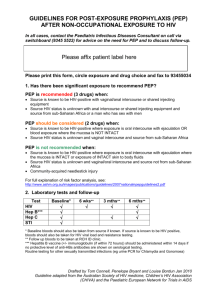
Post Exposure Prophylaxis (PEP)
advertisement

Post Exposure Prophylaxis (PEP) Following Occupational & Non-Occupational Exposure of Adults & Adolescents to HIV; A Trustwide Clinical Guideline Summary statement: How does the document support patient care? This policy provides guidelines for the risk assessment and subsequent management of occupational and nonoccupational exposures to HIV and the use of postexposure prophylaxis. Staff/stakeholders involved in development: Job titles only Consultants & Associate specialists in GU & HIV Medicine Consultants in reproductive & sexual health Consultant in Emergency Medicine Consultants in Occupational Health Occupational Health Manager HIV pharmacist Sexual Health Advisors General Manager Medicine Division: Trustwide Department: Trustwide Responsible Person: Jeannie Baumann, Director of Clinical Services Women and Child Health Author: Dr Emma Rutland, Consultant in Genitourinary & HIV Medicine For use by: All staff Purpose: To provide guidance to WSHT staff who assess patients or members of staff for post exposure prophylaxis following exposure to HIV. To reduce the risk of HIV transmission to WSHT staff or patients following exposure to HIV To outline the processes to be taken by WSHT staff in the event that they are potentially exposed to HIV at work. This document supports: Standards and legislation DoH guidance: HIV post-exposure prophylaxis: Guidance from the UK Chief Medical Officers’ Expert Advisory Group on AIDS. Department of Health. Revised September 2008. National guidelines: Clinical Effectiveness Group (British Association of Sexual Health and HIV). United Kingdom Guideline For The Use Of Post-Exposure Prophylaxis For HIV Following Sexual Exposure. Int J STD & AIDS 2006; 17: 81–92 Key related documents: 1 of 53 WSHT Blood Borne Virus (BBV) Policy (including management of sharps exposure incidents) April 2010 Consent Policy December 2009 Approved by: Divisional Governance/Management Group Women and Child Health Divisional clinical Governance Review Meeting Management Board Approval date: 28 October 2011 / May 2012 Ratified by Board of Directors/ Committee of the Board of Directors n/a Ratification Date: n/a Expiry Date: January 2015 Review date: 28 October 2014 If you require this document in another format such as Braille, large print, audio or another language please contact the Trusts Communications Team Reference Number: To be added by the Library Version date Author Status 1.0 28/10/11 Tracey Rose, Operational Manager on behalf of Dr Emma Rutland draft 2.0 3.0 4.0 2 of 53 Comment Post Exposure Prophylaxis (PEP) Following Occupational & Non-Occupational Exposure of Adults & Adolescents to HIV: A Trust-wide Policy To complement existing Western Sussex Hospitals Trust Policy Blood Borne Virus (BBV) Policy (including management of sharps exposure incidents) April 2010 3 of 53 Contents 1. Introduction 2. Roles and Responsibilities of The Trust, It’s Employees and Departments involved in managing persons exposed to HIV 3. Initial management 4. HIV exposure risk assessment 5. Post Exposure Prophylaxis (PEP) 6. Investigations 7. Other Blood Borne Viruses 8. Follow-Up 9. Availability of the Guidance 10. Specialist Contacts 11. Development of the Guidance 12. Implementation 13. References Appendices: Appendix A - HIV PEP following Occupational Exposure Consultation Record Sheet Appendix B - HIV PEP following non occupational (Sexual / community needlestick / bite) Exposure Consultation Record Sheet Appendix C - PEP (occupational exposure) pathway Appendix D - PEP (non occupational exposure) pathway Appendix E - PEP prescription form Appendix F - PEP consent form Appendix G - Prevalence of HIV in community groups Appendix H - Example of risks from single exposure HIV Appendix I - Letter for source day-case patients Appendix J - Information for prescribers Appendix K - Information for patients Appendix L - flow chart for emergency contraception 4 of 53 1.0 Introduction 1.1 Scope This document should be read in conjunction with the Western Sussex Hospitals NHS Trust blood borne virus (BBV) policy. The BBV policy provides clear guidelines on the management of occupational exposures to blood borne viruses including the initial aspects of dealing with an exposure to HIV and assessment for the use of post exposure prophylaxis (PEP) for HIV. These guidelines focus on the use of PEP for HIV and have been produced for the benefit of clinical staff working in Western Sussex Hospitals NHS Trust who assess patients or members of staff following potential exposure to HIV. This includes staff working in Accident & Emergency Departments, Occupational Health and Sexual Health / HIV Departments. In some cases the exposure will have been occupational. In others the exposure will have been non-occupational, sometimes linked to lifestyle. The guidelines will address risk assessment and subsequent management of exposures to HIV and the use of post-exposure prophylaxis following exposures to HIV. 1.2 Background Healthcare workers (HCW) exposed to blood and body fluids have a low but measurable risk of acquiring blood-borne virus infection through their work. Although the risk of acquiring hepatitis B infection is around 30%, most healthcare workers have now been vaccinated against this infection. The risk of acquiring hepatitis C infection, based on cases reported to the HPA, is 1.6%. The estimated risk from patients with documented HIV is about 0.3% for percutaneous exposure (i.e. accidents where the skin is pierced/broken by a needle or to other sharps incident) and about 0.1% for significant exposure to mucous membranes or non-intact skin (e.g. splashes to the eyes or splashes to areas of the skin that are already broken because of scratches or due to a skin condition). Exposure to intact skin is not considered to pose a risk [1]. 1.3 Rationale for PEP following percutaneous exposure A U.S. case control study concluded that the administration of zidovudine monotherapy as prophylaxis to health care workers occupationally exposed to HIV was associated with an 80% reduction in the risk for occupationally acquired HIV infection. [2] Four factors were associated with increased risk of HIV infection: 1) 2) 3) 4) Deep injury Visible blood on the device which caused the injury Injury with a needle which had been placed in a source patient's artery or vein Terminal HIV-related illness in the source patient It was estimated that the risk for HIV transmission after percutaneous exposures involving larger volumes of blood, particularly if the source patient's viral load was likely to be high, exceeds the average risk of 3 per 1,000. In established HIV infection, the use of combinations of antiretroviral drugs is more potent than zidovudine alone in suppressing viral replication. This, together with the increased prevalence of zidovudine resistance amongst HIV infected people, has led to the introduction of combination antiretroviral drug prophylaxis following occupational exposure to HIV. 5 of 53 Results from animal studies suggest that HIV PEP is most likely to be efficacious if started within the hour 1.4 Rationale for PEP following sexual exposure Rationale for the use of PEP following non occupational sexual exposure (PEPSE) is largely based on data from PEP following percutaneous exposure, a few animal and 2 small prospective studies in humans. Animal studies demonstrate a reduction in HIV seroconversion with the use of antiretroviral drugs following sexual exposure to HIV [3] The use of postnatal AZT given to neonates who were delivered vaginally to HIV positive mothers not on antiretroviral therapy in a subset of the ACTG 076 study demonstrated a protective effect [4] Prospective data on the use of PEPSE is available for men who have sex with men. Two Brazilian studies demonstrated a reduction in HIV seroconversion rates in men utilising PEPSE following high risk HIV exposures [5,6]. 2.0 Roles and Responsibilities of The Trust, It’s Employees and Departments involved in managing persons exposed to HIV The Trust has a duty of care to ensure, so far as reasonably practicable, the health, safety and welfare at work of their employees. It also has a duty to safeguard the health and well-being of patients/clients. The Trust accepts responsibility to protect staff and patients through the development and maintenance of arrangements for: 2.1 Good management of occupational and non-occupational exposure to HIV Overall It is the responsibility of the CEO and Board to ensure that policies, procedures and practices meet the national requirements for management of exposure to HIV. It is the responsibility of the Consultant GUM/HIV at St Richard’s Hospital to champion this policy. The responsibilities of healthcare workers are detailed in the Blood Borne Virus Policy. 2.2 The role of A&E In view of the need for very prompt treatment and the serious consequences of HIV seroconversion, significant occupational exposure to known or possible sources of HIV constitutes a medical emergency. Outside normal working hours, the A&E Department has the responsibility for assessment of occupational exposure and requirement for PEP, and will be the first point of contact for any such exposure, whether or not this arose in the hospital [1]. 6 of 53 Similarly due to the need for prompt treatment with PEP following non occupational sexual exposures to HIV, A&E has the responsibility for assessment for the requirement of PEPSE outside normal working hours [2]. The Trust has a responsibility to ensure that staff in the A&E department are aware of, and have accepted their responsibility to provide cover for PEP where appropriate [1]. For monitoring purposes, PEP consultations will be coded by A&E, Occupational Health and GUM/HIV departments. 2.3 The role of Occupational Health In working hours Occupational Health at WaSH and SRH has the responsibility for assessment of occupational exposure and requirement for PEP for WSHT HCWs. Occupational health at Worthing has the responsibility for assessment of occupational exposure and requirement for PEP for community HCW’s Bank and agency staff who are employed by the organisation should be assessed by occupational health following occupational exposure in working hours. Occupational Health staff to complete PEP consultation sheet and assess the indications for prescribing PEP Occupational Health should also follow up HCWs who do not commence PEP following potential occupational exposure for repeat BBV screening as necessary. Occupational Health should see all HCWs who do commence PEP following potential occupational exposure on at least one occasion for reporting and monitoring requirements. Occupational Health should report confidentially all potential exposures to HIV (regardless of whether PEP was initiated) to the Occupational Exposure Surveillance Team, HIV/STI Department, HPA Centre for Infections, 61 Colindale Avenue, London NW9 5EQ (Tel. 020 8327 7095). In certain circumstances (usually a ‘dangerous occurrence’) it may be necessary to report the event to the Health and Safety Executive under the Reporting of Injuries, Diseases and Dangerous Occurrences (RIDDOR) Regulations 1995. Cases of HIV infection resulting from exposure in the health care setting will also normally be reportable as diseases within the scope of RIDDOR. Occupational health will be responsible for assessment and further management of Hepatitis B prevention following occupational exposure as per the Trust BBV guidelines. 2.4 The role of the GUM/HIV department In clinic hours all non occupational exposures to HIV will be assessed and managed through the Fletcher unit (SRH) or Warren Browne unit (WaSH). The GUM department will provide assessment and further management of Hepatitis B prevention following potential sexual exposure. 