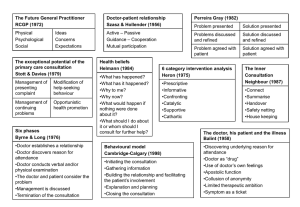
Common MEQ Scenarios
advertisement

1 The Yorkshire MRCGP Prep Course handbook - candidates 2006 edition www.mrcgp.com Yorkshire Faculty of the RCGP 2 3 CONTENTS INTRODUCTION TO THE COURSE AND THE EXAM The Royal College of GPs - membership ...................................................................................................... 7 Why do the MRCGP exam? What Have Other People Who Have Taken it Thought? ....................... 9 Icons Used In this Guide ................................................................................................................................. 11 Do You Want to Pass or Fail? ........................................................................................................................ 13 Course Tutors .................................................................................................................................................... 15 THE MCQ THE MCQ ........................................................................................................................................................... 17 How to fail the MCQ .................................................................................................................................. 19 Preparing for the MCQ .............................................................................................................................. 19 Hot Tips for the MCQ .................................................................................................................................. 20 Format ........................................................................................................................................................... 22 FILLING IN THE BLANKS MADE SIMPLE ...................................................................................................... 23 MCQ PRACTICE (answers at the end) .................................................................................................... 24 MODIFIED ESSAY QUESTIONS Modified Essay Questions (MEQs) ................................................................................................................ 36 What are MEQs all about then? .............................................................................................................. 38 How to fail the Written Paper ................................................................................................................... 38 Preparing for the Written Paper ............................................................................................................... 39 Hot Tips for the Written Paper ................................................................................................................... 40 Specific questions and what they mean ............................................................................................... 41 Answer Construction .................................................................................................................................. 41 Common MEQ Scenarios .......................................................................................................................... 41 MEQs – Made Simple! ................................................................................................................................ 42 Buzz Words and Triads ................................................................................................................................ 43 Mental Grids/Check Lists/Constructs ...................................................................................................... 44 Practise MEQ Paper ................................................................................................................................... 48 CRITICAL READING QUESTIONS Critical Reading Questions (CRQs) .............................................................................................................. 61 How to fail the CRQs .................................................................................................................................. 63 Preparing for the CRQs .............................................................................................................................. 63 Hot Tips for the CRQs .................................................................................................................................. 64 CLINICAL EPIDEMIOLOGY FOR THE MRCGP EXAMINATION................................................................ 65 STATISTICAL TERMS- made simple ............................................................................................................ 77 Critically Evaluating Quantitative Papers – Made Simple! ................................................................. 78 Evaluating Quantitative Papers – Method 2 ......................................................................................... 79 EVALUATING QUALITATIVE PAPERS .......................................................................................................... 80 SCREENING – Made Simple! ......................................................................................................................... 82 Critically Appraising Protocols – MADE SIMPLE! ........................................................................................ 83 A Critical Reading Question Illustrated .................................................................................................. 84 4 THE ORALS The Orals............................................................................................................................................................ 87 Can You Tell Me a Bit More About the Contexts? ............................................................................... 89 Examples of Questions, areas of competence being tested and in what context ...................... 90 What Happens on the Day?..................................................................................................................... 91 Tell me a bit more about the questions ................................................................................................. 92 How to fail the Orals ................................................................................................................................... 92 Preparing for the Orals ............................................................................................................................... 93 Hot Tips for the Orals ................................................................................................................................ 94 Let’s put you at ease….............................................................................................................................. 96 WORKED EXAMPLE: Orals .......................................................................................................................... 97 Practise Oral Questions.............................................................................................................................. 99 Popular Domains tested in the Orals .................................................................................................... 102 MRCGP Orals: Grade Descriptors (revised 05.00) .............................................................................. 104 More on How To Fail The Orals ............................................................................................................... 105 RESOURCES WORTH EXPLORING ............................................................................................................ 106 THE VIDEO The Video (Consulting Skills) ........................................................................................................................ 107 How to fail the Video Component ........................................................................................................ 109 Preparing for the Video Component ................................................................................................... 109 Hot Tips for the MCQ ................................................................................................................................ 110 Asking your trainer to look at the videos .............................................................................................. 111 Consent ...................................................................................................................................................... 111 Try and spend some time with reception staff and explain in detail ................................................. 112 Final Checklist ............................................................................................................................................ 112 30% Fail the Video. Why? ....................................................................................................................... 112 MRCGP Video Assessment Sheet .......................................................................................................... 113 Is Your Collective Video Good Enough? ............................................................................................. 115 …AND NOW FOR SOME OTHER BITS Have You Failed Any Component of the MRCGP exam? ............................................................... 123 Why Patients go to Doctors. ................................................................................................................... 125 MODELS OF THE CONSULTATION ............................................................................................................ 127 SUMMARY 1: Current Models of the Consultation in terms of Dimensions. ................................... 137 SUMMARY 2: THE CONSULTATION MODELS IN TERMS OF TASKS ....................................................... 138 Ethics and Law .......................................................................................................................................... 139 Duties Of the Doctor (GMC)................................................................................................................... 143 Final Word on the Exam… ........................................................................................................................... 144 Hooray, I’ve got my MRCGP. So now what? ......................................................................................... 145 5 Introduction to the Course and Exam 6 7 The Royal College of GPs - membership What’s it all about then? The college was Europe's first academic body for GPs “It is not that we are better doctors, but that we want to become better doctors” (Fraser Rose, 1953) By the way, you might be asked about the RCGP in the orals examination. When was the Royal College of GPs set up? 1952. The examination was introduced in 1965 as the means to entry for new members. Fellows were first appointed in 1967. What are its aims? “to encourage, foster and maintain the highest possible standards in general medical practice and, for that purpose, to take or join with others in taking any steps consistent with the charitable nature of that object which may assist towards the same” Under its royal charter, the college is entitled to: Establish and maintain an academic and educational headquarters for GPs Maintaining an authoritative voice to speak effectively for GPs; lobbying government and other organisations on behalf of GPs and their patients. Taking the initiative for quality patient care in a changing health service Maintain regional faculties to further the college’s objectives Encourage able entrants to medicine and to general practice Undertake training courses designed to enhance the medical knowledge and skill of GPs Grant postgraduate diplomas or other certificates Encourage GPs to publish research into medical and scientific subjects Co-operate with other bodies Can a GP be a member without taking the exam? GPs cannot be full members of the college without first passing the MRCGP exam. There is a separate category of associate membership which those without the MRCGP may wish to consider. With this you can receive the BGJP, RCGP publications and discounts on courses. More on www.rcgp.org.uk . How can “grass root” GPs voice their concerns? All members can give their input via their local RCGP faculty and the area representative on the RCGP council. Tell me more about the RCGP Council. The council represents all members and meets roughly 6 times a year to discuss current issues. The RCGP is run by the council. The council is made up of officers elected by RCGP members or by the members of the council itself. There are also LOCAL faculty meetings (again around 6 times a year) who meet to discuss more local issues and policies. What do members actually get for their money? All members become automatically enrolled in a local faculty which means they have available to them: an educational programme, audit/research opportunities and help, social support and advice. You get the BGJP, RCGP papers and RCGP books at discount price. You can apply for RCGP prizes, travel scholarships and research grants. Access to the RCGP library and information resources centre (including an on-line search service) Support and friendship from like minded colleagues (local faculty support networks) 8 What do you get for your membership? Free monthly copy of the British Journal of General Practice Reduced rates on RCGP publications Use of a comprehensive library and information service Vocational Training Statements free to GP registrars Computer assessment program on CD for GP registrars, available at reduced rates Discounted courses, conferences and study days Residential and conference accommodation at the College's headquarters in London Local support networks through the RCGP's faculties The opportunity to participate in decision making The opportunity to make real changes in primary health care The object of the Royal College of General Practitioners is "...to encourage, foster and maintain the highest possible standards in general medical practice..." The Royal College of General Practitioners: develops policy and clinical guidelines for general practice provides a support network for GPs works to develop teamwork in primary care maintains quality and standards in medical practice facilitates research publishes on clinical areas, management and policy campaigns to raise the profile of primary care works for the benefit of both doctors and patients Royal College of General Practitioners 14 Prince's Gate, London SW7 1 PU Tel: 020 7581 3232 Fax: 020 7225 3047 Your local Facility is the: RCGP Yorkshire Faculty Academic Unit of Primary Care 20 Hyde Terrace, Leeds, LS2 9LN Tel: 0113 343 4182 Fax: 0113 343 4181 Email: yorkshirercgp.org.uk Website: www.rcgp.org.uk 9 Why do the MRCGP exam? What Have Other People Who Have Taken it Thought? “The impression is of a very honest and fair exam which is genuinely trying to tease the best out of candidates” Phil Hammond, Lecturer and GP in Birmingham Almost everyone thinks they have cancer. This is just one of the strange truths I have uncovered since asking about patient's ‘health beliefs’. No matter what symptom a person presents with, if you asked them something along the lines of “Do you have any particular concerns about what you are experiencing?”, you will receive the sometimes shy sometimes bluff reply “Well, could it be cancer?”. This is when you have the chance to really get stuck into the consultation. I sat the MRCGP exam last summer as part of my registrar year. At the time I decided to sit it, it was just another hurdle, but as the year progressed my approach changed. The work for the exam became part of my day-to-day practice and, for the first time ever, revising for an exam seemed directly relevant to my daily work. The preparation for the four modules of the exam was incorporated into practice in different ways. By ploughing through MCQs I went back to the basic medicine that had become a slightly hazy memory from my time at medical school. I read journals and was up to date with current topics, formed opinions, and was able to discuss them coherently with fellow professionals (which is mostly what the oral exam requires). When reading new papers in journals I finally learned to analyse them in enough to draw my own conclusions, a technique that I had never really mastered in the past (I've always been frightened of statistics!). But more than anything, working for the exam gave me confidence in my general medical knowledge, in managing clinical problems, and in my face-to-face consultations. And that raises the issue of that video. How I sweated and cried over the task - especially when my unfortunate trainer accidentally wiped some of my tapes! Nevertheless, the effort was worth while. Using the framework of the video module's past criteria for my consultations transformed the way I dealt with patients, including discovering “health belief”, which was a novel concept to me after my hospital work. And knowing that the examiners had seen my new consulting style and passed me was a great boost. Did the sitting the MRCGP changed my life? No, but it certainly improved the way I practice. Dominique Thomson, The Practitioner September 2001 volume 245 It was so interesting and rewarding to share the decision-making with my patients, and our relationships seem to blossom. I no longer try to hide from them what I didn't know, or when I wasn't sure, and was surprised and delighted when they seem to respect me for my honesty and appreciate the attempts to include them in managing their own health. More importantly, the process of preparation encourages candidates to develop an educational discipline that should last a lifetime. Doctors who have gained the MRCGP have proven that they are capable of being good GPs - but they have also acquired the educational skills to continue to develop professionally. Patti Gardner, The Practitioner, Sep 2001 vol 245 10 11 Icons Used In this Guide How to prepare How to fail Hot tips Tools that might help you with specific types of questions Test papers for practise 12 13 Do You Want to Pass or Fail? How To Pass ☺ ☺ ☺ ☺ ☺ ☺ ☺ ☺ ☺ ☺ ☺ Get into the MRCGP “mind set” – read the article: “Passing the MRCGP: Preparing Your Mind”, Daryl Goodwin, The Practitioner, Feb 2000, vol 244 p148-151 Get the MRCGP regulations early on and READ them Read the GP press regularly. You will probably need to read the last 6 months of stuff in the BMJ and BJGP. Many questions in the written paper are based on topics covered by the BJGP editorials and this is what you should therefore concentrate on. Don’t forget the GP magazines; they detail news items and hot topics currently in vogue. This can be helpful when question spotting and preparing for the orals. Palmer’s “Notes for the MRCGP” is a great book although out of date in various places. It is particularly good on non-clinical areas. Read the book several times to familiarise yourself with some key concepts and principles. Make sure you are familiar with at least one model of the consultation. Peter Tate’s “The Doctor’s Communication Handbook” is easy to read and pretty concise. Many people like the narrative style of Neighbour’s “The Inner Consultation”. Neighbour provides a simple model of five checkpoints and registrars like this. One of the best books around is “Skills for Communicating with Patients” which is often referred to as the CalgaryCambridge Model developed by authors Silverman, Kurtz and Draper. Okay, so you may feel daunted at the prospect of the 72 microskills listed but remember, as the book emphasises, the Calgary Cambridge model aims to provide you with a toolkit of 72 skills, not all of which will be required in any one consultation. You use which ever you feel are appropriate. They cover all the skills listed in the MRCGP video marking schedule and it is the ONLY book that provides the evidence behind each skill. GET INTO A SMALL GROUP MRCGP STUDY GROUP at least 6 months before the exam, ideally 1 year. Work through some past papers with friends/colleagues Use frameworks and lists to help prepare for the written (MEQ) and oral exam Early on, start to complete the PEP CDs from the RCGP Video one surgery a week, beginning five months before the submission date Look through your consultations with another person Attend a course. Local MRCGP preparatory courses are particularly helpful for acquiring good exam technique (the process) whilst hot topic courses are helpful for knowledge acquisition (the content). How to Fail × × × × × × R Neighbour, “How to Fail the MRCGP”, The Practitioner, May 2002 vol 246 Don't bother reading the exam regulations If the worst comes to the worst, you can always sweet talk the powers that be into agreeing they don't apply to you. Remember the examiners are the enemy They rejoice in your failure. Every question is an ambush, every instruction or piece of advice should be ignored. The college is a club for Smart Alecs If you're a smart Alec, you’ll pass. If you're not, your best bet is to pretend you are. General practice thrives on catchphrases Say “ideas, concerns and expectations”, or “the implications for the doctor, the patient, the practice and society”, or “there are pros and cons” at every opportunity and watch the examiners swoon with delight. Leave your revision until a week before the written is Why let the prospect of doing an exam force you to read, think or talk about your chosen career and moment before you absolutely have to you? On the other hand, you can never go on too many exam preparation courses, the more expensive the better. After all, reading the Kama Sutra is better than any amount of experience. Do not read books The Guardian is a great favourite with the examiners, but do not read anything so pretentious as a medical journal or a book. 14 15 Course Tutors Mandeep Aluwahlia Pete Anderson Kirsty Baldwin James Crick Jude Danby Owen Dempsey Adrian Dunbar FRCGP Nigel Fraser Louise Gazeley Gordon Hayes Tillman Jacobi Jennifer Manuel Neal Maskrey FRCGP Sheena McMain FRCGP Ramesh Mehay Nick Price Gail Nichols GP York Undergraduate tutor - 2nd year medical students from Hull and York Medical School Hospital Practitioner in dermatology. GP York GP trainer Section 12 approved GP SA video assessor registrar educational supervisor Trainer mentor GP (Leeds) Course Organiser (Leeds) GP Trainer Undergraduate tutor GP Scarborough Interest in pre-hospital emergency care and am on the BASICs PHEC course GP (Bradford) GP Trainer (Bradford) Salaried GP Bradford Undergraduate teacher (risk management/communication) Honorary Lecturer (Health Services Research in primary Care) Interests in older people with mental health problems, B12 deficiency RCGP faculty board member My main claim to fame is attending the MRCGP course annually since 1983 - first 2 as a registrar and as a tutor ever since - guess I must enjoy it. I am still - for 5 more weeks a GP but then will have left the practice and be part time associate director and part time GPwSI in musculoskeletal medicine and chronic pain management I belong to the educational boards of various organisations including the British Association of Sport and Exercise Medicine and British Institute of Musculoskeletal Medicine When I am no longer a full timer I hope to devote more time to my triathlon and marathon career. GP Scarborough Interest in cancer services Currently engaged in an Msc in Primary Health Care at Leeds. Committed Christian involved in local Scarborough church Medical officer in Cumbria army cadet force, was in regular army in past. GP GP Scarborough town GP Trainer prospective HYMS training practice DVLA medical examiner GP York Teaches undergraduates GP Leeds interests family planning Chair of Northern Inter branch -family planning group trainer since 1997 Medical director of the national prescribing centre, Liverpool. Previously I have been a GP on the East Coast of Yorkshire, Consultant in Primary Care Development for North Yorkshire HA and Clinical Editor of Clinical Evidence (BMJ Publications). In 1993 I wrote the (first) MRCGP Workbook. GP principal (Leeds) Course Organiser (Leeds VTS) Senior Clinical Teaching Fellow and postgraduate programme manager, academic unit of primary care, university of leeds GP Bradford GP Trainer (Bradford) Course Organiser (Bradford) Currently engaged in a MSc in Medical Education RCGP Faculty Board Member GP (Homeless/Assylum Seekers Bradford) Course Organiser (Bradford) Flexible Career Scheme GP in Selby Senior Teaching Fellow in Primary Care at the University of Leeds Co-ordinator and assessor of the Primary Care component of the 4th year 16 Mark Purvis FRCGP Ella Russell Pam Rawal Mal Smith Chris Varnavides FRCGP Mark Williams FRCGP undergraduate Primary Care, Psychiatry and Public Health course. GP in Wilsden, Bradford. Associate Director Yorkshire Deanery, GP Appraiser. GPwSI in Ophthalmology. Provost Yorkshire Faculty (RCGP) GP Bradford Undergraduate training. Registrar training Clinical supervisor for out of hours training Nurse practioner trainer. OOH sessional doctor. Special interest in diabetes Hoping to become trainer next year. GP (Bradford) GPwSI Gastroenterology and Diabetes Member of the exceptional cases committee (Bradford) Training to become a trainer GP (Bradford) GP Trainer (Bradford) GP Leeds College examiner GP trainer Nurse Practitioner facilitator/trainer university undergraduate tutor clinical assistant in dermatology GP Selby Trainer since 1995 on York VTS Yorkshire Faculty RCGP Board member since around 1996 Special interest in Musculoskeletal and sports medicine. 17 THE MCQ 18 MCQ Questions for this section are derived from accredited and referenced sources, including review articles and original papers in journals readily available to all general practitioners: primarily from Clinical Evidence, British Medical Journal, British Journal of General Practice or Drugs and Therapeutics Bulletin. Some of these questions relate to current best practice. They should be answered in relation to published evidence and not according to an individual’s local arrangements. The MCQ is designed to test your factual knowledge and in particular the application of that knowledge to the management of problems presented by patients. Each question is designed to explore a topic which an ordinary GP or registrar could be expected to have a working knowledge. 19 THE MCQ How to fail the MCQ Only answer the questions you are sure about And that means only the ones that you are a really, really sure about. Otherwise the computer that marks your paper will laugh at you. Don't try too hard to analyse papers Real doctors don't understand statistics. Remember that the experts keep changing their minds This year's knowledge is last year's opinion, and next year's nonsense - so anything goes. Say what you like R Neighbour, “How to Fail the MRCGP”, The Practitioner, May 2002 vol 246 Preparing for the MCQ Practise, practise & practise: read the questions carefully. Look for clues in the wording. Keep checking that you are filling in the lozenges in the right place on the answer sheet. Practise from as many MCQ books as possible, but make sure they cover the new style questions. The phased evaluation program available from the RCGP is valuable. Don't forget there's a lot of up-to-date feedback on the MCQ on the Royal College web site. When practising, identify which areas you are weak on and then read around those subject areas. Quite a lot of questions will be based on recent literature. So get to grips with the evidence for common conditions. The questions for the multiple-choice paper are derived from review articles and journals. These include British Medical Journal Clinical Evidence Drug and Therapeutics Bulletin Current Problems in Pharmacovigilance MeReC Bulletins, Briefings and Extras ADR bulletin CMO update Effective Health Care Bandolier NICE guidelines and NSFs British Journal of General Practice Review journals like The Practitioner Therefore in preparing for this component of the examination you should cast your eye over several of these publications regularly. Read effectively. Remember; concentrate on review articles and the BMJ text clinical evidence. Calculators are not needed in the examination. If you are required to work out anything such as numbers needed to treat, the calculations will be simple. Images such as algorithms, ECG traces and photographs may also be shown. Examiners are always playing around with the format so read the latest RCGP guidance which you will usually find on their web site www.rcgp.org.uk 20 Hot Tips For The MCQ Maintain momentum Read the questions carefully. There is no negative marking of any kind so if in doubt take a guess. If you have to guess try and make an educated guess. You can’t really lose. Remember to pace yourself. It is surprising how many candidates say they ran out of time. Make sure your answer all the questions. Consider attempting the extending matching questions first because they take longer to do. In the eventuality where you might be running out of time, you can quickly go through and tick the true-false type ones. If you are of the type that likes to mark the question paper first, make sure you leave enough time to transfer your answers to the Opscan sheets. Only use the pencil provided for you on the examination day. Know your terms: pathognomic, diagnostic, characteristic and in the vast majority imply a feature that would occur in at least 60% of cases. Implies a feature of such diagnostic significance that its absence would cast doubt on the diagnosis. in the majority implies that a feature occurs in greater than 50% of cases in the minority implies that feature occurs in less than 50% of cases lower chance and in a substantial minority implies that feature may occur in up to 30% of cases has been shown, recognised and reported or referred to evidence that can be found in an authoritative medical text (often true) Questions with “always” or “never” are usually false Please note that none of these terms makes any implication about the frequency with which the feature occurs. These types of questions are becoming less and less frequent in the MRCGP MCQ exam. If a question asks for the single most appropriate answer, you may find that the other options are plausible to. Therefore try to interpret appropriate as being recommended by National accepted guidelines or the British National formulary. 21 Question Spotting Question Spotting (I) Social Security Benefits Child Development Milestones Drugs in Pregnancy The Mental Health Act Notifiable Diseases Diagnostic symptoms of Mental Health conditions like schizophrenia, depression The consultation studies eg Balint, Pendleton, Neighbour etc Question Spotting (II) Don't forget that 15% of the marks are for administration and management. Therefore you should know something about: The business aspects such as fees and accounts Certification, allowances and benefits Effective use of resources, such as investigations and prescribing Information technology Legal aspects such as health and safety regulations, and employment issues Professional regulations such as clinical corporate governance, risk management and patient safety Regulatory framework within the NHS Why not spend some time with your practice manager going through some of these areas? I’m sure they’ll be delighted you asked. Question Spotting (III) There are even more marks (20%) on research, epidemiology and statistics. Therefore familiarise yourself with: The principles of audit and it is application to demonstrate the ability of assessing the quality of patient care The application of critical appraisal skills The terms used in both statistics and evidence based medicine as described in the appendices of the journal clinical evidence, BMJ publication. You can also access this online www.clinicalevidence.org.uk Get to grips with statistics; get used to data presented in tables (you can get MCQs asking you to work out NNT etc): Working out true/false positive/negative rates Working out positive/negative predictive values Numbers Needed to Treat (NNT) They are easy marks to get but only if you know how to do the sums. This is Important: The MCQ paper is made up of questions relevant areas: Medicine Administration and management Research, epidemiology and statistics to general practice from the following key 65% 15% 20% 35% So, if you only ever concentrated on the clinical arena, the most you could score is 65% (that’s if you’re brilliant). But the overall pass mark is usually around 70% or so. However, if you were fairly clued up on admin stuff, research, evidence and statistics but average on the clinical areas, that means you could score (10+15+50 =)75% quite comfortably. In addition, you would get some of the remaining 25% by guessing. The clinical domain is limitless but admin, research and statistics is more confined. In preparation for the MCQ, make effective use of time and make sure you concentrate on these areas too. 22 Format Don't forget to look up the format in the current examination by referring to the examination regulations. These are also available for viewing online at www.rcgp.org.uk Extending Matching Questions (EMQ) in which a scenario has to be matched to an answer from a list of options. You may feel that there are several possible answers but you must choose only the most likely from the option list. Single Best Answer (SBA) questions in which a statement or stem is followed by a variable number of items, only one of which is correct. Multiple Best Answer (MBA) questions in which a statement is followed by a variable number of items, a specified number of which are correct. For example: A 65-year-old male smoker presents with blah blah blah. Chest examination reveals blah blah blah. Identify the three most appropriate therapeutic interventions to be considered following the British Thoracic Society COPD guidelines from the list below. (Get the idea?). Summary Completion Questions (SCQ) which test your critical reading ability from a summary of a paper presented in the question paper. For example : For each of the numbered gaps in the critique, choose one word from the following list which best completes the sense, and mark the corresponding lozenge on your answer sheet. Although the authors attempted to carefully match the subjects in each group for clinic (30)____________ , this was neither a (31) a _____________ nor a (32) ____________ study. WORDS TO CHOOSE FROM : association, bias, blinded, cohort, etc etc Standard Multiple True False (MTF) questions which comprise a statement followed by a variable number of items, any or all or none of which may be correct. For example: The signs and symptoms of Parkinsonism: (a) Characteristically remain unilateral for years; (b) Are a recognised side-effect of amitriptyline therapy, (c) Are a recognised sequel to encephalitis etc etc Pictorial data such as charts and photographs may be included in the questions. The number of items in each format is variable. Over recent sessions of the exam we’ve been increasing the number of images used in the test and are in the process of building up a bank including a variety of digital images including: rashes, ENT problems, ECGs, and retinal photographs. These questions, especially the ECGs, are invariably answered well by the majority of candidates. WHY THE CHANGE FROM TRADITIONAL MULTIPLE CHOICE TRUE/FALSE QUESTIONS? In common with many postgraduate medical examinations the MRCGP has stopped using the traditional multiple true false (MTF) questions and moved to newer formats, mainly extended matching questions (EMQ) and single best answer (SBA) questions sometimes referred to as ‘best of five’. These newer type of questions are believed to be more reliable and valid and have the added benefit of testing the application of knowledge as opposed to merely recalling facts. Examinations such as the MRCS, MRCP, MRCPsych and PLAB Part 1 tests are using the EMQ formats, and there are similar trends both internationally and in undergraduate examinations. Some candidates have expressed concern regarding the time pressure, which relate either to the number of questions in the test and/or the lack of time to complete the test. The issue of 'speededness' is something the RCGP continually monitoring. Get a Sample paper. The RCGP is aware of the short supply of up-to-date sample material available to candidates but a number of questions have a short shelf life, are difficult to write or need to be re-used to facilitate ‘linear test equating’, and so they are not in a position to release the whole bank at present. However, the RCGP have constructed a composite sample paper illustrating all of the new question formats, which is now available from the College SALES (Not EXAM) department. Their intention is to update this, approximately every two years. In addition, there should be some sample material on their website. 