File
advertisement

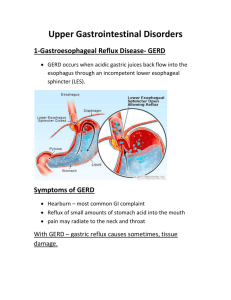
GI-GU EXAM #3 – 10/20/08 *** Missed Both Class Sessions *** 10/21/08 GI SECTION OF THE CLASS *** Flexible Fiber Optic Study *** Flexible fiber optics is a tool to check for inflammatory damage or other problems in the GI system. The tool can be used to investigate biopsy or give interventions in real time. With other tools, you have to schedule the biopsy or provide treatment at a later time GI OVERVIEW History Does the history separate the condition or is it part of the picture? Location of Pain -- Examples Many GI problems do have a pain component associated. Some problems get to the body core (front, side or back). Back pain can be misinterpreted. The problem will actually be internal and refer to the back. The conditions are often retroperitoneal based complaints. 1. GERD & Upper GI Pain: The classic pattern of upper GI problem is substernal pain. Pain behind the sternum may be a direct reflection of the body core. We can’t really test internal complaints with palpation, as we can’t push through the sternum. We note the location and note how the patient description of pain. A couple of fingers over the area of the sternum with a burning pain description may indicate reflux phenomenon (there is a strong correlation between the listed presentation and reflux). There is a 70% association between patients with GERD and patient presentation of fingertips rubbing up the sternum with stated, burning pain. 2. MI Presentation: MI also has a strong correlation between the way the pain is described and patient presentation of pain. The typical presentation and patient report list, “something sitting on the chest” with pain behind the chest and arm radiation. L shoulder is often associated with cardiogenic based pain. Cardiogenic pain can also slip into the R shoulder and into the jaw based on neurological distributions. 3. Gallbladder or Diaphragm Presentation: Referred pain to the deltoid may be diaphragm or gallbladder disease (sometimes R or L shoulder). 4. Epigastric/Stomach Pain: Pain in the epigastric area right beneath the xiphoid (epigastric area) that is poke able/palpable indicates stomach pain. The stomach is intraperitoneal. 5. Mid Back Pain = Pancreas Pain…We also have to worry about the aorta. 6. R scapular pain = Gallbladder or Pancreas (classically is the tip of the scapula). 7. Perimumbilical Pain = The patient describes the pain with fingers circulating around the belly button. In the differential list are: Appendicitis, and Diverticulitis. These conditions all start with belly rubbing and then localize as the disease changes/progresses. Onset of Pain 1. Rapid = Obstruction, or Obstruction Leading to Rupture…These are abrupt events. 2. Gradual Onset = Inflammation with increasing discomfort and fatigue. Other possibilities include: Carcinomas, Chemical Irritations, Reflux Irritation. GERD shows gastric secretions impacting the mucosal tissue. 3. Short Pain/Colicky Pain = Short, colicky pain is often transient distention. Fibrous bands can narrow the colon. When the patient eats, small dilation occurs at the proximal tub. The bowel then empties and allows material through the narrow space. Discomfort doesn’t hit to the next meal when material backs up in restricted areas. Transient distention, intermittent pain lasting seconds is the typical profile. 4. Longer Bouts = Irritation and Inflammation…Longer periods of time with discomfort. 5. Chronic Unrelenting Pain = This is the type of pain caused by cancers, metastasis, or chronic pancreatitis. 6. Pain for years with Mixed Pattern = Motility disorder, Chronic Bowel Disease, Whipple’s, Crohn’s…The motility problem can be neurological in nature. Duration of Pain Colicky Pain = Unsatisfied Contraction Ex. Biliary Colic = In biliary colic, the neurological system is in place and recognizes the stretch.. The motor system attempts to respond to stimulation but can’t fully empty the GI. The patient experiences phases of pain as the material is moved through the system. Character of Pain Burning and Cramping 1. Burning = Causes are either Chemical or Reflux…It is possible that both the pyloric valve and LES are incompetent. When both valves are incompetent, duodenal content goes back into the stomach. The pH then becomes more alkaline. Alkaline pH of the stomach by reflux irritates the gastric mucosa. Gastric juices are force into the esophagus. The esophagus can’t handle the gastric content. The esophagus can be damaged. The 2 valve problems may be iatrogenically induced, disturbing smooth muscles by inducing relaxation of the valves. 2. Cramping Pain = Motor Problem…Interference with motor work, leads to obstruction. The system can contract but is not productive (unsatisfied contraction - colic). DYSPHAGIA Difficulty swallowing. The patient reports that they feel food gets stuck and they need to wash it down with fluid. People can have dysphagia without pain. Odynophagia Odynophagia is problems swallowing coupled with pain. Causes of Dysphagia 1. Neurological = Stroke or CNS Problem…We can have neurological compromise leading to Dysphagia.. Stroke patients can have problems starting swallowing. The middle and lower parts of esophagus will then have problems triggering the motion of peristalsis. 2. Obstruction(Inside-Out Problems) = Cancer…We can also have things push from inside out (cancer) creating obstruction. 3. DISH (Outside-In Problems) = DISH…About 20% of DISH have dysphagia, as the ALL pushes into the area. Solid foods would bother the condition more so than liquids, particularly in DISH. 4. Congenital = Esophageal Atresia…We also have people that never have a normal tube (esophageal atresia) via congenital under-development. 5. Other Conditions Linked to Dysphagia = Reflux, Mallory Weis Syndrome, Varicosities – Esophageal Varices a. Esophageal Varices = Can be seen in people with drug addiction (inducing damage to the liver) or via portal hypertension (damaging the liver). Venous drainage of the esophagus is part of portal system and is valveless. 2 way flow through the venous network of the esophagus occurs with a diseased liver. The condition of portal hypertension can manifest as esophageal varices or as hemorrhoids. Elevation of pressure is exhibited throughout the system because of the liver. Webs can form around the esophagus impacting dilation. The webs cause swallowing of solids to be problematic and even painful. Venous engorgement can be so severe that contour can change in the lumen creating webs and varices. On contrast exam, the contrast would pass slowly and show fluid channels that resist pressure. *** Upper GI Study -- Varices Present *** Bag of Worms presentation, as the veins are overfilled to the point where they stiffen the wall of the esophagus. Types of Dysphagia 1. Total Dysphagia = Think CNS lesion or Meningioma...Total Dysphagia shows inability to swallow solids and liquids. Total Dysphagia is often linked with stroke patients or other CNS lesions (brain injuries, SOL). Loss of motor control of the esophagus occurs. 2. Progressive Dysphagia= Patient often reports that the condition gets worse over time. They go from trouble with solids to trouble with semi-solids to trouble with liquids progressing over time. 3. Fixed Dysphagia = The condition has always been this way. Liquids have never been a problem. Meat and solids are often a problem. They also report the more they chew the better it is or the smaller the portion they are. a. Congenital Webs = A fixed type of Dysphagia that allows passage of smaller items with larger items getting stuck. 4. Cardiogenic Dysphagia = Related to chamber enlargement (mostly the LV or RV) and can occur silently. Chamber enlargement creates an outside in pressure that causes the Dysphagia. 