The Female Reproductive System
advertisement

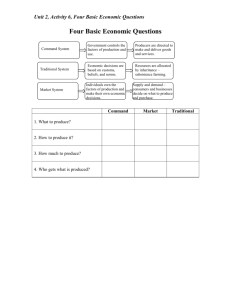
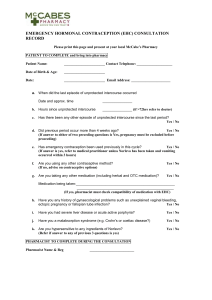
Contraception Background I. Contraception – prevention of conception A. Many problems with unwanted pregnancy – B. Contraceptive & condom use should be routine for sexually active young people & adults unless they seek pregnancy & they are in a mutually monogamous relationship 1. Too many people use contraception inconsistently or ineffectively II. Reasons people give for not using a contraceptive method: Contraceptive Effectiveness I. Effectiveness of each contraceptive method is difficult to determine precisely, so rates cited for each method are approximations only A. Theoretical effectiveness – B. User effectiveness – C. Use is measured by number of women out of 100 who will not become pregnant during the first year of use of the particular method D. Contraceptive use versus safer sex – nowadays must consider contraception & prevention of sexually transmitted infections (STIs) II. Three ways to achieve maximal effectiveness against both STIs & pregnancy relative to sexual intercourse: A. Abstain from all types of intercourse, B. Use condoms & spermicide together, C. Use condom & hormonal contraceptive together Nonprescription Methods: Abstinence I. Abstinence – can mean different things; many adolescents, young adults, & adults choose to abstain A. No sexual contact of any kind or B. No penetrative behaviors, including penile-vaginal intercourse, oral sex or anal intercourse II. People choose abstinence for a variety of reasons A. Their religion teaches that sexual intercourse is appropriate only in marriage B. They are not in a loving, committed relationship C. They do not have a partner D. They want to avoid the risk of pregnancy or STIs III. Choosing abstinence does not necessarily mean forgoing sexual pleasure – can get sexual pleasure without intercourse A. Deep kissing, massages, fondling, dancing, masturbating alone, masturbating together,, showering together IV. Effectiveness – the only 100% effective method of fertility control & STI prevention, if the couple or individual is truly committed to remaining abstinent A. Actual user effectiveness rates unknown; communication & commitment are essential V. Reversibility – abstinence does not affect fertility VI. Advantages & disadvantages A. Excellent method of fertility control & STI prevention B. It is free & you always have it with you, there are no side effects & no one's parents will be upset if you use it Nonprescription Methods: Withdrawal I. Withdrawal (coitus interruptus) – probably the oldest contraceptive method on record; in Bible, Onan practices it so as not to impregnate his dead brother's widow A. Couple has vaginal intercourse until the man feels he is about to ejaculate; he withdraws & ejaculates away from woman's vulva II. Effectiveness – many assume it is an ineffective method, however, many experts believe it is underrated; certainly better than no method at all A. It is about as effective as most barrier methods B. In studies of heterosexual couples among whom the man was infected with HIV & the woman was not, withdrawal cut HIV transmission rate by at least half C. Many people have been taught that preejaculate fluid might contain sperm D. If man does not withdraw in time & woman is at fertile point of cycle, emergency contraception should be considered III. Advantages & disadvantages A. Advantages 1. Withdrawal is free, always available & relatively easy to use B. Disadvantages 1. Some men, particularly young men, do not recognize impending ejaculation & thus ejaculate inside partner, putting her at risk of pregnancy Nonprescription Methods: Male condom I. Condoms are one of the oldest contraceptive methods, dating back to 1350 B. C. when Egyptian men put sheaths on penis before intercourse A. 18th century – Colonel Cundum invented penile sheaths using dried animal intestines B. 19th century – after rubber vulcanized, condoms began to be mass produced C. Today, most are made of latex, a synthetic form of rubber D. 1997 – US FDA approved first condom made of polyurethane, a type of plastic E. >100 available in US today – directions for their consistent & correct use from CDC 1. Consistent - use with every act of sexual intercourse (start to finish) including penile-vaginal, oral & anal intercourse 2. Correct use – store them in cool place out of direct sunlight (not in wallets or glove compartments II. AIDS renewed interest in condoms – experts advocate sexual abstinence, monogamy with uninfected partner & condoms to prevent spread of HIV A. Latex/polyurethane condoms when used correctly can prevent sperm from entering vagina & microorganisms that may cause STI from entering through vaginal/penile tears III. Effectiveness – very effective; only 3% of couples using them correctly & for every act of intercourse became pregnant in first year of use; 86% effective in typical users A. Major reason they fail is that people forget to use them for each act of intercourse IV. Advantages & disadvantages A. Advantages 1. Relatively inexpensive & easy to obtain 2. Do not require visit to a doctor B. Disadvantages – many men complain that they reduce sensitivity & spontaneity; trying different brands can improve sensation; putting it on as foreplay can increase fun Nonprescription Methods: Female Condom I. Female condom is the newest vaginal barrier; appeared on market in US in 1993; currently only one brand on market (Reality Female Condom) A. Loose fitting sheath made of polyurethane with rings on both ends B. Like male condom, it can be used for only one sexual encounter II. Effectiveness – effectiveness is similar to rates of diaphragm & cervical cap A. For perfect users, 95% effective in preventing pregnancy; for typical users, it is 79% effective III. Advantages & disadvantages A. Advantages - most users in preliminary studies were pleased with it B. Disadvantages - others reported that it was awkward to use, messy and made oralgenital contact difficult & unpleasant Nonprescription Methods: Spermicides I. Spermicides kill and/or immobilize sperm on contact thereby preventing their movement toward the egg; may be foams, gels, films, suppositories, creams or jelly foams A. Foams or creams are placed against cervix by means of plastic applicator B. Most spermicides must be inserted within 1 hour of intercourse; some are not effective for the first 10-15 after insertion; users should read instructions carefully II. Effectiveness – theoretical effectiveness rate is relatively high: 94% of women using them perfectly will not get pregnant in 1 year A. However, they have the lowest user effectiveness rate (~76%) of any method including withdrawal B. Spermicides have no effect on future fertility III. Advantages & disadvantages A. Advantages – many advantages to its use 1. Felt it was easy to use & available at drug stores & supermarkets without a prescription, have no serious side effects B. Disadvantages – until recently, family planning counselors would have said the only disadvantage was its low effectiveness rate in actual users 1. Studies in 2000 – suggested Nonoxynol 9, major spermicidal agent used in most products, may also cause lesions & ulcers in vaginal wall 2. 1999 – Penelope Hitchcock, head of STI branch of National Institutes of Allergy & Infective Diseases, advised women to avoid products with Nonoynol 9 at that time Nonprescription Methods: Normal Family Planning I. Natural family planning (NFP) - also known as fertility-awareness methods (rhythm method); several fertility-awareness methods: calendar, ovulation & symptothermal methods A. Each is based on identification of days in menstrual cycle when she is most likely to be fertile & avoidance of intercourse during those days (NFP) or B. Fertility-awareness methods are based on knowledge that there are only ~6 days in a cycle during which a woman can become pregnant C. It is estimated that it requires 4 – 6 hours to learn these methods so they can be used effectively D. Calendar method – first developed in 1930s E. Ovulation methods – much more effective; women can chart basal body temperature ( temperature upon waking) or cervical secretions or both 1. Temperatures usually drop immediately before ovulation& then rise sharply during & after ovulation F. Cervical secretions can also be monitored & charted – after menstruation, cervical secretions are scant 1. As estrogen levels rise, cervical mucus becomes thick & cloudy; when estrogen peaks at midcycle, secretions become clearer, stretchy & slippery 2. At ovulation, mucus can be stretched 2 – 3 inches between thumb & forefinger G. Symptothermal method – involves checking both basal body temperature & cervical secretions & charting them to identify fertile & nonfertile times 1. When used perfectly, only 2% of women become pregnant, making it as effective as the most effective prescription forms of contraception II. Effectiveness – can be highly effective; if used perfectly, only 1 – 9% of women using these methods in a year have an unintended pregnancy A. Symptothermal method is most effective natural family planning method III. Reversibility – natural family planning methods stop preventing pregnancies as soon as they are discontinued IV. Advantages & disadvantages A. Have many advantages B. Primary disadvantage - provide no protection against STIs Prescription Methods: Oral Contraceptives I. Several different types of oral contraceptives (OCs) – 56 brands (33 unique formulations in US alone); 2 general classifications: combined pills/minipills & multiphasic formulations A. Combined pills – used since 1960; contains estrogens & progestins (synthetic progesterone) 1. Woman ingests first pill in packet & takes a pill each succeeding day; most packets contain 28 pills but some contain only 21 2. 