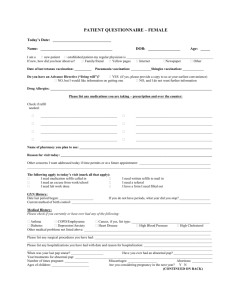
Skin: Rashes, itching, hives, and change in mole.
advertisement

Hawler Medical University
College of Medicine--DEPARTMENT OF INTERNAL MEDICINE-long
Case Sheet No.;
DATE:
/
/
2012
Responsible Specialist:
Department:
Hospital:
…………………….,…….years
old,…………,…………….,…………..…from………………...
Admitted at…………………..Complaining
of………………………..of……………….duration
HPI
Each symptom {site, onset, character, severity, radiation, association,
timing(duration,coars, pattern), exacerbating,& relieving factors}
1
PMH:
Past illnesses:
1-Childhood: Measle, rubella, mumps, whooping cough, chicken pox, rheumatic
fever, polio, scarlet fever, any childhood illnesses.
2-Adult illnesses: D.M ,HTN, IHD, asthma, HIV, TB, stroke, fits, Cancer,
hypercholestrolemia, renal disease, thyroid disease, others.
Past hospitalizations:
History of transfusions:
Drug history:
Immunization history:
Psychiatric history:
History of any allergy:
Past surgical history:
Past obstetric & gynecological history:
Screening tests:
Social history:
-Occupations:
-Marital state:
-Diet:
Alcohol: Unit of alcohol (1U= 10 ml of pure alcohol), (x% proof = x U of alcohol
/litter).
-Tobacco :Pack-year = no. Of pack daily x years of smoking.
-Drug addiction:
2
Family history:
Systemic or general symptom inquiry :
-General health:
State of health, appetite, weight change, fever, chills, night sweats, weakness, fatigue,
sleep, mood.
-Skin: Rashes, itching, hives, and change in mole.
-Eyes: Use of glasses, change in vision, double vision, pain, redness, discharge,
cataract, history of glaucoma.
-Ears: hearing loss, use of hearing aid, discharge, pain, tinnitus.
-Breast: lumps, discharge, pain, self-examination.
-CVS: Chest pain on exertion, Orthopnia, PND, Palpitation, Claudication, Ankle
swelling.
-Vascular: Intermittent claudication, leg cramps, varicose veins, and Raynauds
phenomina leg swelling, ulcers, thrombophlebites.
-Respiratory system: SOB (exercise tolerance), cough, wheeze, sputum production
(color, amount), hemoptysis, chest pain due to inspiration or coughing.
GIT: dysphagia, odynophagia, nausea and vomiting, jaundice, haematemesis,
indigestion, heart burn, abdominal pain, diarrhoea, constipation, change in color of
stools, maelena, rectal bleeding, hemorrhoid.
Genitourinary system :frequency, dysuria, urgency, nocturia, haematuria, hesitancy,
Sexual partners, un protected intercourse, incontinence, urethral discharge, terminal
dribbling, libido, stream of flow, erectile difficulties.
CNS: headache, dizziness (vertigo or light headed), faints, fits, numbness, or tingling,
weakness, visual disturbance, deafness, tinnitus, tremor, nervousness, speech
disorders, hallucinations, gait disorders, loss of memory, anosmia.
Musculoskeletal: joint pain, joint stiffness, joint swelling, mobility, falls.
Endocrine: Heat or cold intolerance, Change in sweating, polydipsia, polyurea, ploy
phagia, heat intolerance, prominence of eyes, swelling in eyes.
3
Blood: Anemia, epistaxis, gum bleeding, easy bruising, purpura, and relation of
symptoms to green vegetable consumption, glandular enlargement.
GENERAL EXAMINATION
A …………. aged thin patient lying on bed comfortably, looks ill (healthy,
depressed), not in respiratory distress, awake, fully conscious, alert, well oriented,
not.confused, attentive, plethoric (Pale), no jaundice, well hydrated, with no
abnormal movement, well dressed, preserved insight, with appropriate affect, no
specific odour, no abnormal sounds, normal speech, depressed mood.
Normal skin temperature and texture, no abnormal skin pigmentation or any skin
lesion.
THE HANDS
Normal hand gripe, hands are normal size, shape, no, muscle wasting, normal power
& tone, normal temperature not sweaty, no palmer erythema or dupuytrens
contracture.
No clubbing, splinter haemorrhage, onycolysis, or nail pitting, no joint deformity, or
any swelling, with no specific abnormal posture, no abnormal movement, normal
temperature.
THE HEAD: The cranium of normal size, with normal hair texture and distribution.
Face: face is symetric, no xanthelasma or facial rash, no waisting of masseter
muscles, no any skin lesion or abnormal movement.