5. Foreign Body Dysphagia = Dentures, chicken bone, egg shell are examples of items than can be stuck 6. Scleroderma, SLE and Reynaud’s = These problems all involve connective tissues including tissues of the upper GI (mouth and esophagus). a. b. 7. Scleroderma = Can be linked with Reynaud’s phenomenon and 80% of the cases have difficulty swallowing. In. Scleroderma, the myoneuronal junction interferes with conduction of impulse causing lack of muscular response. Food gets stuck as the muscles become weak. SLE = Dysphagia is a connective tissue based problem with an active and quiet phase based on active involvement of the disease. Fibrosis can shrink when the acute autoimmune, inflammatory process goes down. Esophageal Cancers= Can create Dysphagia. GI cancers can be benign to very serious. A risk assessment is very important, particularly in the elderly. Anatomy of Dysphagia 1. Pre-esophageal = Patient has trouble clearing the pharynx…a). Plummer Vinson Syndrome = Webs that cross the pharynx 2). Tumor Plummer Vinson – Example of Pre-Esophageal Dysphagia The root cause is profound iron deficiency anemia (microcytic, hypochromic anemia). Some causes of Plummer Vinson induced Dysphagia are: 1. Dietary Iron Deficiency: More commonly seen in the elderly with nutritional deficiencies. 2. Poor Fitting Dentures: The dentures may cause pain in the gums and mouth during eating, so they choose not to eat. 3. Thoroughly Cooked Foods: The iron is cooked out of the foods (ex. spinach) 4. Blood Loss in the GI Tract = Leads to anemia 5. Combination = Combination of some of the above reasons The clinical picture is that liquids pass the web, but solids don’t pass and come back up. This is a pre-esophageal problem occurring around C5. They cough food up. Glossitiis (painful tongue) can occur. Red, Swollen, tender tongue is common to Plummer Vinson. Koilyonchia or spoon nails can develop where the contour of the nail changes as the nails become brittle. Long term, the iron deficiency anemia needs to be addressed. A thorough history helps to find the cause. The webs recede with iron supplementation. Swallowing is restored in weeks to months after supplementation is started. Another treatment is balloon catheter dilating/tearing the web. Supplementation must still be enforced before and after the balloon catheter as the condition can return without supplementation. 2. Esophageal = a). Congenital = A Ring/Schotzke Ring Hypertrophy b). Prior Injury with Fibrotic Repair 3). Carcinoma Barrett’s Esophagus & Epithelium – Example of Esophageal Dysphagia The condition occurs because of long standing GERD. GERD first causes Dysphagia and later shows tissue transformation. Everyone with various epithelium has GERD, but not everyone with GERD has varous epithelium. The frequency of acids that travels to the esophagus causes conversion from squamous to columnar epithelium. We find “gastric tissue” in the esophagus. This is metaplasia to gastric tissue in the esophagus. As a consequence, the patients have less reflux symptoms, but about 20% converts to carcinoma (adenocarcinoma). DIVERTICULUM Diverticulum can occur throughout the entire GI tract. Sigmoid colon statistically is the most likely site for diverticulum (of any kind). 1. Esophageal Diverticulum – Zenker’s Diverticulum, Zenker’s Diverticulum arises from an abnormality with the crico-pharyngeus muscle in the upper 1/3 of the esophagus. Local defect in the upper 1/3 of the esophagus is the most significant and most risky of the esophageal based diverticulum. We initially investigate for Zenker’s because of patient complaint. Failure or disruption to the cricopharygneus muscle is the root cause. The diverticulum enlarges because of one way valves/check vales. Enlargement allows content from esophagus into the diverticulum. The tissue stretches and pulls mucosal tissue in. Swallowing causes the muscle to be forced apart allowing food into the osteum. *** View on Screen *** We see an early defect. We then see mucosal tissue within the muscle (cricopharyngeus). Over time the diverticulum grows. *** Cervical Spine Film with Diverticulum Sketch Overlay *** The esophagus starts at about C5. Zenker’s is an upper 1/3 based problem starting at C5 or slightly lower. We have to go looking for the condition to come up with the diagnosis. The contrast column (white ball) moves into the diverticulum. Contrast can be “grape sized” or “ping-pong ball sized.” *** Chest Film *** 72” PA gives us a good representation of relative size. Zenker’s can even be larger than the aortic arch. If the chest film I taken at 40” AP, the shot gives magnification of Zenker’s. The film on screen demonstrates that the diverticulum is very big. The patient has trouble clearing the pharynx because the diverticulum takes up space. The diverticulum is positioned between the trachea and the spine. The diverticulum pushes on the esophagus anteriorly, but can’t go posteriorly because the spine is rigid. Dysphagia will be the complaint. Relaxation of the Cricopharygeus During Sleep – Zenker’s Diverticulum During sleep, relaxation of the criocpharyngeus occurs. The grip is effectively loosened and progressive Dysphagia occurs. Thick liquids and solids can now be problematic. The muscle loosens its grip and tissue decompresses forcing the content back to the esophagus. Content can end up back in the mouth. These food particles are not digested and putrefied causing bitter tasting vomit. The patients are in deep sleep and may be at risk for vomiting or swallowing the putrefied material. Request that the patient spit the food particles out. Have them bring the particle into the office. Check for mixed meals. Mixed meals means sequestration or obstruction in the esophagus. Ex. Meals over a couple of days in the diverticulum.. Dysphagia, putrefied vomit at night, mixed meals, screams Zenker’s Diverticulum. The most serious complication is aspiration pneumonitis. The epiglottis is relaxed during sleep. Relaxation of the of the epiglottis during sleep can allow food content/foreign body into the lung. The condition can cause foreign body pneumonitis, leaving scarring in lung tissue or bacteria infection of the respiratory system. *** Lateral View – Contrast Exam *** The collection of material is bigger than the vertebral body. Treatment of Zenker’s Diverticulum 1. Surgery = Old method of treatment. The complication rate was severe. 2. Endoscopic Cleaning/Lavage/Stitching = Now they wash it with saline and stitch the opening to close it off. Only in the worst cases, do they buttress the muscle. The procedure is now done endoscopically with minimal complications. 2. Traction Diverticulum MID ESOPHAGUS/HIATAL REGION OF THE LUNG (middle lung field) is the area of this diverticulum. The opening into the diverticulum is big showing free communication. Traction diverticulum are often silent and found incidentally with contrast exam. Lymph node inflammation triggers scar tissue adherence of the node to the esophagus. Scar tissue shrinks and pulls apart the outer layers of the esophagus creating a defect in the outer muscular wall of the esophagus. We don’t have Dysphagia because the diverticulum doesn’t push against any relevant structures. Often nothing needs to be done about traction diverticulum. See it, explain it and forget about it. 3. Pulsion Diverticulum Can occur from both congenital and acquired forms. Pulsion diverticulum occurs in the distal 1/3 of the esophagus and can grow very large. The large size still may not make it noticeable as no pain, no Dysphagia typically occur. The finding is often accidental. Gravity can hold content in the diverticulum. The diverticulum can be seen on plain film as a midline mass above the diaphragm a. Congenital = Esophagus doesn’t form correctly, missing a section of muscular wall coupled with mucosal hypertrophy b. Acquired = Acquired by obstruction due to: a). Foreign Body b). Hiatal Hernia. GU-GU EXAM 10/27/08 GERD *** Pre-printed slides *** Reflux: Dysfunction of anti-reflux mechanisms Caustic Material: Acid, pepsin, bile, pancreatic enzymes (pancreatic enzymes are a 2 valve problem --- LES & Pyloric Valve) Sufficient Duration of Contact: Inadequate clearance mechanisms Most times the caustic material is from the body itself and not exogenous poisons or toxins. In either case, the mucosal resistance is overwhelmed. Gastric Secretions Excess gastric secretions is often not the etiology of the problem. These patients are often prescribed medications for excess secretions, that aren’t effective because they don’t address the underlying problem (Lower Esophageal Sphincter/GastroEsophageal Junction). The source of the problem is lack of tone and un-coordination of the sphincter. Pattern of GERD 1. Erythema/Redness = First sign of injury to the distal esophagus is erythema/redness. The tissue is sensitive and annoyed. There is burning pain. Typically the patient rubs over the sternum. 