28 pill packets contain 7 pills that have no benefit other than convenience; woman need not remember to stop taking her pills & resume taking them 7 days later B. Progestin-only pill (minipill) introduced in 1972 – in spite of lack of estrogen (high doses of which were found to be related to physical complications); never too popular 1. Percentage of women using it remains relatively low 2. Woman takes pill on first day of menstruation & every day thereafter II. Chemical composition of oral contraceptives has changed over years in response to research on their effects & side effects A. Typical amount of estrogen in early ones was 0.1 mg; in 1968, <1% of OC prescriptions had <0.5 mg of estrogen 1. In 1988, ~82% of retail prescriptions for OCs contained <0.5 mg of estrogen B. Regardless of which pill is used, backup method should be used for first 7 days of pill use & as precaution if pill is forgotten 2 or more days in a row C. Good idea for woman using OCs to have regular medical exams; for example, a visit 3 – 6 months after woman starts OCs followed by annual exam thereafter III. Effectiveness – most effective means of preventing pregnancy apart from abstinence, sterilization & hormonal implants A. Only 1 in 1000 women using oral contraceptives gets pregnant in 1 year of perfect use; with typical users (some forget to take pills as directed), up to 5% get pregnant in 1st year IV. Reversibility – some women who have been on pill may need slightly more time to get pregnant than those using other methods V. Advantages & disadvantages A. Advantages – reported as being 99.5% as actually used & 99.9% effective if used correctly all the time; only available in US by prescription from a physician 1. Does not necessitate interrupting sexual activity 2. For some women, it helps to regulate menstrual cycle 3. Combination pill may enlarge breasts, reduce acne, often eliminates mittelschmertz, & reduces menstrual cramps B. Disadvantages – primary disadvantage is lack of protection against STIs including HIV 1. Symptoms can develop after pill use, even after some time 2. Other possible side effects for combination pill – associated with greater risk of circulatory system diseases like heart attacks & strokes 3. Smoking is also a factor, among ~10 million OC users, 500 die each year; rate would be lower if heavy smokers, especially those over 35, did not take pill 4. Women with these problems should not use OCs: 5. OCs & breast cancer – considerable debate over the years VI. Emergency contraception – available in cases of rape or incest or mistakes with contraceptive methods A. Most commonly prescribed method – take 2 OC pills within 72 hours of unprotected intercourse B. Some university clinics offer emergency contraception as part of their reproductive health services; if not offered, phone number in book C. Effectiveness – emergency contraceptive pills prevent pregnancy by delaying or preventing ovulation & possibly altering lining of uterus to prevent implantation D. Advantages & disadvantages 1. Advantage – 2. Disadvantage – Prescription Methods: Contraceptive Patch I. December 2000 – Johnson & Johnson applied for approval to market first patch; became available in March 2003; it releases a steady delivery of hormones over time A. In short time, it became second most popular form of nonoral birth control in prescriptions & sales B. Similar to use of nicotine patch; users wear it on lower abdomen, buttocks or upper arm II. Primary side effects – headache, nausea, site reactions (experienced by 20% of users in clinical trials) Prescription Methods: Depo-Provera I. Depo-provera is another form of progestin-only contraceptive method – it is a shot given every 12 weeks that suppresses ovulation by inhibiting production of LH & FSH II. Effectiveness – even more effective than the pill; in 1 year, only 0.3% of women using it become pregnant A. Since it is an injection, there is no chance that a typical user can use it incorrectly, unless she does not return in 3 months for the next shot III. Reversibility – fertility may resume immediately after 13 weeks has passed since the last injection; women generally do not conceive for an average of 10 months after date of last shot IV. Advantages & disadvantages A. Advantages – B. It has few practical disadvantages – may be difficult for some to schedule every 3 months; some women report minor weight gain; many report changes in their periods 1. Some women have no periods on Depo-Provera; some have frequent bleeding V. October 