The eyes: Normal VA, no periorbital edema, exopthalmous, enopthalmous, jaundice,
red eyes, ptosis or corneal arcus, normal equal sized pupils which reacting to light,
normal eye movement, no nystagmus or strabismus, no conjuctival or corneal lesion,
normal palpebral fisher width, normal fundoscopy.
THE NOSE: Nose of normal size, shape, and no septal deviation.
Lips: No any ulcer, crackles, eruptions or angio-oedema of lips.
Tongue: Tongue of normal size, shape, color, no waisting, deviation or any lesion.
Gum :No gum hypertrophy, bleeding, or any oral ulcers, normal bilateral palatal
movemennt, preserved gag reflex
THE NECK:
In neck there is no visible (asymmetry, scar, mass, or pulsation.
JVP not elevated trachea central, no thyroid or LN enlargment, and no neck rigidity.
No any bruits or thrill.
BREAST: The breasts on examination were normal size, shape & symmetry, no any
mass or axially LN detected.
No axially LAP
VITAL SIGNS
BP:
PR: Rate, Rhythm, Volume, Character, Consistency.
Respiration: Rate, Rhythm, and Consistency.
4
Temperature: Oral, Axially, and Anal.
Chest examination:
Symmetrical
chest
movement
with
respiration,
respiration
mainly
thorachoabdominal, hyper inflated chest with increased AP diameter, there is
sternoclavicular muscle contraction with abnormal retraction of supraclavicular &
intercostal spaces during inspiration, no tracheal tag.
There is no visible skin lesion, dilated veins, scar of any operation, pulsation,
gynecomastia or any swelling, with normal hair distribution.
Trachea central, apex beat not displaced normal Chest expansion & tactile vocal
fremitus, no any tenderness, or swelling.
Normal percussion notes.
Normal vesicular breath sound, no abnormal breath sound or added sounds, with
normal expiratory flow time.
Pericardial examination
Visible apical impulse at 5th intercostal space at mid clavicular line, no any scar, skin
lesion or any abnormal pulsation.
Taping apex beat; cardiac dullness starts at 4th intercostal space.
Normal S1, S2, no added sounds or there is a high pitched ejection systolic at right
second intercostal space radiates to neck, increased or decrease with expiration,
inspiration, standing or squatting.
No pericardial friction rub.
Normal peripheral arterial examination disease.
Peripheral arterial disease
Peripheral arteries are detected symmetrically bilaterally with normal rate, rhythm,
and volume & character no any sign of decreased arterial perfusion or ischemia in
any limb.
No radiofemoral delay or any arterial bruit or murmur.
Abdominal examination
Distended abdomen which moves with respiration, inverted umbilicus, no any visible
skin lesion like scar, pigmentation or striae, or any prominent superficial veins or
Pulsation’s.
On light & deep palpation there is no any tenderness, rigidity, hyperasthesia,
splashing, mass, or organoomegaly.
Normal percussion notes, negative shifting dullness & fluid thrill, liver span was 14
cm
Normal bowel sound, no spleenic & liver friction rub, no bruits or venous hum above
the umbilicus.
Normal hernil orifices, no inguinal gland enlargment, abdominal reflex are present;
examination of genitalia is normal.
Shall I do rectal or gynecological examination?
At the end of examination look at the back of the patient for any swelling, site of
renal biopsy.
5
Lowe limb examination
Legs are symetric, no swelling edema, waisting, fasciculation, abnormal movement,
or any skin lesion, normal hair distribution, no joint swelling, normal peripheral
pulses.
CNS
Cranial nerves are intact
Meningeal signs are negative.
No muscle wasting, fasciculation, abnormal movements, or any tenderness.
Normal tone & power in both upper and lower limbs.
Normal reflexes in both upper and lower limbs.
Cerebellar function like finger nose test, rapid alternating movement, heel-shin test,
heel toe test of gait are normal.
Examination of the sensory system.
The sensory system: (Light touch, Superficial pain, Deep pain, Temperature, Joint
position sense, Vibration sense, Two-point discrimination) is normal.
Normal cortical function: (point localization, stereognosis, graphethesia, sensory
inattention, calculation skills, constructional apaxia, dressing apraxia).
Absent primitive reflexes (Pout reflexes, Grasp reflexes).
INVESTIGATIONS:
RFT,BS,CBC,GUE,GSE,LFT,ELECTROLYT,,,,,,,,,,,,,,,,,,,,,,,,,,,,,
XRAY;
ECG;
ECHO;
CT MRI
BM
OTHERS:
IMPORTANT RESULTS:
FOLLOWUP INVESTIGATIONS;
6
DIAGNOSIS&DDX;
TREATMENT:
-
NOTE;
SUPERVISER NOTE:
DATE:
/
PRESENTED:
/
2012
YES:
NO;
NOTE:
SUPERVISER NAME &SIGNATURE(STAMP AMUST)
7