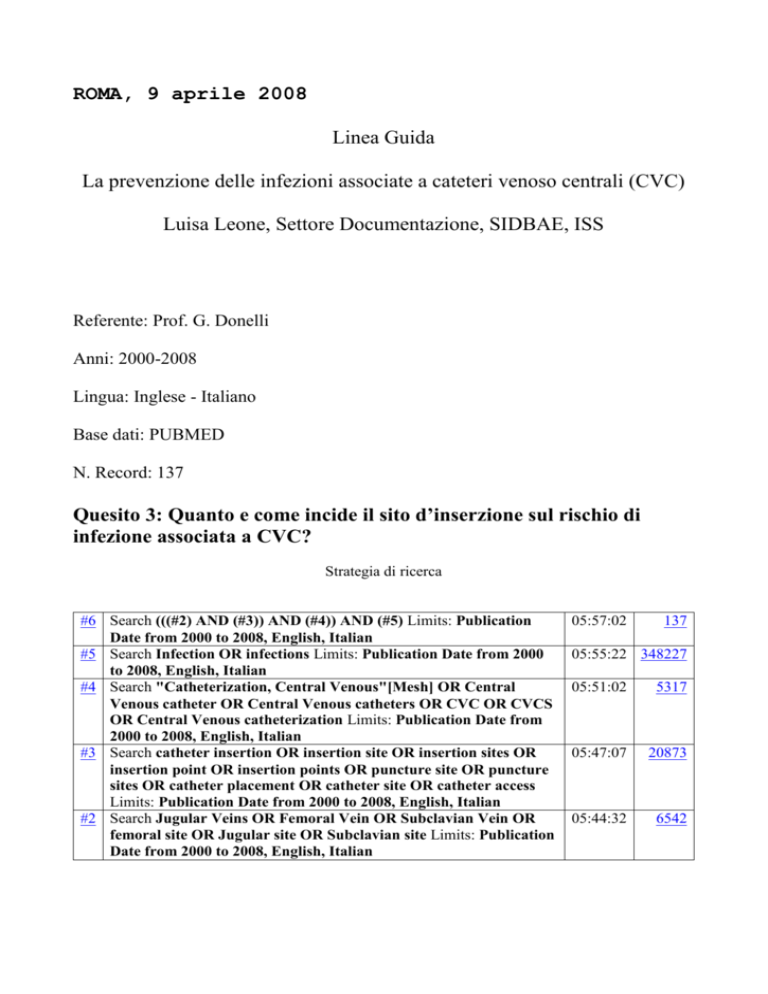
ROMA, 9 aprile 2008
Linea Guida
La prevenzione delle infezioni associate a cateteri venoso centrali (CVC)
Luisa Leone, Settore Documentazione, SIDBAE, ISS
Referente: Prof. G. Donelli
Anni: 2000-2008
Lingua: Inglese - Italiano
Base dati: PUBMED
N. Record: 137
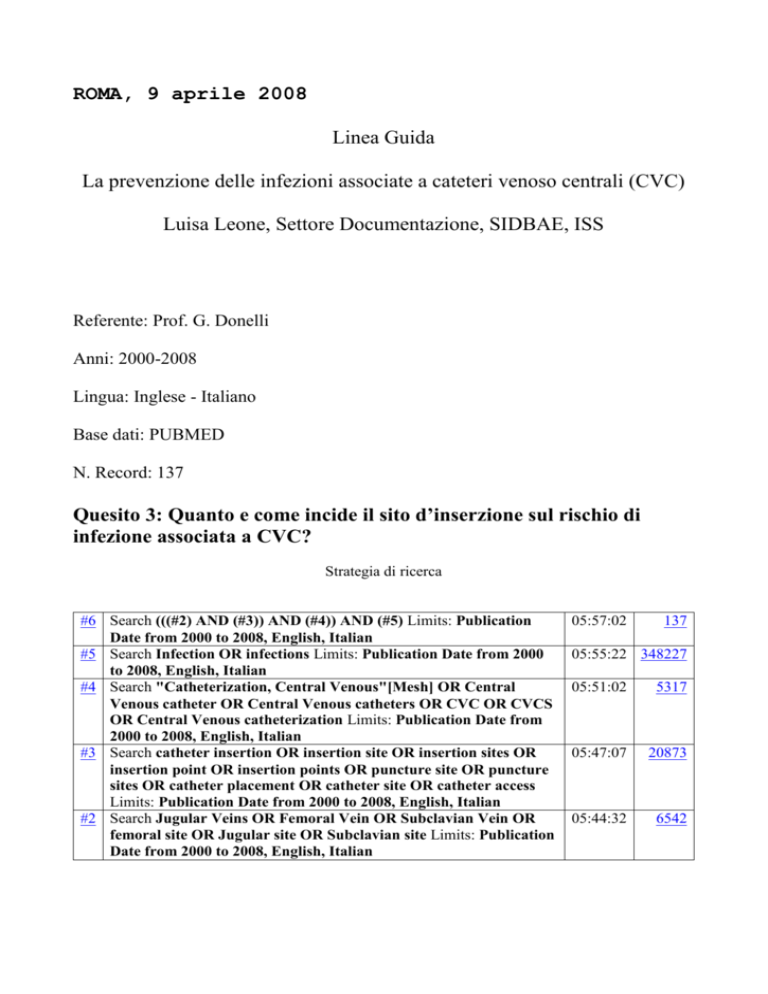
Quesito 3: Quanto e come incide il sito d’inserzione sul rischio di
infezione associata a CVC?
Strategia di ricerca
#6 Search (((#2) AND (#3)) AND (#4)) AND (#5) Limits: Publication
Date from 2000 to 2008, English, Italian
#5 Search Infection OR infections Limits: Publication Date from 2000
to 2008, English, Italian
#4 Search "Catheterization, Central Venous"[Mesh] OR Central
Venous catheter OR Central Venous catheters OR CVC OR CVCS
OR Central Venous catheterization Limits: Publication Date from
2000 to 2008, English, Italian
#3 Search catheter insertion OR insertion site OR insertion sites OR
insertion point OR insertion points OR puncture site OR puncture
sites OR catheter placement OR catheter site OR catheter access
Limits: Publication Date from 2000 to 2008, English, Italian
#2 Search Jugular Veins OR Femoral Vein OR Subclavian Vein OR
femoral site OR Jugular site OR Subclavian site Limits: Publication
Date from 2000 to 2008, English, Italian
05:57:02
137
05:55:22 348227
05:51:02
5317
05:47:07
20873
05:44:32
6542
1: Vojnosanit Pregl. 2008 Jan;65(1):21-6.
Central venous catheters in hemodialysis: to accept recommendations or to stick
to own experience.
Stolić R, Trajković G, Perić V, Jovanović A, Stolić D, Sovtić S, Lazarević T,
Zivić Z, Subarić-Gorgieva G.
School of Medicine, Pristina/Kosovska Mitrovica, Kragujevac, Serbia.
radsto@ptt.yu
BACKGROUND/AIM: Hemodialysis catheter, as an integral part of hemodialysis, is a
catheter placed into the jugular, subclav ian and femoral vein. The most common
catheter-related complications are infections and thrombosis. The aim of the
study was to analyze the prevalence of complications associated with differently
inserted central-vein catheters for hemodialysis. METHODS: The study was
organized as a prospective examination during the period from December 2003 to No
vember 2006, and included all patients who needed an active depuration by
hemodialysis, hospitalized at the Clinical Center Kragujevac. The subject of the
study were 464 central-vein catheters inserted during the mentioned period and
there were recorded all complications related to the placement and usage of
catheters. RESULTS: The largest percent of inserted catheters was into the
femoral vein--403 (86.8%), significantly less into the jugular vein--42 (9.2%),
while into the subclavian vein there were placed only 19 catheters (4%). The
average of femoral catheter functioning was 17 catheter days, in jugular
catheters it was 17.3 days while the subclavian catheters had an average rate of
functioning of 25.9 catheter days; there was found a statistically significant
difference re garding the duration of functioning (p = 0.03). By microbe
colonization of smear culture of the skin at the catheter in sertion site, in
clinically present suspicion of catheter infection, there was obtained a positive
finding in 5.5% of catheters placed into the femoral vein and 7.1% of catheters
instilled into the jugular vein, of which Staphylococcus aureus was the most
important bacterial type, without statistically significant difference (p =
0.51). Haemoculture, done when there was a suspicion of bacteriemia, was positive
in 3.7% of the patients with femoral and 4.8% with jugular catheters;
Staphylococcus aureus was the most common bacteria type, but there was no
statistically significant difference (p = 0.65). Colonizing the smears of the cut
catheter tops, there was found a positive finding in 8.9% of femoral and 4.7% of
jugular catheters in which the mentioned type of staphylococcal bacteria was
prevalent, without statistically significant difference (p = 0.82). In 77% of
femoral, 71.4% of jugular and 68.4% of subclavian catheters, there were no
complications associated with insertion and manipulation of catheters for
hemodialysis and the difference was at the limits of statistical significance (p
= 0.06). CONCLUSION: Unconvincing rate of infections and a smaller percent of
serious complications associated with the placement and use of central vein
catheters instilled into the femoral vein, indicate that personal experience is
sufficient recommendation to convince us that femoral vein does not represent a
region with an increased risk for insertion of hemodialysis catheters.
PMID: 18368934 [PubMed - in process]
2: J Adv Nurs. 2008 Apr;62(1):3-21.
Catheter-related bloodstream infections in intensive care units: a systematic
review with meta-analysis.
Ramritu P, Halton K, Cook D, Whitby M, Graves N.
The Centre for Healthcare Related Infection Surveillance & Prevention, Princess
Alexandra Hospital, Brisbane, Qld, Australia.
AIM: This paper is a report of a systematic review and meta-analysis of
strategies, other than antimicrobial coated catheters, hypothesized to reduce
risk of catheter-related bloodstream infections and catheter colonization in the
intensive care unit setting. BACKGROUND: Catheter-related bloodstream infections
occur at a rate of 5 per 1000 catheter days in the intensive care unit setting
and cause substantial mortality and excess cost. Reducing risk of
catheter-related bloodstream infections among intensive care unit patients will
save costs, reduce length of stay, and improve outcomes. METHODS: A systematic
review of studies published between January 1985 and February 2007 was carried
out using the keywords 'catheterization - central venous' with combinations of
infection*, prevention* and bloodstream*. All included studies were screened by
two reviewers, a validated data extraction instrument was used and data
collection was completed by two blinded independent reviewers. Risk ratios for
catheter-related bloodstream infections and catheter colonization were estimated
with 95% confidence intervals for each study. Results from studies of similar
interventions were pooled using meta-analyses. RESULTS: Twenty-three studies were
included in the review. The strategies that reduced catheter colonization
included insertion of central venous catheters in the subclavian vein rather than
other sites, use of alternate skin disinfection solutions before catheter
insertion and use of Vitacuff in combination with polymyxin, neomycin and
bacitracin ointment. Strategies to reduce catheter-related bloodstream infection
included staff education multifaceted infection control programmes and
performance feedback. CONCLUSION: A range of interventions may reduce risks of
catheter-related bloodstream infection, in addition to antimicrobial catheters.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 18352960 [PubMed - in process]
3: Intensive Care Med. 2008 Mar 4 [Epub ahead of print]
Influence of insertion site on central venous catheter colonization and
bloodstream infection rates.
Gowardman JR, Robertson IK, Parkes S, Rickard CM.
Department of Intensive Care Medicine, Level 3, Ned Hanlon Building, Royal
Brisbane and Woman’s Hospital, Herston, 4029, Brisbane, QLD, Australia,
john_gowardman@health.qld.gov.au.
OBJECTIVE: To compare colonization and catheter-related bloodstream infection
(CR-BSI) rates among three insertion sites (subclavian, internal jugular,
femoral) used for central venous catheter (CVC) placement. DESIGN:
Twenty-four-month prospective study, with relative effects analyzed by Cox
proportional hazards regression. SETTING: Eight-bed intensive care unit.
PATIENTS: Four hundred and ten critically ill patients requiring CVC placement.
MEASUREMENTS AND RESULTS: All short-term multi-lumen CVCs, including
antimicrobial-coated devices, were studied with management standardized. Six
hundred and five CVCs (4,040 catheter days) were analyzed. Colonization and
CR-BSI incidence were, respectively, 15.1 (95% CI 13.5-21.0) and 1.8 (95% CI
1.2-4.2) per 1,000 catheter-days. Colonization was higher at the internal jugular
(HR 3.64; 95% CI 1.32-10.00; p[Symbol: see text]=[Symbol: see text]0.01) and
femoral (HR 5.15; 95% CI 1.82-14.51; p[Symbol: see text]=[Symbol: see text]0.004)
sites than at the subclavian site. The femoral site carried a greater risk of
being colonized by non-S. epidermidis species than the subclavian and internal
jugular sites combined (HR 4.15; 95% CI 1.79-9.61; p[Symbol: see text]=[Symbol:
see text]0.001). CVCs inserted in the Department of Emergency Medicine were more
colonized than those inserted in the ICU or operating room (HR 2.66; 95% CI
1.27-5.56; p[Symbol: see text]=[Symbol: see text]0.01), and CVCs were less
colonized in females than in males (HR 0.49; 95% CI 0.26-0.89; p[Symbol: see
text]=[Symbol: see text]0.02). No difference in CR-BSI rates was noted between
the three sites. CONCLUSIONS: Colonization was lowest at the subclavian site.
Regional differences exist with respect to type of pathogen isolated.
Colonization was influenced by insertion location and gender. The incidence of
CR-BSI was not different.
PMID: 18317732 [PubMed - as supplied by publisher]
4: Semin Dial. 2008 Jan-Feb;21(1):97-9.
New tunneled hemodialysis catheter placement through the old exit site.
Atray N, Asif A.
Interventional Nephrology, Capital Nephrology Medical Group, Sacramento,
California, USA.
Accidental loss of tunneled hemodialysis catheters has been observed in chronic
hemodialysis patients. Although a new catheter could be inserted using a fresh
site, catheter insertion can also be accomplished by utilizing the existing exit
site. In this analysis, we report 10 cases of an extruded tunneled hemodialysis
catheter. The catheters had been in place for 2-6 months. The time elapsed after
catheter extrusion ranged from 6 to 72 hours. None of the patients demonstrated
any evidence of exit site or tunnel infection. Patient age ranged from 45 to 77
years. Diabetes mellitus was the cause of renal failure in 40% of the cases.
Catheter insertion was accomplished by inserting a guidewire into the exit site
and navigating it through the tunnel to the central venous system and into the
right atrium. A diagnostic catheter was then navigated over the wire and contrast
study performed to confirm the position. The wire was reinserted and a new
tunneled hemodialysis catheter fed over the wire and into the atrium. Nine
catheters were successfully placed using this technique. One patient had nausea
and hiccups upon wire insertion into the atrium. There were no hemodynamic
consequences. The wire was removed and a new catheter inserted on the other side
using the left internal jugular vein. All of the catheters inserted using this
technique functioned appropriately. There were no exit site or tunnel infections
for up to 4 weeks' follow-up. We conclude that patients with catheter extrusion
can receive a new catheter through the existing exit site, tunnel, and venotomy.
PMID: 18251964 [PubMed - indexed for MEDLINE]
5: J Perinatol. 2008 Apr;28(4):282-6. Epub 2008 Jan 17.
Peripheral insertion of double-lumen central venous catheter using the Seldinger
technique in newborns.
Bueno TM, Diz AI, Cervera PQ, Pérez-Rodríguez J, Quero J.
1Neonatal Unit, La Paz Children's Hospital, Madrid, Spain.
Objective:To report the experience of peripheral insertion of double-lumen
central catheters (PIDLCC) in preterm and term newborn infants and to analyze the
technical characteristics of the procedure and any observed complications.Study
Design:Retrospective review of 61 newborns that had a PIDLCC between 2003 and
2006. The study comprised clinical data analysis, anthropometrics, indications,
duration, complications and reasons for withdrawal of the catheters.Result:Weight
of the patients was <1 kg in 10%, and >2 kg in 75%. Catheters tip placement was
as aimed, mostly superior cava vein (SCV), in 65.5%, and subclavian vein in
remaining 34.5% and average duration of catheterization was 13.5+/-9.6 and
8.9+/-5.8 days, respectively. Blood sampling through both lumens was possible
especially when the tip was at SCV. Reasons for catheter withdrawal were end of
indication (45.9%), phlebitis/edema (21.3%), suspected infection (3.2%),
accidental withdrawal (3.2%) and rupture of proximal end (3.2%). In three (4.9%)
patients, withdrawal was due to serious complications (two cases of pleural
leakage of infusion fluid and one breakage of the metallic guide). About 16.3% of
the patients died with the catheter still in situ. Infection findings were
positive tip culture (14.7%) and catheter-related sepsis
(3.2%).Conclusion:Insertion of PIDLCC is possible in neonates. The incidence of
complications, mostly mechanical, requires careful evaluation of indications, and
strict adherence to the procedure of insertion and manipulation.Journal of
Perinatology (2008) 28, 282-286; doi:10.1038/sj.jp.7211923; published online 17
January 2008.
PMID: 18200023 [PubMed - in process]
6: J Invest Surg. 2008 Jan-Feb;21(1):9-14.
Usefulness of Groshong catheters for central venous access via the external
jugular vein.
Ishizuka M, Nagata H, Takagi K, Horie T, Sawada T, Kubota K.
Department of Gastroenterological Surgery, Dokkyo Medical University, 880
Kitakobayashi, Mibu, Tochigi, Japan. mm-ishizuka@umin.ac.jp
This study was designed to evaluate the usefulness of central venous access via
the external jugular vein (EJV) employing Groshong catheters, and to compare the
complications with those of conventional internal jugular venous catheterization.
Central venous access was achieved by insertion of a single-lumen 4.0 Fr Groshong
catheter via the EJV or internal jugular vein (IJV) with a single puncture.
Complications associated with insertion and central venous catheter-related
bloodstream infection (CVC-RBSI) were evaluated from the database. Two hundred
and twenty-five patients received 400 catheters for a total period of 5377
catheter-days. Ninety-six patients underwent 201 internal jugular venous catheter
(IJV-C) procedures for 2381 catheter-days, and 129 patients underwent 199
external jugular venous catheter (EJV-C) procedures for 2996 catheter-days. Use
of EJV-C was associated with a longer catheter insertion length (p < .01) and
period (p < .01), a larger number of operations (p < .01), and more frequent use
of total parenteral nutrition (TPN) (p < .01) and less frequent use of
chemotherapy (p < .01) than for IJV-C. However, there were no significant
differences (NS) in complications associated with insertion and CVC-RBSI between
IJV-C and EJV-C. There were no significant differences such complications as
malposition, oozing or hematoma formation of insertion site, arterial bleeding,
nerve damage, pneumothorax, and phlebitis between IJV-C and EJV-C. Moreover,
EJV-C was not associated with morbidities such as pneumothorax, arterial
bleeding, and nerve damage. Thus the study concluded that EJV-C using Groshong
catheters has no severe complications and has the same rates of CVC-RBSI as
conventional IJV-C for central venous access.
PMID: 18197529 [PubMed - in process]
7: Crit Care Med. 2007 Dec 12 [Epub ahead of print]
Prospective study of peripheral arterial catheter infection and comparison with
concurrently sited central venous catheters*
Koh DB, Gowardman JR, Rickard CM, Robertson IK, Brown A.
Registered Critical Care Nurse, Launceston General Hospital, Tasmania, Australia
(DBCK); Senior Specialist, Intensive Care Medicine, Royal Brisbane and Women’s
Hospital, Herston, Senior Lecturer, University of Queensland, Queensland,
Australia (JRG); Professor of Nursing, Griffith University, Research Centre for
Clinical and Community Practice Innovation, Queensland, Australia (CMR); Senior
Research Fellow, School of Human Life Sciences, University of Tasmania,
Launceston TAS, Australia (IKR); Nurse Educator, Intensive/Coronary Care Unit,
Launceston General Hospital, Launceston TAS, Australia (AB).
OBJECTIVE:: Peripheral arterial catheters are perceived as having low infective
potential compared with other catheters and may be overlooked as a cause of
catheter-related bloodstream infection. We aimed to measure colonization and
rates of catheter-related bloodstream infection in arterial catheters, to
investigate risk factors for arterial catheter colonization, and to compare
arterial catheter infection rates with those in concurrently sited and managed
central venous catheters. DESIGN:: Prospective 24-month cohort study. SETTING::
Eight-bed combined general intensive care and high-dependency unit of a 350-bed
Australian teaching hospital. PATIENTS:: Three hundred twenty-one arterial
catheters in 252 adult and pediatric patients were observed for 1,082 catheter
days, and 618 central venous catheters in 410 patients were observed for 4,040
catheter days. All catheters were inserted in, or presented to, the intensive
care unit. Both arterial catheters and central venous catheters were inserted by
trained personnel under aseptic conditions, and management was standardized.
INTERVENTIONS:: None. MEASUREMENTS AND MAIN RESULTS:: The incidence per 1,000
(95% confidence interval) catheter days of colonization (>/=15 colonies) and
catheter-related bloodstream infection was 15.7 (9.5-25.9) and 0.92 (0.13-6.44)
for arterial catheters and 16.8 (13.3-21.3) and 2.23 (1.12-4.44) for central
venous catheters. Arterial catheter colonization was not significantly different
than that in central venous catheters (hazard ratio, 1.17; 95% confidence
interval, 0.41-3.36; p = .77). Arterial catheter colonization increased with
dwell time and was similar to central venous catheters over time. Femoral
arterial catheters were colonized more often than radial arterial catheters
(hazard ratio, 5.08; 95% confidence interval, 0.85, 30.3; p = .075), and
colonization was significantly higher when the catheter was inserted in the
operating theater or emergency department (hazard ratio, 4.45; 95% confidence
interval, 1.42-13.9; p = .01) compared with the intensive care unit.
CONCLUSIONS:: The incidence of catheter-related bloodstream infection from
arterial catheters was low. However, both arterial catheter colonization and
rates of catheter-related bloodstream infection were similar to those in
concurrently sited and identically managed central venous catheters. By
inference, the arterial catheter should be accorded the same degree of importance
as the central venous catheter as a potential source of sepsis. LEARNING
OBJECTIVES: On completion of this article, the reader should be able to:All
authors have disclosed that they have no financial relationships with or
interests in any commercial companies pertaining to this educational activity.All
faculty and staff in a position to control the content of this CME activity have
disclosed that they have no financial relationships with, or financial interests
in, any commercial companies pertaining to this educational activity.Lippincott
CME Institute, Inc., has identified and resolved all faculty and staff conflicts
of interest regarding this educational activity.Visit the Critical Care Medicine
Web site (www.ccmjournal.org) for information on obtaining continuing medical
education credit.
PMID: 18091549 [PubMed - as supplied by publisher]
8: J Clin Anesth. 2007 Dec;19(8):609-15.
Experience of anesthesiologists with percutaneous nonangiographic venous access.
Chen PT, Sung CS, Wang CC, Chan KH, Chang WK, Hsu WH.
Department of Anesthesiology, Taipei-Veterans General Hospital and National
Yang-Ming University, Taipei 112, Taiwan.
STUDY OBJECTIVE: To compare percutaneous nonangiographic insertion of a venous
access device with a standard surgical cutdown insertion technique. DESIGN:
Prospective, controlled, randomized study. SETTING: Operating room and anesthesia
induction room of a university hospital. PATIENTS: 100 consecutive oncology
patients scheduled for intravenous chemotherapy. INTERVENTIONS: Patients were
randomized to two groups: (1) The percutaneous group received implantation
through the internal jugular vein by experienced anesthesiologists, whereas (2)
the surgical group received venous cutdown insertion through the cephalic or
subclavian vein by surgeons (n = 50 for each group). MEASUREMENTS: Duration of
procedure, long-term device function, complications such as hematoma formation,
infection, hemothorax, pneumothorax, and patients' satisfaction with the
placement procedure at two months of follow-up were all measured and recorded.
MAIN RESULTS: The percutaneous technique was found to have several advantages,
including reduced time for insertion and greater patient satisfaction with
procedure. The percutaneously implanted devices also had fewer
insertion-associated complications. CONCLUSION: The simplified, percutaneous,
nonangiographic technique is as effective as the traditional venous cutdown
technique and can be safely done by surgeons as well as by experienced physicians
who are not surgeons.
Publication Types:
Randomized Controlled Trial
PMID: 18083475 [PubMed - indexed for MEDLINE]
9: Anesthesiology. 2007 Dec;107(6):946-53.
Comparison of catheter-related infection and tip colonization between internal
jugular and subclavian central venous catheters in surgical neonates.
Breschan C, Platzer M, Jost R, Schaumberger F, Stettner H, Likar R.
Department of Anesthesiology, Landeskrankenhaus Klagenfurt, Klagenfurt, Austria.
breschan.ch@chello.at
BACKGROUND: The primary aim of this study was to compare catheter-associated
infections and tip contaminations between percutaneously placed central venous
catheters in the internal jugular and subclavian veins in surgical neonates
undergoing major noncardiac surgery. METHODS: The prospectively computerized
protocols of 295 procedures were analyzed retrospectively. RESULTS: One hundred
twenty-nine internal jugular venous (group I) and 107 subclavian venous catheters
(group S) were included. The median postconceptual age was 37 weeks in group I
and 38 in group S. The weight ranged from 580 g to 4.5 kg in group I and from 820
g to 4.5 kg in group S at the time of insertion. Significantly more
catheter-associated infections were observed in group I (15.5 vs. 4.7%;
chi-square analysis: P < 0.01). The internal jugular venous catheters were also
associated with a significantly increased probability of an earlier onset of a
catheter-associated infection compared with the subclavian venous catheters (log
rank test: P < 0.01; Cox model: P < 0.01). This probability was only slightly
increased by a lower weight (Cox model: P = 0.075), and it was not increased by a
lower age (Cox model: P = 0.93). Significantly more catheter tips were
contaminated by pathogens in group I (55.8 vs. 33.6%; chi-square analysis: P <
0.01). CONCLUSION: The internal jugular venous catheters were associated with a
higher infection rate as well as earlier onset of catheter-associated infection
compared with the subclavian venous catheters.
Publication Types:
Comparative Study
Research Support, Non-U.S. Gov't
PMID: 18043063 [PubMed - indexed for MEDLINE]
10: Arch Intern Med. 2007 Oct 22;167(19):2066-72.
Chlorhexidine-based antiseptic solution vs alcohol-based povidone-iodine for
central venous catheter care.
Mimoz O, Villeminey S, Ragot S, Dahyot-Fizelier C, Laksiri L, Petitpas F, Debaene
B.
Département d'Anesthésie Réanimation, Centre Hospitalier et Universitaire de
Poitiers, 86021 Poitiers, France. o.mimoz@chu-poitiers.fr
BACKGROUND: Although chlorhexidine-based solutions and alcohol-based
povidone-iodine have been shown to be more efficient than aqueous povidone-iodine
for skin disinfection at catheter insertion sites, their abilities to reduce
catheter-related infection have never been compared. METHODS: Consecutively
scheduled central venous catheters inserted into jugular or subclavian veins were
randomly assigned to be disinfected with 5% povidone-iodine in 70% ethanol or
with a combination of 0.25% chlorhexidine gluconate, 0.025% benzalkonium
chloride, and 4% benzylic alcohol. Solutions were used for skin disinfection
before catheter insertion (2 consecutive 30-second applications separated by a
period sufficiently long to allow for dryness) and then as single applications
during subsequent dressing changes (every 72 hours, or earlier if soiled or wet).
RESULTS: Of 538 catheters randomized, 481 (89.4%) produced evaluable culture
results. Compared with povidone-iodine, the chlorhexidine-based solution was
associated with a 50% decrease in the incidence of catheter colonization (11.6%
vs 22.2% [P = .002]; incidence density, 9.7 vs 18.3 per 1000 catheter-days) and
with a trend toward lower rates of catheter-related bloodstream infection (1.7%
vs 4.2% [P = .09]; incidence density, 1.4 vs 3.4 per 1000 catheter-days).
Independent risk factors for catheter colonization were catheter insertion into
the jugular vein (adjusted relative risk, 2.01; 95% confidence interval,
1.24-3.24) and use of povidone-iodine (adjusted relative risk, 1.87; 95%
confidence interval, 1.18-2.96). CONCLUSION: Chlorhexidine-based solutions should
be considered as a replacement for povidone-iodine (including alcohol-based)
formulations in efforts to prevent catheter-related infection.
Publication Types:
Comparative Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 17954800 [PubMed - indexed for MEDLINE]
11: Clinics. 2007 Oct;62(5):537-44.
Risk factors for central venous catheter-related infections in pediatric
intensive care.
Vilela R, Jácomo AD, Tresoldi AT.
State University of Campinas (UNICAMP) - Clinical Hospital, Pediatric Intensive
Care Unit. ricardovilela@superig.com.br
OBJECTIVES: To identify risk factors for short-term percutaneously inserted
central venous catheter-related infections in children and to evaluate the
accuracy of a mortality score in predicting the risk of infection. METHOD: After
reviewing the charts of patients who developed catheter-related infection in a
university hospital's pediatric intensive care unit, we conducted a
case-controlled study with 51 pairs. Variables related to patients and to
catheter insertion and use were analyzed. Risk factors were defined by logistic
regression analysis. The accuracy of the Pediatric Risk of Mortality score to
discriminate the risk for infection was tested using the Receiver Operating
Characteristic curve. RESULTS: Infection was associated with respiratory failure,
patient's length of stay, duration of tracheal intubation, insertion of catheter
in the intensive care unit and parenteral nutrition. Insertion site (femoral or
internal jugular) was unimportant. Multivariate logistic regression analysis
identified the following variables. Risk factors included more than one catheter
placement (p=0.014) and duration of catheter use (p=0.0013), and protective
factors included concomitant antibiotic use (p=0.0005) and an intermittent
infusion regimen followed by heparin filling compared to continuous infusion
without heparin (p=0.0002). Pediatric Risk of Mortality did not discriminate the
risk of infection. CONCLUSIONS: Central parenteral nutrition and central venous
catheters should be withdrawn as soon as possible. Femoral vein catheterization
carries a risk of infection similar to internal jugular catheterization. The
Pediatric Risk of Mortality score should not be used to predict the risk of
central catheter-related infections.
PMID: 17952312 [PubMed - in process]
12: Crit Care Med. 2007 Oct;35(10):2424-7.
Comment in:
Crit Care Med. 2007 Oct;35(10):2459-60.
Microorganisms responsible for intravascular catheter-related bloodstream
infection according to the catheter site.
Lorente L, Jiménez A, Santana M, Iribarren JL, Jiménez JJ, Martín MM, Mora ML.
Department of Intensive Care and Research Unit, Hospital Universitario de
Canarias, Tenerife, Spain. lorentemartin@msn.com
OBJECTIVE: Current guidelines for the management of intravascular
catheter-related bloodstream infection (IVC-RBSI) recommend that empirical
antimicrobial therapy must have activity against Gram-positive bacteria, but
additional empirical coverage for Gram-negative bacteria may be needed for
severely ill or immunocompromised patients, and antifungal therapy may be needed
in some situations. We hypothesized that the spectrum of etiological
microorganisms responsible for IVC-RBSI and, in relation to that, the choice of
empirical antimicrobial therapy depends on the catheter insertion site. We
therefore compared the proportion of IVC-RBSI due to Gram-negative bacteria and
yeasts according to catheter site. DESIGN: Prospective cohort study from May 1,
2000, to April 30, 2004. SETTING: A 24-bed medical-surgical intensive care unit
in a 650-bed tertiary hospital. PATIENTS: Patients requiring a central venous or
arterial catheter. MEASUREMENTS AND MAIN RESULTS: We diagnosed 88 IVC-RBSIs,
comprising 36 femoral catheter sites (26 femoral venous and ten femoral arterial
sites) and 52 other catheter sites (36 jugular venous, 11 subclavian venous, and
five radial arterial sites). No differences were found between IVC-RBSI of
femoral vs. other catheter sites for age, sex, Acute Physiology and Chronic
Health Evaluation II, diagnosis at admission, use of antimicrobials, the time the
catheter responsible for IVC-RBSI had been in place, or the duration of intensive
care unit stay before IVC-RBSI. The proportion of IVC-RBSIs due to Gram-negative
bacteria was higher in femoral, 14 of 36 (38.89%), than in the other catheter
sites, 4 of 52 (7.69%) (odds ratio, 7.48; 95% confidence interval, 2.19-25.54; p
= .001). Also, the proportion of IVC-RBSIs due to yeasts was higher in femoral, 6
of 36 (16.67%), than in the other catheter sites, 1 of 52 (1.92%) (odds ratio,
10.20; 95% confidence interval, 1.17-88.85; p = .035). CONCLUSIONS: Empirical
antifungal therapy would seem to be indicated in patients with suspected femoral
catheter-related bloodstream infection.
Publication Types:
Comparative Study
Research Support, Non-U.S. Gov't
PMID: 17717493 [PubMed - indexed for MEDLINE]
13: Saudi J Kidney Dis Transpl. 2007 Sep;18(3):370-7.
Outcome and survival of temporary hemodialysis catheters: a prospective study
from a single center in Iraq.
Altaee KH, Theeb OA, Al-Timimi SM, Saeed HM, Alshamma I.