2. Erosion = 2nd step is erosion with the defect contained by the mucosal layer. 3. Ulceration = 3rd Stage of the progression. Mucosal damage occurs with the problem penetrating to the submucosal layer. 4. Perforation = 4th Stage that shows rupture through the submucosal layer. Small numbers of people arrive at stage 4 (perforation). Sphincter Quality The LES is not a good sphincter and can be interfered with very easily. Mechanical pressure alone can defeat the LES. The condition can even be iatrogenically induced as medications can inhibit smooth and skeletal muscle relaxing the sphincters. Pregnant females in trimesters 2 and e can show GERD with increased IAP and hormones that cause relaxation of tissues and the LES. Pressure Change With Inspiration and Expiration Pressures vary in the LES with inspiration and expiration. Breathing in causes the hiatus to grip the LES a little tighter and causes increased pressure. Breathing out relaxes the LES as pressure drops about 10 mm. WE see a pressure difference of about 10 above and below the diaphragm. Pressure changes favor reflux of stomach content back into the esophagus. Normal Resting Pressures LES = +25 mm Hg (poor excuse for a sphincter…very easy to interfere with) Intra-Thoracic = -5 mm Hg Intra-abdominal = +5 mm Hg *** Study on Overhead *** Mannometers: Long string with yellow pellets that is a series of pressure sensors put into the system. pH Sensors: Can be attached to a string monitoring pH of the area above the GE junction Examples of GERD IN a patient with LES weakness, sudden changes in intra-abdominal pressure will show change in LES pressure leading to symptoms associated with GERD. Breathing in creates better separation between esophagus and stomach. Breathing out may show acid splash due to pressure changes. Pushing on the patient suddenly causes changes in IAP (intra-abdominal pressure) and drop pH as acid is forced into the esophagus. When pressure is release (stop pushing on the patient), the pH goes back to normal. Changes of position, sneezing, coughing, punching or poking the abdomen can mechanically overload the stomach and LES leading to GERD. *** Study on Overhead -- Graphs*** Each pressure spike from the pharynx to the esophagus is called advancing peristaltic wave. The condition is normal. The Upper 1/3 of the esophagus is skeletal muscle (striated). We get obligatory contractions of the middle and lower 1/3. We can’t consciously control the middle and lower 1/3. The advancing waves propel the material down the esophagus. Interruptions of the advancing peristaltic waves lead to dysfunction. The activation of the primary wave shows a pH of near 7. 7 is a normal value. If the LES does its job and isolates the stomach from the esophagus, the pH is neutral. In GERD, stomach recoil occurs because of changes in pressure and poor LES quality. Failed Peristalsis Contractions don’t occur in middle and lower 1/3 of the esophagus. The LES relaxes and acid enters the esophagus. The pH sensor is triggered in the upper portions of the Esophagus. The gastric acid and gastric secretions must travel a good deal upwards to trigger the sensors. Prolonged relaxation allows stomach recoil jutting content back into the esophagus. 24 Hour pH Monitor The test allowed us to discover hormonal, mechanical and other pathological ways (ex. medications) to interfere with the process. Hiatal Hernia Most frequent complaint with a hiatal hernia is GERD. Manual reduction of the hiatal hernia is possible and can help with both the hernia and GERD. The technique is a low tech way to help the patient. Peptic Esophagitis(due to GERD) – Signs and Symptoms Sour Taste: Esophograms show bubbles rising up the esophagus stimulating the taste receptors on the back of the tongue. Sour tastes can be triggered by carbonated beverages and antacids. Difficult or painful swallowing; choking: Early symptom is painful swallowing. Fibrotic repair and shrinkage of fibrotic tissue leads to progressive Dysphagia with limited contraction. Choking is due to more prominent problems like presbyesophagus. Chest Pain (r/o cardiac): Tends to be retrosternal pain. Assess the likelihood that heart disease may be the cause with thorough testing. The DDx can be hiatal hernia or cardiogenic pain. Back Pain: A common complaint of back pain/parathoracic pain. True referral pain is not reproducible, so separate the biomechanical (which can be provoked) and the referral (can’t be provoked). Heartburn Epigastric pain or distress Nausea and vomiting Anemia (blood loss): Long-standing conditions…Check for palor, Low BP, high HR…Do a blood panel to document for anemia GERD WITH CHALASIA *** Picture on Overhead of Young Kid *** Chalasia is an extreme version of GERD that shows free communication between the stomach and the esophagus via the LES. We can’t tell whether contrast goes in or contrast goes out as they look alike. *** Endoscopic Picture on Overhead *** The first 3 destructive stages of GERD are present: 1).Erythema 2). Erosion 3). Ulcer. The outer rim is red indicating erythema. The gray rim is erosion. The white rim is the ulceration. Ulceration goes into the submucosal tissue. The shiny/silvery areas are scar tissue that will shrink over time, restrict the opening and cause Dysphagia. Drug Management Patients are sold anti-secretory meds (proton pump inhibitors or H2 blockers). The condition is usually not over acid production. The condition is weak muscle. Medication to treat the weak muscle of the LES affects every other muscle and valve in the body. Medication to treat the pH/acidic problem masks the condition improving symptoms while not addressing the root of the problem. Overall, drugs are not the solution as they can only treat symptoms and not the problem. GERD With Transition to Barrett’s Esophagus *** Picture on Overhead *** Distal Esophagus above the LES shows ulceration with fibrotic repair. This patient has Dysphagia and reflux. The condition may be driven to metaplasia (Barrett’s Esophagus). Barrett’s occurs when esophagus becomes more gastric in nature. Reduction of irritation occurs as the esophagus becomes a more gastric environment. 1/5th of the time the condition can go to adenocarcinoma, a serious tumor of GI tract. GERD With Hyperplasia and Anemia Hyperplasia (tissue overgrowth) can also occur. Blood leakage is common. Sometimes the patients throw up blood. Blood loss can be sufficient to create anemia. Menstruating females with GI bleeds are more likely to be anemic. GI blood loss is the most common source of iron deficiency anemia in men, and in the top 3 for blood loss iron deficiency anemia in females. It deserves investigation. Ulcer vs. Tumor *** Picture on Overhead *** A white rim is present where contrast collects. White radiating lines are called Spoke Wheel appearance. The ulcer is the hub and the spokes are the white lines. Spoke wheel appearance is typically an ulcer. Tumors can also ulcerate. The most mature center of the tumor outgrows its blood supply as it attempts to push outwards. The lack of blood supply to the tumor foci causes liquifactive necrosis. The tumor collapses into itself as a crater, cradling contrast, looking like an ulcer during radiographic exams. The tumor obliterates the ruggal folds. An ulcer crater without spoke wheel appearance is almost always an aggressive cancer till proven otherwise. Typically, it is comforting to have ulcer with spoke wheel appearance because that is a benign indication that an ulcer (not a tumor) is present. 3 Patterns of Contrast Collection 1. Benign/Intramural Ulcer = a). Contained b). Non-contained 2. Diverticulum = Increased Sized contrast column in the esophagus, SI, or stomach 3. Intraluminal Collection = Cancerous (contrast collects in the center)… Heartburn in Pregnancy Frequency 30-50% in Pregnancy Mechanisms: Hormonal: Increased Estrogen and progesterone ---- LES dysfunction Mechanical: Enlarging Uterus --- Increased Intra-abdominal Pressure Commonly both hormonal and mechanical causes the sphincter to he incompetent…Middle to late trimesters are more common Common Therapies: Antacids, Sucralfate, H2 Blockers Simple Solutions to GERD Management This is a management problem for chiropractors. 