DOC
advertisement

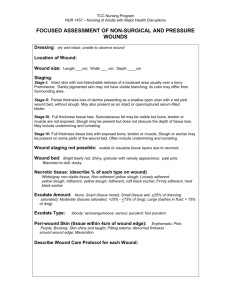
Case Review for Learning Wound Documentation AB is a 75 yo female in “previous good health” when she presented to the hospital with a Right Hip fracture. She was found after being on her bathroom floor for over 24 hours. Upon admission to the hospital, it turns out she had not seen a physician in over ten years and was now diagnosed with DM, renal insufficiency exacerbated by being dehydrated for 24 hours. In addition, she was also found to have CHF. After her hip surgery, she is respiratory failure and required an ICU stay on vent for over 10 days. Every time the nurses attempted to turn her or lay her head down flat, she would desaturate and almost code. She also has been on antibiotics for secondary pneumonia and has developed C. Diff colitis, which is resolving, but still with very watery stools. After this prolonged hospital stay of 4 ½ weeks and losing over 40 lbs, she is finally off the vent and was felt to be ready for discharge to a SNF. The “golden rod” transfer form states that she has a stage II sacral ulcer. She gets transferred to you SNF and on rounds you find this: Wound measurements: Sacral opening 12 cm W 10 cm L 3 cm D Visible fascia, but no exposed bone Part of base is covered with slough Wound edges are somewhat firm Drainage is somewhat purulent, but no foul smell Wound is debrided and there is some drainage coming from the tissues and now you see bone This is obviously a very complex case that has many potentials way to describe the wound. We will focus on the main wound area. Here are the basics: Pain – 0 = none; 10 = worse – Pain is widely considered the 5th vital sign. Assigning pain to a wound can be difficult. It is important to distinguish pain from a dressing change to the actual pain of the wound. In this case there are several possible sources of pain: possible bone infection, excoriation of surrounding tissue resulting in partial thickness tissue loss and thus exposed nerves, chemical excoriation from incontinence of urine and/or stool ( combination of which is very caustic). The one thing pain is NOT due to is necrotic tissue. Dead tissue it just that-> dead. It has no sensation. So if someone has pain, it is important to look for the sources and then document the pain the individual is experiencing. AB says her pain is a 4 – probably due to excoriated open surrounding tissue and from lying in bed for almost a month. Infection – Basic definition – Multiplication and invasion of microorganisms into the body tissue. It is not the same as contamination, where we have bacteria all over our body, but that does not mean infection. Every wound is contaminated, but not every wound is infected. 0= no s/s – most wounds will fall into this category. The reddened areas you see are from excoriation, may be tape abrasions, so the reddened areas do not mean infection 1= s/s local - She has some pain, there is necrotic tissue and you see fascia. But even though we said the redness itself was not a sign of infection, on exam that tissue is boggy and indurated and there is some purulent drainage, though not foul smelling. But you debrided and now you have bone. She needs a culture. 2= s/s systemic – She has no fever, vital signs are stable, she is not confused or obtunded and diaphoretic. She does not have obvious systemic signs of infection, especially since she finished a long course of antibiotics, but the nurses need to watch for this. 3= C&S - I would assign her this number. You have exposed bone. You have some drainage that appears to be coming from the tissue itself. This is very suspicious for infection and thus culturing the wound is indicated. However, it is important to get a tissue culture or even a bone biopsy. Doing a swab culture is inaccurate because you need to know what bacteria are in the tissue, not on top of it and they are not always the same. 4= documented infection – sometimes patients will come with documented infection, but they should be on antibiotics already. 5= on ATB – If someone is on antibiotics for some other reason, it is important to document that they are on something, which could interfere with the culture results. So what if she is on antibiotics and you do a culture – Always choose the higher number. But also, be consistent in choosing the number you want to represent the documentation. Undermining – Wounds, especially pressure ulcers, start at the deeper tissues and work their way out to the skin. In addition, the damage that is done is not straight line. It follows the curve of the bone and therefore, the skin level damage is often considered the “tip of the iceberg.” In addition, no one with a pressure ulcer is strictly only pressure related. There is often a shearing component. For instance, if someone is always sitting up in bed or in a chair, the tissue is often being stretched, which also means blood vessels are