2000 – FDA approved new injectable contraceptive marketed under trade name Lunelle; contains estrogen & progestin while Depo-Provera is only progestin A. Given as an intramuscular injection once-a-month 1. Woman taking Lunelle have a monthly period & need to visit their health provider each month Prescription Methods: Norplant I. 1990 – FDA approved hormonal implants as means of contraception; marketed under brand name Norplant A. Consist of 6 matchstick-sized capsules containing levonorgestrel, a progesteronelike synthetic hormone, which prevents ovulation & causes endocrine dysfunction B. Surgically implanted by physician in simple procedure, using needle to insert implants under skin of upper arm II. Effectiveness – studies of more than a half-million women in many countries have led to conclusion that Norplant is 99.7% effective in preventing pregnancy III. Reversibility – once it is removed, conception can occur immediately; median time to conception after it is removed in women trying to conceive is approximately 1 month IV. Advantages & disadvantages A. Advantages - many including its actual use effectiveness rate 1. Once in place, it can be forgotten; no other action needed B. Disadvantages – some may have difficulty affording initial cost 1. Medicaid does cover their insertion, but Norplant Foundation provides free set for low-income women who are not covered by Medicaid 2. Some women are not good candidates 3. Its use can lead to menstrual irregularities like prolonged bleeding & more frequent bleeding 4. Although safety has been tested & it contains no estrogen, WHO recommends that women with unexplained vaginal bleeding or breast cancer should not use them 5. 2 – 8% of women using Norplant experience minor side effects that lead to implant removal C. Given advantages & disadvantages, implants should be considered if: 1. You are interested in long-term contraception 2. You are unable to use pills containing estrogen V. Norplant no longer being marketed – in 2000, its manufacturer (Wyeth) became concerned that specified lots of Norplant might be ineffective because of a manufacturing error A. Thus they advised health care professionals to stop providing implants from those lots B. They also advised women with implants from those lots to use barrier or hormonal methods of contraception to ensure protection from pregnancy Prescription Methods: Intrauterine Devices (IUDs) I. IUDs - synthetic devices inserted by medical provider into uterus to prevent pregnancy; now, only 2 IUDs available in US: Paragard Copper T 380A & Progestasert Progesterone T A. Paragard IUD can remain in place for10 years; Progestasert must be replaced every year B. No one knows how IUDs prevent pregnancy (current research does not support theories that IUDs act as abortifacients) , but a number of theories proposed: C. IUDs are highly effective birth control method & excellent choice for women who have already had children & are in mutually monogamous relationships 1. Generally not appropriate for teenage or college since they increase risk of STIs II. In US in 1978, 20% of widowed, divorced or separated women aged 15 – 44 who used some contraceptive method used an IUD A. With reports of potential side effects (PID, perforated uterus, ectopic [tubal] pregnancy, pregnancy complications [stillbirths, birth defects, low birth weight] & infertility)….. B. 1986 – manufacturer of most highly used IUDs in US (G. D. Searle & Co.) removed them from market due to concern over pending law suits C. Causes of interference with availability of contraceptive choice D. 1988 – GynoMed Pharmaceutical Inc. marketed Copper-T 380A IUD; gave greater choice E. December 2000 – FDA approved new 5-year IUD marketed under name Mirena III. Effectiveness – IUD is one of most effective birth control methods; 97 – 99% effective in preventing pregnancy IV. Reversibility – once it is removed, fertility resumes immediately V. Advantages & disadvantages – IUD is excellent for adult women in mutually monogamous relationships in which childbearing is completed A. Advantages – in addition to having high level of effectiveness, it is easy to use & has no systemic side effects 1. Once it is inserted, it remains in place so planning before intercourse is unnecessary B. Disadvantages – its effectiveness is offset by complications 1. Can increase chance of pelvic infection, especially in women with multiple sexual partners 2. Can be unknowingly discharged (2 – 10% of first year users) & pregnancy can result 3. Can cause especially heavy menstrual flow, particularly in first several months after insertion 4. There is tiny chance that conception will occur with device in place, which presents dilemma 5. Major disadvantage – actually increases likelihood of being infected with STI; especially