static and dynamic balance performance in children with

Balance Performance in Developmental Disabilities
STATIC AND DYNAMIC BALANCE PERFORMANCE IN CHILDREN WITH
DEVELOPMENTAL DISABILITIES:
Anne Wildekamp a
Marina Schoemaker a
and Libbe Kooistra b a Centre for Human Movement Sciences, University Medical Centre Groningen, University of Groningen,
The Netherlands b Departments of Paediatrics and Community Health Sciences, University of Calgary and Behavioural
Research Unit, Alberta Children’s Hospital
ABSTRACT
The main purpose of this study was to investigate whether children with developmental coordination disorder (DCD) combined with reading disabilities
(RD) differed in their balance performance from children with DCD only or RD only. A total of 41 children between 9 and 13 years old (27 children with developmental problems and 14 control children) participated. To evaluate functional motor competence, the Movement Assessment Battery for Children
(M-ABC) was used. A static balance task and a balance perturbation task were administered to examine balance control abilities in more detail. On the M-ABC, the performance of the DCD/RD group was poorer on the balance subtest than that of the RD group. On the experimental static balance task the DCD only group performed more poorly than the RD only group when at least one of their sensory inputs (i.e., vision, feeling from feet) was disturbed. No pronounced differences were found between the groups on the balance perturbation task. The results of the present study suggest that children with DCD may evidence a deficit in sensorimotor function.
Keywords: developmental coordination disorder; reading disabilities; attention deficit hyperactive disorder; static and dynamic balance; sensorimotor organization;
INTRODUCTION
Many of the motor symptoms seen in children with Reading Disabilities (RD) and
Attention Deficit Hyperactive Disorder (ADHD) are similar to those found in children with Developmental Coordination Disorder (DCD). This has prompted a debate regarding the amount of overlap between these disorders in terms of motor impairment. Some researchers suggest that the motor clumsiness seen in DCD, RD and ADHD merely reflects a heterogeneous neurodevelopmental condition (Kaplan, Wilson, Dewey, &
Crawford, 1998). Others emphasize the possibility that different underlying deficits may be responsible for the motor deficits seen in the disorders (Sugden, 2006). As yet, no convincing support for either standpoint has been put forward. What is thus needed is a further delineation of the common or separate aspects of motor control underlying the motor deficits in children with DCD, RD or ADHD.
1
Balance Performance in Developmental Disabilities
To our knowledge, while motor competence studies including children with combined DCD, RD and ADHD are non-existent, a few studies have been published in which a combined DCD and RD group was included. Smits-Engelsman, Wilson,
Westenberg and Duysens (2003) found that aiming movements in children, especially those with both DCD and RD, were typically characterized by under- and over-shoots
(i.e., dysmetria). Fine motor problems in children with combined DCD and RD were also observed by Jongmans, Smits-Engelsman and Schoemaker (2003). Most importantly however, with regard to the topic of the current study, Jongmans et al. (2003) found that these children were especially affected in their balance skills. Both the dysmetria and the balance problems in the studies of Smits-Engelsman et al. (2003) and Jongmans et al.
(2003) were interpreted as a possible sign of cerebellar dysfunction. This view was essentially substantiated in a recent study aimed at differentiating children with DCD, RD and combined DCD and RD in terms of cerebellar functioning using a motor learning paradigm (e.g., prism adaptation) (Brookes, Nicolson, & Fawcett, 2007). Of notice however, was that, unlike the Smits-Engelsman et al. (2003) and Jongmans et al. (2003) studies, all children in the Brookes et al. study (2007) were similarly affected in their task performance, suggesting cerebellar involvement in both DCD and RD. Nevertheless, unambiguous evidence for the exact involvement of the cerebellum in combined
DCD/RD and/or co-existing ADHD is lacking.