Nephrology and Renal Transplantation Department, Surgical Hospital, Baghdad
Medical City, Baghdad, Iraq.
BACKGROUND: The use of temporary hemodialysis catheters (THC) has facilitated the
delivery of hemodialysis to patients lacking functional vascular access. However,
the use of these catheters is often associated with infections or mechanical
complications. METHODS: A review of experiences at a tertiary referral center in
Iraq with the use of 128 THC catheters in 103 patients was undertaken over one
year, to identify indications for use and outcomes and issues limiting survival.
RESULTS: The indications for insertion of THC included the following: as acute
dialysis access for patients with chronic renal failure (CRF) in 42.1%, failed
arteriovenous fistulae in 14%, acute renal failure in 18%, failed prior THC in
18.7%, absent vascular access in patients with transplant rejection in 6.2% and
severe anasarca in one patient (0.78%). The site of insertion was the right
internal jugular vein in 101 patients, the right subclavian vein in 23 patients,
and the left internal jugular vein in four patients. During follow-up, 86
catheters were removed: 62 in patients with end-stage renal disease (ESRD), 23 in
patients with acute renal failure and one patient with severe anasarca. The
reasons for removal of THC in ESRD patients were elective removal (44%), catheter
related sepsis (CRS) in 30%, mechanical complications (19%) and others (7%). The
subclavian site was associated with infection in 20% of patients, while the
internal jugular site was associated with infection in 22.7% of patients. For
patients in whom THC removal was for infection, a post removal culture of the
catheter tip showed Staphylococcus aureus in 57.8%, Klebsiella in 15.7%,
Pseudomonas in 15.7% and Streptococcus hemolyticus in 10.5% of the cases.
CONCLUSIONS: THC is advantageous for vascular access in patients with acute renal
failure. Infections and blockage significantly reduce the survival of THC in
patients with ESRD. Approaches to minimize these complications are likely to lead
to improved clinical outcomes with THC use.
PMID: 17679748 [PubMed - indexed for MEDLINE]
14: J Vasc Access. 2001 Jul-Sep;2(3):91-6.
Subcutaneous implantation of the LifeSite Hemodialysis Access System in the
femoral vein.
Ross JR.
General Surgery, Bamberg County Hospital, Bamberg, South Carolina - USA.
Cannulation of the femoral vein is often necessary to provide immediate vascular
access for hemodialysis patients in whom a functional permanent access is not
available or in patients who have exhausted other access options. Femoral
placement of dialysis catheters is typically short term - days, not months - and
is associated with high rates of infection, occlusion, recirculation and
intervention as well as a high risk of catheter dislodgment. A new, fully
subcutaneous vascular access device - the LifeSite(R) Hemodialysis Access System
(Vasca, Inc., Tewksbury, MA) - has demonstrated better safety and efficacy
profiles than a standard tunneled dialysis catheter in clinical trails that
evaluated placement within the thoracic veins. The case reported here extends the
use of the Life-Site(R) System to femoral placement in a patient with multiple
failed arteriovenous accesses and dialysis catheters subsequent to central venous
stenosis. The LifeSite(R) System was successfully implanted in the patient's left
femoral vein and has served the patient for 4 months with no infections or
complications requiring intervention, delivering flow rates >400-450 ml/minute
for high-flux, dual-needle hemodialysis. These initial results suggest that the
LifeSite(R) Hemodialysis Access System represents a new, safe and effective
vascular access option in patients with limited access choices due to failed
access in the upper extremities, central venous stenosis, or other vascular
inadequacies.
PMID: 17638268 [PubMed - in process]
15: J Vasc Access. 2001 Apr-Jun;2(2):68-72.
Implantation of permanent jugular catheters in patients on regular dialysis
treatment: ten years' experience.
Ervo S, Cavatorta F, Zollo A.
Department of Nephrology and Dialysis, General Hospital, Imperia - Italy.
Dual-lumen cuffed central venous catheter proved an important alternative
vascular access compared to conventional arteriovenous (Cimino-Brescia) shunt in
a selected group of patients on regular dialysis treatment. Typically, these
catheters are used as bridging access, until fistula or graft is ready for use,
or as permanent access when an arteriovenous fistula or graft is not planned
(NKF-DOQI). We conducted a prospective study on IJV permanent catheter insertion
and its related earlier and long-term complications. From February 1991 to
February 2001 we inserted in 124 patients in end stage renal disease 135 cuffed
catheters (130 in the right IJV and 5 in the left IJV), 92 of which were
Permcath, 27 Vascath, and 16 Ash-Split. We performed the insertion of catheters
by puncturing the IJV under ultrasonographic guid-ance in the lower side of the
Sedillot triangle and checking the accurate position of the tip by endocavitary
electrocardiography (EC-ECG). The duration of catheter use was from 60 to 1460
days, mean 345 days. The actuarial survival rate at 1 year was 82%, at 2 years
56%, at 3 years 42% and at 4 years 20%. The exit site infection and septicemia
rates were 5.2 and 2.86 per 1000 catheter days respectively. Catheter sepsis was
implicated in the death of three patients, all of whom had multiple medical
problems. Several episodes of thrombosis (6% of dialyses) occurred which required
urokinase treatment, and catheter replacement in 12 patients (9.6%). In 3 cases
the catheters were displaced and correct repositioning was performed. Two
catheters (Ash-Split) were replaced due to accidental damage of the external
portion of catheters (alcoholic disinfectant). Catheter tip embolism occurred on
one occasion during elective catheter exchange over guide-wire. One of the common
problems encountered with cuffed tunneled catheters is poor blood flow, most
often secondary to the formation of a fibrin sheath around the lumen. Even if we
conducted a non-randomized study, in our experience, the higher rate of
malfunctioning catheters was in the group with no anticoagulation therapy.
Therefore, we suggest anticoagulation treatment in all patients wearing central
vascular catheters with no contraindication. Just one year ago, we followed
NKF-DOQI clinical practice guidelines for vascular access that indicated that for
patients who have a primary AV fistula maturing, but need im-mediate
hemodialysis, tunneled cuffed catheters are the access of choice and the
preferred insertion site is the right IJV. Considering recent reports of
permanent central venous stenosis or occlusion after IJV can-nulation, currently,
our first choice is femoral vein cannulation with smooth silicone rubber
catheters, tunneled if long-term utilization is needed (more the 3-4 weeks). In
our opinion, the right IJV puncture is to be avoided as much as the venipuncture
of arm veins suitable for vascular access placement, particularly the cephalic
vein of the non-dominant arm. Our data confirm that permanent venous catheters
might rep-resent an effective long-term vascular access for chronic hemodialysis,
particularly for older patients with cardiovascular disease and for cancer
patients.
PMID: 17638264 [PubMed - in process]
16: J Vasc Access. 2001 Apr-Jun;2(2):56-9.
Ultrasound-guided cannulation of the femoral vein for acute hemodialysis access
with silicone catheters.
Zollo A, Cavatorta F, Galli S.
Department of Nephrology and Dialysis, General Hospital, Imperia - Italy.
The percutaneous femoral approach for temporary central venous hemodialysis
access is a mandatory part of patient management in many clinical settings. It is
usually achieved with a blind, exter-nal landmark-guided technique. The aim of
this study is to evaluate whether an ultrasound technique can improve on the
external landmark method. From 1990 to January 2000, cannulation of the femoral
vein was performed on 230 patients (125 male, 105 female, mean age 72 years,
range 52-95 years) for temporary vascular access for hemodialysis (172 patients
with acute renal failure and 58 patients in end-stage renal disease), using
landmark localization with semi-rigid, uncuffed catheters. Between January 2000
and February 2001, ultrasound-guided can-nulation of the femoral vein was
utilized in 38 patients (20 male, 13 female, mean age 71 , range 55-93 years) for
temporary vascular access for hemodialysis (28 patients with acute renal failure
and 10 patients in end-stage- renal failure). Uncuffed, dual-lumen silicone
catheters were used. Cannulation of the femoral vein was achieved in 100% of
cases using ultrasound, and in 87% using the landmark-guided technique. Using
ultrasound, puncture of the femoral artery occurred in 2.6% of patients, and
hematoma in 0%. Using the 'blind' technique, puncture of the femoral artery
occurred in 11.2% of patients, and hematoma in 3.9%. The average catheter dwell
time, in accordance with NKF-DOQI guidelines, was 5 days (range 2 - 14 days) for
semi-rigid catheters and 45 days (range 5-120 days) for silastic catheters. The
number of complications rose significantly in the patients with semi-rigid
catheters. In this group, local exit infection occurred in 105 persons (45% of
cases), total catheter thrombosis in 46 (20%), bacteriemia in 28 (12%), and
phlebitis of the leg in 6 (2.6%). In the group with silicone catheters local exit
infection occurred in 4 patients (10 % of cas-es), total catheter thrombosis in 1
(2.6%), bacteriemia in 2 (5.2%) and phlebitis in 0 (0%). The result of the study
suggests that ultrasound-guided cannulation of the femoral vein is superior to
traditional techniques relying on anatomic landmark; it reduces the numbers of
unsuccessful attempts and the possible acute complications of the procedure. We
believe that femoral cannulation with modern flexible silicone catheters can be
considered as a reliable temporary access, even for extended periods.
PMID: 17638261 [PubMed - in process]
17: Cochrane Database Syst Rev. 2007 Jul 18;(3):CD004084.
Central venous access sites for the prevention of venous thrombosis, stenosis and
infection in patients requiring long-term intravenous therapy.
Hamilton HC, Foxcroft DR.
Oxford Radcliffe Hospitals NHS Trust, TPN and Line Insertion Team, Level 6 C/D,
John Radcliffe Hospital, Oxford, UK, OX3 9DU. Helen.Hamilton@orh.nhs.uk
BACKGROUND: Central venous access (CVA), in which a large bore catheter is routed
through a vein in the neck, upper chest or femoral area, is needed to give drugs
that cannot be given by mouth or via a conventional cannula in the arm.
OBJECTIVES: To establish whether either the jugular, subclavian or femoral CVA
routes result in a lower incidence of venous thrombosis, venous stenosis or
infection related to CVA devices.To determine whether the circumference of a
long-term central venous access device influences the incidence of venous
thrombosis, venous stenosis or infection related to CVA devices. SEARCH STRATEGY:
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The
Cochrane Library 2006, Issue 4), MEDLINE, CINAHL, EMBASE (from inception to
December 2006), reference lists of identified trials, and bibliographies of
published reviews. We also contacted researchers in the field. There were no
language restrictions. SELECTION CRITERIA: We included randomized controlled
trials comparing central venous catheter insertion routes. DATA COLLECTION AND
ANALYSIS: Two authors assessed potentially relevant studies. We resolved
disagreements by discussion. Relevant outcomes were: venous thrombosis, venous
stenosis, infection related to CVA devices, mechanical complications (e.g
misplaced catheter, minor bleeding, haematoma). MAIN RESULTS: We considered 83
studies for inclusion in the review. Six studies appeared eligible but five were
subsequently excluded because they did not randomize participants for either site
of access or catheter circumference size. One study was a high quality block
randomized controlled trial. Allocation concealment was good and randomization
was by a central computer. In all, 293 patients were randomized to a femoral or a
subclavian CVA group. Results from this one trial were as follows. 1.
CATHETER-RELATED INFECTIOUS COMPLICATIONS: Infectious complication (colonization
with or without sepsis: the relative risk (RR) was 4.57 (95% confidence interval
(CI) 1.95 to 10.71) favouring subclavian over femoral access.Major infectious
complications (sepsis with or without bacteremia): the RR was 3.04 (95% CI 0.63
to 14.82) favouring subclavian access. Colonized catheter (greater than 103
colony-forming units/mL of gram positive microorganisms): the RR was 3.65 (95%CI
1.40 to 9.56) favouring subclavian access. Colonized catheter (greater than 103
colony-forming units/mL of gram negative microorganisms): the RR was 5.41 (95% CI
1.61 to 18.15) favouring subclavian access. 2. CATHETER-RELATED MECHANICAL
COMPLICATIONS: Overall complications (arterial puncture, minor bleeding,
haematoma, misplaced catheter): the RR was 0.92 (95% 0.56 to 1.51) favouring
subclavian access. 3. CATHETER-RELATED THROMBOTIC COMPLICATIONS: Catheterrelated
thromboses (fibrin sleeves, major and complete thrombosis): the RR was 11.53 (95%
CI 2.80, to 47.52) favouring subclavian access. AUTHORS' CONCLUSIONS: Subclavian
CVA is preferable to femoral CVA. Further trials of subclavian versus femoral or
jugular CVA are needed. Research on the impact of catheter circumference on
catheter-related complications is required.
Publication Types:
Review
PMID: 17636746 [PubMed - indexed for MEDLINE]
18: J Surg Res. 2007 Oct;142(2):341-50. Epub 2007 Jul 12.
Central venous catheter infections in burn patients with scheduled catheter
exchange and replacement.
O'Mara MS, Reed NL, Palmieri TL, Greenhalgh DG.
The University of California, Davis Medical Center, Shriners Hospital for
Children Northern California, Sacramento, California, USA. momara@shrinenet.org
INTRODUCTION: Consensus in the general critical care patient population is that
routine central venous catheter change is not necessary, and that central lines
should not be rewired in the setting of possible infection. This concept has not
carried over into the burn realm. In burn patients the rewiring of lines may lead
to increased infection rates. METHODS: Fifty-nine consecutive critically ill burn
patients requiring central line placement were included: 277 central lines and
1691 catheter days. Standard care protocol was followed in all patients, with
lines being placed initially by new site insertion, changed over a guidewire on
day 6, and moved to a new site on day 12. New sites were used for all suspected
or documented line infections. All other care was the same. New site placements
were compared to guidewire exchanges. Pediatric patients (under the age of 18)
were considered with and separate from adults. RESULTS: There was no difference
in the incidence of catheter-related bloodstream infections (CRBSI) between lines
placed by new site access (15.4/1000 catheter days) or by guidewire exchange
(15.4/1000). Considering the 979 pediatric line days, there was a distinct
difference, with new sites having 16.6/1000, and rewires 25.2/1000. Adults
revealed the opposite trend, rewires having no occurrences of CRBSI, and new
sites 13.7/1000. Children had a higher rate of CRBSI, 19.4/1000 days, compared to
adults at 9.8/1000 days. Children had larger burns (P < 0.0001), more femoral
lines (P = 0.0003), and lines closer to the burn wound (P = 0.001). CONCLUSIONS:
In pediatric patients guidewire exchange increased the incidence of infection.
This was not noted in adult patients. The utility of guidewire exchange needs to
be further investigated in adults, although this data would imply that it may be
safe to use routine rewire of lines in adult burn patients. Pediatric patients
require an increase in vigilance to minimize CRBSI. Central venous catheters
should be removed as soon as not needed and routine change of lines in burn
patients needs continued evaluation.
PMID: 17631903 [PubMed - indexed for MEDLINE]
19: J Vasc Interv Radiol. 2007 Jul;18(7):875-81.
Radiologically placed tunneled internal jugular catheters in the management of
chronic hemodialysis and long-term infusion therapies in the pediatric
population.
Peynircioglu B, Ozkan F, Canyigit M, Pamuk GA, Geyik S, Cil BE, Balkanci F.
Department of Radiology, Hacettepe University, School of Medicine, Ankara,
Turkey. borapeynir@gmail.com
PURPOSE: To evaluate the long-term outcomes of radiologically inserted dual-lumen
hemodialysis and infusion catheters in pediatric patients. MATERIALS AND METHODS:
The authors retrospectively reviewed the outcomes of 114 tunneled internal
jugular catheters in 71 consecutive pediatric patients between March 2003 and May
2006. Forty hemodialysis catheters were placed in 23 patients (11 girls, 12
boys), and 74 infusion catheters were placed in 48 patients (14 girls, 34 boys).
The mean patient age was 11.2 years (range, 1-16 years) in the hemodialysis group
and 7.86 years (range, 4 months to 16 years) in the infusion group. RESULTS: The
technical success rate was 100%. The mean duration of catheter use was 84 days
(range, 5-730 days) in the hemodialysis group and 58 days (range, 3-206 days) in
the infusion group. Nine hemodialysis (22%) and 29 infusion (39%) catheters were
electively removed. The most common reasons for catheter removal were malfunction
(22%) in the hemodialysis group and completion of therapy (39%) in the infusion
group. Revisions were performed at a rate of 0.6 and 0.4 per 100 catheters days
in the hemodialysis and infusion groups, respectively. Total infection rates were
0.15 and 0.38 episodes per 100 catheter days in hemodialysis and infusion
catheters, respectively. Mean primary device service intervals were 86 and 60
days for hemodialysis and infusion catheters, respectively, with total access
site service intervals of 140 and 71 days. CONCLUSION: Radiologically placed
tunneled internal jugular catheters appear to be safe and effective, with very
low complication rates for both hemodialysis and long-term infusion therapies.
Higher infection rates were seen in patients with cancer.
PMID: 17609447 [PubMed - indexed for MEDLINE]
20: Curr Opin Crit Care. 2007 Aug;13(4):411-5.
Prevention of catheter-related blood stream infection.
Byrnes MC, Coopersmith CM.
Department of Surgery, Washington University School of Medicine, St. Louis,
Missouri, USA.
PURPOSE OF REVIEW: Catheter-related blood stream infections are a morbid
complication of central venous catheters. This review will highlight a
comprehensive approach demonstrated to prevent catheter-related blood stream
infections. RECENT FINDINGS: Elements of prevention important to inserting a
central venous catheter include proper hand hygiene, use of full barrier
precautions, appropriate skin preparation with 2% chlorhexidine, and using the
subclavian vein as the preferred anatomic site. Rigorous attention needs to be
given to dressing care, and there should be daily assessment of the need for
central venous catheters, with prompt removal as soon as is practicable.
Healthcare workers should be educated routinely on methods to prevent
catheter-related blood stream infections. If rates remain higher than benchmark
levels despite proper bedside practice, antiseptic or antibiotic-impregnated
catheters can also prevent infections effectively. A recent program utilizing
these practices in 103 ICUs in Michigan resulted in a 66% decrease in infection
rates. SUMMARY: There is increasing recognition that a comprehensive strategy to
prevent catheter-related blood stream infections can prevent most infections, if
not all. This suggests that thousands of infections can potentially be averted if
the simple practices outlined herein are followed.
Publication Types:
Review
PMID: 17599011 [PubMed - indexed for MEDLINE]
21: J Hosp Med. 2007 May;2(3):135-42.
Comment in:
J Hosp Med. 2007 May;2(3):123-5.
Firm-based trial to improve central venous catheter insertion practices.
Miranda JA, Trick WE, Evans AT, Charles-Damte M, Reilly BM, Clarke P.
Department of Medicine, Cook County (Stroger) Hospital, Chicago, Illinois, USA.
Julio.A.Miranda@Hitchcock.org
BACKGROUND: Central venous catheters placed in femoral veins increase the risk of
complications. At our institution, residents place most catheters in the femoral
vein. OBJECTIVE: Determine whether a hands-on educational session reduced femoral
venous catheterization and improved residents' confidence and adherence to
recommendations for infection control. DESIGN: Firm-based clinical trial between
November 2004 and March 2005. SETTING: General medical wards of Cook County
(Stroger) Hospital (Chicago, IL), a public teaching hospital. PARTICIPANTS:
Internal medicine residents (n = 150). INTERVENTION: Before their 4-week
rotation, intervention-firm residents received a lecture and practiced placing
catheters in mannequins; control-firm residents received the usual training.
MEASUREMENTS: Venous insertion site, adherence to recommendations for infection
control, knowledge and confidence about catheter insertion, and
catheter-associated complications RESULTS: Residents inserted 54 catheters, or
0.24 insertions per resident per 4-week rotation. There was a nonsignificant
decrease in femoral insertions for nondialysis catheters in the intervention
group compared to the control group (44% vs. 58%), difference: -14% (95% CI, -52%
to 24%). The intervention significantly increased residents' knowledge of
complications related to femoral vein catheterization and temporarily increased
their confidence about placing internal jugular or subclavian venous catheters.
Intervention-group residents were more likely to use masks during catheterization
(risk ratio, 2.2; 95% CI, 1.3-2.7), but other practices were similar.
CONCLUSIONS: Our intervention improved residents' knowledge of complications and
use of masks during catheter insertion; however, it did not significantly change
venous insertion sites. Catheter insertions on our general medicine wards are
infrequent, and the skills acquired during the skills-building session may have
deteriorated given the few clinical opportunities for reinforcement. (c) 2007
Society of Hospital Medicine.
Publication Types:
Controlled Clinical Trial
PMID: 17549773 [PubMed - indexed for MEDLINE]
22: Intensive Care Med. 2007 Jun;33(6):1071-5. Epub 2007 Apr 25.
Internal jugular venous catheter-related bacteremia according to central and
posterior accesses.
Lorente L, Jiménez A, Castedo J, Galván R, García C, Martín MM, Mora ML.
Hospital Universitario de Canarias, Intensive Care Unit, Ofra s/n, La Cuesta, La
Laguna, 38320 Santa Cruz de Tenerife, Spain. lorentemartin@msn.com
BACKGROUND: Although there are many studies about central venous catheter-related
infection, we have not found any analysis of the incidence of internal jugular
venous catheter-related bacteremia associated with different accesses. OBJECTIVE:
The objective of this study was to test whether the position of the internal
jugular venous catheter, central or posterior, influences the incidence of
bacteremia. DESIGN: A cohort study. SETTING: A 12-bed polyvalent medical-surgical
intensive care unit (ICU). PATIENTS: Patients admitted to ICU between 1 May 2000
and 30 April 2004 who received one or more internal jugular venous catheters.
MEASUREMENTS AND RESULTS: A total of 1,483 patients were admitted to the
polyvalent ICU, of whom 1,311 underwent central venous catheterization. A total
of 547 patients received 684 internal jugular venous catheters, 169 by posterior
and 515 by central access. There were no significant differences between central
and posterior access patients in sex, age, APACHE II (14.1 +/- 5.0 vs. 13.9 +/5.2, p = 0.40), diagnosis, order of catheter insertion, use of mechanical
ventilation, use of antimicrobials, use of total parenteral nutrition or use of
pulmonary artery catheter. We found a higher incidence of internal jugular venous
catheter-related bacteremia with central (4.8 per 1000 catheter-day) than with
posterior (1.2 per 1000 catheter-day) access (odds ratio 3.9; 95% confidence
interval 1.1-infinite; p = 0.03). CONCLUSION: Posterior access has a lower
incidence of internal jugular venous catheter-related bacteremia than central
access in non-severely ill patients (according to the low APACHE II score values
of the study patients).
PMID: 17457569 [PubMed - indexed for MEDLINE]
23: J Vasc Interv Radiol. 2007 Feb;18(2):227-35.
The natural history of tunneled hemodialysis catheters removed or exchanged: a
single-institution experience.
Alomari AI, Falk A.
Department of Radiology, Mount Sinai Medical Center, One Gustave L. Levy Place,
New York, NY 10029, USA.
PURPOSE: To track the natural history of tunneled hemodialysis catheters
requiring removal or exchange at a single institution. MATERIALS AND METHODS:
Over a 2-year period, tunneled hemodialysis catheters that presented to
interventional radiology for removal or exchange were entered into this
retrospective study. Patient demographics, catheter location, dwell time, and
indication for removal were recorded. Pull-back contrast venography was performed
with imaging over the chest. Catheters were then removed or exchanged. RESULTS:
Three hundred thirty-four tunneled dialysis catheters were removed or exchanged
in 207 patients; 108 male, median age 53 years. Dwell time, available from 296
catheters, ranged from 1 to 114 days (median, 66 days) for a total of 32,847
catheter days. One hundred three catheters were removed for infection, yielding a
rate of infection requiring catheter removal of 3.0 per 1,000 catheter days. One
hundred catheters were removed for other working access, and 96 catheters were
exchanged for poor function. Two hundred sixty-five were removed or exchanged
from the internal jugular vein, 22 from the subclavian vein, and 24 from the
femoral vein. One hundred seventy-two (76%) of the 226 catheters studied with
contrast had fibrin sheaths; of which 42 had thrombus identified along the
catheter tract. One hundred ninety-three catheters were removed, and 141
catheters were exchanged for new catheters with 82 catheters receiving balloon
disruption of the fibrin sheath. CONCLUSIONS: Approximately one third of tunneled
dialysis catheters are removed for infection, one third for other working access,
and one third for poor function. Catheters usually remain in the patient for a
median of 2 months. Fibrin sheaths associated with hemodialysis catheters are
very common. Thrombus formation around the sheath is frequent.
PMID: 17327555 [PubMed - indexed for MEDLINE]
24: J Vasc Interv Radiol. 2007 Feb;18(2):217-25.
Use of the femoral vein as insertion site for tunneled hemodialysis catheters.
Falk A.
American Access Care, 200 Boston Avenue, Medford, Massachusetts 02155, USA.
abigailfalk123@pol.net
PURPOSE: To determine the outcome of tunneled hemodialysis catheters inserted
through the common femoral vein. MATERIALS AND METHODS: From April 2000 to June
2003, 33 consecutive patients had 86 tunneled hemodialysis catheters inserted
through the femoral vein. There were 14 male and 19 female patients with a mean
age of 56 years. Seventeen patients had bilateral central venous and/or superior
vena cava (SVC) occlusions, 12 patients had unilateral central venous occlusions
and were to receive contralateral arteriovenous fistulas or arteriovenous
polytetrafluoroethylene grafts, and 4 patients received femoral catheters for
other reasons. The technical success, complications, and clinical outcomes of
these procedures were retrospectively evaluated. RESULTS: All procedures were
technically successful. Fifty-seven catheters were inserted into the right
femoral vein and 29 into the left femoral vein. This included 25 catheter
exchanges in 13 patients. Two patients developed thigh hematomas. Follow-up data
were available for 68 catheters; mean follow-up period was 51 days with a total
of 3,484 catheter days. The catheter-related infection rate was 6.3 per 1,000
catheter days; 22 catheters were removed for infection. Eighteen catheters were
removed because of poor blood flows (<200 mL/min). Thirteen catheters were
removed because they had become retracted. Primary catheter patency was 44% at 1
month. CONCLUSIONS: The femoral vein provides an alternative access site for
insertion of tunneled hemodialysis catheters when conventional sites are not
available. However, tunneled femoral hemodialysis catheters have low primary
patency rates and significant complications. Catheter retraction is a unique and
common problem.
PMID: 17327554 [PubMed - indexed for MEDLINE]
25: Paediatr Anaesth. 2007 Mar;17(3):301-2.
To prevent tearing of guide wire during central venous catheter insertion.
Mehmood S.
Publication Types:
Case Reports
Letter
PMID: 17263754 [PubMed - indexed for MEDLINE]
26: J Clin Nurs. 2007 Feb;16(2):414-8.
Central venous access for haemodialysis: prospective evaluation of possible
complications.
de Andrade D, Ferreira V.
University of São Paulo at Ribeirão Preto College of Nursing, WHO Collaborating
Centre for Nursing Research Development, Brazil. dandrade@eerp.usp.br
AIMS AND OBJECTIVES: The combination of chronic renal insufficiency and
haemodialysis represents a challenge for health professionals. Chronic renal
insufficiency patients undergoing haemodialysis treatment through a temporary
double-lumen catheter were prospectively studied in order to identify the type
and frequency of local and systemic complications. METHODS: A six-month period
was established with a view to the inclusion of new cases. Data were acquired
through interviews, clinical assessment and patient records, and entered into a
Microsoft Excel database through a double entry system and exported to the
Statistical Package Social Sciences software. Sixty-four patients were evaluated
prospectively, of which thirty-eight (59.4%) were men and 35 (54.7%) required
catheter insertion for immediate treatment. During the study period, 145
catheters were inserted, ranging from 1 to 7 implants per patient, 29 (45.3%)
were single insertions and 127 (87.6%) catheters were inserted into the jugular
vein. The catheters were left in place for an average of 30 days. RESULTS:
Forty-one (64%) presented inadequate functioning, after about 26 days. A febrile
state occurred in 24 (37.5%) patients after 34 days, secretion at the catheter
entry site in 27 (42.2% after 26 days and bloodstream infection was encountered
in 34(53%) after 34 days. Of the 61 blood culture samples, thirty (49%) were
positive for Staphylococcus aureus that was the microorganism most frequently
isolated. CONCLUSION: The findings indicate worrying aspects such as the
catheters permanence time, exposing patients to different complications,
including infection. Furthermore, inadequate catheter functioning leads to
inefficient haemodialysis treatment. RELEVANCE TO CLINICAL PRACTICE: Knowledge
about complications allows for systematic care planning, prevention and control
actions.
PMID: 17239078 [PubMed - indexed for MEDLINE]
27: Saudi J Kidney Dis Transpl. 2007 Mar;18(1):37-42.
Tunneled femoral vein catheterization for long term hemodialysis: a single center
experience.
Al-Hwiesh AK, Abdul-Rahaman IS.
Department of Internal Medicine, Nephrology Division, King Fahd Hospital of the
University, King Faisal University, Al-Khobar, Saudi Arabia. dr_hwiesh@yahoo.com
Femoral veins have been used for decades to position temporary hemodialysis
catheters. Few reports, however, describe its use for permanent vascular access.
This study describes the use of tunneled femoral vein catheters as permanent
vascular accesses. Fourteen chronic hemodialysis patients (nine males and five
females) had tunneled central venous catheters placed in the femoral vein from
November 2004 to July 2005. The age of the patients ranged from 21 to 68 years
with a mean of 49.8 +/- 5.9 years. Placement of a catheter via the internal
jugular veins was impossible in 10 patients whose course was complicated by
thrombosis or strictures of the superior vena cava. The remaining four patients
had exhausted conventional access sites. The insertion of the femoral catheters
involved a subcutaneous tunnel that was created by retrograde passage of the
catheter through the cannula to the point of exit at a preselected site in the
ipsilateral thigh away from the groin. The life span of the tunneled femoral
catheter ranged between 32-240 days; median time in place was 182 days. There
were four incidences of tunnel infection with Pseudomonas aeruginosa, E. coli,
and Streptococcus epidermidis, which were treated successfully without the need
for catheter removal. Other complications such as bleeding, kinking, migration of
the catheter, arterial puncture, retroperitoneal or femoral hematomas were not
observed. We conclude that tunneled femoral catheters are suitable alternatives
for long-term hemodialysis access. Additional studies with a greater sample size
are needed to confirm this conclusion.
PMID: 17237889 [PubMed - indexed for MEDLINE]
28: J Infect Chemother. 2006 Dec;12(6):363-5. Epub 2007 Jan 18.
To reduce catheter-related bloodstream infections: is the subclavian route better
than the jugular route for central venous catheterization?
Nagashima G, Kikuchi T, Tsuyuzaki H, Kawano R, Tanaka H, Nemoto H, Taguchi K,
Ugajin K.
Department of Neurosurgery, Fujigaoka Hospital, Showa University, 1-30 Fujigaoka,
Aoba-ku, Yokohama 227-8501, Japan. goro-n@po1.dti2.ne.jp
The most important targets of hospital-acquired infection control are to reduce
the incidence of surgical-site, catheter-related, and ventilator-associated
infections. In this report, we address previously presented infection-control
strategies for central venous (CV) line catheterization, using a CV
catheter-related infection surveillance system. Data concerning CV catheter
insertion were collected from all facilities in our 650-bed hospital, excluding
the operating and hemodialysis wards. Collected data included the insertion
method, purpose, length of catheter inserted, duration of catheterization,
infection rate, and complication rate. Catheter-related infection was diagnosed
based on bacteriological examinations from blood cultures. The total number of
catheterizations was 806 a year, and average duration of catheterization was 9.8
days. The purpose of catheterization was nutritional support in 210 cases,
hemodialysis in 96 cases, cardiac support in 174 cases, and other treatments in
260 cases. In 66 cases, the purpose of CV catheter was not specified. The rate of
positive cultures was 7.1%, and complications other than infection occurred in
0.5%. The main causative organisms were methicillin-resistant Staphylococcus
aureus (MRSA) in 38.6%, coagulase-negative Staphylococcus epidermidis (CNS) in
33.3%, and S. aureus in 12.3% of infections. Infection rates were 3.8 per 1000
catheter-days in subclavian, 6.1 in jugular, and 15.7 in femoral vein
catheterization. In high-risk departments (intensive care unit [ICU] and
emergency departments) the infection rate was 5.4 for subclavian and 10.2 for
jugular catheterization, whereas it was 3.6 for subclavian and 4.6 for jugular
catheterization in noncritical-care departments. Considering complications such
as pneumothorax, CV catheterization of the jugular vein is recommended in certain
situations.
Publication Types:
Evaluation Studies
PMID: 17235641 [PubMed - indexed for MEDLINE]
29: Diagn Interv Radiol. 2006 Dec;12(4):190-4.
Tunneled catheters placed in bone marrow transplant patients: radiological and
clinical follow-up results.
Parlak M, Sancak T, Arat M, Bilgiç S, Sanlidilek U.
Department of Radiology, Ankara University School of Medicine, Ankara, Turkey.