7 of 53 The GUM / HIV specialist will be available to give telephone advice on the recommendations for PEP / PEPSE provision in complicated cases during and outside of working hours through the on call GUM / HIV specialist. The GUM / HIV specialist will also be available to give telephone advice on HIV testing source patients in special circumstances. The GUM/HIV departments will follow up all patients commenced on PEP / PEPSE. Source patients of occupational exposures will be tested through their clinical teams. The GUM/HIV department Health advisors will provide support to staff in other areas of the Trust in seeking informed consent for HIV testing. The departments can offer confidential testing under a GUM number if the source patient prefers. They will also provide HIV pre-test discussion for source patients identified following needlestick injuries in day surgery or endoscopy (see section 5.2.3). The GUM / HIV specialists will also take an active role in providing specific training to staff involved in the assessment and provision of PEP / PEPSE. This would include the following staff groups: Medical and nursing staff in A&E Medical and nursing staff in the Department of HIV/GUM Medical and nursing staff in the Department of Occupational Health 3.0 Initial management after possible exposure to HIV 3.1 HCWs sustaining a risk incident Remove the hazard to ensure the incident is not repeated. The source patient should be identified if possible. Establish incident details - date, time, source, nature of injury and any known information about the Source patient (name, DoB, Hospital No., BBV risk factors and status if already known). It is the responsibility of the injured employee to report it immediately to the area manager (e.g. ward sister). Complete an accident / incident / Datix following assessment in Occ health / A&E 3.2 Attend appropriate site for assessment 3.2.1 Following occupational exposure Ring the Sharps injury “hotline” (SRH 01243 788122 x 2405) (WASH 01903 205111 x3037 ) immediately and follow the instructions given. SRH Normal working hours - attend Occupational Health without delay (unless the “hotline” instruction states otherwise) Out of hours - attend Accident and Emergency Department immediately WaSH 8 of 53 Normal working hours - attend Occupational Health without delay (unless the “hotline” instruction states otherwise) Out of hours - attend Accident and Emergency Department immediately Community staff (non WaSH / SRH) Normal working hours - attend Occupational Health (WaSH) without delay (unless the “hotline” instruction states otherwise) Out of hours - attend Accident and Emergency Department immediately 3.2.2 Following non occupational / sexual exposure Patients requesting PEP following sexual exposure should be referred to the Fletcher unit, Chichester or Warren Browne unit, Worthing during clinic hours Out of hours patients should attend Accident and Emergency Department for assessment. Members of the public presenting with community needlesticks / bites should be assessed in the local A&E departments (if not already assessed in primary care) 4.0 HIV exposure risk assessment A risk assessment needs to be made urgently by someone other than the exposed individual. If indicated PEP should be started without delay and ideally within 1 hour of exposure. WSHT staff will be assessed by occupational health, during opening hours, and A&E staff at other times. The risk assessment will assess the need to commence PEP and whether reliance on the standard PEP starter pack is appropriate, or whether a modified prescription is required. It may not be possible to attain immediately all the information required to decide whether PEP is indicated (particularly regarding the source individual). A more thorough risk assessment can be performed later as more information becomes available (including results of HIV test from the source person) to inform a decision whether to change or discontinue the regimen. Starting PEP, where appropriate should not be delayed to await the result of source patient testing. If there is a delay before the exposed person presents for PEP, it is usual practice to offer PEP up to 72 hours after exposure. However its efficacy is likely to fall with increasing delay. Decisions on initiation of PEP more than 72 hours after an occupational exposure should made on individual basis in discussion with the exposure recipient and a GUM/HIV specialist and in full knowledge of the lack of evidence of efficacy [1]. The baseline risk assessment must be documented on an ‘HIV PEP Consultation Record Sheet’ (Appendix A&B) These are available in: St Richards Hospital: A&E, Occupational Health, Fletcher unit Worthing hospital: A&E Southlands: Occupational Health, Warren Browne unit The risk of transmission of HIV depends on the: type of exposure 9 of 53 4.1 the nature of the body fluid involved the volume of body fluid involved the source person Type of exposure The risk of HIV transmission following an exposure from a known HIV positive individual is shown below [7]. Type of exposure Blood transfusion (one unit) Receptive anal intercourse Receptive vaginal intercourse Insertive vaginal intercourse Insertive anal intercourse Receptive oral sex (fellatio) Insertive oral sex (receiving fellatio) Needle–stick injury Sharing injecting equipment Mucous membrane exposure Estimated median (range) risk of transmission per exposure 90-100% 1.11% (0.042-3.0%) 0.1% (0.004-0.32%) 0.082 (0.011-0.38%) 0.06% (0.06-0.065%) 0.02% (0-0.04%) 0% 0.3% (95% CI 0.2%-0.5%) 0.67% #0.63% (95% CI 0.018%-3.47%) HIV # derived from a single study including only small numbers of health care workers exposed to HIV following mucous membrane exposures. This is likely to significantly over estimate the risk. 4.2 Type of Fluid Body Fluids which may pose a risk of HIV Transmission if significant occupational exposure occurs: High Risk Body Fluid Amniotic Fluid Blood Cerebrospinal Fluid Human Breast Milk Pericardial Fluid Peritoneal Fluid Pleural Fluid Saliva in association with dentistry (which is likely to be contaminated with blood even when not visibly so) Semen Synovial Fluid Unfixed Tissues or Organs Vaginal Secretions Any other body fluid which is visibly bloodstained. Exudative or other tissue fluid from burns or skin lesions Laboratory cultures and isolates of HIV 4.3 Volume of Fluid The following increase the risk of HIV transmission: 1. Visible blood on the device which caused the injury. 10 of 53 No Risk Body Fluid (unless visibly blood stained) Faeces Saliva Urine Vomit 2. Injury with a needle which has been placed in a source patient’s artery or vein. 3. Injury involving wide bore needle or extensive laceration. 4.4 Source Person There may be increased risk of HIV transmission if the source person is: 1. Known HIV positive Risk is further increased if the patient has a high plasma HIV viral load / is seroconverting An undetectable plasma HIV viral load in a patient taking antiretroviral therapy reduces the risk Sexually transmitted infections enhance HIV transmission in epidemiological studies and increase HIV shedding from the genital tract. Menstruation or other bleeding may also facilitate transmission 2. Known source but unknown HIV status with recognisable risk factors (see table below): Man who has had sex with men Current or ex-injecting drug use. Lived in, or received blood/blood products in areas of high HIV prevalence e.g. Sub-Saharan Africa, Eastern Europe and Central Asia. Multiple transfusion of blood/blood products in the UK (before 1985) or elsewhere HIV indicator disease e.g. PCP pneumonia 3. Is a sexual contact of any of the above. Risk that source is HIV positive [7] – (Based upon HPA 2008 data) Population Group (aged >15 years) Men who have sex with men UK London Elsewhere in UK Brighton Heterosexuals (region of birth) UK Rest of Europe North America Central and South America Caribbean North Africa and Middle East Sub-Saharan Africa South Asia East and South Asia Australasia Injecting drug users UK London Elsewhere in UK 11 of 53 HIV Prevalence (%) Male 5.2 10.5 3.4 13.7 Female - 0.4 1.2 1.1 1.9 1.2 0.5 6.1 0.5 1.1 0.3 0.3 0.6 0.2 1.1 1.0 0.4 10.3 0.5 0.8 0.2 0.3 0.8 0.2 0.3 0.3 0.3 4.5 The Unknown Source In the event of a potential exposure to an untraceable source (e.g. a needlestick injury from a rubbish bag) it is very usually difficult to justify PEP. PEP is not indicated for discarded needles in the community. In secondary care a risk assessment should be made considering the circumstances of the exposure (eg Known HIV positive patient on ward). Discuss with Occupational Health or GUM/HIV specialist if in doubt. 4.6 Assessing the risk PEP is not a licensed indication for antiretroviral therapy; further information on the indications, benefits and risks of PEP can be found in national guidelines [1,7] In circumstances where the risk of HIV exposure is low and PEP is not recommended the person seeking PEP should be advised that the potential risks of toxicity PEP outweigh the negligible risk of HIV transmission. Appendix H gives an example of risks of HIV transmission after a single episode. Cofactors such as STIs, viral load and bleeding may affect the risk estimate [7] 4.6.1 Recommendations for prescribing PEP after non occupational including sexual exposure to HIV (PEPSE) [7] PEPSE is only recommended where the individual presents within 72 hours of exposure. Within that time frame, it is recommended that PEPSE (if given) should be administered as early as possible. See tables in ‘HIV PEP following non occupational (Sexual / community needlestick / bite) Exposure Consultation Record Sheet’ (Appendix B) for situations for which PEP is recommended Attempt should be made, where possible, to establish the HIV status of the source individual (according to appropriate guidance on HIV testing and consent) as early as possible. It is recommended that strong efforts be made to encourage the individual to notify their partner where possible, and to arrange urgent HIV testing of that partner, as early as possible. • Source individual is known to be HIV positive In this scenario attempts should be made at the earliest possible stage to determine the viral load, resistance profile and treatment history in the source individual. Where the viral load is undetectable it is assumed that the risk of transmission will be significantly reduced. The majority of supporting evidence is derived from heterosexual discordant couples although there are some data among MSM. There are anecdotal reports of transmission where the source is thought to have an undetectable plasma viral load. • Source individual is of unknown status Attempts should be made, where possible, to establish the HIV status of the source individual (according to appropriate guidance on HIV testing and consent) as early as possible. There is growing evidence to suggest that significant cases of PEP can be averted through assertive HIV testing of the source individual. It is therefore recommended that strong efforts be made to encourage the individual to notify their 12 of 53 partner where possible, and for the clinic to arrange urgent HIV testing of that partner, with appropriate guidance on HIV testing and consent, as early as possible. Within the UK at present sources from a group or area of high HIV prevalence include men who have sex with men and individuals who have immigrated to the UK from areas of high HIV prevalence particularly sub-Saharan Africa. (see Appendix G for HIV prevalence rates) Other circumstances: Sexual Assault: It is believed that transmission of HIV is likely to be increased following aggravated sexual intercourse, such as that experienced during sexual assault. Clinicians may therefore consider recommending PEPSE more readily in such situations. Needle-stick injuries in the community: It is not uncommon for individuals to request PEP following a needle-stick injury with a discarded needle in the community. In general PEP is not recommended following these exposures as it is usually not possible to determine i) whether the needle has been used or not and for what purpose, ii) the HIV status of the source and iii) the interval between the needle being used and the exposure. Once blood has dried, HIV dies within a couple of hours. However viable HIV has been shown to persist in syringes and needles up to 30 days depending on temperature and the size of syringe/needle. However there is no data on the transmissibility of this virus. In studies where only small amounts of blood are in the syringe viable HIV cannot be detected after 24 hours Human bites: Requests for PEP following human bites have been reported. In general PEP is not recommended following these exposures as although the risk of transmission following a bite is unknown it is likely to be extremely small. Other considerations regarding PEPSE HIV testing is strongly recommended before commencing PEP or as soon as possible thereafter. Following sexual exposure it is important to consider emergency contraception (Appendix L). Sexual exposure can also place a person at risk of other sexually transmitted infections (including hepatitis B). 5.0 Post Exposure Prophylaxis (PEP) 5.1 Indications If there is a delay before the exposed person presents for PEP, it is usual practice to offer PEP up to 72 hours after exposure. However its efficacy is likely to fall with increasing delay. Decisions on initiation of PEP more than 72 hours after an occupational exposure should made on individual basis in discussion with the exposure recipient and a GUM/HIV specialist and in full knowledge of the lack of evidence of efficacy [1]. 