1. Patient education (smaller meals) 2. Do not eat and lay down (it brings fluids and secretions in greater contact) 3. Examine medications 4. Lay R side down = Takes product away from opening and can help reduce discomfort. 5. Eating and staying upright is a good solution. Hiatal Hernia and GERD LES Dysfunction– Pressure often low Gastric Pouch – Intrathoracic Reservoir Diaphragm – No Esophageal Pinch *** Axial/Sliding Hernia *** LES is pulled from esophageal hiatus and we don’t support from diaphragm. The hiatus holds onto the cardiac portion of the stomach. They have an extra 15 mm of pressure differential causing the reflux. The most common complaint is retrosternal burning called heartburn/GERD. Barrett’s Esophagus & GERD Columnar Epithelium replaces squamous epithelium in the distal esophagus Metaplasia occurs. We need to reduce the GERD incidence and reduce further conversion of tissue. Watchful waiting is the appropriate response. 1x per year for the next 2-3 years we biopsy/ check for further neoplastic change. They check for 2-3 years in a row, and then if no problem they then check every 2 years. 8/10 times the change in benign. 2/10 times malignant change can occur. Surgical methods remove GI tissue. Removal of GI tissue comes with complications as nervous plexi and vascular channels need to be restored. We also worry about intra-thoracic and peritoneal complications. (peritonitis). Risk to benefit ratio must favor surgery for it to be performed. Incidence of Adenocarcinoma – Barrett’s Esophagus 800 cancers per 100,000 patients 1 cancer per 125 patients (.8%) Indications for ambulatory Esophageal pH Monitoring Patients with normal endoscopy and: Typical GERD symptoms unresponsive to anti-reflux therapy Atypical Chest Pain Extra-esophageal disorders possibly related to GERD (asthma, chronic cough, chronic hoarseness, posterior laryngitis, and globus) Patients with endoscopic escophagitis unresponsive to anti-reflux therapy Patients considered for anti-reflux surgery: Surgery tightens the hiatus…Lots of risk and expense (including achalasia or diaphragm risk.) Recorder Tool and 24 Hour Monitoring Monitors pH and secretory changes. It may be a better tool than endoscopy and contrast exams. The recorders help explain that there is more ways to interfere with mechanisms than what we thought. Do not choose a – test result from contrast or endoscopy over the patient presentation. 24 Hour pH monitoring is the best way to concur or eliminate the GERD diagnosis. Extra-Esophageal Problems and GERD Extra-esophageal based problems may be linked with GERD (asthma). The gastric secretions inflame the airway and can induce swallowing of material (due to bypass of the epiglottis). Swallowing of material/gastric secretions stimulates an asthmatic attack. Chronic cough and hoarseness are though to be a product of repetitive GERD on the vocal cord with changing vocal characteristics. Lifestyle Modifications Elevate the head of the bed: Little Elevation (2-3 inches) Lose Excess Weight…10% reduction in weight has a big impact on joint pain and GERD. 10% is do-able. Eliminate: Tobacco: Alcohol: Bedtime Snacks: Don’t eat and lay down (1-2 hours before bedtime). Food stays near the opening of the stomach and can create pain. The distress by eating and lying down is related to what they eat. Alcohol and fatty foods can induce the reflux. Hot sauces can be mucosal irritants further damaging/irritating tissue. The stomach takes longer to get rid of proteins, fats, and irritating foods. Certain Drugs: New drugs or changed medication can impact GERD (changes in dosage, changes in drugs) Fatty Foods Chocolate Peppermint Others: Tight Clothing (increased IAP), Back Belts & SI Belts (Increased IAP), Inversion Tables, Thoracic Subluxation 10/28/08 *** Missed 1st hour *** ESOPHAGEAL VARICES & DYSPHAGIA *** Esophogram on Screen *** “BAG OF WORM APPEARANCE “ = A contrast term for coiling, linear filling defects of the esophagus. IN this patient, portal hypertension and esophageal varices are present. As a consequence of alcoholism, damage to liver caused backup and esophageal varices. This is a management problem. MALLORY WEIS SYNDROME Alcoholism, induced vomiting. The vomit causes tearing (vertical/linear) of the esophageal lining. The person may note blood with vomit that is bright red arterial blood. Angiogram is a better test than contrast exam for this patient. Brisk bleeding is managed with cauterization via endoscope. Violent retching causes esophageal tears, inducing blood loss. CHALASIA Classically, chalasia is opening and puking (free communication between stomach and esophagus facilitates the vomiting). In children over 3, reliable vomiting requires a contrast study or endocscopic exam. If +, it may require aggressive management. In newborns and infants, chalasia is normal. PRESBYESOPHAGUS There is age related un-coordination between primary and secondary peristaltic waves. In very bad presbyesophagus, they cant’ swallow properly and must flush the food/bolus down with fluids. The un-coordination can be modest enough to be occasional problem and severe enough to be every meal. Medication and surgery are not effective options. This is a management process. The diagnosis of presbyesophagus is given with testing and diagnosis by exclusion. Doctors rule out diabetic neuropathy of the esophagus causing Dysphagia.. History helps separate the 2. Presbyesophagus is slowly progressive, adult aged, with denial of DM. Diabetic neuropathy of esophagus shows the problem as a juvenile, long history with DM problems, and Dysphagia is the latest complaint. Upper GI barium swallow test shows a weak to absent upper 1/3 contraction. We show suspension of the barium column indicated by more than 2.5 contractions to force the food downward. Solid foods tend to produce prominent symptoms and liquid foods are easier to manage. Radiographic terms include curling phenomenon/barber pole phenomenon, showing white and black areas. The problems is a management problem, not a drug or surgery problem. Have the patient drink fluids. Also, remind them to eat foods that are more liquid/easy to swallow and chew the food more before swallowing. DIFFUSE ESOPHAGEAL SPASM The spasm shows significant pain and can be spontaneous or due to cold liquids. The spasm can be mistaken for a heart attack. They have a normal contrast study. History and exam should be geared towards ruling out DM, SLE, and Scleroderma. Also, rule out hiatal hernia. This is a diagnosis by exclusion done by testing. ESOPHAGEAL ATRESIA Congenital Esophageal Abnormality = A “sheet” across the esophagus that causes blockage. Classification system 1. Class 1 = Complete Absence of the Esophagus = We won’t see this often. The pharynx ends in a stump and there is a space where the tube should be. The tube never united. This occurs with other organ mal-development. Class 1 can be a lethal, congenital abnormality. Regurgitation is a hallmark feature. 2. Class 2 = Membrane Blockage of the Lumen = The motor and nervous system are intact. The parts of the esophagus are there. Antero-lateral surgery can be done to stitch the parts together. At first, there is a fibrous zone that doesn’t react to stimulation. In children, stem cell regeneration occurs. Regurgitation is a hallmark feature. In children, regurgitation occurs very quickly. 