Support for the cerebellar hypothesis of RD as a single deficit has come from both structural (Finch, Nicolson & Fawcett, 2002) and functional neuroimaging studies
(Nicolson, Fawcett, Berry, Jenkins, Dean, & Brooks, 1999) as well as from behavioural studies using tasks designed to examine the functional correlates of cerebellar impairment
(Fawcett & Nicolson, 1999). Cells of brains from patients with RD were found to have a larger mean area in the medial posterior cerebellar cortex and a larger cell size distribution in the anterior and posterior lobe (Finch, et al., 2002). Furthermore, cerebellar activation was found to be lower for adults with RD than for controls in motor learning tasks (Nicolson et al., 1999). These findings provide converging evidence of cerebellar abnormalities in RD. Most of the behavioural studies focused on features of motor control and balance (Fawcett & Nicolson, 1999). In view of this, a series of studies by
Stoodley and colleagues deserves mention. Essentially, it was shown that RD is associated with poor aiming and reaching (Stoodley, Fawcett, & Nicolson, 2006a); impaired sensorimotor processing and visual-motor integration difficulties (Stoodley &
Stein, 2006b); poor motor learning, (Stoodley, Harrison & Stein, 2006c), and balancing deficits and postural instability (Stoodley, Fawcett, Nicolson, & Stein, 2005). The behavioural symptoms in RD were suggested to reflect underlying cerebellar abnormalities, especially in the lateral aspects of the cerebellum.
Compared to the relatively large number of studies reporting on the relationship between RD and cerebellar impairment, studies testing the cerebellar deficit hypothesis in
DCD are remarkably few. In the absence of direct evidence from neuroimaging studies, the few available studies examining underlying processes in DCD have primarily described movement features typically controlled by the cerebellum. Motor timing is a feature of cerebellar motor control frequently assessed by tapping tasks. For instance, in the study of Lundy-Ekman, Ivry, Keele, and Woollacott, (1991), children with DCD participated in a tapping task in which they were asked to maintain a learned steady rhythm. Children with cerebellar ‘soft’ signs produced significantly more variable
2
Balance Performance in Developmental Disabilities intervals than both the control children and a group of children with basal ganglia ‘soft’ signs. In a later study, Piek and Skinner (1999) interpreted a slower reaction time on a sequential tapping task in children with DCD as a possibility of a cerebellar deficit. A movement feature which could also be affected by cerebellar dysfunction is muscle tone regulation. Raynor (2001) for example, showed that children with DCD generated lower levels of maximal strength and power. Finally, O’Hare and Khalid (2002) assessed children with DCD and co-occurring reading problems on tests of cerebellar function.
Both children with DCD only and children with combined DCD and reading problems showed typical signs of cerebellar dysfunction.
Recently, it was suggested that motor impairment in ADHD is characterized by timing, coordination and force deficits (Steger, et al., 2001; Pitcher, Piek, & Barret, 2002), symptoms typically related to cerebellar dysfunction (Brooks & Thach, 1981). However, the exact nature of the motor control processes underlying the motor problems seen in
ADHD remains, as yet, unclear. Both structural (Valera, Faraone, Murray, & Seidman,
2007; Durston, et al. 2004; Castellanos et al., 1996; 2001; 2002; Berquin, et al., 1998) and functional (Mulder et al., 2008; Valera, Faraone, Biederman, Poldrack, & Seidman,
2005) neuroimaging studies show abnormalities throughout the brain in individuals with
ADHD. The brain regions showing the largest and most significant reductions in volumes include, interestingly, the cerebellar areas (Valera, et al., 2007).
Clearly, there is a need for further delineation as to what extent combined
DCD/RD and/or co-existing ADHD differs from DCD or RD as single deficits in terms of cerebellar impairment. To study cerebellar damage in a behavioural setting, impairments of balance and gait appear to be some of the most distinctive clinical signs
(Morton & Bastian, 2004). Previous research already showed that balance deficits are associated with both DCD and RD (Geuze, 2005; Fawcett & Nicolson, 1994). Balance functions in children with a diagnosis of RD have frequently been examined with traditional psychometric measures such as the Movement Assessment Battery for
Children (Henderson & Sugden, 1992) (Iversen, Berg, Ellertsen, & Tønnessen, 2005;
Getchell, Pabreja, Neeld, & Carrio, 2007). This assessment, although clinically useful, only measures a motor end product and does not offer insight into underlying motor control processes (Halperin, McKay, Martier, & Sharma, 1994). Contrarily, balance function in DCD has mainly been studied in experimental studies using a static balance task in which subjects were asked to stand as still as possible while centre of pressure displacement was measured (Geuze, 2003; Cherng, Hsu, Chen, & Chen, 2007; Deconinck et al., 2008; Przysucha & Taylor, 2007; Tsai, Wu, & Huang, 2008). Both type of studies, experimental and behavioural, confirmed that the balance skills in persons with DCD or
RD are poor. Moreover, in most of the studies using the experimental measures of balance, it was hypothesized that the balance problems might be linked to cerebellar deficits (Geuze, 2003; Stoodley et al., 2005; Deconinck et al, 2008).
