Lower-Limb-Prosthetics

Lower Limb Prosthetics
Revised: 02-18-2014
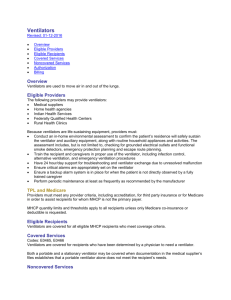
Overview
Lower limb prosthetics are used to restore ambulation to people with missing or amputated legs.
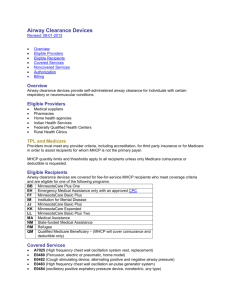
Eligible Providers
Medical suppliers
Indian Health Services
Federally Qualified Health Center
Rural Health Clinic
TPL and Medicare
Providers must meet any provider criteria, including accreditation, for third party insurance coverage or for Medicare coverage in order to assist recipients for whom MHCP is not the primary payer.
MHCP quantity limits and thresholds apply to all recipients unless payment of only the Medicare co-insurance or deductible is requested.
Eligible Recipients
Lower limb prosthetics are covered for all eligible MHCP recipients.
Covered Services
All Covered Lower Limb Prosthetics
A lower limb prosthetic must be prescribed by an enrolled MHCP provider:
A physician who is knowledgeable in orthopedics, physiatry, or vascular surgery
A physician in consultation with an orthopedist, physiatrist, or physical therapist or
A podiatrist within the scope of their professional practice. MHCP covers podiatrist services to treat below the knee.
Evaluation
Evaluation of the recipient’s functional ability is required. For recipients with existing prostheses, for whom a similar replacement is requested, evaluation can be based on the recipient’s history and current condition. For recipients for whom a first prosthesis is requested or for whom a significantly different prosthetic is requested, evaluation must be based on clinical observation.
Evaluations must be performed by a professional who is certified by the American Board of Certification in Orthotics and
Prosthetics or the Board of Certification in Orthotics and Prosthetics or who has similar training and expertise.
Use the following functional levels in the evaluation. Provide specific information about the recipient’s ambulation history, performance and activities of daily living to support assignment of an individual to a functional level. Note that the MHCP functional level definitions are not identical to the Medicare definitions.
Level 0: The recipient does not have the ability or potential to ambulate or transfer safely with or without assistance and a prosthesis does not enhance the quality of life or mobility
Level 1: The recipient has the ability or potential to use a prosthesis for transfers or ambulation on level surfaces at a fixed cadence. Limited or unlimited household ambulator.
Level 2: The recipient has the ability or potential for ambulation with the ability to traverse low level environmental barriers such as curbs, stairs or uneven surfaces. Limited community ambulatory.
Level 3: The recipient has the ability to ambulate over significant distances and over uneven surfaces. Unlimited community ambulator.
Level 4: The recipient has the ability for prosthetic ambulation that exceeds basic ambulation skills, exhibiting high impact, stress or energy levels. The recipient has a demonstrated need for ambulation requiring variable cadence over at least 400 continuous yards or a demonstrated need for regular ambulation on uneven terrain. Unlimited community ambulator with especially rigorous demands.
Specific Additions to Lower Limb Prosthetics
A microprocessor controlled ankle foot system (L5973) may be medically necessary for recipients whose functional level is 4.
A power assist ankle-foot or ankle system (L5969), dynamic response foot with multi-axial ankle (L5979), flex foot system
(L5980), flex-walk system or equal (L5981), or shank foot system with vertical loading pylon (L5987) may be medically necessary for recipients whose functional level is 3 or above.
An energy storing foot (L5976) may be medically necessary for recipients whose functional level is 2 or above.
An axial rotation ankle unit (L5982-L5986) may be medically necessary for recipients whose functional level is 2 or above.
A high activity knee control frame (L5930) may be medically necessary for recipients whose functional level is 3 or above, or for recipients whose weight requires the increased strength of this kind of frame.
A pneumatic knee (L5614, L5822, L5830-L5840) may be medically necessary for recipients whose functional level is 2 or above.
A fluid/hydraulic knee (L5610, L5613, L5614, L5722-L5780, L5814, L5824-L5828, L5848) may be medically necessary for recipients whose functional level is 3 or above.
A knee with stance phase microprocessor control feature (L5858) may be medically necessary for highly motivated recipients whose functional level is 2 or above.
A knee with powered and programmable flexion/extension assist control (L5859) may be medically necessary for highly motivated recipients whose functional level is 3 or above who have a documented comorbidity in their sound limb or spine, or for bilateral amputees.
A knee with swing and stance phase microprocessor control feature (L5856) may be medically necessary for recipients whose functional level is 4.
A pneumatic or hydraulic polycentric hip joint (L5961) may be medically necessary for highly motivated recipients whose functional level is 2 or above.