3. Class 3 = Fistula….Fistulas show abnormal communication/conduit between esophagus and trachea. Mother’s milk can be trapped in the fistula causing aspiration pneumonitis. The foreign proteins of milk annoys the lung tissues. The history is a young kid with multiple episodes of pneumonia. Repeatable episodes make the condition stand out. Chest film may show consolidation. Contrast exam may show a channel. Endoscopic exam cannot be used unless the child is over 5 lbs. Repeat pneumonitis will impact quality of life. Fistula induced pneumonia/aspiration pneumonitis is the most common reason for pneumonia in newborns. Doctors stitch the esophagus during a minimally invasive procedure. The procedure has excellent long term prognosis. MISCELLANOUES ANOMALIES & DYSPHAGIA 1. Duplex Esophagus = One good tube and one bad tube. 2. Duplex Pharynx = A Y shaped entry via 2 pharynxes meeting up. Usually the smaller one causes the problem. Duplex pharynx or esophagus is usually surgically managed if problematic. If not a problem, they will leave it alone. PLUMMER VINSON -- DYSPHAGIA Dysphagia with early vomiting are clues to think about Plummer Vinson. Contrast studies are not good to identify the condition as liquids pass right through the webs. The best study is endoscope or even a mirror on a stick to view the webs. Profound iron deficiency anemia triggers the webs. Iron deficiency anemia can happen in kids and the elderly with poor socio-economic status. Another reason can be poor fitting dentures. Poor fitting dentures will make the gums raw. Another way is via the loss of blood. Webs also keep out foods with iron that further perpetuates the problem. Treatment for Plummer Vinson Supplement with Iron. Iron injections Balloon Popping of the webs + supplementation…If we pop them too quickly and do not supplement, they will come back…You typically wait 3-4 weeks after supplementation to pop the webs. Blended foods with iron are preferable prior to popping of the webs. CONGENITAL ANOMALY OF STOMACH --- DEXTRO POSITION Hiatus on the R. Terminal end is on the L in this condition. The duodenum is dragged over as well. This can be a complete flip (situs inversus where everything is flipped --- all the organs are reversed) or partial flip. The more complete the reversal, the less chance for problems. Situs inversus may be found by mistake, thinking the marker was placed in the wrong spot during an X-ray exam. PYLORIC STENOSIS & GERD The condition is both congenital or acquired. A). Congenital = In infants the situation is congenital. The theory goes, in utero, the fetus gets strong stimulus to the pyloric valve. The valve becomes so massive it is “muscle bound.” The pyloric valve cannot relax or is incompletely relaxed. IN children, strong stomach contraction and improper opening are linked with weakness in the LES. The baby spits due to healthy contraction by the stomach (normal in children). Pyloric stenosis patients will spit for great distance (often feet). B). Acquired Version Seen in adults with peptic ulcer disease. Peptic ulcers irritate/facilitate or damage/fibrose the tissue. If the ulcer is near the pyloric channel, it can be facilitated keeping the pyloric valve in spasm. The condition can show fibrotic repair with closure of he pyloric valve. Stomach contraction forces material through the LES. The description is, “I’ve thrown up before, but not like this and every time now it happens like this.” Contrast exam is used and we see delayed gastric emptying. There may be reverse peristalsis present during vomiting. We watch the contrast in real time and we won’t see dilation of the valve indicating stenosis. HIATAL HERNIA Types of Hernias 1. Sliding Hiatal Hernia/Axial Hiatal Hernia = The simplest and most common of the hiatal hernias. The hiatus is squeezed. The hiatus is pulled or pushed above the diaphragm. The most common complaint is retrosternal burning from GERD. Reflux with retrosternal burning is the most common complication of hiatal hernia. Hernia Terminology A). Incarcerated Hernia = The condition is not reducible. This patient needs to go to the hospital. We need to listen for bowel sounds above the diaphragm (as evidence that function occurs). Loss of bowel sounds is a bad sign indicating an immediate emergency B). Strangulated = Worst Case Scenario…Occurs once the condition goes silent. Venous engorgement increases pressure to match arterial pressure. When pressure equilibrates, no net flow of blood, nutrients and gases occurs. The GI tract becomes ischemic. The patient will be in extreme pain. This is an emergency! C). Double Bubble Sign/Double Density Sign = Thick walled collection of contrast (?) in the GI and biased to the posterior indicates a hiatal hernia. D). Reducible = If the grip is not tight, the condition is reducible. The condition is manageable and does not require surgery (often in sliding hiatal hernia/axial hiatal hernia) *** X-ray *** Flat white line is air fluid level. Gas collection that project above the heart = double density sign. *** X-ray *** Granulomas are present with increased fibrous tissues on R side of the heart. We think a full hiatal hernia is present *** Contrast on Same Patient *** Quite a bit of stomach is above the diaphragm. We see a 9 cm thoracic aortic aneurysm on the film. We take notice at 3 cm, 4 cm is a vascular consult, and at 9 this thing is ready to pop. The study is used to document. In today’s medical world, 9 cm aneurysms always rupture. 2. Rolling Hiatal Hernia/Para-esophageal Hernia = Stomach rolls next to the esophagus in the hiatus. Paraesophageal hernia is a greater producer of Dysphagia than sliding hiatal hernia. Limited ability to dilate causes Dysphagia by not allowing food. through. They point to the area (food is stuck here). Theses patients can get reflux that is not esophageal reflux, but static secretions in the stomach. Prolonged stomach contact can create irritation and is a pain generator. They show retrosternal burning due to retention of HCL above the hiatus. It is more difficult to put food into the esophagus due to the tight fit of the hiatus. . *** Contrast Study *** Contrast above and below the diaphragm indicates a paraesophageal hernia. 3. Intrathoracic Stomach Hernia = The stomach is connected to the pharynx. The stomach is pulled above its normal alignment because of surgery, tumor, or removal of a tumor. The problem can also be congenital. The tissue above the diaphragm is not held by ligaments. The tissue can fold and strangle itself. The name is volvulus (folding of GI tissue). Volvulus and strangulation cuts venous drainage, raises pressure and creates ischemia Serious problems can develop. *** The 3 types of hernias can then be further separated into: A). Reducible B). Incarcerated C). Strangulated *** Reducing a Hiatal Hernia Heel Drops: quickly drinking a little water and have them rise on their toes and drop down (calf raises) At most, go up 1 step and 1 step only and jump landing stiff legged to reduce the hernia. If that doesn’t work, call the doctor and get them in. Put them on a table with about 15 degrees of angulation (bending knees) to soften blow. Breathe in deeply to maximally flatten the diaphragm. The doctor must poke pretty deep in the middle of the diaphragm. As they blow out, traction down. Do it 3-5 times. This maneuver may reduce the stretch irritation causing less problems. 11/3/08 DIAPHRAGMATIC HERNIAS Can be acquired or congenital. 1. Bochdalek Hernia = A diaphragmatic hernia, that tends to congenital and posteriorly located. It is incomplete formation of diaphragm or gap in fibrous tissues. These hernias are usually paired. *** Pneumonic…Bochdalek = Back *** 2. Morgagni = Defect is 1 side or other (typically L) in the area of the xiphoid (anterior hernia). The dome of diaphragm is missing and will show the liver above the diaphragm on the R. 3.Hiatal = Most famous of the diaphragmatic hernias. ______________________________________________________________________________________________________ GASTRITIS Inflammation of the gastric mucosa. The suspected etiology list is long. There are many ways to irritate the mucosa to make the condition symptomatic. Gastritis is not a specific entity. ACUTE GASTRITIS Pink, red and inflamed tissue is present in the mucosa. The condition can progress, but most people stay in this category. 1. Aspirin = Can cause acute gastritis…Older people often take this as a blood thinner to prevent clotting in the arteries. People are using aspirin with greater frequency for pain control and for anti-coagulant properties. The long use and abuse increases the risk for gastritis. We try to take the lowest affective dose (about 25 mg – the baby aspirins) to reduce risk. Inform your patient of this and have them ask their doctor if the dose may be too high. 2. Excess Alcohol = The amount is variable. Generally, drinking so much that your stomach hurts is too much. Alcohol affects gastric secretions (increasing secretions) and irritates your stomach. 3. Heavy Smoking = 2 Main reasons for inflammation: 1). Vasoconstrictive chemicals in the stomach that don’t allow normal dilation. Tobacco keeps the vessels narrow limiting blood flow and limiting repair of GI mucosa. GI mucosa is very metabolically active demanding a lot of blood flow. Decreasing blood flow leads to loss of mixing/mashing function as well as loss of gastric secretions. 