Chapter 1
advertisement

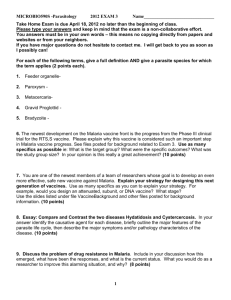
ACKNOWLEDGEMENTS 1 Table of Contents Introduction Chapter 1 MALARIa Chapter 2 DRugs – Out of reach Chapter 3 The lifeblood of economics Chapter 4 The tomorrow of today Conclusion 3 4 4 6 6 17 17 23 23 26 2 Introduction Malaria and Africa is without doubt a very broad topic and there are many aspects in which to view it. The sheer depth and complexity of this raging epidemic is impossible to comprehend much report in a balanced fashion. This dissertation is a whirlwind tour of the science and economic of drugs implemented to aid the crisis of Malaria in the Sub- Sahara Africa. I chose Sub- Sahara Africa to focus on mainly because it is in this poor country that a child is killed every 30 seconds; 3000 die everyday; a staggering 1.5 to 2.7 million African deaths a year, according to the World Health Organization (WHO)’s estimates. 1Most of those dying are children and pregnant women, with 300 to 500 million infected every year. This colossal burden appears to be growing heavier and we will identify the major players and take a quick glance into their inner workings in, I hope, an evenhanded way. We will highlight the development of drugs and incessant search for a vaccine through trials and more trials. The stumbling block in creating a successful cure is discussed as well as the fraught with political, economical and scientific implications which have to be overcome to bring the drugs to where it will be in years to come. From that we will observe the victories through the discovery of effective drugs as well as failures, through inadequacies, incompetence and selfishness. There is no right and wrong, and as this is crisis is on a human level, mistakes are inevitably made. There are however a great many things that we can do. The current situation in sub-sahara Africa emphasizes the need for a more pro-active response by all parties involved to broaden the approach to help the development of the country. Lastly, it is my hope that you will enjoy reading this dissertation as I have writing it. 1 Rachel Mak 1 Due to the nature of some of the contents discussed in this report, I would like to express my sincerest apologies should any material in this dissertation insult or offend you, the reader, in any way and it is by no means my intention and regrettable. 3 Chapter 1 MALARIA 1.1 What is Malaria? M alaria is a life-threatening parasitic disease of the blood which is transmitted to human beings by the female Anopheles mosquito. It is caused by any one of four species of one-celled (protozoan) parasites, called Plasmodium. The four types of plasmodium are P. falciparum (which is the most deadly), P. vivax, P. ovale and P. malariae. The typical symptom of malaria is a violent fever lasting 6 to 8 hours, recurring every two or three days. Plasmodium falciparum malaria presents an irregular tertian fever which leads to a coma and eventually death.2 This is most common in Africa, south of the Sahara, accounting for the extremely high mortality in this region. The three stages of an attack of malaria 1.2 The Vicious Cycle The female Anopheline mosquito transmits malaria parasites from one person to another - male mosquitos do not as they feed only on plant juices. It uses its proboscis to penetrate the victim's skin and the saliva which flows into the victim's skin to ease the pain is where the Protozoan is located. 3The malaria parasite enters the human host when an infected Anopheles mosquito has a blood meal. Inside the human host, the parasite undergoes a series of changes as part of its complex life-cycle. It is these multiple stages that allow plasmodia Figure 1- Man and mosquito play complementary roles in Malaria cycle to evade the immune system, infect the liver and red blood cells and finally develop into a form that is able to infect another mosquito as feeds on an infected person. Inside the mosquito, the parasite matures until it reaches the sexual stage where it can again infect a human host when the mosquito takes her next blood meal, 10 to 14 or more days later. 4 Inside the human blood, the parasites travel to the liver cells to grow and multiply. At this point, the infected person shows no symptoms. About 8 days to several months later, the parasite leaves the liver cells and enters the red blood cells where they grow and multiply again. Upon maturing, the ruptured red blood cells free the parasites (gametocytes) which go on to attack and enter other red blood cells. Toxins released when the red cells burst is what causes fever, headache, vomiting and other flu-like symptoms. 4 Figure 3 – The Life Cycle of Malaria 1.3 How it kills? 5Malaria kills by infecting and destroying red blood cells (anaemia) as well as clogging capillaries that carry blood to the brain (cerebral malaria) or other vital organs affecting the central nervous system. In the less common blackwater fever it is the haemoglobin from the burst red blood cells that damage the kidney and excreted in the urine causing its dark colour. Without immediate treatment or should the parasites be resistant to them the infection is life-threatening. Figure 2 - The effect of Malaria on blood cells providing anaemia in time. 1.4 Transmission The cycle of transmission carries on only if the female Anopheles mosquito bites an infected person and ingests the ‘gametocytes’. Since the malaria parasite is found in red blood cells, blood transfusion, organ transplant, shared use of blood-contaminated syringes will transmit malaria. A mother can also transmit malaria to her fetus before or during delivery, a condition known as ‘Congenital Malaria’.6 1.5 Why the plague goes on… The epidemic outbreak of malaria is closely linked to the weather, surrounding temperatures, humidity and rainfall. Mosquitoes breed in areas of stagnant water such as swamps which become more pronounced in Africa during the rainy seasons.7 Mosquitoes that transmit the disease are becoming increasingly resistant to insecticides and the parasites themselves are evolving with high resistance to drugs used to treat the disease. Humans are left vulnerable to the disease since there is yet to be a vaccine to build antibodies. Lack of resources and political instability prevents the building of solid malaria control programs in Africa. Lack of funding is key as to why this disease still ravages Africa which is closer examined in the later sections. 5 chapter 2 DRUGS – OUT OF REACH 2.1 VACCINE So near yet so far… A malaria vaccine could help; vaccines are seen as the backbone of public health interventions, especially in poor countries, where they help contain or even eradicate leading killer diseases such as polio, measles and tetanus. A vaccine could significantly improve malaria control, particularly in Africa where the ecological habitat is such that effective mosquito control has proved difficult or impossible to maintain. Intensive research is currently conducted into the vaccine development against both falciparum and vivax malaria. The development criteria require that the antigen serves a function critical to the parasite, is associated with naturally acquired immunity, or is protective in animal models.8 RTS,S/AS02A or Mosquirix is the most advanced pre-erythrocytic vaccine intended to prevent invasion of hepatocytes by sporozoites or to destroy infected hepatocytes. It is a hybrid molecule in which circumsporozoite protein of P.falciparum is expressed with Hepatitis-B surface antigens (HBsAg) in yeast. 