13 of 53 5.1.1 if the patient had a significant exposure to blood or another high-risk body fluid from a source either - known to be HIV infected, or - considered to be at high risk of HIV infection, but where the result of an HIV test has not or cannot be obtained, for whatever reason [1]. 5.1.2 PEP is recommended if: PEP is not recommended: after exposure to low-risk materials (e.g. urine, vomit, saliva, faeces) unless they are visibly bloodstained (e.g. saliva in association with dentistry). where testing has shown that the source is HIV negative, or if risk assessment has concluded that HIV infection of the source is highly unlikely PEP is not indicated for discarded needles in the community. PEP would only be indicated in cases of human bites in very exceptional circumstances (eg where an HIV+ individual with a detectable viral load with blood in their mouth bites another individual where the teeth have broken the skin) Exceptionally, PEP may be indicated following a negative test if there is reason to suspect the source may be seroconverting (i.e. in the window period) [1]. 5.2 Standard PEP A standard course of PEP must be taken for 28 days as in the following table: Starter pack: days 1-5 Drug Truvada Kaletra Strength & Form Combined tablet: Tenofovir 300mg & Emtricitabine 200mg Combined tablet: Lopinavir 200mg & Ritonavir 50mg Dose ONE (1) tablet ONCE a day Duration Days 1-5 TWO (2) tablets TWICE a day With or without food Days 1-5 In addition an anti-emetic and an anti-diarrhoeal agent is routinely prescribed: Domperidone 10mg Tablet ONE(1) tablet THREE times a Pack of 10 day when needed for nausea or vomiting Loperamide 2mg Tablet TWO (2) tablets at the first Pack of 12 sign of diarrhoea or loose bowel motion then ONE(1) tablet when needed thereafter. Maximum of 8 tablets in 24 hrs Then: Days 6-28 (prescribed by Doctor from Fletcher unit / Warren Browne unit) Drug Truvada 14 of 53 Strength & Form Dose Combined tablet: ONE (1) tablet ONCE a day Tenofovir 300mg & Emtricitabine 200mg Duration Days 6-28 Combined tablet: TWO (2) tablets TWICE a day Lopinavir 200mg & With or without food Ritonavir 50mg Kaletra Days 6-28 Although PEP should be continued for 28 days, the exposed person may be advised to stop taking PEP after further information is obtained (e.g. the source tests negative). It is unlikely that all the necessary information will be available when you initially prescribe PEP. Full adherence to PEP is critically important; the patient will need careful flow up and support in achieving this. Symptom control is an important element of this follow up. A Patient Information Leaflet is included with each drug in the starter pack (Appendix K). These drugs are not licensed for PEP, however, the Department of Health recommends them for this indication. These drugs can be prescribed for PEP only on an 'off-label' basis since their use in this context is outside approved indications. A prescription sheet is included for use in all starter packs. (Appendix E) 5.3 PEP Starter Packs and Location Starter packs of PEP will be available in each of the following locations: St Richards Hospital Worthing hospital Southlands hospital A&E Emergency Drug Cupboard Fletcher Pharmacy A&E Emergency Pharmacy Drug unit Cupboard Emergency Drug Cupboard Pharmacy Warren Browne unit Each area will be responsible for ensuring PEP stock available, intact and in date. Starter packs of PEP contain enough medication for 5 days of treatment. During this time the patient will be followed up by the HIV/GUM Department. Patients requiring PEP should be given a starter pack from one of these areas, the balance of the medication will be prescribed at the follow up visit. Rarely it may be necessary to issue 2 packs e.g. to cover a long weekend. The full 1 month course of PEP should not be prescribed at the time when PEP is initiated. 5.4 Consent to PEP The PEP Starter Pack also contains an Information Sheet. It is important that the information on the sheet is understood by the exposed person and that they give verbal informed consent before starting PEP. This consent must be documented on the consultation sheet. 5.5 Variations to standard PEP Advice from a GUM/HIV Specialist Consultant should be sought before deviating from standard PEP. Uncertainty regarding the optimal combination should not be 15 of 53 allowed to delay initiation of PEP. If in doubt start standard PEP as soon as possible and then seek further advice. Information about the virus present in the source patient, previous and current antiretroviral therapy and drug resistance may be relevant when the GUM/HIV specialist chooses alternative PEP drugs. 5.6 PEP: Special Considerations 5.6.1 Paediatric Patients (<16 years of age) This document applies to adults. Specific guidelines on the paediatric management of potential exposure to HIV should be referred to when the exposed person is less than 16 years of age and advice taken from a Paediatric HIV consultant. Children and adolescents under 16 years of age presenting for consideration of PEP, either following needlestick injury or sexual exposure (consensual and following assault) should be referred to the Paediatric Consultant. Paediatric PEP Regimen Outline (following discussion with Paediatric Consultant / advice from the Paediatric Infectious Disease Consultant at St George’s Hospital, London, available via St Georges Hospital switchboard 020 8672 1255): Children who weigh < 40kg should NOT receive Tenofovir (i.e. Truvada) containing PEP but should be offered Kaletra, lamivudine and zidovudine at doses appropriate to their weight and surface area. Adolescents weighing 40kg and above can be treated with the adult PEP regimen. Follow up: All patients under 16 years of age considered for PEP (whether prescribed or not) should be referred for follow up. It is appropriate that patients considered for PEP following sexual exposure should be followed up by the Paediatric Consultant and/or GUM/HIV specialist Following assessment a completed Consultation Record Sheet (see adult proforma) should be faxed to the Consultant Paediatrician and/or GUM/HIV specialist Children prescribed PEP will be followed up by the Consultant Paediatrician 5.6.2 Drug History A full history of current or recent (in the preceding 2 weeks) medication taken by the exposed person (including prescription, OCP, non-prescription, over-thecounter, recreational drug use and herbal preparations) should be taken prior to prescribing PEP. A list of important potential drug interactions is provided in the PEP pack along with instructions for prescribers (Appendix J) The contraceptive effect of oestrogens and progestogens is reduced by Kaletra If in doubt, advice should be sought from the HIV specialist pharmacist during clinic hours, from the on-call pharmacist out of hours or online at www.hivdruginteractions.org/ [8] 16 of 53 5.6.3 Hepatitis B infection in the exposed patient If the exposed patient is HBsAg positive there is a risk of flare of hepatitis after Truvada has been stopped. Therefore baseline Hepatitis B serology should be taken in all patients starting PEP and the GUM /HIV specialist will consider withdrawal of Truvada / change in regimen in these patients when reviewed in clinic. 5.6.4 HIV seroconversion illness or established HIV infection in the exposed patient PEP is not recommended in the context of HIV seroconversion illness or established HIV infection in the exposed patient. 5.6.5 Pregnancy and breast feeding Pregnancy does not preclude the use of HIV PEP. The possibility of pregnancy should always be considered. Urgent pregnancy testing should be arranged for any female worker who cannot rule out the possibility of pregnancy, as part of the assessment consultation. The antiretroviral in pregnancy register has shown no increased risks to the babies of HIV-infected women who have become pregnant whilst taking the drugs used in the PEP starter packs. National guidelines exist for the prescription of antiretroviral therapy in pregnancy [9]. A pregnant health care worker who has experienced an occupational HIV exposure should be counselled about the risks of HIV transmission as per any other health care worker. If started on PEP she will receive extra information about the risks for transmission to her baby, and about what is known and not known about the potential benefits and risks of antiretroviral therapy for her and her baby when she attends the appointment with the HIV specialist. If the exposed person is pregnant or suspects pregnancy then seek specialist advice from an HIV Consultant. If the woman is breast feeding specialist advice from an HIV Consultant should be sought. 5.6.6 Viral drug resistance If the source patient is known to be HIV+ve, exposure to drug resistant HIV should be considered. The resistance profile of HIV from the source will depend on the source’s drug history and may sometimes influence the choice of antiretrovirals used in PEP. Specialist advice from an HIV specialist is required. Starting standard PEP should not be delayed; Truvada/ Kaletra should be started and specialist advice sought thereafter. The GUM/HIV specialist may recommend that blood samples should be taken from the source at baseline (with the patient’s consent) and sent as a high priority for analysis for viral drug resistance genotype. Interpretation of the results and any modifications to the PEP regimen should only be made on advice from an HIV specialist. 5.6.7 HIV exposures in laboratory staff Knowledge about the source virus and originating patient is very important. Specialist advice from an HIV specialist should be sought. Starting standard PEP should not 17 of 53 be delayed; Truvada/ Kaletra should be started and specialist advice sought immediately thereafter. 6.0 Investigations 1. Investigations for the exposed person 2. Investigations for the source person 6.1 Investigations for the exposed person If PEP is not prescribed, consent should be sought for the following: 10ml blood sample for ‘Serum Save’ and sent to virology for storage for 2 years Hepatitis B serology as appropriate (see Trust policy on BBV section 5.7) Testing for HIV and other sexually transmitted infections should be recommended after sexual exposure If PEP is commenced consent should be sought for the following: HIV antibody testing - at earliest opportunity on follow up with GUM/HIV. Hepatitis B serology - all patients FBC U&E, LFTs, glucose, calcium and phosphate Testing for all other sexually transmitted infections should be recommended after sexual exposure Ensure request for copy to be sent to Fletcher unit, Chichester / Warren Browne unit, Worthing 6.1.1 HIV antibody testing After occupational exposures In patients commencing PEP HIV antibody testing should be recommended at or near baseline. This will be carried out at first follow up with sexual health at the Fletcher unit / Warren Browne unit which should be at the earliest opportunity the next working day. Confidential testing will be offered. After non-occupational exposures HIV antibody testing is strongly recommended after sexual exposure (PEPSE). Ideally this should be done before commencing PEP although unnecessary delay in commencing PEP should be avoided If the Fletcher unit / Warren Browne unit is closed at the time of commencing PEPSE patients should attend for testing at their follow up appt with sexual health on the next working day. 6.2 Investigations for the source person This depends on the HIV status of the source person: 6.2.1 Source person known to be HIV+ve 18 of 53 Important information about the source’s virus can be gained from blood tests. It is important that these are taken near to the time of exposure (i.e. within a few days at most). After all significant exposures the GUM/HIV specialist will organise any viral load and resistance tests as required. 6.2.2 Source person of unknown to HIV status: HIV-Ab testing Testing of the source patient is only necessary after a significant exposure. The named Consultant for the source patient or a delegated team member should approach the patient and ask for their informed agreement to HIV testing. This approach should not be undertaken by the exposed worker. In the event of the exposed worker being the Consultant him/herself the approach may be made by a Consultant colleague within the same department or by making arrangements with the GUM / HIV specialist. If the HIV status of the source cannot be established, the exposed person will have the opportunity to consider whether or not to take or continue PEP when followed up in GUM/HIV departments. 