23 FILLING IN THE BLANKS MADE SIMPLE These questions usually present a research paper followed by a critical appraisal with missing words or phrases. Useful terms that may help you in these sorts of questions include: Aug 2005 - Filling in the blanks questions have now gone; the College doesn't include them any more but they serve as useful revision. Descriptive Words Methods - Sample Size - Inclusion/Exclusion criteria = Selection criteria = case definition - Outcome Measure Results - Response Rate Drop Out Rate Sensitivity/Specificity Positive Predictive Value/Negative Predictive Value Interpretation - Exposure - Over diagnosis/ Under diagnosis - Confounding Variables - Recall Bias - Observer bias/error - Subject error/bias - Technical bias/error - Contamination - Consistency - Power of the Study - Secular Trends (ie changes with time) - Verification - Applicability - Conflicts of Interest - Ethics - References Types of Study - Randomised Observational Retrospective/Prospective Case Control (retrospective) Cohort (prospective) Cross Sectional Study (descriptive) = Prevalence Study Randomised Control Trial Meta-analysis BECOME FAMILIAR WITH THESE WORDS. READ THEM OUT LOUD TO YOURSELF SEVERAL TIMES AND KNOW WHAT EACH MEANS. 24 MCQ PRACTICE (answers at the end) EXTENDED MATCHING QUESTIONS: A. Theme: Management of Symptoms in Advanced Cancer Options A. B. C. D. E. F. G H I. Bisacodyl suppositories "Brompton" cocktail Co-dydramol Co-proxamol Diamorphine elixir Diamorphine injection Diamorphine via a syringe driver Diazepam Dihydrocodeine J. K. L. M. N. 0. P. Q. Lactulose Metoclopramide Paracetamol Pethidine injection Pethidine tablets Prednisolone Slow release morphine Naproxen For each of the cases below select the one option from the list above which you consider the most appropriate. Each option may be used once, more than once, or not at all. 1. A 50 year old man with carcinoma of the pancreas who has severe abdominal pain and is constantly vomiting. He was previously pain controlled on MST. He is within one week of dying. 2 . A 65 year old man who has advanced carcinoma of the oesophagus. He has chest pain and great difficulty swallowing solids. He is drinking well. His previous analgesia was coproxamol which is now no longer relieving the pain. 3 . A 50 year old female patient with advanced carcinoma of the breast is well pain controlled with dihydrocodeine. She presents acutely with severe colicky abdominal pain. She is not vomiting, is passing urine normally and has not had a bowel action for 4 days. 4 . A 90 year old man with carcinoma of the prostate presents with pain in the rectum. He has not been taking any analgesia and has not needed any until the present consultation. He is eating well, sleeping well, and is not constipated. 5 . A 55 year old female patient with advanced ovarian carcinoma is well pain controll ed with slow release morphine on a twice daily basis. She is nauseated and does not want to continue with her pain killers. She takes lactulose and her bowels are working normally. 6 . A 23 year old man with advanced lymphoma is well pain controlled on a regime of MST, metoclopramide and lactulose. He is developing bone pain which is stopping him from sleeping at night and making it uncomfortable to lie down in the day. 25 B. THEME: Weight Loss A. B. C. D. E. F. G. H. Achalasia Addison's disease AIDS Anorexia nervosa Anxiety Carcinomatosis Cardiac failure Depression I. J. K. L. M. N. O. P. Diabetes Mellitus Malnutrition ME Myxoederna Oesophageal cancer Thyrotoxicosis Threadworms Tuberculosis Options For each of the cases described below select the most probable diagnosis. Each option can be used once, more than once or not at all. 1. A 25 year old male who has been steadily losing weight over the last 6 months, but has been too "frightened" to seek medical advice. On examination he is emacia ted, is dyspnoeic, has enlarged lymph glands and has odd looking purple papules on his skin. 2 . A 65 year old female patient who has recently reluctantly retired as a nursing sister. She has rapidly lost two stone in weight since her retirement. She is eating normally and does not feel ill but has slight diarrhoea. On examination she shows signs of weight loss and muscle wasting. She also has atrial fibrillation. 3. A 70 year old man who has some difficulty swallowing solids but not fluids. He has lost one stone in weight and he has a feeling of saliva filling the mouth after meals. He has been feeling unwell for about one month. 4. The 70 year old mother of a colleague registers with you. She has recently moved to this country from India. She has a cough and has lost weight. On direct questioning she admits that she sweats at night despite finding the climate cold. 5 . An obese 50 year old lorry driver presents with an itchy bottom. He tells you that he has been on a diet and has lost one stone in weight over the last six months. He does not drink alcohol but does drink a lot of sweet drinks and even wakes at night to have a glass of lemonade. 6. A 15 year old girl presents with secondary amenorrhea for 12 months. She says she is very fit and runs in the school team. She has a slow pulse, she is emaciated, has facial hair and lack of breast development. 26 C. The literature of General Practice includes the following books and papers: A B C D E F G H I J K L M N The exceptional potential in each primary care consultation, by Stott & Davis The Doctor, his Patient and the Illness, by Michael Balint The Doctor-Patient Relationship, by Freeling & Harris The Consultation: An Approach to Learning and Teaching, by Pendleton, Schofield, Tate & Havelock On Learning from the Patient, by Patrick Casement The Symptom Iceberg, by D R Hannay The Inner Consultation, by Roger Neighbour The Exceptional Potential of the Consultation Revisited, by J F Middleton The Future General Practitioner, by a working party of the RCGP Games People Play, by Eric Berne Doctors Talking to Patients, by Byrne & Long Six Minutes for the Patient, by Balint & Norell Culture, Health & Illness, by Cecil Helman The Ailment, by T F Main Match each of the following descriptions to the appropriate title listed, by writing one identifying letter in the space provided. (N.B. Each title may appear once, more than once, or not at all.) 1. Identifies six questions patients ask themselves when faced by an episode of ill health 2. Is based on the analysis of audio-taped consultations 3. Distinguishes between 'curtain raisers' and 'gambits' 4. Describes the 'collusion of anonymity' 5. Describes human behaviour in terms of Parent, Adult and Child 6. Discusses features of 12 patients who proved very difficult to manage in a hospital setting 7. Stresses the importance of identifying patients' ideas, concerns and expectations 8. Suggests encouraging 'appropriate help-seeking behaviour' 9. Describes 'the flash' 10. Discusses the doctor's 'apostolic function' 27 D. Theme: CHEST PAIN Options A. angina pectoris B. aortic stenosis C. compression fracture spine D. dissecting aneurysm E. herpes zoster F. hyperventilation G. oesophageal spasm H. mitral stenosis I. musculoskeletal pain J. myocardial infarction K. pericarditis L. pneumonia M. pneumothorax N. pulmonary embolism Instructions: for each patient below select the most likely diagnosis. Each option may be used, once, more than once or not at all. Items: 1) A 55 year-old businessman who ruptured his right Achilles tendon one month previously and has his leg in a plaster of Paris cylinder. He complains of progressive shortness of breath and chest pain worse on taking a deep breath. 2) A 20 year-old shop assistant who complains that she cannot get her breath, that her chest feels tight and her fingers are numb. The peak flow is normal and her chest is clear. You know that she's breathing rapidly. 3) A78-year-old man who, following a head cold, became short of breath and developed a cough productive of yellow sputum. He is pyrexia and you note areas of diminished breath sounds with fine crepitations at the right base 4) A 55 the old man presents with sudden onset of crushing central chest pain out at 4am. He is vomiting and sweating, very frightened and his blood pressure is 100/55. 5) An 80-year-old woman lives in sheltered accommodation. She has had falls with loss of consciousness from which he makes a quick recovery. She admits to chest pain on exertion and of feeling giddy. She has a basal systolic murmur radiating to the neck. 6) A19 year-old student has sudden onset of severe pain in the left side of his chest. He is very short of breath and is slightly cyanosed. His left lung is resonant with absent breath sounds. 28 E. Health Promotion in General Practice for Patients at High Cardiovascular Risk. Aug 2005 - Filling in the blanks questions have now gone; the College doesn't include them any more but they serve as useful revision. First read the methods section of the paper: Patients and Methods Patients were identified from 18 group general practices in the greater Belfast area. General practitioners were asked to identify patients aged under 75 years who had had angina for at least six months and did not have any other severe illness. Angina was defined as recurrent, transient and reproducible discomfort in the chest, arms, jaw or shoulders, discomfort being reproduced by physical exertion or emotional excitement and relieved by rest or drugs. We sent letters to 1431 patients asking for their consent to be interviewed by a research worker interested in angina. The initial appointment took place in the patients local health centre or surgery or in their own home. Trained health visitors asked questions about the effect of angina on everyday activities, the frequency of attacks of angina, drugs taken, smoking, exercise, and diet. They also administered a questionnaire to determine intake of various foods based on that used in a Department of Health and Social Services survey in Northern Ireland. Exercise levels were rated as the number of episodes each week of physical activity sustained for at least 20 minutes. Patient’s height (Microtois tape, Rayen equipment, Dunnow), weight (Seca scales, Seca, Birmingham), blood pressure (random zero sphygmomanometer, Hawksley and Son, Lancing) and breath carbon monoxide concentration (Smokerlyzer, Bedfont Technical Instruments, Sittingbourne) were measured. An electrocardiogram was recorded and a sample blood taken for measurement of serum cholesterol and thiocyanate concentration and a urine sample for cotinine assay. Each subject was then randomly allocated to one of two groups. The health visitor opened an opaque, sealed, and numbered envelope containing the allocation, which had been generated by a computer program using random permuted blocks. For the control group the interview ended at this point. Patients in the intervention group were given practical relevant advice regarding cardiovascular risk factors. They were reviewed at four monthly intervals and given appropriate health education. After two years, both groups were reviewed by a research worker who had not previously been involved with the subjects. Now consider the following critique of the paper, from which some words or phrases have been removed. Please insert what you think will most appropriately fill the gaps in the corresponding spaces in the answer sheet. You may mark this sheet as a preliminary but you must make sure that you transfer your answers to the answer sheet. This is a study of _____(a)_____ prevention of ischaemic heart disease in general practice. The setting is Belfast: Northern Ireland has a particularly high prevalence of ischaemic heart disease making it a convenient setting for the study. The design is a(n) _____(b)_____ of _____(c)_____ provided by health visitors every four months over a period of 2 years. The _____(d)_____ measurement is not spelt out in this extract, but one may assume that it is based on a repeat of the interview administered at the initial encounter asking about the effect of angina on everyday life and the frequency of angina attacks. The text does not describe how the practices were selected. Recruiting from practices in more affluent areas may mean the patients in the study are at a lower baseline risk of ischaemic heart disease. This would in turn tend to _____(e)_____ the effectiveness of the _____(f)_____. Substantial numbers of patients were recruited, 29 although the text does not show a _____(g)_____ calculation to estimate how many would be required in each arm of the trial to be _____(h)_____. _____(i)_____ criteria are well described and seem consistent with a clinical diagnosis of angina. No more objective test for angina such as _____(j)_____ has been completed. While the omission makes it easier for general practitioners to apply the results of the study, it also means there is no check on the _____(k)_____ of the general practitioners’ application of the study protocol. It would help to know the _____(l)_____ by each general practitioner. This will not affect the result of the study itself, provided the randomisation is well conducted, but it may affect _____(m)_____. It is intrinsic to the design of this study that it could not be _____(n)_____. The importance of having an assessor not previously involved with the trial is that it reduces _____(o)_____. However, knowing to which group they had been assigned allowed the possibility of _____(p)_____ to influence the results on items such as diet and the amount of exercise taken. ANSWERS: (a) (i) (b) (j) (c) (j) (d) (k) (e) (l) (f) (m) (g) (n) (o) (h) (p) 30 F. Establishing a minor illness nurse in a busy general practice. Aug 2005 - Filling in the blanks questions have now gone; the College doesn't include them any more but they serve as useful revision. First read the methods section of the paper: Methods The practice is a first wave fundholding practice in an urban-suburban area. It has been a training practice since 1965 and takes medical students for clinical attachments. The social class of patients is similar to that in the whole of England and Wales. There are almost 15 000 patients served by six whole time equivalent general practitioners, three practice nurses, and managerial, records, and administrative staff. Community, psychiatric, and psychogeriatric nurses, a health visitor, a midwife, a dietician, two counsellors, a physiotherapist, and an osteopath are also attached to the practice. The nurse concerned (MLD) is a registered nurse and state certified midwife. She has worked as a midwife in hospital and in the community for 15 years and is accustomed to working independently. She also has the customary life experience from bringing up two children. She had worked in the practice for two years before being trained in diagnosing and treating minor illness. She was trained by sitting in surgeries with the duty doctor in the practice for three half days a week over about a year. She learnt the techniques that are used in brief consultations about acute minor illness and was given experience in using a tongue depressor, torch, auroscope and stethoscope. After the training year she began her own consultations, working for two hours each afternoon. Her speed gradually increased up to 10 minute appointments. The receptionists were taught to offer a consultation with the nurse practitioner to patients requesting an urgent same day appointment. Patients were told that if either they or the nurse was unhappy with the diagnosis or treatment after the consultation, the duty doctor would be consulted. If patients demurred in any way they were given an appointment with a doctor. When prescriptions were required they were signed by doctors without the patient being seen by them The nurse provided a one line summary of symptoms and signs and a diagnosis on the back of the prescription, which she wrote out. All patients were advised about the development of symptoms that would make further consultation advisable. Those with non-minor illness – for example, family planning or gynaecological problems – had their immediate problem attended to and were advised to attend appropriate clinic sessions. The nurse did not ask patients to come back and see her. When she felt that follow up was necessary she asked patients to see their own doctor. If samples were taken for tests she advised patients to telephone her for the results. These telephone consultations were not included in the total. Now consider the following critique of the paper, from which some words or phrases have been removed. Please insert what you think will most appropriately fill the gaps in the corresponding spaces in the answer sheet. You may mark this sheet as a preliminary but you must make sure that you transfer your answers to the answer sheet. This is a(n) _____(a)_____ study describing the process of introducing a nurse practitioner. It is trying to examine an area that is both topical and therefore of considerable interest. Introducing a nurse practitioner ought to take work away from the doctors. However, this must be set against the known tendency for some workload to be driven by _____(b)_____. It is a study from _____(c)_____ and this can pose problems of _____(d)_____. In this case a(n) _____(e)_____ list size is likely to mean _____(f)_____ demand for a nurse practitioner. 31 The title includes the term ‘a minor illness nurse’, and the text describes her being trained in diagnosis and treatment of minor illness. However, the training is not defined. To test the paper’s _____(g)_____ the readers need to know how it was defined by the partners of the practice, either explicitly or implicitly. It is also well known that individual general practitioners vary considerably in the extent to which they identify _____(h)_____ in the presentation or symptoms of minor illness and this too would affect the training received. The reader needs to know more about patients treated; this would have been helped by including _____(i)_____ in the study protocol. However, this would also have made the study more complicated with implications of involving a receptionist or researcher, raising the ethical problems of _____(j)_____. For the study patients were offered a consultation with the nurse if they asked for an urgent same day appointment. Equating these two poses many problems. Variable which might affect the numbers or the nature of problems seen by the nurse practitioner included _____(k)_____ or _____(l)_____. In assessing the effect of the nurse practitioner the design could have been improved by including some patients to act as _____(m)_____. This would be best done by _____(n)_____ those requesting an urgent appointment to nurse or doctor. Measuring the _____(o)_____ of this initiative is difficult because of the absence of any _____(p)_____ for the diagnosis and management of patients with minor illness. Information routinely available from medical records that might help in assessing outcomes might include _____(q)_____ or _____(r)_____. With additional resources, the patients included in the study could be asked to fill in satisfaction questionnaires evaluating such areas as _____(s)_____ or _____(t)_____. Answers A G M S B H N T C I O D J P E K Q F L R 32 G. SINGLE BEST ANSWER In vesicoureteric reflux in childhood it is recognised that: a) the majority of children with a urinary infection have reflux as the underlying cause b) antibiotic prophylaxis can safely be discontinued at the age of three years c) a single documented urinary tract infection in a girl aged five does not merit further investigation d) a normal urinary tract ultrasound examination will satisfactorily exclude all grades of reflux e) the risk of renal scarring is greatest in infancy H. MULTIPLE BEST ANSWER Vaginal candidosis. Which three answers are true? Give three answers. a) treating the male partners of women with recurrent infection reduces the rate of recurrence among infected women b) rates of cure of candidal infection during pregnancy are significantly lower than in the none pregnant state c) vaginal discharge is absent in a significant number of women with candidosis d) treatment with oral preparations has been shown to be more effective than topical therapy e) oral itraconazole is safe in the third trimester of pregnancy f) long-term oral nystatin does not affect the relapse rate in women with recurrent thrush 33 34 PRACTICE MCQ - ANSWERS A - Management of Symptoms in Advanced Cancer 1. G 2. G 3. A 4. L 5. K 6. Q B - Weight Loss 1. 2. 3. 4. 5. 6. C N M P I D C. The literature of General Practice includes the following books and papers: M K G B J E D A L B D. CHEST PAIN Answers 1) 2) 3) 4) 5) 6) N F L J B M E. Health Promotion in General Practice for Patients at High Cardiovascular Risk. Model Answers (a) (b) (c) (d) (e) (f) (g) (h) (i) (j) (k) (l) (m) (n) (o) (p) secondary prospective study health education outcome reduce intervention sample size statistically significant Inclusion/Selection stress testing validity/reliability breakdown of outcome applicability double blinded observer bias expectation bias 35 F. Establishing a minor illness nurse in a busy general practice. Model Answer A. B. C. D. E. F. G. H. I. J. K. L. M. N. O. P. Q. R. S. T. descriptive service availability one practice applicability large higher validity markers/hidden agenda’s/red flags inclusion criteria confidentiality time of month, time of day, availability time of month, time of day, availability controls randomly allocating outcome objective measure/test/endpoints re-attendance/prescribing re-attendance/prescribing availability of appointments/quality of advice given availability of appointments/quality of advice given These types of ‘fill in the blanks’ questions are often very difficult. The possibility of more than one alternative makes the marking of such responses difficult. As a result, in the actual exam, you may be provided with a list of terms from which you will need to select the best response G. SINGLE BEST ANSWER Vesicoureteric reflux answer 5 H. MULTIPLE BEST ANSWERS Vaginal Candidosis ANSWER : 2,3 and 6 are true; the remaining are false 36 Modified Essay Questions (MEQs) 37 MEQs MEQs aim to do two things: a) in terms of doctor-patient relationship, MEQs test your 1. understanding of the influences that cause patients to consult the Dr 2. ability to recognise the variety of possible responses from the Dr b) in terms of the practice, the NHS and decision making process, MEQs test your 1. ability to recognise problems in the partnership and PHCT 2. appropriate use of NHS resources 3. awareness of legal and ethical dilemmas 38 MODIFIED ESSAY QUESTIONS (MEQs) What are MEQs all about then? The following two scenarios may help to illustrate this: “A difficult consultation involving conflict over a patient's "unreasonable" demand for prescribed drugs or specialist referral may involve feelings of anger, frustration and tiredness on the part of the doctor. He or she is trying to juggle patient satisfaction against clinical (does the patient need the treatment?), ethical (what if I give it anyway to please the patient in the short term and take the pressure off my already late surgery?), financial (would a cheaper treatment be as effective?) and time constraints (of course I could explain the pros and cons fully and clearly and persuade the patient to the medically sound point of view, but not in 7.5 or 10 minutes). A consultation with a diabetic patient not previously known to the practice would involve not only eliciting the patient's beliefs and concerns and dealing with their clinical problems, but recognition of other non-clinical "constructs": Have they adequate sharps disposal facilities? Have they informed the DVLA and their insurance company of the diagnosis? Are they aware of support available from Diabetes UK? Do they have adequate colour vision to read blood glucose testing strips accurately?” (taken from “The MRCGP Examination”, RCGP publication) How to fail the Written Paper × × × × × × × The printed question is never the real question “Site the evidence on the issue of X means: tell us what your Uncle Bill's mother swears sorted her out when she thought she had X. Either that, or cite the evidence on the issue of Y. Every word in the question teams with hidden meaning Underline what you think are important words before starting your answer. For example, if the question is “what issues does this raise?”, underline the word ‘does’ (or ‘this’, or ‘what’) three times and write down what ever thought processes this stimulates Practice terrible handwriting The examiners, being practising GPs, can read illegible writing and know what you mean even if you don't say it. Write beautiful prose Full marks will be awarded for answers beginning: “in the garden of human experience which is general practice, problems are to the doctor what manure is to the roses of disease….” GP should never risk taking any unsupported decisions No problem is unworthy of involving the health visitor, discussing with other members of the primary health care team, or seeking the advice of your defence organisation Critical reading doesn't really matter No one really expects GPs to read anything published in a grown up scientific journal. Facts are for nerds and research is for anoraks. Don't worry about anything but medicine Examiners, being ordinary working doctors, don't give a fig about finance, business, Ethics, sociology or politics. R Neighbour, “How to Fail the MRCGP”, The Practitioner, May 2002 vol 246 39 Preparing for the Written Paper Preparatory reading should be broadly based on reputable mainstream journals and books of relevance to general practice (BMJ, esp the editorials and the GP section; BJGP) guidelines of national status (NICE; CMO reports; DTB; Bandolier; MeReC) RCGP Occasional Papers systematic reviews and meta-analyses relevant to general practice the national press, as it reflects medicine in society and one or two GP magazines (Doctor, Pulse – these often do a ‘round up’ of important articles and their strength and weaknesses but also have articles on tips for the MRCGP exam (don’t assume accuracy though). This should give grounding in new developments and emerging knowledge. However, many studies which still influence general practice today were performed several years ago and they should not be neglected on that account. In order to best achieve the broad reading base required you are advised to study common clinical problems and general practice themes and familiarise yourself with the literature relating to these rather than reading recent consecutive back issues of journals. An effective method is to reflect on your clinical experience and then read about it and then to discuss with peers the challenges encountered. If you take this approach throughout your period of vocational training then most subjects likely to be asked will have been encountered and covered. Often, the paper looks like it requires you to have read loads and loads of journals and acquired a vast amount of knowledge; the truth is, it doesn’t. Only 2-4 of the twelve questions usually ask DIRECTLY for evidence based medical knowledge. So don’t be put off by trying to learn tonnes and tonnes of evidence. It is likely you probably know most of it anyway but you just don’t know the papers. How many of you prescribe aspirin post MI? (most of you I hope) Why? (because you know it reduces mortality). And what’s the evidence? (“Aspirin reduces mortality” is the evidence and is adequate. A better answer would quote the ISIS2 study). Don’t forget to look at the RCGP web site which furnishes you with examiner’s detailed comments on past questions. Reading these will tell you what kind of answer they are looking for, where candidates did well and where they could have done better. Practice MEQ papers in your MRCGP study group under mock exam conditions. Compare your answers with each other and then against the examiner’s comments. Try and focus on what you could have done better. If you prefer a problem orientated approach then you might wish to maintaining a log diary of your patients and cross-referencing the issues elicited with the relevant reading. One of the big advantages of this method is that it ensures you cover common problems in general practice and the evidence around those areas which is what the MRCGP exam aims to explore. Consider keeping a card index of topics with each card detailing the evidence and around that topic. Work collaboratively. Because there is so much evidence out there, it is difficult for one individual person to research and summarise everything for every single hot topic. A more effective way of doing this is to formulate a hot topic list. Every week each member from your MRCGP Study Group should take a hot topic to research and summarise the current thinking and references. They should try and do this on no more than two sides of A4. Ask them to photocopy this according to how many members are in your group. The following week, each member should be allowed 15 minutes to present their hot topic and dish out their handouts. This then carries on the following week until the hot topic list is exhausted. To create the list in the first place, hold an initial brainstorming session with your group. 