true in first month after insertion Prescription Methods: Diaphragm I. Diaphragm – when in place, it prevents sperm from traveling through uterus & up fallopian tubes to fertilize an egg & it holds spermicide against cervix A. It is a shallow rubber or synthetic rubber cap surrounding a flexible metal ring that covers cervix; available in several sizes & styles 1. Since its purpose is to prevent sperm from going beyond vagina, its size & shape are very important B. It must remain in place for at least 6 hours after intercourse; spermicide must be added for each act of intercourse II. Effectiveness – when inserted properly & used with spermicide, diaphragm is theoretically 94% effective & 80% effective as actually used III. Reversibility – does not affect fertility, except when it is in place IV. Advantages & disadvantages A. Advantages 1. Major – it is highly effective if used correctly & consistently, is easy to learn to use & has no systemic side effects B. Disadvantages – it must be inserted before intercourse & inserted properly, requiring woman or couple to plan ahead 1. Some women are not comfortable touching their genitals & therefore find diaphragm use uncomfortable Prescription Methods: Cervical Cap I. Cervical cap – rubber, plastic or metal cap that covers cervix; holds spermicidal cream or jelly A. Similar to, but smaller than, diaphragm, meant to stay in place longer; slightly less effective than diaphragm B. 1988 – FDA approved sale of cervical cap in US, although they have been used in Europe for decades C. Cap made in different sizes; not all women can use it because of variation in shapes & sizes of cervixes II. Effectiveness – diaphragm & cervical cap have similar rates of effectiveness; 91% effective theoretically, but user rates are 80% A. Much more effective (80%) in women who have never been pregnant (nulliparous women), but only 60% in women who have been pregnant B. In nonmonogamous couples, condoms should also be used to prevent STI transmission III. Reversibility – does not affect fertility (unless it is in place) IV. Advantages & disadvantages A. Advantages – B. Disadvantages – some studies found slightly higher than expected precancerous cervical abnormalities in cap users, but other studies have not been able to verify this Prescription Methods: NuvaRing I. NuvaRing – vaginal ring that provides hormonal protection from pregnancy; approved by FDA in 2001 & became available in 2002 A. Emits 0.015 mg of ethinyl estradiol (estrogen component) & 0.120 mg etonogestrel (progestin component) daily for 21 days B. Unlike diaphragm & cervical cap, NuvaRing need not be positioned correctly to provide maximal protection 1. Cannot be inserted incorrectly & has a timer as a reminder when it needs to be replaced C. Not recommended for use by women who smoke cigarettes, nor for those who have heart disease or are prone to circulatory diseases such as blood clots II. Effectiveness – effective hormonal contraceptive with many advantages; theoretical & user effectiveness rate between 98% & 99% A. Characteristic that once it is in place there is nothing else to do B. Reversibility – reversible once removed III. Advantages & disadvantages – contains less estrogen than even the low-dose OCs, thereby decreasing risks associated with synthetic estrogens A. Advantages – ring does not require any daily action as does taking a pill each day; ring must simply be replaced after 21 days B. Disadvantages – risk of synthetic estrogen is not eliminated; it is merely reduced 1. Smokers & those susceptible to blood clots should not use ring as advised by manufacturer 2. 14% of users experienced vaginitis & 25% of males felt ring during intercourse, although most reported that they did not perceive that to be a problem Permanent Methods: Sterilization I. Sterilization is a form of contraception that renders a person biologically incapable of reproducing; men & women may choose to be sterilized if they have all children they want A. Women in ill health (serious heart conditions) may choose to prevent life-threatening pregnancies & births B. >15 million people have been sterilized; each year ~1 million more are sterilized; it has not always been so popular C. Male sterilization rates have remained steady between 1982 & 1995 at 11% of those using contraception using sterilization II. Effectiveness – male & female sterilization is highly effective III. Reversibility – reversal is expensive, not readily available, requires major surgery & results are not guaranteed; although it can be reversed, it should be considered permanent IV. Advantages & disadvantages – only for people who are certain that they want no more children & who are fertile; both male & female sterilization have same advantages A. Advantages – B. Primary