6.2.2.1 Pre-test discussion This should include [1]: Details of the incident and the reason for requesting for a test. Wherever possible the identity of the health care worker should not be disclosed. The difficulties of the exposed health care worker's situation should be discussed either in terms of the worker not missing the opportunity to benefit from PEP, or conversely not being subjected unnecessarily to its potentially unpleasant short term and unknown long term side effects. Consent to disclose the test result to the exposed health care worker and Occupational Health. The source person’s right to refuse testing must be respected. The source patient may wish to test confidentially at the Fletcher unit / Warren Browne unit; if so this can be arranged by contacting the relevant department. If the patient has been sedated or has recently had a general anaesthetic the validity of such consent would be open to challenge (see section 5.2.2.4 below). 6.2.2.2 Requesting urgent HIV serology HIV testing available from Monday to Friday. A single 7-10 ml clotted blood sample (no anti-coagulant) Yellow microbiology request form stating exposure incident and stating the name of the exposed HCW. Request: HIV Ag/Ab test plus HepBSag / HCV Ab This should be sent to the microbiology lab and requested as urgent. Results will normally be available on the day of receipt as long as it is received in the lab by 2PM, (or later by arrangement). 19 of 53 6.2.2.2 Results In all cases the result of HIV testing should be communicated to the source patient without delay (and before it is communicated to the exposed worker). The clinical team (Consultant or delegated member of the team) who requested HIV testing should have access to the result from the laboratory and give the result to the patient without delay. The exposed health care worker should have the results communicated to them and receive appropriate advice from occupational health or the GUM/HIV specialist following up their case. If the source tests negative (with no known risk in last 3 months), then PEP can be stopped and HIV testing of the exposed person is not necessary. If the source reported recent possible HIV exposure (window period) PEP may still be recommended [1]. If the source patient tests HIV positive s/he should be referred to the HIV team within 24 hours for ongoing medical care and support. The exposed person should be complete the course of PEP. 6.2.2.3 Patients lacking capacity to consent Where a source patient lacks capacity to consent (e.g. because they are unconscious), his/her tissue etc can only lawfully be tested for serious communicable diseases if it is reasonably held to be in his/her best interests in accordance with the Mental Capacity Act 2005 [1] and the Trust’s Consent Policy. These cases can be discussed with the HIV specialist. 6.2.2.4 Exposures where the source patient is a day case who has been sedated or had a general anaesthetic When a day case patient has been sedated or had a general anaesthetic and a potential exposure incident has occurred no attempt should be made to seek consent for HIV-AgAb testing on the day of the procedure. Given that the patient has been recently sedated the validity of such consent would be open to challenge. The patient should be given a simple, brief but clear verbal explanation of the incident If necessary a translator should be employed Refer the patient to the Fletcher unit, Chichester or Warren Browne unit, Worthing for follow up the next working day. Complete the information on the standard letter in Appendix H and take a photocopy Give the original to the source patient with a brief explanation of its contents Ensure that the patient’s contact details (including home and mobile telephone numbers) and GP are up to date. Fax and/or post the copy of the letter to Fletcher unit or Warren Browne unit At the Fletcher unit / Warren Browne unit the health advisor or nursing staff will: Provide pre-test discussion and seek informed consent for HIV testing 20 of 53 Provide confidential testing which will not form part of their main hospital medical record Give the source patient their results as soon as possible Seek the consent of the source patient for release of results to the exposed HCW Actively recall patients who fail to attend 6.2.2.5 Deceased patients In the event of a deceased patient being the source of a needlestick injury and whose HIV status is unknown, the taking and testing of samples requires consent in accordance with the Human Tissue Act 2004. Assuming the deceased did not give consent (or refuse it) while alive, this can be obtained from a “nominated representative” (if appointed) or by a person in a “qualifying relationship” to the deceased [1]. If the testing shows that the patient was a carrier of a virus, seek advice from an HIV specialist before giving the information to the patient’s close contacts. 7.0 Other Blood Borne Viruses Guidelines for management of HCWs exposed to other blood borne viruses is outlined in the Trust BBV policy Following all significant exposures the source patient should also be approached regarding testing for hepatitis B and C infection. 7.1 Follow-Up 7.2 HCW not receiving PEP HCW who are not receiving PEP will be followed up by the Occupational Health Department. If initially assessed in A&E the HCW will be given a copy of their assessment / consultation record sheet to take to the appropriate Occupational Health Department and the A&E department will leave a message on the appropriate Occupational Health Departments answer phone with the staff members details. 7.3 HCW receiving PEP HCW receiving PEP will be advised to attend the Fletcher unit, Chichester, or Warren Browne unit, Worthing, at the earliest opportunity the next working day. HCWs should also be advised to contact Occupational Health on the next working day. The Consultation Record Sheet completed by A&E / Occupational Health should be faxed to the Fletcher unit / Warren Browne unit and if out of hours a message should be left on the Fletcher unit / Warren Browne units answer phone with the staff members details. If patient fails to attend Fletcher unit / Warren Browne unit the Health Advisors will make all efforts to contact the HCW. 21 of 53 7.4.1 Patients commencing PEP following sexual / non occupational exposure in A&E Patients who commence PEPSE in A&E will be advised to attend the Fletcher unit / Warren Browne unit at the earliest opportunity the next working day. If assessed in A&E the Consultation Record Sheet completed by A&E should be faxed to the Fletcher unit / Warren Browne unit and a message should be left on the Fletcher unit / Warren Browne units answer phone with the patients details. If patient fails to attend the Health Advisors will make all efforts to contact the patient 7.4.2 Patients not commencing PEP following non occupational exposure in A&E Patients following sexual exposure should be advised to attend the Fletcher unit / Warren Browne unit for an STI screen. Patients following community needlestick exposures / bites etc should be followed up in primary care as per normal practice. 7.5 Tests for BBV following potential exposure / PEP 7.5.1 Persons taking PEP Follow up tests will be undertaken by the GUM/HIV units managing the patients as outlined in their follow up protocols. 7.5.2 HCW not taking PEP These people will be followed up in the Occupational Health department. Hepatitis B serology / management as per Trust policy on BBV 3 months – 4th Generation HIV Ag/Ab test 6 months – HCV Ab test 7.6 HIV seroconversion During the follow up period patients should seek medical advice about any acute illness. Illnesses characterised by fever, rash, myalgia, fatigue, malaise or lymphadenopathy may represent a seroconversion illness. Some of these symptoms may, however, be side effects of antiretroviral medication [1]. Advice is available from the HIV team. If HIV infection is diagnosed, health care worker should be advised and managed in line with DoH recommendations [10]. 8.0 Availability of the Guidance This Guidance should be available in all wards and departments and on the Trust intranet. 22 of 53 9.0 Specialist Resources Sharps hotline: SRH 01243 788122 x 2405 WASH 01903 205111 x3037/01273 446037 **On the back of each staff member ID card GUM & HIV Medicine: St Richards Hospital Consultant: Dr Emma Rutland – extension 3660 or contact via switchboard Associate Specialist: Sam Gamalath - extension 3660 or contact via switchboard Health advisors: Barbara Hayman and Sandie Parker – 3669 GUM & HIV Medicine: Worthing / Southlands Hospital Consultant: Dr Andrew Nayagam – extension 3681 or contact via switchboard Associate specialist: Dr Vasu Selvadurai – extension 3681 or contact via switchboard Speciality Doctor: Dr Ruwani Jayaweera – extension 3681 or contact via switchboard Health Advisor: Richard Williams – ext 3681 Specialist HIV Pharmacy David Moore: On Monday, Tuesday am and Friday: Southlands Hospital Extension: 3750 (office) or ext 3413 (dispensary) On Wednesday and Thursday am: Sexual Health clinic, Crawley Hospital 01293 600300 ext 4007 Mobile: 07790295575, if fail to contact using above numbers Kin Ing: On Mondays pm and Thursday am: Fletcher Unit, (SRH) - ext 3660 Tuesdays all day, Wednesdays am, Fridays am: Warren Browne unit (Southlands), ext 3681 (reception) or Bleep 908 Other times: Beeding House, ext 3750 (Southlands site) or Bleep 908 work mobile: 07876 031464, if fail to contact using above numbers. Occupational Health Department, St Richards Hospital Reception: 01243 788122 x2403; direct dial 01243 831478 Sharps Hotline: 01243 788122 x2405 Occupational Health department, Southlands/Worthing Hospital 23 of 53 Telephone: Fax: Sharps Hotline: 01273 446056 01273 446027 01273 446037 10.0 Development of Guidance The sources of reference on which this guidance is based are shown below. In addition the guidance reflects current practice within the Trust (where this does not conflict with published evidence and expert opinion) combined with information about good practice from other NHS Trusts. A draft version of the guidance was circulated to consultants, associate specialists and health advisers within the Department of HIV/ GUM for their approval. In addition specific consultation was sought with senior medical staff in the Accident and Emergency Department, Department of Occupational Health and Microbiology. The Guidance was then submitted for approval to the Trust Policies Committee . Amendments were made as necessary before the final guidance was submitted for ratification. 11.0 Implementation 12.1 Dissemination of the Guidance The Guidance will be sent to all Consultants, Ward Managers, Out Patient Department, Theatres, Imaging Departments and Laboratories. The manager in each of these areas will be responsible for disseminating copies of the Guidance to relevant staff and ensuring that copies of the Guidance are available for immediate reference in the event of a potential HIV exposure. 12.2 Staff Induction and Training of Non-Specialist Staff In line with the Blood Borne Virus Policy training on the correct use of sharps and what to do in the case of an inoculation incident is provided to relevant staff on the health and safety update day and in accordance with the Learning and Development Policy. To minimise delay in seeking advice about PEP all Trust staff must be aware of how to avoid occupational exposure, possible risks from occupational exposure to HIV and action to be taken following possible exposure including immediate first aid and how to report an exposure, and to whom and reasons why this is important Responsibility for this rests with the line manager for any given staff group. Basic information about PEP must form a part of the Trust Induction Programme for new staff [1]. 12.3 Training of Staff Involved in Assessment and Administration of PEP The following groups of staff will require specific training regarding assessment of the need to access immediate expert advice and about supplying an initial dose of PEP and awareness of current protocols: Medical and nursing staff in A&E Medical and nursing staff in the Department of HIV/GUM 24 of 53 Medical and nursing staff in the Department of Occupational Health This will involve regular teaching conducted at a frequency determined by the rate of turnover and training needs of each staff group. 12.4 Monitoring In line with section 3.0 of the Blood Borne Virus Policy: Sharps injuries and other body fluid exposure incidents: A quarterly occupational health report is presented to the Health and Safety Committee. Staff attendance at training is monitored in accordance with the Learning and Development policy. 