9 The vaccine provides short-lived protection in volunteers, exposed experimentally to bites by infected mosquito.10 A trial of RTS,S/AS02A in Mozambican children,11 gave 30% protection against the first clinical episode of malaria and 58% protection against severe malaria. MSP-1 (merozoite surface protein-1) and AMA (apical merozoite antigen)-1 blood-stage vaccines are designed at eliminating or reducing the number of blood-stage parasites.12 A combination vaccine of three blood-stage antigens contributing to erythrocyte invasion reduced parasite density in a strain-specific manner. Unfortunately, it had no pronounced effect on the overall number of clinical malaria episodes.13 These vaccines are currently undergoing trials. Figure 2 - AMA-1 molecular structure segment Transmission blocking vaccines are designed to reduce transmission by preventing mosquitoes from becoming infected from feeding on vaccinated individuals.14 Transmission-blocking vaccines against P falciparum and P vivax are in phase I trials. 6 Vaccines to trigger and boost T cells aims to elicit cytotoxic T cells that can kill malaria parasites in infected liver cells. Unlike red blood cells, liver cells can alert the immune system to the parasite invasion and thereby render themselves targets for killing. This ‘'prime-boost' vaccines involve a two-step procedure in which volunteers are first given a DNA-based vaccine to instruct body cells to produce malaria proteins as if they were infected with the parasite. This first step provides the initial stimulus to T cells that can detect these liver-stage antigen targets. The second step, booster vaccination contains attenuated viruses that carry synthetic portions of various pre-erythrocytic, liver-stage antigens, including CSP (circumsporozoite protein) and also another sporozoite protein known as TRAP (thrombospondin-related adhesion protein). It is capable of recognizing and killing malaria-infected cells. Phase I trials have shown safety and some immunogenicity, Phase IIb trials on adult male Gambian volunteers have not shown significant protective efficacy of such vaccines. Further clinical trials of alternative prime-boost vaccines designed to produce stronger responses are underway.15 Approximately 40 malaria vaccines are now in clinical trials, according to WHO. Some 45 are in preclinical development and about 20 are at the research stage. It has progressed rapidly by the availability of more funds and by improved organisation mediated through organisations such as the Malaria Vaccine Initiative.140 However, it is likely to be at least a decade before an effective vaccine is available for widespread use in malariaendemic countries. Fever, represented as a frenzied beast, and ague, depicted as a blue monster. 1788 2. 2 DRUGS Evolution- from witchcraft to….. For centuries, fever has haunted mankind and in turn mankind came up with ingenious remedies to combat them. In ancient times, vomiting, amputation, limb blood-letting, even skull operations, were tried to treat malarial fever. It finished off sufferers in a fairly short time. In England, they tried opium laced beer with opium grown from local poppies. The help of astrology was also sought as the periodicity of the malarial fever suggested a connection with astronomical phenomena. Believe it or not, many turned to witchcraft. One suggestion by the Dominican scholar Albertus Magnus, was to have insects devour 77 small cakes made from dough prepared by mixing flour with the patient’s urine. For the patient, the remedy was to drink brandy with a concoction of pepper and three drops of cat’s blood from its cut ear. Ironically, the poor who could not afford the help of the medical profession managed to survive! 16 Discoveries It was in the remarkable year of 1820, that a feasible antimalarial drug was isolated by Pelletier and Caventou from the yellow cinchona bark in the form of a sticky, pale yellow gum, which Figure 3 - Cinchona Ledgeriana is non Figure 4 – Cinchona Ledgeriana bark 7 crystallizable. The gum was soluble in acid, alcohol and ether and highly effective against malaria. The four chief alkaloids (a basic compound from amino acid metabolism which usually contains at least one nitrogen atom in a heterocyclic ring) extracted from this Cinchona ledgerian bark are two pairs of diastereoisomers, quinine and quinidine and cinchonidine and cinchonine, the latter pair lacking the 6-methoxy group.17 What’s so great about Quinine or NOT? Quinine (C20H24N2O2) is one of the 36 alkaloids with a structure containing ‘asymmetric’ carbon atoms, which are connected to four different chemical groups and allows the overall structure to be arranged in different ways. Hence, 16 stereoisomers are possible but only one corresponds to the active drug form. Haemoglobin is the main protein inside a red blood cell. The malaria parasite creates a vacuole in the cell where it breaks the hemoglobin down for its own use in building up its own protein for growth. This causes the release of the iron-containing haemo part of the molecule, which could build up and become toxic, so the parasite detoxifies it by converting it into an insoluble form. Quinine interferes with this conversion and the parasite is killed by the buildup of iron compounds. 18It is thought that because the quinine structure resembles DNA bases, it can interfere with DNA replication within the malarial parasite by forming complexes using its flat aromatic rings. Though quinine kills malarial parasites in red blood cells, alleviates fever and is analgesic (pain-relieving), it does not kill the parasites living outside the red blood cells allowing relapses to occur if quinine therapy is halted. 19Resistance to the drug has been reported sporadically in 1844 and 1910; hence, research was initiated to find a quinine substitute. Nonetheless, it still remains an important and effective treatment especially for severe falciparum malaria in most parts of the world. 20The total synthesis of quinine shows how the formation of quinine by oxidation of deoxyquinine with oxygen in tert- butyl alcohol-DMSO, in the presence of potassium tert-butoxide, proceeded selectively, as had been found by the Hoffmann-La Roche group. 21 It was this group that illustrated a number of syntheses of quinine in which the quinuclidine ring was created by forming the bond between N-1 and C-8. That strategy, which may be called the Rabe connection, was endorsed by the workers who followed Rabe, starting with Woodward and Doering, 22 presumably because of the attractive structural simplification it seemed to offer. 8 Current biotechnology has developed a method to produce quinine by culturing plant cells. Grown in test tubes on a special medium containing absorbent resins, the cells can be manipulated to release quinine which is absorbed by the resin and then extracted. This method has high yields but is extremely expensive and fragile. 23 With the advent of World War II, many more drugs were developed to counter the shortage in quinine when Japan invaded Java in 1941 and took most of the supplies. Two main derivatives of quinine are Chloroquine and Mefloquine. CHLOROQUINE: ARALEN™ AN D Chloroquine MEFLOQUINE: L AR I AM ™ Mefloquine These two compounds have similar molecular structure to quinine, composing of two flat aromatic rings, with an offset section. They both have a mechanism of action similar to Quinine, but with their own special ‘something’. In 1934, the introduction of Chloroquine (a 4-aminoquinoline derivative of quinine) by Hans Andersag24 was seen as a breakthrough and this is now regarded as ‘the’ prototype anti malarial drug, most widely used to treat ALL types of malaria infection. It was also the cheapest, time tested and safe anti malaria agent. 