40 Hot Tips for the Written Paper You might want to quickly read through all the questions first to allow your subconscious to work on the others whilst you tackle the one at hand. Read each question carefully word by word. Consider underlining important words to help you focus on the question and answer what they are asking. Answers should be in the form of constructs (or themes) with HEADINGS. Each construct should be expanded further (i.e. meat on the bone!) Think laterally not literally - broad but structured. Don’t forget to think of the patient in the context of their family & culture. Don’t forget about finance, business, ethics, sociology and politics. It’s not all about clinical medicine! You should answer each question fully, even if this involves repetition of part of an earlier answer. Constructs may be repeated for different questions. Each MEQ question is independent of all others and each will be marked by different examiners. You should answer all the questions and NOT just spend time on the ones you are comfortable with. With a bit of thought, the first few marks of every question are not that difficult to achieve. Write legibly and avoid abbreviations. The question booklet is split up and each sheet is sent to a different examiner. You should therefore not continue the answer to one question on a sheet designed for a different question. You need to be able to structure you answer. This not only makes it easier to mark but also helps you to organize your thoughts and even come up with issues/dilemmas one might not have come up with if a brainstorming approach was used alone. So: If a question has clinical dimensions: think how you would manage it in your surgery If a question has a consultation process dimension: detail your thought processes during the consultation If a question relates to a primary care problem, remember the problem affects not only the patient but the doctor, the family, other health care staff and society And remember, factors affecting a patient’s health can by physical, psychological, social and cultural. Try and use buzzwords (detailed below); these catch the examiner’s eye and will almost always score a point. Quoting the Evidence: You should not assume that only those questions which deal overtly with general practice literature should be approached in this way; it may be just as pertinent to cite evidence in a question on clinical management or dilemmas within the primary care team. When referring to the evidence base, you should convince the examiner of your familiarity with that source. This can be often be more effectively achieved by a short summary of the important features of a trial and its results rather than by a bibliographical citation. Indeed, precise citations are not required, and a mere list of references is unlikely to demonstrate that you have absorbed the messages from those sources. People working in an MRCGP study group often do better than those who decide to prepare alone. Study groups enhance the cross fertilisation of a variety of ideas and thinking from a variety of people which in turn will encourage you to think even more laterally Reference book: Modified Essay Questions for the MRCGP Examination by TS Murray. Good questions, crap answers though (but your study group will make up for this). In Summary: Answers should be legible and concise. You may use short note format, and abbreviations which are in common use in medical English. You should: - read each question carefully, and answer it as asked; - think in a wide-ranging way but realistically about how a competent and sensitive general practitioner would deal with each scenario; - avoid jargon, cliché and over-generalisation; - include illustrative details, explanations and relevant examples. Where appropriate, you should justify your answer by making reference to the evidence base. 41 Specific questions and what they mean Issues – A question that asks for issues to be considered is an invitation to think broadly. Using a single model to structure the answer, for example an ethical framework, candidates risk overlooking important elements in the question. Unfamiliar scenario - some questions may pose an unfamiliar scenario, for example: Rosy Barrett asks you to arrange paternity testing of her nine month old baby. What issues does this raise? Questions like these examine the ability of the candidates to deal with an unfamiliar, complex situation. As general practitioners we can often find ourselves in unfamiliar situations, which have we have to manage. Often these situations have an ethical component with many implications. Questions like these often present practical challenges as well as intellectual ones. Phrases - when responding to questions which detail a specific phrase, be sure to identify the meaning of that phrase clearly in your mind first. For example: “How might changes currently occurring in general practice affect continuity of care?” In this example it is important that the candidate understands the term “continuity of care”. If you don't identify the meaning of the phrase clearly this will make it difficult for you to indicate how the changes impacted on patient care and the work of professionals involved in care. Answer Construction Lecture note format Principle of constructs (= themes) Introduction to triads and model mnemonics – how to use them, use not compulsory. Universal framework. Beware, using a single model to structure the answer risks overlooking other important elements in the question Linking in the evidence: author’s name not really that important, how to put down the evidence (not just a regurgitation of facts; some critical analysis required Common MEQ Scenarios Clinical diagnosis and management. This includes : information gathering hypothesis formation preparation of management plans and anticipation of possible future problems Psychological and social problems affecting individual and families. Hidden Agendas. Caritas (caring, empathy) The consultation process. Health Beliefs. Recognition of Dr's own feelings, motivation (self-awareness) Preventative medicine including protocol development and assessment A difficult consultation scenario or difficult patients: For example, the somatising patient, the conflict situation or a breach of confidentiality. How would you respond? The problems may be Ethical Psychosocial Medico-legal and or Clinical Relationship with colleagues and others - an awkward request from one of your partners or practice staff for example. How would you respond? Practice organisation including PHCT Appreciation of ethical and medico-legal problems Cost Effectiveness 42 MEQs – Made Simple! Think as laterally as possible The Universal Framework The ‘Universal’ Framework can be applied to most MEQ questions that ask about issues or implications. Use it as a skeleton for building up your answer; not all points will be relevant to every question. Make sure you add enough ‘meat’ on to the bone (i.e. hang things off the skeleton) Build Rapport(& caritas ie caring/empathy) Empathy& Listening Approach Patient Issues Further Hx, Ex & Ix Relative Issues Doctor Issues Practice Issues & Dynamics Family Dynamics Social Issues Work Issues Ethical Issues & Patient Autonomy Medico-Legal Aspects Management Options & Care in the Community Health Education/Promotion Other PHCT Members (getting them involved) Follow up - Quote for all questions Notes: In the frequent attender - don’t forget: ‘Ownership of the problem’ In the case of children, don’t forget : Advice from HV, school etc, parent using the child as a ‘ticket’ to presentation Types of Question the ‘Universal’ Framework can be applied to: ‘What issues does this raise?’ ‘How would you proceed?’ ‘How would you approach the consultation’ 43 Buzz Words and Triads Buzz Words Examiners get all excited when they see the following words. appropriate to the question. Include them if Patient: Autonomy, Involvement, Ventilation of feelings, Guilt/Blame, Life Events, Compliance, Somatic Fixation, Self-help Groups Dr: Eliciting, Facilitating, Empathising, Counselling, Open/Closed Questions, Reflective Questioning, Authoritarian, Rejecting Dr-Pt Relationship: Dependence, Control, Manipulation, Collusion, Transference, Counter-transference, “Heart Sink” Triads Triads are useful aide memoirs; they can help you think more laterally. For example, when discussing management, think in terms of immediate, short term and long term. Get the idea? Physical History Immediate Patient Culture Doctor Ideas Options Knowledge Psychological Examination Short term Family Status Partners Concerns Implications Skills Social Investigations Long term Community Image PHCT Expectations (ICE) Choice Attitudes 44 Mental Grids/Check Lists/Constructs The following mental grids are other frameworks which you can use to build up an answer and hang things off when asked about specific situations. As with the universal framework, make sure you add enough meat on to the bone! All examiners are familiar with these and they don’t like them being transcribed word for word. In the actual exam alter the wording to make it more personal and make sure you use them in the context of the scenario. The following lists are not exhaustive. Play about with them. You may want to improve on some or you may want to formulate completely new ones of your own . CONSTRUCTS ABOUT THE CONSULTATION Why do Patients Consult? Example Question: Mr Brown comes to see you for the eighth time in a two month period with headaches. Why might this be? PHYSICAL underlying disease PSYCHOLOGICAL SOCIAL/ Financial Reasons Poverty MEDIA brain cancer - Genuine physical symptoms as a result of - Depression, Anxiety etc - Dysfunctional family dynamics, Work Problems, - Scare on the TV or press eg mobile phones and Managing a Consultation Example Question: Mrs. Trulove, a 26 y old nurse comes to see you regarding troublesome eczema of her hands. How would you handle this consultation? Method 1 EXPLORE EXPLAIN CONSIDER ADVISE CONSIDER INVOLVE Method 2 History Examination Investigations Diagnosis Education Explanation Prevention Treatment Referral Follow Up patients knowledge, Ideas, Concerns & Expectations (ICE) their symptoms & signs treatment options patient on options patient preference patient in management plan THE 10 POINT MANAGEMENT PLAN 45 Management Options Example Question: Mr. Simon comes to see you regarding back pain. What are the options available to you? Method 1 R Reassure A Advise/Educate (leaflets, books, videos) P Prescribe/Carry out a procedure R Refer ? To whom I Investigate O Observe & FU & Opportunistic Health Promotion Method 2 Mx of Presenting Problem Mx of Continuing Problems Modification of Help Seeking Behaviour Opportunistic Health Promotion Mnemonic : RAP RIO The Full Potential of Consultations REFERRAL OPTIONS Example Question: Who else would you involve in further management? Method 1 Within the PHCT practice nurse, district nurse, HV, midwife, CPN, practice manager (e.g. for complaints) Social Services social worker, home care, meals (on wheels/frozen delivery), day centre, sheltered housing, residential care Voluntary Sector carer support groups, Citizens Advice Bureau, CRUSE (bereavement, support) etc Hospital Consultant, Direct Access Services (endoscopies, physiotherapy etc) Method 2 Patient Dr Practice PHCT Hospital Family & Carers Social Services Persons/Institutions Involved WHEN TALKING ABOUT PREVENTION THE FOLLOWING TWO THINGS SHOULD BE MENTIONED Health Education Preventative Medicine ETHICS/PROFESSIONAL VALUES R R Respect for life Respect for people E I R E Empathy & Sensitivity Integrity & Ethics Responsibility & Reliability Enjoyment & Enthusiasm Mnemonic: RR EIRE 46 FACTORS AFFECTING DOCTOR RESPONSE Example Question: What would affect your decision? His own feelings and how they are dealt with Consideration of the Practice Finances Involvement of other Professional and Voluntary Bodies in addition to the Dr’s consideration of purely medical management options PLUS Time available Feelings engendered Financial (items of service fees?) Ethical Medico-legal (breach of driving regulations or confidentiality) Constraints on the Dr PERSONAL & PROFESSIONAL GROWTH Example Question : How can you become a better doctor? Self Awareness Self Assessment Reading & Literature Continued Education Personal Professional Balances PLANNING CHANGE Example Question: How would you set up a new diabetic clinic? A Assessment. P Plan R Resources… I Implementation delegation E Evaluation Consider all problem areas Decide what needs to be done? check availability, How to raise more funds? Decide who does what, when and where. Consider candidates almost always forget this! PLUS : A T T P Accessibility Team Work Time Management Priorities Organisation GIVING BAD NEWS Example Question: You receive an chest x-ray report on Mr X that confirms your suspicions of a bronchial carcinoma. How would you impart this information? Provide protected time Check your facts, Check their knowledge (?warning shot) Do not interrupt the pt, Cup of tea? PLUS A Anxiety try to elicit pt anxieties (All of the concerns) K Knowledge try to elicit pts knowledge E Explanation in simple terms, Rx, prognosis & UNDERSTANDING S Sympathy & support FU. RECHECK Mnemonic : AKES 47 CONFLICT SITUATION Example Question: What would you do with a patient who demands a specialist referral for something you consider trivial? It may be appropriate to A Agree/Disagree R Refer to 3rd party N Bargain or Negotiate a compromise C Counsel E Educate DEALING WITH ANGER Example Question: Mr. Davies, a 24 y old man, comes to you demanding a repeat prescription of Viagra. He does not fulfil the criteria for treatment on the NHS. He is clearly irritated by this news. How would you handle the consultation? A F V E R Avoid Confrontation Facilitate discussion Ventilate Feelings Explore Reasons Refer/Investigate Mnemonic : AFVER 48 Practise MEQ Paper Question 1 Read Paper 1: Oral Contraceptives and Myocardial Infarction: results of the MICA case-control study. Dunn et al, BMJ June 1999: 7198: 1579-1583 Comment on this study. PAPER 1 Oral contraceptives and myocardial infarction: results of the MICA casecontrol study Nicholas Dunn, Margaret Thorogood, Brian Faragher, Linda de Caestecker, Thomas M MacDonald, Charles McCollum, Simon Thomas, Ronald Mann BMJ June 1999: 7198: 1579-1583 Abstract Objectives To determine the association between myocardial infarction and use of different types of oral contraception in young women. Design Community based case-control study. Data from interviews and general practice records. Setting England, Scotland, and Wales. Participants Cases (n=448) were recruited from women aged between 16 and 44 who had suffered an incident myocardial infarction between 1 October 1993 and 16 October 1995. Controls (n = 1728) were women without a diagnosis of myocardial infarction matched for age and general practice. Main outcome measures Odds ratios for myocardial infarction in current users of all combined oral contraceptives stratified by their progestagen content compared with non-users; current users of third generation versus second generation oral contraceptives. Results The adjusted odds ratio for myocardial infarction was 1.40 (95% confidence interval 0.78 to 2.52) for all combined oral contraceptive users. 1.10 (0.52 to 2.30) for second generation users, and 1.96 (0.87 to 4.39) for third generation users. Subgroup analysis by progestagen content did not show any significant difference from 1, and there was no effect of duration of use. The adjusted odds ratio for third generation users versus second generation users was 1.78 (0.66 to 4.83). 87% of cases were not exposed to an oral contraceptive, and 88% had clinical cardiovascular risk factors or were smokers, or both. Smoking was strongly associated with myocardial infarction: adjusted odds ratio 12.5 (7.29 to 21.5) for smoking 20 or more cigarettes a day. Conclusions There was no significant association between the use of oral contraceptives and myocardial infarction. The modest and non-significant point estimates for this association have wide confidence intervals. There was no significant difference between second and third generation products. 49 Question 2 The following is a diagrammatic representation from the Practice Annual Report with regards to referrals for a 5 doctored practice. Comment on the above data. Give possible explanations for the variation in hospital referrals made by each doctor. Question 3 You receive a telephone call from the headmaster at a local primary school. He reveals his concerns regarding a 6 year old boy, Robert, who has become increasingly disruptive in class. Robert has recently been placed in the care of foster parents (less than 3 months ago). His foster mother is a social worker. How would you handle this situation? Question 4 Moira Featherstone, a 49 year old frequent attender, comes to see you about generalised aches and pains. This is your eighth consultation with her in the past 6 weeks! She has seen numerous other doctors regarding this and detailed investigations have failed to yield anything fruitful. What might be responsible for her behaviour pattern and how can you help her? 50 Question 5 Your practice nurse develops the following asthma protocol as a result of discussions following a multidisciplinary team meeting. Word ‘Asthma’ to be written on top of the notes Indexed in disease register Treat energetically in the chronic phase with a B-stimulant Encourage patients always to have medication in reserve. Allow practice nurse to use nebuliser before being seen by the doctor. Must have pre- and post-peak flow rates Nebuliser not to be used more than 4 hourly by patients and not longer than 24 hours without a review by doctor. One nebuliser must stay on surgery premises at all times. Comment on this protocol – what alterations would you make What are the implications of introducing new protocols? Question 6 What interventions have been shown to be effective in the primary prevention of ischaemic heart disease? Question 7 Does prostate screening fulfil the criteria required for an effective and valid screening procedure? Justify your response with evidence from the literature. Question 8 What is the evidence for the effectiveness of different secondary stroke prevention strategies? Question 9 John Cottingham is a 70 year old man who has recently been diagnosed with colorectal carcinoma. He informs you that a letter is on its way to confirm this to you. He also explains that he is finding it more and more difficult to cope with his wife who suffers from severe rheumatoid arthritis. What issues does this raise (include how you might be able to help)? Question 10 You are currently in a 5 partner practice that does its own on call cover. However, one of the full time female partners suggests joining in with the neighbouring deputising service. What issues does this raise? 51 Question 11 The following is a graphical representation of the prescribing data for two practices (A and B) with regards to the musculoskeletal system. Both practices have 3 partners and both have a list size of around 6000 patients each. Musculoskeletal System 6 Cost (£,000) 5 Practice A 4 Practice B 3 2 1 2 3 4 5 6 7 Quarters (of the year) Comment on the presented data. Can you give reasons for the difference prescribing patterns seen between the two practices. What additional information might be helpful in interpreting these results? How can you investigate the high prescribing costs for practice B ? How might you modify prescribing behaviour in order to curb high prescribing costs? Question 12 Louise Thorpe, a 59 year old woman tells you that she is fed up of having to take HRT pills every day. She says she is going to stop them and try more ‘natural’ homeopathic regimes instead. How would you handle this situation? 52 MEQ PRACTISE PAPER ANSWERS QUESTION 1 Mnemonic: BARO DOS URDS CCA TWERC Background/Methods Background of the study and methods clearly indicated- good. Community based case control study using interviews and general practice records. Specific age group looked at in a specific time period - good. Patients selected from a variety of geographical areas, rather than, say Ireland, which has a high rate of acute MI’s- good. However, how were the women selected. What were the inclusion/exclusion criteria? Were the patients selected across a range of social classes or were they just from one specific class The subdivision of risk according to the generation of COC in use is good. Case controlled – good. And the controls were matched for age and General Practice – good. But were they matched for other confounding variables such as obesity, FH etc Method of collecting results : interviews are subjective and therefore prone to bias. Are patient notes reliable? Subgroup analysis used in statistical evaluation. Aims Clearly stated Relevance Issue is of great clinical importance. May affect future prescribing pending results. Originality This paper explores a specific issue. Not many studies have been done on this. Understandable Odds ratio clearly stated. Are there too many figures quoted? The results could have been better displayed by graphical/tabular means. Response Rate Not mentioned. Drop-Outs Not mentioned. How many were lost to the study at follow up??? Statistics Number of Cases = 448, Controls 1728, good numbers for statistical analysis. However, no mention of how an MI was defined/diagnosed! No average age, No age distribution mentioned! (are older women for instance more likely to get an MI post COC use?) A subdivision of patient characteristics would have been helpful. What is subgroup analysis? Odds Ratios clearly stated – good Confidence Intervals stated are good, but note that the confidence intervals are wide and therefore places a question mark on the odds ratio thus quoted. Confounding variables….obesity, cholesterol levels, family history….were these considered? Critical Evaluation Of Results Weaknesses of study not addressed re: bias, statistical error, wide confidence intervals etc Conclusion ‘No significant association between the use of oral contraceptives and MI’ – this is not a valid statement in view of the wide confidence intervals??? Conclusions are not justified. No comparison of results to that of other studies. No suggestions for future studies/improvements Applicability Community based. – good (applicable to general practice) However, inclusion/exclusion criteria not mentioned…..the patients in the study may not be representative of those found in general practice. Although the concept of the study is one of great importance, the wide Confidence Intervals place doubt on the significance of the results. The study is therefore not applicable to real life. Title, Author, Insitute, Journal Clear title (But what is MICA???), relevant to general practice Authors mentioned – but who are they, clinical psychologists??? Are they reputable? However, no mention of the institution! Study published in the BMJ…. A reputable peer reviewed journal Writing Style Essentially good and easy to understand Ethics Was it ethical to undertake such a study. No mention of application for clearance from an ethical committee References This is an abstract - No references to other up-to-date literature Conflicts of Interest Who was the study sponsored by?? Not mentioned. Did the sponsors have any influence on the way the study was conducted or in the analysis of the resutls 53 Question 2 Comment Well presented diagrammatic representation. Clearly laid out and well labelled. Dr A appears to refer the most (over 200) which is nearly 4 times that of Dr B and twice that of the others. (NB Comparisons like this gain marks!) Dr B refers the least (only 50) Drs C, D and E refer somewhere in between. Explanations Candidate must first point out that it is difficult to interpret the findings without further information: Individual list size Part time/Full time Special Interests of the partners What sort of referrals are these – inpatient/outpatient or both?? Why Dr A refers so much. Better diagnostician – picks up more general cases Has a special interest in something - hence picks up and refers more of these for Ix eg may run a cardiac clinic or something Dr A has a different patient group than the others eg more elderly or cardiac patients etc Dr A has a large individual list size Dr A is a trainer (hence, the GPR referrals are added on to his data) Dr A is over referring – has not much confidence in managing general practice problems Why Dr B refers so little Dr. B has a different patient group that does not require referral so much eg teenagers Dr B has a small list size Dr B is part time eg a clinical assistant Dr B has been on the sick leave, study leave or on annual leave during this period Dr B is under diagnosing (?needs more education) Question 3 First of all: Need to build rapport with child and family. Empathetic & Caring approach (cf CARITAs) Patient Issues What does Robert think ? Does he think he has a problem. Does he know what he is doing. Does he know why he is doing it What does he expect out of it Does he know why you are talking to him? Any reasons for his behaviour? Eg new parents, new home, uncertainty of the future Need for the consultations to be performed at the level of the child Family Issues Where are Roberts genetic parents How will they react – anger etc Family dynamics are foster parents themselves not getting on (marital dysfuction) is there a new addition to the family eg a new baby or other foster child Not settled in new home? Loss of genetic parents? Exclude abuse - verbal, sexual, neglect (either by former parents or current foster parents) School Issues What is the rest of his schooling & learning like? information from teachers, school nurse etc what does the Headmaster think is going on Is he being bullied himself?? Abuse by teacher? Effect on other children – how to handle the situation & caring for the victims of his behaviour What does the headmaster expect from you? Doctor Issues Need to take further history & examine the child Why is he in foster care in the first place Past history needs reviewing – re: behaviour, medical, psychiatric Exclude organic cause : eg depression, anxiety, supratentorial lesion? Developmental Assessment Eliciting further information from other sources eg teachers, the headmaster 54 Doctors Own Feeling : Divided loyalties, Sensitivity of the issue Difficulty in discussing with foster mum who is a social worker! Calling in the police – it always gets nasty Effect on the future doctor-family relationship Medico-legal/Ethical Issues : Foster Parents may sue for defamation of character if everything turns out to be okay However, remember : Child Protection Act (Best Interests of the Child is paramount) Confidentiality Issue : re discussing the case with others eg teachers, headmaster Management Issues Getting all parties involved Making parents aware of the situation (both genetic & foster) Help from other PHCT workers : social workers, heath visitor (have they noticed any problems), child psychologist, local child development unit Police protection if necessary Advising school on how to handle the situation/Robert FOLLOW UP Practice Issues & Dynamics What practice protocols are there to detect such at risk children eg is there a register may need too review the situation (an Audit!) Question 4 What might be responsible for her behaviour? Genuine Organic Disease polymyalgia rheumatica, arthritis, MS, malignancy Psychological Cause Attention seeking Behaviour; lonliness Somatisation Disorder – underlying depression/anxiety Personality Disorder Abnormal Health Beliefs Hidden Agenda’s work/family problems, Carer strain Doctor Dependancy has no self help management plans of her own Confabulation with a view to secondary gain getting med 3’s and hence social benefit How Can I Help Her Caring & Empathetic Approach (CARITA’s) & Developing a rapport Detailed listening make her feel like she is being taken seriously Further History elicit her concerns, what is she hoping for? Hidden Agenda’s; other problems in her life (including family, work etc) moods menopausal status etc Examination has someone else missed something? Exclude Depression (detailed MSE) Family Dynamics & educate them! Further Investigation as necessary (beware, further unnecessary Ix may fuel her behaviour!) Referral as necessary Management Advise on sticking to one Doctor.....continuity of care Provide self help management plans (helping her to treat herself) Treat any depression If somatisation disorder: limit further Ix as this may fuel her illness behaviour Reducing the Workload Get others involved (sharing the workload) eg could she see the nurse now and then rather than a Dr, counsellor, psychologist, referral to psychiatric consultant (beware: ‘Collusion of Anonymity’ (BALINT) ) Limitations and Boundariess: agree on frequency of visits (eg regular monthly visits and no other) and lay down firm rules on calling into the doctors....stick to this, make other aware Care of the Doctor 55 re: heart sink patients – need to recognise own feelings re-energise yourself for the next patient Ethics respect patient autonomy & her right to consult a doctor of her choice Key issue: Referrals If somatisation Disorder suspected avoid medicalising this! Avoid numerous Ix and Question 5 There are some basic rules that all protocols should follow. These are detailed below along with the critical appraisal of this particular protocol. The following mnemonic is provided as an aide memoire. ABCD SR RAF Comment & Improvements Aims The aims of the protocol are not stated – audit cannot be performed unless aims are quoted. Alterations: Better quality of care for chronic asthmatic patients, Education of asthmatics, Asthmatics to be involved in self-care programmes, Register of Asthmatic Patients Background Background as to why the protocol is being done not stated. Clinical Evidence Clinical Evidence upon which this protocol is based is not mentioned. Alterations: I would create a protocol that followed the BTS guidelines, BMJ 1993 (summary) Diagnosis criteria What are the criteria for diagnosing asthma so that you can follow this protocol? How do you separate asthma from other wheezy chest conditions? Alterations: Asthmatics diagnosed either by hospital consultant, or proven reversibility of airways obstruction (steroid trial) Subjects (target group) This protocol does mention that it is asthmatics that this guidance applies to. However, it does not say which type of asthmatics – acutes or chronics? As before, no mention on the definition of asthma. Alterations: Subject group: Chronic Asthmatics Responsibility Of AdministeringUpdating/Audit Someone should be responsible for administering and updating the protocol. The protocol mentions the use of a doctor and nurse in administering the protocol (point 5), but is there anyone else that should be involved. No mention of who is to update it, and how often should it be updated? Alterations: Doctor and Nurse to be involved in the administering of the protocol. Acute cases to be referred to the doctor. Nurse responsibility for updating the protocol in the light of new evidence and guidance. Referral Criteria No mention of the criteria that indicate emergency/non-emergency referral. Alterations: Refer all cases of acute asthma (mild/moderate/severe) to the doctor. I would include a list of alarm symptoms in the protocol. Audit No mention of when an audit is to be done, how often and by whom. Audit is essential for improving the delivery of care to patients. Alterations: Nurse to do audit. First audit on (Date). Subsequent audits yearly. Follow-Up Follow-up arrangements are not clear in this protocol. Alterations: Follow up of patients 6 monthly if stable. If not stable, frequent review pending stability. Implications of Protocols. To the Doctor/Practice Disadv More workload (in creating and administering it) More staff may be required Another room required for the clinic More expense (re: in prophylactic prescribing) Litigation: may (if you stick rigidly to protocols) may (re: improvement of care being delivered) Adv Better education of doctor of nurse attendance of patient Peace of Mind for the doctor (knowing good care being delivered) Improved Practice Quality of Care and hence prestige. work To the Patient Disadv. Label of Asthma Anxiety Adv Better care happier pt Better care Referrals Better care A&E Better care Mortality Better care Quality of Life Better care less time off 56 Question 7 Need to state Wilson’s Criteria for an Effective Screening Test C N E T Disease is Common and an important health problem Natural history of the disease is known There is a recognisable Early stage Suitable Test available T F T Test is simple, acceptable and cheap Facilities are available for and Rx Early Treatment should be of benefit P I C Chances of Physical and Psychological harm less than chances of benefit Interval for repeat screening should be set Cost effective (ie cost can be balanced against the benefit the service provides) Disease is Common Yes- 9000 deaths/year in the UK Lifetime risk : 1 in 11 Natural History of Disease Known No – It is still difficult to predict which Carcinomas will grow slow and which will metastasise Early recognisable Stage Current Screening tool : PSA level plus DRE (Digital Rectal Examination) Problem with PSA Sensitivity & Specificity (PSA with other diseases and with age) Test Available Yes – Urine DNA amplification test available, & very effective Test is Simple & Acceptable – yes, blood test and DRE generally acceptable to most. Other regard as an invasion of privacy! No studies on acceptability! But Quebec Study BMJ 1998, 46 000 men enrolled in Prostate Screening trial, only 25% uptake. Test is simple to perform (DRE – examination, PSA – labs) but the quality of DRE interpretation is dependant on the doctor) Cheap – yes Facilities available for and Rx; Treatment Available Contraversial (Editorial BMJ 1998) No controlled trials to show whether survival by active intervention Surgery vs DXT vs Hormonal Physical & Psychological Harm from Screening Not really studied. Most people with Prostate Ca will die of something else rather than their cancer! Also, the diagnosis Anxiety +++ Interval for Repeat Screening Set No – No agreed interval yet Cost Effective Little known Summary In view of this, routine screening should not be undertaken. (also agreed by Effectiveness Matters, University of York, 1997 Question 9 Firstly, develop rapport with both John & his wife. Empathetic approach with a good listening ear. Patient Issues Find out what does john know about Colorectal Ca & the treatment (ideas) Find out what his concerns are about Colorectal Ca with regards to his wife the future What is John particularly finding difficult to cope with? What is John hoping for, and what would he like from you? (expectations) Family Issues Discuss the following Informing the rest of his family (esp his wife)....... who is he intending on telling and how will he do it? Remember, this may affect the husband-wife-relative relationship How will other family members be affected by the new news? eg wife may get reactive depression denial, angry feelings, guilt , blame Doctor Issues 57 Recognise own feelings cancer and death are always difficult issues handling other family members, will family blame you? Need to take further history and examination Ring consultant & find hospital letter, more details: extent of the Ca, prognosis, treatment & its effects How has John reacted to the bad news (?coping, ?adjustment reaction, ?clinical depression)…..treat as necessary, explain it is natural to feel this way & he is not to blame Handling bad news Avoid confrontation, Facilitate discussion, Ventilate feelings, Explore his reasoning (re: fears of death/dying) Don’t forget to ‘debrief’ yourself Management/Social Issues Involve both John and his wife (and any other family members) in developing Management Plans. Immediate plans Symptomatic treatment for John (eg constipation, analgesia) Home help, other support services, meals on wheels etc Alteration to home to make life easier (eg rails, have they got a shower ?etc)....call in social services, help of Occupational therapist Be aware of ones own limitations & call in the help of other experts early (Palliative Care, Macmillan Nurses, your own PHCT members eg health visitor, social workers - PLUS DS1500 claim) Liaise frequently with hospital Longer term Can relatives or other supporting neighbours help out? ?Respite care ?Nursing home for wife? (depends on severity of disability) good and regular follow up (care in the community) provide emotional support for John & his wife during and after the illness (make sure John & his wife are being emotionally open with each other) Review wife & other family members is wife your patient? (if not, communicate with her GP’s) how much does she know? how bad is his wife’s condition is wife being adequately controlled (involve rheumatologist if not already done so) see husband and wife together (assess dynamics)......preferably in their own home & see if any adjustments required to home (social worker involvement) review other family members & monitor their adjustment to the news treat any depression Communicate with Hospital Practice Issues Place John on high priority list for visiting do we have such a list for such patients? Communication Ensure all PHCT members are aware of the management plan (re: terminal illness) Communication with hospital Need to ensure an efficient & effective set up is in place to communicate any changes in the status of such high priority patients eg weekly multidisciplinary team meeting Ethical Issues / Medico-legal Isues respect patient autonomy respect patient confidentiality living wills - will John want one??, how do they legally stand? Question 10 Female Partner Issues (Put yourself in her shoes!) Why is she considering the DDS? other commitments or hobbies family life being disrupted is she coping, ?too stressful, burnout What is she hoping for from a DDS? Other Partner Issues Are we all happy about transfering to a DDS. What do we all think need to arrange a practice meeting to elicit everybody's concerns acknowledge own feelings (To explore everyone’s concerns, to avoid confrontation, to manage and ventilate angry feelings) What to do if no uniformity in agreement? Lower workload better GP family life, lower stress/burnout risk, better morale Lower GP isolation as they get to know the other GP’s in the DDS 58 Practice Issues Less income - paying for the DDS, loss of night visit fees etc) More paperwork/new system set up eg screening and logging all calls on to the computer More workload on rest of staff eg educating patients about the service & how to contact it new leaflets etc Will patients leave the practice!!!! Effect on other team members (nursing staff, receptionists etc) Patient Issues Will they be unhappy wanting to see their own doctor quality of care from DDS fear of the unkown fear from bad publicity of similar DDS’s Continuity of care But may be better ease of access to medical care/advice DDS Issues Open to abuse Less likely to know patients - ?more litigation risk? Will need more staff & doctors to cover the extra workload/catchment area But more income - from the practice joining in Question 11 Comments Describe what you see! Well presented clearly labelled graphs. Practice A generally has a lower prescribing cost than practice B for the first 4 quarters. During the 5th quarter, there is a marked increase in prescribing for practice A. The 6 th quarter and thereafter there is a general decline for both practices Reasons for the Difference Prescribing Doctors – Practice B doctors prescribe more drugs than Practice A Practice B doctors prescribe more expensive drugs than Practice A ie A prescribe generically Practice B doctors are over diagnosing Practice B doctors are very active in disease management (ie ?Audit in place, ?Interested Dr) Practice A doctors are under diagnosing Practice A Drs send most to physio or alternative Rx, hence no need for medication Patient demographics Practice B has more sporty patients than practice A eg is practice B a student practice?? Drug Rep Influence on Practice B Reasons for decline in both practices after the 7th quarter Education Programme for patients – more self help Management, less drugs Audit completed, Dr more aware of prescribing costs! New partner employed with an interest in more alternative therapies Reasons for Peak in Practice A during 5th quarter Locum employed here prescribed heavily? New Drug rep? Additional Information that would be helpful More Prescribing Info Cost per item – was it drug volume or expensive drugs? Proportion : Generic vs trade name prescribing Proportion : Private prescriptions/patients (often this data not included in PACT!!) More details on the drugs prescribed ie more detailed PACT information Patient demographics – age, sex ratio, social class etc Partner details Special interests of the various partners Specialised in house clinics Drug Reps - frequency of visits, is there a deal??? Investigate the high Prescribing Detailed PACT report – Individual partner prescribing habits 59 High prescribing volume vs More expensive drugs? Generic vs Trade name prescribing Comparison to a similar practice matched for age, sex, social class etc (available from PPA) Look for explanations practice demographics (do they have more injury prone patients) More effective screening Partner interests, clinics, protocols etc Exclude unnecessary high prescribing ie appropriateness of Rx, Doctor knowledge of disease management, do they get too influenced by drug reps?? PPA may help further – ask them! For help Modifying Prescribing Behaviour to curb high costs Generic rather than trade name prescribing Dr. education – re: avoiding unnecessary Rx Use of protocols, audit to ensure protocols being adhered to Don’t see reps!!! Too much of an influence Drug formulary to develop – so practice cheap ones prescribed Awareness of all (partners, pharmacists, registrar etc) Question 12 Firstly, develop rapport with Louise. Provide empathy & a listening ear Patient Issues What does Louise know about the menopause, CVS risk, osteoporosis & HRT etc Why does Louise want to stop? inadequate control monthly bleeds other scares (eg Breast/Cervical Ca) expense of HRT (re: two prescription costs) or is she simply into natural medicines? Why has she come to me? What is she wanting from me? Why now? Doctor Issues Be aware of your feelings if she feels that conventional medicine has failed Further History & Examination & Investigations elicit any breakthrough symptoms that are not being controlled exclude co-existing pathology (eg irregular bleeding & endometrial Ca) Educate yourself are you up-to-date on HRT & the menopause? Management Issues Open discussion limited benefits of HRT other than symptom control provide leaflets the limitations & evidence base surrounding ‘natural’ therapies Treatment do what she wants consider non-bleed preparation if bleed free > 2 years control other symptoms (antidepressants, acne, vaginal creams etc) treat any co-existing pathology Referral to Gynaecologist for further expert advice??? Be aware of your own limitations discuss with practice nurse, gynaecologist, endocrinologists etc contact HRT society Practice Issues Audit : how many other women feel like this ? how many drop out of HRT? What has been the trend in HRT following publication of WHO and other recent data on its limited benefits Is there a need to set up a HRT clinic in order to ensure regular review of HRT patients? Ethics Respect patient autonomy 60 61 Critical Reading Questions (CRQs) 62 CRQs What Sort of Things Are They Looking for in the Critical Appraisal Questions? Answer: Your ability to state the main types of study design and methodology to recognise the strengths and weaknesses of each to identify the sources of bias and the efforts made to eliminate bias, including questionnaires and to identify the validity and reliability of studies interpret the results of presented material. This includes the ability to interpret (but not to calculate) commonly-used statistical measures such as power of studies, p values, confidence intervals, NNT, odds ratio, sensitivity, specificity and predictive value apply the strength of evidence to a clinical scenario apply an evidence-based medicine approach to a clinical scenario: e.g. formulation of a question, search strategy, appraisal of evidence, and application of evidence to the clinical problem 63 CRITICAL READING QUESTIONS - CRQs How to fail the CRQs × × × × Critical reading doesn't really matter No one really expects GPs to read anything published in a grown up scientific journal. Facts are for nerds and research is for anoraks. Make up some numbers if they really get picky Don’t answer what they’re asking for; if you have something more interesting to state, state it Approach frameworks for quantitative research papers on qualitative ones Preparing for the CRQs I would strongly urge you to read Trisha Greenhalgh’s entire 12 lessons on “How to Read a Paper” which can be viewed online at bmj.com. Here’s how: Go to www.bmj.com On the top right hand corner, you will see a “quick search box” Type in “greenhalgh” for author and “how to read a paper” under keyword Click go Hey presto, a list of what she has done. By default, bmj.com displays the first 10 articles. There are two more on the next page (click “next 10” at the bottom of the page) Critical appraisal is not an art. It is a SKILL than can be LEARNT. So practise! There are many toolkits available to help you scrutinise papers and derive balanced conclusions. Some of these can be found later on in this section. They tend to go into quite some detail and one must be careful not to lose sight of the main themes. When reviewing papers ask yourself four things: 1. WHY: Why was the study done? Is the question they are trying to answer reasonable? 2. HOW: How was the study done? Was it biased in any way (e.g. sample being studied, investigators) 3. WHAT: What did the study find? What statistics were used; were they sensible; do the numbers add up? 4. SO WHAT: So, what are the implications of the results? Are the conclusions sensible? How will they affect future practice? Appraising evidence is something most GPs do (and will do in the future). Think of it as a core competency skill (just like examining a patient). Make the process enjoyable as much as possible. The more papers you look and appraise, the easier it will become. Remember neurological examinations at medical school training? Most of us found it difficult, but with practice, you can do it in a jiffy. Critical appraisal is no different; a skill which, like any other skill, becomes easier the more you practice 64 Hot Tips for the CRQs Like I’ve said before, it might look like the CRQ questions require you to have read loads and loads of journals and acquired a vast amount of knowledge; the truth is, they don’t. Only 2-4 of the twelve questions usually ask DIRECTLY for evidence based medical knowledge. So don’t be put off by having to know tonnes of evidence. The likelihood is that you probably know most of it anyway but you just don’t know the papers. How many of you prescribe aspirin post MI? (Most of you) Why? (because you know it reduces mortality) And what’s the evidence? (The knowledge: “aspirin reduces mortality” is the evidence! A better answer would say by 30% as shown in the ISIS2 study). Most marks a given for your understanding of the literature, whereas relatively few marks are awarded for accurately quoting references. The examiners will have a prepared marking schedule and an up-to-date list of references; so forget the idea of making something up like “as shown in the Journal of Indian Medicine, Jan 2005” 65 CLINICAL EPIDEMIOLOGY FOR THE MRCGP EXAMINATION “Today’s therapy, instigated solely as a result of clinical experience, becomes tomorrow's bad joke." Clinical Epidemiology. A Basic Science for Clinical Medicine, D.L.Sackett, R.B. Haynes, G.H. Guyatt, P. Tugwell 2nd. Edition. 1991. Little, Brown The concept of "evidence based medicine" (EBM) has received much attention in recent years. It was first advocated by Archie Cochrane in "Effectiveness and Efficiency" and has been taken on David Sackett (now of Oxford University) and his colleagues from McMaster and Ottawa Universities 1i1. The development of EBM is inextricably linked with the landmark publication of "Effective Care in Pregnancy and Childbirth" by Ian Chalmers and colleagues in 1989 [2]. It involves the application of clinical trial evidence to everyday care as a means of closing the gap between research and everyday practice. Four steps are involved: 1. Accurate identification of the question to be investigated. 2. A search of the literature to select relevant articles. 3. An evaluation of the evidence in the literature selected. 4. Implementation of the findings in clinical practice. The fears of some clinicians that these developments threaten the concept of the individual doctor - patient relationship are an understandable emotional reaction to the change threatening current practice. In fact the obverse is true. In order to deliver evidence based medicine to individual patients greater clinical skills are required. Diagnoses must be ever more accurate, communication skills need to be honed to a fine art to achieve a jointly agreed and understood management plan between doctor and patient, and new skills learnt to master the scientific basis of clinical practice. It must be recognized even by evidence-based enthusiasts that there are limits to this approach. As knowledge about specific effective interventions becomes clearer, the difficulties of applying this knowledge and judgment to individual patients who may will have multiple pathologies or risk factors means that increased professional expertise will be demanded of doctors. As treatment improves the stakes involved in delivering optimal clinical care increase. Combining multiple interventions into clinical strategies on an evidence base is problematical. Two interventions can be combined in two different ways. Five interventions results in a possible one hundred and twenty combinations. The risk of "cookbook medicine" taking over is not credible but neither is continuing with practice based solely on opinion and clinical experience. Continuing Medical Education for the 21st. Century. There is increasing emphasis on effectiveness and efficiency from patients and professional leaders. The challenge is to achieve the best care for individuals and the population in the face of increasing health care costs, demographic change and the pattern of disease (notably the ageing population and the increase in chronic health problems), biomedical advances and communication of knowledge previously only vested intra-professionally. These forces lead inevitably to changing requirements in medical education; the inclusion of clinical epidemiology in the MRCGP syllabus is a response to this obligation. Attitudes, behaviour, critical appraisal skills, consultation skills flexible thinking, and access to data about and implementation of effective care are now as important as the mere possession of biomedical information (Fig. 1.). 66 Chance, Bias and Confounding Variables. In any study of the effect of a medical intervention on the natural history of a disease one would expect to see results clearly stated. They may show that the intervention has been successful and reduced deaths or disability. We need to know whether it is likely that these results have occurred by chance, whether the results could be biased by the design of the study or by the inclusion or exclusion of some patients, and also to consider whether another factor (termed a confounding variable), independent of the intervention, is producing an erroneous conclusion. Chance and bias are straightforward issues. An example of a confounding variable (Fig. 2) is the study which shows an association of coffee drinking with an increased rate of carcinoma of the bronchus. In fact it is smoking that is the intervention responsible for the lung cancer and coffee drinkers were more likely to be smokers. The solution to avoid this confounding variable would be to have two groups of coffee drinkers - smokers and non-smokers. The rates of lung cancer could then be determined in both groups. A confounding variable may therefore be considered as a particular type of bias, and several biases may occur (and therefore need to be taken account of) in a single study. If we were to run a study to determine whether regular exercise lowers the risk of coronary heart disease we might do so by offering aerobic classes to employees of a large company and then measuring the number of coronary events in the groups 67 who did and did not volunteer for the classes. The events would be determined by regular check ups including a careful history, an electrocardiogram and a review of GP and hospital records. The results of this (hypothetical) study show that the exercise group had fewer cardiac events. However, the review of records also showed that the exercise group smoked less. Selection bias could also operate if the exercise group were at lower risk before the programme began - did they have less hypertension, lower blood cholesterol and more favourable family histories? Measurement bias may occurred because those participants who knew they had had coronary events could be more likely to attend for their study check up and report their problem. Finally the lower cigarette consumption in the exercise group would be a confounding bias. TYPES OF STUDY It is helpful to separate out studies that are observational (and are therefore hypothesis-forming) from those that are analytical (and therefore hypothesis testing). Observational - Hypothesis Forming: (i) Case reports and case studies. Many important advances in medical knowledge begin with simple descriptions of a small series of cases presenting clinically to astute doctors. e.g. five cases of male homosexuals in San Francisco with pneumocystis carnii as the cause of their pneumonia, subsequently shown to have HIV infection and AIDS. There is usually no attempt to determine whether causal association in the study - the purpose of the report is to raise awareness. Proof will only be provided by more extensive investigation. (ii) Cross Sectional Studies. Also termed prevalence studies (see below), this method involves a survey of a given population and attempts to correlate between personal factors and disease states. It cannot measure cause and effect, nor can it determine changes between exposure and disease. Again, it may lend weight to a more rigorous investigation being required. (iii) Correlational Studies. Sometimes termed ecological or geographic studies, these look at the number of cases in a given population at any given time (the prevalence) or the number of new cases occurring in a given time (the incidence), and compare the prevalence or incidence with another population. Limited information as to causation can be obtained but useful inferences can sometime be forthcoming e.g. migrant studies of Japanese from - their home country to the United States and their rate in successive generations of acquiring the pattern of ischaemic heart disease of Americans. Analytical - Hypothesis Testing: In order to determine whether a possible factor really is involved in a disease, or a particular intervention really does improve the treatment of that disease we need a different type of analysis. (i) Case Control Studies. Case control studies take a sample of patients with the disease - the cases - and match these cases with a sample of the population who do not have the disease - the controls. The controls need to be as similar as possible to the cases (except in respect of the risk exposure) to reduce bias. The case control study then looks backwards in time and tries to determine the frequency of exposure to the identified risk factor in both cases and controls. 68 The odds ratio of the exposure resulting in the disease can then be calculated from: ad bc An odds ratio of I would show no association, a value below this a protective effect of exposure and numbers in excess of one a possible association, though a causal relationship would require further consideration in almost all circumstances. It should be noted that an odds ratio from a case control study is not a measure of the risk in the general population - as an inherent part of their design case control studies cannot provide incidence data. Hypothetical results from a case control study designed to see whether lung cancer is linked to smoking might produce the following table: Table 1. EXPOSURE (lung cancer) Yes (smoking) (lung cancer) No Yes The odds ratio would therefore be DISEASE Cases 56 Controls 230 7 246 56 x 246 = 13776 = 8.6. 7 x 230 1610 This would be a large enough odds ratio to indicate the possibility that there was a true association between exposure and disease. An example of the usefulness of the case control design was published in 1994 [3]. Several case series had previously shown that in patients with low back pain a magnetic resonance imaging scan (MRI) had demonstrated lumbosacral disc abnormalities in the majority of patients. However, when a control group was also studied a similar incidence of disc abnormalities was found in the control group. This results an odds ratio approximating to 1 and therefore doubts being expressed concerning the hypothesis that the abnormalities seen on MRI scanning in cases of low back pain are related to the cause of the pain. 69 (ii) Cohort Studies. In a cohort study a sample of the population who have the potential to develop a disease are assembled. This sample is then classified into characteristics (possible risk factors) that might be related to outcome. Observation over time then takes place with collection of data to see which members of the cohort experience the outcome being measured. Cohort studies are sometimes called longitudinal or incidence studies. Fig. 4. Sometimes cohort studies are performed where the sample is selected historically. A good example of this is the UK birth cohorts where all babies born in a single week in 1948, 1958 and 1970 have been followed throughout their lives. The sample is available for follow up in the present but the cohort is assembled in the past. A concurrent or prospective cohort study assembles the cohort in the present and is then destined to follow the cohort forward with follow up at a designated point or points in the future. Cohort studies also usually present their main results in the form of a table: The simplest analysis consists of attributable risk (sometimes called absolute risk or risk difference) and relative risk (sometimes called risk ratio). Attributable risk answers the question "What is the incidence of disease attributable to exposure" and is simply a - c. Relative risk answers the question "How many times are exposed persons more likely to develop the disease, relative to non-exposed persons?" i.e. the incidence in the exposed divided by the incidence in the non-exposed. This is expressed as _a_ a+b divided by _a_ c+d As an example let us consider the development of deep vein thromboses (DVT) in oral contraceptive users. Hypothetical results might look something like Table 2. OUTCOME (DVT) Table 2. Exposed (on oral contraceptive) Not exposed (not on o.c.) Yes 41 7 No 9996 10009 70 These results would give an attributable risk of 34 and a relative risk of 6 - significantly large enough numbers to indicate the possibility of a real association between exposure and outcome. However, the possibility of biases very often arises in studies and the risk is greater in designs that are other than randomized trials. In this case, are women at higher risk of DVTs given an oral contraceptive? Is it possible that women on oral contraceptives are more likely to themselves report symptoms of a DVT, whereas women not on the treatment will ignore them? Are doctors more likely to make the diagnosis when their own suspicions have been raised by their patient's current medication? These are real possibilities and a well designed study will provide evidence to restrict or refute influences that may skew the result. A good example of a cohort is the Framingham study [41 which was started in 1949 when a sample of 5209 men and women aged between 30 and 59 were selected as a representative sample from about 10,000 persons of that age living in Framingham, near Boston, USA. The study was set up to identify factors associated with coronary heart disease and 5127 of the cohort were free of the disease when first examined. As is well known, the risk factors that have been identified that are associated with the development of coronary heart disease are elevated blood pressure, hypercholesterolaemia, cigarette smoking, diabetes mellitus and left ventricular hypertrophy. Since the sample is representative of the population and its size is related to the true population, real incidence figures are availab le from cohort studies. This is one of their major advantages. (iii) Randomized controlled trials. Randomized controlled trials (RCTs) are often referred to as "the gold standard" when evidence based medicine is discussed. This is because their design restricts the biases that may influence the results of case control and cohort studies. They are undoubtedly the standard of excellence for assessing the effects of treatment. Fig. 5. The design of randomized controlled trials is familiar. The patients to be studied are selected by defined criteria from a larger number of patients with the condition under investigation. Those who then agree to participate in the , study are then randomized (by a system analogous to tossing a coin) into two groups of comparable prognosis. Randomization produces two groups which differ only by chance - the purpose is not to produce equal groups, though in large trials the groups that emerge are balanced. Two comparable interventions are then applied to the groups and the outcomes measured. Ideally patients, their attending physicians and the study investigators should all be unaware of which patients received which treatments - a process known as blinding. Both randomisation and blinding are used to avoid bias, with errors in the results obtained therefore restricted to chance. Where small improvements in outcomes are expected from the intervention under investigation, large numbers of patients are required for the trial. Finally the RCT design needs to consider whether the objective is to find out whether offering treatment helps in normal clinical practice or whether the treatment is efficacious under ideal circumstances. For example, if we were investigating a new antibiotic used for pneumonia we could design an RCT where the outcomes could 71 either be clearance of the causative organism from the sputum or the length of stay in hospital. The first study might show that the organism was cleared faster than placebo or an alternative antibiotic and (all other aspects being equal) would produce a valid assessment of the drug's efficacy. However, for this result to be generalisable to everyday practice we would want to know that patients got better quicker and were able to leave hospital earlier. Conducting a trial with such an outcome would, however, potentially lead to the introduction of other variables (e.g. concurrent or intercurrent illnesses, variations in administration procedures and policies on discharge from hospital) which could bias the result. RCTs therefore often try and strike a balance between validity and generalisabilty. They may often only answer one or other question - and the subsequent debate fills up the correspondence columns of medical journals. An additional problem is that RCTs are, by definition, measuring treatment being provided in an experimental (and therefore artificial) setting. Transferring a valid result from the RCT carries the risk of sub-optimal results due to the different setting and conflicting pressures of everyday clinical care. Presenting the results of an RCT would produce table 3. The results of an RCT are often only presented as a relative risk reduction (RRR) e.g. "magicillin reduces the length of stay in hospital in patients with pneumonia by 45%." Whilst the RRR answers the question "How much better is the active treatment than the comparison intervention?", it does not take into account the incidence of the disease in the population. If we are to assess the value of magicillin to society we need the absolute risk reduction (ARR) which answers the question "How many fewer patients will get the outcome I am measuring if I use active treatment instead of the comparison intervention". Table 3. OUTCOME Yes No Comparison intervention a b Experimental intervention c d Absolute risk reduction is therefore the comparison intervention patients with the outcome out of the total of the comparison patients minus the experimental patients with the outcome out of the total patients on experimental treatment. i.e. _a_ _ _c_ a+b c+d Relative risk reduction is ARR in a ratio to the outcomes measured in the comparison group. i.e.. _a_ _ _c_ a+b c+d _________________________ _a_ a+b These complicated formulae become clearer if we consider real data from the recent 4S study [5]. Table 4. OUTCOME (death) Yes No Total Comparison intervention (placebo) 256 1967 2223 Experimental intervention (simvastatin) 182 2039 2221 The ARR is (256/2223) - (182/2221) = 0.115 - 0.082 = 0.033. The RRR is 0.033/0.115 = 0.29 or expressed as a percentage 29%. 72 Treating patients with established coronary heart disease (CHD) with simvastatin for a mean duration of 5.4 years in the 4S study therefore reduced all cause mortality by 29%. All in all, a pretty impressive result - even when the particular circumstances of a RCT and the patients excluded from the study are taken into account. However, in order to assess the benefits when the study is applied to the population we need to consider the incidence of deaths from coronary from heart disease. The ARR takes this into account but the figure of 0.033 is difficult to interpret. The figure contains more useful information than the crude risk reduction but the decimal form is unfamiliar to clinicians. What does 0.033 mean in practice? This difficulty is solved by dividing the ARR into 1 i.e. by taking its reciprocal. This turns out to be the number of patients we need to treat with the experimental intervention to prevent one outcome. 1/0.033 = 30. We therefore now know the number needed to treat - we need to treat 30 patients with coronary heart disease for 5.4 years with simvastatin to prevent one death - a much more accessible and meaningful statement than "the absolute risk reduction is 0.033". Numbers needed to treat (NNTs) are now starting to be quoted in trials in the mainstream peer-reviewed medical journals. The clinical effectiveness industry is also busy calculating NNTs for current interventions. Some of these are presented in table 5 (N.B. Refer to the original studies for full details - this data is accurate and very interesting as a crude comparison between interventions, but the full picture from the original papers is required to obtain the nuances of e.g. trial design, withdrawals, exclusions, blinding and other potential biases.) Table 5. Source: [6]. INTERVENTION OUTCOME NNT Streptokinase + aspirin v. placebo (ISIS 2) prevent 1 death at 5 weeks 20 tPA v. streptokinase (GUSTO trial) save 1 life with tPA usage 100 Simvastatin v. placebo in CHD prevent 1 major event in 5y 15 Treating hypertension in the over-60s prevent 1 major event in 5y 18 Aspirin v. placebo in healthy adults prevent MI or death in 1y 500 Now the clinical effectiveness picture begins to make a little more sense. We can advocate streptokinase with aspirin in myocardial infarction, treating hypertension in the over 60s and using simvastatin in coronary heart disease, whilst being very cautious at first glance about primary prevention of CHD with aspirin and about the overall benefits of tPA over streptokinase. We need to know more about the particular studies to determine their generalisability and whether there are some special subgroups of patients where the benefits might be greater or less than the population in general, but the numbers needed to treat allows some useful comparisons between the proportional benefits of different medical treatments and their overall contribution to healthcare. Even so there are caveats to be added. We have not considered the side effects of our interventions. How many patients with hypertension will develop impotence, gout or diabetes as a result of our treatment? How serious a risk is there of rhabdomyelosis or hepatitis with simvastatin? How great is the risk of causing a haemorrhagic stroke or serious anaphylactic reaction with streptokinase? Further development is therefore likely towards a combined index which will result in accessible compilation of data that will incorporate both the benefits and the risks of interventions, together with an indication of the likely improvement in the quality as well as the quantity of life. Still there will be difficulties in applying this data to individual patients with multiple pathologies and risk factors. But it is easy to envisage not very far in the future expert guidance software on the GP's desktop that will calculate the odds of different interventions based on an biological data for that patient - patient and clinician then discussing and compiling a management plan based on 73 evidence rather than clinical experience and opinion. Clinicians therefore need to understand how to access and assess information on effective interventions individual studies, meta-analyses and systematic reviews - and to be effective communicators of this new information to their patients. TESTS OF SIGNIFICANCE Statistics is for many clinicians a concept even more detestable than management. This is due to our own value systems, mathematical ineptitude and the fact that mathematics and statistics are almost always taught by highly competent and qualified mathematicians. Unfortunately this means that not only do they speak another language from their students but they also find it a frustrating experience in trying to instruct what are to them very simple concepts. Disillusion quickly sets in upon both parties, confusion and bewilderment are not far behind and another biological scientist thinks understanding statistics is an impossibility. Two principles stand out when it comes to statistics. 