PURPOSE: To present the radiological and clinical follow-up results of 75 bone
marrow transplant patients who underwent fluoroscopy-guided tunneled catheter
placement between June 2001 and June 2004. MATERIALS AND METHODS: Tunneled
catheters were placed in 75 bone marrow transplant patients with fluoroscopic
guidance. The left subclavian vein was used in 67 patients, whereas the right
side was used in 9. RESULTS: The first attempt of catheter insertion was failed
in 3 patients who then underwent contralateral catheter placement. No
complications were noted during or immediately after the procedures. Late
complications included 8 cases of infection, 2 cases of fibrin sheath formation,
and 1 case of persistent hiccups, which began at the time of catheter insertion.
Inadvertent catheter removal was noted in 4 cases. CONCLUSION: Fluoroscopy-guided
central venous catheterization should be preferred over the anatomical landmark
technique due to its higher technical success rate, shorter procedure time, and
lower complication rate. When placing a central venous catheter, multiple factors
should be considered, such as catheter type, number of lumens, duration and
frequency of pertinent treatments, and patient needs. The procedural and early
post-procedural complications were mostly related to the placement technique;
however, the late complications could have been prevented by nurse care and
patient education.
PMID: 17160804 [PubMed - indexed for MEDLINE]
30: Crit Care. 2006;10(6):175.
Comment on:
Crit Care. 2006;10(6):R162.
Can you justify not using ultrasound guidance for central venous access?
Bodenham AR.
Department of Anaesthesia, Leeds General Infirmary, Leeds, LS1 3EX, UK.
Andy.Bodenham@leedsth.nhs.uk
Karakitsos and coworkers, in this journal, reported further compelling evidence
on the value of ultrasound in guiding internal jugular vein catheterization. In a
large, prospective, randomized study of 900 patients, comparisons were made
between patients in whom the procedure was performed using landmark-based
techniques and those assigned to ultrasound guidance. The key benefits from use
of ultrasound included reduction in needle puncture time, increased overall
success rate (100% versus 94%), reduction in carotid puncture (1% versus 11%),
reduction in carotid haematoma (0.4% versus 8.4%), reduction in haemothorax (0%
versus 1.7%), decreased pneumothorax (0% versus 2.4%) and reduction in
catheter-related infection (10% versus 16%). The implications of these findings
are discussed, and a compelling case for routine use of ultrasound to guide
central venous access is made.
Publication Types:
Comment
PMID: 17129362 [PubMed - indexed for MEDLINE]
31: Crit Care. 2006;10(6):R162.
Comment in:
Crit Care. 2006;10(6):175.
Real-time ultrasound-guided catheterisation of the internal jugular vein: a
prospective comparison with the landmark technique in critical care patients.
Karakitsos D, Labropoulos N, De Groot E, Patrianakos AP, Kouraklis G, Poularas J,
Samonis G, Tsoutsos DA, Konstadoulakis MM, Karabinis A.
Department of Intensive Care, General State Hospital of Athens, 154 Mesogeion
Avenue, 11527 Athens, Greece. echolabicu@gmail.com
INTRODUCTION: Central venous cannulation is crucial in the management of the
critical care patient. This study was designed to evaluate whether real-time
ultrasound-guided cannulation of the internal jugular vein is superior to the
standard landmark method. METHODS: In this randomised study, 450 critical care
patients who underwent real-time ultrasound-guided cannulation of the internal
jugular vein were prospectively compared with 450 critical care patients in whom
the landmark technique was used. Randomisation was performed by means of a
computer-generated random-numbers table, and patients were stratified with regard
to age, gender, and body mass index. RESULTS: There were no significant
differences in gender, age, body mass index, or side of cannulation (left or
right) or in the presence of risk factors for difficult venous cannulation such
as prior catheterisation, limited sites for access attempts, previous
difficulties during catheterisation, previous mechanical complication, known
vascular abnormality, untreated coagulopathy, skeletal deformity, and cannulation
during cardiac arrest between the two groups of patients. Furthermore, the
physicians who performed the procedures had comparable experience in the
placement of central venous catheters (p = non-significant). Cannulation of the
internal jugular vein was achieved in all patients by using ultrasound and in 425
of the patients (94.4%) by using the landmark technique (p < 0.001). Average
access time (skin to vein) and number of attempts were significantly reduced in
the ultrasound group of patients compared with the landmark group (p < 0.001). In
the landmark group, puncture of the carotid artery occurred in 10.6% of patients,
haematoma in 8.4%, haemothorax in 1.7%, pneumothorax in 2.4%, and central venous
catheter-associated blood stream infection in 16%, which were all significantly
increased compared with the ultrasound group (p < 0.001). CONCLUSION: The present
data suggest that ultrasound-guided catheterisation of the internal jugular vein
in critical care patients is superior to the landmark technique and therefore
should be the method of choice in these patients.
Publication Types:
Randomized Controlled Trial
PMID: 17112371 [PubMed - indexed for MEDLINE]
32: J Card Surg. 2006 Nov-Dec;21(6):553-8.
Hemodiafiltration during cardiac surgery in patients on chronic hemodialysis.
Fukumoto A, Yamagishi M, Doi K, Ogawa M, Inoue T, Hashimoto S, Yaku H.
Department of Cardiovascular and Thoracic Surgery, Graduate School of Medical
Science, Kyoto Prefectural University of Medicine, 465 Kaiji-cho,
Kawaramachi-Hirokoji, Kamigyo-ku, Kyoto 602-8566, Japan.
fukumoto@koto.kpu-m.ac.jp
BACKGROUND: We have developed a hemodiafiltration (HDF) protocol used during
cardiac surgery to preserve fluid and electrolyte balance and prevent
postoperative bleeding in patients on chronic hemodialysis. This retrospective
study examined the operative results associated with our new protocol. METHODS:
The study included 33 consecutive patients on long-term hemodialysis who
underwent cardiac surgery at our hospital between January 2001 and April 2005,
including off-pump coronary artery bypass grafting (CABG) in 19 patients.
Vascular access was achieved via a 12-French double-lumen catheter inserted into
the left femoral vein under general anesthesia, and HDF begun when the operation
was started. After completion of cardiopulmonary bypass or, in patients who
underwent off-pump CABG, after the distal anastomoses were completed, HDF was
continued until target hematocrit between 30% and 35%, central venous pressure
between 3 and 5 mmHg, and serum potassium concentration between 3.0 and 3.5 mEq/L
were reached. The chest was closed after confirmation of hemostasis. RESULTS:
There was no in-hospital death. Three patients were extubated in the operating
room. There were no postoperative wound infection, mediastinitis, respiratory
tract infection, or hemorrhage. The patients were discharged at a mean of 15.6
days after operation. CONCLUSIONS: These results suggest that intraoperative HDF
lowers postoperative morbidity and mortality in chronic dialysis patients. Other
advantages include early extubation and ambulation, and a shortened
hospitalization.
Publication Types:
Evaluation Studies
PMID: 17073952 [PubMed - indexed for MEDLINE]
33: Invest Radiol. 2006 Nov;41(11):777-80.
Evaluation of catheter loops in central venous port systems.
Behrendt FF, Wingen M, Katoh M, Guenther RW, Buecker A.
Department of Diagnostic Radiology, University Clinic of Aachen, Aachen, Germany.
behrendt@rad.rwth-aachen.de
OBJECTIVES: We sought to evaluate the cause for catheter loops of central venous
ports. MATERIAL AND METHODS: A total of 241 patients who received a central
venous port via subclavian vein access were included in this retrospective study.
Eighty of these patients had undergone a computed tomography of the chest,
allowing retrospective evaluation of the course of central venous catheters.
Complications were evaluated by review of the clinical data charts. RESULTS: In
49 patients, the catheter penetrated only the major pectoralis muscle. Only one
of these patients (2.0%) showed a loop. In 31 cases, the catheter went through
both the major and minor pectoralis muscle, and in 26 of these patients (83.9%),
a loop was seen. Complications after port implantation were catheter occlusion (n
= 2), pneumothorax (n = 2), thrombosis (n = 2), infection (n = 1), and catheter
dislocation (n = 1). CONCLUSIONS: The loop of catheter of central venous ports is
caused by catheter penetration through pectoralis major and minor.
Publication Types:
Evaluation Studies
PMID: 17035867 [PubMed - indexed for MEDLINE]
34: J Vasc Access. 2006 Jul-Sep;7(3):132-5.
Dislocation of central venous catheters in paediatric patients.
Giretti R, Caruselli M, Zannini R, de Vivo E, Piattellini G, Bechi P, Catani F,
Amici M, Santelli F, Pagni R.
Anesthesia and Intensive Care Unit, Ospedali Riuniti di Ancona, Presidio
Materno-Infantile G. Salesi, Ancona, Italy. robertogiretti@libero.it
Children have limited venous access possibilities; therefore, when long-term
therapy is necessary, it is better to place a catheter in a central vein. The
Port catheter, totally implanted, is less exposed to the risk of infection and
permits a normal life. However, there is the possibility of the displacement or
fragmentation of the catheter that can be diagnosed initially only by clinical
symptoms and later by a chest X-ray. We report a case of disconnection between
the Port catheter and the reservoir resulting in catheter migration to the left
pulmonary artery.
Publication Types:
Case Reports
PMID: 17019666 [PubMed - indexed for MEDLINE]
35: Korean J Intern Med. 2006 Sep;21(3):187-90.
Transluminal removal of a fractured and embolized indwelling central venous
catheter in the pulmonary artery.
Kim OK, Kim SH, Kim JB, Jeon WS, Jo SH, Lee JH, Ko JH.
Department of Internal Medicine, Kosin University Gospel Hospital, Busan, Korea.
Vascular catheters are associated with complications such as infection,
thrombosis and stenosis. The embolization of a venous catheter fragment is a rare
complication. A 39-year-old woman underwent placement of a totally implantable
venous access device for chemotherapy to treat a recurrent liposarcoma of the
left thigh. The "pinch-off sign" was noted on a routine chest X-ray but that was
ignored. Three-months after implantation of the intravenous access device, the
indwelling central catheter was fractured and embolized to the pulmonary trunk.
The catheter in the pulmonary trunk was successfully removed through a
percutaneous femoral vein approach using a pigtail catheter and goose neck snare.
Publication Types:
Case Reports
PMID: 17017669 [PubMed - indexed for MEDLINE]
36: Infect Control Hosp Epidemiol. 2006 Jul;27(7):662-9. Epub 2006 Jun 9.
Comment in:
Infect Control Hosp Epidemiol. 2007 Mar;28(3):370; author reply 370-1.
A multicenter intervention to prevent catheter-associated bloodstream infections.
Warren DK, Cosgrove SE, Diekema DJ, Zuccotti G, Climo MW, Bolon MK, Tokars JI,
Noskin GA, Wong ES, Sepkowitz KA, Herwaldt LA, Perl TM, Solomon SL, Fraser VJ;
Prevention Epicenter Program.
Department of Medicine, Washington University School of Medicine, Saint Louis, MO
63110, USA. dwarren@im.wustl.edu
BACKGROUND: Education-based interventions can reduce the incidence of
catheter-associated bloodstream infection. The generalizability of findings from
single-center studies is limited. OBJECTIVE: To assess the effect of a
multicenter intervention to prevent catheter-associated bloodstream infections.
DESIGN: An observational study with a planned intervention. SETTING: Twelve
intensive care units and 1 bone marrow transplantation unit at 6 academic medical
centers. PATIENTS: Patients admitted during the study period. INTERVENTION:
Updates of written policies, distribution of a 9-page self-study module with
accompanying pretest and posttest, didactic lectures, and incorporation into
practice of evidence-based guidelines regarding central venous catheter (CVC)
insertion and care. MEASUREMENTS: Standard data collection tools and definitions
were used to measure the process of care (ie, the proportion of nontunneled
catheters inserted into the femoral vein and the condition of the CVC insertion
site dressing for both tunneled and nontunneled catheters) and the incidence of
catheter-associated bloodstream infection. RESULTS: Between the preintervention
period and the postintervention period, the percentage of CVCs inserted into the
femoral vein decreased from 12.9% to 9.4% (relative ratio, 0.73; 95% confidence
interval [CI], 0.61-0.88); the total proportion of catheter insertion site
dressings properly dated increased from 26.6% to 34.4% (relative ratio, 1.29; 95%
CI, 1.17-1.42), and the overall rate of catheter-associated bloodstream
infections decreased from 11.2 to 8.9 infections per 1,000 catheter-days
(relative rate, 0.79; 95% CI, 0.67-0.93). The effect of the intervention varied
among individual units. CONCLUSIONS: An education-based intervention that uses
evidence-based practices can be successfully implemented in a diverse group of
medical and surgical units and reduce catheter-associated bloodstream infection
rates.
Publication Types:
Multicenter Study
Research Support, N.I.H., Extramural
Research Support, U.S. Gov't, P.H.S.
PMID: 16807839 [PubMed - indexed for MEDLINE]
37: Intensive Care Med. 2006 Sep;32(9):1449-50. Epub 2006 Jun 28.
The micro-organism responsible for central venous catheter related bloodstream
infection depends on catheter site.
Lorente L, Jiménez A, Iribarren JL, Jiménez JJ, Martín MM, Mora ML.
Publication Types:
Letter
PMID: 16804728 [PubMed - indexed for MEDLINE]
38: J Vasc Interv Radiol. 2006 May;17(5):823-9.
Use of the right external jugular vein as the preferred access site when the
right internal jugular vein is not usable.
Cho SK, Shin SW, Do YS, Park KB, Choo SW, Choo IW.
Department of Radiology, Samsung Medical Center, Sungkyunkwan University School
of Medicine, 50 Ilwon-dong, Kangnam-gu, Seoul 135-710, Korea.
PURPOSE: The present study describes the authors' experience with central venous
access through the right external jugular vein (EJV) when the right internal
jugular vein (IJV) is not available. MATERIALS AND METHODS: A retrospective study
of 23 patients in whom a central venous catheter placement was attempted via the
right EJV was conducted. The reasons for catheterization via the right EJV
included clinically silent occlusion of the right IJV (n = 17), localized skin
infection overlying the right IJV related to a previous catheterization (n = 3),
presence of an existing Hickman catheter in the right IJV (n = 1), and concern
regarding the risk of catheter-related infection secondary to right IJV
catheterization in patients with a tracheostomy tube device adjacent to the
presumed site of right IJV catheterization (n = 2). Technical success, procedural
complications, and follow-up results including catheter dwell time and delayed or
late complications (eg, symptomatic venous thrombosis, catheter-related
infection, and catheter malfunction) were assessed. Adverse events were expressed
as events per 100 catheter-days of use. RESULTS: Technical success was achieved
in 22 of 23 patients (96%). There were no procedural complications. The catheter
dwell time ranged from 2 to 182 days, with a mean dwell time of 62.7 days. There
were four delayed or late complications (three catheter-related infections, 0.22
per 100 catheter-days; one catheter malfunction, 0.07 per 100 catheter-days). No
cases of symptomatic venous thrombosis were noted. CONCLUSION: The right EJV is
an acceptable and preferred access site when the right IJV is not available for
central venous catheterization.
PMID: 16687748 [PubMed - indexed for MEDLINE]
39: Transplant Proc. 2006 Apr;38(3):707-10.
Use of catheters with the AgION antimicrobial system in kidney transplant
recipients to reduce infection risk.
Loertzer H, Soukup J, Hamza A, Wicht A, Rettkowski O, Koch E, Fornara P.
Department of Urology and Transplant Center of the Martin Luther University,
Halle, Germany. Hagen.Loertzer@medizin.uni-halle.de
Microbial blood infection represents a high risk for immuno-suppressed patients.
Of all catheter-related infections in the bloodstream, 90% result from the use of
central venous catheters, the main cause being microbial colonization at the
catheter's insertion point or the catheter hub. Between January 2003 and December
2004, 102 patients received a renal transplant including 57 who received a
triple-lumen central venous catheter (CVC) during the procedure. Two catheters
were used: a standard polyurethane catheter placed in the jugular veina or the
subclavian veina for group I, and polyurethane catheters with the AgION
antimicrobial system always placed in the subclavian veina for group II. Care and
maintenance of the CVCs was standardized in both groups. After catheter removal,
the tips were analyzed microbiologically. Of 57 (43.9%) CVCs, 25 were found to be
contaminated. In the first group 24 out of 41 CVCs (58.5%) showed bacterial
growth, whereas in group II only one catheter (6.6%) had a biofilm. The most
common contaminant (18 out of 25, 72%) was Staphylococcus epidermidis. In group
II, two patients had positive blood cultures yet a microbiologically sterile CVC.
None of the catheters with the AgION antimicrobial system had to be removed owing
to local infection or intolerance. The continuous release of silver ions
increases the protection against bacteria and fungi during the entire time of
catheterization. Use of catheters with the AgION antimicrobial system lead to a
marked reduction in catheter-associated infections of the bloodstream.
PMID: 16647450 [PubMed - indexed for MEDLINE]
40: Niger Postgrad Med J. 2006 Mar;13(1):26-30.
Internal jugular and subclavian catheterisation: indications, problems and
prospects in a Nigerian dialysis centre.
Arogundade FA, Sanusi AA, Badmus TA, Ibrahim A, Akinsola A.
Renal Unit, Department of Medicine, Obafemi Awolowo University, Ile-Ife, P. M. B
5538, Ile-Ife, Osun State, Nigeria.
AIMS AND OBJECTIVES: To highlight the indications, problems and prospects of
bedside non-surgically inserted jugular and subclavian dual lumen catheters.
PATIENTS AND METHODS: Renal failure patients being managed in our centre with
indications for central catheterisation were consecutively recruited at
presentation. They had bedside non-surgical jugular and subclavian insertion of
central catheters using modified Seldinger wire technique and the performance of
the catheters monitored. RESULTS: Sixteen patients aged between 23 and 65 years
had 32 central catheterizations during the 12-month period. The indications
included its use as haemodialysis access in all catheterisations, additional
indications were CVP monitoring in 5, and parenteral hyperalimentation in 1.
Three catheterisations were in right subclavian vein, 4 in left internal jugular
vein and 25 in right internal jugular vein. The duration of use ranged between 3
days and 11 weeks and blood flow rate used ranged between 250 and 350 mls/min.
Nine (28.1%) catheterisations were complicated with exit site and systemic
infection. Catheter blockage and accidental catheter removal were recorded in 3
patients each. Carotid artery puncture was recorded in 2 patients but haemostasis
was maintained with direct digital compression. CONCLUSION: We conclude that
percutaneous bedside internal jugular and subclavian (venous) catheterisation
using dual lumen catheter is safe and devoid of major complications.
PMID: 16633375 [PubMed - indexed for MEDLINE]
41: Am J Kidney Dis. 2006 May;47(5):879-87.
Catheter colonization in acute renal failure patients: comparison of central
venous and dialysis catheters.
Souweine B, Liotier J, Heng AE, Isnard M, Ackoundou-N'Guessan C, Deteix P, Traoré
O.
CHU Clermont-Ferrand, Service de Néphrologie Réanimation Médicale, Hôpital
Gabriel Montpied, Clermont-Ferrand, France. bsouweine@chu-clermontferrand.fr
BACKGROUND: Little is known about vascular access infections in patients with
acute renal failure. METHODS: We prospectively compared infection rates of
dialysis catheters (DCs) and central venous catheters (CVCs) in patients in the
intensive care unit treated with renal replacement therapy for acute renal
failure. The same insertion and maintenance procedures were used for CVCs and
DCs. To circumvent the allocation bias caused by severity of patient condition,
only patients with both types of catheters were included. RESULTS: A total of 150
CVCs and 130 DCs were analyzed in 99 patients with a mean Simplified Acute
Physiology Score II of 67 +/- 21. The major cause of acute renal failure was
sepsis (62%). Hospital mortality was 62%. Mean catheter duration was shorter for
DCs (6.7 +/- 4.4 days) than CVCs (7.8 +/- 4.9 days; P = 0.03). There was no
difference between CVCs and DCs in cumulative incidence of catheter colonization
(quantitative catheter cultures > or = 10(3) colony-forming units/mL; 4.7% versus
6.2%; P = 0.58) or incidence density of catheter colonization per 1,000 catheter
days (5.9 versus 9.1; P = 0.44, respectively). There also was no difference
between CVCs and DCs in cumulative incidence and incidence density regardless of
whether catheters were placed at the internal jugular (P = 0.34 and P = 0.23) or
femoral site (P = 0.57 and P = 0.80), respectively. Three cases of CVC-related
bacteremia (the same microorganism responsible for both catheter colonization and
blood culture result) were recorded, but none with DC use. CONCLUSION: When
severity of patient condition is controlled for, epidemiological characteristics
of colonization in CVCs and DCs are similar if similar infection control measures
are used for insertion and maintenance.
Publication Types:
Comparative Study
PMID: 16632028 [PubMed - indexed for MEDLINE]
42: J Vasc Access. 2004 Oct-Dec;5(4):174-8.
Complications and management of long-term central venous access catheters and
ports.
Yildizeli B, Laçin T, Batirel HF, Yüksel M.
Department of Thoracic Surgery, Faculty of Medicine, Marmara University Hospital,
Acibadem, Istanbul, Turkey.
PURPOSE: Although prolonged venous access devices (PVADs) are used in case
prolonged intravenous therapy is required, implantation and use of these devices
is associated with complications. The purpose of this study was to evaluate
perioperative and long-term complications associated with PVADs and the
management of these complications. METHODS: A retrospective review was undertaken
of 225 PVADs implanted in 217 patients from February 1993 to June 2004. This
included 144 single-lumen port infusion systems, 49 single-lumen Hickman
catheters and 32 double-lumen Groshong catheters. The PVADs were inserted using
either the percutaneous Seldinger method (n=183) or cutdown access to the
subclavian vein (n=42). Indications for placement were as follows: chemotherapy
in 66.2% of patients, drug-infusion treatment in 31.6% of patients and total
parenteral nutrition in 2.2% of patients. RESULTS: Perioperative complications
occurred in 13 patients (5.7%): catheter malposition in seven patients (3.1%),
pneumothorax in three patients (1.3%), hemorrhage in two patients (0.9%) and
catheter embolization in one patient (0.4%). Long-term complications appeared in
15 patients (6.6%): infection in five patients (2.2%), thrombosis in three
patients (1.3%), extravasation in three patients (1.3%), and catheter fracture in
four patients (1.8%). The fractured fragments were removed by the Amplatz snare
device. In 10 patients (4.4%) only were PVADs removed prior to completion of the
intended therapy. Indications for removal were catheter infection in five
patients (2.2%) and catheter fracture in five patients (2.2%). CONCLUSIONS: PVAD
implantation is associated with some risk of serious perioperative and long-term
complications. Care of the catheter and the patient should be maintained with the
proper and immediate evaluation of the perioperative and long-term complications.
PMID: 16596562 [PubMed]
43: J Vasc Access. 2004 Apr-Jun;5(2):49-56.
Salvage insertion of tunneled central venous catheters in the internal jugular
vein after accidental catheter removal.
Bellasi A, Brancaccio D, Maggioni M, Chiarelli G, Gallieni M.
Renal Unit, Azienda Ospedaliera San Paolo, Milan, Italy.
PURPOSE: Tunneled catheters are widely used for intermediate to long-term
hemodialysis (HD) access, but are prone to several complications that can require
catheter replacement. Replacing malfunctioning catheters with a new line, placed
in a different access site, can lead to problems with multiple vein occlusions.
This has led many nephrologists to continue using the same vein as long as
possible by guidewire catheter exchanges, to preserve other veins for future use.
We describe a guidewire exchange technique for the Ash-Split catheter in the
internal jugular vein. METHODS: In three patients, the exchange was performed
because of partial catheter removal, as evidenced by the outward dislocation of
the Dacron cuff. In these patients, the guidewire was inserted through the
catheter. In two additional patients, the catheter had been completely removed by
accident: the replacement of the dislodged tunneled venous catheters was
attempted 5 hr and 1 day after accidental removal. In these patients, the
guidewire was inserted through the previous tunnel. After guidewire placement, a
skin incision was made in the supraclavicular region. The metal guidewire was
easily located inside the fibrous structure that had previously surrounded the
catheter. The guidewire was then extracted from the subcutaneous tunnel and used
to insert a new catheter safely and easily after creating a new tunnel. Patients
were routinely given antibiotic prophylaxis (1 g of cefazolin) immediately before
the procedure. A strict aseptic technique was used, including several sterile
glove changes. RESULTS: No infections developed following this procedure, which
has the potential for bacterial contamination. All procedures were successful.
Only in one patient did we have to convert to a different catheter: it was not
possible to replace the old Ash-Split catheter with the same dual-lumen catheter
because of difficulties in inserting the peel away introducer-catheter complex.
In this patient, rather than forcing it with larger dilators or trying to disrupt
the fibrin sheath with balloon dilatation, a single lumen Tesio catheter was
successfully placed. In both patients who completely lost the previous catheter,
the guidewire was readily reinserted through the subcutaneous tunnel into the
vein. Catheter function was excellent in all patients, with a test blood flow
rate on the 1st catheter use >350 ml/min. CONCLUSIONS: We described a new method
for catheter exchange, which allows the easy insertion of a new catheter and the
creation of a new and safer subcutaneous tunnel. In addition, we demonstrated
that in cases of complete catheter removal, it is possible to reinsert a catheter
in the same vein through a guidewire, even when reinsertion was attempted up to 1
day later.
PMID: 16596541 [PubMed]
44: Support Care Cancer. 2006 Nov;14(11):1162-5. Epub 2006 Apr 5.
Implantation of central venous ports with catheter insertion via the right
internal jugular vein in oncology patients: single center experience.
Charvát J, Linke Z, Horáèková M, Prausová J.
Medical Department of 2nd Faculty of Medicine of Charles University and the Motol
Faculty Hospital, Prague, Czech Republic. jiri.charvat@lfmotol.cuni.cz
AIM OF WORK: Evaluation of suitability and safety of venous port implantation
with catheter insertion via the right internal jugular vein in oncology patients.
PATIENTS AND METHODS: One hundred one totally implantable venous ports were
placed in 100 patients with malignancies from January 1, 2003 until March 31,
2005. Catheter of venous port was preferably inserted via the right internal
jugular vein. We recorded a number of successful implantations using this venous
approach and the rate of complications during the procedure and follow-up. MAIN
RESULTS: Ninety-seven catheters (96%) of totally implantable venous ports were
inserted via the right internal jugular vein in 96 patients, and only in four
cases were we not able to access this vein. We had no complications related to
catheter insertion via the right internal jugular vein. Follow-up was made in all
96 patients with a total access days of 41 in 151 days (mean: 407 days).
Premature catheter removal was required in six (6.2%, 0.144 per 1,000 access
days) due to complications: three catheter dislocations/malfunctions (3.1%, 0.072
per 1,000 access days), one port-related sepsis, one pocket port infection, and
one decubitus over port (1%, 0.024 per 1,000 access days). Six venous ports were
removed after completion of the treatment at the patient's request. CONCLUSION:
The placement of totally implantable venous ports with catheter insertion via the
right internal jugular vein has a high success rate without any early
complications. Follow-up also demonstrates a low incidence of late complications
requiring port removal.
Publication Types:
Evaluation Studies
PMID: 16596418 [PubMed - indexed for MEDLINE]
45: Pediatr Blood Cancer. 2007 Dec;49(7):1034-6.
Multiple brain abscesses in a child with autoimmune hemolytic anemia.
Bay A, Yilmaz N, Nalbantoglu O, Yilmaz C, Etlik O, Faik Oner A.
Division of Hematology, Yuzuncu Yil University Faculty of Medicine, Van, Turkey.
bayalibay@yahoo.com
A 14-year-old female with autoimmune hemolytic anemia (AIHA) developed an acute
hemolytic crisis with acute renal failure under conventional treatment with
corticosteroids. Because of the life-threatening situation, we decided to start
pulse dose methylprednisolone and also hemodialysis with a femoral catheter
placement was performed. Fifteen days after initiating of dialysis subfebrile
fever was developed, followed within 2 days with a left hemiparesis. Brain
magnetic resonance imaging (MRI) revealed multiple intracerebral abscesses. The
clinical picture worsened and the patient died before scheduled surgery for the
abscesses. 2007 Wiley-Liss, Inc
Publication Types:
Case Reports
PMID: 16514615 [PubMed - indexed for MEDLINE]
46: Dermatology. 2006;212 Suppl 1:47-52.
Our method of povidone-iodine ointment and gauze dressings reduced
catheter-related infection in serious cases.
Fukunaga A, Naritaka H, Fukaya R, Tabuse M, Nakamura T.
Department of Neurosurgery, Keio University School of Medicine, Tokyo, Japan.
fukunaga@sc.itc.kei.ac.jp
In experiment 1, we evaluated our method of catheter care at subclavian vein
insertion sites for the control of catheter-related infections in seriously ill
neurosurgical patients who needed prolonged catheter placement, compared with an
older method. In our method, the insertion site was prepared with 10%
povidone-iodine solution, followed by application of 10% povidone-iodine
ointment, and covered with sterile gauze and a transparent polyurethane dressing.
The older method was based on 1996 guidelines for the prevention of intravascular
device-related infections. Catheter colonization and mortality were both found to
be significantly reduced with our method (p = 0.0214, p = 0.0379, respectively).
In experiment 2, we evaluated whether a regimen of catheter care with 10%
povidone-iodine ointment was more effective than that without povidone-iodine
ointment for the prevention of infections. This suggested effectiveness of 10%
povidone-iodine ointment for reduction of infection. Our method of catheter care
was useful even in seriously ill neurosurgical patients.
PMID: 16490975 [PubMed - indexed for MEDLINE]
47: Eur J Vasc Endovasc Surg. 2006 Jun;31(6):667-78. Epub 2006 Feb 3.
Iliofemoral deep vein thrombosis in childhood; developing a management protocol.
Brightwell RE, Osman IS.
Regional Vascular Unit, St Mary's Hospital, Praed Street, Paddington, London W2
1NY, UK. r.brightwell@imperial.ac.uk
OBJECTIVE: To develop an evidence-based protocol for the management of
iliofemoral deep vein thrombosis (IDVT) in childhood. METHODS: A search of the
literature was undertaken. All publications pertaining to IDVT in childhood were
analysed and then categorised according to their level of evidence.
Recommendations were then made on the basis of this. RESULTS: The commonest
presenting symptoms were pain and swelling in the affected limb (evidence level
II). Predisposing risk factors of special significance in children included the
recent use of a venous access device, malignancy, prothrombotic disorders,
infection, surgery and congenital venous anomalies (evidence level II). The most
frequently described imaging modalities were B-mode ultrasonography, duplex,
venography, and helical CT (evidence level III). The mainstay of treatment was
anticoagulation with LMWH alone or followed by warfarin (evidence level I). Early
clot removal through catheter-directed thrombolysis or surgical thrombectomy has
been shown to be beneficial (evidence level II/III). There is little evidence for
the benefit of early mobilisation and compression therapy in childhood.
CONCLUSION: Level I evidence relating to IDVT in childhood is sparse. The
possibility of IDVT should be considered when examining a child with a swollen
and painful limb. Imaging should be with duplex ultrasound, followed by spiral CT
to include assessment of the IVC. A thrombophilia screen should be taken prior to
anticoagulation with LMWH (and warfarin). Thrombolysis should be considered in
cases of extensive IDVT.
Publication Types:
Case Reports
Review
PMID: 16458548 [PubMed - indexed for MEDLINE]
48: JPEN J Parenter Enteral Nutr. 2006 Jan-Feb;30(1 Suppl):S7-12.
Anatomy and physiology of venous system vascular access: implications.
Grant JP.
Duke University Medical Center, Durham, North Carolina. 27710, USA.
Grant003@mc.duke.edu
Ideal characteristics for long-term vascular access that can be managed in the
home environment include a large vascular lumen in a high-flow blood system to
minimize risks of obstruction and phlebitis, ease of sterile dressing
maintenance, patient comfort, and longevity of the access site. Additionally,
adaptation to placement at the bedside or in the home, technical ease and safety
of placement, and minimal expense would be beneficial. With these considerations,
possible anatomical sites would include the external and internal jugular veins,
subclavian vein, cephalic vein, basilic vein, femoral vein, right atrial
appendage, and translumbar and transhepatic access to the inferior vena cava. Of
these, the internal jugular vein, subclavian vein, cephalic vein, basilic vein,
and femoral vein would seem best suited for long-term venous access.
Publication Types:
Review
PMID: 16387914 [PubMed - indexed for MEDLINE]
49: Kidney Int. 2005 Dec;68(6):2886-9.
Outcomes of tunneled femoral hemodialysis catheters: comparison with internal
jugular vein catheters.
Maya ID, Allon M.
Division of Nephrology, University of Alabama at Birmingham, Birmingham, AL
35233, USA.
BACKGROUND: Tunneled femoral vein dialysis catheters are used as a last resort
when all other options for a permanent vascular access or thoracic central vein
catheter have been exhausted. There is little published literature on the
complications or outcomes of tunneled femoral catheters. METHODS: Using a
prospective, computerized vascular access database, we identified all tunneled
femoral dialysis catheters placed at the University of Alabama at Birmingham
during a five-year period. The clinical features, catheter patency, and
complications in these patients were compared to those observed in a group of
sex-, age-, and date-matched control patients with tunneled internal jugular vein
dialysis catheters. RESULTS: During the study period, 27 patients received a
tunneled femoral dialysis catheter, accounting for 1.9% of all tunneled catheters
placed. Only 7 patients (26%) were able to convert to a new permanent dialysis
access. The primary catheter patency (time from placement to exchange) was
substantially shorter for femoral catheters than for internal jugular dialysis
catheters (median survival, 59 vs. >300 days, P < 0.0001). Infection-free
survival was similar for both groups (P= 0.66). Seven patients with femoral
catheters (or 26%) developed an ipsilateral deep vein thrombosis, but catheter
use was possible with anticoagulation. CONCLUSION: Tunneled femoral dialysis
catheters have a substantially shorter primary patency, but a similar risk of
catheter-related bacteremia, as compared with internal jugular vein catheters. An
ipsilateral lower extremity deep vein thrombosis occurs commonly after placement
of a femoral dialysis catheter, but does not preclude continued catheter use.
