Efficiency Collaborative: Reduction of ED Utilization
advertisement
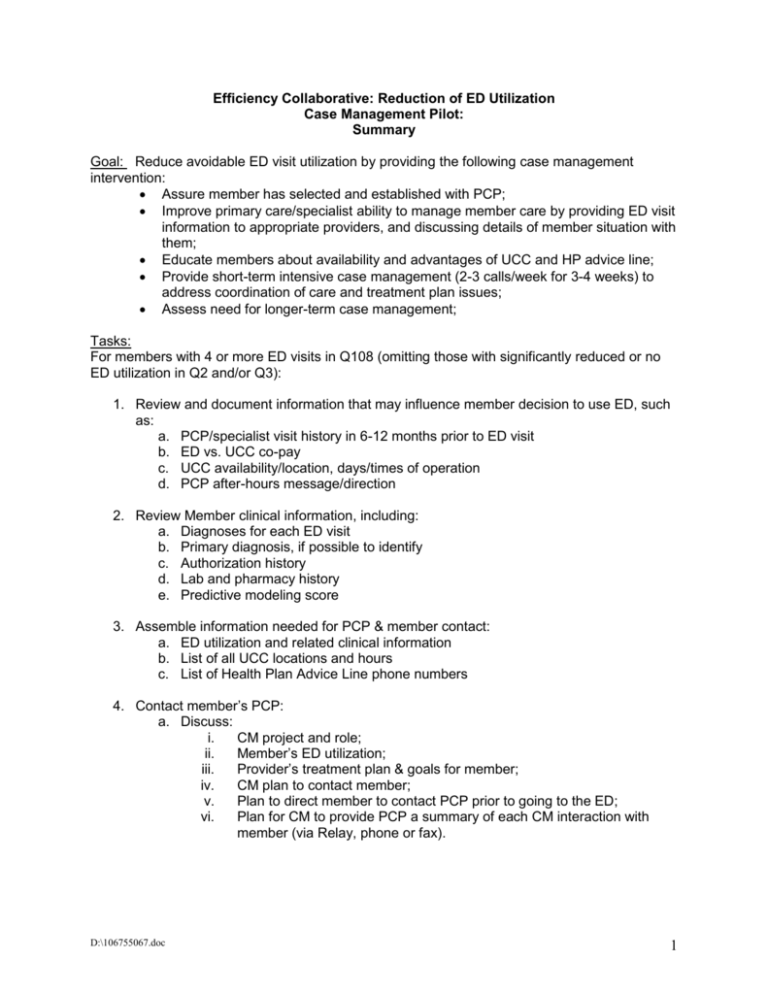
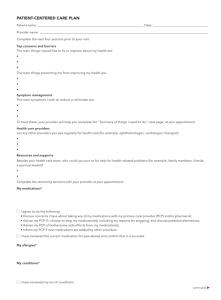
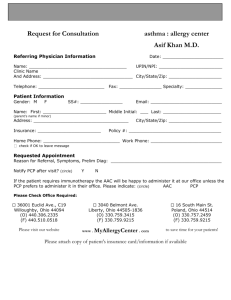
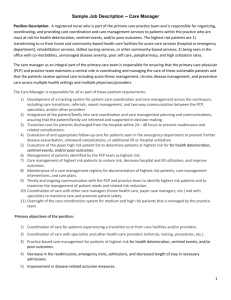
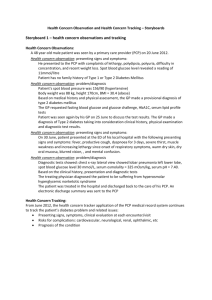
Efficiency Collaborative: Reduction of ED Utilization Case Management Pilot: Summary Goal: Reduce avoidable ED visit utilization by providing the following case management intervention: Assure member has selected and established with PCP; Improve primary care/specialist ability to manage member care by providing ED visit information to appropriate providers, and discussing details of member situation with them; Educate members about availability and advantages of UCC and HP advice line; Provide short-term intensive case management (2-3 calls/week for 3-4 weeks) to address coordination of care and treatment plan issues; Assess need for longer-term case management; Tasks: For members with 4 or more ED visits in Q108 (omitting those with significantly reduced or no ED utilization in Q2 and/or Q3): 1. Review and document information that may influence member decision to use ED, such as: a. PCP/specialist visit history in 6-12 months prior to ED visit b. ED vs. UCC co-pay c. UCC availability/location, days/times of operation d. PCP after-hours message/direction 2. Review Member clinical information, including: a. Diagnoses for each ED visit b. Primary diagnosis, if possible to identify c. Authorization history d. Lab and pharmacy history e. Predictive modeling score 3. Assemble information needed for PCP & member contact: a. ED utilization and related clinical information b. List of all UCC locations and hours c. List of Health Plan Advice Line phone numbers 4. Contact member’s PCP: a. Discuss: i. CM project and role; ii. Member’s ED utilization; iii. Provider’s treatment plan & goals for member; iv. CM plan to contact member; v. Plan to direct member to contact PCP prior to going to the ED; vi. Plan for CM to provide PCP a summary of each CM interaction with member (via Relay, phone or fax). D:\106755067.doc 1 5. Contact Member: a. Standard CM introduction; b. Assure established with PCP. If not, facilitate PCP selection & appt.; c. Educate: i. Location/hours of nearest UCC, ii. phone number for HP nurse advice line, iii. clinical condition, treatment plan, medications, etc, iv. How/when to contact CM for assistance, v. contact PCP/specialist prior to going to the ED d. Survey member re: i. What provider do they call when they have an urgent need ii. Did they attempt to contact PCP/specialist prior to ED visit iii. Did they speak with provider prior to going to ED iv. Why did they use ED instead of UCC v. Have they tried to call their PCP/specialist after-hours in the past vi. If so, was the provider easy to reach, call back promptly, vii. Is member able to get a same day appointment when needed viii. Has member used UCC in the past; if so, what was the experience like? e. Assess for case management needs; f. Establish date/time of future call(s); g. All interaction based on member consent to participate D:\106755067.doc 2