9 Technology and the drug’s pathway With improving technology, an electron microscope was used to study the effect of quinolinecontaining drugs on Plasmodium Falciparum. It appeared that the first physical changes were the swelling of the food vacuole and accumulation of undigested hemoglobin. As mentioned above, this vacuole is the site of hemoglobin degradation to provide amino acids for growth, and the drug operates by blocking action of the food vacuole. Chloroquine is a diprotic weak base and is attracted to the acidic pH of the parasite’s food vacuole raising the pH. Once in the vacuole it deprotonates and become membrane impenetrable, accumulating toxic haem in the vacuole-within the parasite.25 THE TARGET The latest research reference 26suggests that the target for drugs to act on is Ferriprotoporphyrin IX (FP), a self-toxic protein involved in the parasite enzyme heme polymerase that converts toxic heme into non-toxic hemazoin (malaria pigment). Chloroquine is effective because it binds to FP and the complex acts as a catalytic poison to the polymerization process and stops the conversion. It operates against asexual forms of pathogenic malaria parasites (called the "haemo-schizontocidal effect"). However, it is inefficient against gametocytes or exoerythrocytic liver forms and induces many side effects. The most serious reaction is pigmentary retenitis with an irreversible loss of visual field; however, this only occurs after an accumulative dose of 1000 mg or more. Nevertheless in Chloroquine sensitive malaria, it reduces the fever and clears blood of parasites within 24 hours. This is a radical cure for P. falciparum infection, but not for P. ovale or P. vivax as there is always an exo-erythrocytic phase in which the hypnozoites may lead to a clinical relapse attack. THE ANTAGONISTIC EFFECT 27 Mefloquine inhibits the uptake of chloroquine in infected cells by blocking ingestion of hemoglobin which in turn disrupts the generation of FP to which chloroquine binds to. This is the antagonistic effect of chloroquine and mefloquine on parasite growth – increased resistance of parasites to chloroquine makes it more sensitive to mefloquine. Mefloquine works well because it interferes with the transport of hemoglobin and other substances from erythrocytes to the food vacuoles of the malaria parasite. Like Chloroquine, 28Mefloquine affects only the asexual form of the parasite with no effect on exo-erthrocytic liver forms or on gametocytes. Resistance has been reported, but if combined with Chloroquine or quinine it is overcome. Mefloquine is a blood schizonticidal of the erythrocytic malaria and will kill hypnozoites if given as a combination treatment with primaquine. Side effects include: vertigo, nausea, vomiting, abdominal pain and diarrhoea. On very rare occasions neuropsychiatric sympto€ms may occur. 10 Yet another to battle Chloroquine resistant-Pyrimethamine/Sulfadoxine Pyrimethamine Sulfadoxine Pyrimethamine and sulphadoxine are adjuncts which are useful for treatment of uncomplicated, chloroquine resistant, P. falciparum malaria. They cause the failure of nuclear division during schizont formation in erythrocytes and liver. 29Pyrimethamine inhibits the dihydrofolate reductase of plasmodia and blocks the biosynthesis or purines and pyrimidines, which are essential for DNA synthesis and cell multiplication. Sulofadoxine inhibits the utilisation of para-aminobenzoic acid in the synthesis of dihydropteroic acid. The combination of pyrimethamine and sulfa thus offers two step synergistic barrier of plasmodial division. However, the side effects of Pyrimethamine are occasional skin rashes and depression of hematopoiesis. Excessive doses can produce megaloblastic anemia. 30Sulfonamides on the other hand, can cause numerous adverse effects such as Agranulocytosis; a plastic anemia; hypersensitivity reactions like rashes, fixed drug eruptions, erythema multiforme of the Steven Johnson type, exfoliative dermatitis, serum sickness; liver dysfunction; anorexia, vomiting and acute hemolytic anemia can also occur. So far, all the drugs discussed all under the category of Blood schizonticidal drugs whereby they act on the blood forms of the parasite and thereby terminate clinical attacks of malaria. These are the most important drugs in anti malarial chemotherapy. The Gametocytocidal Drug These drugs destroy the sexual forms of the parasite in the blood and prevent transmission of the infection to the mosquito. Chloroquine and quinine have gametocytocidal activity against P. vivax and P. malariae, but not against P. falciparum. The main drug is Primaquine. Primaquine (8-aminoquinolines) It is the essential co-drug with chloroquine because it is both gametocytocidal drug as well as a prototype for the tissue schizonticides to prevent relapses. It is highly effective against the gametocytes of all plasmodia and thereby prevents spread of the disease to the mosquito from the patient. 31It is also effective in treating the dormant tissue forms (hypnozoites) of P. Vivax or Ovale malaria in the liver. Once the parasite has been eliminated from the bloodstream, the remaining schizonts must be removed from the liver and this is done by administering a 14 day course of 11 Primaquine. It has insignificant activity against the asexual blood forms of the parasite and only affects the parasite in tissue therefore it is always used in conjunction with a blood schizonticide and never as a single agent. If Primaquine is not administered there is a very high likelihood of a P. Vivax relapse within weeks or months, sometimes even years. The mechanism of action is not well understood, but it may be acting by generating reactive oxygen species or by interfering with the election transport in the parasite. Atovaquone/Proguanil: Malarone™ NH HN CH3 C CH HN C CH3 N H NH HCl Cl Atovaquone Proguanil Hydrochloride This is a prophylactic antimalarial drug; its purpose is to prevent, rather than treat or cure, disease. The difference between this and a vaccine which is also prophylactic is the drug measures are divided between primary prophylaxis (to prevent the development of a disease) and secondary prophylaxis (whereby the disease has already developed and the patient is protected against worsening of this process). A vaccine is used before an illness has developed. 32Proguanil Hydrochloride with atovaquone prevents malaria caused by Plasmodium falciparum. Proguanil Hydrochloride prevents malaria by stopping the parasite from reproducing once it is in the red blood cells. It does this by blocking the action of an enzyme that is found in the Plasmodium parasite. Then, the enzyme dihydrofolate reductase is involved in the reproduction of the parasite by converting folic acid into folinic acid in the parasite, which is a step essential for the parasite to produce new genetic material (DNA). New DNA is necessary for the parasite to reproduce. By blocking its production, proguanil prevents any malarial parasites that have entered the red blood cells from reproducing and increasing in number. Atovaquone also works by interfering with the production of substances needed for malarial parasites reproduction. It works in a slightly different way, but when combined with Proguanil Hydrochloride, it is an effective drug. Proguanil with atovaquone may be particularly useful for preventing malaria in areas where this parasite is known to be resistant to other antimalarial medicines, such as Chloroquine. Some of the 33side effects of this drug include nausea, vomiting, diarrhoea or abdominal pain; fever (pyrexia); headache; inflammation of the lining of the mouth (stomatitis); mouth ulcers; loss of appetite and dizziness. This drug is also unsuitable during pregnancy or breastfeeding as safety has yet to have been established. 12 2.3 THE REMARKABLE CHINESE DRUG ARTEMISININ- The sweet wormwood 34The Chinese call it Qinghao; western botanists dub it Artemisia annua or sweet wormwood. The Chinese have used this to treat fevers for thousands of years but little did they realize that Artemisia held the key to beating malaria. In the 1970s, without the sophisticated knowledge of organic chemistry, Tu Youyou managed to extract a chemical called Artemisinin. In 1979, chemists successfully determined the structure of artemisinin using X-ray crystallographic analysis. They discovered that artemisinin was a sesquiterpene (consisting of three isoprene units and have the molecular formula C15H24) with five oxygen atoms, two of them in a peroxide bridge system over a seven-membered ring and two others in a lactone ring structure. As Artemisinin is highly insoluble in oil and water, it can only be administered orally. Artemisinin’s reaction to malaria was ground breaking. Its mechanism worked with such pace and effectiveness that when the drug encountered the parasite, it immediately acted as a deadly toxin eradicating the parasite from the bloodstream. 