Publication Types:
Research Support, N.I.H., Extramural
PMID: 16316366 [PubMed - indexed for MEDLINE]
50: J Hosp Infect. 2006 Feb;62(2):207-13. Epub 2005 Nov 22.
Rate, risk factors and outcomes of catheter-related bloodstream infection in a
paediatric intensive care unit in Saudi Arabia.
Almuneef MA, Memish ZA, Balkhy HH, Hijazi O, Cunningham G, Francis C.
Department of Infection Prevention and Control, King Abdulaziz Medical City/King
Fahad National Guard Hospital, Riyadh, Saudi Arabia.
The aim of this study was to determine the rate, risk factors and outcomes of
catheter-related bloodstream infections (CRBSIs) in patients in a paediatric
intensive care unit (PICU). A prospective cohort study was performed in King
Abdulaziz Medical City, Riyadh, Saudi Arabia; a 650-bed academic/tertiary care
centre with a combined 10-bed medical and surgical PICU. All patients admitted to
the PICU from July 2000 to February 2003 who had a central line placed were
monitored for the development of bloodstream infection (BSI) from insertion until
48 h after removal. Four hundred and forty-six patients with 2493
central-line-days were documented; 273 (55%) were male and the mean age was 2.6
years. Of the 446 patients, 278 (56%) had congenital heart disease, 108 (22%) had
genetic disorders and/or congenital malformations, 55 (11%) had respiratory
disease, and 42 (8%) had trauma. There were 50 episodes of CRBSI in 46 patients
with a rate of 20.06 per 1,000 central-line-days and a device-utilization rate of
57%. Of these 50 episodes, 24 (48%) were polymicrobial, 16 (32%) were due to
Gram-negative organisms, five (10%) were due to Gram-positive organisms, and five
(10%) were fungal. The most common organisms isolated were Klebsiella pneumoniae
(N=12, 16%), coagulase-negative staphylococci (N=10, 14%) and Pseudomonas
aeruginosa (N=8, 11%). The mean duration of line insertion was 11.8 days for
CRBSI patients and 4.22 days for non-BSI patients (P<0.0001). The mean PICU stay
was 30.20 days for CRBSI patients and 6.35 days for non-BSI patients (P<0.0001).
BSI occurred more often in catheters inserted in the PICU compared with the
operating room, and in the femoral site compared with jugular or subclavian sites
(P<0.001). In multiple logistic regression analysis of the risk factors, CRBSI
patients were more likely to have multiple central lines [odds ratio (OR) 9.19;
95% confidence intervals (CI): 3.76-22.43), the line was more likely to be used
for total parenteral nutrition (OR: 8.69; 95% CI: 3.5-21.4), and guidewire
exchange was more likely to be performed on the line. CRBSI was not associated
with a higher mortality rate. The CRBSI rate in our hospital is high compared
with that reported by the National Nosocomial Infection Surveillance system. This
study has established a benchmark for future comparisons. Additional studies from
Saudi Arabia are necessary for national comparison and development of preventive
measures.
PMID: 16307822 [PubMed - indexed for MEDLINE]
51: Crit Care. 2005;9(6):R631-5. Epub 2005 Sep 28.
Central venous catheter-related infection in a prospective and observational
study of 2,595 catheters.
Lorente L, Henry C, Martín MM, Jiménez A, Mora ML.
Department of Intensive Care, Hospital Universitario de Canarias, La Laguna,
Santa Cruz de Tenerife, Spain. lorentemartin@msn.com
INTRODUCTION: Central venous catheterization is commonly used in critically ill
patients and may cause different complications, including infection. Although
there are many studies about CVC-related infection, very few have analyzed it in
detail. The objective of this study was to analyze the incidence of
catheter-related local infection (CRLI) and catheter-related bloodstream
infection (CRBSI) with central venous catheters (CVCs) according to different
access sites. METHODS: This is a prospective and observational study, conducted
in a 24-bed medical surgical intensive care unit of a 650-bed university
hospital. All consecutive patients admitted to the ICU during 3 years (1 May 2000
and 30 April 2003) were included. RESULTS: The study included 2,018 patients. The
number of CVCs and days of catheterization duration were: global, 2,595 and
18,999; subclavian, 917 and 8,239; jugular, 1,390 and 8,361; femoral, 288 and
2,399. CRLI incidence density was statistically higher for femoral than for
jugular (15.83 versus 7.65, p < 0.001) and subclavian (15.83 versus 1.57, p <
0.001) accesses, and higher for jugular than for subclavian access (7.65 versus
1.57, p < 0.001). CRBSI incidence density was statistically higher for femoral
than for jugular (8.34 versus 2.99, p = 0.002) and subclavian (8.34 versus 0.97,
p < 0.001) accesses, and higher for jugular than for subclavian access (2.99
versus 0.97, p = 0.005). CONCLUSION: Our results suggest that the order for
punction, to minimize the CVC-related infection risk, should be subclavian (first
order), jugular (second order) and femoral vein (third order).
Publication Types:
Comparative Study
PMID: 16280064 [PubMed - indexed for MEDLINE]
52: Thromb Res. 2006;118(4):439-45. Epub 2005 Oct 7.
Is guidewire exchange a better approach for subclavian vein re-catheterization
for chronic hemodialysis patients?
Hou SM, Chou PC, Huang CH, Chin CH, Wang PC, Chen YH.
Department of Cardiovascular Surgery, Cathay General Hospital, Taipei, Taiwan.
BACKGROUND: The objectives of this study were to compare outcomes and survival
rates of subclavian vein re-catheterization through guide wire exchange (GWE) or
de novo insertion (DN). MATERIALS AND METHODS: The study was conducted in a
retrospective manner. Medical records of 36 patients who received percutaneous
subclavian vein re-catheterization for hemodialysis in our institution during the
period from April 1, 2001 to September 30, 2004 were reviewed. All patients had
at least 2 catheter insertions records in our institute. Incidences of adverse
events (infection, thrombosis) were compared between GWE and DN groups using x2
test. Predictors for adverse event occurrences were analyzed using logistic
regression models. Cox proportional hazard model was used to investigate the
predictors for adverse event-free catheter days. Kaplan-Meire survival curves
were computed and compared using log rank test. RESULTS: Information were
generated from 98 catheters (41 from DN, 57 from GWE groups). The average
catheter usage was 2.8+/-0.9 devices per patient and the mean
catheter-indwelling-day was 125.4+/-129.5 days in this cohort. We found GWE group
had significantly lower thrombosis rate (49.1% vs. 85.4% for DN group, P<0.000)
in general. Surgical approach was a significant risk factors for catheter
thrombosis (GWE vs. DN, odds ratio=0.261, P=0.05). The actuarial survival rates
for GWE were > or =30 days, 85.4%; > or =60 days, 75.5%; > or =90 days, 64.5%; >
or =180 days, 44.3%. The actuarial survival rates for DN were > or =30 days,
70.7%; > or =60 days, 58.5%; > or =90 days, 34.2%; > or =180 days, 18.4%. GWE
group catheters had significantly higher catheter survival rates (P=0.0009).
Mahukar catheter (hazard ratio 0.514, P=0.03), non-shock (hazard ratio 3.358,
P=0.04), and older age (hazard ratio 0.958, P=0.026) were predictors of adverse
event-free remaining catheter days. CONCLUSION: We suggest that GWE might be a
favorable option over DN insertion when revised subclavian vein catheterization
is inevitable. GWE can be performed repeatedly without compromising catheter
outcomes.
PMID: 16214203 [PubMed - indexed for MEDLINE]
53: Transplant Proc. 2005 Sep;37(7):3171-3.
Internal jugular versus subclavian vein catheterization for central venous
catheterization in orthotopic liver transplantation.
Torgay A, Pirat A, Candan S, Zeyneloglu P, Arslan G, Haberal M.
Baskent University Faculty of Medicine, Department of Anesthesiology, Ankara,
Turkey. adnant@baskent-ank.edu.tr
The aim of this study was to compare incidence rates of mechanical and infectious
complications associated with central venous catheterization via the internal
jugular vein (IJV) versus the subclavian vein (SV) among 45 consecutive patients
undergoing orthotopic liver transplantation (OLT) between January 2000 and June
2004. The subjects were divided into two groups according to the site of central
venous catheterization (IJV or SV). We recorded each patient's physical
characteristics, international normalized ratio (INR), partial thromboplastin
time, platelet levels, number of puncture attempts, success/failure of central
venous catheterization, duration of catheter placement, occurrence of catheter
tip misplacement, arterial puncture, incidence of hematoma or pneumothorax,
catheter-related infection, or bacterial colonization of the catheter. Senior
staff anesthesiologists performed 22 SV and 23 IJV catheterizations for the 45
OLT procedures. The SV and IVJ groups both had minor coagulation abnormalities
with slightly increased INR values at the time of catheterization. There were no
significant differences between the groups with respect to success of central
venous catheterization (100% for both), numbers of attempted punctures, duration
of catheter placement, and incidence rates of mechanical and infectious
complications. Both groups showed high frequencies of catheter tip misplacement,
with right atrium as the site of misplacement in all cases. Two patients in the
IJV group (8.7%) developed hematomas after accidental carotid artery puncture.
The results suggest that, when performed by experienced anesthesiologists,
central venous catheterization via the SV is an acceptable alternative to IJV
catheterization for patients undergoing OLT.
Publication Types:
Clinical Trial
Comparative Study
Controlled Clinical Trial
PMID: 16213340 [PubMed - indexed for MEDLINE]
54: Can J Anaesth. 2005 Oct;52(8):801-4.
Broken guide wire--a fault of design?
Monaca E, Trojan S, Lynch J, Doehn M, Wappler F.
Department of Anesthesiology, Hospital Cologne-Merheim, University
Witten/Herdecke, Ostmerheimer Str. 200, D - 51109 Köln, Germany.
MonacaE@Kliniken-Koeln.de
PURPOSE: To report a potentially serious complication resulting from a faulty
guide wire during central venous catheterization. CLINICAL FEATURES: We report
breakage of a guide wire with potential severe implications for a 47-yr-old
critical care patient. The tip of the J-wire became lodged in the internal
jugular vein, and required fluoroscopic guidance for removal, which occurred
without complication. CONCLUSION: Breakage of a guide wire during central venous
catheter insertion has been very rarely reported. However, inherent faults in
design or in the manufacturing process of the guide wire could lead to this rare
complication. A simple bedside test is proposed to detect breakage in the core
section of the guide wire.
Publication Types:
Case Reports
PMID: 16189330 [PubMed - indexed for MEDLINE]
55: Minerva Anestesiol. 2005 Sep;71(9):555-60.
Central venous catheters. Observations on the implantation technique and its
complications.
Paoletti F, Ripani U, Antonelli M, Nicoletta G.
Pain therapy center, Division of Anesthesia, Analgesia and Intensive Care,
Department of Clinical and Experimental Medicine, University of Perugia, Italy.
The growing utilization of central venous catheterism is linked to the necessity
of treating with an always larger number of hospitalized and nonhospitalized
patients. The technological development provided us with different devices and
materials for specific indications. In the majority of cases the central venous
catheter is positioned through direct puncture of a central vein using Seldinger
method. The vessels used for the catheterism are: the internal jugular vein, the
subclavian vein and femoral vein. The choice of the vein to use is influenced by
the operator's experience and by factors depending on the patient. The internal
jugular vein via posterior or median and the subclavian vein via subclavicular
are the most used sites in the central venous catheterism. However, also the
femoral vein can be considered a resource when the clinical conditions of the
patient render problematic the positioning in the above mentioned sites. The
positioning into the internal jugular vein is generally burdened with a very low
risk of pneumothorax and other potentially dangerous complications for the
patient. The femoral vein is generally burdened with a larger incidence of
thrombosis and infections. The subclavian vein, even if it is the most used, is
burdened with a larger incidence of immediate or retarded pneumothorax and
accidental venous puncture. The most frequent immediate complications for
catheterism are the arterial puncture, pneumothorax, arrhythmias and the wrong
positioning. Among the late complications there are the catheter infections
correlated, catheter and vessel thrombosis. The use of a proper technique,
completed by the operator's experience and the right management of the device,
lead to a decrease of the risk level related to the central venous catheterism.
Publication Types:
Review
PMID: 16166917 [PubMed - indexed for MEDLINE]
56: Ann Vasc Surg. 2005 Sep;19(5):734-6.
Spontaneous migration of a Port-a-Cath catheter into ipsilateral jugular vein in
two patients with severe cough.
Wu PY, Yeh YC, Huang CH, Lau HP, Yeh HM.
Department of Anesthesiology, National Taiwan University Hospital, Taipei,
Taiwan.
Port-A-Cath systems are widely used for long-term therapy in the treatment of
malignancies and infection. Spontaneous migration of Port-A-Cath catheters after
satisfactory initial placement is uncommon but is associated with a number of
complications, including neck pain, shoulder pain, ear pain, infection, venous
thrombosis, and neurological complications. We describe two cases of migration of
the Port-A-Cath catheter into the ipsilateral internal jugular vein. Both
received surgical reposition of the catheter with a longer one. We speculate that
the migration is related to severe cough and vigorous changes of intrathoracic
pressure. We also review the literature regarding such unusual complications of
Port-A-Cath. Because catheter migration might be asymptomatic, monitoring the
catheter position bimonthly when not used is recommended. Before a new course of
chemotherapy or encountering symptoms of migration, obtaining a chest
roentgenogram is essential to provide early detection and repositioning
management of a migrated catheter.
Publication Types:
Case Reports
PMID: 16010503 [PubMed - indexed for MEDLINE]
57: Ther Apher Dial. 2005 Jun;9(3):250-3.
Temporary hemodialysis catheters as a long-term vascular access in chronic
hemodialysis patients.
Ponikvar R, Buturović-Ponikvar J.
Department of Nephrology, University Medical Center Ljubljana, University of
Ljubljana, Ljubljana, Slovenia. rafael.ponikvar@kclj.si
The objective was to review our experience with temporary, precurved, jugular
catheters used for long-term vascular access in chronic hemodialysis patients.
Thirty chronic hemodialysis patients, 14 men and 16 women, with an average age of
65.3 +/- 13.5 years (30-90 years), treated by dialysis for 1 month to 30 years
(average +/- SD, 6.3 +/- 8.1 years), had single lumen, 'temporary' precurved
non-tunneled jugular catheters placed into the right jugular vein as permanent
vascular access, with 4% trisodium citrate as a locking solution and mupirocin at
the exit site. Hemodialysis catheters were used for vascular access on average
for 9.1 +/- 6.5 months, (1-22.7 months), and for a total of 271.7 months (8151
days). Average catheter functioning time was 3.1 +/- 1.9 months (0.5-10 months).
The total number of side-effects was 55 (6.7/1000 catheter days), including 26
cases of thrombosis (3.2/1000 catheter days), 9 ruptures of the catheter
(1.1/1000 catheter days), 15 catheter malfunctions (1.8/1000 catheter days), 2
exit site infections (0.2/1000 catheter days), 2 bacteremias (0.2/1000 catheter
days), 1 avulsion of the catheter (0.1/1000 catheter days), and 2 catheters were
removed because an AV fistula was successfully used. In 21 patients single-needle
hemodialysis was performed, mean blood flow 251 +/- 16 mL/min (250-300), mean
Kt/V 0.96 +/- 0.16 (0.72-1.27) and in 9 patients double-needle hemodialysis was
performed (catheter and peripheral vein) with mean blood flow 252 +/- 14 mL/min
(200-300), mean Kt/V 1.63 +/- 0.25 (1.21-1.96). 'Temporary' jugular single lumen
non-tunneled hemodialysis catheters, with 4% citrate as locking solution and
mupirocin ointment at the exit site provided good long-term vascular access with
acceptable functioning time and low infection rate. The main reasons for catheter
exchange or removal were malfunction and mechanical damage of the catheter.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 15967000 [PubMed - indexed for MEDLINE]
58: Crit Care Med. 2005 Jun;33(6):1276-80.
Comment in:
Crit Care Med. 2005 Jun;33(6):1437-9.
1293.
Crit Care Med. 2006 Apr;34(4):1293; author reply
Prospective study of arterial and central venous catheter colonization and of
arterial- and central venous catheter-related bacteremia in intensive care units.
Traoré O, Liotier J, Souweine B.
Service d'Hygiène Hospitalière, Hôpital G. Montpied, Clermont-Ferrand, France.
OBJECTIVE: To compare the rates of positive quantitative culture (PQC) of
arterial catheter (AC) and central venous catheter (CVC) tips and of CVC- and
AC-related bacteremia in intensive care unit patients undergoing placement of
both ACs and CVCs. DESIGN: Prospective, descriptive survey. To control for a
difference in the severity of patients having an AC or CVC, only patients having
both an AC and a CVC were included. SETTING: An adult, nine-bed medical/surgical
intensive care unit at a university teaching hospital. SUBJECTS: The analysis
included 308 CVCs and 299 ACs inserted in 212 severely ill patients, with a mean
+/- sd Simplified Acute Physiology Score II of 52 +/- 22 and an intensive care
unit mortality of 33% (69 of 212). INTERVENTIONS: None. MEASUREMENTS AND MAIN
RESULTS: The same insertion and maintenance procedures were used for both types
of catheter. A PQC was defined by a catheter tip culture yielding >/=10(3) colony
forming units/mL. Catheter-related bacteremia was defined by a PQC and a blood
culture positive for the same microorganism. The cumulative incidence
(PQCs/number of catheters inserted) was 9.4% (29/308) for CVCs and 7.7% (23/299)
for ACs (p = .44). Incidence density (PQCs/1,000 catheter days) was 12.0 for CVCs
versus 9.3 for ACs. At the femoral site, there was no significant difference
between CVCs and ACs in the cumulative incidences and incidence densities of
PQCs. Two instances of catheter-related bacteremia were observed, one involving a
CVC and one involving an AC. CONCLUSIONS: Among severely ill patients with both
CVCs and ACs, the epidemiology of PQCs of CVCs and ACs is comparable when the
same infection control measures are used for the insertion and maintenance of
both types of catheters.
Publication Types:
Comparative Study
Research Support, Non-U.S. Gov't
PMID: 15942344 [PubMed - indexed for MEDLINE]
59: Artif Organs. 2005 May;29(5):399-405.
Survival and complications of indwelling venous catheters for permanent use in
hemodialysis patients.
Develter W, De Cubber A, Van Biesen W, Vanholder R, Lameire N.
Renal Division, Department of Internal Medicine, University Hospital Ghent,
Ghent, Belgium. wdevelter@skynet.be
BACKGROUND: The risk factors influencing the survival of indwelling central vein
catheters and their potential complications have not been assessed in depth and
on a large scale. METHODS: We investigated the general characteristics of 245
single lumen cuffed tunneled catheters and analyzed their survival by
Kaplan-Meier and Cox regression analysis. Risk factors for bacteremia and
thrombosis were assessed by logistic regression analysis. RESULTS: The incidence
of exit-site infection, tunnel infection, bacteremia and thrombotic events was
0.35, 0.25, 1.71, and 1.94/1000 catheter days, respectively. The mean survival
time per catheter was 276 days. After censoring for non catheter-related events
leading to the removal of the catheter (n = 245 with 120 catheters censored and
125 events), the mean survival time of the catheter appeared to be 615 +/- 67
days (95% CI of 483-747) and the median survival time 310 +/- 50 days (95% CI of
212-408). The localization of the catheter into the right internal jugular vein
results in significantly better survival as compared with other insertion sites
both in Kaplan-Meier (mean survival of 650 days compared to a mean survival of
519 days, P value < 0.009) and in Cox regression analysis (relative risk of
0.537, P value < 0.001). Localization of the catheter into the right internal
jugular vein seemed to increase the risk for bacteremia (relative risk of 1.798,
P value of 0.063). The use of anticoagulant agents was not protective for
thrombosis, although this might be due to lack of power (relative risk of 0.626,
P value of 0.141). CONCLUSION: We provide evidence of a mean survival in
long-term hemodialysis catheter close to 2 years with an acceptable complication
rate. If a long-term hemodialysis catheter is required, it is best placed in the
right internal jugular vein.
PMID: 15854216 [PubMed - indexed for MEDLINE]
60: Minerva Anestesiol. 2005 May;71(5):197-206.
Effect of different sterile barrier precautions and central venous catheter
dressing on the skin colonization around the insertion site.
[Article in English, Italian]
Carrer S, Bocchi A, Bortolotti M, Braga N, Gilli G, Candini M, Tartari S.
Anesthesia and Resuscitation Unit, San Luca Hospital, 45027 Trecenta, (Rovigo),
Italy.
AIM: The purpose of this prospective, randomized, controlled study was the
comparison of maximal sterile barrier (consisting of mask, cap, sterile gloves,
gown, large drape) vs control precautions (mask, cap, sterile gloves, small
drape) and of transparent polyurethan film vs gauze dressing for use on central
venous (CVC) nontunneled catheters, inserted via the jugular vein. Skin
colonization at the insertion site (defined by quantitative skin cultures
performed at the time of insertion and in days 2 and 5) was used as a primary
endpoint. Catheter tip colonization was also assessed through qualitative culture
and CVC related sepsis was defined by the isolation of the same organism from the
catheter tip and the blood, with clinical sepsis of no other apparent source.
METHODS: Eighty-two consecutive patients were enrolled, admitted to a mixed
medical-surgical ICU, aged 72+/-12 years, 58% male, SAPS II 42+/-13. One-hundred
and seven CVCs were studied (presenting 750 catheter in situ days); CVCs were in
place for a mean period of 6.9+/-4.7 days and 5 episodes of central
catheter-related bloodstream infection were detected (6.6 per 1000 catheter
days). RESULTS: A multiple logistic regression detected an increased risk of skin
colonization in male gender (OR=2.5) and control precautions (OR=3.4) and no
difference with regard to age, dressing and diagnostic group. CONCLUSIONS:
Maximal sterile barrier proved to be an effective and recommended practice.
However surveillance skin cultures revealed the common and changing nature of
colonization of skin at the insertion site.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 15834348 [PubMed - indexed for MEDLINE]
61: Nephrol Nurs J. 2005 Jan-Feb;32(1):41-50.
Incidence and influencing factors associated with exit site infections in
temporary catheters for hemodialysis and apheresis.
Young EJ, Contreras G, Robert NE, Vogt NJ, Courtney TM.
Vascular Therapy Division, Tyco Healthcare/Kendall, Mansfield, MA, USA.
The authors examined the incidence and influencing actors of exit site infections
(ESIs) in patients using dual and triple lumen dialysis catheters. The
prospective, randomized study was conducted at 11 centers. Data were analyzed on
473 patients randomized to receive 235 dual lumen catheters (DLCs) or 238 triple
lumen catheters (TLCs). RESULTS: ESIs occurred in 10 patients (2.1%). The number
of intertreat-ment uses (p = 0.006), total number of uses (p = 0.009), and
catheter placement duration (p = 0.03) were significantly associated with
incidence of ESI in both treatment groups. Although patients with TLCs had a
significantly higher inter-treatment use than patients with DLCs (p = .04), no
sgnificant difference in the incidence of ESI was found (p = 0.11). Diabetic
status and catheter insertion site were not found to be significantly related to
ESI ( p= 0.09 and p = 0.54, respectively), although a trend toward significance
was noted for diabetic status. CONCLUSIONS: Stringent exit site care by specially
trained staff and shorter catheter duration most likely contributed to the low
incidence of ESIs. Other influencing factors included numbers of inter-treatment
uses, total number of uses, and catheter placement duration.
Publication Types:
Clinical Trial
Comparative Study
Multicenter Study
Randomized Controlled Trial
PMID: 15787083 [PubMed - indexed for MEDLINE]
62: Vascular. 2004 Jul-Aug;12(4):256-62.
Totally subcutaneous hemodialysis access: experience with the LifeSite
Hemodialysis System.
Comerota AJ.
Jobst Vascular Center, Toledo, OH, USA. acomerota@jvc.org
The LifeSite Hemodialysis System (Vasca, Inc., Tewksbury, MA) is totally
subcutaneous, incorporating two silicone catheters positioned in the central
venous system and connected to a stainless steel-titanium valve implanted in a
subcutaneous pocket. A randomized trial and nonrandomized clinical experience
have demonstrated lower rates of infection and longer device survival when 70%
isopropyl alcohol is used as the antimicrobial solution with the LifeSite.
Internal jugular vein placement with positioning of the valve on the anterior
chest wall further improves results.
Publication Types:
Clinical Trial
Clinical Trial, Phase I
Clinical Trial, Phase II
Multicenter Study
Randomized Controlled Trial
PMID: 15704320 [PubMed - indexed for MEDLINE]
63: Crit Care Med. 2005 Jan;33(1):234-5.
Comment on:
Crit Care Med. 2005 Jan;33(1):13-20; discussion 234-5.
The femoral site as first choice for central venous access? Not so fast.
O'Grady NP, Dezfulian C.
Publication Types:
Comment
Comparative Study
Editorial
PMID: 15644678 [PubMed - indexed for MEDLINE]
64: Crit Care Med. 2005 Jan;33(1):13-20; discussion 234-5.
Comment in:
Crit Care Med. 2005 Jan;33(1):234-5.
The incidence of infectious complications of central venous catheters at the
subclavian, internal jugular, and femoral sites in an intensive care unit
population.
Deshpande KS, Hatem C, Ulrich HL, Currie BP, Aldrich TK, Bryan-Brown CW, Kvetan
V.
Montefiore Medical Center and the Jacobi Medical Center, The Albert Einstein
College of Medicine, USA.
OBJECTIVE: The objective was to assess the risk of central venous catheter
infection with respect to the site of insertion in an intensive care unit
population. The subclavian, internal jugular, and femoral sites were studied.
DESIGN: An epidemiologic, prospective, observational study. SETTING: The setting
is a well-functioning intensive care unit under a unified critical care medicine
division in a university teaching hospital. Critical care medicine attendings and
fellows covered on site 17 and 24 hrs per day, respectively. PATIENTS: Patients
were critically ill. All patients were triaged into the intensive care unit by
on-site critical care medicine fellows. INTERVENTIONS: None. MEASUREMENTS AND
MAIN RESULTS: In an intensive care unit population, we prospectively studied the
incidence of central venous catheter infection and colonization at the
subclavian, internal jugular, and femoral sites. The optimal insertion site for
each individual patient was selected by experienced intensive care physicians
(critical care medicine attendings and fellows). All of the operators were
proficient in inserting catheters at all three sites. Confounding factors were
eliminated; there were a limited number of experienced operators inserting the
catheters, a uniform protocol stressing strict sterile insertion was enforced,
and standardized continuous catheter care was provided by dedicated intensive
care nurses proficient in all aspects of central venous catheter care.Two groups
of patients were analyzed. Group 1 was patients with one catheter at one site,
and group 2 was patients with catheters at multiple sites. Group 1 was the
primary analysis, whereas group 2 was supporting.A total of 831 central venous
catheters and 4,735 catheter days in 657 patients were studied. The incidence of
catheter infection (4.01/1,000 catheter days, 2.29% catheters) and colonization
(5.07/1,000 catheter days, 2.89% catheters) was low overall.In group 1, the
incidence of infection was subclavian: 0.881 infections/1,000 catheter days
(0.45%), internal jugular: 0/1,000 (0%), and femoral: 2.98/1,000 (1.44%; p =
.2635). The incidence of colonization was subclavian: 0.881 colonization/1,000
catheter days (0.45%), internal jugular: 2.00/1,000 (1.05%), and femoral:
5.96/1,000 (2.88%, p = .1338). There was no statistically significant difference
in the incidence of infection and colonization or duration of catheters (p =
.8907) among the insertion sites.In group 2, there was also no statistically
significant difference in the incidence of infection and colonization among the
three insertion sites. CONCLUSION: In an intensive care unit population, the
incidence of central venous catheter infection and colonization is low overall
and, clinically and statistically, is not different at all three sites when
optimal insertion sites are selected, experienced operators insert the catheters,
strict sterile technique is present, and trained intensive care unit nursing
staff perform catheter care.
Publication Types:
Comparative Study
PMID: 15644643 [PubMed - indexed for MEDLINE]
65: Anesth Analg. 2004 Dec;99(6):1625-9, table of contents.
The anterior jugular venous system: variability and clinical impact.
Schummer W, Schummer C, Bredle D, Fröber R.
EDIC, Department of Anesthesiology and Intensive Care Medicine, Friedrich
Schiller-University of Jena, Erlanger Allee 103, 07747 Jena, Germany.
cwsm.schummer@gmx.de
The anterior jugular venous system, with its interconnections to the subclavian
and deep jugular veins, provides a collateral venous network across the midline
of the neck area, which is especially important in unilateral occlusion of an
innominate vein. We illustrate the variability of this system and its clinical
impact on catheterization by three cases of landmark-guided central venous
cannulation. Case 1: Cannulation of the left internal jugular vein with a central
venous catheter and of the left innominate vein (LIV) with a pulmonary artery
catheter resulted in correctly positioned catheter tips. However, these catheters
were actually not placed in the innominate vein but coursed through the jugular
venous arch. Case 2: Cannulation of the left subclavian vein was complicated by
resistance of guidewire advancement at 13 cm. Occlusion of the LIV and
enlargement of the jugular venous arch were present. Case 3: Insertion of a
pulmonary artery catheter and a central venous catheter through the LIV. The
pulmonary artery catheter was correctly placed. The tip of the central venous
catheter was mistakenly positioned in the left anterior jugular vein. We describe
the normal anatomy of the anterior jugular venous system and its role as a major
collateral. Correct placement of central venous catheters may be possible via the
anterior jugular venous system. Conversely, central venous catheters
malpositioned in the anterior jugular vein can increase the risk for
complications and should be removed.
Publication Types:
Case Reports
PMID: 15562044 [PubMed - indexed for MEDLINE]
66: Int J Artif Organs. 2004 Oct;27(10):848-54.
Temporary vascular catheters for hemodialysis: a 3-year prospective study.
Naumovic RT, Jovanovic DB, Djukanovic LJ.
Clinic of Nephrology, Institute of Urology and Nephrology, Clinical Center of
Serbia, Belgrade - Serbia and Montenegro. rnaumovic@drenik.net
BACKGROUND: Temporary hemodialysis catheters are necessary in patients with
uremia, but complications associated with these catheters represent one of the
most important sources of morbidity among ESRD patients. There is no general
agreement about the optimal venous access for insertion of a central venous
catheter, while risk factors of catheter related complications have not been
entirely elucidated. METHODS: One hundred and seven consecutive patients who
required a temporary hemodialysis catheter were prospectively examined. RESULTS:
Catheters were placed in 107 consecutive patients (66 right jugular (JC), 41
right femoral (FC)) and maintained in situ for a cumulative total of 2101 days.
Early complications (puncture site hemorrhage, hematoma formation, artery
puncture) were infrequent, without clinical sequelae. The main late complication
was catheter related bacteremia (CRB). There were 16 episodes of CRB (JC-10;
FC-6) and Staphylococcus aureus was the most frequently isolated cause of CRB.
The mean catheter duration before the onset of CRB was 19.9 and 18.2 days for JC
and FC, respectively. Duration of catheter use, and the number of hemodialyses
significantly increased the risk for CRB. Actuarial survival for FC was
significantly worse than for JC, while Cox proportional hazard models revealed
that the femoral site, chronic renal failure and kidney transplantation increased
the risk of catheter failure significantly. CONCLUSION: CRB was the most common
late complication. Its frequency was similar in JC and FC. The main risk factors
for development of CRB were duration of catheter use and the number of performed
dialyses. Cumulative hazard of CRB was significantly magnified 3 weeks after
insertion for both JC and FC, but actuarial survival with JC was significantly
longer.
PMID: 15560679 [PubMed - indexed for MEDLINE]
67: Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004 Oct;98(4):418-22.
Relationship between oral bacteria and hemodialysis access infection.
Shariff G, Brennan MT, Louise Kent M, Fox PC, Weinrib D, Burgess P, Lockhart PB.
Department of Oral Medicine, Carolinas Medical Center, Charlotte, NC, USA.
galib.shariff@calgaryhealthregion.ca
OBJECTIVE: Controversy exists concerning the association between oral bacteria
and infection of hemodialysis (HD) shunts. The purpose of this study was to
determine the extent to which oral bacteria are associated with vascular access
site infections in a group of HD patients. STUDY DESIGN: Microbial blood culture
data for 87 HD patients were collected: 53 via chart review (retrospective), and
34 with newly suspected vascular access infections (prospective). The primary
outcome was the nature (i.e., species) of the bacteria recovered from blood
cultures of subjects with vascular access infection, specifically those bacteria
considered to be oral flora. RESULTS: The predominant bacteria reported to cause
HD vascular access infections were Staphylococcus (48.6%) and Enterococcus
(17.6%) species. Most infections occurred in hemodialysis catheters (89%)
compared with AV grafts (11%) and AV fistulas (0%). The subclavian venous access
(41%) and the internal jugular venous access (38.9%) were more commonly infected
than other sites. None of the bacteria identified by blood cultures were
considered to be oral flora. CONCLUSION: The results suggest that oral bacteria
rarely, if ever, cause vascular access infections in hemodialysis patients.