disadvantage – Permanent Methods: Male Sterilization I. In males, sterilization entails interruption of vas deferens in procedure called vasectomy A. Became popular as method of contraception in late 1960s & early 1970s B. Interest in vasectomy was result of several factors: C. Early 1980s – number of vasectomies performed declined as result of publicity from received by a couple of research studies 1. In study of vasectomized monkeys, it was found that they had greater degree of atherosclerosis (clogged arteries) II. Vasectomy is simple, minor surgical procedure that takes about 30 minutes A. Small opening is made in scrotum & vas deferens is severed, blocking sperm from entering ejaculate since it has no route out of the testes B. Done under local anesthesia & require little care afterwards; vasectomized men are advised to avoid hard work or strenuous exercise for several days III. Unlike female, sterilization, it does not provide immediate infertility – sperm may be stored in urethra or elsewhere in reproductive tract & may not be expelled for 10 weeks or more A. Amount of time needed to expel these sperm depends partly on ejaculation frequency IV. Still considered to be permanent means of contraception, but with new microsurgical techniques, some may be reversed in very expensive procedure (vasovasectomy) A. 2 problems exist with these reversals B. 81 – 98% of vasectomies can be reversed so that sperm appears in ejaculate, but only about half of reversals (depending on the study) result in a preganancy Permanent Methods: Female Sterilization I. Female sterilization takes several forms – goal is to prevent egg from moving down fallopian tube to be fertilized by sperm; the methods include: A. Minilaparotomy B. Laparoscopy C. Open laparoscopy D. Vaginal approaches E. Transcervical methods II. Minilaparotomy (minilap) – procedure takes about 20 minutes & woman can usual leave medical setting in 2 – 3 hours A. Requires small incision just above pubic hairline B. Instrument then inserted into cervix to move uterus & pull each fallopian tube into incision III. Laparoscopy – involves inserting into abdomen a narrow stainless steel tube with fiberoptic cylinders that transmit light; this tube is called a laparoscope A. 2 types of laparoscope are used B. Ligation by electrocoagulation (high frequency electrical current) or application of clips or rings can take place during procedure to prevent passage of egg IV. Open laparoscopy – designed to minimize chance of bowel or blood vessel injury A. Small incision is made, through which special tube (cannula) can be inserted & around which skin is sutured V. Vaginal approaches – 2 types of vaginal female sterilization techniques used: culpotomy & culdoscopy; both involve small incision (3 cm) made in vaginal wall behind cervix A. Fallopian tubes are then pulled through incision into vagina, where they are occluded by ligation, clips or rings B. Minilap has been so successful that & has had so few complications that culpotomy & culdoscopy are not often used VI. Transcervical methods – sterilization methods that do not require surgery are being tested A. These techniques occlude fallopian tubes through cervix B. The potential for infection exists & these techniques are used only experimentally VII. Nonsurgical female sterilization - quinacrine is a permanent, nonsurgical method of female sterilization that is not approved for use in US VIII. Reversibility – female sterilization should generally be considered irreversible, like male sterilization A. Although surgical techniques can be successful in opening up fallopian tubes, highly skilled surgeons & modern microsurgical equipment are required & very costly B. Some experts report only 30% - 70% of women who undergo reversal surgery eventually conceive C. Several other factors also affect reversibility of female sterilization D. Another consideration is greater chance of ectopic pregnancy; women who have had reversal surgery are 3 times as likely to have ectopic pregnancy as other women Future of Contraceptives I. Perfect method of contraception, which will probably never exist, would have following properties: II. 1990s saw introduction of new methods, including female condom, nonlatex male condoms, Norplant, Depo-Provera & Lunelle III. New contraceptive methods are presently being researched A. Male contraceptive implants – in 2001, clinical trials began B. Implanon – a single rod progesterone implant, only ~4 cm long, that inhibits ovulation while impeding motility in reproductive tract C. Jadelle – manufactured by Wyeth, former manufacturers of Norplant D. Lea's shield – cervical cap that allows the release of cervical fluids & air E. Essure – causes sterility without surgical anesthesia or incision & does not result in any visible scar