35Artemisinin derivatives such as the water soluble ester called artesunate and two oil soluble preparations called artemether and arteether have now been developed. Artemisinin Mode of Action The commonality between Artemisinin and its derivatives is a trioxane pharmacophore containing a peroxide bridge. The peroxide bridge present undergoes reductive scission by low-valency transition metals to generate oxygen-centred radicals. These radicals, due to affinity for hydrogen, might generate carbon-centred radicals and produce an FP=O, leading to an epoxidea highly active alkylating agent. The carbon-centred radicals may alkylate either haemo or other proteins, such as Translationally Controlled Tumor Protein 13 (TCTP) – it still remains unknown. It is also unclear whether haem-bound artemisinin can react with proteins which do not bind to haem.36 In fact, there are loopholes with the carbon-centered radical theory. It is common in reductive cleavage of endoperoxides but not linked with antimalarial activity. Radical proteins are short lived – they do not survive to even reach the target molecules. With that, comes yet another proposal. 37The trioxane pharmacophore acts as a source of hydroperoxide by generation of an oxo-stabilised cation upon heterolyisis of the C3-O2 bond. By reduction, an electrophilic oxygenating species or hydroxyl and alkoxyl radicals would be capable of hydroxylating biomolecules or abstracting hydrogen atoms. Nonetheless, the true mode of action is still being investigated. As for now, a simple explanation would be the two oxygen atoms forming the epoxide bridge reacts with the detoxified iron compound and releases free radicals which damage proteins produced by the malarial parasites. It also disrupts the normal function of the electron transport chain within mitochondria. This exploits the difference between the human red blood cell - which does not need to produce proteins and also does not contain mitochondria - and the malarial parasite - which needs both. 38The WHO accorded high priority to the development of fast acting, effective artemisinin derivatives drugs for the treatment of cerebral malaria as well as for the control of multi-drug resistant P. falciparum malaria. WHO lists in its 2005 malaria control guide the following advantages of artemisinin derivatives: Rapid reduction of parasite densities; rapid resolution of clinical symptoms; effective action against multi-drug resistant P. falciparum; no documented parasite resistance to artemisinin and its derivatives; few clinical adverse reactions; and reduction of gametocyte carrier rate, which may reduce transmission (i.e., fewer of the parasite’s gametocytes within an infected person lowers the probability of a biting mosquito becoming a carrier). They highly recommend combination therapy that includes artemisinin drugs as the standard treatment in countries where malaria is resistant to the older individual drugs such as Quinine and Chloroquine. ACT A combination of artemisinin derivatives with another effective antimalarial medicine is called artemisinin-based combination therapy (ACT) and is currently the most effective medicine available to treat malaria. The total effect of artemisinin combinations (which can be simultaneous or sequential) is to reduce the chance of parasite recurrence, improve cure rates, and prevent transmission. 39Studies have revealed high levels of resistance to chloroquine and sulfadoxine-pyrimethamine of up to 78%. In the few areas where amodiaquine and sulfadoxinepyrimethamine remain effective, they can be partnered with artemesinins as artesunate-amodiaquine and artesunate/sulfadoxine-pyrimethamine combinations. Where parasite resistance to these partner drugs has built up, artemether-lumefantrine or artesunate-mefloquine is more successful. Artemisinin based combinations Artesunate + Chloroquine Artesunate + Amodiaquine Artesunate + Mefloquine Artesunate + Sulfadoxine/Pyrimethamine (SP) 14 Artemether + Lumefantrine (Coartem,TM RiametTM) To optimize cure rates, four particularly challenging requirements must be fulfilled: the entire course of treatment must be completed by patient; the drugs need to be good-quality; they also need to be appropriately selected; and the vast majority of malaria infections need to be treated with ACTs. Uganda- doing it THEIR way! For centuries, Ugandans have used herbs to treat the symptoms of malaria. Effective as it has been, it has not gone through any safety tests. These traditional anti-malaria ‘drugs’ are derived from three plants: ⊱ Aristolochia elegans, known locally as kapapula or 'little paper' ⊱ Vernonia amygdalina, commonly known as mululuza ⊱ Artemisia annua, introduced to Africa from its native Asia Jar of seeds and tree bark used in African Traditional Medicine 40Along with HIV/AIDS, malaria is widespread in Uganda — so common it is accepted as ordinary to be infected by either. Nambatya, director of research at the state-run Natural Chemotherapeutic and Research Laboratory (NCRL) says the remedies "clearly treat malaria", and explains that tests on people who have used them have shown that they do rid the parasite. The aim is to scale up extraction of key components from herbs that prove to be safe and effective and to mass-produce remedies based on them, so that they may be sold cheaply while retaining their quality. Eventually, they might even be exported to other needy countries. “To be inflicted with malaria is considered normal and to go to a burial as a result is thought normal too, but we have to reject this situation because we do not have to be so sick or die so ” prematurely in such large numbers. -Jim MuhzewiUganda Minister of Health 15 2.4 DRUG RESISTANCE – greatest threat to malaria control! Drug resistance has been confirmed in 2 out of 4 of the human malaria parasites, Plasmodium falciparum and P. vivax. Drug-resistant Plasmodium falciparum 41In the late 1950’s and early 1960’s, Chloroquine was resistant to the P.falciparum and since then, it has only gotten worse with the resistance spreading to nearly all areas of the world where P.falciparum malaria is transmitted. As other drugs were developed to overcome chloroquine’s resistance, P. Falciparum eventually developed resistance to them as well. They are sulfadoxine/ pyrimethamine, mefloquine, halofantrine, and quinine. In Africa, chloroquine resistance was first documented in Tanzania in 1979 and has spread and intensified in the last 20 years. In most countries of East Africa and in Ethiopia more than 50% of patients currently experience a recurrence of parasitaemia with symptoms by day 14 after treatment. In some areas of the world, this would cause an extensive impact on the multi-drug resistant malaria. Drug-resistant Plasmodium vivax In 1989, Chloroquine resistant P. vivax malaria was identified among Australians living in or traveling to Papua New Guinea. Now, all over Southeast Asia, on the Indian subcontinent, and South America have all been affected. Nearly 50% of strains from these areas currently show evidence of reduced susceptibility in 28-day in vivo tests. Particularly in Oceania, Vivax malaria exhibits decreased susceptibility to Primaquine. Tests for Drug Resistance The four basic methods are: i. 42 In vivo tests: Patients with clinical malaria are given a dose of an antimalarial drug and are observed and monitored over time for any signs of reappearance of parasites or failure to clear parasites. ii. 