PMID: 15472656 [PubMed - indexed for MEDLINE]
68: Eur J Surg Oncol. 2004 Sep;30(7):771-5.
Totally implantable femoral vein catheters in cancer patients.
Wolosker N, Yazbek G, Munia MA, Zerati AE, Langer M, Nishinari K.
Department of Vascular Surgery, Hospital do Câncer A.C. Camargo, São Paulo,
Brazil. nwolosker@yahoo.com.br
INTRODUCTION: Totally implantable devices are increasingly being utilized for
chemotherapy treatment of oncological patients. When it is impossible to implant
the reservoir on the anterior wall of the thorax, or when there is an obstruction
of the superior vena cava system, alternative access routes must be sought. Of
these, the femoral vein is the most utilized. Few studies have been performed to
analyse the results obtained from the implantation and utilization of such
catheters in the femoral vein. The goal of this work was to prospectively study
the results obtained from the implantation of 20 TIC in femoral veins in a
large-sized cancer hospital with its own dedicated vascular clinical team.
MATERIAL AND METHODS: Twenty femoral TIC were inserted in 20 patients out of a
group of 560 cancer patients submitted to TIC implantation for chemotherapy.
Evaluations were made of the early and late-stage complications and patient
evolution until removal of the device, death or the end of the treatment.
RESULTS: The prospective analysis showed a mean duration of 215 days for the
catheters. There were 16 patients with no complications. There were no early
complications. Among the late complications, three were infections, representing
0.69/1000 days of catheter use, and one was a deep vein thrombosis (0.23/1000
days of catheter use). One catheter was removed due to primary bacteremia and one
due to subcutaneous pocket infection. Fourteen patients died while the catheter
was functioning and four patients are still making use of the catheter.
CONCLUSION: The low rate of complications implying catheter loss in this study
confirms the safety and convenience of the use of femoral TIC in patients who
cannot be submitted to implantation in the superior vena cava system.
Publication Types:
Evaluation Studies
PMID: 15296992 [PubMed - indexed for MEDLINE]
69: Br J Nurs. 2004 Jul 22-Aug 11;13(14):862-70.
Central venous catheters: choosing the most appropriate access route.
Hamilton H.
Oxford Radcliffe Hospitals NHS Trust.
Intravenous therapy and care is a complex and intricate area of practice, which
is being subsumed into the core role of registered nurses. As more patients
become recipients of a vascular access device (VAD), particularly those requiring
intermediate to long-term central venous access, it is important to ensure that
not only the device but also the most appropriate vein meets their clinical
physiological and psychological needs. There is much research and literature on
the insertion and care of central venous catheters (CVCs) as well as the
detection and treatment of complications. However, apart from a few small studies
comparing the performance of devices placed either in the subclavian or jugular
veins, there is little to guide doctors or nurses as to which vein is preferable,
if secondary complications are to be avoided. This article will describe a number
of primary and secondary complications associated with both the subclavian and
internal jugular veins and how these can be minimized by selecting the most
appropriate vessel. The article concludes with the author's suggestions for
correct patient assessment in order that the correct vein is utilized.
Publication Types:
Review
PMID: 15284651 [PubMed - indexed for MEDLINE]
70: Artif Organs. 2004 Aug;28(8):728-33.
Right versus left internal jugular vein catheterization for hemodialysis:
complications and impact on ipsilateral access creation.
Salgado OJ, Urdaneta B, Colmenares B, García R, Flores C.
Center of Experimental Surgery and Medicine, University of Zulia, Maracaibo,
Venezuela. ojsalg@hotmail.com
This study investigated whether the anatomical differences between right and left
internal jugular vein catheterization (RJVC and LJVC) would lead to differences
in the frequency of complications, in particular, central vein occlusion (CVO). A
group of 479 jugular vein catheterizations, 403 RJVC and 77 LJVC done in 294
prevalent hemodialysis patients were analyzed. A right-sided carotid
pseudoaneurysm was the only major puncture-related complication. A total of 78
RJVC and 17 LJVC were inserted more than once in the same position. Of the RJVC,
44 (10.9%) of 403 were removed because of infection compared with 16 (20.8%) of
77 LJVC (P < 0.02). The overall incidence of infections was 1.58 episodes of
infection per 1000 catheter days, 1.57 for RJVC and 3.72 for LJVC, respectively.
Catheter dwell times were not different. A group of 127 patients with former RJVC
and 44 with LJVC had ipsilateral arteriovenous access (RJVC+ and LJVC+ group,
respectively). Four diabetic LJVC+ developed severe arm swelling secondary to CVO
leading ultimately to access ligation. The RJVC+ group had no access ligated.
LJVC may cause CVO in diabetics.
Publication Types:
Comparative Study
Research Support, Non-U.S. Gov't
PMID: 15270954 [PubMed - indexed for MEDLINE]
71: Niger Postgrad Med J. 2004 Mar;11(1):58-63.
Patterns of presentation and mortality in tetanus: a 10-year retrospective
review.
Arogundade FA, Bello IS, Kuteyi EA, Akinsola A.
Department of Medicine, Obafemi Awolowo University, Ile-Ife, Osun State, Nigeria.
AIMS AND OBJECTIVES: To highlight the indications, problems and prospects of
bedside non-surgically inserted jugular and subclavian dual luman catheters.
PATIENTS AND METHODS: Renal failure patients being managed in our centre with
indications for central catheterisation were consecutively recruited at
presentation. They had bedside non-surgical jugular and subclavian insertion
using modified seldinger wire technique and the performance of the Gatheters
monitored. RESULTS: Sixteen patients aged between 23 and 65 years had 32 central
catheterisations during the 12-month period. The indications included its use as
haemodialysis access in all patients, additional indications were CVP monitoring
in 5, and parenteral hyperalimentation in 1. Three catheterisations were in right
subclavian vein, 4 in let internal jugular vein and 25 in right internal jugular
vein. The duration of use ranged between 3 days and 11 weeks and blood flow rate
used ranged between 50 and 350ml/min. Nine (28.1%) catheterisations were
complicated with exit site and systemic infection. Catheter blockage and
accidental catheter removal were recorded in 3 patients each. Carotid artery
puncture was recorded in 2 patients but haemostasis was maintained with direct
digital compression. CONCLUSION: We conclude that percutaneous bedside internal
jugular and subclavian (venous) catheterisation using dual lumen catheter is safe
and devoid of major complications. BACKGROUND: Tetanus, an ubiquitous disease
still ravages our population despite the fact that it is totally preventable. The
mortality had remained high with its attendant socio-economic implications as it
affects mainly farmers in their prime of life. We conducted this retrospective
review to be able to determine pattern of presentation, case fatality rate and
factors influencing mortality with a view to mapping out control strategies.
PATIENTS, MATERIALS AND METHODS: The case records of all managed patients aged 16
and above over a ten-year period (1992-2001) were retrieved and socio-demographic
and clinical data as well as results of laboratory investigations were collated.
Analysis was done using SPSS package. Chi-square analysis and student t-test were
used for comparison of means as appropriate. P-values of <0. 05 was taken as
significant. RESULTS: There were a total of 114 patients managed during the
period, which comprised of 85 males and 29 females. The means age (+/- SD) was
35.96 (+/-17.76). Sixty six (57.89%) patients are either jobless or farmers.
Majority of the patients had injuries in the lower limb 59.65% when compared with
20.18% that had theirs in the upper limb. 107 (93.86%) of the patients presented
with trismus while only 82 (71.93%) had opsthotonus. Only 51 (44.73%) patients
survived while 61 (53.5%) died. The mean age (+/- SD) of the survivors was 32.35
(+ 14.45) years while that of those that died was 39.4 (+/- 19.89) years (P =
0.036). Other factors that significantly influenced survival included severity of
spasms (P = 0/003), tachycardia (P = 0.044), and degree of sedation (P <0.0001).
No association was found between survival and incubation period, period of onset,
site of injury and associated medical conditions. CONCLUSIONS: Tetanus is still
associated with high mortality rate. Factors such as severity of spasma, age,
sedation and tachycardia were found to significantly influence mortality. It is
recommended that prophylactic life immunisation against tetanus be given to all
Nigerians.
PMID: 15254574 [PubMed - indexed for MEDLINE]
72: Semin Dial. 2004 Jul-Aug;17(4):307-9.
An alternative approach to the central circulation from above the diaphragm.
Ross J.
Department of Nephrology, Ochsner Clinic Foundation, New Orleans, Louisiana
70121, USA. Jross@ochsner.org
This is a review of a new fluoroscopically guided safe technique to place
tunneled cuffed hemodialysis (HD) catheters via the supraclavicular location.
Right supraclavicular catheters were placed in 12 patients who had no patent
internal jugular veins. The placements were all successful and without serious
complications. Over the 2 years of follow-up, two episodes of thrombosis/stenosis
(16.7%) resulted in catheter removal. The rate of infection was 8%, or one
episode in 1204 patient-days. The average length of use was 111 days. The average
rate of blood flow was 354 cc/min. The right supraclavicular approach for
tunneled HD catheters is safe and compares favorably to the internal jugular
approach for patients with limited access options.
PMID: 15250924 [PubMed - indexed for MEDLINE]
73: Eur Radiol. 2004 Nov;14(11):2015-9. Epub 2004 Jul 13.
Radiological placement of chest ports in pediatric oncology patients.
Cil BE.
Department of Radiology, Hacettepe University School of Medicine, Ankara, Turkey.
barbaros@hacettepe.edu.tr
A single center's procedural and follow-up results of radiological chest port
placement in pediatric oncology patients are presented. Between July 2002 and
December 2003, 37 children (20 boys, 17 girls; age range, 4 months to 16 years;
mean 6.7 years) underwent chest port placement. All patients received only one
port through the internal jugular vein access, and all of the implantations were
performed in the interventional radiology suite. Our database and electronic
charts were retrospectively reviewed to obtain follow-up data. All chest ports
were successfully implanted. The mean catheter life was 223 days (range: 15-450
days), with a total of 8,258 catheter days. Twenty-eight ports are still in use,
four patient deceased, one port was prematurely removed because of a late
infection, and four patients were lost to follow-up. Infection rate was 2.7%
(0.12/1,000 catheter days). Malfunction due to partial catheter thrombosis and
fibrin sheath formation was observed in three patients (8.1% or 0.36/1,000
catheter days), and all were relieved with rt-TPA dwell. None of the ports were
revised or removed because of blockage, malposition or difficulty accessing the
port. The peri-procedural complication rate was 0%. Chest ports in children can
be inserted in interventional radiology suites under imaging guidance with high
rates of technical success. The rates of infection and complications are
comparable to that of surgically placed ports.
PMID: 15249980 [PubMed - indexed for MEDLINE]
74: Intensive Care Med. 2004 Aug;30(8):1681-4. Epub 2004 May 25.
Catheter-related infection in critically ill patients.
Lorente L, Villegas J, Martín MM, Jiménez A, Mora ML.
Department of Intensive Care, Hospital Universitario de Canarias, Ofra s/n La
Cuesta, 38320 La Laguna, Santa Cruz de Tenerife, Spain. lorentemartin@msn.com
OBJECTIVE: To describe the incidence of the catheter-related local infection
(CRLI) and catheter-related bloodstream infection (CRBSI) of central venous
catheters (CVCs) and arterial catheters (ACs). DESIGN: Prospective, observational
study. SETTING: A 24-bed medical-surgical intensive care unit of a 650-bed
university hospital. PATIENTS: We included 988 consecutive patients admitted to
the ICU during 18 months. MEASUREMENTS: The incidence density of CRLI and CRBSI,
per 1000 catheter-days, of CVC and AC. RESULTS: Central venous catheters had a
significantly higher incidence density of CRLI (4.74 vs 0.97/1,000 catheter-days;
p<0.001) than ACs. Femoral venous access had a higher incidence density of CRLI
than subclavian (13.15 vs 1.81/1,000 catheter-days, p=0.003) and than peripheral
access (13.15 vs 2.30/1,000 catheter-days, p<0.001). Jugular venous access had a
higher incidence density of CRLI (6.29 vs 1.81/1,000 catheter-days, p<0.001) than
subclavian access. We found no significant differences in the incidence density
of CRLI and CRBSI between the different AC accesses. CONCLUSIONS: In the CDC
guidelines, catheter insertion at the subclavian site is recommended in
preference to femoral and jugular accesses, and there is no recommendation about
AC site insertion. Our data support these recommendations about CVCs. Because the
AC infection rate was very low, our study suggests that the access site is
probably not of major importance for this type of catheter.
PMID: 15160239 [PubMed - indexed for MEDLINE]
75: Aust Vet J. 2003 Mar;81(3):136-9.
Catheters: a review of the selection, utilisation and complications of catheters
for peripheral venous access.
Tan RH, Dart AJ, Dowling BA.
University Veterinary Centre Camden, The University of Sydney, 410 Werombi Road,
Camden, New South Wales 2570.
Intravenous catheters are used for the administration of medications and fluids
and are an integral part of veterinary practice. The aim of catheter use is to
optimise administration of medication and minimise complications such as thrombus
formation, thrombophlebitis and sepsis. Catheters made from teflon are less
flexible, less durable and stimulate more tissue reaction than polyurethane or
silicon. However silicon catheters are more expensive and complicated to insert.
Generally, for veterinary practice, the biostability and cost of polyurethane
catheters make them preferable for short and long-term use. The smallest diameter
catheter should be selected to minimise internal vessel wall contact and
irritation without compromising medication delivery. The site of insertion varies
with individual preference, vessel access and patient compliance. The jugular,
cephalic, saphenous, ear, lateral thoracic and subcutaneous abdominal veins are
accessible. Hair removal and a thorough aseptic skin preparation should be
performed prior to catheter insertion. Daily maintenance is required to detect
complications and maximise catheter longevity. Potential complications include
thrombus formation, thromboembolism, bacterial colonisation and septicaemia,
blood loss and air embolism. Permanent or transient skin dwelling bacteria are
commonly isolated if sepsis occurs. The development of novel antiseptic and
antibiotic impregnated catheters may reduce the complications associated with
catheter infection in the future.
Publication Types:
Review
PMID: 15080425 [PubMed - indexed for MEDLINE]
76: Intensive Care Med. 2004 May;30(5):837-43. Epub 2004 Apr 2.
Prevention of intravascular catheter-related infection with newer
chlorhexidine-silver sulfadiazine-coated catheters: a randomized controlled
trial.
Brun-Buisson C, Doyon F, Sollet JP, Cochard JF, Cohen Y, Nitenberg G.
Réanimation Médicale, Hôpital Henri Mondor (AP-HP), Av du Maréchal de Lattre de
Tassigny, 94010 Créteil Cedex, France. christian.brun-buisson@hmn.ap-hop-paris.fr
BACKGROUND: The indication of antiseptic-coated catheters remains debated.
OBJECTIVE: To test the ability of the new generation of chlorhexidine-silver and
sulfadiazine-coated catheters, with enhanced antiseptic coating, to reduce the
risk of central venous catheter (CVC)-related infection in ICU patients. DESIGN:
Multicentre randomized double-blind trial. PATIENTS AND SETTING: A total of 397
patients from 14 ICUs of university hospitals in France. INTERVENTION: Patients
were randomized to receive an antiseptic-coated catheter (ACC) or a standard
non-coated catheter (NCC). MEASUREMENTS: Incidence of CVC-related infection.
RESULTS: Of 367 patients having a successful catheter insertion, 363 were
analysed (175 NCC and 188 ACC). Patients had one (NCC=162, ACC=180) or more
(NCC=13, ACC=11) CVC inserted. The two groups were similar for insertion site
[subclavian (64 vs 69)] or jugular (36 vs 31%)], and type of catheters
(single-lumen 18 vs 18%; double-lumen 82 vs 82%), and mean (median) duration of
catheterisation [12.0+/-11.7 (9) vs 10.5+/-8.8 (8) days in the NCC and ACC
groups, respectively]. Significant colonisation of the catheter occurred in 23
(13.1%) and 7 (3.7%) patients, respectively, in the NCC and ACC groups (11 vs 3.6
per 1000 catheter-days; p=0.01); CVC-related infection (bloodstream infection)
occurred in 10 (5) and 4 (3) patients in the NCC and CC groups, respectively (5.2
vs 2 per 1000 catheter days; p=0.10). CONCLUSIONS: In the context of a low
baseline infection rate, ACC were associated with a significant reduction of
catheter colonisation and a trend to reduction of infection episodes, but not of
bloodstream infection.
Publication Types:
Clinical Trial
Multicenter Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 15060765 [PubMed - indexed for MEDLINE]
77: Nephron Clin Pract. 2004;96(2):c43-7.
Risk factors of nontunneled noncuffed hemodialysis catheter malfunction. A
prospective study.
Hryszko T, Brzosko S, Mazerska M, Malyszko J, Mysliwiec M.
Department of Nephrology and Internal Medicine, Medical University of Bialystok,
Bialystok, Poland. tomhry@poczta.onet.pl
BACKGROUND: The use of noncuffed nontunneled central venous catheters is a widely
accepted method of gaining temporary vascular access for hemodialysis.
Malfunction and bacteremia are the main factors limiting catheter survival.
METHODS: We followed up prospectively 73 hemodialysis catheters (HC) (40 internal
jugular, 33 femoral) in order to establish factors influencing HC malfunction. HC
malfunction was defined as a catheter that was unable to attain and maintain
blood flows of at least 150 ml/min. 73 HC were used for a total 1,100 days.
RESULTS: HC malfunction occurred in 23 cases (31.51%) during the study period,
giving an overall rate of 21 episodes per 1,000 catheter days at risk. An
analysis revealed a higher risk of HC malfunction with the catheterization of the
femoral vein compared to the internal jugular vein (hazard ratio (HR) 6.3; 95%
confidence interval (CI) 5.3-7.3). After correction for confounding factors in
multivariate Cox analysis, the site of the catheterization remained a
statistically significant predictor of HC malfunction (HR 5.03, 95% CI
3.83-6.23). After the first week malfunction rate was 42 and 8% for femoral and
internal jugular site, respectively (relative risk (RR) for malfunction 5.3 (95%
CI, 2.5-8). After the second and third week, the incidence of malfunction was 51
and 14% for femoral and internal jugular vein, respectively (RR 3.6, 95% CI
2.2-5.1). CONCLUSIONS: Catheterization of the internal jugular vein is associated
with longer catheter survival when compared to the femoral vein. Hemodialysis
catheters should be placed, if possible, in internal jugular vein to prevent
their premature malfunction. Copyright 2004 S. Karger AG, Basel
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 14988597 [PubMed - indexed for MEDLINE]
78: Ann Oncol. 2004 Feb;15(2):296-300.
Use of totally implantable central venous access ports for high-dose chemotherapy
and peripheral blood stem cell transplantation: results of a monocentre series of
376 patients.
Biffi R, Pozzi S, Agazzi A, Pace U, Floridi A, Cenciarelli S, Peveri V, Cocquio
A, Andreoni B, Martinelli G.
Division of General Surgery, European Institute of Oncology, Milan, Italy.
roberto.biffi@ieo.it
BACKGROUND: The complication rate of central venous totally implantable access
ports (TIAP), used for high-dose chemotherapy with autologous stem cell
transplantation support, has not been fully investigated to date, due to the
almost exclusive use of externalised, tunnelled devices in this clinical setting.
PATIENTS AND METHODS: During a 66-month period (from 1 January 1997 to 30 June
2002), 376 patients suffering from breast cancer, ovarian cancer, lymphoma or
multiple myeloma were treated with high-dose chemotherapy and autologous stem
cell transplantation at the European Institute of Oncology (Milan, Italy). A
single type of port was used, constructed from titanium and silicone rubber,
connected to a 7.8 F polyurethane catheter (Port-A-Cath; SIMS Deltec, Inc., St
Paul, MN, USA) inserted into the subclavian vein. They were followed
prospectively for device-related complications until the device was removed, the
patient died or the study was closed (30 June 2002). RESULTS: No TIAP-related
deaths were observed in this series. Seven pneumothoraxes (1.8%) occurred as a
complication of TIAP placement, one patient only (0.2%) requiring a tube
thoracostomy. Port pocket infection occurred twice in this series (0.53%, 0.01
episodes/1000 days of use), whereas three patients suffered from port-related
bacteraemia (0.8%, 0.016/1000 days of use). Infections were successfully treated
with antibiotics; all three cases had the ports removed at programme completion.
Four cases of deep vein thrombosis were detected (1.06%, 0.022/1000 days of use);
low molecular weight heparin was given, followed by oral anticoagulants. Finally,
one case of extravasation occurred (0.26%, 0.005/1000 days of use), requiring
port removal and local medical therapy. CONCLUSIONS: The use of TIAPs has
resulted in a safe and effective option for high-dose chemotherapy deliverance
and stem cell transplantation, in spite of inducing severe neutropenia and
increasing the risk of sepsis in this category of oncology patient.
Publication Types:
Clinical Trial
Research Support, Non-U.S. Gov't
PMID: 14760125 [PubMed - indexed for MEDLINE]
79: J Vasc Interv Radiol. 2004 Jan;15(1 Pt 1):57-61.
Do simultaneous bilateral tunneled infusion catheters in patients undergoing bone
marrow transplantation increase catheter-related complications?
Kaufman LJ, Clark TW, Roberts DA, Freiman DB, Shlansky-Goldberg RD, Patel AA,
Mondschein JI, Stavropoulos SW, Soulen MC, Solomon JA, Tuite CM, Cope C, Porter
DL, Stadtmauer EA, Cunningham KA, Trerotola SO.
Department of Radiology, Division of Interventional Radiology and Medicine,
University of Pennsylvania Medical Center, 1 Silverstein, 3400 Spruce Street,
Philadelphia, PA 19104, USA.
PURPOSE: Secure venous access with multiple lumens is necessary for the care of
allogeneic hematopoietic stem cell transplant (HSCT) recipients. The outcomes
associated with simultaneous bilateral tunneled internal jugular infusion
catheter placement in the HSCT recipient population were investigated in an
attempt to determine whether simultaneous introduction of these catheters
compounds or magnifies the risks (infection, venous thrombosis) associated with
tunneled catheters. MATERIALS AND METHODS: Patients undergoing HSCT and receiving
bilateral tunneled infusion catheters in a single procedure were identified using
a quality assurance data base. Medical records for the duration of
catheterization were reviewed; 43 patients were included in the study (mean age,
42 years; range, 22-56). Diagnoses included acute lymphocytic leukemia (n = 4),
acute myelogenous leukemia (n = 8), aplastic anemia (n = 2), chronic myelogenous
leukemia (n = 17), chronic lymphocytic leukemia (n = 1), Hodgkin lymphoma (n =
1), myelodysplasia (n = 4), myelofibrosis (n = 2), and non-Hodgkin lymphoma (n =
4). Cox proportional hazards regression analysis was performed to determine
differences in infection rates between dual- and triple-lumen catheters. RESULTS:
Forty-three pairs of catheters were placed. All met venous access needs for HSCT
recipient care. Complete follow-up was achieved for 77 of 87 (89%) catheters. The
overall infection rate was 0.25 per 100 catheter-days. The rate was 0.19 and 0.33
for dual- and triple-lumen catheters, respectively (P =.15). Mechanical failure
did not differ between catheter types (dual: 0.14 episodes per 100 days, triple:
0.05 per 100 days, P =.2). CONCLUSIONS: Bilateral multilumen tunneled infusion
catheter placement in a single procedure using imaging guidance is safe with
acceptable outcomes and meets venous access needs for HSCT. There is a trend
toward higher infection rates, with more lumens and more mechanical failure with
dual-lumen catheters.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 14709689 [PubMed - indexed for MEDLINE]
80: Infect Control Hosp Epidemiol. 2003 Dec;24(12):950-4.
Electronic interpretation of chest radiograph reports to detect central venous
catheters.
Trick WE, Chapman WW, Wisniewski MF, Peterson BJ, Solomon SL, Weinstein RA.
Health Outcomes Branch, Division of Healthcare Quality Promotion, National Center
for Infectious Diseases, Centers for Disease Control and Prevention, Public
Health Service, U.S. Department of Health and Human Services, Atlanta, Georgia,
USA.
OBJECTIVE: To evaluate whether a natural language processing system, SymText, was
comparable to human interpretation of chest radiograph reports for identifying
the mention of a central venous catheter (CVC), and whether use of SymText could
detect patients who had a CVC. DESIGN: To identify patients who had a CVC, we
performed two surveys of hospitalized patients. Then, we obtained available
reports from 104 patients who had a CVC during one of two cross-sectional surveys
(ie, case-patients) and 104 randomly selected patients who did not have a CVC
(ie, control-patients). SETTING: A 600-bed public teaching hospital. RESULTS:
Chest radiograph reports were available from 124 of the 208 participants.
Compared with human interpretation, SymText had a sensitivity of 95.8% and a
specificity of 98.7%. The use of SymText to identify case- and control-patients
resulted in a sensitivity of 43% and a specificity of 98%. Successful application
of SymText varied significantly by venous insertion site (eg, a sensitivity of
78% for subclavian and a sensitivity of 3.7% for femoral). Twenty-six percent of
the case-patients had a femoral CVC. CONCLUSIONS: Compared with human
interpretation, SymText performed well in interpreting whether a report mentioned
a CVC. In patient populations with less frequent CVC placement in femoral veins,
the sensitivity for CVC detection likely would be higher. Applying a natural
language processing system to chest radiograph reports may be a useful adjunct to
other data sources to automate detection of patients who had a CVC.
Publication Types:
Comparative Study
Evaluation Studies
PMID: 14700412 [PubMed - indexed for MEDLINE]
81: Infect Control Hosp Epidemiol. 2003 Dec;24(12):942-5.
Prevalence of the use of central venous access devices within and outside of the
intensive care unit: results of a survey among hospitals in the prevention
epicenter program of the Centers for Disease Control and Prevention.
Climo M, Diekema D, Warren DK, Herwaldt LA, Perl TM, Peterson L, Plaskett T,
Price C, Sepkowitz K, Solomon S, Tokars J, Fraser VJ, Wong E.
Hunter Holmes McGuire Veteran Affairs Medical Center, Richmond, Virginia 23249,
USA.
OBJECTIVE: To determine the prevalence of central venous catheter (CVC) use among
patients both within and outside the ICU setting. DESIGN: A 1-day prevalence
survey of CVC use among adult inpatients at six medical centers participating in
the Prevention Epicenter Program of the CDC. Using a standardized form, observers
at each Epicenter performed a hospital-wide survey, collecting data on CVC use.
SETTING: Inpatient wards and ICUs of six large urban teaching hospitals. RESULTS:
At the six medical centers, 2,459 patients were surveyed; 29% had CVCs. Among the
hospitals, from 43% to 80% (mean, 59.3%) of ICU patients and from 7% to 39%
(mean, 23.7%) of non-ICU patients had CVCs. Despite the lower rate of CVC use on
non-ICU wards, the actual number of CVCs outside the ICUs exceeded that of the
ICUs. Most catheters were inserted in the subclavian (55%) or jugular (22%) site,
with femoral (6%) and peripheral (15%) sites less commonly used. The jugular
(33.0% vs 16.6%; P < .001) and femoral (13.8% vs 2.7%; P < .001) sites were more
frequently used in ICU patients, whereas peripherally inserted (19.9% vs 5.9%; P
< .001) and subclavian (60.7% vs 47.3%; P < .001) catheters were more commonly
used in non-ICU patients. CONCLUSIONS: Current surveillance and infection control
efforts to reduce morbidity and mortality associated with bloodstream infections
concentrate on the high-risk ICU patients with CVCs. Our survey demonstrated that
two-thirds of identified CVCs were not in ICU patients and suggests that more
efforts should be directed to patients with CVCs who are outside the ICU.
Publication Types:
Comparative Study
Research Support, U.S. Gov't, P.H.S.
PMID: 14700410 [PubMed - indexed for MEDLINE]
82: Bone Marrow Transplant. 2004 Feb;33(3):347-50.
Efficacy and safety of femoral vascular access for peripheral blood stem cell
(PBSC) collection.
Moreiras-Plaza M, Albo C, Ares C.
Department of Nephrology, CH Xeral-Cíes Vigo, Spain.
Mercedes.Moreiras.Plaza@sergas.es
Central venous catheters are frequently used in leukapheresis to provide high
flow rates. The most common locations are the subclavian or jugular vein, but
insertion-related complications and inadequate flow are frequent problems.
Experience using femoral venous access is limited, because this has been
discouraged due to the high incidence of infectious or thromboembolic
complications. We evaluated the safety and efficacy of 108 short-term femoral
venous dialysis catheters used for the collection of peripheral blood stem cells
(PBSCs). All catheters were placed by a member of the dialysis unit, and they
remained in situ for the days needed to reach the target number of CD34+cells. No
prophylactic antibiotic or antithrombotic therapy was used. A total of 232
apheresis sessions was performed. The longest duration a catheter remained in
situ was 5 days. Most of the patients finished the collection in one or two
apheresis sessions. There were no thrombotic or infectious complications, and
insertion-related complications or mechanical problems were minimal. Apheresis
results were similar to those reported using subclavian or jugular venous access.
The short-term use of femoral venous dialysis catheters appears safe and
effective for PBSC collection, simplifying the procedure, improving patient
comfort, and reducing cost.
PMID: 14676783 [PubMed - indexed for MEDLINE]
83: Health Technol Assess. 2003;7(36):iii, ix-x, 1-99.
A randomised controlled trial to evaluate the clinical and cost-effectiveness of
Hickman line insertions in adult cancer patients by nurses.
Boland A, Haycox A, Bagust A, Fitzsimmons L.
Prescribing Research Group, Department of Pharmacology and Therapeutics,
University of Liverpool, UK.
OBJECTIVES: To examine the clinical and cost-effectiveness of image-guided
Hickman line insertions versus blind Hickman line insertions undertaken by nurses
in adult cancer patients. DESIGN: A cost-effectiveness analysis was carried out
alongside a randomised controlled trial. SETTING: A large acute cancer centre in
Manchester, UK. PARTICIPANTS: Cancer patients due to have a Hickman line
insertion who were over 18 years of age and were clinically and physically
compliant with specified protocols. INTERVENTIONS: In order to obtain central
venous access for the patient, two interventions were investigated: (i) blind
insertion of a Hickman line and (ii) image-guided insertion of a Hickman line.
Both interventions involved blind venipuncture of the subclavian vein. In the
blind arm, the Hickman line was routinely inserted without the use of image
guidance at any point in the procedure. Transfer to the interventional X-ray
suite and use of image guidance were options immediately available to the
operator during the procedure if required. In the image-guided arm, the position
of the guidewire was checked before the Hickman line was introduced and later the
Hickman line was positioned with the use of X-ray fluoroscopy. MAIN OUTCOME
MEASURES: The primary clinical outcome measure was catheter-tip misplacement and
this was expected to be higher in the blind arm. When comparing the skill level
of the trainer and the trainees, pneumothorax was the primary clinical outcome
measure. Other outcomes measures included arterial puncture, haematoma,
infection, failed insertion and assistance from other healthcare professionals.
RESULTS: No statistically significant difference was found between the mean cost
per patient in the two arms of the trial. The only statistically significant
difference in clinical outcomes was the frequency of catheter-tip misplacement,
which was higher in the blind arm of the trial. At very low costs, the
image-guided approach dominates the blind approach as fewer costs and greater
benefits are incurred. It is evident that nurses previously inexperienced in the
procedure can be trained to insert Hickman lines successfully both at the bedside
and under image guidance within a 3-month period. CONCLUSIONS: This report
indicates that nurse insertion of Hickman lines in the majority of adult cancer
patients is both safe and effective. However, there are a select group of
patients for whom image-guided insertion may be preferred. The results reveal
that skills and expertise can be transferred from trainer to trainee through a
relatively short, but intensive, training course. It is also evident that
patients support nurse insertion. Further research is suggested to compare the
safety and efficacy of nurse versus doctor insertions in particular subgroups of
patients and also to assess the quantity and quality of current service provision
in order to inform NHS decision-making in this area.
Publication Types:
Clinical Trial
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 14611735 [PubMed - indexed for MEDLINE]
84: J Hosp Infect. 2003 Nov;55(3):212-9.
A prospective, randomized study in critically ill patients using the Oligon
Vantex catheter.
Corral L, Nolla-Salas M, Ibañez-Nolla J, León MA, Díaz RM, Cruz Martín M, Iglesia
R, Catalan R.
Intensive Care Unit, Hospital General de Catalunya, C/ Gomera s/n, Sant Cugat del
Vallès, 08190, Barcelona, Spain.
Microbial colonization and the incidence of catheter-related bloodstream
infections (CR-BSI) associated with Oligon Vantex silver central venous catheters
(CVC) in critically ill patients were determined. A prospective, randomized,
controlled 17-month trial was carried out in an intensive care unit (ICU). All
patients requiring a triple-lumen CVC for four days or longer were enrolled.