1. Since most of the really important evidence-based medicine is based on randomized clinical trials, only knowledge of what probability and confidence intervals are and what they mean is required. 2. For those who wish to learn a little more there is an understandable introduction to statistics written by a psychologist in terms that non-mathematicians can understand. Most medics usually only come to this advanced stage of development after the passage of some time and the internal kindling of a spark of interest by a chance event, rather than being driven by the external forces of needing to pass an examination. "Simple Statistics" [7] is a truly wonderful book and deserves to be regarded as a classic. Probability. Trials are analyzed on the basis that there is no difference between the treatments. This is termed the "null hypothesis". The probability that the observed differences could have occurred by chance is tested and the familiar p value is obtained. By convention, if a result is obtained which could only have occurred by chance once in twenty times this is judged to be "significant". Once in twenty is the same as five times in a hundred and this is expressed as p = 0.05. For example, in a randomized controlled trial there is found to be fewer deaths with treatment A than with treatment B. We need to know whether this result could have occurred by chance. Our statistician with the computer software tells us that the p value is 0.001. This means that there is only a 1 in 1000 chance of that result occurring by chance and there is a significant difference between our treatments. The usefulness of p values is limited on some occasions. A result of 0.049 is by convention significant (since it is less than 0.05), whereas one of 0.051 is by convention not significant. Clearly that is nonsense. The second problem is that the magnitude of the differences between treatments is not explained by probability. No statistical test can definitely prove anything. All statistics can do is quantify the likelihood that the observed result is a real effect rather than due to chance. Clinical significance should always be considered as well as statistical significance. Confidence Intervals. The confidence interval (CI) around a result observed in a sample of patients in a study indicates the range of values within which it is fairly certain (usually 95% certain) that the result of the same intervention applied to the true population would lie. For example, we have seen that the results of the 4S study show that we need to treat 30 patients with established ischaemic heart disease with simvastatin for 5.4 years to 74 save one life. If we apply confidence intervals to the data we get 95% CI of 18 - 80. In other words, if we use simvastatin in the same way as the 4S researchers did, in the population as a whole we will save one life for somewhere between every 18 and every 80 people treated. ADVANTAGES AND DISADVANTAGES OF DIFFERENT TYPES OF STUDY We need to look for studies that produce the strongest evidence in order to provide valid answers to clinical questions. This means reducing the biases which in turn means that a well designed randomized clinical trial will always be the preferred type of study. Enthusiasts of evidence based medicine will often only consider in their systematic reviews evidence from RCTs and reject results from other types of study. Experience has shown that many interventions adopted on the basis of evidence other than a well done RCT has subsequently been shown to be harmful when that RCT is done [8]. However, the non-experimental case control and cohort studies clearly do have a place. They are often the only methods that are applicable to determine adverse effects - it would be unethical to conduct a randomised controlled trial in which the investigators were to expose the active group of participants to something that was likely to do them harm. For example, imagine in the 1950s discovering for the first time that there was evidence from a case series and geographical data that smoking seemed to be associated with lung cancer. Would it be ethical to take 200 medical students and get half of them to smoke 20 cigarettes a day for thirty years and get the other half to be non-smokers? A much more sensible approach would be to construct a cohort or case control study and reduce the possibility of an erroneous result by limiting the potential for bias. Case control studies are also particularly useful to analyse rare disorders. However, a clear hierarchy of evidence exists with RCTs providing the strongest evidence, next come cohort studies and then case control studies. Figure 6 illustrates the influence of bias in studies of the effectiveness of beast screening. Figure 6 shows that all the studies have a relative risk of less than 1, i.e. screening produces a protective effect - a reduction in mortality in the screened women. The horizontal lines and bars indicate the 95% confidence limits. It will be noticed immediately that the geographical and case control studies show greater benefits than the randomized trials. Three biases operate to produce this effect: 75 lead time bias - screening advances the date of the diagnosis and hence the survival time, although the date of death is not altered by the earlier detection. length time bias - the preferential detection of slowly growing tumours. selection bias - tendency for people who volunteer for screening to be atypical of the population from which they come. Selection bias is removed by randomisation whilst the others remain. These details are not in themselves important but they illustrate why caution is required when considering evidence other than from randomised trials. If a study is well designed and conducted the results can be considered to be valid. However, other factors such as the subjects being equivalent to those in one's own practice, the result being clear statistically (and in addition having clinical significance) and the setting of the study (e.g. in a health care system similar to the NHS) will influence whether the results are generalisable. SCREENING FOR DISEASE There is an inherent attraction in being able to detect a disease at an early stage that will lead to a greater proportion of the detected cases being successfully treated. With cervical and breast screening already well established and advocates for prostate and colonic cancer becoming ever more vocal, there is an increasing need to look closely at current practice and judge it and future programmes against explicit criteria of benefit for individuals and for the population. "Wilson's Criteria". (Wilson and Jungen. World Health Organisation, 1968) Condition should be common and important / serious Natural history of disease understood with latent period in which disease can be detected Successful treatment by an agreed method available when detection occurs Screening test should be safe, acceptable to patients, screening to be continuous, on a group agreed to be high risk 6. Test should be cheap (or at least cost-effective) 7. Screening programme delivered via an agreed policy TEST 1. 2. 3. 4. 5. POSITIVE DISEASE POSITIVE NEGATIVE a b NEGATIVE c d A successful screening test will have few false negatives (sensitivity = a/a+c) and few false positives (specificity = d/b+d). Judging screening programmes is further complicated by lead time bias, length time bias, and compliance bias. Not surprisingly the Chief Medical Officer has accepted the first recommendation of the new (1996) National Screening Committee - no new local screening programmes are to introduced in the UK until rigorous evaluations are made available by this expert group. 76 References. 1. D.L.Sackett, R.B. Haynes, G.H. Guyatt, P. Tugwell. Clinical Epidemiology. A Basic Science for Clinical Medicine. 2nd. Edition. 1991. Little, Brown. 2. Chalmers, M. Edkin and M.J.N.C. Keirse (eds). Effective Care in Pregnabcy and Childbirth (Vols 1&2). Oxford. Oxford University Press. 1989. 3. M.C.Jensen et al. Magnetic resonance imaging of the lumbar spine in people without back pain. New Engl J Med 1994; 331: 69-73. 4. TR Dawber. The Framingham Study. The Epidemiology of Atherosclerotic Disease. Cambridge, MA. Harvard University Press, 1980. 5. T.R.Pedersen et al. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994; 344: 1383-89. 6. Bandolier. No 17. 1994. Oxford. 7. Frances Clegg. Simple Statistics. 1982. Cambridge. 8. The Cardiac Arrythmia Suppression Trial (CAST) Investigators. Special Report. Preliminary Report: Effect of ecainide and flecainide on mortality in a randomised trial of arrythmia suppression after myocardial infarction. N Endl J Med 1989; 321: 406. 9. Breast Screening Advisory Committee. Breast Cancer Screening: Evidence and Experience since the Forrest Report. 1991. NHSBSP. 10. NE Day. Screening for Breast Cancer. British Medical Bulletin. 1991; 47: 400 15. This handout has been adapted from "Clinical Effectiveness in and Through Primary Care" by Mark Baker, Neal Maskrey and Simon Kirk; Radcliffe Publications (in press). Copyright applies. Neal Maskrey. February 1997 77 STATISTICAL TERMS- made simple Consider: Antibiotics in children with Otitis Media 2 groups Treatment group: with antibiotics Control group: NO antibiotics Study to measure symptom of pain at 7 days Results as follows: Results Still had pain No pain Total number Treatment Arm 20 91 111 Control Arm 29 85 114 Let’s look at some terms and relate them to these results: RISK 20/111 = 0.18 Risk of having pain is 18% 29/114 = 0.25 Risk of having pain is 25% ODDS 20/91 = 0.22 29/85 = 0.34 ODDS is a similar way of looking at the risk. Odds are used in metanalyses where several studies are used RELATIVE RISK (OR RISK RATIO, RR) RR = 0.18/0.25 = 0.72 (72%) If: RR=1 This implies that there is no difference in pain RR<1 This implies that there is less risk of having pain with antibiotics ODDS RATIO (OR) RELATIVE RISK REDUCTION (RRR) OR = 0.22/0.34 = 0.6 RR = 0.72 ie less pain with antibiotics, but by how much? I - 0.72 = 0.28 (28%) ie antibiotics reduce pain by 28% = RRR Another way of doing it is: (Control - Treatment)/Control = 0.25-0.18/0.25 = 0.28 = 28% ABSOLUTE RISK REDUCTION(ARR) (aka risk difference) = control risk - treatment risk = 0.25-0.18 = 0.07 (7%) i.e. 7% of Children would have benefited from antibiotics with respect to pain symptoms NUMBER NEEDED TO TREAT (NNT) Defined as 1/ARR = 100/7 = 14 i.e. need to treat 14 children for 1 to benefit from antibiotics with respect to pain CLINICALLY, NNT IS THE MOST USEFUL OF THE INDICES 78 Critically Evaluating Quantitative Papers – Made Simple! Example Question: The following paper was published in the BMJ 2000 . Critically evaluate this paper. Mnemonic : BARO (think of a barometer) DOS URDS CCA TWERC The Introduction Bit Background Aims Relevance Originality The Methods Section Design Outcome Measures Subjects The Results Section Understandable Response Rate Drop-Outs Statistics The Discussion Bit Critical Evaluation of Results Conclusion Applicability Other Bits n Bobs Title, Author, Institute, Journal Writing Style Ethics References Conflicts of Interest Background to the study is clearly stated…ie why what it done? Clearly stated? Is it relevant to general practice? Is it an original concept or is it something that we already know a lot about? Appropriate design? Instruments (eg survey questionairres) should be valid and reliable. Any confounding variables? Should be valid and reliable (consistent) Good enough Numbers? Randomisation? Control group included? Are they representative of the population? Clearly stated results? Easy to digest format eg graphs, charts etc? Is it stated? How many drop outs, failure to follow up etc were there? Big or small? Statistical tests should be appropriate Are results discussed critically? Do authors discuss possible sources of bias? Are results discussed in light of other literature/research? In keeping with the results? Is it applicable to your practice population? Will it change the way you practice? What further research needs to be done? Author…professor or researcher?? Institute/Journal – reputable?, peer reviewed? Easy to read format? If ethics involved, did they go to the local ethics committee for approval? Clearly stated? Up to date references? Any sources of conflict eg who funded the study…was it the pharmaceutical company manufacturing the drug??? Adapted from ‘Critical Reading Questions for the MRCGP’ by Ese Stacey & Yinkori Toun, BIOS Scientific Publishers Limited, 1997 79 Evaluating Quantitative Papers – Method 2 RCTs: Questions to help you make sense of a paper. Adapted from: Greenhalgh,T and Taylor, R. How to read a paper: Papers that go beyond numbers (qualitative research). BMJ, 1997;315:740-743 and work by John Wright, Consultant in Clinical Epidemiology, Bradford Royal Infirmary, by Nick Price. Question 1: Did the paper address a clearly focused issue? Population, intervention, outcomes Comment: Yes Can’t tell No Question 2: Was the assignment of patients to treatments randomised and was the randomisation concealed? Comment: Yes Can’t tell No Question 3:Were all of the patients who entered the trial properly accounted for at its conclusion? Yes Can’t tell No Yes Can’t tell No Yes Can’t tell No Yes Can’t tell No Question 6: Were the groups treated equally other than the experimental intervention? Comment: Yes Can’t tell No Question 7: What are the results? Are they clinically important? How large is the treatment effect? Is this statistically important? What is the probability this occurred by chance? Comment: Yes Can’t tell No Yes Can’t tell No Question 9: Are the findings of the study transferable to other clinical settings? Are your patients similar or different to those in the trial? Are you working in a similar context? Comment: Yes Can’t tell No Yes Can’t tell No Question 11: Does this fit with your and your patients’ values and preferences? Comment: Yes Can’t tell No Question 12: Will your patients’ needs and preferences be met by this regimen? Comment: Yes Can’t tell No Were they analysed in the groups to which they were randomised?. Comment: Question 4: Were patients, health workers and researchers ‘blind’ to the treatment? Comment: Question 5: Were groups similar at the start of the treatment? e.g. in terms of other factors that might affect outcome. Comment: Question 8: Are the results clinically important? What are the NNTs, NNHs, would you take this treatment? Comment: Question 10: Were all the clinically important outcomes considered? Comment: OVERALL, WHAT DO YOU THINK: (weigh up the 12 questions? 80 EVALUATING QUALITATIVE PAPERS Qualitative research: Questions to help you make sense of a paper. Adapted from: Greenhalgh,T and Taylor, R. How to read a paper: Papers that go beyond numbers (qualitative research). BMJ, 1997;315:740-743. John Wright & Nick Price, Bradford Question 1: Did the paper describe an important clinical problem addressed via a clearly formulated question? Comment: Question 2: Was a qualitative approach appropriate? Yes Can’t tell No Yes Can’t tell No If the objective of the research was to explore, interpret, or obtain a deeper understanding of a particular clinical issue, qualitative methods were almost certainly the most appropriate ones to use. If, however, the research aimed to achieve some other goal (such as determining the incidence of a disease or the frequency of an adverse drug reaction, testing a cause and effect hypothesis, or showing that one drug has a better riskbenefit ratio than another), a case-control study, cohort study, or randomised trial may have been better suited to the research question. Comment: Question 3: How were the setting and the subjects selected? Yes Can’t tell No In qualitative research, however, we are not interested in an "on average" view of a patient population. We want to gain an in depth understanding of the experience of particular individuals or groups; we should therefore deliberately seek out individuals or groups who fit the bill. If, for example, we wished to study the experience of non-English speaking British Punjabi women when they gave birth in hospital (with a view to tailoring the interpreting or advocacy service more closely to the needs of this patient group), we would be perfectly justified in going out of our way to find women who had had a range of different birth experiences— an induced delivery, an emergency caesarean section, a delivery by a medical student, a late miscarriage, and so on—rather than a "random" sample of British Punjabi mothers. This is termed purposeful sampling. Comment: Question 4: What was the researcher's perspective, and has this been taken into account? Have the researchers described in detail where they are coming from so that the results can be interpreted accordingly? Yes Can’t tell No Comment: Question 5: What methods did the researcher use for collecting data—and are these described in enough detail? "have I been given enough information about the methods used?", and, if you have, use your common sense to assess, "are these methods a sensible and adequate way of addressing the research question?" Comment: Yes Can’t tell No Question 6: What methods did the researcher use to analyse the data—and what quality control measures were implemented? It is simply not good enough to flick through the text looking for "interesting quotes" which support a particular theory. The researcher must find a systematic way of analysing his or her data, and, in particular, must seek examples of cases which appear to contradict or challenge the theories derived from the majority. (This is termed ‘deviant case analysis’.) Comment: Yes Can’t tell No 81 Question 7: Are the results credible, and if so, are they clinically important? We obviously cannot assess the credibility of qualitative results through the precision and accuracy of measuring devices, nor their significance via confidence intervals and numbers needed to treat. It usually takes little more than plain common sense to determine whether the results are sensible and believable, and whether they matter in practice. Comment: Yes Can’t tell No Question 8: What conclusions were drawn, and are they justified by the results? How well does this analysis explain why people behave in the way they do? How comprehensible would this explanation be to a thoughtful participant in the setting?; How well does the explanation cohere with what we already know? Comment: Yes Can’t tell No Question 9: Are the findings of the study transferable to other clinical settings? One of the commonest criticisms of qualitative research is that the findings of any qualitative study pertain only to the limited setting in which they were obtained. In fact, this is not necessarily any truer of qualitative research than of quantitative research. Yes Can’t tell No Comment: OVERALL, WHAT DO YOU THINK: (weigh up the 9 questions) Doctors have traditionally placed high value on numerical data, which may in reality be misleading, reductionist (=looking at the minutiae rather than the whole picture), and irrelevant to the real issues. The increasing popularity of qualitative research in the biomedical sciences has arisen largely because quantitative methods provided either no answers or the wrong answers to important questions in both clinical care and service delivery.1 If you still feel that qualitative research is necessarily second rate by virtue of being a "soft" science, you should be aware that you are out of step with the evidence. 82 SCREENING – Made Simple! Example Question: Outline whether screening for Prostate Cancer is justified. Having trouble remembering Wilson’s & Junger’s Criteria (1969)? Be troubled no more: Mnemonic C-NET TFT PIC (as in Thyroid Function Tests) (as in picture) The disease itself should be common enough to warrant screening….no point screening for something extremely rare if it is not cost effective. Common disease Natural history of disease known Early window for intervention Test available, sensitive & specific No point in picking up something when it is too late! (refers to the test used in screening) Test – cheap, acceptable and simple test (CAST) Facilities available for diagnosis and treatment Treatment is effective (refers to the test used in screening) No point doing screening if no-one knows where it is to be done or where to send the patient for treatment should that be necessary. Goes without saying! This refers to the psychological and/or physical harm as a result of the screening test. Don’t forget…a lot of current screening tests do cause unnecessary anxiety (especially if they have a high false positive rate!) Psychological/Physical Harm is low Interval for repeat screening agreed Cost Effective Speaks for itself. Other Notes Screening questions are common in the MRCGP examination. Start answering these type of questions with a starting statement; something like: ‘Applying Wilson’s & Junger’s Criteria (1969) for a good screening test will help determine whether screening for disease x is justified. The following is a list of the criteria: CRITERION DOES SCREENING FOR PROSTATE CARCINOMA SATISIFY IT? 1. Common disease autopsy) 2. Natural History Known 3. There is an early window for intervention. Yes. Prostate Carcinoma is common. (Many have prostate Ca on For prostate Carcinoma - No NO Get the idea? Make it easy for yourself. It is also easy for the examiner to mark and (s)he’ll think the sun shines from …….. 83 Critically Appraising Protocols – MADE SIMPLE! Example Question: The following COPD protocol was developed by the nurse at your practice. Suggest areas for improvement. Mnemonic ABCD SR RAF Aims Background / Clinical Evidence Diagnosis Subjects Responsibility Refer (Red Flag Symptoms) Audit Follow Up (as in Senior Registrar) (as in Royal Air Force) Are the aims of the protocol clearly stated? Audit can only be done it aims are stated. Protocols & Guidelines should be based on evidence. Does the protocol provide details on how a diagnosis is to be uniformly reached? Only once a clear diagnosis has been made can a protocol or guideline be followed. Who is the target group. The protocol must clearly define this. Does the protocol state who is responsible for what? There should be someone responsible for Championing it Keeping it up to date Performing an Audit Protocols should tell us when to refer (urgent and nonurgent) Does it specify the red flag symptoms? Does it state when audit is to take place to ensure that our quality of care is improving? Should be clearly stated. Adapted from ‘Critical Reading Questions for the MRCGP’ by Ese Stacey & Yinkori Toun, BIOS Scientific Publishers Limited, 1997 Further Reading. So you want to read some more? Try the following occasional paper produced by the RCGP. Report from General. Practice No. 26, ‘The Development and Implementation of Clinical Guidelines’ 84 A Critical Reading Question Illustrated With reference to the literature, discussed the value of using a prescribing formulary in modern general practice A GOOD ANSWER Definition a preferred list of medication is that a group of GPs have agreed to use within their practice three-quarters of NHS prescribing costs by duty GP prescribing GPs are bombarded with information every day and have potential access to a huge range of medication. Increasing interest in formularies in the last 10 years with debate about whether they do increase the effectiveness of prescribing and over the cost of prescribing Why Have A Formulary? Various formularies available for many years for example British National Formulary main use is as an educational tool formularies should highlight those drugs which prescribers are familiar avoid drug-induced disease secondary benefit may be to cut costs of prescribing Three formularies have been produced for national and regional use in recent years: the Lothian formulary, the Northern Ireland's faculty RCGP formulary and the basic Formulary for general practice (Department of primary care Newcastle, Grant Gregory and Zwanenberg). The latter was produced as part of a study to look at developing a European formulary The formularies should be flexible, provide adequate and appropriate treatment and encourage generic prescribing provides opportunity to liaise with hospital consultants, pharmacists and community pharmacist agree district formularies provides opportunity to audit practices prescribing and can be helped by using PACT data may encourage development of formularies for use by community nursing staff prescribing of dressings and so on Arguments Against All Formularies prevents new ideas being generated, encourages cook-book medicine and rigidity not always possible to convince other partners to add a new drug cost is not always contained by formulary hospital consultants may discharge patients on medication not previously agreed once constructed, formulary must be kept up to date Patients Views Overall no difference in patient satisfaction between a practice using a practice formerly and a control practice (field 1989) Conclusion There is increasing pressure for doctors to prescribe effectively. Audit commission report 1994 cited in MIMS magazine comments about GPs over prescribing in some areas (for example, ulcer healing drugs) and under prescribed in others (for example, asthma). Above all, a practice formulary is a powerful learning tool. References Waine et al how to produce a practice formerly our sea G. P1989 Constructing a practice formulary drugs and therapeutics bulletin 1991 29 (7) Gilleghan prescribing in general practice rcgp occasional paper 54 1991 MIMS magazine 1994 21(8) Field J. how do doctors and patients react to the introduction of a practice formulary? Family practice June 1989: 6 (2): 135 – 40 85 A SATISFACTORY ANSWER A practice formulary uses drugs voluntarily agreed by partners in a practice Argument For A Formulary formulary will have medication agreed by partners use pact level 3 data valuable teaching/learning tool useful to GP trainees joining the practice ensures that treatment is acceptable to patients, safe and effective off-the-peg formularies available are Lothian, Northern Ireland formulary, RCGP potential to discuss with consultants and agree local district formularies Argument Against difficult for partners to agree on drugs to be used in formulary time-consuming May not contain costs, produces rigid thinking. New patients on well tried medication joining the practice will not be keen to change. Influence of fundholding and indicative budget prescribing incentives A POOR ANSWER Arguments For practice formulary to help partners to discuss prescribing helps to keep prescribing costs down uses PACT data although medication is chosen by GPs, more government pressure to contain prescribing Arguments Against time to prepare practice formulary partners resistant to change Notes: I hope the responses to this question illustrates that whilst a satisfactory answer demonstrates the candidate has considered most of the issues, to obtain the most marks, the candidate will have reflected on the literature and adopted a more considered personal view. I also hope that these three responses illustrate the need to have read other text as well as the mainstream journals. 86 87 The Orals 88 ORALS The oral examination assesses: 1. your decision-making skills in general practice and 2. the professional values underpinning them = communication professional values personal and professional growth 89 THE ORALS The ability to make and justify everyday decisions on a rational basis is fundamental to GPs. The orals assess your ability to make decisions and justify the conclusions that you reach, in the face of critical challenges from the examiners. You will be asked to appraise a set situations or clinical problems. These are examined in the following contexts: 1. 2. 3. 4. care of patients working with colleagues the social role of general practice (society) the doctor's personal responsibilities So, the examining crib sheet looks something like this: Context Area of Competence Care of Patients Working With Colleagues Society Personal Responsibility Communication Professional Values – usually involves decision making based on sound ethical principles Personal & Professional Growth Testing of factual knowledge should be entirely the preserve of the written papers, leaving the oral exam to test decision making processes. However, some knowledge may come up such as knowledge of consultation models. The type of knowledge expected of you is that knowledge which forms the basis (or justifies) the way you do things in every day general practice. Can You Tell Me a Bit More About the Contexts? Care of patients = relationship with patients, how care is organised Working with colleagues = working with the PHCT and beyond, relationships and boundaries; team working; the sick colleague Personal Responsibility (for care, decisions and outcomes) = selfmanagement, duties of a doctor Society = society as a whole: its expectations and the GP’s role; legal responsibilities; society’s view of how doctors behave, public debate on medical issues 90 Examples of Questions, areas of competence being tested and in what context AREA OF COMPETENCE CONTEXT Care of Patients Working With Colleagues Society Personal Responsibility Communication Breaking Bad News Favourite Consultation Models and how such a model helps in xxx Principles of verbal and non-verbal communication (generally) What do you understand by the term “a doctorcentred consultation”? Patients with communication disabilities Communication between different members of the practice team How do you decide who is to chair your PHCT meeting Effective information transfer Violence in practice Information flows inside and outside the practice Internet GPs and the media – eg how would you decide whether to take part in a radio phone-in? Awareness and strategies for improving your own communication skills. Empathy Listening Use of video recordings Professional Values – usually involves decision making based on sound ethical principles moral and ethical principles Confidentiality Dealing with terminally ill patients about their illness e.g. relative who wants you not to tell the patient Patient autonomy implications of styles of practice PCTs Sick colleagues roles of health professionals working as a member of a team dealing with conflicting interests Core Values GP’s role in rationing cultural and societal influences moral issues Medico-legal issues Flexibility and tolerance Duties of a Doctor (GMC) What ethical principles guide your decision making? Personal & Professional Growth What effect does the rising number of nonprincipals have on patient care? How does employing locums affect patient care? Leadership Change Management Team Building Needs assessment Assessment against external standards, re-accreditation Keeping up to date Identifying your learning needs Recognising/Preven ting Burnout Appraisal Evaluation CPD Managing resources CME Regular review of own and practice’s educational needs and performance Awareness of potential for and signs of stress/burnout in self and colleagues Assessment against internal standards e.g. practice audits 91 What Happens on the Day? Approximately 15 minutes before the examination begins you will be briefed on the procedure by an examiner or marshal, and you have the opportunity to ask questions at this time. There are two consecutive oral examinations, each lasting twenty minutes and conducted by two examiners. There will be a break of approximately five minutes between the two orals while the examiners mark your performance. During this time you will be asked to wait outside the examination room until called in to the second oral, which is conducted by a different pair of examiners. Candidates should not be examined by examiners who have significant personal or professional knowledge of them. Candidates who know an oral examiner to such an extent should declare this fact on entering the examination room (when an alternative examiner will be provided). Although the questions will obviously be different, there is no planned difference in emphasis between the two orals. The orals will not make significant reference to your own practice or patients, and there is no need for you to bring any aides-memoirs with you. The examiners will cover approximately five-six questions in each twenty-minute oral (total number of questions asked = 10-12). THIS MEANS THAT THERE WILL BE ON AVERAGE 4 minutes PER TOPIC. So during the course of the 2 x 20 minute oral examinations, the candidate can expect to be asked a question from at least 10 of the 12 different boxes on the marking crib. Therefore, you should not be surprised if the pace of examining seems brisk, nor be alarmed if the examiners move abruptly on to the next question. You might have heard of examiners “going deep”. Understanding what this means is best illustrated with an example: Examiner asks “how do you identify a doctor who is burning out” You think “Great, I know everything about this” and then you start to convey your response. After a third of a way through your response, the examiner interrupts and asks “So, what would you do if a partner who seems to be burning out fails to get help?” You think “But I haven’t finished my previous response, and I want to show them how well I know all that stuff”. It is at this point, the examiner is going deep. It is obvious in that first 30 seconds that you know quite a bit and by allowing you to continue would not add to the grade (s)he is planning to give you and would waste time by preventing the exploration of other areas by pushing you harder. So going deep allows the examiners to assess the depth of your knowledge, skills and attitudes. In the situation where you don’t know much about a topic, the examiners will stay there until they can be sure in their minds the extent of your ability. By the way, if you are a bit slow with getting your responses out, the examiners will try and make it easy for you. They may even gently ask you to speed up. They cannot grade what has not been said. Be reassured that the examiners will try to help you show your best, although (as in any face-to-face examination) it may sometimes feel uncomfortable to be 'stretched' towards the limit of your ability. You should feel “stretched” at the end of any topic because the examiners intend to test the limit of your understanding of that topic. 