43 In vitro tests: Blood samples are taken from malaria patients and the malaria parasites are exposed to different concentrations of antimalarial drugs in the laboratory. One method is by adaptation of parasites to culture first, and the other, the blood from patients is directly put into the test system. iii. Molecular characterization: Molecular markers of P. falciparum that confer resistance have been identified for some drugs like chloroquine, SP, atovaquone and cycloguanil), whilst for others, they are yet to be determined. Molecular techniques such as polymerase chain reaction (PCR) or gene sequencing can identify these markers in blood taken from malaria patients. iv. Animal model studies: These tests allow for the testing of parasites which cannot be adapted to in vitro enviroments (provided a suitable animal host is available) and the testing of drugs not yet approved for use in humans. [This is not routinely done compared to the other 3 tests] 44 16 Chapter 3 THE LIFEBLOOD OF ECONOMICS Some say Malaria is like the ‘silent tsunami’. Ironically, the distressing statistical death toll rises every year and millions of cases are audible enough to many- as are the economic costs, by WHO. Malaria and poverty are intimately connected. 46T.H. 45estimated at US$12 billion per annum Weller, a Nobel laureate in medicine, once said, ‘It has long been recognized that a malarious community is an impoverished community.’ The risk of malaria has always been geographically specific as is poverty. Almost all rich countries are outside the bounds of the killer Sending a clear signal to the world community: No money-no drugs. The Players Malaria sufferers Pharmaceuticals The players all play a part in the fight against malaria. Some may be complacent, Scientists Non-profit organizations Malaria but others try their best. The economic implications all draw the players together and in some way or another they are all linked. Countries Philanthropists 3.1 The ARTEMISININ DRUG Drawbacks, drawbacks, drawbacks Artemisinin is isolated from Artemisia annua- a plant that takes up to 18 months to get from seed to pill. This lengthy period makes it very difficult to secure the drug, resulting not only in delays and shortages but in making scale-up production a highly costly venture. The World Health Organisation (WHO) estimates the world will need 132million courses of ACT treatment (which cost up to $2.40 each) in 2005 – a four-fold increase over 2004 – and almost eightfold in 200647. In fact, at $2.40, it is at least 10 times more expensive than other anti-malarial drugs. As effective as ACTs are where extensive tests have proven effectiveness of more than 90%, they do have a number of drawbacks. Since 2001, the WHO has recommended that countries where drug resistance occurs to switch to ACT. Unfortunately, international efforts were sluggish until early 2004, when a stinging paper published in the Lancet accused the WHO and the Global Fund to Fight AIDS, Tuberculosis and Malaria of “ medical malpractice” for 17 continuing to approve and fund proposals from poor countries to treat malaria using older, cheaper drugs even though it may be less effective than of ACT. Getting countries to switch to ACT is merely a question of securing drugs. Doctors need proper training on how to use and administer them and surveillance systems have to be set up to monitor resistance. One project aimed at addressing these problems attempts to engineer an artificial artemisinin. OneWorld Heath, a California-based nonprofit pharmaceutical company, is using technology developed at the University of California, Berkeley (which granted royalty-free licenses to the company) to create the drug. 48With a $42 million grant from the Bill and Melinda Gates Foundation, OneWorld Health over the next five years will use synthetic biology technology to try to lower the price from $2.40 to $0.24 per treatment. In fact, Chinese firms such as Guilin Pharmaceuticals are also trying to cultivate the plant – both on their own plantations and through contracts with local farmers, rather than relying on wild leaves. The cost of Artemisinin treatment threatens to undermine not only the OneWorld Health effort, but the very effectiveness of artemisinin itself. This has proliferated the counterfeiting trade of ACT in Southeast Asia where fraudulent treatments contain minute amounts of artemisinin. This negligible amount fools simple dye authenticity tests. Paul Newton of Oxford University emphasizes that a diluted treatment is by no means a cure. "This would be a disaster for malaria control globally,” Newton has said in a number of publications. "We may have malaria that could not be treated in any affordable way." Medicines for Malaria Venture (MMV) has set the goal of registering at least one new effective and affordable drug before 2010 as a means of avoiding such a disaster. An optimistic J Carl Craft, MMV’s chief scientific officer, has said that he expects to have one or two new combination drugs by 2007 and as many as three or four by 2010 to meet any change in resistance patterns.49 3.2 THE VACCINE Scientists are optimistic as prospects for a malaria vaccine have been boosted by “tantalising” results from trials on children in Mozambique in 2000 which investigators reported in an article in the Lancet, a British medical journal.50 The big question though, is how these new vaccines will be introduced in low income countries and how long it will take regulatory authorities to approve them? These two other hurdles need to be overcome in order for these vaccines to get to the people who need them most as quickly as possible. The discovery of a successful and effective vaccine is the best chance of sending the disease into retreat, however hopes for that fall as quickly as they rise. Therefore, as a result of this, research into malaria receives only some $60million a year, compared with $140million for asthma, $300million for Alzheimer’s disease and $950million for AIDS. 51 Malaria Vaccine Initiative (MVI), a non-profit organization, coordinated and funded the trials conducted by researchers from GlaxoSmithKline (GSK) – the world’s second largest drug company, the University of Barcelona 18 and Mozambique’s health ministry. GSK which own the Mosquirix (RTS,S/AS02A) vaccine has said it will make it for the public sector but since it is so costly, and as the vaccine is not suitable for the more lucrative travelers’ market, the company will need assurances that rich countries will buy it for poor ones. The Bill and Melinda Gates Foundation gave a $108 million grant in November 2005 to support clinical development of the vaccine but at 1/10 th of the research money of AIDS, much more is required 52 3.3 POVERTY – the driving force of parasitic infection A WHO report pointed out that various economic analyses show that malaria is not only the product of poverty; they also create poverty. 