2). Tobacco weakens the control over the pyloric valve and pyloric reflux develops. Stomach contents return from the duodenum. Mucosa weaken when alkaline products are forced back into the stomach. Bile salts, pancreatic and liver products come back and attack of gastric mucosa. The stomach attempts to fight the rise in pH, by increasing the capacity of chief and parietal cells to increase acid load. The end result is injured tissue that can’ resist alkaline loads that irritates itself by its own acidic productions. ***The key ingredient is choice. We choose to take aspirin, choose to drink and choose to smoke *** Other Etiologies: 4. Chemotherapy 5. Food Poisoning 6. Uremia 7. Infection a. Cytomegalovirus b. B). H. Pylori = Linked with peptic ulcers & duodenal ulcers. 7/10 people with peptic ulcers have H. Pylori. 15% of people with culturable levels of H. pylori show acute gastritis 8. Stress Gastritis Complaints Most complaints are due to contact irritation. Pain is listed as being below the liver, burning pain projecting to the abdominal wall (not retroperitoneal). The patient’s condition can get bad enough to get the true anorexia. The inflammation of the gastric mucosa is so great, that edema forms in the wall of the organ triggering the stretch receptors in the satiety center of the brain causing anorexia. Gastritis patients live in a persistent state of stretch simulation. The stretch stimulation suppresses the appetite. Other complaints are fullness, vomiting and general discomfort. We often miss gastritis with a lot of – studies. Endoscopic analysis increases our findings of erythema (typical of gastritis). The endoscope allows us to sample tissue. The endoscopic exam with biopsy is the poof + or proof – for gastritis. We find the irritating substances in the gastric mucosa tissue. The worst cases of acute gastritis may show slight elevation of body temp. They can even get some shaking and chills. This tends to be the patient that may transition into chronic gastritis. The worst cases of acute often transition into chronic gastritis. Treatment Ask the patient about recent nutrition, smoking, drinking, aspirin use and other habits. You may want to ask them to amend their habit. Another thing to do is to adjust the mid-thoracic subluxations. Endoscopy with Biopsy They have to complain about the case several times to get endoscopy and biopsy done. The first time, the test is usually not approved. Most of the time, they improve with specific dietary and habit recommendations. If the case continues and the episodes repeat, you need to address the issue. CHRONIC GASTRITIS Histological change in the wall of the stomach with fibrous tissue found on endoscopic exam in the mucosa indicates a change from acute to chronic . The increase in fibrotic tissue causes loss of function: 1). Loss of muscular activity 2). Decreased Secretions. The repair site and tissue continue to get inflamed. The patient tends to worsen/progress with time as more tissue becomes fibrotic. Causes of Change from Acute to Chronic 1. Drugs = Specific drugs, including aspirin can lead to the fibrotic change. 2. Inflammatory Bowel Disease = Particularly Crohn’s….Most famously the site is the distal ileum, but it can be anywhere from mouth to anus. The condition can even affect the stomach. 3. Viral Infections = Can lead to fibrotic change. 4. Idiopathic = We can’t identify truly the source of the insult. We can identify the histological evidence and diagnosis, but can’t find the etiology. Our Role Observe the situation and make available the choices to the patient. AS fibrotic changes increase, secretory levels decrease.. We lose the ability to break down proteins and our poop becomes protein laden. The patients may go after endogenous proteins and we see “mushy muscle” (muscle is a source of protein storage). WE may see anemia(pernicious anemia). Patients can have low levels of acid (achlorhydria). Supplementation is often the best conservative way to treat chronic gastritis. GIANT HYPERTROPHIC GASTRITIS/MENTRIERE’S DISEASE *** Upper GI Study on the Screen *** The hills are too big and the “valleys are too small” as thin contrast streaks in the antrum are present. We see enlargement of the cells of the rugal folds generating the “high hills.” Gastritis occurs as pain/irritation occurs in the stomach. The hypertrophied tissue displaces gastric and parietal cells. We lose secretory capacity. We see bulky stools with large molecular weight proteins. Acid output of stomach declines. The condition is progressive. The etiology is idiopathic. We are concerned because we cannot tell the difference in contrast between lymphoma and giant hypertrophic gastritis. Lymphoma is more serious and should be considered with + contrast study. Stretch receptor stimulation is present that sends message to the cord. The satiety center is stimulated. They show true anorexia. This is a patient that cannot break down proteins n the stomach. Uptake is not available in the SI. They go after muscle or endogenous protein sources. Patients lose strength and get “mushy muscles.” They are overly tender (myomalacia --- softening of the muscle). Hypoalbuminemia can also be present. *** Menetriere’s Slide = Looks identical to Zoellinger Ellison on Contrast Exam because of impact to ruggal folds *** ACID OUTPUT TESTING BAO and PAO Testing – Acid Output Testing Nasogastric tube is introduced by the nose and worked down to the antrum of the stomach (pre-pyloric area). The first measurement is the BAO (Basal or Base Acid Output). This is the pre-stimulus measurement or the measurement at rest. We then do a histamine challenge test. Histamine increases Gastrin. Gastrin is the hormone responsible for chief and parietal cell secretion. With histamine ---- gastrin ---- chief and parietal cell increase --increased release of HCl ---- PAO (Peak Acid Output). 1. Normal BAO should be less than PAO (drop in pH should occur when going from rest to stimulus to peak stimulus) (E/N = Essentially Normal for BAO and PAO) *** Gastritis has normal secretory profile, even with a complaint. BAO is less than PAO, with BAO and PAO normal in gastritis *** 2. Hypo-secretory patients will have BAO at normal range. Histamine administration shows low PAO. So in hypo, BAO is less than PAO (but PAO is decreased when compared to normal). This is the Giant Hypertrophic Gastritis patient. (BAO is essentially normal for Hypo) *** Menetriere’s/Giant Hypertrophic Gastritis shows less #’s of chief and parietal cells (early hypo-secretory condition). *** 3. Hypo-Late = We see decreased BAO and very low PAO…Hypo-Late shows BAO less than or equal to PAO (with decreased BAO) *** Hypo-Late can show great compromise in the stomach and BAO can equal PAO levels but BAO is very low and PAO is exceedingly low (due to low BAO levels). The patient is at peak due to loss of cells. *** 4. Hyper Secretory = Increased BAO, yet PAO is essentially normal…BAO is roughly equally to PAO (PAO is roughly normal). We say that the stomach is living in an maximal secretory environment. We can’t get the stomach to go beyond maximum...Ex. person running on a treadmill and you force then to run faster and faster, at a certain point that can’t go faster and they are at peak output. The same occurs in the stomach where the stomach is at max output and peak demand. *** Hyper (Zoellinger Ellison or GASTRINOMA where the patient is in a persistent state of hyper secretion (BAO levels are high, give them histamine, and we see PAO levels in normal range and BAO about equal to PA…So we think the stomach is in stimulated state because BAO is very high) *** *** Be able to predict an outcome with information from the chart *** ZOELLINGER-ELLISION SYNDROME/GASTRINOMA Gastrin secreting tumor present, that can’t be shut off. They are outside the – feedback loop. The stomach always produces acid. The duration of peak level production of acid overwhelms the mucosa. The ruggal folds hypertrophy. Persistent demand of peak output from the body requires reserve capacity. The stomach tries to be more capable with HCl and Pepsin. The body reacts to the