being stretched and compromised. That is why you will often find a wound with an extensive undermined or tunnel that extends “up” the spine because the tissue is being stretched and compromised in the direction. When you measure undermining, use 12, 3, 6 and 9 o’clock points. AB has 4.5 cm undermining at 3 and 9 o’clock, 1 cm at 6 o’clock, but 5 cm at 12 o’clock. So you would assign her as a 4= > 4cm for >50% circumference. She may heal this wound where because the bone is exposed and often the last area to granulate, it heal down to a narrow opening. This would now be 5= tunneling. Exudate type 1= none – This usually means the wound is dry and thus you should hydrate the wound, unless it is dry eschar on a heel, which you would leave as dry and intact. 2= serosanguinous,thin, pale pink – This usually means the wound is clean, fully granulating, but there is still drainage. Because granulation tissue can bleed easily, you will get a mix of blood and serous drainage, which make the drainage look link. The point is that it is clear and there is no cloudiness or purulent nature to the drainage. 3= thin clear – This could be from a clean granulating wound with no bleeding or could be from an open blister. 4= purulent, yellow, tan/green, no odor – AB has this described above. It could be from the necrotic tissue that is dissolving, fat necrosis, from the dressing materials. If there is some odor, do not confuse this with infection. Clean the wound and if there is no odor, then document it as 4. 5= purulent, foul, thick opaq, w/odor – the wound is infected and you are describing pus. Odor is unmistakable for infection. Exudate amount – This is why it is important to look at the old dressing. Ask how long the dressing has been in place. How often are the nurses changing the dressing due to drainage? Also, the amount of drainage can help you choose the right choice of dressings 1= none – wound is dry. If you want to hydrate, then try hydrogel and hydrocolloid, change 3x/wk + prn 2= scant – can continue to use hydrogel, but the wound will be stimulated and should increase in drainage. May want to try moistened alginate to provide some hydration, but absorb some, cover with hydrocolloid, change 3x/wk + prn 3= small – alginate and hydrocolloid 4= moderate – go to more absorbent dressings like alginate and foam, change 3x/wk + prn 5= AB has a large amount of drainage because the wound is large, there is a lot of undermining, which means more surface area to drain from. But also, she has lost 40 lbs, most of which is lean body mass. She is going to still in catabolic phase and most likely will have a low albumin. Low ALB means low oncotic pressure to keep fluids in the vascular space and thus there will be a lot of leakage of fluid into the tissues and thus drainage. We will talk about NPWT (Negative Pressure Wound Therapy) later on. For now, you may have to go a daily dressing change with alginate/ABD daily or Mesalt daily as long as you do not have exposed bone(AB has it so don’t use Mesalt here). Once the wound is clean and you have either ruled out or started to treat osteomyelitis, then you can consider NPWT. Granulation Tissue – This is an indication that you have healing going on. It has the classic granular appearance with “buds” of healthy appearing tissue that helps to fill the wound and then allow epithelialization to occur. 1= skin intact – wound is closed OR is intact blister 2= beefy red 75-100% – just as says. Healthy, clean looking tissue with buds granulation over most of the wound surface. 3= beefy red 25 – 75% - little more than half about still not complete yet. We estimate the amount becaue no two people will estimate the same amount 4= pink dull <25% - granulation just starting. Not much present, but it is starting to form. AB has about 25 present of some granulation starting to form, but some of this could be exposed muscle. But it is not beefy red so assigning a 4 is reasonable. 5= none – This could mean a wound that is completely necrotic OR a wound that was just debrided and is clean, but there is no granulation. Epithelialization – How much do you think the wound has healed? This is sometimes hard to tell since you may be seeing the wound in the middle of its existence. But often you can see new skin that has developed on the edges of the wound. It is usually lighter in color than the normal skin tone. For AB, it is still in the process of “declaring itself”, which means there is still more debridement and cleaning up of the wound that needs to be done. For AB, this a 5= none. No epithelialization has occurred yet. Necrotic Tissue and Amount - Dead tissue can be either eschar =dry necrotic tissue, or slough=dissolving necrotic tissue. Again, estimate on the high side when trying to determine the amount present. If you have a mixture of dry and dissolving necrotic tissue, choose the higher number and estimate the necrotic tissue based upon the total amount of necrotic tissue. 