Patients were randomized to receive a standard polyurethane CVC or an Oligon
Vantex silver CVC. Before removal of the catheter either due to discharge from
the ICU or suspected infection, blood for cultures was taken via the CVC and a
peripheral site. Skin and hub swabs and catheter-tips were also cultured. Two
hundred and six catheters, 103 in both groups, were evaluated. In the control
group (CG) 45/103 (44%) and in the silver group (SG) 30/103 (29%) were colonized
or had a CR-BSI (P=0.04). The SG was less likely to be colonized than the CG when
the catheter remained in situ for eight days or less (P=0.03) or over 15 days
(P=0.01); a second or subsequent catheter was present in the same patient
(P=0.002), or if the CVC was placed in the internal jugular vein (P=0.05).
Multivariate logistic-regression showed predisposing factors for catheter
colonization were jugular and femoral sites, second or subsequent catheter, and
being a member of the CG. CR-BSI occurred in five cases (four in CG). Rates of
CR-BSI per 1000 catheter-days in the CG were 2.8 and in the SG, 0.8 (P<0.001).
The Oligon Vantex silver catheter reduced the incidence of catheter-colonization
and may decrease the risk of CR-BSI.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 14572489 [PubMed - indexed for MEDLINE]
85: J Vasc Interv Radiol. 2003 Sep;14(9 Pt 1):1163-8.
Histologic changes in the human vein wall adjacent to indwelling central venous
catheters.
Forauer AR, Theoharis C.
Section of Vascular/Interventional Radiology, Department of Radiology, B1D 530,
University of Michigan Medical Center, 1500 E. Medical Center Drive, Ann Arbor,
Michigan 48109-0030, USA. forauer@umich.edu
PURPOSE: Central venous catheter dysfunction can be caused by thrombosis (of the
catheter or vessel itself), fibrin sheath formation, or infection. These sequelae
can lead to costly interventions, loss of the access device, or loss of access
sites in as many as one-third of patients. This study examined the histologic
changes in the access vein and superior vena cava wall that is adjacent to
central venous catheters in humans. MATERIALS AND METHODS: The access vein,
brachiocephalic vein, and superior vena cava were excised en bloc at autopsy from
six patients with central venous catheters. The specimens were processed and
stained with hematoxylin and eosin. The specimens were examined for histologic
changes in the vein wall adjacent to the catheters, changes in the intima, and
the presence of associated thrombus. RESULTS: Three catheters had been in place
<14 days (short term), and three for >90 days (long term). Two microscopic
patterns were observed. The short-term catheters displayed foci of local intimal
injury with endothelial denudation and a layer of adherent thrombus. The second
pattern, seen in the long-term catheters, consisted of smooth muscle cell
proliferation leading to vein wall thickening. Focal areas of catheter attachment
to the vein wall, composed of thrombus in varying stages of organization,
collagen, and endothelial cells, were also observed. CONCLUSIONS: After
short-term catheter placement, focal areas of endothelial injury were seen in the
vein wall adjacent to the catheter. Associated thrombus may or may not be
present. Long-term catheters displayed vein wall thickening and bridges from the
vein wall to the catheter. These observations represent a progressive reaction of
the human vein wall to access devices.
PMID: 14514808 [PubMed - indexed for MEDLINE]
86: Braz J Infect Dis. 2003 Apr;7(2):142-8. Epub 2003 Nov 19.
Comparison between the jugular and subclavian vein as insertion site for central
venous catheters: microbiological aspects and risk factors for colonization and
infection.
Sadoyama G, Gontijo Filho PP.
Laboratory of Microbiology - ARIMP - Federal University of Uberlândia,
Uberlândia/MG, Brazil. sadoyama@umuarama.ufu.br
Bacterial counts were made of catheter insertion site and of catheter tips to
help determine risk factors associated with catheterization of the jugular and
subclavian veins. Among the 116 patients included in this study, 69% had central
venous catheters (CVC) in the subclavian vein. Seven or more days catheterization
(p=0.001) and > or =3 invasive devices (p=0.01) were infection risk factors
associated with catheterization of the jugular vein. More than half of the
patients presented high colony counts at the insertion site (> or =200 CFU/20
cm2) and 27% of the catheter tips were contaminated. The risk factors associated
with contaminated catheter tips were > or =14 days hospital stay (p=0.02), > or
=7 days catheterization (p=0.01) and antibiotic therapy (p=0.04).
Coagulase-negative staphylococci (CoNS) and Staphylococcus aureus were the most
common microorganisms at the insertion site (78%) and in the catheter tip (94%).
Five patients presented sepsis (4.1%), four caused by Staphylococci and one by
GNB. Twelve patients had the same microorganisms at the insertion site and
catheter tip. We found a high prevalence of ORSA (62.5%) and ORCoNS (57.1%) in
catheter tips. The high counts of staphylococci, including ORSA and ORCoNS, at
the insertion site, and the significant association of this colonization with
catheter tip contamination, indicate that the skin is an important reservoir of
microorganisms associated with catheter-related bloodstream infection (CR-BSI).
Health professionals should be aware of this potential source of infection at the
CVC insertion site.
Publication Types:
Comparative Study
PMID: 12959686 [PubMed - indexed for MEDLINE]
87: Tumori. 2003 Jul-Aug;89(4 Suppl):292-5.
[Total implantable venous systems in day surgery]
[Article in Italian]
Sperlongano P, Piatto A, De Falco M, Parmeggiani D, Pisaniello D, Allocca A,
Vitolo M, Parmeggiani U.
Dipartimento di Scienze Anestesiologiche, Chirurgiche e dell'Emergenza, V
Divisione di Chirurgia Generale e Tecniche Chirurgiche Speciali, Seconda
Università degli Studi di Napoli.
Total implantable venous system (port-cath)in day surgery. AIMS: Most of patients
underwent to a total implantable venous system (port-cath) can be treated in day
surgery. METHODS: Since January 2000 to March 2003 we have implanted 31
port-a-cath, preferring access in subclavia v. We've treated all patients in day
surgery and we've performed a Rx-control with a medium follow up of two hour.
RESULTS: We have not reported any early complication, only 3 late complications:
a device malfunction, a "kinking" reservoir and an infection of the subcutaneous
pocket. The last two complications have required the explantation of the device.
In difficult catheterizations can be helpful to use a pediatric kit. The rules of
an aseptic and antiseptic operative procedure and the utilization of a short term
antibiotic prophylaxis can avoid infective complications. We have proposed, after
the device implantation, cardioaspirina like preventive therapy of septic and no
septic thrombosis. In the thrombotic occlusion of the catheter we propose the use
of activase. In malfunction's prevention we propose a lateral placement (to the
skin incision) of the subcutaneous pocket and a 45 degrees reservoir rotation.
CONCLUSIONS: The total venous system (port-cath) implantation can be mostly
performed in day surgery, improving the compliance of the patients with a low
cost procedure.
Publication Types:
English Abstract
Evaluation Studies
PMID: 12903624 [PubMed - indexed for MEDLINE]
88: Nephrol Dial Transplant. 2003 Aug;18(8):1631-8.
Repeated femoral vein puncturing for maintenance haemodialysis vascular access.
Kaneda H, Kaneda F, Shimoyamada K, Sakai S, Takahashi M.
Artificial Kidney, Kamome Clinic, Fukushima, Japan. h.kaneda@kamome-clinic.org
BACKGROUND: When access cannot be achieved using a native arteriovenous fistula
or a synthetic prosthetic graft, central venous catheters are usually placed.
This mode of access is short-lived, prone to infection, stenosis and thrombosis
of central veins. To overcome access problems, we developed a new native vascular
access ('femoral vein access') and devices. We report here on our experience with
the availability, longevity, procedure and morbidity of haemodialysis (HD) using
femoral vein access. METHODS: Repeated (three times a week) patient's native
femoral vein puncturing has been used as the vascular access (femoral vein
access) for maintenance HD in 30 patients (mean age +/- SD: 61.70 +/- 15.27 years
old; 18 female/12 male). The femoral vein was punctured beneath the inguinal
ligament (on a length ranging from 30 to 100 mm) after disinfection and local
anaesthesia. Long (effective length 56 mm) 19- and 18-gauge needles with four
side holes were used for the femoral vein puncture as an arterial site of the
extracorporeal circuit of HD and shorter (effective length 40 mm) similar gauge
needles for the subcutaneous vein puncture used as the return site. The needle is
inserted blind into the femoral vein after the femoral artery has been located by
palpation and the perception of a pulse. Patients returned home the same day.
RESULTS: The mean duration of HD treatment using femoral vein repeated puncture
was 4.99 +/- 3.42 years (up to 16.0 years). This represented a total experience
of 23 369 femoral vein punctures. The mean blood flow achieved on dialysis was
165 +/- 20 ml/min. The average Kt/V was 1.74 +/- 0.48 per session. CONCLUSIONS:
The femoral vein repeated puncture technique has substantial advantages over
venous catheters. It does not require surgery, while permitting adequate blood
flow. This method can be used as a long-term (over 10 years) blood access. Apart
from a few local haematomas, no serious complications have been observed.
Moreover, it does not carry a heavy financial burden.
PMID: 12897105 [PubMed - indexed for MEDLINE]
89: Am J Crit Care. 2003 Jul;12(4):328-35.
Comment on:
Am J Crit Care. 2003 Jul;12(4):326-7, 380.
Risk of colonization of central venous catheters: catheters for total parenteral
nutrition vs other catheters.
Dimick JB, Swoboda S, Talamini MA, Pelz RK, Hendrix CW, Lipsett PA.
School of Medicine, Johns Hopkins University, Baltimore, Md., USA.
BACKGROUND: Infected central venous catheters cause morbidity and mortality.
OBJECTIVE: To compare the risk for colonization of central venous catheters used
for total parenteral nutrition with that of catheters used for other purposes.
METHODS: Retrospective review of prospectively acquired data on 260 patients with
a stay in a surgical intensive care unit longer than 3 days. Single-lumen
catheters used solely for total parenteral nutrition were inserted into the
subclavian vein and cared for by a dedicated team. Catheters for other purposes
were placed and cared for by other staff. Catheters were cultured if clinical
findings suggested infection. RESULTS: Of 854 central venous catheters, 61 (7%)
were used for total parenteral nutrition. During 4712 catheter days of
observation, 89 catheters of all types were colonized. Risk factors for
colonization included duration of catheterization (P < .001), having 3 or more
lumens (hazard ratio, 1.7; 95% CI, 1.1-2.6), pulmonary artery catheterization
(hazard ratio, 1.7; 95% CI, 1.1-2.7), and placement in the internal jugular vein
(hazard ratio, 1.6; 95% CI, 1.1-2.5). Catheters used for total parenteral
nutrition (hazard ratio, 0.14; 95% CI, 0.04-0.57) and those in the subclavian
vein (hazard ratio, 0.51; 95% CI, 0.3-0.8) were at lower risk of colonization. In
a multivariate Cox model, the only significant factor was a 5-fold lower risk of
infection for catheters used for total parenteral nutrition (hazard ratio, 0.19;
95% CI, 0.04-0.83). CONCLUSION: Rates of colonization were lowest for catheters
used solely for total parenteral nutrition, suggesting that a team approach
improves patients' care.
Publication Types:
Comment
Comparative Study
PMID: 12882063 [PubMed - indexed for MEDLINE]
90: Pacing Clin Electrophysiol. 2003 Aug;26(8):1649-52.
Venous occlusion of the access vein in patients referred for lead extraction:
influence of patient and lead characteristics.
Bracke F, Meijer A, Van Gelder B.
Department of Cardiology, Catharina Hospital, Eindhoven, The Netherlands.
The aim of this study was to determine the effect of patient and lead
characteristics on occlusion of the access vein in pacemaker and ICD patients.
Contrast venography of the access vein was obtained in 89 patients (17 patients
with an ICD) scheduled for lead extraction. The indication for extraction was
infection in 57 patients (systemic infection in 9) and lead malfunction in 32
patients. In 6 of the 89 patients, leads were introduced in both the right and
left subpectoral area, resulting in a total of 95 venous entry sites. In 22 of
these entry sites one lead was present, in 61 two leads, in 11 three, and in 1
four leads. The vessel patency was graded open or occluded. Occlusion of the
subclavian vein occurred in four (13%) patients with lead malfunction versus 18
(32%) patients with infection (P = 0.07). In patients with systemic infection, 5
of 9 showed venous occlusion (P = 0.01 when compared to patients with
malfunction, odds ratio 8.75, 95% confidence interval 1.21-64.11). Considered per
entry site, the incidence of occlusion was 7 of 22 with one lead present, 17 of
61 with two leads, 0 of 11 with three leads, and 0 of 1 with four leads (P =
0.13). No patient had a superior vena caval occlusion. Patients with systemic
infection have an increased risk of occlusion of the access vein. On the
contrary, the study found no support for the concept that the risk of venous
occlusion increases with a higher number of leads present.
PMID: 12877695 [PubMed - indexed for MEDLINE]
91: G Ital Nefrol. 2003 May-Jun;20 Suppl 22:S35-7.
[Permanent vascular catheters: Effectiveness and duration of the Ash-Split Cath]
[Article in Italian]
Conz PA.
Unita' Operativa di Nefrologia e Dialisi, Presidio Ospedaliero di Monselice (PD),
Italy.
In absence of a permanent and useful native arterio-venous fistula, the use of a
tunnelled catheter allows dialysis therapy to be carried out. The Ash Split Cath
is a recently introduced chronic hemodialysis catheter. An ASC was inserted in
nine patients (7.1% of our prevalent dialysis population), for repeated venous
thrombosis in seven patients and a poor venous tree in two. The average blood
flow rate was 250 +/- 50 mL/minute and the mean venous pressure measured was
140mm Hg +/- 35. Recirculation determined by low flow technique was less than 5%
and 4 months after the catheter placement, calculated Kt/V, was 1.2 +/- 0.02.
During the follow up we did not document any infection of the exit site or
related to the catheter.
Publication Types:
English Abstract
Evaluation Studies
PMID: 12851919 [PubMed - indexed for MEDLINE]
92: Ren Fail. 2003 May;25(3):431-8.
Using cuffed and tunnelled central venous catheters as permanent vascular access
for hemodialysis: a prospective study.
Cetinkaya R, Odabas AR, Unlu Y, Selcuk Y, Ates A, Ceviz M.
Department of Nephrology, Ataturk University, Faculty of Medicine, Erzurum,
Turkey. ramazancetinkaya@yahoo.com
BACKGROUND: Adequate care of a hemodialysis patient requires constant attention
to the need to maintain vascular access (VA) patency. VA complications are the
main cause of hospitalization in hemodialysis patients. The native arteriovenous
fistula (NAVF), synthetic arteriovenous grafts fistula (GAVF) and silastic cuffed
central venous catheters (CVCs) are used for permanent vascular access (PVA).
CVCs are primary the method of choice for temporary access. But using this access
modality is increasing more and more for PVA in elderly hemodialysis patients and
when other PVA is not possible. The primary aim of this study is to investigate
survivals and complications of the CVCs used for long-term VA. METHODS: We
prospectively looked at 92 CVCs (Medcomp Ash Split Cath, 14 FR x 28 cm (Little,
M.A.; O'Riordan, A.; Lucey, B.; Farrell, M.; Lee, M.; Conlon, P.J.; Walshe, J.J.
A prospective study of complications associated with cuffed, tunnelled
hemodialysis catheters. Nephrol. Dial. Transplant. 2001, 16 (11), 2194-2200) with
Dacron cuff) inserted in 85 (50 females, 35 males) chronic hemodialysis patients
(the mean age: 56.6 +/- 14.1 years) from July 1999 to January 2002. The overall
survival and complications were followed up. Furthermore, the patients were
evaluated for demographic and clinical characteristics. Data were analysed by
chi-square, Wilcoxon rank and Kaplan-Meier survival tests. RESULTS: The median
duration of CVC survival was 289 days (range: 10-720). Eleven (11.9%) CVCs were
removed due to complications. In 79 (92.9%) patients, 1, in 5 (5.8%) patients, 2
and in 1 patient, 3 CVCs were inserted. Of the 85 patients, 56 have CVCs
functioning. In addition, 27 (31.76%) patients have CVCs functioning for over 12
months, 17 (20%) patients have CVCs functioning for 6 months. The total incidence
of CVC related infections was 0.82 episodes/1000 catheter days. Besides,
thrombosis was occurred in 10 (10.8%) CVCs. The most frequent indications for CVC
removal were patient death (69.4%), thrombosis (16.6%) and CVC-related infections
(13.8%). CONCLUSIONS: CVCs are primarily used for temporary access. But this
study indicates that CVC may be a very useful alternative permanent vascular
access for hemodialysis patients when other forms of vascular access are not
available.
Publication Types:
Comparative Study
PMID: 12803506 [PubMed - indexed for MEDLINE]
93: Pediatr Crit Care Med. 2001 Jan;2(1):57-62.
Complications of central venous catheterization in critically ill children.
Casado-Flores J, Barja J, Martino R, Serrano A, Valdivielso A.
Pediatric Intensive Care Unit, Hospital Infantil Niño Jesus, Universidad Autonoma
de Madrid, Madrid, Spain.
OBJECTIVE: Analysis of central venous catheterization complications in different
access sites with the Seldinger technique. Patients and Methods: A prospective
study (May 1992 through December 1996) of 308 central venous catheterizations in
children of different ages in a pediatric intensive care unit. RESULTS: Access
sites were the subclavian vein (76.3%), femoral vein (20.4%), and jugular vein
(3.2%). The frequency of catheter placement-related complications was 22%, and
the frequency of serious catheter placement-related complications was 2.9%
(pneumothorax 1.9%, hemothorax 1%). Catheter placement-related complications were
more common in the subclavian than in the femoral vein (chi-square, p =.02) for
the larger bore catheters (chi-square, p =.01) and for the higher number of
attempts (Student's t -test, p <.001). Catheter placement-related complications
were not related to the age, weight, or whether the procedure was performed by
the staff physician or resident. The overall complication rate for
maintenance-related complications was 36%. Maintenance-related complications were
more common in younger children (Student's t -test, p =.03). The most frequent
maintenance-related complications were mechanical complications (catheter
obstruction and central venous thrombosis), and these were higher for femoral
access (chi-square, p <.01) and for catheters indwelling for a longer period of
time. Infection was found in 5.8% of patients, mainly due to Staphylococcus
epidermidis. Infection was not related to the site of venous access or to the
length of time the catheter was left indwelling. CONCLUSIONS: Central venous
catheterization can be performed readily in children of all ages with an
acceptable degree of risk. The immediate complications were more frequent and
severe for subclavian vein catheterization, and the highest risk factor was the
number of attempts at catheter insertion. Although the most frequent late
complications were mechanical, which were higher for the femoral access and
long-indwelling catheters, femoral catheters can be left indwelling for longer
periods if routine ultrasound follow-up is performed. Infectious complications
were independent of the venous access site or the duration of catheterization.
PMID: 12797890 [PubMed - as supplied by publisher]
94: Crit Care Med. 2003 May;31(5):1318-24.
Comment in:
Crit Care Med. 2003 May;31(5):1583-4.
Antiseptic chamber-containing hub reduces central venous catheter-related
infection: a prospective, randomized study.
León C, Alvarez-Lerma F, Ruiz-Santana S, González V, de la Torre MV, Sierra R,
León M, Rodrigo JJ.
Intensive Care Units of Hospital Universitario de Valme, Sevilla, Spain.
OBJECTIVE: The hub connecting the catheter and the infusion equipment is a common
portal of entry for bacteria causing catheter-related sepsis. We assessed the
efficacy of a new hub model (Segur-Lock) that incorporates an antiseptic chamber
filled with 3% iodinated alcohol in preventing endoluminal catheter contamination
and catheter-related bloodstream infection arising at the hub. DESIGN:
Prospective, randomized, multicenter study. SETTING: Seven medical and surgical
adult intensive care units in Spain. PATIENTS: A total of 230 patients aged 18
yrs or older requiring the insertion of a nontunneled central venous catheter for
>or=6 days from January 1, 1998, to April 30, 1999. INTERVENTIONS: Patients were
randomized at the time of catheter insertion to receive catheters with standard
Luer-lock connector (control group, n = 114) or catheters with the new hub model
(n = 116). MEASUREMENTS AND MAIN RESULTS: Skin, catheter tip, and hub cultures
were performed at the time the catheter was withdrawn because therapy was
terminated or due to suspicion of sepsis, in which case peripheral blood and
infusate cultures were simultaneously taken. Catheter-related bloodstream
infection was diagnosed in 19 (8.3%) patients. Catheters were more often
withdrawn because of suspicion of infection in the control group (43.8%) than in
the new hub model group (30.1%, p <.035). The prevalence of culture-positive
catheter hubs without associated bacteremia (colonization) was higher in the
control group (14.4% vs. 4.3%, p <.001). Catheter-related bloodstream infection
from the catheter hub also occurred more frequently in controls than in patients
assigned to the new hub model (7% vs. 1.7%; p <.049; relative risk, 4.14; 95%
confidence interval, 0.8-19). CONCLUSIONS: This new antiseptic chamber-containing
hub has proved to be effective in preventing endoluminal bacterial colonization
and catheter-related bloodstream infection from hub contamination in intensive
care unit patients with central venous catheters inserted for >or=6 days.
Publication Types:
Clinical Trial
Multicenter Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 12771597 [PubMed - indexed for MEDLINE]
95: Minerva Anestesiol. 2003 Apr;69(4):302-7.
[Infection prevention and control in intravascular devices]
[Article in Italian]
Colombo D, Russolillo C.
Servizio di Anestesia e Rianimazione, Azienda Ospedaliera Luigi Sacco, Polo
Universitario, Milano, Italy.
Intravascular devices (IVD) are indispensable in the care of the critical
patient; even so, their use can be complicated by infection, which is generally
associated with longer hospital stay and ensuing higher hospital costs. It is
therefore imperative that guidelines are applied that constitute a basis of
information upon which the individual facility can develop its own strategy. The
strategy can be outlined under the following points: a) staff training, b)
surveillance of IVD-associated infections, c) hand washing, d) barrier measures
during catheter introduction and management, e) insertion site management and
medication systems for the insertion site, f) choice and replacement of the IVD,
g) replacement of intravenous administration devices and liquids, h)
antimicrobial prophylaxis. In the management of central venous catheters (CVC),
recommendations call for: 1) the use of a single lumen CVC, unless multiple
accesses are needed; 2) the peripheral placement of CVCs, both in the use of
tunneled catheters and/or implantable vascular devices in patients over 4 years
of age in which long-term vascular access (> 30 days) is planned; 3) the use of
completely implantable devices in pediatric patients less than 4 years of age
requiring long-term vascular access; 4) the use of the subclavian artery as the
site of CVC insertion unless clinically contraindicated (e.g. coagulopathy,
anatomic alterations); 5) the application of barrier precautions during CVC
introduction and in the management of the catheter and the insertion site.
Publication Types:
English Abstract
Review
PMID: 12766724 [PubMed - indexed for MEDLINE]
96: J Pediatr Surg. 2003 Apr;38(4):594-6.
A complication associated with central line removal in the pediatric population:
retained fixed catheter fragments.
Jones SA, Giacomantonio M.
Division of Pediatric Surgery, Dalhousie University, IWK Health Center, Halifax,
Nova Scotia, Canada.
BACKGROUND: There are many reports on the complications that occur at the time of
insertion and during the life of central venous indwelling catheters. However,
there is no literature that describes the complications that occur at the time of
removal of these lines. METHODS: A retrospective review of 136 central line
(Broviacs [B], Port-A- Caths [PC] and Hickmans [HC]) removals during the last 5
years was undertaken. RESULTS: A total of 97% were removed after completion of
chemotherapy, and 3% because of sepsis or malfunction. Three PC lines broke at
the time of removal resulting in a length of line remaining in the central venous
system (the superior vena cava, innominate vein, and bracheo-cephalic subclavian
junction). Two lines were inserted by a cut-down technique into the external
jugular and one line by the percutaneous technique into the subclavian vein. At
follow-up, none of the residual lines were associated with thrombus formation,
and none showed any evidence of migration. CONCLUSIONS: This review identifies a
specific problem that can occur with central line removal. Both the long-term
affects of residual catheter within the central venous system and the need to
remove the foreign body have yet to be addressed. Copyright 2003, Elsevier
Science (USA). All rights reserved.
Publication Types:
Case Reports
Review
PMID: 12677573 [PubMed - indexed for MEDLINE]
97: Br J Haematol. 2003 Mar;120(6):1073-8.
Ultrasound screening for internal jugular vein thrombosis aids the detection of
central venous catheter-related infections in patients with haemato-oncological
diseases: a prospective observational study.
Lordick F, Hentrich M, Decker T, Hennig M, Pohlmann H, Hartenstein R, Peschel C.
Third Department of Internal Medicine, Klinikum rechts der Isar, Technical
University of Munich, Germany. f.lordick@lrz.tum.de
To prove the hypothesis that central venous catheter-related thrombosis and
infection are associated, 43 haemato-oncological patients with an internal
jugular vein catheter underwent ultrasound screening for thrombosis every 4 d.
Catheter-related thrombosis was detected in 13/43 patients (30%).
Catheter-related infection, as defined by the U.S. Hospital Infection Control
Practices Advisory Committee, was found in 14/43 patients (33%) with colonization
of the catheter in two patients, exit site infection in eight patients and
catheter-related bloodstream infection in four patients. Catheter-related
thrombosis and catheter-related infection coincided in 12 patients and were
significantly correlated (Fisher's exact test, P < 0.0001). Detection of
thrombosis indicated a catheter-related infection with a superior sensitivity
(86% vs 57%) and an equivalent specificity (97%) compared with the presence of
clinical signs (erythema, tenderness, warmth or swelling). Neutropenia, which
occurred in 32 patients, was found in 13/14 patients (93%) with a
catheter-related infection and, therefore, seemed to be an important covariate
for the development of a catheter-related infection. This study showed a close
correlation between catheter-related thrombosis and infection. Ultrasound
screening for thrombosis was helpful for detecting catheter-related infection.
These findings could be clinically useful for the handling of central venous
catheters in patients with an elevated risk of infectious complications.
PMID: 12648081 [PubMed - indexed for MEDLINE]
98: Ann Clin Microbiol Antimicrob. 2003 Feb 27;2:3.
Central venous catheter related infections: risk factors and the effect of
glycopeptide antibiotics.
Oncü S, Ozsüt H, Yildirim A, Ay P, Cakar N, Eraksoy H, Calangu S.
Department of Infectious Diseases and Clinical Microbiology, Adnan Menderes
University Faculty of Medicine, Aydin, Turkey. serkanoncu@hotmail.com
BACKGROUND: We undertook a prospective study of all new central venous catheters
inserted into patients in the intensive care units, in order to identify the risk
factors and to determine the effect of glycopeptide antibiotics on catheter related infections. METHODS: During the study period 300 patients with central
venous catheters were prospectively studied. The catheters used were nontunneled,
noncuffed, triple lumen and made of polyurethane material. Catheters were
cultured by semiquantitative method and blood cultures done when indicated. Data
were obtained on patient age, gender, unit, primary diagnosis on admission,
catheter insertion site, duration of catheterization, whether it was the first or
a subsequent catheter and glycopeptide antibiotic usage. RESULTS: Ninety-one
(30.3%) of the catheters were colonized and infection was found with 50 (16.7%)
catheters. Infection was diagnosed with higher rate in catheters inserted via
jugular vein in comparison with subclavian vein (95% CI: 1.32-4.81, p = 0.005).
The incidence of infection was higher in catheters which were kept in place for
more than seven days (95% CI 1.05-3.87, p = 0.03). The incidence of infection was
lower in patients who were using glycopeptide antibiotic during catheterization
(95% CI: 1.49-5.51, p = 0.005). The rate of infection with Gram positive cocci
was significantly lower in glycopeptide antibiotic using patients (p = 0.01). The
most commonly isolated organism was Staphylococcus aureus (n = 52, 37.1%).
CONCLUSION: Duration of catheterization and catheter insertion site were
independent risk factors for catheter related infection. Use of glycopeptide
antibiotic during catheterization seems to have protective effect against
catheter related infection.
PMID: 12643811 [PubMed]
99: Indian Pediatr. 2003 Jan;40(1):41-4.
Medium and long term central venous access in children.
Rao S, Alladi A, Das K, Cruz AJ.
Department of Pediatric Surgery, St. John s Medical College Hospital, Bangalore,
India.
From September 2000 to August 2001, 104 central venous access devices (CVAD) were
inserted in 91 children, governed by a uniform protocol. Thirty catheters were
inserted in neonates, 29 in infants, 37 in children and 8 in adolescents.
Fifty-one were planned insertions in the operating suite and 53 were emergencies
- often by the bedside. There were 12 insertion related complications-all of
which were minor. Neonatal age and bedside introduction had a higher risk of
insertion related problems. The incidence of non-infectious complications was 20%
(rate of 13.7/1000 line days) and was influenced by the child's age and insertion
site. Femoral route was the safest. Incidence of catheter associated infections
(CAI) was 15.4% (rate of 11/1000 line days). Only 2 children had catheter
associated bloodstream infection. Neonates were at higher risk of catheter
related infections. Age, insertion site and occurence of insertion complications
influenced duration of catheterization (median 7.5 days, range 2-243 days) There
was no major complication, though more than 50% insertions were in neonates and
infants. In our practice, use of CVAD is feasible and safe, especially in
neonates and infants.
PMID: 12554917 [PubMed - indexed for MEDLINE]
100: Crit Care Med. 2002 Dec;30(12):2632-5.
Comment in:
Crit Care Med. 2002 Dec;30(12):2776.
Inflammation at the insertion site is not predictive of catheter-related
bloodstream infection with short-term, noncuffed central venous catheters.
Safdar N, Maki DG.
Section of Infectious Diseases, Department of Medicine, University of Wisconsin
Medical School, Madison, WI, USA.
BACKGROUND: Noncuffed, percutaneously inserted central venous catheters (CVCs)
are widely used and cause at least 250,000 bloodstream infections (BSIs) in U.S.
hospitals each year. We report a prospective study to determine whether
inflammation at the insertion site is predictive of CVC-related BSI. METHODS:
Percutaneously inserted, noncuffed CVCs inserted into the subclavian, internal
jugular, or femoral vein in two randomized trials during 1998-2000 were
prospectively studied; most patients were in an intensive care unit. The
condition of the insertion site was evaluated daily by research nurses,
quantifying pain (0, 1), erythema (0-2), swelling (0, 1), and purulence (0, 1);
the lowest possible overall inflammation score was 0 and the highest was 5.
CVC-related BSI was confirmed in each case by demonstrating concordance between
isolates from the catheter segment and from blood cultures by
restriction-fragment DNA subtyping. RESULTS: Among 1,263 CVCs prospectively
studied, 333 (26.3%) were colonized at removal; of these, 35 catheters (2.7%)
caused BSIs (5.9 per 1000 CVC days). BSIs were caused by coagulase-negative
staphylococci (n = 27), enterococci (n = 4), enteric Gram-negative bacilli (n =
3), or (n = 1). Most insertion sites showed little or no inflammation at the time
of removal. There were no significant differences among mean scores for each
inflammatory variable examined or overall score among colonized CVCs (0.1 +/0.1), catheters causing CVC-related BSI (0.2 +/- 0.4), and noncolonized CVCs (0.1
+/- 0.1). The sensitivity of local inflammation for diagnosis of CVC-related BSI
was dismal (0-3%). CONCLUSION: Local inflammation is uncommon with infected CVCs,
probably because most catheter-associated infections are currently caused by
coagulase-negative staphylococci, a pathogen that incites little local or
systemic inflammation. Whereas overt inflammation of the insertion site should
raise suspicion of CVC-related BSI caused by or Gram-negative bacilli, especially
if the patient has fever or other signs of sepsis, in general, site appearance
cannot be relied on to identify catheter colonization or CVC-related BSI.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 12483050 [PubMed - indexed for MEDLINE]
101: Pediatr Infect Dis J. 2002 Nov;21(11):1000-4.
Efficacy of subcutaneous tunneling for prevention of bacterial colonization of
femoral central venous catheters in critically ill children.
Nahum E, Levy I, Katz J, Samra Z, Ashkenazi S, Ben-Ari J, Schonfeld T, Dagan O.
Unit of Pediatric Intensive Care, Schneider Children's Medical Center of Israel,
Petah Tikva, Israel. enahum@cw.bc.ca
BACKGROUND: Blood stream infections are a common and serious complication of
central venous catheters (CVCs). To decrease catheter colonization, some authors
advocate tunneling the catheter in the subcutaneous tissue during insertion. This
technique has proved effective in adults, but there are no data on its safety and
efficacy in critically ill children. Our objective was to evaluate the efficacy
and safety of subcutaneous tunneling of short term, noncuffed CVCs for the
prevention of CVC-related infections in critically ill children. METHODS: A
prospective randomized controlled trial was performed at a tertiary children's
medical center in Israel and included children ages 0 to 18 years admitted to the
pediatric intensive care unit or the pediatric cardiac intensive care unit from
September 2000 to April 2001 who required placement of a femoral central venous
catheter for >48 h. The children were randomized for tunneled or nontunneled
insertion. The main outcome measures were bacterial colonization of proximal and
distal catheter segments tested by semiquantitative technique and infectious or
noninfectious complications of the CVC. RESULTS: Of 98 eligible children, 49
received tunneled catheters and 49 received nontunneled catheters. Patients' age
ranged from 1 month to 16.5 years (mean, 3.07 +/- 2.48 years). There were no
significant differences between the groups in age, sex, disease severity
[Pediatric Risk of Mortality III (PRISM) score], duration of catheterization and
underlying diseases. Bacterial colonization was found in 11 (22.4%) catheters in
the nontunneled group compared with 3 (6.1%) in the tunneled group (P = 0.004).