92 Tell me a bit more about the questions Each examiner will ask a question in turn. The topics are all rooted in the examiner’s experience of general practice and each topic can be examined in a number of ways e.g. communication in terminal illness might be a question about breaking bad news (context: care of the patient) or how you communicate issues relating to a dying patient to other members of the PCHT (context: working with colleagues). The second pair of examiners are not informed of the marks awarded by the first pair. They only know what areas that have been tested. When both sets of orals are over, that is when they group together to discuss and formulate a final mark. Within each question the examiner will include some difficult aspect to try and identify the distinction candidate, and so you may at times reach a point in a question where you feel stuck; this doesn't necessary mean that you are doing badly - the examiner may in fact be asking hard questions to find out whether the candidate concerned is in the top group. You will not be offered “props” like letters, pictures or ECG tracings. So don’t worry. The examiners will not use value judgement words like “good”, “excellent”. If this was allowed to happen, you might get the situation where the examiner might actually be trying to encourage a poor candidate by saying “good” but the candidate might interpret that as an indication of a good grade. Instead, examiners will use nonverbal encouragement but will give no verbal indication of how well you are doing. That is one reason why people often walk out of the orals not knowing whether they have passed or failed. Although you are all examined in one big hall, the tables are screened off which helps minimise noise. When the bell goes, the examiners will usually allow you to finish your sentence. Sometimes examiners can seem quite abrupt in stopping candidates at the bell. Don’t be put off by this. Merit?: Around 1 in 4 gets a merit; so it’s not that difficult to achieve. If you feel like you’ve been really stretched and almost slaughtered in the exam, you’ve probably got a merit or you have failed. How to fail the Orals Sit back and put your feet on the table. You need to get one up on the examiners. Argue with them just to make a point rather than saying what you really feel. Pay no consideration to the effect of your decisions on anyone but yourself. After all, it is YOUR decision and therefore YOUR call. The only safe place in an oral is on the fence. See all six sides of every issue. If absolutely pressed for your opinion, offer three for the examiner to choose from. Don't tell them what you really think. You’re only a candidate - the examiners aren't really interested in what you'd do in a given dilemma. Tell them what your trainer would do. Or what you reckon the college line is. Or (best of all) just lie. After all, oral questions are only hypotheticals, aren't they, and we all like a good story. Remember, the examiners are the enemy – argue with them, ignore any advice they offer – it’s a trip up trick question, try and get one over on them, conflict with everything they say and if all that doesn’t work, spit on them. If in doubt, say nowt. A long silence will give the impression that you're Jean Paul Sartre, or Solomon. Name drop shamelessly. Tell the examiners what Neighbour recommends, or Balint describes, or Palmer states, or Pendleton advocates, or Confucius says. The examiners may have had a drink in the bar with all of them, but won't actually have read a single word they wrote. If in doubt, make it up. The examiners have selective anosmia, and can't tell bullshit from reality. And finally if you feel the question is going badly, get emotional - it works every time... Adapted from: R Neighbour, “How to Fail the MRCGP”, The Practitioner, May 2002 vol 246 93 Preparing for the Orals Its all about practise: make trainer/peers/friends/partners. use of those around you - Try to form a study group. You’ll probably only need around 4-6 practice sessions in the month prior the exam. Devise questions to ask each other. Ask for feedback on your performance. Constantly reflect on the ethical and professional aspects of your everyday decision making in general practice. Discuss this with other members of your GP team (not just your trainer). Consider a more in depth tutorial for the more difficult areas. Brainstorm the implications of such issues with your trainer or other candidates. Think critically about any ethical dilemmas or clinical problems that you encounter in everyday general practice. The word “Why” will be asked loads. In everyday practise, try and ask yourself why you make decisions the way you do. You might even wish to look up and see if there are any papers that support your view. When you generate a question from everyday GP real-life issues try to pigeonhole that question into one of the 12 competence boxes as illustrated above. Formulate a database of questions in each of the twelve boxes. Once you have identified some questions, try and apply ethical frameworks and consultation models to the appropriate ones e.g. how do you use Neighbour’s model to break bad news, what ethical principles guide you in…… Things to read: 1. RCGP information sheets – they contain some good stuff on general practice in the UK. 2. GP magazines for recent “GP news” and politically based issues. You are likely to be asked about developments in this area. Pay particular attention to articles 2-3 months before the exam. 3. GMC publications which have a professional, ethical or medico-legal slant. Colleagues who have recently passed their orals are an excellent resource for mock exams, as they often remember difficult questions; make use of them. Don't get hung up about clinical details; this has been covered in the other parts of the exam. They are more interested in you as a person and as a professional. They want to try and get inside you to get a feel for your attitudes and values. Therefore, don't try to be something you are not; show your true colours. Although this exam is not about facts and figures (that is the place of the MCQ), you should still keep up to date with the literature. Examiners are impressed when candidates can provide literature evidence to back up their decision making process. Also try to keep up to date with current affairs through television, news, radio and newspapers. Try not to treat it as an exam – cramming is inappropriate, preparation definitely helps 94 Hot Tips for the Orals Although the structure of the oral examination is based on an objective nature, it is human nature that first impressions still count. So, try and look smart and pay particular attention how you come across over the first few minutes. Get feedback on the initial impressions you impart from your study group mock oral sessions. Stay calm and speak clearly. If you don't understand a question, ask them to repeat, rephrase or clarify it. Don’t be put off by the examiners constantly interrupting you. Remember, they are trying to assess the limits of your knowledge in the given topic and have little time to do it in. Hence, the pace of the oral being pretty brisk with constant interruptions. Don't be put off by really hard questions. The possibilities are that you are either doing really badly or (more likely) you are doing well and they are going "deep" very quickly in order to locate the limits of your abilities. The examiners are looking for safe doctors, capable of thinking clearly and making rational decisions with ethical dilemmas being at the fore. In a sense the decision you make isn't so much what the examiners are interested in but, how you arrived at them. Expect to be asked to justify almost everything you say. Like the consultation, there are three basic rules that you should observe: avoid any unnecessary confrontation, think before you say anything, and be honest. Be honest about what you would to if faced with a particular situation. For instance, if you feel you would have asked for expert advice, say so. Most questions will start with an open question and you should respond with a structured answer in a broad framework. As the oral proceeds, the examiners will hone into the area they want to focus on and ask more specific questions requiring a more specific justified response (“yes, but what would you actually do?”) When a question is posed, don't rush in. Take a few seconds to collect your thoughts. You may wish to use a few "fill in statements" while you gather such thoughts e.g. "that's an interesting question because..." Try and think what the purpose of the question is before you answer it. There must be some underlying point (often, the examiner will clearly state this before (s)he asks the question). One candidate wrote: “I forgot this [bit of advice] when I was asked about my personality. As I babbled on about my good nature and great sense of humour I remember wondering how they could mark this. Only when it was too late did I realise they wanted to discuss the dynamics of group practice and interpersonal skills!” (Dr. Anthony O’Brien, Pulse Registrar, May 13 2000) A straightforward response, such as “ in this situation, I would without hesitation do this”, may seem decisive, but it may also be viewed as rigid or dogmatic. It is the reasoning process that is being examined more than the ultimate decision. You will gain more credit from approaching the questions by analysing options and look advantages and disadvantages of any possible solution before reaching a final conclusion. If asked: “what you would do?”, try and start off by giving them a list of options. Then tell them exactly which one you would go for. Try not to sit on the fence! Don't be surprised if they cut you short of your list and ask you to cut to the chase. 95 The most common question format is: What options are open to you now? What are the implications of each? What would you decide on and why? Frameworks and lists are helpful to a point: One of the most useful ones is: The ethical framework (Gillon): autonomy; beneficience; non-malevolence and justice Use key phrases or words like clinical governance, revalidation, audit, personal development plans: this shows the examiners you are well read. Cite evidence where appropriate and only if you can remember it. However, don't get too hung up about it. The minimum you should try and do is to justify your responses e.g. "I would do blah blah blah, because ________" Don’t be afraid to change your mind early on in an answer if you feel you’re digging a hole. At the same time, if you are comfortable with your decision and feel you have demonstrated proper consideration, stick to your guns; this is the real test! Remember to be yourself. If you are presented a dilemma which you have not previously encountered or considered, consider how you might approach it in real life. Many questions posed in the orals don’t have a right or wrong answer, but require you to justify whatever course of action you would take. Specific Types of Questions: 1. In decision making skills, the examiners will be looking for evidence that your approach is coherent, rational, ethical and sensitive. 2. With regard to professional values, the examiners will see whether you include a respect for the evidence base of practice, effectiveness, an ethical framework, respect for patient autonomy, equity, caritas, selfawareness, and commitment to high and sustained standards of practice. 3. If they ask you “what else you could do?”, basically they are asking you for more options. 4. If they ask you “what are you going to do?”, please state what you would exactly do in that situation. 5. Someone will always get a question on consultation models. Know something about different consultation models but become particularly familiar with one that you use in practice. The examiner will probably get you to apply the consultation model to a particular situation such as breaking bad news. 6. Read up and be familiar with the key points on the “Management of Change”; a tutorial with your trainer perhaps? 7. Examiners also have personal favourites for books. Think of some books you have particularly found helpful and try and figure out SPECIFICALLY how they have helped you in everyday GP life. The same applies to journals and other media like the ever expanding electronic databases. 8. Always start off broad but be agile enough to sit on the fence and only jump off at the end of an answer. If you don’t jump off, the examiner will eventually ask you (“Yes, but what would YOU actually do?”). 9. You should try and be tolerant, show respect for others and their views, and be self aware of your own limitations. Before your second oral, you will have a break. Use that time to relax. Try and put off the first orals experience behind you. Try not to look up or engage in last minute revision; that will just push up your anxiety levels. 96 Attributes of Candidates who fail. 10% usually fail this exam because of being: Unimaginative, Dogmatic, Authoritarian, Unstable, Obsessive, Doctor-Centred Let’s put you at ease… I get all nervous when people are going to grill me. The examiners will greet you and start of with an initial comment about the weather for instance to put you at ease. They will conduct the oral with friendliness, decorum and informality. They will also be mindful of equal opportunity considerations. They will examine candidates from other cultures sensitively. Remember, they are here to try and pass you NOT to trip you up. Quasi-role play (i.e. “Show me how you might tell her the bad news, pretend I’m the patient”) will be avoided for all candidates. I’m worried that I might not be familiar with some of the professional terms they use. Examiners will introduce each topic AND they will indicate which area they are testing in PLAIN English. If you don’t understand something, ask them to repeat it. Listen to this introductory phase carefully as it indicates what they are testing and to some extent how you should be constructing your response. Example: “I want to ask you something about how we explain things to patients. Let’s take diabetes as an example”; from this you should realise that the question that is going to be asked is testing: Area of competence : COMMUNICATION Context: CARE OF PATIENTS I heard that sometimes there is an observer. What for? You may find there is an observer seated at the side of the table during one or both of your orals. Most observers are current or potential members of the Panel of Examiners who are observing their colleagues in order to help maintain the quality of the examination. Other observers may occasionally attend the orals at the invitation of the Convenor if they have a legitimate academic or professional interest in the examination. Observers are there primarily to observe the examiners rather than the candidate, and they will not contribute to, or influence, the conduct and results of the oral. In fact, if you get an observer in your orals, consider yourself lucky - it is more likely examiners will behave themselves (not that I am suggesting that they don't do otherwise). Some of the Orals are video taped. Why is this? As part of ongoing quality control and training for examiners, the college video-record randomly selected candidates’ oral examinations (about 7% of all candidates). Candidates are not in view on the tapes and only their voices are heard, so it is not possible to identify individuals without access to the paperwork which is held confidentially in the Examination Department. The tapes are viewed only by examiners and consultants to the panel of examiners, who are committed to respecting candidates’ anonymity. Recordings of this kind do not contribute in any way to the assessment of a candidate’s performance. With these safeguards in place we would hope that candidates would normally agree to their examination being video-recorded. If you do have a religious, cultural or personal reason for not being video-recorded please attach a letter of explanation to your application, and the college will respect your wishes. In the absence of such a letter your consent to be video-recorded will be assumed. I’m generally good are Orals. I’m quite good at taking the examiner to areas that I am familiar with. You’re in for a bit of a surprise! Examiners will have identified exactly where they want to go with their questions. You will find it difficult to pull them away from their tracks and onto yours. Unlike consulting, in which we are encouraged to be patient led, the oral examination is very much examiner led. It is important to remember that marks will only be scored for answering the examiners question; the verbose candidate who avoids addressing issues raised and attempts to take control will not score well. Be warned. 97 WORKED EXAMPLE: Orals EXAMPLE 1 What would you do in the situation of an unreasonable out of hours call from a mother requesting a visit for her five year old son who has a sore throat? Wrong answer: “this is the college examination and I must give the gold answer that I would visit without hesitation in case he had meningitis” Correct response: would look at the available options and weigh up the pros and cons of each before justifying the decision. So for example in this visit Why is she asking for the visit? What are your local on call arrangements? How well do you know her? How experienced are you as a GP? Any advice from anyone else? Etcetera EXAMPLE 2 Putting it all into context (Adapted from Pulse 2000 Melanie Wynne-Jones) “Your partner breath tested positive in hospital following an RTA while on-call. What issues does this raise?” You should start off broadly and think as laterally as possible. Try and form a structural framework on which you can hang things: E.g. “Well, this would have issues for patients, me, other colleagues and society in general. For instance, for patients one would have to check that the partner was providing safe care and correcting any lapses found. It might result in the doctor having to take sick leave and one would have to explain that to patients in a suitable way. The partner’s case load would have to be managed and maintaining the practice services in the partner’s absence (which could be prolonged or indefinite) could prove a difficult task. Then there are issues for me….” Because the question is initially posed in a broad manner, you could go on and on for ever! Expect the examiner to interrupt you. They’ll want you to start off like this so that they get a feel for your thinking processes and ability to think laterally. The examiners need to test your performance in several areas and that is why they cannot allow you to simply “roll on”. When they interrupt you, they will do so either to a) b) c) d) seek clarification of what you have said seek an example of what you have just said alter the scenario/provide more information to push you OR navigate you to a particular area they want you to talk about. So, in this example, they could navigate you to any one (or more) of the following 12 areas: (see next page) 98 Communication Professional Values Care of Patients Explaining Dr X will be on sick leave Practical follow-up Arrangements for Dr X’s caseload Maintaining practice services in Dr X’s indefinite and possibly prolonged absence Personal Responsibility Awareness of, and willingness to discuss, signs of stress or distress in self, colleagues and staff Working with colleagues Will Dr extra return to work and when? What to say to staff, other team members about Dr X. Relationship when Dr X returns Strategy for maintaining services Liaising with PCG/ Health Authority LMC Confidential advice Dr X’s reputation The practice’s reputation Handling the media Checking Dr X has been providing safe care to his patients Correcting lapses in care Conflict between duty to patient and support for colleague Informing individual patients of any problems uncovered and reassurance that they will be resolved Implications of “shopping” a sick colleague Awareness of own health and stress levels; duty to act Practice policy for monitoring use of controlled and other drugs Who is Dr X’s GP? Issues relating to being a patient in one’s own practice Dr X is right to confidentiality as a patient Attitudes to sick doctors Partnership agreement Continuation of partnership Society Drink and driving Whistle blowing GMC - Duties of a Dr Sick doctors schemes/help lines Medical defence societies Legal redress for patients Personal and Professional Growth Review practice care and record keeping- are they robust enough to identify and correct a similar problem in the future? Review practice behaviour – can changes be made which support staff and doctors without compromising patient care? Stress management strategies Mentoring Sabbaticals Teambuilding and adequate training to prevent stress Health and safety policies – workloads, support structures etc Managing change – effects on those involved Selection and training of doctors Occupational health service for GPs Dope testing for GPs Redefining the GP job description to reduce stress It could be argued that in real life, any of the three competencies might be needed in any one of the four contexts. However the way the question is phrase should indicate the main area under scrutiny. 99 Practise Oral Questions SAMPLE QUESTIONS illustrating which domains might be under test How can we ensure that patient’s abnormal results are acted upon? Communication/Care of patients You suspect your 13-year-old patient has been sexually abused. How might you proceed? Professional values/Personal responsibility The NHS net will give GPs access to huge amounts of information; how can we avoid being overwhelmed? Personal and professional growth/Care of patients What would you do if you suspected your partner was suffering from burnout? Professional Values/Working with colleagues How would you respond to being given an expensive present by a patient's husband? Professional Values/Personal Responsibility What would you do if a patient asked you to exclude her pregnancy termination history from her insurance report? Where do your loyalties lie? Personal responsibility/Professional Values/Communication How would you respond to a patient bringing a printout from a website about alternative treatments for his lymphoma? Communication/Care of Patients 100 SAMPLE QUESTIONS and supplementary follow up questions A patient offers you a gift of £10 to thank you for caring for them during a recent illness. How would you respond? What are the potential problems that may arise? If you decline their gift because you feel uncomfortable with the way in which it may affect the doctor-patient relationship, what might happen? If you refused based on monetary terms would you accept chocolates instead? Notes: the wider issues – partners, practice, ethics, future consultations What do you understand by the term ‘principle of double effect’ when it comes to morphine administration in palliative care How would you explain this to a dying patient’s relatives? What implications does administering diamorphine carry for you as a doctor? Consequently, the family refuse to allow any medical practitioner or nurse to administer diamorphine to their distressed and dying father who is now incompetent of making any decision about his own care. How would you deal with this? How is this different form euthanasia? Notes: Double Effect: This is where a lethal dose of morphine may be inadvertently administered through attempts to alleviate patient’s agitation/pain in palliative care. How do you learn day to day in practice? Why is a PDP useful? What would you put in your PDP? There is a complaint following a significant event at your practice. You are the subject of this complaint. Would you put this information in your PDP? Why? What are the possible benefits and problems with adding this to your PDP? Would you add minor event to the PDP? If not, how is this different to adding a significant event? Investigation of significant event – what would you do? You are delegated by your partners to talk to a member of staff who is the subject of a patient complaint. How would you go about this? Who would you involve? One to one? Is this potentially threatening? Notes: Think about what options you have?; Practice meeting first?, One to one with representative/witness?; How formal does this need to be?; Are you planning on issuing a written warning? Another doctor at your practice asks you for an antibiotic prescription in a practice meeting. What would you do? If you refuse/agree – why? You refuse and he/she says there is no time – going on holiday tomorrow and he is not registered with a practice- what now? Notes: Professional values/ GMC guidelines to Good Medical Practice; Care of patient primary concern; Encourage to see own GP?; Concern for colleague- fitness to practice?; Do you need to discuss this outside of the meeting?; Why ask you? 101 A 55 yr old smoker has come to you after the surgeon to whom you referred him with peripheral vascular disease has refused to operate. What would you do? The surgeon has written to you stating that recent evidence points to increased morbidity/mortality and failure rate in smokers. He has a budget and must ration his treatments. What next? You refer for a second opinion. Do you include the reasons for the first surgeon’s refusal to operate in your letter? Is the surgeon making a judgement call? Notes: Acknowledge rationing is well established within current political /economical climate. Is this Explicit or Implicit rationing. What’s the difference?, Encourage smoking cessation - motivate/handover to patient; If you are going to refer for second opinion; ask the patient whether he agrees with your letter and whether he wishes you to put in reason for seeking second opinion. What do you understand by the term ‘difficult patient?’ How would you deal with a patient demanding a particular treatment? How would you deal with this now and in the future? Notes: Training issues for you, practice, partners; Safety issues; training and support issues What are the advantages to having a young principles group? What use is a mentor? A patient comes to see you because they are dissatisfied with the care their elderly father received in hospital. How do you deal with this? How would you run the consultation? Notes: Consider different consultation models and their applicability. Allow the patient to ventilate; Empathise and acknowledge their concerns; Do not make unsubstantiated or derogatory comments about clinicians – never helpful! It comes to your attention that one of your CHD patients has been admitted to hospital with an MI and was seen last week in the CHD clinic. What issues does this raise? Is it a significant event? What would you do? Notes: No blame culture; Investigate: look at records, talk to staff recently involved in his care; If a systems error; how would you stop this happening again in the future? A patient invites you to become a member of a local pressure group set up to oppose the building of a new waste disposal site in your catchment area. What is your response? He tells you they are planning to build the site 400 yds from your home, does this alter your standpoint in anyway? You are invited to an interview with the local paper on this issue. What do you do? Notes: Ethics: think in terms of the four main pillars - justice, autonomy, beneficence and non-munificence and use Deantological (selfish/rights based reasons) and Utalitarian (for the greater good) approaches. Last part of the question: Identify the aims and objectives of the interview: who are you interviewing for? What do you expect to gain? Find out your partners feelings before agreeing to anything? 102 Popular Domains tested in the Orals Try and go through some of these in your study groups and/or with your trainer/other colleagues. A sample of some popular domains tested in the orals include: Abortion Breaking Bad News Burnout - prevention, coping with own anger, stress and fatigue Complaints procedure Consent - age to consent for treatment (children), justification of sectioning, treatment without consent Confidentiality Consultation models, consultation structure and length, the consultation process (verbal/non verbal cues) Counselling in General Practice Difficult Patients & Dysfunctional Consultations The Doctor-Patient relationship Educational needs Euthanasia/Life Prolonging Rx/Advanced Directives Genetical Manipulation – ethics Gifts – accept or not? The Pharmaceutical industry Prenatal Screening Personal & Professional Development: self awareness: insight, reflective learning, ‘the doctor as a person’; Commitment to maintaining standards: personal and professional growth, continuing medical education Rationing Referral rates Self Inflicted Illnesses (e.g. smoking, alcohol, drugs) – views on treatment Sick Doctors/ Addicted Doctors/Alcohol Teamwork/Belbin theory Terminal Care (Death & Dying) The Underperforming Dr Transcultural Medicine, Ethnicity & Diversity Whistle blowing Hot topics change with time. Remember to read the medical news to see what the latest flavour is. Some topics will always remain important e.g. rationing. MRCGP Examination: ORAL 1 …………………………………... Date/Start Time …………………………………... Candidate Name 103 Examiner’s Marking Sheet 2 Changes? Y or N Which Oral ………………….. Examination Number …………………………………….. Examiner 2 …………………………………….. Co Examiner 1 …………………………………….. Co Examiner 2 working w. colleagues society pers. responsibilit y GRADE (circle) care of patients CONTEXT Pers/Prof growth AREA OF COMPETENCE prof values WHOSE Q? (circle) communication TOPIC AND NOTES (consider using the “classified comments on candidates” crib sheet where appropriate) …………………………………….. Examiner 1 1.__________________________________ Own CoEx ○ ○ ○ □ □ □ □ O E G S B N U P D 2. _________________________________ Own CoEx ○ ○ ○ □ □ □ □ O E G S B N U P D 3. _________________________________ Own CoEx ○ ○ ○ □ □ □ □ O E G S B N U P D 4. _________________________________ Own CoEx ○ ○ ○ □ □ □ □ O E G S B N U P D 5. _________________________________ Own CoEx ○ ○ ○ □ □ □ □ O E G S B N U P D 6. _________________________________ Own CoEx ○ ○ ○ □ □ □ □ O E G S B N U P D 7. _________________________________ Own CoEx ○ ○ ○ □ □ □ □ O E G S B N U P D CONSTRUCTIVE COMMENTS OVERALL GRADE (circle) O S U E B P G N D 104 MRCGP Orals: Grade Descriptors (revised 05.00) O Outstanding Very well informed, coherent, rational, consistent, critical. Stretches the examiner. Supports arguments by reference to the evidence, both published and topical. Can reconcile conflicting views and data. Very robust justification of proposed actions. Impressive exploration of ethical issues. E Excellent Impressive but not superlative candidate. Rational, consistent. Impressive range of options/implications. Well informed, uses rigorous and well-substantiated arguments, and justifies decisions. Relevant ethical issues explored in depth. G Good Definitely passing but not especially impressive candidate. Generally rational and consistent. Good options/implications. Sound evidence base, makes acceptable rather than robust or rigorous arguments, generally justifying decisions. Important ethical issues recognised and explored. S Satisfactory Examiner is only just comfortable with candidate's adequacy at MRCGP level, but he/she is solid. Main options and implications seen and understood, but no sophistication of approach. Decision making informed by some evidence. Some ethical issues recognised. B Borderline Examiner not comfortable with candidate's adequacy for Membership. Not enough justification of decisions. Decision making skills are, on balance, not quite acceptable. Superficial appreciation of ethical aspects. N Not adequate Cannot discuss topic in a depth appropriate for a Member of the College. Examiner not satisfied with candidate 's decision-making skills. Limited range of options seen. Very limited use of evidence. Unable to apply ethical principles. U Unsatisfactory Cannot discuss topic in a depth appropriate for a doctor entering general practice. Poor decisionmaking skills. Almost no evidence for approaches. Options rarely seen. I s unaware of ethical dimension. P Poor Cannot discuss topic in a depth appropriate for a medically-qualified person. Inconsistent. Unable to see range of options. No evidence of rational decision-making or ethical considerations. D Dreadful Candidate worse than poor, adopts such arbitrary approaches as to affect patient care adversely. 105 More on How To Fail The Orals (with "translated" feedback as transmitted to candidates) 1. Disorganised / inconsistent There was some evidence of inconsistency and a disorganised approach to problem solving and decision making. 