53"You don't need to sustain it (donations from wealthy countries) indefinitely...Healthy people can get themselves out of poverty," said David L. Heymann, head of communicable disease programs at WHO. The scale of carnage wrought by malaria in Africa afflicts a hundred times more people than it kills - the cost of treatment impoverishes those who could initially afford it, and those who are already impoverished are left to knock on death’s door. African’s health budget is minuscule- they do not have enough money to fight this disease. The anti-malarial drugs are inaccessible and unaffordable leading to a limited access of drugs and a very small percentage of children who need treatment actually get it. There is also the problem of a dis- regulated with counterfeit drugs on offer, so environment is very poor and very often the drug taken is not what they think it is. The country itself does not have sufficient income to bring in the effective drugs that have proved useful against multi the system regulatory drug resistant strains. In fact, it would be some time before such drugs or vaccines will be widely available in Africa due to low production, comparatively costs, dosing complexity and the lack of clinical experience - all of high which is due to poverty one way or another. Africa does not have money set aside for research development, and hence, it is up to the developed nations for aid and research funding to help find a cure and save millions of lives. The lack of research capacities leads to severe constraints in Africa. Time and time again, we come across the issue of poverty, since many of the interventions required are simply unaffordable. There are many constraints to ideal control measures of a severe disease such as malaria – this in the form of strong infrastructures in place for immediate treatment, referral to more detailed medical care and ultimately, hospital-based management. Underdeveloped health care services and severe shortages of trained staff to administer treatments continue to be one of the key underlying failures of the African healthcare system. Health and wealth are inextricably linked. A malaria sufferer would not only be spending accumulated wealth on treatments but loss in productivity would also cause the economy to suffer. Its mind boggling how so little has been done to curb it. 19 3.4 Lacking Investment The global burden of malaria is unevenly distributed with malaria-endemic countries like Africa absorbing large economic and social penalties. Studies have shown that the growth rate of per capita gross domestic product (GDP) in countries with malaria is markedly lower than those countries that are malaria free. The difference appears modest – malaria-endemic countries have a rate of between 0.25% to 1.3% lower than non-malarial countries but when extrapolated over a 25 year period, this difference adds up to almost half the per capita GDP of poor countries.54 Richard Feachem, executive director of the Global Fund to Fight AIDS, Tuberculosis and Malaria, has said that he is convinced that the Millennium Development Goals (MDG) target of halting and reversing the incidence of malaria may only actually be achievable by 2015. Experts beg to differ, saying that malaria research and development receiving inadequate funding to ensure the MDG will be met. It somehow seems that donations by The Gates Foundation are the only factor making a difference. The New York Times, published on the 25th of April 2006, reported that the World Bank has failed to follow through on its pledges to spend up to $500 million to combat malaria. Public health experts writing inThe Lancet claims that they have allowed the staff working on the disease to shrink to zero, used false statistical data to claim success and wasted money on ineffective medicines whilst recommending that the bank should relinquish the money it has to fight malaria and reduce mortality and it be put to more effective uses.55 Even diabetes’s burden to society which is about one-third of that of malaria Problem of money which is given to charities ends up in the hands of the government gets nearly six times more money for R&D. 3.5 Pharmaceutical Companies Lives should come before profit shouldn’t they? Malaria is neglected by the pharmaceutical industry because there is more money to be made from other more ‘lucrative’ disease. Without commitment to strengthening malaria vaccine research capacity, an effective malaria vaccine may never be produced and tested, or, if it is, may even benefit the Africans who need it most. For example, pharmaceutical companies target tourists and provide them with more lucrative malaria vaccines rather than the inhabitants of developing countries who cannot afford them. Profit driven pharmaceuticals therefore,have very little incentive to research a vaccine or drug for a disease that affects mainly the poor resulting in them missing out on breakthroughs. “Although the technology is there it is not affordable by majority of our people," says a paediatrician in a research institute in Nairobi. 20 Evidence: A highly effective drug – Coartem –recommended by the Ministry of Health as a drug of choice and currently in the market, but not accessible at public hospitals. Where it is available though, the poor are definitely locked out. Dr Wellington Muiruri of Novartis Pharmaceuticals – manufacturers of Coartem – made an agreement with WHO to supply the drugs to the government, on one condition. The drugs have to be offered free of charge to the public. Those who can afford the drugs could obtain it from the private sector. So, the question is why has the state not stocked them in government hospitals? The answer to that is the government, without donor assistance cannot buy the drugs for free distribution. , hence, Africans can say goodbye to effective drugs. Without organizations like the Bill and Melinda Gates Foundation who have generously sponsored some encouraging research, Africa’s population would deplete and no one would care! 3.6 TAXATION- making things worse There are several proven, cost effective techniques for curbing malaria, none of which is as widely used as it should. One example is the Insecticide-treated bed net. In 2002, the government of Malawi launched one of the largest insecticide-treated bed net (ITN) distribution programmes in Africa. ITNs were subsidised to the highest levels possible and distributed through child health clinics, community networks and the private sector. The programme proved to be successful to a significant degree and reduced the number of people infected with malaria. So why is it that those who live in some of the most isolated and malaria-infested areas are still unable to buy ITNs, despite the reduced prices? That is because these ‘reduced’ prices are still too expensive! Although nets have grown cheaper in the recent years, they still cost about $5 each – equivalent to as much as a typical African country spends on health care, per person per annum! Malaria prone countries need to abolish taxation on bed nets because as it is, they might not even be able to pay for them even if it were tax free. In fact, they should give it out for free! African governments should realise that making life-saving devices more costly is hardly a rational health policy. Their argument against subsidising ITNs has been that subsidies could not be sustained unless rich nations were prepared to provide funding indefinitely.56 21 3.7 MONOPOLY– developed countries It cannot be denied that developed countries have the upper hand in terms of research, pre-clinical research and early phases of clinical trials. This headstart allows for them to gain academic accolades with their research published and products patented quickly. African institutions lack the necessary facilities and expertise with African researchers and study participants finding themselves out in the cold. Researchers in Africa may be forced to take on the later stages of research which are highly demanding but less rewarding academically. Along with study participants, they may be excluded from patent negotiations. At the end of the day, products may never become available to people on whom it was tested. 57 3.8 African Scientists What is holding Africa back? Research has two driving forces: the quest for basic knowledge, and the need to use scientific understanding to improve our lives. Are African researchers trained to ask the right questions? Before there even is research there has to be researchers. Being faced with rising debt, struggling healthcare systems and food shortages, many African governments rank scientific research — even for a disease of such magnitude as malaria — the lowest on their list of priorities. This lack of support means that researchers often battle with basic infrastructure problems such as frequent power cuts and poor access to water and electricity. Without these improvements, many observers fear the competent researchers would leave the continent, taking vital knowledge and experience with them. “As we see more and more drugs and vaccines that need to be tested in African populations, the presence of well-trained African scientists could become the critical factor in their success or failure,” said Ogobara Doumbo, director of the Malaria Research and Training Centre at the University of Bamako in Mali. Apart from that, experts are also concerned about the deaths of malaria researchers in Africa. 