Proximal segment colonization occurred in 7 (14.2%) nontunneled catheters and 2
(4.8%) tunneled catheters (P = 0.07), and distal segment colonization occurred in
3 (6.1%) and 9(18.3%) tunneled and nontunneled catheters, respectively (P =
0.053). The main pathogens were coagulase-negative staphylococci, Pseudomonas
spp. and Klebsiella spp. There was no statistically significant difference
between the groups in the rate of bloodstream infection (2 in the tunneled group,
3 in the nontunneled). Except for 1 case of subcutaneous hematoma, which
resolved, there were no immediate or late complications of the tunneling
procedure. CONCLUSION: Subcutaneous tunneling of CVCs in the femoral site is a
safe procedure and decreases significantly the rate of CVC colonization in
critically ill children.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 12442019 [PubMed - indexed for MEDLINE]
102: Medicine (Baltimore). 2002 Nov;81(6):466-79.
A review of risk factors for catheter-related bloodstream infection caused by
percutaneously inserted, noncuffed central venous catheters: implications for
preventive strategies.
Safdar N, Kluger DM, Maki DG.
Department of Medicine, University of Wisconsin Medical School and University of
Wisconsin Hospitals and Clinics, Madison, 53792, USA.
Strategies for preventing central venous catheter (CVC)-related bloodstream
infection are most likely to be effective if guided by an understanding of the
risk factors associated with these infections. In this critical review of
published studies of risk factors for CVC-related bloodstream infection that were
prospective and used multivariable techniques of data analysis or that were
randomized trials of a preventive measure, a significantly increased risk of
catheter-related bloodstream infection was associated with inexperience of the
operator and nurse-to-patient ratio in the intensive care unit, catheter
insertion with less than maximal sterile barriers, placement of a CVC in the
internal jugular or femoral vein rather than subclavian vein, placement in an old
site by guidewire exchange, heavy colonization of the insertion site or
contamination of a catheter hub, and duration of CVC placement > 7 days.
Prospective studies or randomized trials of control measures focusing on these
risk factors have been shown to reduce risk significantly: formal training in CVC
insertion and care, use of maximal sterile barriers at insertion, use of
chlorhexidine rather than povidone-iodine for cutaneous antisepsis, applying a
topical anti-infective cream or ointment or a chlorhexidine-impregnated dressing
to the insertion site, and the use of novel catheters with an anti-infective
surface or a contamination resistant hub. Better prospective studies of
sufficient size to address all potential risk factors, including insertion site
and hub colonization, insertion technique, and details of follow-up care, would
enhance our understanding of the pathogenesis of CVC-related bloodstream
infection and guide efforts to develop more effective strategies for prevention.
Publication Types:
Review
PMID: 12441903 [PubMed - indexed for MEDLINE]
103: Crit Care Med. 2002 Nov;30(11):2481-8.
Comment in:
Crit Care Med. 2002 Nov;30(11):2598-600.
Safety and efficacy of a novel intravascular cooling device to control body
temperature in neurologic intensive care patients: a prospective pilot study.
Schmutzhard E, Engelhardt K, Beer R, Brössner G, Pfausler B, Spiss H, Unterberger
I, Kampfl A.
Department of Neurology, University Hospital Innsbruck, Austria.
OBJECTIVE: To determine the safety and efficacy of a novel intravascular cooling
device (Cool Line catheter with Cool Gard system) to control body temperature
(temperature goal <37 degrees C) in neurologic intensive care patients. DESIGN: A
prospective, uncontrolled pilot study in 51 consecutive neurologic intensive care
patients. SETTING: A neurologic intensive care unit at a tertiary care university
hospital. PARTICIPANTS: Patients were 51 neurologic intensive care patients with
an intracranial disease requiring a central venous catheter due to the primary
(intracranial) disease. We excluded patients under the age of 19 yrs and those
with active cardiac arrhythmia, full sepsis syndrome, bleeding diathesis and
infection, or bleeding at the site of the intended catheter insertion. Male to
female ratio was 31:20, and the median age was 55 yrs (range, 24-85 yrs).
Forty-four of 51 patients (86.3%) had an initial Glasgow Coma Scale score of 3,
three patients had a Glasgow Coma Scale score of 9, one patient presented with an
initial Glasgow Coma Scale score of 11, two patients had an initial Glasgow Coma
Scale score of 13, and one patient had an initial Glasgow Coma Scale score of 15.
The mean initial tissue injury severity score was 45.1 and the median initial
tissue injury severity score 45.0 (range, 19-70). INTERVENTIONS: Patients were
enrolled prospectively in a consecutive way. Within 12 hrs after admission, the
intravascular cooling device (Cool Line catheter) was placed, the temperature
probe was located within the bladder (by Foley catheter), and the Cool Gard
cooling device was initiated. This Cool Gard system circulates
temperature-controlled sterile saline through two small balloons mounted on the
distal end of the Cool Line catheter. The patient's blood is gently cooled as it
is passed over the balloons. The Cool Gard system has been set with a target
temperature of 36.5 degrees C. The primary purpose and end point of this study
was to evaluate the cooling capacity of this intravascular cooling device.
Efficacy is expressed by the calculation formula of fever burden, which is
defined as the fever time product ( degrees C hours) under the fever curve.
MEASUREMENTS AND MAIN RESULTS: The cooling device was in operation for a mean of
152.4 hrs. The ease of insertion was judged as easy in 42 of 51 patients; in a
single patient, the catheter was malpositioned within the jugular vein, requiring
early removal. The rate of infectious and noninfectious complications (nosocomial
pneumonia, bacteremia, catheter-related ventriculitis, pulmonary embolism, etc.)
was comparable to the rate usually observed in our neurologic intensive care
patients with such severe intracranial diseases. The total fever burden within
the entire study period of (on average) 152.4 hrs was 4.0 degrees C hrs/patient,
being equivalent to 0.6 degrees C hrs/patient and day. Thirty of 51 patients
showed an elevation of the body temperature (>37.9 degrees C) within 24 hrs after
termination of the cooling study. One awake patient (subarachnoid hemorrhage,
Glasgow Coma Scale score 15) experienced mild to moderate shivering throughout
the entire period of 7 days. The mortality rate was 23.5%. CONCLUSION: This novel
intravascular cooling device (Cool Line catheter and Cool Gard cooling device)
was highly efficacious in prophylactically controlling the body temperature of
neurologic intensive care patients with very severe intracranial disease (median
Glasgow Coma Scale score, 3-15). Morbidity and mortality rates were consistent
with the ranges reported in the literature for such neurologic intensive
patients.
Publication Types:
Clinical Trial
Research Support, Non-U.S. Gov't
PMID: 12441758 [PubMed - indexed for MEDLINE]
104: Clin Nephrol. 2002 Aug;58(2):128-33.
Use of the Tesio catheter for hemodialysis in patients with end-stage renal
failure: a 2-year prospective study.
Webb A, Abdalla M, Harden PN, Russell GI.
St. Lukes Hospital, Bradford, UK. alan.webb@bradfordhospitals.nhs.uk
BACKGROUND: The Tesio catheter system has been proposed to be a reliable source
of vascular access for the dialysis patient with low rates of infection and other
complications. Whether such catheters provide reliable short- and long-term
access remains undetermined. METHODS: This study prospectively examined all Tesio
lines inserted over a 2-year period in patients with end-stage failure with
careful recording of all catheter complications and reasons for catheter loss.
RESULTS: 100 catheters were inserted in 82 patients giving a total experience of
13,749 catheter days; 74 catheters were inserted into the jugular veins, the
remainder into the femoral veins; 82 insertions were covered with antibiotics. At
the end of the study, 29 catheters remained in situ. Of the remaining 71
catheters, 27 catheters were removed because of fashioning of definitive access.
Nine catheters were lost due to infection and 10 were lost due to non-function;
19 patients died with a functioning catheter. Episodes ofnon-function were the
major complications, although catheter patency was restored in 90% of cases
utilizing urokinase and warfarin. Overall 80% of femoral and 16% of jugular
catheters required anticoagulation. CONCLUSIONS: Tesio catheters inserted into
the jugular or femoral veins can provide excellent access whilst awaiting
definitive dialysis access. They are well-tolerated with a low complication rate
compared to standard temporary central venous catheters. Non-function remains a
significant problem, especially in femoral catheters, which should be
anticoagulated following insertion. Because of our results we suggest that these
catheters be used as part of the co-ordinated approach to the management of
vascular access in end-stage renal failure patients without definitive access.
PMID: 12227685 [PubMed - indexed for MEDLINE]
105: Acta Radiol. 2002 Jul;43(4):371-5.
Subcutaneous chest ports via the internal jugular vein. A retrospective study of
117 oncology patients.
Yip D, Funaki B.
Department of Radiology, University of Chicago Hospitals, Chicago, IL 60637, USA.
PURPOSE: To review image-guided chest port insertion using the right internal
jugular vein as the access site of choice. MATERIAL AND METHODS: One hundred and
eighteen subcutaneous chest ports were placed via the internal jugular vein in
117 patients with malignancies using both fluoroscopic and US guidance in
interventional radiology suites. RESULTS: The technical success rate was 100%
with no procedural complications. Follow-up was obtained in all patients with
total access days of 40,450 days (mean, 342.8 days). Premature catheter removal
was required in 8 patients (6.8%, 0.20 per 1,000 access days) due to
non-treatable complications: 2 catheter occlusions/malfunctions (1.7%, 0.05 per
1,000 access days), 1 catheter-related skin erosion (0.85%, 0.024 per 1,000
access days), and 5 infections (4.2%, 0.15 per 1,000 access days). Two
symptomatic right upper extremity venous thromboses also occurred (1.7%, 0.05 per
1,000 access days) that were treated successfully with anticoagulation.
CONCLUSION: Image-guided placement of internal jugular vein chest ports has a
high success rate and low complication rate compared with reported series of
unguided subclavian vein port insertion. The internal jugular vein should be used
as the preferred venous access site compared to the subclavian vein.
PMID: 12225477 [PubMed - indexed for MEDLINE]
106: Am J Kidney Dis. 2002 Sep;40(3):E8.
Reversal of pulmonary hypertension after ligation of a brachiocephalic
arteriovenous fistula.
Clarkson MR, Giblin L, Brown A, Little D, Donohoe J.
Renal Division, Department of Medicine, Brigham and Women's Hospital, Boston, MA
02115, USA. mrclarkson@partners.org
The arteriovenous (AV) fistula is the access method of choice for long-term
hemodialysis according to DOQI guidelines. Among the recognized complications of
upper extremity AV fistulae fashioned for hemodialysis are infection, aneurysm
formation, and high-output left ventricular failure. We describe a novel
cardiopulmonary complication--secondary pulmonary hypertension resulting from an
aneurysmal brachiocephalic AV fistula. The clinical presentation, investigation,
management, and pathophysiology of this complication are discussed. Copyright
2002 by the National Kidney Foundation, Inc.
Publication Types:
Case Reports
PMID: 12200825 [PubMed - indexed for MEDLINE]
107: G Ital Nefrol. 2002 Jan-Feb;19(1):44-8.
[Temporary vascular access for haemodialysis: is infection still the most
important complication?]
[Article in Italian]
Barracca A, Pili GF, Spina M, Murgia MG, Menneas AP, Manca O.
Dipartimento Rene, Ospedale S.Michele, Azienda Ospedaliera G. Brotzu, Cagliari.
BACKGROUND: Aging in the dialitic population currently shows the problem of
vascular access for haemodialysis. The use of temporary catheters for
haemodialysis has increased the risk of infections. DOQI guidelines underline
this problem. We think that the thrombosis of central veins is a problem as
important as infection. METHODS: In the last two years we studied prospectively
310 patients. 686 catheters for haemodialysis were placed. Infection,
malfunctioning of catheters and thrombosis of central veins were studied. We
compared femoral catheters with jugular catheters. Finally we studied by
ultrasound the jugular vessels diameter and thrombi of jugular vein. RESULTS.
Fever was present in 5.55% of patients with femoral catheters and in 5.84% of the
patients with jugular catheters. The malfunctioning incidence in patients with
femoral catheters was 22.75% and 8.76% in patients with jugular catheters with
statistic difference. Ultrasound study of jugular veins showed thrombotic
incidence of internal jugular vein in 20,8% of patients. CONCLUSIONS: We think
that with correct management of catheters there is no difference in the incidence
of fever in patients with jugular catheters versus femoral catheters. Probably
jugular catheters have better performance than femoral catheters. We need
controlled studies to better understand the problem of central vein thrombosis.
Publication Types:
English Abstract
PMID: 12165945 [PubMed - indexed for MEDLINE]
108: Int J Artif Organs. 2002 May;25(5):354-64.
Approach to vascular access for hemodialysis: experiences from the Republic of
Macedonia.
Oncevski A, Dejanov P, Gerasimovska V, Polenakovic MH.
Department of Nephrology, Clinical Center, Skopje, Republic of Macedonia.
oncevski@ukim.edu.mk
Eight thousand eight hundred and forty nine different vascular hemodialysis
accesses were performed in the period from 1976 until 1999 at the Department of
Nephrology, Skopje: 3,114 native arterial-venous fistula (AVF), 715
arterial-venous shunts (AVS), 4,964 temporary or permanent catheters
(4,411/88.86% femoral, 410/8.26% subclavian, 143/2.88% jugular) and 56 PTFE
vascular grafts. Femoral catheterization (4,312/86.86%) is the favoured solution
if a temporary vascular dialysis access is taken into consideration. The most
popular chronic dialysis angio-access in our country is native AVF (90.5% of
3,440 permanent dialytic vascular accesses). The tunneled subcutaneously
positioned catheters as a permanent dialytic angio-access were present in 270
cases (7.9%): 99 in femoral veins (our original method), 123 in subclavian veins
and 48 catheters in jugular veins. The synthetic vascular grafts-PTFE
(polytetrafluoro-ethylene) represent only 1.6% of all dialysis angio-accesses.
The number of preventive AVFs created in patients with preterminal end-stage
renal disease eventually increased; from 14% in the eighties, 20.8% after 10
years and 31.50% in 1999. Most of the preventive AVFs are done in outpatients
71.8% in 1999. This year 44.4% of all chronic vascular access were created in the
same way. We prefer femoral catheters for both temporary and permanent access
because our results show that femoral catheterization has a lower rate of early
complications when compared to the subclavian catheterization group; the rate of
late complications (thrombosis, stenosis, infections) is lower or the same;
infections in femoral catheterizations are less frequent, compared to subclavian
and jugular ones. Our contributions in the field of vascular access surgery are
the three original methods which are constantly used at the Department: 1.
Combination of temporary (AVS) and permanent vascular access (AVF) using the same
blood vessels, performed in one surgical act; 2. Tunneled femoral catheter as a
permanent vascular access for hemodialysis (2 types: on the abdominal wall and on
the infrainguinal region - thigh); 3. Reduction of hyper-flow in AVF without the
operation of "banding", with ligation of the artery before arteriovenous
anastomosis.
PMID: 12074331 [PubMed - indexed for MEDLINE]
109: Semin Nephrol. 2002 May;22(3):211-20.
Hemodialysis catheters and ports.
Work J.
Renal Division, Emory University, Atlanta, GA 30322, USA. jwork1@emory.edu
Percutaneous placement of cuffed tunneled catheters for hemodialysis access has
become a firmly established method of providing vascular access to patients with
end-stage renal disease. Considerable evidence supports the right internal
jugular vein as the preferred site for catheter insertion. The use of real-time
imaging using both ultrasound and fluoroscopy permits simple, safe, and effective
placement of the catheter for hemodialysis. The use of these imaging techniques
has significantly reduced the number of and severity of complications associated
with catheter placement. A specific method of placement is described including
variations for specific catheter types. The new subcutaneous port as an
alternative to the cuffed tunneled catheter appears to provide another option for
vascular access; preliminary data suggests higher flow rates and lower infection
rates compared with externalized cuffed tunneled catheters. Finally, the criteria
for obtaining training and proficiency in placement of cuffed tunneled catheters
are outlined. Copyright 2002, Elsevier Science.
Publication Types:
Review
PMID: 12012307 [PubMed - indexed for MEDLINE]
110: Chest. 2002 May;121(5):1527-30.
Are femoral Broviac catheters effective and safe? A prospective comparison of
femoral and jugular venous broviac catheters in newborn infants.
Murai DT.
Kapi'olani Medical Center for Women and Children, John A. Burns School of
Medicine, Department of Pediatrics, Honolulu, HI 96826, USA.
STUDY OBJECTIVES: Patients with femoral venous catheters are commonly believed to
be at higher risk of infectious complications as compared to patients with
jugular catheters. Although reports have suggested that femoral venous Broviac
catheters (Davol; Cranston, RI) are safe, no comparisons with jugular catheters
were presented. Thus, we compared our efficacy and complications of femoral and
jugular venous Broviac catheters in newborns. METHODS: We prospectively recorded
demographic data, cannulation requirements, duration of catheter use, and
complications. SETTING: Special-care nursery. PATIENTS: Newborns. INTERVENTIONS:
Insertion of tunneled single-lumen Broviac catheters into vessels of the femoral
triangle or the internal jugular, external jugular, or facial veins by surgical
cutdown. MEASUREMENTS AND RESULTS: Sixty infants had 2,503 catheter-days with 111
catheters. Twenty-six infants had 47 femoral catheters, and 34 infants had 64
jugular catheters. All insertion attempts were successful. The median durations
of catheter use were 24.0 days and 17.0 days for femoral and jugular catheters,
respectively (p = 0.021). Group characteristics, insertion variables, incidences
of complications, and deaths were not significantly different between groups.
CONCLUSIONS: We conclude that compared to jugular catheters, femoral venous
Broviac catheters are an effective means to vascular access, with similar
incidences of complications in newborn infants.
Publication Types:
Comparative Study
PMID: 12006439 [PubMed - indexed for MEDLINE]
111: Pediatr Int. 2002 Feb;44(1):83-6.
Central venous catheters in pediatric patients--subclavian venous approach as the
first choice.
Citak A, Karaböcüoğlu M, Uçsel R, Uzel N.
Pediatric Emergency Department, Institute of Child Health, University of
Istanbul, Istanbul, Turkey. agopcitak@hotmail.com
BACKGROUND: It is critical to establish a safe and functional i.v. access in
severely sick patients. We evaluated the frequency of application and
complications of central venous catheters in a pediatric intensive care unit.
METHODS: Pediatric patients in whom central venous catheters were inserted
between March 1997 and May 1999 in the Pediatric Emergency Room and Intensive
Care Unit were enrolled in this study. Patients were evaluated with respect to
age, sex, weight, central venous catheter indication, site, duration of catheter
stay and complications. RESULTS: During the study period a total of 156 central
venous catheters were successfully inserted into 146 patients. Of the 156 central
venous catheter attempts, 148 (94.9%) were placed into the subclavian vein, six
were inserted into the femoral vein, and two into the jugular vein. In 156
attempts, arterial injuries occurred in 20 cases (12.8%). Pneumothorax developed
in two patients on mechanical ventilation. Three catheters had to be removed due
to catheter related infections. The mortality rate was 0%. CONCLUSIONS: We
concluded that subclavian central venous catheterization is a safe procedure with
minimal complications in pediatric patients. Arterial injury was the most
frequent complication. In experienced hands, the success rate was 100%.
Subclavian central venous catheter insertion may be considered as the first
approach in critically ill patients.
PMID: 11982878 [PubMed - indexed for MEDLINE]
112: Eur J Dermatol. 2002 May-Jun;12(3):291-2.
Guess what! Pseudomonas aeruginosa sepsis.
Bugatti L, Nicolini M, Filosa A, Filosa G.
Department of Dermatology A. Murri Hospital via dei Colli, 52, 60035 Jesi (AN),
Italy. dermjesi@yahoo.it
A 62-year-old woman affected by end-stage renal disease secondary to
Waldenstrom's disease was admitted to place a central venous catheter for
hemodialysis purposes. During the admission, she gradually developed a number of
necrotic ulcerative and fluctuant nodular skin lesions on the submammary
flexures, groins and limbs accompanied by high fever and chills. Yellow-green
purulent material could be drained from the site of introduction of the jugular
catheter. Skin biopsies were taken from the edge of an inguinal
necrotic-ulcerative lesion and from a fluctuant nodular lesion of the thigh,
where pus was drained and cultured.
Publication Types:
Case Reports
PMID: 11978576 [PubMed - indexed for MEDLINE]
113: Cardiovasc Intervent Radiol. 2001 Nov-Dec;24(6):395-9. Epub 2001 Nov 8.
Radiologic placement of a low profile implantable venous access port in a
pediatric population.
Nosher JL, Bodner LJ, Ettinger LJ, Siegel RL, Gribbin C, Asch J, Drachtman RA.
Department of Radiology, UMDNJ-Robert Wood Johnson Medical School, New Brunswick,
NJ 08903-0019, USA. nosher@umdnj.edu
PURPOSE: To evaluate the feasibility and complications of placement of a
low-profile venous access port in the chest in children requiring long-term
venous access. METHOD: A low-profile peripheral arm port (PAS port; Sims Deltec,
St. Paul, MN, USA) was implanted in the chest in 22 children over a 4-year
period. The mean age of the study group was 6 years (range: 9 months to 20
years). Ports were placed for the administration of chemotherapy,
hyperalimentation and frequent blood sampling. Sonographic guidance was used to
access the internal jugular or subclavian vein in each case. A review of all
inpatient and outpatient charts was undertaken to assess catheter performance and
complications. RESULTS: Access to the central venous circulation was successfully
achieved in each case without complication. Ports remained implanted for 6579
catheter-days (mean: 299 days). Ten ports have been removed. Of three patients
(13%) experiencing device-related infections (0.45 infections/1000 catheter
days), two (9.1%) were unresponsive to antibiotics and removed (0.3
infections/1000 catheter days). One port was removed because of pain in the
shoulder adjacent to the port implantation site. One port was removed because of
difficult access. The final port was removed in order to place a dual-lumen
catheter prior to bone marrow transplant. Twelve ports remain implanted.
Aspiration occlusion occurred in four patients (18%). Deep venous thrombosis did
not occur in any patient. CONCLUSION: Low-profile chest ports placed by
interventional radiologists in the interventional radiology suite can be placed
in children as safely as traditional chest ports placed in the operating room.
The incidence of infection, venous thrombosis and aspiration occlusion is
comparable to that of ports placed operatively.
Publication Types:
Evaluation Studies
PMID: 11907746 [PubMed - indexed for MEDLINE]
114: Crit Care Med. 2002 Feb;30(2):454-60.
Comment in:
Crit Care Med. 2002 Feb;30(2):486-7.
Crit Care. 2003 Dec;7(6):397-9.
Complications of central venous catheters: internal jugular versus subclavian
access--a systematic review.
Ruesch S, Walder B, Tramèr MR.
Division of Anaesthesiology, Department Anaesthesiology, Pharmacology, and
Surgical Intensive Care, University Hospitals of Geneva, Geneva, Switzerland.
OBJECTIVE: To test whether complications happen more often with the internal
jugular or the subclavian central venous approach. DATA SOURCE: Systematic search
(MEDLINE, Cochrane Library, EMBASE, bibliographies) up to June 30, 2000, with no
language restriction. STUDY SELECTION: Reports on prospective comparisons of
internal jugular vs. subclavian catheter insertion, with dichotomous data on
complications. DATA EXTRACTION: No valid randomized trials were found. Seventeen
prospective comparative trials with data on 2,085 jugular and 2,428 subclavian
catheters were analyzed. Meta-analyses were performed with relative risk (RR) and
95% confidence interval (CI), using fixed and random effects models. DATA
SYNTHESIS: In six trials (2,010 catheters), there were significantly more
arterial punctures with jugular catheters compared with subclavian (3.0% vs.
0.5%, RR 4.70 [95% CI, 2.05-10.77]). In six trials (1,299 catheters), there were
significantly less malpositions with the jugular access (5.3% vs. 9.3%, RR 0.66
[0.44-0.99]). In three trials (707 catheters), the incidence of bloodstream
infection was 8.6% with the jugular access and 4.0% with the subclavian access
(RR 2.24 [0.62-8.09]). In ten trials (3,420 catheters), the incidence of hematoor pneumothorax was 1.3% vs. 1.5% (RR 0.76 [0.43--1.33]). In four trials (899),
the incidence of vessel occlusion was 0% vs. 1.2% (RR 0.29 [0.07-1.33]).
CONCLUSIONS: There are more arterial punctures but less catheter malpositions
with the internal jugular compared with the subclavian access. There is no
evidence of any difference in the incidence of hemato- or pneumothorax and vessel
occlusion. Data on bloodstream infection are scarce. These data are from
nonrandomized studies; selection bias cannot be ruled out. In terms of risk, the
data most likely represent a best case scenario. For rational decision-making,
randomized trials are needed.
Publication Types:
Comparative Study
Meta-Analysis
Research Support, Non-U.S. Gov't
Review
PMID: 11889329 [PubMed - indexed for MEDLINE]
115: Indian J Pathol Microbiol. 2001 Apr;44(2):125-9.
Infective complications of central venous catheters in cardiac surgical patients.
Dhawan B, Chaudhry R, Hote M, Bhan A, Venugopal P.
Department of Microbiology & Cardiothoracic Centre, All India Institute of
Medical Sciences, New Delhi.
Prospective randomised study was conducted over a 24 months period in a cardiac
surgical intensive care unit to determine the incidence of infection associated
with multilumen venous catheters. The influence of various factors including
fever, peripheral blood culture, catheter site, catheter usage for monitoring
central venous pressure and/inotrope therapy on infection rates were
statistically evaluated. A total of 100 catheters submitted to the Microbiology
laboratory were bacteriologically examined. Forty-nine of these were inserted
into upper body sites, and 51 were inserted into the femoral vein. Twenty-one
were triple-lumen catheters. Catheters were removed when a central line was no
longer necessary. Catheter tips were cultured by semiquantitative technique for
aerobic and anaerobic bacteria. Bacteremia occurred in 3% of catheter insertions;
(Enterococcus faecalis, one; Enterobacter spp. One; Acinetobacter spp., one); and
catheter colonisation developed in 24%. Neither catheter colonisation nor
catheter related infection were associated with any of the risk factors
evaluated. Our data indicates that central venous catheters are safe to use in
our patients. The inability to identify "risk factors" for catheter infection
emphasise the need to maintain a high index of suspicion.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 11883126 [PubMed - indexed for MEDLINE]
116: Korean J Intern Med. 2001 Dec;16(4):242-6.
Percutaneous catheterization of the internal jugular vein for hemodialysis.
Yeum CH, Kim SW, Nah MY, Ma SK, Ko JH, Kim NH, Choi KC.
Department of Internal Medicine, Seonam University College of Medicine, Gwangju,
Korea.
OBJECTIVES: The present study was aimed at evaluating the clinical experiences in
the internal jugular venous catheterization for hemodialysis. METHODS: We
retrospectively analyzed the data on internal jugular venous catheterization at
Chonnam National University Hospital from May 2000 to February 2001. RESULTS:
There were 132 uremic patients with a total of 150 attempts of internal jugular
cannulation. Overall success rate was 90.9% with average puncture trials of 2.3
+/- 2.1. 124 (82.7%) of the catheterization attempts were made on the right side
and 26 (17.3%) were made on the left. The catheters were left in place from 2 to
87 days with an average of 19.5 +/- 15.3 days per catheter. The dialysis sessions
per catheter were from 2 to 58 with an average of 11.3 +/- 6.8. The mean blood
flow during hemodialysis immediately after catheterization was 213.4 +/- 42.2
ml/min. Thirty two (21.3%) patients had early complications. These included
carotid artery puncture (11.3%), local bleeding (4.7%), local pain (3.3%), neck
hematoma (0.7%) and malposition of the catheter (1.3%). Seventeen (11.3%)
patients had late complications. These included fever or infection (11.3%),
inadequate blood flow rate (3.3%) and inadvertent withdrawal (2.0%). There was no
catheter-related mortality. CONCLUSIONS: Our experiences revealed that the
internal jugular vein catheterization is relatively safe and efficient for
temporary vascular access for hemodialysis.
PMID: 11855153 [PubMed - indexed for MEDLINE]
117: Semin Dial. 2001 Nov-Dec;14(6):432-5.
Acute dialysis catheters.
Oliver MJ.
Division of Nephrology, Department of Medicine, Sunnybrook and Women's College
Health Sciences Centre, Toronto, Ontario, Canada. mathew.oliver@swchsc.on.ca
Acute dialysis catheters are non-cuffed, non-tunnelled catheters used for
immediate vascular access. They are primarily used for acute renal failure in
bed-bound patients and for short-term use in patients with malfunction of
permanent access. Long-term use of acute catheters is not recommended, but does
occur with acceptable infection rates in dialysis centers where tunnelled, cuffed
catheters are not available. Most acute catheters are made of polyurethane, but
silicone catheters are now available with larger lumen sizes capable of
delivering blood flow rates over 300 ml/min. Acute catheters should be inserted
in the internal jugular or femoral vein under ultrasound guidance to minimize
complications. Subclavian catheters cause stenosis, thrombosis, and perforation
of vessels. Intermittent catheter malfunction still occurs, particularly for
left-sided internal jugular catheters and catheters placed in women. Blood flow
may improve with lumen reversal, intraluminal t-PA, or guidewire exchange.
Limiting duration of use and dressing catheter exit sites with dry gauze and
antiseptic ointments can prevent catheter-related infections.
Publication Types:
Review
PMID: 11851928 [PubMed - indexed for MEDLINE]
118: Haemophilia. 2001 Nov;7(6):551-6.
Complications of central venous catheters in patients with haemophilia and
inhibitors.
Morado M, Jimenez-Yuste V, Villar A, Quintana M, Del Castillo F, Garzon G,
Acitores I, Ibañez F, Sanjurjo MJ, Gago J, Hernandez-Navarro F.
Haemophilia Centre, Servicio de Hematología y Hemoterapia, Hospital Universitario
La Paz, Madrid, Spain. martamorado@hotmail.com
We report our clinical experience with central venous catheters (CVCs) in 15
patients with haemophilia who, in total, had 34 catheters inserted. Eighteen
devices were Hickman, six were Port-A-Cath and 10 were nontunnelled catheters
(one Quinton, seven antecubital, one jugular and one subclavian vein access). All
patients had factor VIII/IX inhibitors at the time of insertion. The mean age at
operation was 8.8 years (range 16 months-39 years). Eight of the 15 patients
(26/34 implanted catheters, 76%) presented some kind of complication.
Pericatheter bleeding during the postoperative period affected a total of seven
CVCs (7/34, 20%) in six patients, which required substitutive treatment for
several days. Infection was reported in 15 of the CVCs (15/34, 44%), and four of
these (4/15, 26%) had more than one episode, with a mean of 1.4 infection
episodes per catheter (21/15). The infection rate was 0.2 infections per 1000
patient days or 0.1 per 1000 catheter days. Despite the usefulness of CVCs in
haemophilic patients, the high incidence of complications requires careful
assessment of the type of device as well as continuous surveillance.
Publication Types:
Evaluation Studies
PMID: 11851752 [PubMed - indexed for MEDLINE]
119: Cancer. 2002 Jan 1;94(1):245-51.
Catheter-related infection and thrombosis of the internal jugular vein in
hematologic-oncologic patients undergoing chemotherapy: a prospective comparison
of silver-coated and uncoated catheters.
Harter C, Salwender HJ, Bach A, Egerer G, Goldschmidt H, Ho AD.
Department of Internal Medicine V, University of Heidelberg, Heidelberg, Germany.
Christoph.Harter@t-online.de
BACKGROUND: Catheter-related venous thrombosis is one of the most frequent
complications of central venous catheters (CVCs). This complication occurs in 440% of patients with hematologic malignancies receiving conventional chemotherapy
after placement of CVCs. METHODS: The objective of this prospective study was to
assess whether a silver-coated CVC poses an additional risk in the development of
catheter-related thrombosis in hematologic-oncologic patients. Patients were
randomized to receive either silver-coated polyurethane catheters (BactiGuard;
Metacot, Stockholm, Sweden) or uncoated standard polyurethane catheters
(Cavatheter, Fresenius AG, Bad Homburg, Germany) for central venous access.
Silver-coated catheters (n = 120) and standard catheters (n = 113) were inserted
into the jugular vein in 233 consecutive patients. Variables that may be
significant for the development of thrombosis were comparable in the two groups.
After removal of the CVC, the patency of both jugularian veins internal as well
as external was assessed with real-time ultrasound (Sonolayer-SAL-35A; Toshiba,
Tokyo, Japan). RESULTS: Four of 233 patients (1.5%) were found to have venous
thrombosis. Incomplete occlusion of the internal jugular vein occurred in 2
patients (0.75%, parietal thrombosis), and complete thrombosis, although
clinically silent, was found in 2 patients (0.75%). There was no difference
between patients with silver-coated and uncoated CVCs. CONCLUSIONS: The authors
concluded that this novel silver-coated CVC does not cause a higher rate of
central venous thrombosis compared with standard CVCs. The low overall incidence
of central venous thrombosis might be attributed to the routine application of
low-dose heparin in our patients during chemotherapeutic treatment. Copyright
2002 American Cancer Society.
Publication Types:
Clinical Trial
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 11815983 [PubMed - indexed for MEDLINE]
120: Radiology. 2001 Dec;221(3):697-703.