2. Slow / ponderous candidate / had to be led The candidate needed to be led and demonstrated a slow and slightly ponderous approach. 3. Garrulous and verbose The candidate was somewhat garrulous and needed to be guided and interrupted in order to be allowed the opportunity to score marks. 4. Superficial and shallow / lack of justification There appeared to be a shallow and superficial appreciation of some of the questions and there was a lack of justification for decisions that were made. 5. Difficulty understanding candidate The examiners found it very difficult to understand the points that the candidate was trying to convey. 6. Difficulty recognising dilemma There appeared to be some difficulty in recognising dilemmas that the candidate was confronted with. 7. Failure to see a range of options The candidate found it difficult to contemplate the range of options that needed to be considered in order to justify a rational approach to decision making. 8. Inability to apply knowledge The candidate was hesitant in applying knowledge to a given situation. 9. Rigid and inflexible The candidate appeared to take a somewhat rigid and inflexible approach to some of the dilemmas with which he/she was confronted. 10. Unable to apply an ethical framework There was not much evidence of being able to apply ethical frameworks to assist in decision making. 11. Lack of self-awareness There appeared to be little or no evidence of self-awareness. 12. No evidence of patient-centredness There was little or no evidence of a patient centred approach to problem solving and/or decision-making. 13. Unable to take personal responsibility There appeared to be an unwillingness to take personal responsibility for decision making. 14. No evidence of empathy & caring There was insufficient evidence of empathy & caring demonstrated. 15. No evidence of decision-making skills The candidate appeared to have difficulty in making decisions. 16. Lack of evidence to support decision-making There appeared to be a lack of evidence supporting decisions that were made. The candidate found it difficult to contemplate the range of options that needed to be considered in order to justify a rational approach to decision making. The candidate was hesitant in applying knowledge to a given situation. The candidate appeared to take a somewhat rigid and inflexible approach to some of the dilemmas with which he/she was confronted. There was not much evidence of being able to apply ethical frameworks to assist in decision making. There appeared to be little or no evidence of self-awareness. There was little or no evidence of a patient centred approach to problem solving and/or decision-making. There appeared to be an unwillingness to take personal responsibility for decision making. 17. Failed to see issue at all The candidate failed to appreciate the issues he/she was confronted with. 106 RESOURCES WORTH EXPLORING www.rcgp.org.uk – look at the latest regulations and advice on the orals component of the MRCGP exam. Familiarise yourself! An Insider’s Guide to the MRCGP Orals, Amar Rughani – a super buy. Video plus book with hints, tips and actual questions. RCGP Information Sheets – these can be obtained from the college and give an excellent base to your general knowledge of British General Practice. Available online at www.rcgp.org.uk (click publications & BJGP > information publications) GPC publishes advice leaflets on a number of administrative topics and also an annual report that gives an easily digested overview of current issues on the political front. GMC – and other defence unions publish reports that keep you up to date with issues of a professional, ethical and medico-legal importance. Toby J and Wakeford R. A study of desirable attributes. Exam for membership of the RCGP, 1990. Development, current state and future trends. Occaisonal paper 46. London: RCGP 1990. 10+ years since publication, but still contains loads of stuff relevant to the current MRCGP oral examination. 107 The Video (Consulting Skills) 108 VIDEO This assessment is based on the concept of competency, meaning that combination of knowledge, skills and attitudes which when applied to a particular situation leads to a given outcome. Thus, to use the analogy of the driving test, the competency "three point turn" requires the candidate to turn the car to face the opposite direction, using forward and reverse gears, safely, without endangering other road users, nor striking the kerbs or other obstacles. The number of forward/reverse iterations is not specified, nor is there a time limit, but the examiner would expect the manoeuvre to be carried out with a certain smoothness. Clearly many skills are involved (clutch control, road awareness, steering, etc.), but the competency includes them all, but has a specific, recognisable outcome, viz. the car pointing the other way. Similarly, consulting skill competences have been specified that, for example, require the candidate to demonstrate the ability to discover the reasons for a patient’s attendance, by eliciting their symptoms, which includes two competences: encouraging the patient to "spill the beans", and not ignoring cues. The college do not specify how the patient is encouraged to give their account of their symptoms: this may be by open questions, by appropriate use of silence, or some other way. Nor does the college need to specify how the cues are responded to. They do expect that at least some bits of unsolicited information are picked up by the doctor. Thus a competence is a complex skill, the possession of which is demonstrated by achieving the relevant performance criterion. Possession of the competence does not imply that the doctor uses it all the time. However, unless the candidate demonstrates the competence in action, the examiners cannot assume they possess it. “analysing my consultations was one of the best things I did in my registrar year and I know that it helped me improve my skills” Dr. Anthony O’Brien (Bath) This is statistically the hardest part of the exam. More people fail on the video than any other section. Whilst most people have had some experience of MCQs, written papers and oral examinations in the past, most will never have had to produce a video as part of an examination. But this is the only part of the exam where you are given the answer sheet up front! The marking crib is basically whether you scored on the performance criteria or not (which can be found in the workbook). 40% still fail this section despite having the criteria in advance and (in reality) having unlimited time to produce your perfect selection. The video module is an unusual exam; the candidate has total control of the content on which they will be judged. 109 THE VIDEO (CONSULTING SKILLS) Most candidates find this the trickiest bit. It takes a lot of time to prepare and finalise. “the camera never lies” How to fail the Video Component Only submit easy consultations Why risk ruining up on anything complicated? If the examiners can't spot the elegance, compassion and patient-centredness with which you sign a repeat certificate for fractured femur, that's their problem. Don't read the video workbook until after you have selected your consultation. It will only confuse you. Make sure your trainer hasn't read it either. It'll only confuse both of you. Superficial empathy is all you need To show that you can share management options, say “okay” every 15 seconds. To demonstrate responding to cues, offer the patient a tissue every two minutes. As evidence of your understanding of the patient social context, ask “what did you say your job was?” as the door closes behind them. Spend at least 80 hours editing your tape The better a doctor is at consulting the harder it is to show it on tape. R Neighbour, “How to Fail the MRCGP”, The Practitioner, May 2002 vol 246 Preparing for the Video Component Read the booklet of regulations from beginning to end before you start: learn the list of past criteria and make sure you can demonstrate them obtain a full copy the RCGP consent form in the video workbook Get the consent form signed at the beginning and end of your video consultations BUT make sure that none of the consent process is visible are on your consultations. Remember only the first 15 minutes of each consultation will be viewed the video timing strip must be visible for summative assessment but is not a requirement for the MRCGP. Make sure you have it turned on if you're planning to go down the single route. All sensitive examinations must be done with the lens cap on and the tape still running so that you can hear the dialogue between you and the patient. If you’re in a practice which has separate rooms for consulting and examining, you will need to find a surgery set up more suitable. Sorry, there is no other way around this. There are no concessions for non English speakers and the use of interpreters “Passing the video component of the MRCGP exam gave me more headaches than all of the other sections put together. On days when the patients behaved and my clinical skills rivalled the most eminent professors in the land, either the battery would run out with the tape would come to an end as the consultation reached its climax. And when my apparatus was perfectly adjusted and ready to roll, I would either have a surgery full of coughs, colds and whingers, or a child that trashed the whole setup” (Dr. Simon Atkins, Bristol). Sounds familiar? To avoid this, you need to start videoing early so that you become familiar with the equipment and the MRCGP marking crib sheet. Okay, the first few consultations aren't 110 going to be up to MRCGP standard but by reviewing these with your trainer you will get there. Set aside specific sessions for video; discuss this with your trainer and practice manager. Make sure the appointments are slightly longer to allow for time getting patient consent and fiddling with the camera (full time GPR will need around 2 sessions per week) Before each video session make sure you've got a blank tape and a fully charged battery. Don't forget to review the final camera shot to ensure that it includes both you and the patient. Practise, practise and practise. The more you do, the less you’ll notice the camera running – trust me. During the initial stages, you might want to tape a summary of the performance criteria on your desk or wall to help you become familiar with them. Review the list after each consultation and see what you think you covered, what you didn’t but could have done and what you didn’t because the opportunity simply wasn’t there or it was inappropriate. Providing you understand exactly what each performance criteria means, there is no reason why you should not be able to assess your own consultations. Try and put ticks in the boxes where you think you have fulfilled the criteria. You will soon realise which criteria you usually achieve and which you forget every time. This will help you focus on future consultations. You may even want to leave notes on the desk to remind you of these weak areas such as “ explore psychosocial issues” or “involve patient in management plan” Choose challenging consultations. This assessment is about you demonstrating your competence, and not about avoiding mistakes. A succession of sore throats may appear 'safe' because you are unlikely to do anything wrong, but you are also unlikely to have the opportunity to demonstrate many of the required competences. The editing process is incredibly laborious and time-consuming. Do this well in advance of the deadline for submissions so that if you need to make any revisions you've got plenty of time to do it. Don't forget about the log book. This takes time too. When writing it up, try and demonstrate that you were aware of what was going on in each consultation. Jot down something about the patients agenda, put some background information on each patient to put the consultation into context and don’t forget to write down something about followup. Hot Tips for the Video Rather than stopping and starting the video with every consultation, I recommend you let the camera roll, unless of course the patient does not want to have the consultation recorded. Letting it roll is less distracting and makes you forget that the camera is there. The end result being a consultation with a more natural flow. Ensure that you have read about or know patients before they come in. Make sure you know where basic equipment, paperwork etc. are kept especially if different room used for video. Pay particular attention to: asking patients how they feel about their illness or the proposed management. getting a psychosocial perspective on the illness. All consultations have a psychosocial perspective. For instance, the mother who brings her child in with a URTI. A psychosocial enquiry may reveal that she is a single parent, living alone, who was up all night with the child’s persistent coughing and yet still had to work the next day stocking shelves. You can see how a simple presenting complaint (cough) can have a massive impact on someone’s life. What initially might seem trivial to us now doesn’t do so because of the impact it has on the patient’s/carer’s live(s). In this scenario, empathising with the mother would help develop rapport. checking with patients whether they are allergic to medication or whether there are any significant contraindications. properly explaining to patients on how to take their medication. 'safety netting', or making follow up clear to the patient 111 asking patients if they have any questions. Remember, a lot of videos fail for technical reasons, so don’t let poor sound or picture quality ruin your chances. Get it sorted! If sound is poor, consider investing in an external desktop microphone. Ensure picture quality is acceptable. The camera should be positioned on a tripod or platform and in such a way that both doctor and patient are visible. This may be achieved if, for example, doctor and patient sit at adjacent sides of a desk rather than facing each other across the desk. You may wish to purchase a wide angle lens adaptor for this purpose. The camera should not be directed towards a source of light, such as a table lamp or a window immediately behind the patient or doctor. Make sure that there is an area of the room which is clearly out of view of the camera and in which examinations of an intimate or sensitive nature could take place; or have an alternative strategy such as a lens cap which can be fitted to the camera. Get a colleague to check if you are unsure. as your training year progresses you will find that you will see more and more patients with chronic problems that you have seen time and time again. Other than the very first consultation that you had with them, subsequent ones tend not to prove as fruitful in terms of eliciting the performance criteria. For instance you may have initially explored the psychosocial context of a chronic problem when you first saw the patient but it might be inappropriate to keep revisiting this on every subsequent one. In that way subsequent consultations will get less ticks than the first one. One way around this is to video emergency surgeries. This will provide you with new patients who you may not have had contact before and therefore provide the perfect opportunity for exploring other areas. Be aware of submitting videos of middle-aged men who drop their trousers in front of the camera without the slightest warning. Don't be distracted by unnecessary fiddling with notes or computer. Don't forget to get your videos reviewed by other people. Whilst your trainer may be great to please remember that the trainer is not an examiner and in all probability never sat a video module as it was not a requirement when they did it. Therefore you may wish to seek the views of colleagues taking the exam at the same time. Often they can provide you with more objective feedback based on very good knowledge of the criteria. Asking your trainer to look at the videos Remember, trainers are not examiners. If you and your trainer think that your seven selected consultations have a reasonable chance of passing, please do not blame him or her if you fail. Your trainer can only tell you what they think but most are not MRCGP examiners and many have not been trained in this skill. It’s also likely they never sat an MRCGP video exam (if they’re over 40). So please don’t blame them; this is your own piece of work, not theirs. Try to get several opinions on your videos, not just the trainer’s. Your fellow registrars or other candidates sitting the exam tend to have a good critical eye more consistent with the examiner’s. If you do pass, don’t forget to thank your trainer; it is probably because of the numerous video tutorials you have had with him or her that has cumulatively led to your development in consulting skills and therefore in achieving a pass mark. 112 Final Checklist Competence demonstrated - Clear evidence of competence in each pass-level performance criterion demonstrated at least four times in your consultations. Paperwork - (a) Workbook: All consultations listed with timings in the log. A consultation assessment form filled out for every consultation, (b) Patient Consent Forms (to be retained in your surgery) One consent form fully completed for each recorded consultation The consultation reference number entered on each consent form Video tape - (a) A single tape in VHS-PAL format recorded at normal speed, (b) Sound and picture quality checked by an independent viewer for quality Identifying materials - (a) Your initials, surname and candidate number labelled on the workbook, on the video tape, and on the tape box. 30% Fail the Video. Why? ……and here are some specific comments made by the assessors about common pitfalls: Failure to clearly define patient's reasons for attendance i.e. having seen the video recording one is left with the impression that the patient's underlying concerns etc. have not been identified. Poor listening skills i.e. poor eye contact. Interruption of patient's narrative, particularly early on in the consultation. Missed cues (but this is now a merit criterion; it used to be a basic one!) Poor negotiation skills i.e. a consistently doctor centred approach even when this might not be appropriate. There are too many low challenge consultations for minor self-limiting problems which really do not give the Registrars a chance to demonstrate their skill. The Registrars' logbook entries often merely describe the tape rather than reflecting on what happened and identifying possible errors. Too many tapes are still of poor technical quality with consultations that are longer than 15 minutes. Registrars often lack skills relating to children. They usually talk to the parent rather than the child and often lack any toys to put a child at ease. Registrars often lack skills in "therapeutic" dialogue. When taking to depressed people they rarely seem to challenge the patient to reflect on their situation or facilitate any change. Registrars often fail to "make contact" with the patient in terms of finding out anything about their fears, their expectations or even what their job is. Consent Ensure truly informed consent has been obtained from the patient. Check your set up for obtaining patient consent; receptionists sometimes have a habit of forgetting! Make sure your receptionist understands what you are doing and why, and explains it to the patient. Your receptionist should not attempt to persuade patients to consent, but the giving or refusal of consent may depend in part on the attitude of the receptionist or other person handing out the form. A patient's consent cannot be genuinely ‘informed’ if the way they have been asked appears perfunctory or coercive. Try not to get any part of the consent process on video; otherwise, you might be judged on it! Try and spend some time with reception staff and explain in detail a) what truly informed consent is b) what phrases they should use when asking for consent c) what forms they need to become familiar with 113 MRCGP Video Assessment Sheet (use a separate sheet for each video consultation) 10 Pass Criteria: each demonstrated at least 4 times in total of 7 videos □ Active listening. Open questions. Reflecting. Facilitation. Comments: □ □ Encourage patient contribution Appropriate working diagnosis Social, occupational & psychological context Use the information. Causes of illness. Consequences. Family. Comments: Explore patient’s health understanding ICE. Only if additional info is actually elicited. Comments: □ Sufficient history: PC, PMH, relevant symptoms Exclude relevant significant conditions. Comments: □ Appropriate management in appropriate language plan Involve patient in management options Good understanding of modern medical practice. EBM. Give & explain appropriate options. Sharing/Negotiation. Comments: Comments: □ Appropriate physical & mental examination Choice of examination. Outline intended examination to patient Comments: □ Explain problem / diagnosis Plain English. Avoid jargon. Check understanding/acceptance Comments: □ □ Comments: □ Specify F/U conditions & interval Clear reference to further contact. “Safety-netting.” Comments: 4 Merit Criteria: □ Respond to signals and cues Face, body language, phrasing, omissions, med records. Only if relevant additional info is elicited Comments: □ Incorporate patient’s health beliefs when explaining problem Incorporate ICE when explaining problem. Comments: □ □ Seek to confirm patient’s understanding of diagnosis Explore patient’s understanding of treatment to enhance concordance “Does that make sense to you; anything you want to ask?” Offer to explain to a third party. Similar. Regards to treatment Comments Comments: Drs. Ramesh Mehay & Matthias Hohmann, Bradford 114 115 Is Your Collective Video Good Enough? overall distribution of PCs in the submitted collection of 7 consultations Each number (1-7) represents a consultation being submitted for MRCGP. Simply circle the consultations which demonstrate that PC. After assessing all 7 consutlations, ensure you have at least 5 circles (the examiners will look for 4) in each box. I recommend 5 as a safety netting procedure. 10 Pass Criteria: each demonstrated at least 4 times in total of 7 videos Encourage patient contribution Social, occupational & psychological context Explore patient’s health understanding Sufficient history: PC, PMH, relevant symptoms Appropriate physical & mental examination 1 2 3 4 5 6 7 1 2 3 4 5 6 7 1 2 3 4 5 6 7 1 2 3 4 5 6 7 1 2 3 4 5 6 7 Active listening. Open questions. Reflecting. Facilitation. Use the information. Causes of illness. Consequences. Family. ICE. Only if additional info is actually elicited. Exclude relevant significant conditions. Choice of examination. Outline intended examination to patient Appropriate working diagnosis Explain problem / diagnosis in appropriate language Appropriate management plan Involve patient in management options Specify F/U conditions & interval 1 2 3 4 5 6 7 1 2 3 4 5 6 7 1 2 3 4 5 6 7 1 2 3 4 5 6 7 1 2 3 4 5 6 7 Plain English. Avoid jargon. Good understanding of modern medical practice. EBM. Give & explain appropriate options. No choice necessary. Clear reference to further contact. “Safety-netting.” Respond to signals and cues Incorporate patient’s health beliefs when explaining problem Seek to confirm patient’s understanding of diagnosis Explore patient’s understanding of treatment to enhance concordance 1 2 3 4 5 6 7 1 2 3 4 5 6 7 1 2 3 4 5 6 7 1 2 3 4 5 6 7 Face, body language, phrasing, omissions, med records. Only if relevant additional info is elicited Incorporate ICE when explaining problem. “Does that make sense to you; anything you want to ask?” Offer to explain to a third party. Similar. Regards to treatment 4 Merit Criteria: Drs. Ramesh Mehay & Matthias Hohmann, Bradford 116 EXAMPLE VIDEO LOG SHEETS 117 Camera Clock Time :09-44 3 Duration of Consultation: 13 mins Wheezing, ?Exacerbation of Asthma Patient new to area. Asthma since childhood years … never been followed up. Nil acute hospital admissions. Smokes 5/week. Nil acute cough/cold. Living with fiancee and currently decorating new house. Has a pet cat. ? Breathing difficulty secondary to paint fumes +/- Anxiety element/Hyperventilation syndrome Reassurance. Asthma Nurse Referral (to consider stepping down treatment). General measures for inhalation of paint fumes given (masks, windows open etc) Nil As this young lady was new to the practice, I decided to build a rapport and reduce any apprehension by starting off with some non-medical chat. A detailed written drug history was taken to hep me gain a good understanding of what she was taking. The affect of the asthma on her social life was inquired about. I did not try to lecture her too much about the smoking as I did not want her to feel guilty. A recent BMJ article (Butler et al, 1998) commented that a ‘preaching’ style approach was unlikely to cause change. Some found it irritating and he suggested that the thought should be put forward by the doctor but the decision be left to the patient…in their own time. An examination failed to reveal even the slightest of wheeze despite good air entry. Her Peak flow technique was poor. In view of this and her tolerability to pets, I felt that her childhood asthma had probably cleared up (60% of childhood asthma clears up by teenage years). However, because I had not seen her before, I emphasised that we would be looking at her in the asthma clinic on several occasions before considering this option. I also emphasised that this would be done in a controlled fashion. She seemed happy with this. 118 Camera Clock Time :10-28 00 5 Duration of Consultation: 13 mins Right Sided Back and Groin Pain This man had been laying down paving slabs recently. He has a history of depression and is on Prozac for this (no current symptoms) Musculoskeletal strain Rest & Analgesia Lifting Advice Supplemented with Leaflets Over The Counter Aspirin This gentleman’s health belief system with regards to his perception of the origin of his back pain was explored. The chronological sequence of events was ascertained. My initial thoughts centred on excluding the groin pain being secondary to a hernia. Examination : no hernia, no focal neurological signs, no hernia. He reported no red flag symptoms. This thorough examination was fed back to the patient who subsequently felt reassured. The advice given regarding the TENS machine this man had recently bought was purely based on simple rationale. Towards the end of the consultation, a summary of the findings and management plan was reiterated. The consultation was drawn to a close with an open appointment should further problems re-occur. This was made on the basis of the Croft et al Studies (BMJ 1998) which stated that acute back pain often persists after many months….it is just that patients do not like to bother the Doctor again. Simple back advice augmented by a leaflet was given in order to promote self help behaviour. 119 Camera Clock Time :12-11 20 7 Duration of Consultation: 10 minutes Review of Eczematous skin Single parent family. Household of 2 children (both under 5). Mother is a frequent presenter (re: minor illnesses). Social circumstances are not that great and she does have financial difficulty. Childhood vaccinations up to date. Mild Eczema General skin care advice. Negotiation of a Management Plan. Prescription given. Alphaderm to be applied tds E45 cream General advce This lady is a demander for steroids, and I felt it appropriate to re-iterate the side effects of long term use in order to discourage frequent use. Her concerns were elicited. The consultation is otherwise set at the level of the child in order to engage her co-operation. On examination, she has mild eczematous patches which are not acutely infected. The pathophysiology of this condition is re-explained. The mother was not keen to stop the steroids, despite good clinical effect, and so we both negotiated a management plan. General measures on skin care was given in order to promote self help behaviour and reduce Doctor Dependency. She seemed happy with this. An enquiry is made into her present social circumstances and finances (presently stable, though previous hardship known). This consultation was performed towards the end of my attachment at this practice. As she is a frequent attender, the management plan was recorded on to the computer in order to communicate the plan to the next doctor and in order to prevent conflict of advice. The consultation was then rounded up of a summary of what had been achieved and a social chat. Despite a demanding mother, the rapport between us remains unharmed. 120 121 ….and now for some other bits 1. Have you failed one or more components of the MRCGP exam? 2. Why patients go to see the doctor 3. Models of the consultation 4. Medical ethics & law 5. Duties of the doctor 122 123 Have You Failed Any Component of the MRCGP exam? Please, do not be disheartened. Many candidates fail 1 of the four components of the exam. You need to pick yourself up and try again. Most get through on their second attempt. Let’s look at some simple stats (promise, this wont bore you): In the old exam (pre 1998), when it was NOT modular and you just did all of it in one go: The pass rate was 80% That means 20% failed ie 1 in 5 people failed! In this new modular exam (may 1998 onwards), where most people take different bits at different times: The pass rate is still quoted as 80% BUT there are four components to the exam! I hear you say “so, what’s that got to do with anything?”. Well, look at it from this point of view: MCQ: 80% pass Video: 80% pass (it’s actually 70%, but let’s keep it at 80% to make the maths easier) Written: 80% pass Orals: 80% pass That means, if you attempt any one module, you have an 80% chance of passing (like the old exam). However, if you attempt all four, the chances of you passing are = 0.8 x 0.8 x 0.8 x 0.8 = 0.41 = 41%. That means you have a 41% chance of passing if all four modules are taken and a 59% chance of failing! 2 in every five will get all four components on the first sitting. I don’t want to dishearten you. All I am trying to do is to illustrate the point that it is not uncommon for candidates to fail one of the four modules and that you should not be too distressed by this nor consider yourself a bad GP. By putting in a little extra oomph into your work and revision, you should be able to get that final nugget. Most candidates do go on to pass the offending module next time round. So don’t despair. 124 125 Why Patients go to Doctors. Dr. Albert Cave, Surrey Why? The supposition that a patient go to the doctor when they have symptoms does not hold true. The non-attender fails to go to the doctor despite gross symptoms and the frequent-attender attends for trivial reasons. Prevalence Dunnell 1972 : most people can recall up to 4 symptoms in the last two weeks. Wadsworth 1971 : 95% experiences at least one symptom in the past two weeks. Health diaries detect daily symptoms, retrospectively however people only report on average one or two symptoms per week. a) Symptoms are common - a constant barrage in every day life. b) Most are soon forgotten. C) It is not the symptom that is important it is the significance placed upon it that is important. d) Perception is important eg mood affects detection and significance. Illness behaviour: Perception Common Symptoms Illness behaviour Significance One's illness behaviour is learnt from one's Family, Community and sub-communities - Norms. Normalizations are accepted symptoms Eg aches and pains in old age. Normalization can block the emergence of important diagnostic information. Eg “Do you have a cough?” “No.” “Do you have a smokers cough?” (a norm) “Yes” Socially acceptable Norms Family Norms Illness behaviour Previous illness experience It is the patient’s perception as to whether a symptom is normal or abnormal that causes them to attend and not the symptom itself 126 Zola 1973: There are five social triggers leading to presentation a) Perceived interference with vocational or physical activity. b) Perceived interference with social or personal relationships. c) Occurrence of an interpersonal crisis. d) Temporising – “if not better by Monday”, or “just two more nosebleeds”. e) Sanctioning - pressure from family and friends. Four Courses of Action: a) b) c) d) Ignore the symptom Consult family or friend - the lay referral system. The patient sees different people with successive claims to knowledge. Self medication - on average it takes two weeks and two medicines are tried, of which 2/3 are over the counter medicines. Consult the Medical Services - GP, A&E, hospital. The Role of the Doctor. The patients asks will he be able to do anything more than offer: a) Sympathy and support. b) Therapeutic The doctor offers treatment. The patient will often have their own idea as to what treatments the doctor can offer and this influences their decision to attend. Some people attend with abnormal expectations about treatments and cures that do not exist. Two Responses Some patients do not attend because they feel or do not know that a doctor can help them with treatment. c) Legitimise The doctor eases the transition from person to patient (the sick role), which may have a role with family and employer. In our society, only the doctor can legitimise the sick role. The Sick Role - has two benefits and two obligations. 1) Temporary excuses the normal role family and work. 2) Removes responsibility for the illness from the patient. 3) The patient must want to get better. The sick role is an abnormal state. 