12.5 Audit The recommendations within the Guidance will be audited. Auditable outcomes may include: Proportion of PEPSE prescriptions that fit within recommended indications: (target 90%) Proportion of PEPSE prescriptions administered within 72 hours of risk exposure: (target 90%) Proportion of patients started on PEP referred to GUM / HIV unit (target 100%) Proportion of patients prescribed PEP completing 28 day course (target 75%) Proportion of individuals completing 12 week post-PEP HIV antibody test (target 60%) 13.0 References 1. HIV post-exposure prophylaxis: Guidance from the UK Chief Medical Officers’ Expert Advisory Group on AIDS. Department of Health. Revised September 2008. 2. Cardo DM, Culver DH, Ciesielski CA, Srivastava PU, Marcus R, Abiteboul D, Heptonstall J, Ippolito G, Lot F, McKibben PS, Bell DM. A case-control study of HIV seroconversion in health care workers after percutaneous exposure. Centers for Disease Control and Prevention Needlestick Surveillance Group. N Engl J Med. 1997; 337: 1485-1490. 3. Otten RA, Smith DK, Adams DR, et al. Efficacy of postexposure prophylaxis after intravaginal exposure of pig-tailed macaques to a human-derived retrovirus (human immunodeficiency virus type 2). J Virol 2000;74:9771–5 4. Wade NA, Birkhead GC, Warren BL, et al. Abbreviated regimens of zidovudine prophylaxis and perinatal transmission of the human immunodeficiency virus. N Engl J Med 1998;339:1409–14 5. Praca Onze Study Team. Behavioural impact, acceptability, and HIV incidence amongst homosexual Men with access to postexposure chemoprophylaxis for HIV. J Acquir Immune Defic Syndr 2004;35:519 6. Schecter M. Occupational and sexual PEP – benefit/risk? 6th International Conference on Drug Therapy in HIV Infection, 2002. Glasgow, UK (abstr. PL 6.1) 7. Clinical Effectiveness Group (British Association of Sexual Health and HIV). United Kingdom Guideline For The Use Of Post-Exposure Prophylaxis For HIV Following Sexual Exposure. Int J STD & AIDS 2006; 17: 81–92 reference new guideline** 25 of 53 8. Website of Liverpool HIV Pharmacology Group, Department of Pharmacology and Therapeutics, University of Liverpool, UK. 9. British HIV Association and Children’s HIV Association guidelines for the management of HIV infection in pregnant women 2008. HIV Medicine 2008; 9: 452–502. 10. HIV infected Health Care Workers : Guidance on Management and Patient Notification. Department of Health 2005. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/do cuments/digitalasset/dh_4116416.pdf 14.0 Glossary A&E AIDS BASHH BBV CDSC DoH DNA EAGA FBC GMC GUM/HIV HAART HBV HCV HCV-Ab HCW HIV HIV-AgAb HPA LFT MSM NHS PCR PEP PEPSE PHLS STI U.S. U&E 26 of 53 Accident and Emergency Acquired Immunodeficiency Syndrome British Association for Sexual Health and HIV Blood-borne virus Communicable Disease Surveillance Centre Department of Health Deoxyribonucleic acid Chief Medical Officer’s Expert Advisory Group on AIDS Full Blood Count General Medical Council Sexual Health Service Highly Active Anti-Retroviral Therapy (Combination of drugs) Hepatitis B virus Hepatitis C virus Hepatitis C antibody Health care worker Human Immunodeficiency Virus HIV antigen antibody Health Protection Agency Liver function tests Men who have Sex with Men National Health Service Polymerase Chain Reaction Post-exposure prophylaxis PEP after sexual exposure Public Health Laboratory Service Sexually transmitted infection United States of America Urea and Electrolytes Appendix A HIV PEP following Occupational Exposure Consultation Record Sheet Prompt Assessment Is Important: PEP Is Most Effective If Started Within the Hour Contacted sharps hotline number? YES / NO If NO: contact sharps hotline (SRH 01243 788122 x 2405 or WASH 01903 205111 x3037) Part 1: About the Person Requesting PEP (to be completed by HCW) Name of exposed person: ____________________ WSHT Staff? Yes No DOB: ____________________ Sex: Male/ Female Patient sticker (A&E) Today’s date __/__/____ Time now: ___:___ Date of incident __/__/____ Time of incident ___:___ Part 2: Information about the Source Person (to be completed by HCW) a) Is the source unknown and unidentifiable: YES Go to part 4 Is the source known: YES Give any identifying information e.g. name, hospital number, ward & Consultant: b) Is the source: Known to be HIV+ve: Unknown or uncertain HIV status: Go to part 3A Go to part 3B Part 3A: The HIV+ve Source Person (to be completed by HCW) Is any of the following information immediately available? If not PEP should not be delayed to collect more information about the source. PEP can be altered later if necessary (after discussion) if more information does become available a) Most recent HIV viral load: copies/ml Date: __/___/__ b) Is the source currently on antiretroviral treatment? If yes which drugs? c) Has the source previously taken any/ any other antiretroviral treatment? If yes which drugs? 27 of 53 d) Is there any known HIV drug resistance? (now go to part 4) Part 3B. Identified source of unknown or uncertain HIV status a) Does the source have a known HIV risk behaviour? Man who has sex with men Current/ ex IVDU Born or recently arrived from area of high HIV prevalence (see attached HIV prevalence data / Appendix G)) Recipient of multiple blood transfusions or blood products pre 1985 Sexual partner of person with risk factor(s) above b) Date of last HIV test? __/__/__ Never had HIV test (now go to part 4) Part 4: About the Exposure (to be completed by HCW) A: Material involved (tick all that apply): Blood Saliva in association with dentistry Amniotic Fluid Vaginal Secretions / Semen Cerebrospinal Fluid Unfixed Tissues or Organs Human Breast Milk Pericardial / peritoneal / pleural Fluid Exudative or other tissue fluid from burns or skin lesions Other body fluid which is visibly bloodstained B: Type of exposure: I. Was there a sharps injury: Superficial (surface scratch) Moderate (Skin penetrated) Deep (penetrating injury) II. Was there exposure of non intact skin? (e.g. abrasions, cuts, eczema etc): III. Was there mucous membrane exposure? C: Was an instrument involved: Was the instrument: 28 of 53 No Hollow bore needle Solid needle Other instrument Visibly contaminated with blood Previously in an artery or vein (Now go to part 5) Part 5 is PEP indicated? – (to be completed by A&E nurse/Dr) ***Note PEP is not indicated if the source is unknown or cannot be identified go to Part 8 HIV Risk Assessment Table Use the following risk assessment table to determine whether HIV post-exposure prophylaxis (PEP) is indicated. Risk assessment of injury Score Nature of exposure Splash to broken or mucosal membrane 1 Percutaneous penetration 2 Non bloody fluid excluding faeces, saliva, urine, vomit 0 Blood or blood stained fluid 2 Solid 0 Hollow 1 Suture / IM / subcutaneous 0 IV / arterial access 1 Superficial (scratch/graze) 1 Moderate (penetrated skin) 2 Deep 3 Material exposed to Type of sharp Sharp use Wound description Risk factors for HIV (source patient) (see part 3b) Enter score Score Low risk factors / unknown 1 High risk factors 5 Known HIV positive 6 TOTAL SCORE □ Total score 10 or more PEP recommended – Go to Part 6 & refer to A&E Dr □ Total score below 10 do not give PEP – Go to Part 7 29 of 53 Part 6: PEP Indicated – Other medical details required ( to be completed by A&E doctor) a) Past medical history: b) Medication History: Current medication or in preceding 2 weeks (including Oral contraceptive pill); Check for any interactions with PEP on information for prescribers sheet provided / Appendix J) c) Allergies (to Truvada (tenofovir, emtricictabine) or Kaletra (lopinavir, ritonavir) d) If female: LMP If possible pregnancy do urinary Pregnancy test. Result: **IF SOURCE PATIENT IS KNOWN HIV POSITIVE / DRUG INTERACTIONS ARE HIGHLIGHTED OR PATIENT IS PREGNANT CONTACT HIV CONSULTANT WHO WILL ADVISE WHETHER ANY CHANGES SHOULD BE MADE TO PEP REGIME **If none of the above continue to provide PEP starter pack as below a) Having read the PEP information sheet (Appendix K) does the patient understand: how to take PEP potential side effects drugs licensed to treat HIV but not PEP; however recommended by national guidelines Importance of follow-up b) Does the patient consent to PEP (sign consent form Appendix F) Yes No Continue below… Why: c) Provide PEP starter pack and complete prescription sheet in PEP pack (Appendix E): Truvada 1 tablet once a day & Kaletra 2 tablets twice a day for 5 days Date of first dose: __/__/__ Time of first dose: ___:___ d) Discuss following issues: Safer sex / condom use for 3 months Safe injecting practice (if appropriate) No Blood / semen donation for 3/12 30 of 53 Now go to part 7 below Part 7. Hepatitis B/C Management All cases of occupational exposure must be referred to Occupational Health regardless of level of risk. Hepatitis B management (as per BBV policy) If known HepBsAg positive source or known non responder to vaccine (see shaded boxes consider HBIG). If not refer to occupational health next working day for ongoing management. HBV prophylaxis for reported exposure incidents Significant exposure Non-significant exposure HBV status of person HBsAg Unknown HBsAg negative Continued risk No further risk exposed positive source source source < 1 dose HB vaccine HBIG × 1 Accelerated Initiate course of HB Initiate course of HB No HBV pre-exposure course of HB vaccine vaccine prophylaxis. Accelerated vaccine* Reassure course of HB vaccine* > 2 doses HB vaccine One dose of HB One dose of HB Finish course of HB Finish course of HB No HBV pre-exposure vaccine vaccine vaccine vaccine prophylaxis. (anti-HBs not known) followed by second dose Reassure one month later Known responder to Consider Consider Consider booster Consider booster No HBV prophylaxis HB vaccine booster dose of booster dose of dose of HB vaccine dose of HB vaccine (anti-HBs > 10mIU/ml) HB vaccine HB vaccine Reassure Known non-responder HBIG × 1 HBIG × 1 No HBIG Consider No HBIG No HBV to HB vaccine Consider Consider booster dose of HB prophylaxis. (anti-HBs < 10mIU/ml booster dose of booster dose of vaccine Consider booster 2–4 months post- HB vaccine. HB vaccine dose of HB vaccine Reassure immunisation) 2nd dose of 2nd dose of HBIG should be HBIG should be given at one given at one month month *An accelerated course of vaccine consists of doses spaced at zero, one and two months. A booster dose may be given at 12 months to those at continuing risk of exposure to HBV. Source: PHLS Hepatitis Subcommittee (1992). Hepatitis C (HCV) Management There is no vaccine / prophylaxis for Hepatitis C. All cases of occupational exposure to hepatitis C must be referred to occupational health for follow up and further management. Part 8. Baseline Bloods All exposed patients: Serum store & HepBsAb will be taken by the Occupational Health department on the next working day (clotted samples) If starting PEP: 31 of 53 FBC U&Es, LFTs, Glucose, Calcium, phosphate Full Hepatitis B & C serology (EDTA) (Yellow top) (clotted sample) **HIV testing will be done at first follow up in GUM/HIV dept **Please request copy to Fletcher unit, Chichester or Warren Browne unit, Worthing Tests for the source person will be arranged with his/ her consent of by the Clinical team responsible for their care if WSHT patient Part 9. Follow - Up Arrangements a) WSHT staff not commencing PEP: Patient must attend occupational health on next working day Ring occupational health and leave a message with exposed staff members details Give a copy of paperwork to exposed staff member to take to occupational health b) Patients commencing PEP: Patient must attend Fletcher unit / Warren Browne unit on next working day in addition to attending occupational health. Please fax all sheets in this form with A&E front sheet to the GUM/HIV Department (Fletcher unit on: fax number 01243831606 or Warren Browne unit on: fax number 0173446049)** AND Telephone Fletcher unit on 01243831607 or Warren Browne unit on 01273446049 to inform them of referral (leave message on answer phone out of hours) **Health advisors from Fletcher unit / Warren Browne unit will contact patients who do not attend according to the contact details you fax to them. Please ensure that these are accurate. Signed:________________Print name:_______________ Date: __/__/__ 32 of 53 Appendix B HIV PEP following non occupational (Sexual / community needlestick / bite) Exposure Consultation Record Sheet Prompt Assessment Is Important: PEP Is Most Effective If Started Within the Hour Person completing form: __________________________ Part 1: About the Person Requesting PEP Name of exposed person: ____________________ DOB: ____________________ Sex: Male/ Female Patient sticker Today’s date __/__/____ Time now: ___:___ Date of incident __/__/____ Time of incident ___:___ Part 2: Information about the Source Person a) Is the source unknown and unidentifiable: Is the source known: b) Is the source: YES Go to part 4 YES Known to be HIV+ve: Unknown or uncertain HIV status: Go to part 3A Go to part 3B Part 3A: The HIV+ve Source Person Is any of the following information immediately available? If not PEP should not be delayed to collect more information about the source. PEP can be altered later if necessary (after discussion) if more information does become available e) Most recent HIV viral load: f) copies/ml Date: __/___/__ Is the source currently on antiretroviral treatment? If yes which drugs? g) Has the source previously taken any/ any other antiretroviral treatment? If yes which drugs? h) Is there any known HIV drug resistance? 