58In 1999, there were only 752 trained malaria researchers in sub-Saharan Africa, according to the Multilateral Initiative on Malaria (MIM). Unfortunately however, very few of them are experienced at preparing research proposals and protocols, mobilising money, acting as consultants, networking with the scientific, health and donor communities, or liaising with policy and decision makers. Malaria researchers in Africa must not simply sit back and wait for a malaria vaccine to appear. They must become fully familiar with the scientific advances, and establish early collaborative links with malaria vaccine developers. 22 Chapter 4 THE TOMORROW OF TODAY 59In “The simplicity of the theory of malaria this final chapter, we examine the prospects for malaria eradication and how much, or how little it has changed in the three or more decades since Hackett’s cry of exasperation. control is surpassed only by the difficulties ” involved in its application. In terms of antimalarial drugs and the development of resistant strains of malaria parasites, a number of single drugs and drug combinations -L.W.Hackett (1937)An Ecological Study are available to treat and prevent infections with such strains. Unfortunately, the ‘ideal drug’ which is a good and safe anti-relapse agent with complete curative action, sporontocidal activity, low toxicity, prolonged action, little liability to produce resistance, palatability and low cost is unlikely to be forthcoming. The rapid expansion in parasite biochemistry may well allow the development of a rationale or the design of new drugs with the involvement of universities. Dr. Oliver Bilker from the Divison of Cell and Molecular Biology at Imperial College and the biological science team are investigating the key life cycle in the malaria parasite and studying a number of parasite gene family which are involved in regulating the calcium- dependent protein kinase 4 (CDPK4) - a molecule found in plants. By doing so, they will be one step closer in identifying the drug targets. “There is a high potential that the drugs needed may be found in the environment ” itself. As for now, drug combinations will probably continue to stem the tide for the next decade until new drugs become available. -Dr. Oliver Billker- 4.1 The Role of Vector Control Drugs can only do so much, but when they fail, other options become a possibility. The major weapon in the fight to reduce transmission to the anopheline vectors is spraying with residual insecticides. New insecticides of all types continue to be developed to cope with the DDT-resistant strains. Carbamate Figure ? : DDT and organophosphate insecticides were introduced and thought to be comparatively free from the resistance liability associated with DDT. Indoor residual spraying (IRS) does not directly prevent people from being bitten by mosquitoes. Rather, it usually kills mosquitoes after they have fed, if they come to rest on the sprayed surface, thus preventing transmission 23 60DDT of infection to other people. However, was banned in the United States in 1973 due to its high toxicity especially to fishes, although it is still in use in some other parts of the world. Another major intervention in malaria control is the Insecticide treated bed nets which provide protection by killing mosquitoes and other insects. They have repellent properties that reduce the number of mosquitoes that enter the house and attempt to feed on humans. 61The government is trying to achieve high community coverage so as to reduce the numbers and longevity of mosquitoes. When this happens, all members of the community will be protected, regardless of bed net ownership. In Chapter 1, we discussed on why the plague goes on. We saw that it was because there were habitats for mosquitoes to breed and now, a method of source reduction or larval control is aimed at destroying the larval habitats by filling depressions that collect water, by draining swamps or by ditching muddy areas to remove standing water. Container-breeding mosquitoes are particularly susceptible to source reduction as Mosquitoes that breed in irrigation water can be controlled through careful water management. People can be educated to ensure standing water in cans or rain barrels are covered. 4.2 Reaching out to lend a helping hand “We do not have the money, the 62Those manpower or the health facilities to protect people as we would like to do. ” -Dr. Samuel MabundaMozambique’s Health Ministry Official words of Dr. Samuel Mabunda can all change with the help of developed countries; one of it being Britain. British Chancellor of the Exchequer, Gordon Brown, was very much aware that there were insufficient funds to make sure the vaccine goes into commercial production and was affordable to the world’s poorest countries like Africa. 63He then made the statement “I can announce that the British government, working with other governments, is ready to enter into agreements to purchase these vaccines in advance to ensure a secure market and that the vaccines are available more cheaply." With scientists confident that the new vaccine may be able to protect a significant proportion of children against the mosquito-borne disease, Africa can be hopeful of malaria free future. GSK says its vaccine could reach the market in 2010, if it is successful in a final round of large-scale clinical testing. 64On June 30, 2005, President Bush announced the President’s Malaria Initiative (PMI), a U.S. government program designed to cut malaria deaths in half in target countries in sub-Saharan Africa. To make this a reality, the President pledged to increase U.S. funding of malaria prevention and treatment in sub-Saharan Africa by more than $1.2 billion over 5 years. Other donors;, 24 foundations; and private, public, and voluntary organizations were called on to complement the U.S. commitment by providing additional funding. They work together with Roll Back Malaria among many others with their goal being partnership and raising awareness. 65RBM was launched in 1998 by the World Health Organization (WHO), the United Nations Children’s Fund (UNICEF), the United Nations Development Programme (UNDP) and the World Bank. The RBM Partnership’s goal is to halve the burden of malaria by 2010. 25th of April is a very special day for Africans. It is the Africa Malaria Day and this event is commemorated every year offering an annual opportunity to raise the world’s awareness of Africa’s fight against malaria. It is also an occasion to take stock of the situation, midway toward the goal of 2010. 