not undergo frequent changes; and (3) seeks legislation and/or regulation to ensure that all insurance companies and group payers recognize all published CPT codes including modifiers. (Sub. Res. 801, A-97; Appended: Res. 806, A-98; Appended: Res. 814, I-99; Reaffirmed: BOT Rep. 8, I-00; Reaffirmation I-04) H-70.962 Changes in the Bundling of Medical Services by Managed Care Plans Our AMA will introduce or support legislation or regulation that would require that managed care plans be monitored and prohibited from the arbitrary and inappropriate bundling of services to reduce payment to participating physicians; and that the medically indicated patient services such as consultations and diagnostic procedures provided by physicians on the same day be paid on a separate basis in conformity with the AMA Current Procedural Terminology (CPT) coding policy and not inappropriately bundled as they currently are by managed care plans. (Res. 811, A-96; Reaffirmed: Res. 814, A-00; Reaffirmed: BOT Rep. 8, I-00; Reaffirmation I-01) See also: H-70.992 CPT Coding D-70.968 National Standard for Code Combinations D-70.983 Inappropriate Bundling of Medical Services by Third Party Payers