0=none 1=crust – use for dry blister or scab 2=yellow slough, easy separated – very loose, dissolving slough that can come off with sharp debridement with a suture removal kit 3= loose adherent yellow slough – necrotic tissue still somewhat intact, but in the process of dissolving 4= adherent soft, black eschar – in between level of where dry necrotic tissue is starting to soften. As it dissolves or is removed, the slough is usually lighter in color (brown, tan, yellow) 5= firmly adherent, hard black eschar – I use this for dry, hard intact eschar anywhere on the body,but for the dry intact eschar on the heel. Some would choose 1=crust. Be consistent in how you describe dry eschar on heels. For AB, there is 25% adherent soft eschar, not necessarily black, but eschar that is dissolving. Also, there is about 50% loose adherent yellow slough. There is about 25% some granulation tissue that is trying to form. So she would be assigned 4=adherent soft black eschar and 4= 50 -75% necrotic amount. Wound Edges The basic guide to this section is 1= nonvisible 2= distinct outline attached 3=Not attached 4=Rolled under, thickness 5=Fibrotic, scarred = = = = = unable to clearly distinguish wound outline even or flush with wound base, no sides or walls present; flat sides or walls are present; floor or base of wound is deeper than edge soft to firm and flexible to touch hard, rigid to touch, chronic scar tissue So for AB, the edges are not attached. There is undermining, thus “walls” and there is definitely depth. So oyu would assign this section as a 3. Color - This pertains to the surrounding skin and tissue around the wound OR if the area is not open, i.e. bruise, potential Deep Tissue injury. It will tell you if there is more damage either around the wound or the area that could open. 1= normal ethic 2=red, blanches – related to inflammation. You push on the area and it will blanch 3= white, gray pallor – Tissue is damaged from maceration, or is ischemic looking. It is not healthy and potentially will breakdown further 4= Dark Red, nonblanchable – this is like a bruised area. It is darker in color and pushing on it will not result in blanching. 5=black, hyperpigmented – this is tissue that is dying. It represents deep tissue injury (DTI) For AB, there is surrounding tissue that is damaged from excoriation and tape burns. I would call it a 2 because since it related to inflammation and does blanch. Edema- This is a sign of either fluid overload or low protein state such that fluid cannot stay in the vascular space and leaks into the interstitial tissues. Nonpitting edema is skin that is shiny and taut. Pitting edema is when you press your finger down into the tissue and wait 5 seconds. On release of pressure, tissue fails to resume previous position and an indentation appears. Crepitus can be an ominous sign and requires immediate attention. It is the accumulation of air or gas in tissue, i.e. gas gangrene. 1= none – AB really does not have edema present 2= nonpitting edema < 4cm from edge of wound 3= nonpitting edema > 4 cm from edge of wound 4= pitting edema < 4 cm from edge 5= pitting > 4 cm, crepitus present Induration - The definition of induration is very simply the hardening of a normally soft tissue or organ, especially the skin, because of inflammation, infiltration of a neoplasm, or an accumulation of blood. We see this especially when inflammation creates a lot of swelling within the tissue and causes it to be hard and firm. This is also seen with infection. In fact, even after an abscess is opened and drained, the induration may linger for many days. 0= none 1=minimal – slight firmness of the surrounding tissue 2= < 2 cm – firmness is present but less than 2 cm from wound edge 3= 2 – 4 cm < 50% - firmness present beyond 2 cm less than 4 cm and involves less than 50% of the circumference of the wound 4= 2 -4 cm >50% - as above , but more than 50% of circumference 5= 4 cm any area – self explanatory AB has some inflammation with slight firmness, which is seen with almost every wound. So AB would be assigned a 1 for this section. Follow up Visit After several weeks of managing the wound, it has made great progress. Wound measurements: Sacral wound 10 cm W 8 cm L 1.5 cm D Though the wound was debrided , bone that was exposed is now covered with granulation tissue with only slight amt visible fascia. Drainage is serosanguinous with no foul smell Surrounding excoriation resolved No further complaint of pain and off ABX How would you document the wound now? Look at the documentation and complete it below with any comments you want to make. Pain ______ Infection ______ Undermining ______ Exudate Type ______ Exudate Amount ______ Granulation ______ Epithelialization ______ Necrotic Tissue ______ Necrotic Tissue Amount ______ Wound Edges ______ Color ______ Edema ______ Induration ______