33 of 53 (now go to part 4) Part 3B. Identified source of unknown or uncertain HIV status a) Does the source have a known HIV risk behaviour? Man who has sex with men Current/ ex IVDU Born or recently arrived from area of high HIV prevalence (see attached HIV prevalence data / Appendix G) Recipient of multiple blood transfusions or blood products pre 1985 Sexual partner of person with risk factor(s) above b) Date of last HIV test? __/__/__ Never had HIV test (now go to part 4) Part 4: About the Exposure A) Sexual exposure: Sexual partner: Male / Female Contactable / Uncontactable Was there sexual assault? Yes / No Tick appropriate box(es) for sexual exposure and condom use. Leave blank if any information for an exposure is not known. Types of Type of sex? sex Anal Receptive Insertive Vaginal Receptive Insertive Oral Receptive Insertive B) Discarded needle: Describe injury: C) Bite: Describe injury: 34 of 53 Condom Used? Condom Internal Break? Ejaculation? Has the person requesting PEP ever had an HIV test? Yes : date of last HIV test (approx.): _____________ Since last HIV test has patient had any of the following risks for HIV infection: No has the patient ever had any of the following risks for HIV infection: unprotected anal/vaginal sex with known HIV+ve person man having unprotected anal sex with unknown man IVDU originates from / unprotected sex in HIV endemic area (see HIV prevalence sheet in appendix) (Sexual health unit only: Consents to HIV antibody test?: (Now go to part 5) 35 of 53 Yes No ) Part 5 is PEP indicated? **PEP is not indicated for exposures over 72 hours ago – go to part 7 Use the table to help decide whether PEP is indicated. Type Of Source Known HIV +ve Unprotected Viral load Viral load Sexual Exposure detectable / undetectable unknown Receptive anal Recommended Recommended sex Insertive anal sex Recommended Not recommended Source HIV Status Unknown Source High Source not High Risk# Risk# Receptive vaginal sex Insertive vaginal sex Fellatio with ejaculation Fellatio without ejaculation Cunnilingus Recommended Not recommended Considered Not recommended Recommended Not recommended Considered Not recommended Recommended Not recommended Considered Not recommended Considered Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Considered Not recommended Not recommended Not recommended Not recommended Not recommended Not recommended Splash of semen Considered into eye Sharing injecting Recommended drug equipment Human bite *Not recommended Needlestick from discarded needle in the community # Within the UK at present this is men who have sex with men and individuals who have immigrated to UK from areas of high HIV prevalence particularly sub-Saharan Africa *This may be considered in exceptional circumstances where an HIV+ individual with a detectable viral load with blood in their mouth bites another individual where the teeth have broken the skin No, PEP is not recommended Advise patient that the potential side effects and toxicity of taking PEP outweigh the negligible risk of transmission posed by the type of exposure because it is considered insignificant, whether or not the source patient is known or considered likely to be HIV infected. Continue to Part 7 Yes, PEP indicated; continue to Part 6 PEP is considered – discuss with HIV Specialist 36 of 53 Part 6: PEP Indicated – Other medical details required e) Past medical history: f) Medication History: Current medication or in preceding 2 weeks (including Oral contraceptive pill); Check for any interactions with PEP on information for prescribers sheet provided / Appendix J) g) Allergies (to Truvada (tenofovir, emtricictabine) or Kaletra (lopinavir, ritonavir) h) If female: LMP If possible pregnancy do urinary Pregnancy test. Result: **IF SOURCE PATIENT IS KNOWN HIV POSITIVE / DRUG INTERACTIONS ARE HIGHLIGHTED OR PATIENT IS PREGNANT CONTACT HIV CONSULTANT WHO WILL ADVISE WHETHER ANY CHANGES SHOULD BE MADE TO PEP REGIME **If none of the above continue to provide PEP starter pack as below i) Having read the PEP information sheet (Appendix K) does the patient understand: how to take PEP potential side effects drugs licensed to treat HIV but not PEP; however recommended by national guidelines Importance of follow-up j) Does the patient consent to PEP (sign consent form Appendix F) Yes Continue below… No Why: k) Provide PEP starter pack and complete prescription sheet (Appendix E) in PEP pack: Truvada 1 tablet once a day & Kaletra 2 tablets twice a day for 5 days Date of first dose: __/__/__ l) Time of first dose: ___:___ Discuss following issues: For sexual exposures: 37 of 53 Safer sex / condom use for 3 months Safe injecting practice (if appropriate) No Blood / semen donation for 3/12 Consider emergency contraception Now go to part 7 below Part 7. Hepatitis B/C Management Hepatitis B management If high risk exposure to a known HepBsAg positive source consider HBIG (Discuss with GUM/HIV specialist on call). Otherwise further assessment and management of Hepatitis B prevention following sexual exposure will be carried out by GUM/HIV unit or following nonsexual exposure by primary care. Hepatitis C (HCV) Management There is no vaccine / prophylaxis for Hepatitis C. All cases of sexual exposure will be referred to Fletcher unit / Warren Browne unit for follow up and further management. Part 8. Baseline Bloods Patients not starting PEP: No bloods in A&E. Patients will be advised to have follow up in GUM/HIV service or primary care (see below) If starting PEP: FBC U&Es, LFTs, Glucose, Calcium, phosphate Full Hepatitis B serology (EDTA) (Yellow top) (clotted sample) Baseline HIV testing will be carried out at first follow up visit at Fletcher unit / Warren Browne unit next working day **Please request copy to Fletcher unit, Chichester or Warren Browne unit, Worthing Tests for the source person will be arranged with his / her consent by the GUM/HIV unit Part 9. Follow - Up Arrangements a) Patients not commencing PEP: i) Sexual exposures: Patient should be advised to attend Fletcher unit / Warren Browne unit for STI screening / Hep B/C follow up. Ask patient to ring for appt / details of walk in service. Please fax all sheets in this form with A&E front sheet to the GUM/HIV Department (Fletcher unit on: fax number 01243831606 or Warren Browne unit on: fax number 0173446049)** ii) Non sexual exposures: Patient can be followed up in Primary care b) Patients commencing PEP: Patient must attend Fletcher unit / Warren Browne unit on next working day** Please fax all sheets in this form with A&E front sheet to the GUM/HIV Department (Fletcher unit on: fax number 01243831606 or Warren Browne unit on: fax number 0173446049)** AND telephone Fletcher unit on 01243831607 or Warren Browne unit on 01273446049 to inform them of referral (leave message on answer phone out of hours) **Health advisors from Fletcher unit / Warren Browne unit will contact patients who do not attend according to the contact details you fax to them. Please ensure that these are accurate. 38 of 53 Signed:_________________Print name:_______________Date: __/__/__ APPENDIX C Post exposure prophylaxis (occupational exposure) pathway Staff Member (patient) presents with occupational exposure Occupational Health (working hours) o o o o A&E (out of hours) o o Complete risk assessment form Do serology for Hep B Do save serum (with consent) Consider need for HBIG / Hep B vaccination Complete risk assessment form Consider need for HBIG Low risk (score <10) No PEP required High risk (score >10) PEP recommended PEP declined Arrange follow up If assessed in A&E: Ensure follow up arranged with occupational health, leave message on occupational health answer phone and give copy of paperwork to exposed staff member F/U: (Occupational health) - HepB serology results - HIV AgAb 3/12 - HepC Ab 6/12 PEP accepted PEP accepted. Information leaflet given to patient Consent form signed by patient and prescribing medical officer 5 day PEP pack given to patient to start asap Do baseline FBC, U&E, LFT, calcium and phosphate, Hepatitis B serology (request copy to Fletcher / WBU) Refer to GUM clinic next working day & leave telephone message at GUM Copy of assessment notes faxed to GUM/HIV unit If assessed in A&E: Ensure follow up arranged with occupational health, leave message on occupational health answer phone and give copy of paperwork to exposed staff member GUM/HIV Clinics Chichester – Fletcher Unit SRH WaSH – Warren Browne Unit Tel:01243831607 Tel:01273446075 Fax:01243831606 Fax:01273446049 Occupational Health Departments Chichester: 01243 788122 x2403; direct dial 01243 831478 Sharps Hotline: x2405 39 of 53 Worthing/Southlands Hospitals: Hotline: 01273 446037 Telephone: 01273 446056; Fax 01273 446027; Sharps APPENDIX D Post exposure prophylaxis following exposure: pathway for out of hours non occupational Patient presents with sexual / community needlestick / bite exposure o o A&E (out of hours) Complete risk assessment form Consider HBIG if high risk exposure to known HepBsAg+ve source (D/W GUM/HIV specialist) PEP not recommended PEP considered – discuss with GUM/HIV specialist on call via switchboard PEP not recommended / declined PEP recommended PEP recommended and accepted PEP declined Arrange follow up Sexual exposures: strongly advise follow up arranged with GUM/HIV Ensure risk assessment form faxed to relevant unit Non sexual exposures: follow up in primary care PEP accepted. GUM/HIV Clinics Chichester – Fletcher Unit SRH WaSH – Warren Browne Unit 40 of 53 PEP accepted Tel:01243831607 Tel:01273446075 Information leaflet given to patient Consent form signed by patient and prescribing medical officer 5 day PEP pack given to patient to start asap Do baseline FBC, U&E, LFT, Hepatitis B serology (request copy to Fletcher unit / WBU) Refer to GUM clinic next working day & leave telephone message at GUM Copy of assessment notes faxed to GUM/HIV unit Fax:01243831606 Fax:01273446049 APPENDIX E Prescription for HIV Post Exposure Prophylaxis (PEP) Date: __/__/____ Name of exposed person or GUM clinic number: _____________ DOB: _____________ Hospital/ A&E no: _____________ Type of exposure: Occupational Sexual Post code Please Supply PEP pack containing: Truvada 1 tablet o.d. for 5 days (5 tablets) Kaletra 2 tablets b.d. for 5 days (20 tablets) Domperidone 10mg t.d.s as required (10 tablets) Loperamide 4mg q.d.s as required (12 tablets) Prescriber’s signature Name Date: Please ensure the patient receives the patient information leaflet: "HIV Post Occupational Exposure Prophylaxis". Please file in A&E notes and fax with consultation sheet to Fletcher unit, Chichester or Warren Browne unit, Worthing 41 of 53 Appendix F Consent Form HIV Post Exposure Prophylaxis Truvada (Tenofovir + Emtricitabine) and Kaletra (Lopinavir + Ritonavir) have been recommended for the prevention of transmission following exposure to HIV by the Department of Health and Specialist HIV organisations. Their efficacy and long term toxicity are not known. However, their use may prevent HIV transmission. Because these drugs are not licensed for this indication, it is necessary to obtain your written consent to receive treatment. ****************************** I wish / do not wish* to receive Truvada® and Kaletra® for prophylaxis. I have read and received a copy of "HIV Post Exposure Prophylaxis" and my consent is based on this written information. Signature of person at risk ........................................................................................ Name of person at risk ..................................... Contact tel. No. ............................. (Block capitals) Date ........................................................................................................................... * delete as necessary 42 of 53 Appendix G Risk that source is HIV positive [7] Population Group (aged >15 years) Men who have sex with men† UK† London† Elsewhere in UK† Brighton* Heterosexuals (region of birth)‡ UK Rest of Europe North America Central and South America Caribbean North Africa and Middle East Sub-Saharan Africa South Asia East and South Asia Australasia Injecting drug users† UK London Elsewhere in UK HIV Prevalence (%) Male 5.2 10.5 3.4 13.7 Female - 0.4 1.2 1.1 1.9 1.2 0.5 6.1 0.5 1.1 0.3 0.3 0.6 0.2 1.1 1.0 0.4 10.3 0.5 0.8 0.2 0.3 0.8 0.2 0.3 0.3 0.3 † Prevalence numerator is derived from MPES estimates for 2008 (published 2009), Health Protection Agency. Prevalence denominator is derived from multiplying ONS mid-2008 population estimates by the estimated proportion of UK population reporting homosexual partners or injecting non-prescribed drugs in past five years, as relevant (Johnson et al.Lancet 2001). ‡HIV prevalence among GUM clinic attendees by work region of birth in 2008. http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1226046271991 Contemporaneous prevalence estimates can be obtained at: http://www.hpa.org.uk/infections/topics_az/hiv and sti *Dodds JP, Johnson AM, Parry JV, Mercey DE. A tale of three cities: persisting high HIV prevalence, risk behaviour and undiagnosed infection in community samples of men who have sex with men. Sex Transm Infect. 2007; 83(5): 392–396 Areas of high Hepatitis B prevalence Areas shaded dark green = prevalence >8% Saharan and sub-Saharan Africa East and South East Asia Tropical South America Romania Saudi Arabia Northern Canada (Inuits) and Greenland Areas shaded dark green = prevalence >8% Areas shaded light green = prevalence 2-8% (From WHO, 2006) 43 of 53 Appendix H Estimate of Risk of HIV Acquisition from a single exposure = risk of source having HIV x risk of exposure Examples: Needlestick injury from local intravenous drug user. Risk = 0.3% X 0.3% = approximately 1/111,111 Needlestick injury from SSA man of unknown status Risk = 6.1% x 0.3% = approximately 1 in 5,464 Needlestick injury from UK born heterosexual man of unknown status Risk = 0.4% x 0.3% = approximately 1 in 83,333 Sharing drug injecting equipment with a known HIV positive Risk = 100% X 0.67% = approximately 1 in 149 Unprotected receptive anal sex with HIV positive MSM. Risk = 100% x 1.11% = approximately 1 in 90 Unprotected receptive anal sex with local MSM of unknown status. Risk = 3.4% x 1.11% = approximately 1 in 925 to 1 in 2650 Unprotected insertive anal sex with local MSM of unknown status. Risk = 3.4% x 0.06% = approximately 1 in 49,020 Unprotected receptive oral sex (giving fellatio) with MSM of unknown status. Risk = 3.4% X 0.02% = approximately 1 in 147,049 Unprotected receptive vaginal sex with known HIV positive man. Risk = 100% x 0.1% = approximately 1 in 1000 Unprotected receptive vaginal sex with African man of unknown status. Risk = 6.1% X 0.1% = approximately 1 in 16,393 Unprotected insertive vaginal sex with African woman of unknown status Risk = 10.3% X 0.082% = approximately 1 in 1/11,840 Unprotected receptive vaginal sex with UK born man of unknown status Risk = 0.4% X 0.1% = 1/250,000 Based on seroprevalence data from the Health Protection Agency, 2008 44 of 53 Appendix I Information For Day Case Patients A Member of Staff Has Been Accidentally Exposed to Your Body Fluids What You Need to Know; Why We Need Your Help Today’s date: __/__/____ Patient Details Name of patient: _____________ Hospital no.: _____________ DOB: _____________ Male/ Female Patient’s address: Patient’s day time tel. no.: _____________ Mobile tel. no.: _____________ Brief explanation of event: Appointment in GUM/HIV clinic: Date: _____________Time: _____________ Where: Hospital Tel: Why Have You Been Given This Letter? This letter is to help you remember some important information given to you after your procedure. A member of staff will have given you a full explanation. Today you have had an investigation or treatment at Western Sussex Hospitals NHS Trust. During this treatment a member of our staff became accidentally exposed to your blood or another of your body fluids. This has not placed you at any risk and there will be no effect on your future health. Why We Need Your Help When healthcare workers (nurses, doctor etc.) are accidentally exposed to body fluids in certain circumstances there may be a risk to their health. 45 of 53 If this risk is high it can be reduced if the healthcare worker takes a special treatment for a month. The treatment is effective but can be difficult to take and cause side effects. However in order to assess how high the risk is for them extra information is needed from the patient who they were treating If the risk turns out to be low the healthcare worker can stop the treatment and be greatly reassured. Unfortunately it is the uncertainty about their future health that many healthcare workers find so distressing. They find themselves placed at risk simply because they were doing their job caring for patients. Western Sussex Hospitals NHS Trust cares for its employees. Therefore in line with guidelines from the Department of Health we routinely try to get as much of this important information as we can in these situations. However we can only do this with your consent and help. Therefore we need your help At the top of this letter there is an appointment for you to see a nurse at the GUM/HIV clinic’ When you come to the clinic the nurse will Explain more about why we need your help Answer any questions you may have Ask your permission to take a blood sample for testing If you agree to the blood sample the nurse will arrange to see you with your results as soon as possible Nothing you tell us in the clinic will go in your hospital notes or be told to anyone outside the clinic (including other hospital staff or GP and even the effected healthcare worker) without your consent. The clinic uses separate notes which never leave the clinic. The staff working there are bound to keep strict confidentiality by law. We will understand if you do not feel you can help us. However if this is the case we would value the opportunity to meet you. Even if you do not want to have a blood sample taken you may be able to give us some information which will reassure the member of staff affected. Where to get further information St Richards Hospital Fletcher unit, St Richards Hospital, extension …………… Worthing and Southlands Hospital Warren Browne unit, Southlands Hospital, extension…………… Signed:_______________ Print name:_________________ 46 of 53 Date: __/__/__ APPENDIX J Information for prescriber on HIV post exposure prophylaxis Prophylaxis, if required, must be commenced as soon as possible after the incident, ideally within 1-2 hrs. 1) The Regimen Truvada [combination of Tenofovir disoproxil 245mg and Emtricitabine 200mg] – one tablet every day orally, and Kaletra [combination of Lopinavir 200mg & Ritonavir 50mg] – two tablets every 12 hours orally Currently no anti-retroviral is licensed for HIV post exposure prophylaxis however, the Department of Health recommends them for this indication. These drugs can be prescribed for PEP only on an ‘off-label’ basis since their use in this context is outside approved indications. 2) Administration, Side-Effects and Warnings NB: The majority of the side effects occur after LONG TERM use (> 4 weeks) Truvada Administration:- one tablet every day Common side effects:- headache, dizziness, diarrhoea, vomiting, nausea, abdominal pain, allergic reaction, skin rash, pain, asthenia, insomnia, abnormal dreams, dyspepsia, flatulence, hyperglycaemia, hypertriglycerideamia, hypophosphataemia, raised serum lipase, amylase, raised liver enzymes, neutropenia, hyperbilirubinaemia, raised creatine kinase, Rare side effects:- anaemia, lactic acidosis, pancreatitis, renal impairment, Caution:- renal impairment: monitor renal function; pregnancy and breast-feeding Kaletra Administration: - two tablets every 12 hours Common side effects: - diarrhoea, nausea, vomiting, headache, flatulence, abdominal pain, rash, pruritis, lipodystrophy, asthenia, raised triglycerides, raised total cholesterol, raised γGT Rare side effects: - bleeding problems in haemophiliacs, pruritis, myalgia, exacerbation of or manifestation of diabetes mellitus, hepatitis, hyperglycaemia, pancreatitis, abnormal liver function tests, leucopenia, anaemia, Drug interactions: - Metabolised by CYP450 enzymes; (see interaction pages) Caution: - impaired hepatic function. Pregnancy and breast-feeding haemophilia diabetes concomitant use with medicines that prolong QT interval Domperidone Anti – emetic As all three medicines can cause nausea, an anti-emetic, Domperidone, is prescribed with the prophylaxis. The dose is 10mg orally, every 12 hours, before taking the HIV medicines. See BNF for cautions and side effects. 47 of 53 Loperamide Anti-diarrhoeal As diarrhoea is a common side-effect with Kaletra, an anti-diarrhoeal is prescribed with the prophylaxis. The dose is 2 capsules at the onset of diarrhoea and one capsule to be taken after each subsequent bowel movement up to a maximum of eight capsules in 24 hours. See BNF for cautions and side-effects. Important drug interactions All drug/dose changes must be made on an individual patient basis. Contact HIV pharmacy / HIV specialist on-call for more information. Drug interactions can also be checked on-line using the University of Liverpool’s HIV Drug interaction website wwww.hiv-druginteractions.org Drug Simvastatin (Zocor™) Problem Contraindicated therefore stop at once. Large increase in simvastatin levels – greatly increased risk of myopathy inc rhabdomyolysis Alternative Atorvastatin – start 10mg prescribing opportunity. Atorvastatin (Lipitor™) Rosuvastatin (Crestor™) The levels of atorvastatin rosuvastatin are increased Piroxicam (Feldene™) Inhaled/Intranasal corticosteroids; Fluticasone (Flixotide™, Flixonase™, Seretide™) Increased risk of toxicity from piroxicam High systemic absorption of corticosteroid. Advise patient to stop using if possible (i.e. only if no risk of severe asthma) Use low dose of statin and monitor for toxicity or consider stopping statin for the duration of PEP Any other NSAID e.g. diclofenac Budesonide (Rhinocort Aqua™, Pulmicort™, Symbicort ™) Diazepam, midazolam, Zolpidem Erythromycin Clarithromycin . Levels of hypnotic/anxiolytic likely to be increased Potential for increase in levels of these agents – may prolong QT interval St John’s Wort Enzyme inducer therefore will reduce Kaletra levels. Induction effect will persist for approx 2 weeks after cessation. Enzyme inducer – will reduce Kaletra levels. Induction effect will persist for approx 2 weeks after cessation; co-administration causes hepatotoxicity. Will get increase in rifabutin levels and may require dose reduction Rifampicin Rifabutin Amiodarone and antiarrhythmics Calcium channel blockers (diltiazem, verapamil) 48 of 53 and other Contraindicated – likely to get increase in levels of anti-arrhythmic drug – risk of serious and/or life threatening reactions such as cardiac arrhythmias. Increased levels – increased risk of heart block OD at next Beclomethasone (e.g. Becotide™ inhalers, Beconase™ nasal spray) Please note compound preparations e.g. (Seretide TM, Symbicort) also include bronchodilators (salmeterol, formoterol). The bronchodilators will need to be prescribed separately to the steroid inhalers. Warn patient re potential interaction: avoid concomitant use or decrease dose Advise patient to stop if short course or reduce dose if possible. Consider switch to azithromycin to finish antibiotic course if appropriate. Don’t issue Kaletra® – prescribe Truvada ® one tablet OD + Zidovudine 250mg BD Don’t issue Kaletra® – prescribe Truvada ® one tablet OD + Zidovudine 250mg BD Don’t issue Kaletra® – prescribe Truvada ® one tablet OD + Zidovudine 250mg BD or consider reduction in rifabutin dose (e.g. to 150mg 3x/week) for duration of PEP Don’t issue Kaletra® – prescribe Truvada ® one tablet OD + Zidovudine 250mg BD Consider using alternative third PEP drug*. Alternatively liaise with GP/cardiologist re dose adjustment Digoxin Initial acute increase in digoxin levels – could lead to toxicity. Anticonvulsants (phenytoin, phenobarbitone, carbamazepine) Enzyme inducers – will reduce Kaletra levels. Induction effect will persist for approx 2 weeks after cessation. Other anticonvulsants probably safe. Increased risk hypotension Propranolol Antipsychotics/neuroleptics Pimozide, Clozapine Antipsychotics/Neuroleptics :Quetiapine,haloperidol, risperidone,thioridazine Increase in levels and potential for life threatening arrhythmias Increase in levels may result in serious haematological abnormalities PIs may increase the drug levels of these agents Antidepressants (especially SSRIs and Related antidepressants, mirtazepine) May get increase in drug levels of antidepressants Immunosuppressants (ciclosporin, tacrolimus, sirolimus) Methadone Significant interaction to increase levels of immunosuppressants Oral contraceptives and depot contraceptive injections Effectiveness likely to be reduced Warfarin Levels (and therefore INR) can be increased or decreased Prednisolone, dexamethaxone Levels likely to be increased Recreational drugs: Ecstasy (MDMA), gammahydroxybutyrate (GHB), methamphetamine Erectile dysfunction agents (sildenafil, vardenafil, tadalafil) Levels of ecstasy, gammahydroxybutyrate (GHB) and methamphetamine may be significantly increased by ritonavir. Significant increase in drug levels and effect/side effects of erectile dysfunction agents 49 of 53 Potential for decrease in methadone levels. Methadone levels are likely to be affected from Day 7-10 on starting Kaletra. Don’t issue Kaletra® – prescribe Truvada ® one tablet OD + Zidovudine 250mg BD Don’t issue Kaletra® – prescribe Truvada ® one tablet OD + Zidovudine 250mg BD Continue at same dose but counsel patient regarding potential hypotension Don’t issue Kaletra® – prescribe Truvada ® one tablet OD + Zidovudine 250mg BD Dose reduction may be required (liaise with GP or psychiatrist) or prescribe Truvada ® one tablet OD + Zidovudine 250mg BD Consider dose reduction and monitor for toxicity. Alternatively prescribe Truvada ® one tablet OD + Zidovudine 250mg BD (especially with high doses of antidepressants) Don’t issue Kaletra® – prescribe Truvada ® one tablet OD + Zidovudine 250mg BD Counsel patient; monitor and increase dose only if pt complains of withdrawal symptoms. On completion of PEP, methadone dose may need to be reviewed, especially if any dose adjustments have been made. Discuss with substance misuse service Counsel patient – use barrier method of contraception (e.g.condom) as well whilst on PEP and for 4 weeks after (N.B. also risk of transmission) with no pill break. According to indication for warfarin – monitor INR closely or prescribe Truvada ® one tablet OD + Zidovudine 250mg BD In long-term use decrease dose of steroid whilst on PEP (consider reducing dose of prednisolone by approx 30%) Individuals should be advised that co-administration should be avoided. Avoid co-administration where possible. If given use with caution at low doses, do not exceed maximum doses (see below) and increase monitoring for adverse events Maximum doses: sildenafil 25mg every 48 hours, tadalafil 10mg every 72 hours, vardenafil 2.5mg every 72 hours NB: Advice regarding safer sex for the duration of PEP APPENDIX K HIV Post Exposure Prophylaxis Information for Patient March 2011 50 of 53 HIV Post Occupational Exposure Prophylaxis Information Information for patients 1) Introduction You have been involved in an incident that might have put you at risk of HIV infection. It is important that you read the following information before deciding whether or not to take preventative treatment (post exposure prophylaxis: PEP). Background information for healthcare workers The risk of acquiring HIV infection following occupational exposure to HIV-infected blood and body fluids is low. Taking PEP may significantly reduce the risk of you acquiring HIV. The estimated risk from source patients with documented known HIV infection is about 3 in 1000 for percutaneous exposure (i.e. accidents where the skin is pierced/ broken by a needle or to other sharps incident) and about 1 in 1000 for significant exposure to mucous membranes or non-intact skin (e.g. splashes to the eyes or splashes to areas of the skin that are already broken because of scratches or due to a skin condition). It has been considered that there is no risk of HIV transmission where intact skin is exposed to HIV-infected blood. Although preventing exposure remains vital, recent evidence suggests that when significant exposure occurs prompt treatment with anti-HIV drugs decreases the risk of HIV infection. A case-control study of HIV infection in health care workers following percutaneous exposure to HIV infected material has shown that prophylaxis with Zidovudine (AZT) is associated with a 79% decrease in risk of HIV transmission. Over the years the use of combined anti-HIV drugs has proved to be more effective than AZT alone in suppressing viral replications in people with HIV. The Department of Health has issued guidelines on post-exposure prophylaxis (PEP) for persons exposed to HIV. However, knowledge about the efficacy and toxicity of drugs used for PEP are limited. Background information for people exposed to HIV outside of work People may be exposed to HIV through vaginal or anal sex (either without a condom or when the condom broke or fell off), through sharing equipment for injecting drugs or through sexual assault. The risk of HIV infection associated with each such exposures are approximately 0.5-3% for unprotected anal sex between men, 0.1% for unprotected vaginal sex and 0.7% for needle sharing. However these risks vary widely among individuals. Minimising your risk of HIV exposure through safer sex (especially correct use of condoms for penetrative sex) and safer drug use (especially avoiding sharing of needles and other equipment) is the most important factor in avoiding HIV infection. There is research evidence that healthcare workers exposed to HIV infected blood have a low but measurable risk of acquiring HIV infection. Taking PEP significantly reduces this risk but cannot eliminate it. There is some research demonstrating a reduction in HIV transmission in persons taking PEP after exposure in other situations (especially after sexual exposure). 2) The Prophylactic Regimen Truvada [combination of Tenofovir disoproxil 245mg and Emtricitabine 200mg] – one tablet every day orally, and Kaletra [combination of Lopinavir 200mg & Ritonavir 50mg] – two tablets every 12 hours orally Currently no anti-retroviral is licensed for HIV post exposure prophylaxis however, the Department of Health recommends them for this indication. These drugs can be prescribed for PEP only on an ‘off-label’ basis since their use in this context is outside approved indications. Prophylaxis, if required, must be commenced as soon as possible after the incident, ideally within 1-2 hrs (Can be up to 72 hours) 3) Administration, Side-Effects, interactions with other medicines and Warnings 51 of 53 Before taking the PEP regimen please inform the doctor about: All other drugs that you are taking, including any that you buy over the counter in a community pharmacy, any herbals medicines or any illicit substances that you may take. Any previous allergy to any medicines If you have ever have liver or kidney disease If you are diabetic If you have ever had any bone disease If you are pregnant or thinking about becoming pregnant Please note: The majority of the side effects of these medications result after LONG TERM use (> 4 weeks) Truvada Administration: One tablet every day at the same time with or after food for 28 days Side effects: Tenofovir, like all other medicines has some side effects. The most common (incidence of more than 1 in 100 patients) are: Diarrhoea, nausea and vomiting, problems with digestion resulting in discomfort after meals, stomach pain, flatulence, dizziness, fatigue (lack of energy), headache, rash or changes in skin colour, difficulty sleeping. Please read the manufacturers ‘patient information leaflet’ for a full list of possible side-effects Other medications and Truvada: Truvada is removed from the body by the kidneys. It is important to tell the prescribing doctor about any medication that you take, especially any of the following: Kaletra Aminoglycosides (for bacterial infection), Amphotericin B (for fungal infection), Cidofovir (for viral infection), Foscarnet (for viral infection), Ganciclovir (for viral infection), Interleukin-2 (to treat cancer), Pentamidine (for infections), Vancomycin (for bacterial infection) Administration: Two tablets every 12 hours (twice a day) for 28 days Side effects: Kaletra, like all other medicines has some side effects. The most common (incidence of more than 1 in 100 patients) are: Diarrhoea, headache, nausea and vomiting, dry mouth, flatulence, stomach pain, difficulty sleeping, fatigue (lack of energy), rash Please read the manufacturers ‘patient information leaflet’ for a full list of possible side-effects Other medications and Kaletra: Kaletra is metabolised (processed in the body) by the liver. Some other medicines are metabolised in the same way. That is why is important to tell the doctor about any medicines that you take even occasionally. Examples of some medicines/drugs that should not be taken with Kaletra include: Simvastatin, piroxicam, inhaled corticosteroids (fluticasone, budesonide), rifampicin, rifabutin, antiarrhythmics (amiodarone, digoxin), anticonvulsants (phenytoin, carbamazepine, phenobarbital), antipsychotics (pimozide, clozapine), immunosuppressants (ciclosporin, tacrolimus, sirolimus), St. Johns wort, Erectile dysfunction agents (sildenafil, vardenafil, tadalafil), recreational drugs, ecstasy, GHB, methamphetamine. Other examples of medicines that are metabolised in the same way and may need to have the dose or medicine changed are: atorvastatin, rosuvastatin, diazepam, midazolam, zolpidem, antibiotics (erythromycin, clarithromycin), heart medications (calcium channel blockers such as diltiazem, verapamil, nifedipine), propranolol, antipsychotics/neuroleptics (quetiapine, haloperidol, risperidone), antidepressants (fluoxetine, paroxetine, sertraline, mirtazepine), methadone, oral contraceptive pills and depot injections, warfarin, prednisolone, dexamethasone. Anti-sickness As all three medicines can produce nausea, an anti-sickness, domperidone, is prescribed with the prophylaxis. The dose is one tablet orally, every 12 hours, before taking the HIV medicines . Anti-diarrhoeal As diarrhoea is a common side-effect with Kaletra, an anti-diarrhoeal, loperamide, is prescribed with the prophylaxis. The dose is 2 capsules at the onset of diarrhoea and one capsule to be taken after each subsequent bowel movement up to a maximum of eight capsules in 24 hours 52 of 53 Appendix L Patient identified as at risk of pregnancy from assault 1. Enquire about current/recent method of contraception, compliance with method, or any other reason current method not effective contraceptive cover for this assault 2. Enquire about day of last menstrual period, normality, cycle length and variation a. Establish day of cycle sexual assault (s) took place 3. Estimate likely date of ovulation and risk of pregnancy 2. Exclude established pregnancy or risk of pregnancy other than assault, exclude contra-indications to EC and use of interacting medications (especially liver enzyme-inducing drugs) Did 1st assault occur within the previous 120 hours? NO YES If assault is first UPSI since LMP, refer for emergency IUD if no more than 5 days since earliest calculated date of ovulation If UPSI within <72hrs, offer option of Levonelle 1500 or emergency IUD. If IUD fit planned, encourage use of Levonelle 1500 now, as interim measure If 2 or more episodes of UPSI earlier in cycle did patient take Levonelle 1500 within 72 hrs or ellaOne with 120 hours? NO If all episodes of UPSI occurred no more than 5 days since earliest calculated date of ovulation, refer for emergency IUD. For patients declining emergency IUD and requesting Levonelle or ellaOne, explain not recommended as risk of pregnancy earlier in cycle. If within 72 -120 hrs of assault and assault is 1st UPSI, offer option of ellaOne or emergency IUD. If IUD fit planned, encourage use of ellaOne now, as interim measure YES Patient at higher risk of pregnancy therefore refer for emergency IUD. For patients declining emergency IUD and requesting Levonelle or ellaOne, explain not recommended and efficacy / failure rates unknown with subsequent doses. NB ellaOne can only be taken once in cycle. EXPLAIN: - Mode of action, efficacy and risk of pregnancy (possibility of ectopic) of different types of emergency contraception. -Negative pregnancy test at the time of request of EC does not rule out conception that may have occurred earlier in the menstrual cycle if a woman has had unprotected intercourse more than 72 hours ago, including second or subsequent act(s) of unprotected intercourse in the same menstrual cycle, unless the first episode was more than 21 days ago and a pregnancy test is negative. -Explain how to take oral emergency contraception, low side-effect profile, what to do if vomits within 3 hours, and possible effects on menstrual cycle. -Ulipristal (ellaOne) is not recommended to be used more than once per cycle as the safety and efficacy of repeated exposure has not been assessed. -If hormonal contraception is continued after administering ulipristal, barrier contraception should be used until the next period or withdrawal bleed. -Option of emergency IUD should be discussed with all women as use of on-going contraception. -Need for effective contraception or abstinence for rest of cycle and need for follow-up if next period >7 days late or abnormal. -Offer STI screening to all women and discuss long-term contraceptives and refer as appropriate 53 of 53