25 Conclusion My perceptions and views when I embarked on this dissertation are no different from what it is now, following more in-depth research and analysis into this topic. There is no one enemy to point your guns at, but a host of contributory factors, some easily corrected, and others, a more daunting challenge. I still believe that not nearly enough has been done by the different parties involved, when there is still much more room for improvement. There are still hard truths that have to be faced. The wily Plasmodium remains extraordinarily adept at evading the effects of toxic chemicals and will continue to present the chemotherapist with one of his greatest challenges. A malaria vaccine may ultimately be the greatest promise as it would break the cycle of transmission and possibly achieve a global state of anophelism without malaria that exists only in certain parts of the world. Nonetheless, Africa has to realize that they need to take responsibility and play its part before seeking any assistance, which at the moment has to expect. Incompetence and complacency has to be eradicated. Education and pro-active involvement by the government should be priority. It is clearly essential to balance the probable benefits of eradication of malaria, in terms of improvement in health and economic advancement, against the cost in human resources and money. The events of the last two decades have served to teach that neither the parasite nor the vector keeps to the status quo; they remain flexible, and the successful drugs of today are invariably the failures of tomorrow. Malaria remains a formidable global problem. Nevertheless, success has been achieved in some African nations; there is no reason why others cannot achieve the same. Millions are suffering and dying, the plague raging on. ф Don’t let the innocent and helpless be a victim of this apocalypse. ф Don’t let 2 people die every minute, leaving 3000 African lives perished by the end of the day. ф 26 We can make a difference - 27 we have to act now ! References 1 http://www.malaria-vaccines.org.uk/1.shtml 2 A.J. Knell, 1991, Malaria – The tropical programme of The Wellcome Trust, Oxford University Press. 3 http://malaria.who.int/cmc_upload/0/000/015/372/RBMInfosheet_1.htm 4 http://www.cdc.gov/malaria/biology/life_cycle.htm 5 A.J. Knell, 1991, Malaria – The tropical programme of The Wellcome Trust, Oxford University Press. 6 http://www.cdc.gov/malaria/faq.htm 7 Nature 427, 690 - 691 (19 February 2004); doi:10.1038/427690b 8 Greenwood B, Alonso P. Malaria Vaccine Trials. Chem Immunol 2002; 80: 366-395. 9 Stoute JA, Slaoui M, Heppner DG, et al. A preliminary evaluation of a recombinant circumsporozoite protein vaccine against Plasmodium falciparum malaria. N Engl J Med 1997; 336: 86-91. 10 Kester KE, McKinney DA, Tornieporth N, et al. Efficacy of recombinant circumsporozoite protein vaccine regimens against experimental Plasmodium falciparum malaria. J Infect Dis 2001; 183: 640-647 11 Alonso PL, Sacarlal J, Aponte JJ, et al. Efficacy of the RTS,S/AS02A vaccine against Plasmodium falciparum infection and disease in young African children: randomised controlled trial. Lancet 2004; 364: 1411-1420. 12 World Health Organization. Portfolio of candidate malaria vaccines currently in development. October, 2004 13 Genton B, Betuela I, Felger I, et al. A recombinant blood-stage vaccine reduces Plasmodium falciparum density and exerts selective pressure on parasite populations in a Phase 1–2b trial in Papua New Guinea. J Infect Dis 2002; 185: 820-827. 14 Kaslow DC. Transmission-blocking vaccines. Chem Immunol 2002; 80: 287-307. 15 http://www.scidev.net/dossiers/index.cfm?fuseaction=policybrief&policy=83&section=536&dossier=23 16 http://www.wellcome.ac.uk/en/malaria/MalariaAndControl/chist1.html 28 17 Roger M. Pinder, 1973, MALARIA- The design, use, and mode of action of Chemotherapeutic Agents, Bristol: Scientechnica Ltd. 18 R.B. Woodward and W.E. Doering, J. Am. Chem. Soc., 1945, 67, 860 19 http://www.malariasite.com/malaria/history_treatment.htm 20 The First Stereoselective Total Synthesis of Quinine, J. Am. Chem. Soc. 2001, 123, 3239-3242 21 Uskokovic´, M.; Gutzwiller, J.; Henderson, T. J. Am. Chem. Soc.1970, 92, 203. 22 Woodward, R. B.; Doering, W. E. J. Am. Chem. Soc. 1944, 66,849 23 http://www.malariasite.com/malaria/history_treatment.htm 24 http://www.cdc.gov/malaria/history/index.htm 25 (http://www.tcd.ie/tsmj/2003/antimal.htm) 26 Ferriprotoporphyrin IX: a mediator of the antimalarial action of oxidants and 4-aminoquinoline drugs. Prog Clin Biol Res. 1984;155:119-30. 27 Olliaro P. Mode of action and mechanisms of resistance for antimalarial drugs. Pharmacology and Therapeutics 2001; 89(2): 207-219. 28 Olliaro PL, Haynes RK, Meunier B, et al. Possible modes of action of the artemisinin-type compounds. Trends in Parasitology 2001; 17(3):122-6. 29 East African Network for Monitoring Antimalarial Treatment (EANMAT). The efficacy of antimalarial monotherapies, sulphadoxine-pyrimethamine and amodiaquine in East Africa: implications for sub-regional policy. Trop Med IntHealth 2003; 8: 860-867. 30 http://www.rxlist.com/cgi/generic3/fansidar_ad.htm 31 http://www.rbm.who.int/cmc_upload/0/000/014/923/am2_1-9.htm 32 http://us.gsk.com/products/assets/us_malarone.pdf 33 http://www.rxlist.com/cgi/generic2/malarone_ad.htm 34 The Economist- Science and Technology, Treating Malaria, 18th Novemeber 2004, Beijing and Guilin 35 White NJ, 1999, et al. Averting a malaria disaster. Lancet ;353:1965–1967 36 Olliaro P. Mode of action and mechanisms of resistance for antimalarial drugs. Pharmacology and Therapeutics 2001; 89(2): 207-219. 29 37 Famin O, Ginsburg H. Differential effects of 4-aminoquinoline-containing antimalarial drugs on hemoglobin digestion in plasmodium falciparum-infected erythrocytes. Biochemical Pharmacology 2002 ; 63(3):393-8. 38 http://www.irinnews.org/webspecials/malaria/51345.asp 39 http://www.doctorswithoutborders.org/publications/ar/i2002/goodmedicine.cfm 40http://www.scidev.net/dossiers/index.cfm?fuseaction=dossierReadItem&type=2&itemid=356&language=1&dossier =23 41 42 Peter B. Boland, 2001, Drug Resistance in Malaria, WHO/CDS/CRS/DRS/2001.4 White NJ, 1997, Assessment of the pharmacodynamic properties of antimalarial drugs in vivo. Antimicrobial Agents and Chemotherapy, 41: 1413-1422 43 Rieckmann KH, 1978, et al. Drug sensitivity of Plasmodium falciparum. An in-vitro microtechnique. Lancet 1:22–23 44 http://www.cdc.gov/malaria/drug_resistance.htm 45 The Africa Malaria Report 2003, WHO/UNICEF, http://childinfo.org.areas/malaria 46 Quoted in John Luke Gallup and Jeffrey D. Sachs, The Economic Burden of Malaria 1 (Center for Intl. Development at Harvard University, CID Working Paper No. 52 (2000), http://www2. cid.harvard.edu/cidwp/052.pdf. 47 www.economist.com/displaystory.cfm?story_id=3398810 48 Science and Development Network News; 22nd December 2004 49 http://www.irinnews.org/webspecials/malaria/51336.asp 50 http://www.irinnews.org/webspecials/malaria/51336.asp 51 www.economist.com/displaystory.cfm?story_id=154443 52 www.economist.com/displaystory.cfm?story_id=5165423 53 http://www.psi.org/news/021502d.html 54 http://www.irinnews.org/webspecials/malaria/51346.asp 55 http://query.nytimes.com/gst/fullpage.html?sec=health&res=9DO 30 56 http://www.nationmedia.com/dailynation/nmgcontententry.asp?premiumid=0&category_id=30&newsid=20928 57 http://www.scidev.net/dossiers/index.cfm?fuseaction=dossierreaditem&dossier=23&type=3&itemid=452&language= 1 31 Bibliography 1. Michael F. Good, Allan J. Saul, Molecular Immunological considerations in Malaria Vaccine development. 2. 1990, Malaria and the Red Blood Cell, Vol. 16, No.2/3 3. 1951, Recent Research in Malaria, Vol. 8, No. 1 4. R. Stephen Philips, Malaria Studies in Biology, No. 152 5. P. Perlmann, H. Wigzell, Malaria Immunology 6. W.H. Wernsdorfer, Sir I. Mc Gregor, Malaria (Principles and Practice of Malarialogy), Vol. 1 &2, pg. 1263 7. Malaria - Epidemiology, Chemotherapy, Morphology & Metabolism 58 http://www.irinnews.org/webspecials/malaria/51336.asp 59 Roger M. Pinder, 1973, MALARIA- The design, use, and mode of action of Chemotherapeutic Agents, Bristol: Scientechnica Ltd. 60 http://www.chem.ox.ac.uk/it_lectures/chemistry/mom/ddt/ddt.html 61 Centers of Disease Control and Prevention, http://www.cdc.gov/malaria/control_prevention/vector_control.htm 62 BBC News, 26th November 2001, http://news.bbc.co.uk/1/hi/world/africa/1677073.stm 63 BBC News, 24th November 2004, http://news.bbc.co.uk/1/hi/uk_politics/4038377.stm 64 Centers of Disease Control and Prevention, http://www.cdc.gov/malaria/cdcactivities/presidential_initiative.htm 65 The Roll Back Malaria Partnership, http://www.rbm.who.int 32