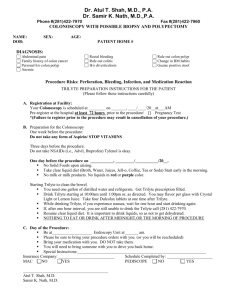
Preparation instructions
advertisement

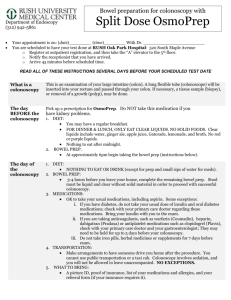
Colonoscopy Bowel Preparation Instructions Your procedure is scheduled on __________________________ at ___________ AM/PM. (Please arrive 1 hour early for registration) Facility: Manhattan Surgical Center, 1829 College Ave, Manhattan, KS 66502, 785-776-5100 Mercy Regional Health Center, 1823 College Ave, Manhattan, KS 66502, 785-776-3322 PLEASE READ ALL INSTRUCTIONS ON THE DAY YOU RECEIVE THEM General Information: A good bowel preparation (cleansing) is critical to effective colonoscopy. Any stool remaining in the colon can hide lesions and may result in the need to repeat the colonoscopy. Split dose (evening and morning dosing) has been shown to be most effective for obtaining good bowel preparation. This will mean getting up in the middle of the night if you have an early morning appointment. Day of Procedure: The day of your procedure, you will be at the facility for approximately 2 to 3 hours. Wear comfortable, easy to remove clothing. Leave jewelry and other valuables at home. Every effort will be made to perform your procedure at the scheduled time, but unexpected delays or emergencies may occur and your wait time may be prolonged. Be assured that appropriate attention will be given to each patient’s procedure. After the procedure, Dr. Zachary will discuss the results with you; but, due to the sedation, often times patients do not remember this conversation. It is important to have someone with you who can hear the results as Dr. Zachary is discussing them with you. If you receive sedation for your procedure you must have someone drive you home. 1 What to Bring With You the Day of Your Colonoscopy 1. The completed and signed enclosed patient information sheet, informed consent, disclosure of ownership (Manhattan Surgical Hospital procedures only) and advanced beneficiary notice (Medicare patients undergoing screening colonoscopy). 2. Names and addresses of all doctors you wish to receive a copy of your report. 3. List of your current medications and any drug allergies. 4. Copies of any relevant records from your referring physician. 5. Your insurance card and drivers license. 6. Someone to drive you home if you are receiving sedation. Insurance: If during a screening colonoscopy (meaning you have no symptoms), a polyp or tissue is removed, it is no longer considered a screening colonoscopy, but a surgical colonoscopy by some insurance companies. This may affect the benefits your insurance company pays. If you have any questions about your particular coverage, please check with your insurance company prior to starting your preparation. Some insurance companies require pre-authorization for procedures. As a courtesy, we will make every effort to obtain authorization. To obtain coverage for these procedures, we recommend that you check with your insurance to see if pre-authorization is required. If your insurance information has changed, please contact us several days before your procedure. Diabetic Patients: If you are diabetic, please check with your primary or treating physician regarding your dose of insulin or other diabetic medication needed the day before and the day of your procedure. Inform your doctor that you will be on clear liquids the day before your procedure. Medications: If you take aspirin or other non-steroidal anti-inflammatory drugs (ibuprofen, naproxen or other prescription arthritis medications) or take blood thinners such as warfarin (Coumadin), clopidogrel (Plavix), enoxaparin (Lovenox), or heparin; please check with your primary or treating physician to ask how you should take them or stop them before and after your procedure. If you are unable to contact your primary doctor(s), 2 please call us several days before your procedure. Please also notify us if you have any history of bleeding disorders. If you take regular narcotic pain medicine or regular benzodiazepine such as those listed below, please notify us as we may need to make arrangements for an alternative sedation for your procedure. Narcotics include: propoxyphene (Darvocet), oxycodone (Percocet), hydrocodone (Lortab, Vicodin), codeine (Tylenol #3), hydromorphone (Dilaudid), fentanyl (Duragesic), methadone, morphine (MS Contin, Roxanol) Benzodiazepines include: alprazolam (Xanax), triazolam (Halcion), lorazepam (Ativan), temazepam (Restoril), chlordiazepoxide (Librium), diazepam (Valium), clonazepam (Klonipin), flurazepam (Dalmane) Please also notify us if you have had any prior difficulties with sedation or endoscopic procedures. Cardiac Devices: If you have an implanted cardiac device such as a defibrillator, please let us know several days before the procedure. Antibiotic Recommendations: The American Society for Gastrointestinal Endoscopy (ASGE) and the American Heart Association no longer recommend antibiotics prior to any endoscopic procedure for any heart condition. The ASGE also does not recommend antibiotics prior to any endoscopic procedure for patients who have prosthetic joints (artificial joint replacements). If you have any questions about your procedure or must cancel your procedure please call us at 785-539-8900 or the endoscopy unit at Manhattan Surgical Hospital (785-7765100) or Mercy Regional Health Center (785-776-3322), whichever hospital where your procedure will be done. 3 Miralax Preparation Instructions: 5 Days before your Colonoscopy: 1. Read all instructions. 2. Contact your prescribing physician for instructions on diabetic medication, antiinflammatory medication, and blood thinners. 3. Obtain bowel prep products from your pharmacy: One 238 gram bottle of Miralax, 4 Dulcolax (bisacodyl) tablets, and two 32 oz bottles of Gatorade (no red or purple color). 4. Stop herbal, vitamins, and oral iron supplements. 5. Stop nuts and fruits and vegetables with small seeds. 6. Arrange for a driver for your procedure. 2 Days before your Colonoscopy: 1. 2. 3. 4. Complete the forms sent to you. Make a list of all your current medications and medication allergies. Find insurance cards. Get names and addresses of all physicians you wish to receive a copy of your report. The Day before your Colonoscopy: 1. No solid food. No alcohol. Only clear liquids all day. (see next page for acceptable clear liquids) 2. Drink an extra 8 oz of clear liquid every hour while awake. Gatorade is preferred. 3. Mix ½ of the Miralax 238 gram bottle in each 32 oz Gatorade bottle until dissolved and keep cold in the refrigerator. 4. 4PM Take 4 Dulcolax tablets with water and continue clear liquids. 5. 6PM Begin drinking Miralax/Gatorade solution at a rate of 8 oz every 15-30 minutes (over 1-2 hours) until the first bottle is gone. 6. You are encouraged to continue to drink clear liquids until you go to bed. 7. You may apply petroleum based product or diaper rash ointment to the rectal area if you experience discomfort from frequent stools. 8. Confirm that you have a driver for your procedure. 4 The Day of your Colonoscopy: 1. No solid food. No alcohol. 2. 4-5 hours before the time of your procedure is scheduled, take the second 32 oz bottle of Miralax/Gatorade over 1-2 hours as you did the night before. If your procedure is scheduled early in the morning, you will need to get up in the night to take this dose. The correct timing of the dose is essential to an effective preparation. NOTE: You must take both 32 oz bottles of Miralax/Gatorade solution as directed to adequately cleanse your bowel. If you do not think your prep is working, notify us (785-539-8900) or the endoscopy unit at Manhattan Surgical Hospital (785-776-5100) or Mercy Regional Health Center (785-776-3322), wherever your procedure is being performed. 3. You may and should drink clear liquids until 3 hours before your scheduled procedure time. Have nothing to eat or drink for 3 hours prior to your procedure. Clear Liquids Include: In general, if you can see through it, you can drink it. Water Gatorade is the preferred clear liquid (no red or purple) Soda pop Clear fruit juices, such as white grape or apple juice Hard candies Kool-Aide, PowerAde (no red or purple) Jell-O (no red or purple) Clear soup, broth or bouillon Popsicles (no red or purple) Tea or coffee without cream After your Colonoscopy: After your procedure you may eat your usual diet and resume your usual medications unless otherwise instructed. Drink 8 oz of liquid at least 6 times after the procedure and before retiring for the night. You should not drive the day of your procedure. If biopsies are taken or polyps are removed, you will receive a letter in 1-2 weeks explaining the results. If there are serious findings Dr. Zachary will call you and/or have you come to the office to discuss the results. 5