Outcomes and performance of the Tesio twin catheter system placed for
hemodialysis access.
Wivell W, Bettmann MA, Baxter B, Langdon DR, Remilliard B, Chobanian M.
Department of Radiology, Dartmouth-Hitchcock Medical Center, One Medical Center
Dr, Lebanon, NH 03756, USA.
PURPOSE: To assess the effectiveness of and outcomes with a twin catheter system.
MATERIALS AND METHODS: The authors retrospectively reviewed the medical records,
hemodialysis records, and clinical information system data from 132 consecutive
patients who were referred for placement of a tunneled catheter for hemodialysis
access. A commercially available twin catheter system was placed in all patients.
Outcomes evaluated included infection rate, complication rate, and catheter
malfunction and failure rates. Performance parameters evaluated included blood
flow rates, urea reduction percentages, and recirculation percentages. RESULTS:
One hundred eighty-four twin catheter systems were placed in 132 patients from
January 11, 1996, to October 23, 1997. The initial technical success rate was
100%. There were four immediate procedural complications: Air emboli occurred in
two patients, and prolonged bleeding necessitating intervention occurred in two.
The total number of days a catheter was in place was 13,200 (mean, 74.6 days).
Thirty-one infections occurred in 20 patients (total infection rate, 0.23
episodes per 100 catheter days). Sixty-five catheters malfunctioned during the
study period, 19 of which necessitated removal, for a rate of 0.14 episodes per
100 catheter days. The average blood flow rate was 281.4 mL/min (range,
117.1-405.6 mL/min; median, 295.2 mL/min). Mean and median urea reductions were
both 61%. Mean and median recirculation was 6.1% and 3.5%, respectively (range,
0%-31%). CONCLUSION: Percutaneous placement of the tunneled twin catheter system
can be performed with excellent technical success and safety and acceptable
catheter performance and outcomes for effective intermediate- to long-term
hemodialysis.
Publication Types:
Clinical Trial
PMID: 11719665 [PubMed - indexed for MEDLINE]
121: Arch Dis Child Fetal Neonatal Ed. 2001 Sep;85(2):F119-22.
Percutaneous femoral arterial and venous catheterisation during neonatal
intensive care.
Wardle SP, Kelsall AW, Yoxall CW, Subhedar NV.
Department of Child Health, University of Liverpool, Liverpool Women's Hospital,
Liverpool, UK.
BACKGROUND: Femoral vessel catheterisation is generally avoided in the neonatal
period because of technical difficulties and the fear of complications. AIM: To
review the use of femoral arterial and venous catheters inserted percutaneously
on the neonatal intensive care unit. METHODS: Infants admitted to one of two
regional neonatal intensive care units who underwent femoral vessel
catheterisation were identified. Information collected included basic details,
indication for insertion of catheter, type of catheter and insertion technique,
duration of use, and any catheter related complications. RESULTS: Sixty five
femoral catheters were inserted into 53 infants. The median gestational age was
29 weeks (range 23-40). Twenty three femoral arterial catheters (FACs) were
inserted into 21 infants and remained in situ for a median of three days (range
one to eight). Twelve (52%) FACs remained in place until no longer required, and
four (17%) infants developed transient ischaemia of the distal limb. Forty two
femoral venous catheters (FVCs) were inserted into 40 infants and remained in
situ for a median of seven days (range 1-29). Twenty seven (64%) FVCs remained in
place until no longer required, and eight (19%) catheters were removed because of
catheter related bloodstream infection. CONCLUSIONS: FACs and FVCs are useful
routes of vascular access in neonates when other sites are unavailable.
Complications from femoral vessel catheterisation include transient lower limb
ischaemia with FACs and catheter related bloodstream infection.
Publication Types:
Multicenter Study
PMID: 11517206 [PubMed - indexed for MEDLINE]
122: Ann Acad Med Singapore. 2001 Jul;30(4):419-29.
Catheter-related infection: diagnosis, prevention and treatment.
Heard SO.
Department of Anesthesiology, Umass Memorial Medical Center, 55 Lake Avenue
North, Worcester, MA 01655, USA. stephen.heard@umassmed.edu
INTRODUCTION: Catheter infection continues to be a serious problem in critically
ill patients. This review will examine the incidence, epidemiology, microbiology,
diagnosis, risk factors for and treatment of catheter-related bloodstream
infections. METHODS: Relevant articles were culled from a Medline search and
other review articles on catheter-related infection. Important abstracts
presented within the past year were included in the review if the data had not
been published in a peer-reviewed journal. RESULTS: Catheter-related bloodstream
infections (CRBSI) increase morbidity and the cost of care of patients. The
predominant organisms associated with CRBSI are coagulase negative staphylococci,
enterococci and Staphylococcus aureus. Diagnosis usually requires catheter
removal and culture but newer techniques such as "differential time to
positivity" may permit diagnosis of CRBSI in situ. Reducing risk factors for
infection are important: education of house staff, use of the subclavian
insertion site, skin preparation with chlorhexidine solutions, use of maximum
barrier precautions during catheter insertion and catheter maintenance with
chlorhexidine sponges. If infection rates are still high after institution of
these measures, use of antiseptic or antibiotic-impregnated catheters should be
considered. Treatment of CRBSI in critically ill patients mandates catheter
removal and treatment with systemic antibiotics. CONCLUSIONS: The best treatment
for CRBSI is prevention. Ongoing studies are evaluating the effectiveness of
newer antiseptic catheters, the risk of developing antibiotic resistance when
using antibiotic-impregnated catheters and the contribution of multiple
interventions on the development of CRBSI.
Publication Types:
Review
PMID: 11503552 [PubMed - indexed for MEDLINE]
123: JAMA. 2001 Aug 8;286(6):700-7.
Comment in:
ACP J Club. 2002 Jan-Feb;136(1):1.
Complications of femoral and subclavian venous catheterization in critically ill
patients: a randomized controlled trial.
Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, Rigaud JP,
Casciani D, Misset B, Bosquet C, Outin H, Brun-Buisson C, Nitenberg G; French
Catheter Study Group in Intensive Care.
Service de Réanimation Médicale, Hôpital de Poissy/St Germain-en-Laye, 10 Rue du
Champ-Gaillard, 78303 Poissy, France. jmerrer@chi-poissy-st-germain.fr
CONTEXT: Whether venous catheterization at the femoral site is associated with an
increased risk of complications compared with that at the subclavian site is
debated. OBJECTIVE: To compare mechanical, infectious, and thrombotic
complications of femoral and subclavian venous catheterization. DESIGN AND
SETTING: Concealed, randomized controlled clinical trial conducted between
December 1997 and July 2000 at 8 intensive care units (ICUs) in France. PATIENTS:
Two hundred eighty-nine adult patients receiving a first central venous catheter.
INTERVENTIONS: Patients were randomly assigned to undergo central venous
catheterization at the femoral site (n = 145) or subclavian site (n = 144). MAIN
OUTCOME MEASURES: Rate and severity of mechanical, infectious, and thrombotic
complications, compared by catheterization site in 289, 270, and 223 patients,
respectively. RESULTS: Femoral catheterization was associated with a higher
incidence rate of overall infectious complications (19.8% vs 4.5%; P<.001;
incidence density of 20 vs 3.7 per 1000 catheter-days) and of major infectious
complications (clinical sepsis with or without bloodstream infection, 4.4% vs
1.5%; P =.07; incidence density of 4.5 vs 1.2 per 1000 catheter-days), as well as
of overall thrombotic complications (21.5% vs 1.9%; P<.001) and complete
thrombosis of the vessel (6% vs 0%; P =.01); rates of overall and major
mechanical complications were similar between the 2 groups (17.3% vs 18.8 %; P
=.74 and 1.4% vs 2.8%; P =.44, respectively). Risk factors for mechanical
complications were duration of insertion (odds ratio [OR], 1.05; 95% confidence
interval [CI], 1.03-1.08 per additional minute; P<.001); insertion in 2 of the
centers (OR, 4.52; 95% CI, 1.81-11.23; P =.001); and insertion during the night
(OR, 2.06; 95% CI, 1.04-4.08; P =.03). The only factor associated with infectious
complications was femoral catheterization (hazard ratio [HR], 4.83; 95% CI,
1.96-11.93; P<.001); antibiotic administration via the catheter decreased risk of
infectious complications (HR, 0.41; 95% CI, 0.18-0.93; P =.03). Femoral
catheterization was the only risk factor for thrombotic complications (OR, 14.42;
95% CI, 3.33-62.57; P<.001). CONCLUSION: Femoral venous catheterization is
associated with a greater risk of infectious and thrombotic complications than
subclavian catheterization in ICU patients.
Publication Types:
Clinical Trial
Comparative Study
Multicenter Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 11495620 [PubMed - indexed for MEDLINE]
124: Cardiovasc Intervent Radiol. 2001 May-Jun;24(3):180-4.
Central venous access ports placed by interventional radiologists: experience
with 125 consecutive patients.
Lorch H, Zwaan M, Kagel C, Weiss HD.
Department of Radiology, Medical University of Lübeck, Ratzeburger Allee 160,
D-23538 Lübeck, Germany. lorch@medinf.mu-luebeck.de
PURPOSE: To assess safety and function of central venous port systems implanted
percutaneously in the interventional radiology suite. METHODS: One hundred and
twenty-five consecutive ports in 123 patients were evaluated retrospectively. One
hundred and twenty ports were implanted via the subclavian vein. RESULTS:
Technical success was 100%. Fourteen patients (11.2%) experienced immediate
procedural complications, all minor (pneumothorax 1.6%). During follow-up (4-343
days, mean service period 97.8 days), nine complications occurred, six of which
were major. These were three port infections which led to hospitalization and
port removal, one chamber penetration through the skin, and two port occlusions.
Port removal as a result of complications was performed in six patients.
Altogether, 20 complications occurred within a total of 11,056 days of service,
which means 1.8 events per 1000 days of service. CONCLUSION: Percutaneous
implantation of central venous port systems is safe and easy to perform.
Complication rates of this study compare favorably with those of other
radiological and surgical series.
PMID: 11443406 [PubMed - indexed for MEDLINE]
125: Pediatrics. 2001 Jun;107(6):E104.
Tunneled femoral central venous catheters in children with cancer.
Sovinz P, Urban C, Lackner H, Kerbl R, Schwinger W, Dornbusch H.
Department of Pediatrics, Division of Pediatric Hematology and Oncology,
University of Graz, Auenbruggerplatz, Graz, Austria.
petra.sovinz@klinikum-graz.at
OBJECTIVE: We discuss the feasibility of long-term femoral venous access by means
of a cuffed subcutaneously tunneled central venous catheter (Broviac catheter) in
selected pediatric cancer and stem cell transplant patients in whom access via
the veins of the upper part of the torso is difficult or contraindicated and in
whom alternative routes must be used. PATIENTS AND METHODS: We report on our
experience with 9 patients (3 of whom underwent stem cell transplantation) who
received femoral Broviac catheters between December 1990 and November 1999.
Results. Time in place ranged from 4 to 155 days with a median of 58 days (mean:
71.2 days). Three catheters had to be removed: 1 because of infection of the
subcutaneous tunnel and 2 because of catheter obstruction. The remaining 6
catheters functioned well without problems as long as they were needed; 1 of them
got accidentally dislodged while the patient was off treatment. No episodes of
catheter-related septicemia, thrombosis, kinking, or drug extravasation were
noted; there were no catheter-related infectious complications in the transplant
patients. CONCLUSIONS: Our experience indicates that in those instances in which
customary access to the superior vena cava is precluded, long-term venous access
by way of the femoral vein is a feasible and safe alternative in children, even
in the setting of stem cell transplantation.
Publication Types:
Clinical Trial
PMID: 11389302 [PubMed - indexed for MEDLINE]
126: J Clin Anesth. 2001 Mar;13(2):131-2.
An unusual complication during central venous catheter placement.
Duong MH, Jensen WA, Kirsch CM, Wehner JH, Kagawa FT.
Department of Medicine and the Division of Respiratory and Critical Care
Medicine, Santa Clara Valley Medical Center, San Jose, CA 95128, USA.
A 31-year-old man with disseminated Coccidioides imitis infection required
central catheter placement for access. The patient had an inferior vena cava
(IVC) filter placed as a result of previous deep venous thrombosis of the left
lower extremity. The guidewire could not be removed following placement of the
right internal jugular catheter by the Seldinger technique. Fluoroscopic
examination revealed entanglement of the J-tip guidewire in the apex of the IVC
filter. The catheter was successfully removed by interventional radiologists
using a snare tip catheter through the left femoral vein.
Publication Types:
Case Reports
PMID: 11331175 [PubMed - indexed for MEDLINE]
127: Europace. 2001 Jan;3(1):56-9.
Permanent pacemaker implantation via the femoral vein: an alternative in cases
with contraindications to the pectoral approach.
Mathur G, Stables RH, Heaven D, Ingram A, Sutton R.
Department of Invasive Cardiology and Electrophysiology, Royal Brompton Hospital,
Sydney Street, London SW3 6NP, UK.
BACKGROUND: This paper presents a consecutive series of permanent pacemakers
(PPM) implanted via the femoral vein in patients with contraindications to pacing
systems via the superior vena cava (SCV). The femoral vein approach is a less
invasive and feasible alternative to epicardial lead placement. METHODS:
Twenty-seven patients had femoral pacemakers inserted. Indications for femoral
vein pacemaker insertion were: SVC/subclavian obstruction (12 patients, 44.4%),
previous infection in SVC leads (four patients, 14.8%), mastectomy and/or
radiotherapy to chest (four patients, 14.8%), multiple leads in SVC (two
patients, 7.4%), recurrent erosion (two patients, 7.4%), abnormal anatomy (one
patient, 3.7%), painful pacemaker pocket (one patient, 3.7%) and burns (one
patient, 3.7%). Fifty-one leads, 25 atrial and 26 ventricular, were inserted. The
majority of leads were active fixations (96% of atrial leads and 85% ventricular
leads). RESULTS: During a mean follow-up of 36.5 months (range 0.9-116.5), six
additional unplanned procedures were performed in four patients. Atrial lead
displacement occurred in five leads (20%). There were no ventricular lead
displacements. In two patients, box revision for pre-erosion was required. One
patient had persistent pain at the site of abdominal pacemaker generator.
Infection, thromboembolic events, thromophlebitis, evidence of lower limb venous
occlusion and lead fracture did not occur. CONCLUSION: Femoral vein PPM are a
simple and feasible alternative in patients in whom the SVC approach is
contraindicated.
Publication Types:
Comparative Study
PMID: 11271953 [PubMed - indexed for MEDLINE]
128: AJR Am J Roentgenol. 2001 Apr;176(4):991-4.
Radiologic placement of implantable chest ports in pediatric patients.
Lorenz JM, Funaki B, Van Ha T, Leef JA.
Department of Radiology, The University of Chicago Hospitals, 5841 S. Maryland
Ave., MC 2026, Chicago, IL 60637, USA.
OBJECTIVE: We evaluated the technical success and complications associated with
radiologic placement of implantable chest ports in children for long-term central
venous access. MATERIALS AND METHODS: Between May 1, 1996 and January 11, 2000,
29 chest ports were placed in 28 children (15 girls, 13 boys; age range, 2-17
years; mean, 11.7 years). The patient's right internal jugular vein was used for
access in 93% (27/29) of the procedures, and a collateral neck vein was used as a
conduit to recanalize the central veins in two procedures because of bilateral
jugular and subclavian vein occlusion. All procedures were performed in
interventional radiology suites. Both real-time sonography and fluoroscopy were
used to guide venipuncture and port insertion. Follow-up data were obtained
through the clinical examination and electronic review of charts. RESULTS:
Technical success was 100%. Fourteen percent of the catheters were removed
prematurely, including one catheter removed 17 days after placement because the
patient's blood cultures were positive for Candida albicans. No patients
experienced hematoma, symptomatic air embolism, symptomatic central venous
thrombosis, catheter malposition, or pneumothorax. The median number of days for
catheter use by patients was 280 days (total, 9043 days; range, 17-869 days). The
rate of confirmed catheter-related infection was 14% or 0.04 per 100 venous
access days. One catheter occluded after 132 days. CONCLUSION: In pediatric
patients, radiologists can insert implantable chest ports using real-time
sonographic and fluoroscopic guidance with high rates of technical success and
low rates of complication.
PMID: 11264096 [PubMed - indexed for MEDLINE]
129: Am J Nephrol. 2000 Nov-Dec;20(6):476-82.
Transverse cervical artery pseudoaneurysm: a rare complication of internal
jugular vein cannulation.
Cuhaci B, Khoury P, Chvala R.
Department of Medicine, Hahnemann Hospital, MCP/Hahnemann University,
Philadelphia, PA 19129, USA. bulentcuhaci@yahoo.com
Internal jugular vein cannulation has become the preferred approach for temporary
hemodialysis catheter placement following reports of an increased incidence of
subclavian vein stenosis due to subclavian vein catheterization. Internal jugular
vein catheterization is associated with a high rate of successful catheter
placement. However, significant complications such as internal carotid artery
(ICA) puncture, pneumothorax, vessel erosion, thrombosis, airway obstruction and
infection can occur. The most common complication is ICA puncture. More recently
a few cases of thyrocervical trunk pseudoaneurysm and fistula following internal
jugular vein and subclavian vein catheterization attempts have been reported.
Patients with renal failure who are on hemodialysis may have to undergo multiple
catheter placements and vascular access interventions. This, along with their
comorbid conditions, increases the risk of such complications. Here we report a
patient on hemodialysis who developed transverse cervical artery pseudoaneurysm
following an attempted right internal jugular vein catheterization. We report
this case because of its rarity, to raise awareness of such a complication and to
discuss different treatment options, in particular endovascular coil occlusion. A
review of relevant literature is also presented. Copyright 2000 S. Karger AG,
Basel.
Publication Types:
Case Reports
Review
PMID: 11146316 [PubMed - indexed for MEDLINE]
130: Kidney Int. 2000 Dec;58(6):2543-5.
Risk of bacteremia from temporary hemodialysis catheters by site of insertion and
duration of use: a prospective study.
Oliver MJ, Callery SM, Thorpe KE, Schwab SJ, Churchill DN.
Division of Nephrology, Duke University Medical Center, Durham, North Carolina,
USA.
BACKGROUND: Uncuffed, nontunneled hemodialysis catheters remain the preferred
means to gain immediate access to the circulation for hemodialysis. Bacteremia is
the primary complication that limits their use. The risk of bacteremia by site of
insertion and duration of use has not been well studied. METHODS: Two hundred
eighteen consecutive patients who required a temporary hemodialysis catheter were
prospectively followed. RESULTS: Catheters were placed at 318 new insertion sites
and remained in use for a total of 6235 days. The incidence of bacteremia was
5.4% after three weeks of placement in internal jugular vein and 10.7% after one
week in femoral vein [relative risk for bacteremia 3.1 (95% CI, 1.8 to 5.2)]. The
incidence of bacteremia was 1.9% one day after the onset of an exit site
infection but increased to 13.4% by the second day if the catheter was not
removed. Guidewire exchange for malfunction and patient factors did not
significantly affect the risk of bacteremia. CONCLUSIONS: Internal jugular
catheters may be left in place for up to three weeks without a high risk of
bacteremia, but femoral catheters in bed-bound patients should be removed after
one week. Catheter exchanges over a guidewire for catheter malfunction do not
increase bacteremia rates. Temporary catheters should be removed immediately if
an exit site infection occurs.
Publication Types:
Clinical Trial
Research Support, Non-U.S. Gov't
PMID: 11115089 [PubMed - indexed for MEDLINE]
131: Radiology. 2000 Oct;217(1):89-93.
Tunneled infusion catheters: increased incidence of symptomatic venous thrombosis
after subclavian versus internal jugular venous access.
Trerotola SO, Kuhn-Fulton J, Johnson MS, Shah H, Ambrosius WT, Kneebone PH.
Departments of Radiology and Medicine, Indiana University School of Medicine,
University Hospital, Rm 0279, 550 N University Blvd, Indianapolis, IN 46202-5253,
USA. streroto@iupui.edu
PURPOSE: To compare the incidence of symptomatic venous thrombosis after tunneled
infusion catheter placement via the internal jugular vein (IJV) versus the
subclavian vein (SCV). MATERIALS AND METHODS: A retrospective analysis was
performed of 774 catheters placed. Only patients with complete follow-up were
included, which yielded a population of 279 catheters in 238 patients (166 in the
SCV, 113 in the IJV; total of 26,242 catheter days). All catheters were placed by
interventional radiologists with ultrasonographic (in IJV) or venographic (in
SCV) guidance. RESULTS: Initial complications were limited to one pneumothorax in
the SCV group and one episode of oversedation in the IJV group. There was no
difference in infection rates between the two sites (SVC vs IJV: 0.25 vs 0.32 per
100 catheter days; P >.99). The mean dwell time was slightly longer for SCV
catheters (103 days) than for IJV catheters (79 days) (P =.04). Venous thrombosis
developed in 13% of patients (0.12 per 100 catheter days) with an SVC catheter
placed as compared with in 3% (0.04 per 100 catheter days) with an IJV catheter
(P =.018). This difference persisted after adjustment for catheter size and side
of placement (P =.025). The mean time to thrombosis was 36 days for SCV catheters
and 142 days for IJV catheters. CONCLUSION: The IJV is the preferred site for
tunneled infusion catheter placement because of the lower incidence of
symptomatic venous thrombosis.
Publication Types:
Comparative Study
Research Support, Non-U.S. Gov't
PMID: 11012428 [PubMed - indexed for MEDLINE]
132: Surg Laparosc Endosc Percutan Tech. 2000 Aug;10(4):264-7.
Isolated thrombosis of the external jugular vein.
Colomina MJ, Godet C, Bagó J, Pellisé F, Puig O, Villanueva C.
Department of Anesthesiology, Hospital Unversitario Traumatología Vall D'Hebron,
Barcelona, Spain.
Thrombosis of the external jugular vein (EJV) is an infrequent clinical condition
that has been associated with central venous catheterization, head and neck
infections, intravenous drug abuse, and compression at the affected site. The
authors report a case of thrombotic obstruction of the EJV in the late
postoperative period after laparoscopic anterior lumbar interbody fusion. A
40-year-old morbidly obese woman with a depressive syndrome was diagnosed with
L5-S1 discopathy and was submitted to laparoscopic anterior isthmic fusion. The
operation lasted approximately 6 hours, during which the patient remained in a
supine decubitus and Trendelenburg position. The left radial artery, peripheral
veins, and right internal jugular vein were canalized. The internal jugular vein
catheter was electively withdrawn 24 hours after the intervention. The
postoperative period was satisfactory, and the patient was started on prophylaxis
with low-molecular-weight heparin. She sat up and began walking at 24 hours and
was discharged to her home 4 days after the procedure. Eight days after discharge
she returned, experiencing right cervical pain. Palpation revealed a painful
induration and erythematous area under the anterior edge of the
sternocleidomastoid muscle. Results of otoscopy and laryngoscopy were normal.
Cervical echo-Doppler disclosed an image consistent with EJV thrombosis. The most
frequent causes of jugular vein thrombosis are mentioned above. A higher
incidence has been described after upper abdomen and pelvic surgery; other
contributing factors are age, obesity, and associated illness. There are few
references in the literature to position-induced EJV thrombosis in the late
postoperative period. The authors' patient presented signs and symptoms of EJV
thrombosis (probably because of various factors), which was confirmed by
echo-Doppler study and treated with 10 days of calcic heparin.
Publication Types:
Case Reports
PMID: 10961761 [PubMed - indexed for MEDLINE]
133: Ann Surg Oncol. 2000 Aug;7(7):496-502.
Comment in:
Chir Ital. 2003 Mar-Apr;55(2):313.
A prospective analysis of the cephalic vein cutdown approach for chronic
indwelling central venous access in 100 consecutive cancer patients.
Povoski SP.
Department of Surgery, West Virginia University, Robert C. Byrd Health Science
Center, Morgantown 26506, USA. spovoski@hsc.wvu.edu
BACKGROUND: Chronic indwelling central venous access devices (CICVAD) generally
are placed by the percutaneous subclavian vein approach. The cephalic vein
cutdown approach is used only infrequently. Although the technique has been well
described, few prospective data are available on the cephalic vein cutdown
approach. METHODS: From September 9, 1998, to July 20, 1999, the cephalic vein
cutdown approach was attempted in 100 consecutive cancer patients taken to the
operating room with the intention of placing CICVAD. Median patient age was 54.5
years (range 18-88), with 46 men and 54 women. Twenty-five patients had
gastrointestinal malignancies, 17 had breast cancer, 15 had lymphoma, 13 had lung
cancer, 12 had leukemia, 5 had multiple myeloma, and 13 had other malignancies.
Patients were followed prospectively for immediate and long-term outcome.
RESULTS: CICVAD placement via the cephalic vein cutdown approach was successful
in 82 patients; the remaining 18 patients required conversion to a percutaneous
subclavian vein approach. The reasons for inability to place CICVAD via cephalic
vein cutdown approach were a cephalic vein that was too small (10 patients), an
absent cephalic vein (7 patients), and inability to traverse the angle of
insertion of the cephalic vein into the subclavian vein (1 patient). There were
56 subcutaneous ports and 26 tunneled catheters. Median operating time was 44
minutes (range, 26-79 minutes). No postoperative pneumothorax occurred. Median
catheter duration was 198 days (range, 0-513 days). Long-term complications
included catheter-related bacteremia (6%), site infection (2%), deep venous
thrombosis (5%), port pocket hematoma (1%), and superior vena cava stricture
(1%). Thirty-seven percent of patients have died since CICVAD placement.
Twenty-nine percent of the CICVADs have been removed. CONCLUSIONS: The cephalic
vein cutdown approach was successful in 82% of patients. This approach is a safe
and useful alternative to the percutaneous subclavian vein approach.
Publication Types:
Clinical Trial
PMID: 10947017 [PubMed - indexed for MEDLINE]
134: Crit Care Med. 2000 May;28(5):1376-82.
The safety of prolonging the use of central venous catheters: a prospective
analysis of the effects of using antiseptic-bonded catheters with daily site
care.
Norwood S, Wilkins HE 3rd, Vallina VL, Fernandez LG, McLarty JW.
East Texas Medical Center, Tyler, USA.
OBJECTIVE: To determine rates of catheter colonization and catheter-related
bloodstream infection (CRBSI) when antiseptic-bonded central venous catheters
(CVCs) and standardized daily site care are used with no predetermined interval
for removal. DESIGN: Prospective observational study. SETTING: Two major trauma
centers. PATIENTS: All trauma patients admitted to two major trauma centers that
received a CVC from May 1996 through May 1998. INTERVENTIONS: None.
MEASUREMENTS
AND MAIN RESULTS: Catheters were semiquantitatively cultured to identify
bacterial colonization and CRBSI. Monitored variables included total catheter
days, anatomical site of catheter insertion, and area in hospital of catheter
insertion. CVC tips and intracutaneous segments were semiquantitatively cultured.
A total of 460 (92%) of 501 catheters placed in 324 trauma patients were
evaluable, representing 95.5% of all catheter days during the study period. Rates
of catheter colonization and CRBSI were 5% (5/1000 catheter days) and 1.5%
(1.511000 catheter days), respectively. Subclavian catheters were in place longer
than femoral or internal jugular catheters (p < .0001), but the colonization rate
was significantly lower (p = .03; relative risk, 0.34; 95% confidence interval,
0.15-0.77). No differences in CRBSI rates among anatomical sites or between
catheters used < or =14 days and those used >14 days were identified. CONCLUSION:
Femoral and internal jugular antiseptic-bonded CVCs develop bacterial
colonization earlier than subclavian CVCs. Subclavian antiseptic-bonded CVCs
combined with standardized daily site care may be safely used >14 days in trauma
patients.
Publication Types:
Comparative Study
PMID: 10834681 [PubMed - indexed for MEDLINE]
135: Minerva Chir. 2000 Mar;55(3):139-46.
[Central venous access systems in the oncologic patient]
[Article in Italian]
Ragusa M, Alberti D, Argento R, Avenia N, Bartolucci R, Esposito S, Ferilli F,
Marini C.
Clinica Chirurgica Generale e Toracica, Università degli Studi, Perugia.
BACKGROUND: A safe and dependable venous access is mandatory in order to perform
cancer chemotherapy and monitor blood values in the neoplastic patient. Prolonged
infusions of medications with sclerosing action may damage the vessel wall,
inducing chemical thrombophlebitis. Furthermore, extravasation of necrotizing
compounds may be a danger to the patient. The application of totally implantable
venous access systems (VAS) started in 1982, in the United States of America,
where at present 500,000 devices are implanted annually. In Italy such method has
been introduced in a later period, with a constantly growing trend. VAS devices
have evolved since their first presentation, and so have application techniques:
the original surgical route has been supported by the percutaneous one,
considered most appropriate by several Centers. In this study, personal
experience concerning application of VAS in cancer patients is presented.
METHODS: From July 1994 to February 1998, at the General Thoracic Surgery Dept.
of the University of Perugia, 198 VAS have been implanted in 195 patients. During
the first period all the systems have been applied by surgical cutdown of the
cephalic vein (150 cases). In the last 12 month the percutaneous technique for
vein puncture has been adopted in 48 patients. RESULTS: Immediate and late
complications have occurred: among the former, pneumothorax, hematoma,
malposition; among the latter, infection, subclavian vein thrombosis, catheter
rupture. The results are analysed after an extensive review of the international
literature; pros and cons of the different implantation techniques and the
technical aspects useful for preventing complications are underlined.
Publication Types:
English Abstract
PMID: 10832298 [PubMed - indexed for MEDLINE]
136: Pacing Clin Electrophysiol. 2000 Apr;23(4 Pt 1):446-9.
Permanent transfemoral pacemaker implantation is the technique of choice for
patients in whom the superior vena cava is inaccessible.
Barakat K, Hill J, Kelly P.
Department of Cardiology, London Chest Hospital, United Kingdom.
K.barakat@mds.qmw.ac.uk
We describe transfemoral pacemaker implantation in three patients in whom pacing
via the superior vena cava was not possible or suboptimal. The first was an
88-year-old man with superior vena cava obstruction presenting with fractured
epicardial pacing leads. Recent pneumonia increased the risks of a general
anesthetic. The second patient was a 57-year-old man who was intolerant of a
pectorally sited pacemaker because of the thinness of his anterior chest wall.
The third patient was a 69-year-old woman who presented with an infected eroding
pectorally sited pacemaker. Scarring secondary to a previous pacemaker infection
rendered the contralateral pectoral site inaccessible. Since the subclavian route
was inaccessible (case 1) or suboptimal (case 2 and 3), we implanted transvenous
pacemakers via the femoral route, which was safe, and effective, during a 6-month
follow-up period.
Publication Types:
Case Reports
PMID: 10793432 [PubMed - indexed for MEDLINE]
137: Heart Lung. 2000 Mar-Apr;29(2):113-7.
Spectrum of upper-extremity deep venous thrombosis in a community teaching
hospital.
Marinella MA, Kathula SK, Markert RJ.
Department of Internal Medicine, Wright State University School of Medicine,
Dayton, Ohio, USA.
OBJECTIVE: The goal of this study was to characterize the spectrum of
upper-extremity deep venous thrombosis in a community teaching hospital. DESIGN
AND SETTING: A retrospective analysis was used at a large urban teaching
hospital. MATERIAL AND METHODS: We reviewed the records of 90 patients with
ultrasound-documented thrombosis of the internal jugular, subclavian, axillary,
or brachial veins to determine clinical characteristics, risk factors, and
outcome. RESULTS: The most common underlying conditions associated with
upper-extremity deep venous thrombosis were the presence of a central venous
catheter in 65 patients (72%), infection in 25 (28%), extrathoracic malignancy in
20 (22%), thoracic malignancy in 19 (21%), renal failure in 19 (21%), and a prior
lower-extremity deep venous thrombosis in 16 (18%). Pain was noted in 31 (34%)
patients, and 76 patients (84%) had edema of the involved extremity. The left
subclavian vein was involved in 44 patients (49%), and 35 patients (39%) had a
central venous catheter in the left subclavian vein. When a central venous
catheter was present, the deep venous thrombosis was usually ipsilateral (P
<.001). Heparin and warfarin were administered to 65 (72%) and 53 (59%) of the
patients, respectively. Eleven patients (12%) died. Of these patients, 8 (73%)
had an underlying infection, whereas only 22% of survivors had an infection (P
=.0012). CONCLUSION: Upper-extremity deep venous thrombosis typically occurs in
patients with a systemic illness in the presence of a central venous catheter.
The left subclavian vein is frequently involved because this is a common site for
placement of a central venous catheter. Pain is uncommon, but edema of the
involved extremity is noted in the majority of patients. The mortality rate of
patients in this study with an upper-extremity deep venous thrombosis was 12%;
most patients who died had a central venous catheter and an underlying infection.
PMID: 10739487 [PubMed - indexed for MEDLINE]