stimulus hypertrophying the ruggal folds. This patient is in the hyper category on the acid load chart. The cause is tumor. The tumor can be in many locations including pancreas, stomach, and Meckel’s diverticulum. Zoellinger Ellison Syndrome Clinical Triad Gastric Acid Hyper-secretion Severe Peptic Ulcer Disease Non-beta islet cell tumors of the pancreas The tumors produce Gastrin (G17 and G34); referred to as “gastrinomas” Tumors localized usually to head of pancreas, duodenal wall or regional lymph nodes. About ½ of gastrinomas are multiple and 2/3 malignant About ¼ have multiple endocrine impact???? Clinical Features That Can distinguish ZE Syndrome from DU Diarrhea = Increased gastric acid secretion Weight Loss/steatorrhea = Decrease duodenal/jejunal pH inactivation of lipase, Mucosal Inflammation Large Gastric Folds = Trophic Effect of Gastrin Large amounts of gastric secretions = Secretory effect of gastrin Family history of endocrine tumor, Increased Calcium= MEN 1 = Parathyroid tumor/hyperplasia Intractable or Post-surgical recurrence of ulcer disease = Acid Hyper secretion due to ??? Fasting and Stimulated Plasma Gastrin are Sensitive and Specific in the DX of ZE Syndrome ZE Peak # = 150-100,000 in fasting state Normal Patient = Less than 150 in fasting state Treatment of ZE Syndrome is Based Upon Clinical Findings A). If isolated duodenal wall tumor is present on CT and/or visceral angiography = Surgical resection followed by measurement of gastric acid secretion B). If no evidence of primary tumor, or metastatic tumor = H/K ATPase inhibitor or H2 receptor antagonist therapy in dose determined individually to suppress fasting acid output to less than 10 mmol/h. Drug efficacy check at 3 month intervals *** Total gastrectomy is generally obsolete. Removing the tumor rather than the stomach will reduce gastric secretions (we recognize we change gastrin levels by removing the inappropriately secreting tumor *** Imaging Studies MRI, PET, Radionucleotide Studies = Tumors signal very differently than surrounding tissue . ZE looks very similar to Menetriere’s on Contrast Study. ZE vs. Menetriere’s ZE hypertrophy shows stimulated capacity to increase (hyper-secretory on acid output testing) vs. Menterieres which shows a hypo-secretory condition. Mentriere’s treatment is just management. ZE treatment is the hunting and removal of tumors. 11/4/08 PEPTIC ULCER DISEASE The cause of why people ulcerate may be multi-factorial, including: environmental, what they eat, bad formation of mucosal tissue, bacteria (H. Pylori), medication (Prilosec, Tagament, Zantac, and Nexium). The medical community thought too much acid was the problem. In reality, the medical pathomechanical model may be wrong. 90% of duodenal ulcers are associated with H Pylori and 70% of gastric ulcers are related to H. Pylori. Research found that you do indeed feel better on the standard medical drugs for ulcer, but when you stop the meds you feel the same or worse. The patients were experiencing relief of symptoms, but the volume of tissue damaged increased and greater # of ulcers occurred with traditional drug management. . What they found, was acid bothers ulcers. 8/10 patients on meds relapsed and got the disease again. He found that 8/10 treated by antibiotics stayed better, 1/10 was about the same and 1/10 relapsed. This is a complete flip of the response, generated by aggressively treating the cause of ulcers (H. Pylori) and not the symptoms (acid production). Overproduction occurs in less than 10% of the ulcer conditions. Most drugs don’t treat the disease, they manage the condition. Peptic Ulcer disease Remains One of the Most Prevalent and Costly GI Disease Prevalence Patients seen by physician….3-4 million (increased more today) Patients self-medicating…….3-4 million (increased more today) Total Patient Visits to Physicians…….12-14 million Hospitalizations…….Grater than 400,000 (down) Total Days…… About 4 million (down) Deaths….About 9,000 (down) Operations….Greater than 130,000 Total Costs (indirect and direct) = Around 7 billion (increased more today) Peptic Ulcer is a Common Disease The annual incidence of active ulcer (Gastric Ulcer and Duodenal Ulcer) in the US is about 1.8% - 500,000 new cases per year In addition there are over 4 million recurrences yearly Hospitalizations For Bleeding Upper GI Lesions are Increasing Along with Increased NSAID Use Prescription for NSAID’s tripled from 1975 to 1985. NSAID use today has increased dramatically and so have complications . Peptic Ulcers are Caused by Increased Aggressive Factors and/or Decreased Defensive Factors Increased Aggressive Factors and/or Decreased Defensive Factors…(leads to)…Mucosal Damage…(leads to)…Ulcer Examples Ex. Too much alcohol and drugs --- Aggressive chemical attack (increased aggressive factor - drugs) and secondary decreased defenses of the mucosa lead to damage (decreased defensive factor). Gastroduodenal Mucosal Integrity is Determined by Protective (“Defensive”) and Damaging (“Aggressive”) Factors Protective Factors = HCO3, Mucus, Blood Flow, Growth Factors, Cell Renewal, PG VS. Destructive Factors = H+, Pepsins, Smoking, Ethanol, Bile Acids, Ischemia, NSAIDs, Hypoxia, H. Pylori…H Pylori and NSAIDs cause the most damage….H+ should be at the bottom of the list as we’ve found it is not as big a concern…Hypoxia occurs in smokers’. Smoking impacts valve function and bile acids can reflux back to the stomach. Gastric mucosa is designed to resist acidic pH. Alkaline load regurgitated back into a acidic environment can destroy tissue. *** In healthy people = Protective balances Damaging factors *** The Ingestion of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) Daily is a Major Factor in Ulcer Pathogenesis, Complications and Death 3x10 to the 6th power in the US take NSAIDs daily About 1 in 10 patients taking NSAIDs daily have an acute ulcer 2-4% of NSAID users have GI complications each year Greater than 3000 deaths/year and Greater than 25,000 hospitalizations/year NSAID’s Are associated with an Increased Incidence of Bleeding Ulcers Gastric Ulcers: Risk Ratio (Increased 10-20x) Duodenal Ulcers: Risk Ratio (Increased 5-15x) Increased risk proportional to daily dose of NSAID NSAID Ingestion Causes Both Acute and Chronic Gastroduodenal Injury All NSAIDs produce mucosal damage Ulcer risk is dose-related Acute Mucosal Response does not predict subsequent ulcer risk Acute Ulcer & Damage (1-2 Weeks): Mucosal Erythema (60-100%), Subepithelial Hemorrhages (60-100%), Erosions (60-100%), Increased Fecal Blood Loss (60-100%), Chronic (greater than 1 month): Gastric and duodenal erosions (40-60%), Gastric and duodenal ulcers (10-30%) 11/4/08 Gastric Acid Secretory Rates Are Altered In Patients With Upper GI Diseases Normal: Basal = 1-8 mmol Peak Pentagastrin = 6-40 Decreased with: Pernicious Anemia = 0-1 0-5 Gastric Atrophy = 0-2 0-10 Gastric Ulcer = 1-3 2-20 Gastric Cancer = 0-5 0-30 Increased With Duodenal Ulcer 1-15 12-60 Gastrinoma 5-80 20-110 *** There is extensive overlap between groups *** Duodenal Ulcer is a Disease of Multiple Etiologies Gastric acid and pepsin secretion are ??? Antral gastritis is present and almost universally associated with H. Pylori Proximal Duodenal mucosal Bicarbonate secretion is frequently (about 70% of the time) impaired Nocturnal acid secretion and duodenal acid load are frequently increased Secretory Abnormalities in Duodenal Ulcers Decreased Duodenal HCO3 Secretion Increased Nocturnal H+ Secretion Increased duodenal Acid Load Increased Daytime Acid Secretion Increased Pentagstrin – stimulated MAO Increased Sensitivity to Gastrin Increase Basal Gastrin Increased Gastric Emptying Decreased Inhibition of Gastrin Release Increased Postprandial Gastrin Release Mean Parietal Cell Number is Increased In DU but not in GU *** At least 2/3 of DU’s and GU’s fall within the normal range *** Even tough duodenal ulcers can be hyper-secretory, they typically are not Maximal Acid Outputs are Greater in DUs Compared with Normals Gastric Ulcer Disease Involves Loss of Mucosal Defenses in the Presence of Acid Gastritis involves the antrum and distal corpus Other contributing factors: NSAIDs, Bile Reflux, Smoking, Alcohol, H. Pylori H. Pylori has High Urease Activity High molecular weight (300-500 kDA) pI (isoelectric