4) The patient must comply with treatments prescribed by the Doctor. Relying on lay help is adjudged as not complying with a basic obligation of the sick role. The chronically sick are frustrated in their sick role – ie they are unable to fulfil the obligations of the sick role. Not every patient follows the above rules or considers all options. The patient’s decision making may seem irrational but often complex reasoning lies behind their attendance. Summary : The GP needs to ask two questions 1) 2) What is the presenting problem Why did the patient come now – ie what is their (hidden) agenda 127 MODELS OF THE CONSULTATION Juliet Draper A summary of models that have been proposed over the last 20 years: There have been a number of helpful models of the consultation which have been produced over the last 30 years. Some are task-orientated, process or outcome-based; some are skillsbased, some incorporate a temporal framework, and some are based on the doctor-patient relationship, or the patient’s perspective of illness. Many incorporate more than one of the above. Models of the consultation give a framework for learning and teaching the consultation; the toolbox is a useful analogy. Models enable the clinician to think where in the consultation they are experiencing the problem, and what they and the patient aiming towards. This is helpful in then identifying the skills that are needed to achieve the desired outcome. A particularly useful general book on Understanding the Consultation by Tim Usherwood (see the book list at the end of this document) describes a number of the models below in more detail, and also includes psychological concepts such as projection, transference and counter-transference. 1. ‘Physical, Psychological and Social’ (1972) The RCGP model encourages the doctor to extend his thinking practice beyond the purely organic approach to patients, i.e. to include the patient’s emotional, family, social and environmental circumstances. 2. Stott and Davis ( 1979) “The exceptional potential in each primary care consultation” suggests that four areas can be systematically explored each time a patient consults. (a) Management of presenting problems (b) Modification of help-seeking behaviours (c) Management of continuing problems (d) Opportunistic health promotion 3. Byrne and Long (1976) “Doctors talking to patients”. Six phases which form a logical structure to the consultation: Phase I The doctor establishes a relationship with the patient Phase II The doctor either attempts to discover or actually discovers the reason for the patient’s attendance Phase III The doctor conducts a verbal or physical examination or both Phase IV The doctor, or the doctor and the patient , or the patient (in that order of probability) consider the condition Phase The doctor, and occasionally the patient, detail further treatment or further investigation V Phase VI The consultation is terminated usually by the doctor. Byrne and Long’s study also analysed the range of verbal behaviours doctors used when talking to their patients. They described a spectrum ranging from a heavily doctordominated consultation, with any contribution from the patient as good as excluded, to a virtual monologue by the patient untrammelled by any input from the doctor. Between these extremes, they described a graduation of styles from closed information-gathering to nondirective counselling, depending on whether the doctor was more interested in developing his own line of thought or the patient’s. 128 4. Six Category Intervention Analysis (1975) In the mid-1970’s the humanist Psychologist John Heron developed a simple but comprehensive model of the array of interventions a doctor (counsellor or therapist) could use with the patient (client). Within an overall setting of concern for the patient’s best interests, the doctor’s interventions fall into one of six categories: (1) Prescriptive - giving advice or instructions, being critical or directive (2) Informative - imparting new knowledge, instructing or interpreting (3) Confronting - challenging a restrictive attitude or behaviour, giving direct feedback within a caring context (4) Cathartic - seeking to release emotion in the form of weeping, laughter, trembling or anger (5) Catalytic - encouraging the patient to discover and explore his own latent thoughts and feelings (6) Supportive - offering comfort and approval, affirming the patient’s intrinsic value. Each category has a clear function within the total consultation. 5. Helman’s ‘Folk Model’ (1981) Cecil Helman is a Medical Anthropologist, with constantly enlightening insights into the cultural factors in health and illness. He suggests that a patient with a problem comes to a doctor seeing answers to six questions: (1) (2) (3) (4) (5) (6) 6. What has happened? Why has it happened? Why to me? Why now? What would happen if nothing was done about it? What should I do about it or whom should I consult for further help? Transactional Analysis (1964) (Eric Berne) Many doctors will be familiar with Eric Berne’s model of the human psyche as consisting of three ‘ego-states’ - Parent, Adult and Child. At any given moment each of us is in a state of mind when we think, feel, behave, react and have attitudes as if we were either a critical or caring Parent, a logical Adult, or a spontaneous or dependent Child. Many general practice consultations are conducted between a Parental doctor and a Child-like patient. This transaction is not always in the best interests of either party, and a familiarity with TA introduces a welcome flexibility into the doctor’s repertoire which can break out of the repetitious cycles of behaviour (‘games’) into which some consultations can degenerate. 129 7. Pendleton, Schofield, Tate and Havelock (1984, 2003) ‘The Consultation - An Approach to Learning and Teaching’ describe seven tasks which taken together form comprehensive and coherent aims for any consultation. (1) To define the reason for the patient’s attendance, including: i) ii) iii) iv) (2) the nature and history of the problems their aetiology the patient’s ideas, concerns and expectations the effects of the problems To consider other problems: i) ii) continuing problems at-risk factors (3) With the patient, to choose an appropriate action for each problem (4) To achieve a shared understanding of the problems with the patient (5) To involve the patient in the management and encourage him to appropriate responsibility (6) To use time and resources appropriately: i) ii) (7) accept in the consultation in the long term To establish or maintain a relationship with the patient which helps to achieve the other tasks. The authors’ 2nd edition, “The new consultation” includes recent relevant research material and a wealth of experience accumulated by the authors since their first publication. The first part of the book covers the consultation; the “central act of medicine”, and puts both the perspectives of the doctor and the patient, and the outcomes that both are looking for at the heart of the process of the medical interview. The second half of the book is concerned with learning and teaching effective consulting. 8. Neighbour (1987) Five check points: ‘where shall we make for next and how shall we get there?’ (1) Connecting - establishing rapport with the patient (2) Summarising getting to the point of why the patient has come using eliciting skills to discover their ideas, concerns, expectations and summarising back to the patient. (3) Handing over - (4) Safety netting (5) Housekeeping - doctors’ and patients’ agendas are agreed. Negotiating, influencing and gift wrapping. - “What if?’: consider what the doctor might do in each case. ‘Am I in good enough shape for the next patient?’ 130 9. McWhinney’s Disease - Illness Model (1984) McWhinney and his colleagues at the University of Western Ontario have proposed a “transformed clinical method”. Their approach has also been called “patient-centred clinical interviewing” to differentiate it from the more traditional “doctor-centred” method that attempts to interpret the patient’s illness only from the doctor’s perspective of disease and pathology. The disease-illness model below attempts to provide a practical way of using these ideas in our everyday clinical practice. The doctor has the unique responsibility to elicit two sets of “content” of the patient’s story: the traditional biomedical history, and the patient’s experience of their illness. Patient presents problem Gathering information Parallel search of two frameworks Illness framework Patient's agenda Ideas Concerns Expectations Feelings Thoughts Effects Disease framework Doctor’s agenda Symptoms & Signs Investigations Underlying pathology Understanding the patient’s uniques experience of illness Differential Diagnosis Integration Explanation & Planning In terms the patient can understand We some how need to get the doctor’s and patient’s agenda to meet. A possible way of doing this would be: Patient presents problem Gathering information Parallel search of two frameworks Disease framework Illness framework The biomedical perspective Weaving back and forth between the two frameworks The patient’s perspective Symptoms Signs Investigations Feelings and thoughts Underlying pathology Ideas Concerns Expectations Differential diagnosis Understanding the patient’s unique experience of the illness Feelings and thoughts Effects on life Integration of the two frameworks Explanation and planning Shared understanding and decision-making After Levenstien et al in Stewart and Roter (1989) and Stewart et al (1995 & 2003) 131 10. Levenstein JH, Belle Brown J Weston WW et al (1989) Patient-centred clinical interviewing. In Communicating with medical patients (eds M Stewart and D Roter) Sage Publications, Newbury Park, CA. Stewart M. (2001) Towards a global definition of patient centred care. BMJ. 322(7284):444-5, Stewart M et al (2003) Patient-centred medicine: transforming the clinical method. Radcliffe Medical Press Abingdon Oxford The Three Function Approach to the Medical Interview (1989) Cohen-Cole and Bird have developed a model of the consultation that has been adopted by The American Academy on Physician and Patient as their model for teaching the Medical Interview. (1) Gathering data to understand the patient’s problems (2) Developing rapport and responding to patient’s emotion (3) Patient education and motivation Functions Skills 1. Gathering data a) b) c) d) e) f) g) h) i) j) k) Open-ended questions Open to closed cone Facilitation Checking Survey of problems Negotiate priorities Clarification and direction Summarising Elicit patient’s expectations Elicit patient’s ideas about aetiology Elicit impact of illness on patient’s quality of life 2 Developing rapport a) b) c) d) e) Reflection Legitimation Support Partnership Respect 3 Education and motivation a) b) Education about illness Negotiation and maintenance of a treatment plan Motivation of non-adherent patients c) In 2000 the authors published a second edition, where they altered the order of the three functions of effective interviewing, putting “Building the relationship” in front of “Assessing the patient’s problems”, and “Managing the patient’s problems”. The authors have included three excellent chapters on: Understanding the patient’s emotional response Managing communication challenges Higher order skills The section on overcoming cultural and language barriers and troubling personality styles and somatisation are particularly helpful. 132 11. The Calgary-Cambridge Approach (1996) Suzanne Kurtz, Jonathan Silverman & Juliet Draper have developed a model of the consultation, encapsulated within a practical teaching tool, the Calgary Cambridge Observation Guides. The guide is continuing to evolve and now includes Structuring the consultation. The Guides define the content of a communication skills curriculum by delineating and structuring the skills that have been shown by research and theory to aid doctor-patient communication. The guides also make accessible a concise and accessible summary for facilitators and learners alike which can be used as an aide- memoire during teaching sessions The following is the structure of the consultation proposed by the guides: (1) Initiating the Session a) preparation b) establishing initial rapport c) identifying the reason(s) for the consultation (2) Gathering Information exploration of of the patient’s problems to discover the: a) biomedical perspective b) the patient’s perspective c) background information - context (3) Building the Relationship a) b) c) (4) using appropriate non-verbal behaviour developing rapport involving the patient Providing structure a) making organisation overt b) attending to flow (5) Explanation and Planning a) b) c) d) (6) providing the correct amount and type of information aiding accurate recall and understanding achieving a shared understanding: incorporating the patient’s perspective planning: shared decision making Closing the Session a) ensuring appropriate point of closure b) forward planning 133 12. Comprehensive Clinical Method/Calgary-Cambridge Guide Mark 2. (2002) This method combines the traditional method of taking a clinical history including the functional enquiry, past medical history, social and family history, together with the drug history, with the Calgary-Cambridge Guide. It places the Disease-Illness model at the centre of gathering information. It combines process with content in a logical schema; it is comprehensive and applicable to all medical interviews with patients, whatever the context. Below is an example of the skills required to elicit the disease, the illness and the background content when gathering information. gathering information process skills for exploration of the patient’s problems (the bio-medical perspective and the patient’s perspective) patient’s narrative question style: open to closed cone attentive listening facilitative response picking up cues clarification time-framing internal summary appropriate use of language additional skills for understanding patient’s perspective content to be discovered: the bio-medical perspective (disease) the patient’s perspective (illness) sequence of events symptom analysis relevant functional enquiry ideas and concerns expectations effects feelings and thoughts essential background information past medical history drug and allergy history social history family history functional enquiry 134 13. BARD 2002 Ed Warren (2002) The BARD model attempts to consider the totality of the relationship between a GP and a patient and the roles that are being enacted. The personality of the doctor will have considerable influence on the doctor-patient encounter, as will the doctor’s previous experience of the patient. The model attempts to include how the doctor’s personality can be used to best effect, and looks specifically at the doctor and patient roles in the medical encounter. It aims to “encompass everything that happens during a consultation” and encourage reflection. It is important that GPs play to their strengths, and use their role and personality and behaviour positively for the benefit of the patient. The four proposed avenues for analysis are: 1. Behaviour 2. Aims 3. Room 4. Dialogue Behaviour A doctor has many alternatives in how they present to a patient, and these choices will reflect the needs of the patient and the personality of the GP. It includes non-verbal and verbal skills as well as confidence, “lightness of touch”, and behaviours which feel “just right”. The key is for the doctor to choose the most appropriate behaviour with each patient in front of them Aims It is important for the aims of a consultation to be clear in order to help the doctor and the patient to head in the right direction. However not all the aims will necessarily need to be achieved in one consultation, and priorities have to be clarified. Room The consultation will be affected by the environment in which the doctor works, as well as for example, where the doctor sits, or whether a side room is used for the examination. Dialogue How you talk to the patient is crucial. Tone of voice, what you say, language, the ability to confront or challenge needs thought. How can you be sure that both you and the patient are talking the same language? 14. Balint 1986 Michael Balint and his wife Enid, who were both psychoanalysts, started to research the GP/patient relationship in the 1950s, and over many years ran case-discussion seminars with GPs to look at their difficulties with patients. The groups’ experiences formed the basis for a very important contribution to the general practice literature; The doctor, the patient and the illness. In exploring the doctor-patient relationship in depth, Balint helped generations of doctors to understand the importance of transference and counter-transference, and how the doctor himself is often the treatment or drug. Balint groups are still popular, and are usually run on psychodynamic lines and often one of the group leaders is a psychotherapist. Balint’s tenet was that doctors decide what is allowable for discussion from the patient’s offer of problems, and that doctors impose constraints on what is acceptable to explore in the consultation, often unconsciously. This selective neglect or avoidance is often related to something in the doctors life which is threatening. For example a doctor may not wish to explore alcoholism in a patient if he or she either drinks to excess themselves, or someone close to the doctor has an alcohol problem. It the patient is also reluctant to discuss the issue then this can lead to collusion. 135 Balint groups commonly begin with “has anyone a case today?” A doctor then tells the story of a patient who is bothering him and the group will help the doctor to identify and explore the blocks which are constraining exploration and management of the patient’s problem. 15. Narrative-based Medicine, Launer J (2002) Narrative studies explore the way people tell stories. The modernist approach had been to be attentive to these stories and the particular approach described in this book is a specific one, developed by a team of teachers at the Tavistock Clinic in London. In primary care we have an option not only to reflect on these stories, we can respond to and even challenge them. Thus the post-modern and more radical view would be that a clinical interaction is one in which two parties bring their own individual contexts and preferences, to create what is a unique and developing conversation. For example, in the context of the consultation between a patient and the GP, there is often no “ultimate truth” to the answer to the question “why has the patient attended”, or what the patient is hoping for from the doctor, because in an attempt to explore these important questions, even more important questions and ideas will emerge. Skills which help the patient to understand better what is happening to them not only include the basic skills of listening, and empathising. Question style is crucial; appropriately timed questions asked with respect and in the spirit of caring about the eventual outcome for the patient can be used with great effect in contexts where the clinician is trying to help the patient look at a problem from a different point of view, and encourage behaviour change. They might be compared with to Socratic questioning, and form the basis of narrative-based interviewing and originally come from family systems therapy. The six key concepts are: 1. conversations 2. curiosity 3. circularity 4. contexts 5. co-creation 6. caution Some examples: “When you get home, what do you think your husband might say when you tell him what we have been talking about?” “Who in the family thinks you are depressed as well as your husband?” “If we can’t get to the bottom of your problem, what do you think you might do next?” Constructing a genogram with the patient is a good example of one of the other techniques used in narrative-based medicine. 136 REFERENCES 1 Working Party of the Royal College of General Practitioners ( 1972) 2 Stott N C H & Davis R H ( 1979) The Exceptional Potential in each Primary Care Consultation: J R Coll. Gen. Pract. vol 29 pp 201-5 3 Byrne P S & Long B E L (1976) Doctors talking to Patients: London HMSO 4 Heron J (1975) A Six Category Intervention Analysis: Human Potential Research Project, University of Surrey 5 Helman C G (1981) Disease versus Illness in General Practice J R Coll. Gen. Pract. vol 31 pp 548-62 6 Stewart Ian, Jones Vann (1991) T A Today: A New Introduction to Transactional Analysis Lifespace Publishing 7 Pendelton D, Schofield T, Tate P & Havelock P (1984) The Consultation: An Approach to Learning and Teaching: Oxford: OUP 8 Neighbour R (1987) The Inner Consultation MTO Press; Lancaster 9 Stewart M et al (1995) Patient Centred Medicine Sage Publications 10 Cohen-Cole, S (1991) The Medical Interview, The Three Function Approach Mosby-Year Book Cohen-Cole S, Bird J. (2000) 2nd edition Mosby Inc. 11 Kurtz S & Silverman J (1996) The Calgary-Cambridge Observation Guides: an aid to defining the curriculum and organising the teaching in Communication Training Programmes. Med Education 30, 83-9 Silverman J, Kurtz S and Draper J, (1998) Skills for Communicating with Patients Radcliffe Medical Press, (2nd edition in preparation) 12 Kurtz S, Silverman J, Benson J, Draper J. (2003) Marrying Content and Process in Clinical Method Teaching; Enhancing the Calgary-Cambridge Guides Academic Medicine volume 78 no. 8 pp 802-809 (see also www.SkillsCascade.com) 13. Warren E. (2002) An introduction to BARD: a new consultation model Update 5.9.02 152-154 14. Balint M. (1986) The Doctor, the Patient and the Illness Edinburgh: Churchill Livingstone 15. Launer J. (2002) Narrative-based primary Care: a practical guide. Radcliffe Medical Press Abingdon Oxford Other useful texts Usherwood T (1999) Understanding the consultation: evidence, theory and practice OUP Buckingham Philadelphia 137 TWO THINGS I WOULD URGE YOU TO CONSIDER: 1. download and read Bill Bevington’s “The Consultation Handbook” - simply brilliant 2. Buy a copy of the Calgary Cambridge Model - SUMMARY 1: Current Models of the Consultation in terms of Dimensions. Dimensions Explored in the Model 2 3 4 5 6(i) 7 What Dimensions? Doctor centred vs Patient-centred Physical Psychological Social Presenting Problem Continuing Problems Modifying Help-Seeking Health Promotion Checkpoints: Connecting Summarising Hand-over Safety-netting Housekeeping (i) Phases Relationship Agenda Examination Consideration Treatment Closure (ii) Health beliefs What? Why? Why me? Why now? What if? What next? Tasks Agenda Other Problems Choice of Action Shared Understanding Involvement Use of Resources Maintaining Relationship Reference Byrne & Long, Doctors talking to patients (1976) (BOOK) Working part of the RCGP, The Future General Practitioner: learning and teaching (1972) (REPORT) Scott & Davies, The exceptional potential in each primary care consultation (1979) (JOURNAL PAPER) Neighbour, The Inner Consultation (1987) (BOOK) Byrne & Long, Doctors talking to patients (1976) (BOOK) Helman C, Disease versus illness in general practice (1981) (JOURNAL PAPER) Pendleton, Schofield, Tate & Havelock, The consultation: an approach to learning and teaching (1984) (BOOK) SUMMARY 2: THE CONSULTATION MODELS IN TERMS OF TASKS (summary from Bill Bevington’s Consultation handbook HOSPITAL MODEL HEALTH BELIEF MODEL BYRNE & LONG STOTT & DAVIS PENDLETON NEIGHBOUR History of Present Complaint Establish Relationship Management of Presenting problems Reason for Attending Organiser vs Responder Health Motivation Past Medical History Discover Reason for Attending Nature & History of Problem Connecting Perceived Vulnerability Summarising Perceived Seriousness Handing Over Costs v Benefits Safety Netting Cues to Action Housekeeping Locus of Control Modification of Help Seeking Behaviour Medication Physical and/or Verbal Examination Family History Aetiology Management of continuing problems Social History Dr or Dr Pt Consider Problem Direct Questions Dr & ?Pt Detail Rx and Investigations Examination Dr or ?Pt Ends Consultation Opportunistic Health Promotion Ideas, Concerns & Expectations Effects of the Problem Continuing Problem Internal or External At Risk Factors Diagnosis The Powerful Other Choose Action Investigation Sharing Understanding Treatment Involve Abet in Management Sharing Responsibility Use Time Appropriately Maintain positive relationship Ethics and Law (Maggie Eisner, Bradford) Principles (Beauchamp and Childress; Gillon) beneficence - doing good - i e looking after the patient’s best interests. Does this sound paternalistic now? non-maleficence - primum non nocere (Latin - ? origin) = first, do no harm. May be useful, when faced with a dilemma, to ask what harms may result respect for autonomy - people’s capacity to make their own decisions. Who is competent to make their own decisions (i e deserves respect for their autonomy?). How much information might they need to do this? justice - distributive justice ie fairness for populations. Involved in all resource allocation decisions. GPs now involved more closely in these, via PCTs. Moral theories virtue (Aristotle) - people with good character traits make good decisions; we should develop those qualities in ourselves. (What qualities for a doctor? determination, consistency, sense of humanity) duty (Kant) - the deontological principle - we have absolute obligations to each other based on respect for another’s person. We must treat people as ‘ends’ rather than ‘means’. utility (Jeremy Bentham, John Stuart Mill) - the rightness and wrongness of an action is determined only by its consequences: the greatest good for the greatest number rights - more modern notion - e g everyone has a right to medical care - but Human Rights Act 1998 includes many others relevant to medicine, e g dignity of the human person, right to life, prohibition of torture, right to liberty and security, right to respect for private and family life, freedom of thought, conscience and religion, freedom of expression, right to marry, prohibition of discrimination. Areas which commonly raise ethical considerations professional duties confidentiality consent reproductive issues mental health end of life issues children screening rationing (resource allocation) Legal aspects of consent Form of consent may be implied or expressed implied consent usually sufficient for minor procedures, expressed consent nec for major/invasive procedures oral and written consent equally valid, but written more useful for proof doctors should document and file consent to treatment safely Battery and negligence Patients treated without valid consent can take action for battery (intentional injuring) or for negligence (breach of duty of care). Main differences: Nature of action Battery criminal charge Level of consent req’d to defend Broad terms of treatment Need for pt to show actual loss/injury No Need for pt to show loss foreseeable No Negligence compenstion claim or compensation claim Informed consent Yes Yes How much info should be given to patients? No clear legal criteria. Need sufficient info to make informed decision about whether to accept treatment Specific questions about potential complications must be answered as truthfully as possible Info given to patient should be documented in medical records Who can give legally valid consent? Any competent persons over 16 can consent to own treatment Children under 16 if they are regarded as competent Those with parental responsibiliyt can give legally valid consent for under 18s No other persons can give legally valid consent Who has capacity to consent? Criteria for capacity to consent are 1. understanding and retaining treatment information 2. believing it 3. weighing it in the balance to arrive at a choice 4. anyone over 16 has capacity unless shown otherwise Possible reasons for incapacity: 1. age under 16 - but competent if sufficient maturity/intelligence. however docs should try to persuade them to involve parents. 2. temporary or permanent physical disability (eg drowsiness, unconsciousness) - doctors can then give emergency or life saving treatment in pt’s best interests 3. mental handicap - for mentally retarded adults over 18, valid consent may be impossible. May need to apply to courts for declaration that treatment without consent wd not be unlawful 4. Mental Health Act - compulsory treatment allowed only if related to the mental disorder; other treatments must be given under common law 5. mental disorder - capacity to consent must be separately assessed for each particular treatment considered (my be competent to consent to one treatment and not another) 6. undue influence from another person - in this case (esp life threatening decisions), medical staff should treat according to patient’s best interests Legal aspects of confidentiality There is no unified legal source on confidentiality - law has developed haphazardly. All personal info divulged by a patient to a health professional shoud be treated confidentially and not divulged to a third party except in particular circumstances Unless authorised explicitly by patient, this includes their friends and relatives Most breaches of confidentiality are inadvertent Duty of confidentiality continues after patient’s death Exceptions: 1. patient consent 2. those with a need to know for the patient’s care 3. statutory duty (e g DVLC) 4. warrant issued by circuit judge under Police and Criminal Evidence Act eg suspected terrorism 5. explicit instructions from a judge in court 6. wider public interest outweighs duty of confidentiality Legal aspects of access to information There are no common law rights of access to medical records - rights are covered in various different statutes covering different areas Data Protection Act 1984 gives access to computer records Access to Health Records Act 1990 gives access to manual records made since 1.11.1991 Access to Medical Reports Act 1988 cover access to medical reports made for employment or insurance purposes Safeguards built into all these Acts exempt health professionals from disclosing info which would harm physical or mental health of a patient or would breach confidences of a third party Further reading on Ethics and Law Orme-Smith A and Spicer J (2001) Ethics in General Practice - a handbook for personal development Radcliffe Medical Press, Oxford Leung W (2000) Law for Doctors Blackwell, Oxford Duties Of the Doctor (GMC) The duties of a doctor registered with the General Medical Council Patients must be able to trust doctors with their lives and well-being. To justify that trust, we as a profession have a duty to maintain a good standard of practice and care and to show respect for human life. In particular as a doctor you must: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. make the care of your patient your first concern; treat every patient politely and considerately; respect patients' dignity and privacy; listen to patients and respect their views; give patients information in a way they can understand; respect the rights of patients to be fully involved in decisions about their care; keep your professional knowledge and skills up to date; recognise the limits of your professional competence; be honest and trustworthy; respect and protect confidential information; make sure that your personal beliefs do not prejudice your patients' care; act quickly to protect patients from risk if you have good reason to believe that you or a colleague may not be fit to practise; avoid abusing your position as a doctor; and work with colleagues in the ways that best serve patients' interests. In all these matters you must never discriminate unfairly against your patients or colleagues. And you must always be prepared to justify your actions to them. Final Word on the Exam… No matter how well you have prepared yourself for the MRCGP examination most candidates at some point convince themselves that they have not done enough. They will even convince themselves that they are doomed to failure. Despite these convictions, you will probably pass and in doing so prove that you have the capabilities of a good GP. Hooray, I’ve got my MRCGP. So now what? Contact the secretary of your local faculty of the RCGP. You can do this via the RC GP web site www.rcgp.org.uk . He or she will be a better tell you what groups/individuals will be able to support new members and how. Contact your local GP tutor This is a person who is employed by the regional Department of postgraduate general practice education. He or she will either help you directly or put in touch with the people and organisations you need. (S)he will also guide you with your personal development plan and will give you advice on appraisal and revalidation. Many regions also have a specific tutor for non principals and again this is another person you may wish to contact. If you're an non-principal consider joining the the National Association of sessional GPs. Why not have a look at their website? www.nasgp.org.uk They can provide you with invaluable advice on things like how to get a job, career options, certification, finances and the practicalities are working different practices. They also provide a good forum for online discussion which should help reduce the feeling of social isolation. Consider forming a peer group. For instance, why not continue meeting you’re your MRCGP study group. Groups like these can provide a safe haven from discussing difficult professional and personal issues but it can also help you keep informed and up-to-date. These groups are therefore inviolable and providing both professional and social support. Plan for diversity. The secret of maintaining motivation and sustaining a career is to build variety into your working life. The MRCGP opens many avenues and pathways so start thinking about your major professional interests. For instance you may wish to engage in teaching, training, undertaking research or developing specialist GP skills. Getting career advice from your GP tutor and undertaking courses will help you make a choice that is right for you. Remember that now that you have got your MRCGP, you are now in a better position to help redefine general practice and shape the future of the benefit of doctors and patients alike. The world of general practice is open to you. Good luck in whatever choices you make. Adapted from “Planning for life beyone the MRCGP, Amar Rughani, The Practitioner, April 2002 vol 246)