Noncovered Services
A prosthetic or orthotic device for which Medicare has denied the claim as not medically necessary
A device whose primary purpose is to serve as a convenience to a person caring for the recipient
A device that serves to address social and environmental factors and that does not directly address the recipient’s physical or mental health
A device that is supplied to the recipient by the physician who prescribed the device or by a provider who is an affiliate of the physician who prescribed the device
Repair costs for a prosthetic device that is under warranty
Repair costs for any rented prosthetic equipment
Lower limb prosthetics for recipients who have been found to have functional ability or potential functional ability of level 0.
User-adjustable heel height feature (L5990) is considered not medically necessary.
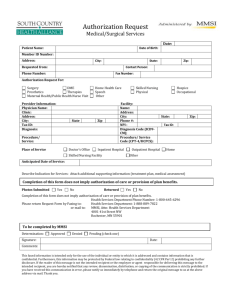
Authorization
Authorization is not required for immediate postsurgical or early fittings (L5400-L5460), initial prostheses (L5500-L5505), preparatory prostheses (L5510-L5600) or the first test socket for any prostheses (L5618-L5628).
Authorization is required for the second or subsequent test socket (L5618-L5628) for any prosthetic. Documentation must clearly show why the current test socket cannot be modified and must demonstrate that an additional test socket is needed before a final socket is selected. Test sockets which must be replaced due to provider error will not be approved.
Authorization is required for all lower limb prosthetic services L5000-L5999 not specified above, including repairs to existing prosthetics.
Submit authorization requests through MN −ITS (Authorization Request 278). Fax the MN−ITS response with the required documentation, physician’s orders and appropriate additional information to the authorization medical review agent . Write the
MN −ITS Authorization Request number on each page of each document.
Submit the prosthetic base HCPCS code with appropriate modifiers on the first line of the authorization request if a new prosthetic is being requested.
List all add-on items on separate lines on the authorization request. List each item by HCPCS code with appropriate modifiers, quantity and submitted charge.
Do not list items on an authorization request when the item never requires authorization. These items should be billed on a separate claim.
MHCP will not authorize more units per line than are allowed by Medicare’s Medically Unlikely Edits (MUEs). When requesting authorization for bilateral prosthetics where more units are required than are allowed by the MUEs, the units must be requested on different lines, with modifiers NU RT and NU LT as appropriate. Documentation must clearly establish that the greater number of units is required.
When multiple items that are different but require the same miscellaneous code are requested, each item must be listed on a separate line of the authorization request. A unique description of each item must be entered into the model number field for each line. The unique description may be a model number or a narrative description up to 20 characters.
Docume ntation for purchase must address the recipient’s medical and functional needs, and how the requested prosthetic meets those needs.
Documentation for purchase must include the assessment of the recipient’s functional status, and how the recipient’s functional status relates to the need for the requested items.
Documentation for purchase must establish that the requested device is the least costly appropriate way to meet the recipient’s needs.
When requesting authorization for identical replacement of components on an existing prosthetic, it is not necessary to establish medical necessity for those components. Document that the component needs to be replaced and is not covered by a warranty.
When requesting authorization for non-identical replacement of components on an existing prosthetic, document the medical necessity for the requested components.
Each line will be approved or denied, with the allowed dollar amount listed if approved.
Billing
Use X12 Batch or MN −ITS 837P Professional electronic claim
Report the ordering provider in the Other Provider Types section of the MN −ITS Interactive claim
If the recipient has Medicare, MHCP will pay only the deductible / co-insurance on any item for which Medicare made payment, regardless of any MHCP prior authorization.
Shipping / delivery/ set-up costs are included in the MHCP maximum allowable payment and may not be separately billed to
MHCP or the recipient.
MHCP will not pay claims for more units per line than are allo wed by Medicare’s Medically Unlikely Edits (MUEs). When billing for bilateral prosthetics where more units are required than are allowed by the MUEs, the units must be billed on different lines, with modifiers NU RT and NU LT as appropriate.
Prosthetic d evices for which fabrication has begun but which have not been dispensed as of the date of the recipient’s termination from MHCP eligibility may be reimbursed on a prorated basis to the extent that customization renders all or part of the device unsuitable for use by someone else.
When billing labor for repairs, specify the number of units and the hourly rate. Do not bill for setup and delivery, or for service calls that do not involve actual labor time for repairs.
When billing for items approved on a prior authorization:
Submit one claim for all approved lines. Make sure the HCPCS codes, modifiers, and descriptions on the claim match the same information on the prior authorization.
Enter the authorization number in the authorization field for each line
When the model number field is used, do not use the Notes field on the Services tab in MN −ITS. Use the Claim Notes field on the Claim Information tab.
Submit the usual and customary charge for each line, not the approved amount from the authorization letter. Payment will be the balance of the lesser of the billed amount or the approved amount after any primary or secondary payers have made payment.
Bill items without an authorization number on a separate claim.
Definitions
Affiliate: A person that directly or indirectly, through one or more intermediaries, controls or is controlled by, or is under common control with, the referring physician or consultant.
Physiatrist: A physician who specializes in physical medicine or who possesses specialized knowledge of rehabilitation and who is certified by the American Board of Physical Medicine and Rehabilitation.
Prosthetic: An artificial device, as defined my Medicare, to replace a missing or nonfunctional body part