point) 5.9 20x more activity than Proteus Vulgaris High affinity for urea (Km = 0.8 mM) Urease reaction is the basis for the diagnostic 14 C/13 C breath tests The presence of ammonia raises local pH H. Pylori Infection Can be Detected by Various Methods --- Testing Methods Endoscopic biopsy tests Sensitivity Specificity Culture 60-90% 100% Histologic examination 95% 98% Rapid Urease Test 90% 95-100% Non-Invasive Tests Serologic (IgG antibodies to H. Pylori) 80-95% 80-95% Urea Breath Test 13 C or 14 C urea ---- CO2 95% 95% A complication of biopsy is perforation and peritonitis. We should first do a blood test for antibodies for H. Pylori that has 80-95% Sensitivity. The urea breath test is another very good test. So, use the less invasive tests for about the same results. Test and re-test to confirm the diagnosis. Genetic Factors Influence Ulcer Incidence Identical Twins = Risk Ratio of about 5x…This is about 5x the normal rate of getting the ulcer First Degree Relative = Risk Ratio of about 3x…The rate is still 3x the normal rate of getting the ulcer DU (duodenal ulcer) and GU (gastric ulcer)cluster independently…You should ask about history of ulcers (peptic and duodenal) in the patient history. If there is family history, suggesting testing and treatment of other family members. Certain Diseases are Associated with an Increased Prevalence of Ulcer Chronic Pulmonary Disease = Risk Ratio of 3-5x..Chronic CO2 retainers and chronically hypoxic Hepatic Cirrhosis = Risk Ratio of 5-8x…this comes from portal hypertension Chronic Renal Failure = Risk Ratio of 1.5-3x …he patient with chronic renal failure maintaining mucosal integrity. A risk of chronic renal failure is ulcer. Cigarette Smoking is Strongly Associated with Ulcer Disease Smokers have: A higher incidence of ulcers More ulcer recurrences More Frequent complications Greater Ulcer – Related Mortality A portion of this effect can be attributed to smoking-induced chronic pulmonary disease Cigarette smoking also decreases pancreatic bicarbonate production There Are a Number of Myths Surrounding the Causes and Treatment of Ulcer Diseases Spicy Foods: The foods are irritants but spices are not ulcerogenic in nature. They can irritate the patient’s symptoms when they do have an ulcer. You don’t have to give the foods up altogether, but you may have to limit them whey symptoms are present. You may also have to watch the foods the spice goes on, because the food and not the spice may be an irritant. Alcohol: Extreme utilization of alcohol may induce the ulcer. Overwhelming of the mucosal tissue by the insult of alcohol can occur. Loss of mucosal tissue with repetitive insults can causes ulceration. Psychological Stress: There is little downside to asking the person to reduce their stress levels….Stress may or may not be part of the generation of the ulcer, but it doesn’t hurt to reduce stress levels (regardless). Ulcer is an executive’s disease: Not true as all types of people can get ulcers A bland diet heals ulcers: Not true The Diagnosis of Ulcer Disease by Symptoms Alone I s Imprecise We can’t predict the ulcer by onset and duration of symptoms. Ulcers occur without symptoms (10-40%) and ulcer symptoms occur without ulcer 30-60% of time. Classic pain presentation is substernal pain on R side, including pain with palpation. Pilot Study of Chiropractic vs. Medical Care *** 11 Adult men and women from 18-34 were studied. ½ the group had adjustment and the other half had medical management (drugs). SMT caused pain relief within 9 days (within 3 days in most subjects) and clinical remission 10 days earlier than the medical group based on endoscope. The endoscope saw better healing in the chiropractic group than the drug group. The drug group still showed signs of ulceration and ulcerative damage.*** BEEZOR *** AP Spine Film *** A mid-late teenager is studied in the film. The mother thought the child had anorexia. The child was thin and appetite diminished over time. The mother tried to listen to the child to see if she vomited after meals. The mother took the child to the chiropractor. The chiropractor shot films and the films show a soft zone of white crossing over the L1-Ll2 vertebral levels. We don’t see the fundal gas vertebra. This is a gas-less stomach. We don’t see the Meganblaz or Splenic Gas Flexure. This is worrisome and requires contrast exam. *** Contrast Exam of Same Patient *** Contrast is pushed to the periphery. Something has to push the contrast to the periphery. Most contrast is on the pyloric side, but doesn’t pool. The chiropractor asks a couple of questions. The patient admits they are losing weight. They are admitting they just aren’t hungry. They do not have anorexia nervosa as they don’t have disordered body image. The girl has long hair down to the buttock. The child runs the hair through the mouth as a nervous habit. As a habit, the child would swallow the hair. The condition is called Trichobeezor. The condition is trapping of substance in the stomach (beezor). Tricho for hair. This is why the child doesn’t have an appetite and also has stomach based problems. Actually, the girl has OCD and needed counseling. A haircut would have helped, but remember she had OCD. The child had manual extraction of the hair under anesthesia. Other beezors are glue or clay which can be swallowed and “stick” to the stomach. The stomach cannot empty itself of soluble products. Typically all the beezors have to be removed usually by endoscopy. GASTRIC CANCERS 1. Metastasis: Should be first thought for cancer. The #1 for metastasis is melanoma (most common for both GU and GI). 2. Benign Primary Cancer: Adnenoma and Lyomyoma are the big 2. They are equally distributed (40% and 41%). Lipoma is a distant 3rd place specific to the stomach (5%). The remaining 14% is spread amongst the remaining primary cancers. a. Adenoma: Growth into the stomach. Cessile adenoma = projection into the lumen…Pedunculated Adenoma or Polyp = Stalk like growth into the area (lumen)…Another key feature is that 40% of adenomas grow to become adenocarcinomas. There are histologically benign at first and later go onto malignancy. b. Lyomyoma: Wall based tumors that infiltrate the walls of the stomach. We see it best by contrast exam. As the tumor infiltrates stomach wall, motor function is compromised. So there is dampening of peristaltic wave. This is wall based infiltrative process that presents like lymphoma. If it is wall based and shows dampening or peristalsis, it should be biopsied to differentiate from lymphoma. If it comes back lyomyoma, it is good news and watchful waiting should be done. When it is removed, it is because it is in a bad location more than any other reason. 3. Primary Malignant = #1 Carcinomas account for 90-95% of aggressive cancers. #2 is Lyomyosarcoma (2%) #3 Lymphoma (Less than 2%). GI carcinomas are on the rise across the US. The #2 cause of death in this country is cancer death. There are countries with rates 30x greater than ours. The higher rates could be due to genetics. The counties are Chile, Japan, and Iceland. These are 3 homogenous genetic groups. These are very costal countries that rely heavily on fish and seafood. Costal pollution goes up and we see a later rise in cancer Products in water and seafood can cause the metaplasia (mercury). Other risks are diet, metal or coal industry workers, firemen, tobacco workers or people who work in smoking areas, nitrites. All of these lead to metaplasia. Grilling meats is another reason for induction of carcinoma as grilling can leave carcinogens on the meat. If we find the condition earlier, we can treat it more successfully. Treatment and Identification 1. Unexplained Weight Loss = 85-95% have weight loss unexplained at the time of diagnosis with gastric cancers. There should not be a good reason to lose weight unexplained (typically about 10 lbs per month or about 3 lbs per weak) 2. Episodes of Dysphagia = It is hard to force food through a tumor lumen (80-90%). 3. Occult Bleeding = 65% have bleeding. 7 mL will show a + Hemoccult test. 4. Anemia = 50% have GI blood loss. No good reason for a patient to be anemic. 5. Pain = 50-70% claim pain. We can’t reliably use pain. _______________________________________________End of Test 3 Material___________________________________