The aforementioned research has shown that there is an indication of cerebellar involvement in RD and DCD as well as ADHD. This study therefore aimed at recording the performance of children with DCD/RD and or co-existing ADHD compared to children with RD or DCD as single deficits on motor tasks assumed to be related to cerebellar function. More specifically, both kinematic and kinetic aspects of balance control were examined. It was hypothesised that balance impairment would increase as a function of co-occurring disorders, with children with combined DCD, RD and ADHD
3
Balance Performance in Developmental Disabilities being most affected. Two experimental balance control tasks were used: a static balance task in a stationary situation and a perturbation task requiring active balance restoration.
Both tasks are known to differentiate children with ADHD from those with fetal alcohol spectrum disorder (FASD) (Hofstetter, 2007).
In both static balance and balance perturbation tasks, the cerebellum is suggested to be involved in coordinating the strategy for maintaining balance control (Loram,
Maganoris, & Lakie, 2005; Brooks, 1986). After a balance perturbation the gastrocnemius, hamstrings and the paraspinals act together as a unit in a fixed sequence
(i.e., functional synergy) (Sundermier, Woollacott, Roncesvalles, & Jensen, 2001). This functional synergy always appears in the same order and with intensities determined by perturbation levels, which suggests that these muscle patterns are pre-programmed.
Cerebellar control is significantly involved in preserving these synergies (Brooks, 1986).
Furthermore, in a static balance task by Loram et al. (2005) it was suggested that the cerebellum is involved in human quiet standing. They showed that quiet standing in humans is controlled by an active, impulsive, ballistic process consistent with complex sensorimotor integration and predictive planning; an automatic controlled process by the cerebellum. The role of the cerebellum in quiet standing might explain why patients with cerebellar ataxia suffer impaired postural control (Loram et al., 2005). Studies of humans with cerebellar damage have contributed to our knowledge regarding the function of the cerebellum in movement control and balance. It was demonstrated that subjects with cerebellar damage were unable to scale their responses to expected perturbations (Horak
& Diener, 1994; Diener, Dichgans, Bacher, & Guschlbauer, 1984).
Examining balance in experimental studies however, only provides indirect evidence of cerebellar involvement. Nevertheless, analysis of the performance of the children on balance tasks in the present study might provide an indication of the underlying cerebellar aetiology of RD, DCD and ADHD.
METHODS
Participants
A total of 41 children participated in the study; 27 children with developmental problems and 14 control children. Six children were classified in the RD group, 8 children in the
DCD group and 13 children in the DCD/RD group. All the children in the DCD group were also diagnosed with ADHD.I In the RD group, 2 children were diagnosed with cooccurring ADHD and in the DCD/RD group, 6 children were diagnosed with cooccurring ADHD. As illustrated in table 1, group classification was based on a combination of information from teachers, parents, physicians plus the scores on the following measures: i.e., the Wechsler Individual Achievement Test II, the Movement
Assessment Battery for Children, the Developmental Coordination Disorder
Questionnaire and the Conners Parent Rating Scale- Revised (Long version).
Children with developmental problems were recruited from the Foothills
Academy, a Calgary-based government designated school for elementary, junior and senior high school students with special learning needs. The control group consisted of children recruited from a Calgary-based public elementary school and through word of mouth. Control children were without developmental problems, and matched group-wise
4
Balance Performance in Developmental Disabilities for age and gender. Both boys and girls participated in the study, with an age range from
9.0 to 13.9 years old. Exclusion criteria were: estimated full scale IQ < 70, neurological abnormalities (e.g., seizures, head trauma), or medical conditions that affect cognitive or motor function (e.g., diabetes). Children from the experimental groups were tested on the
Wechsler Intelligence Scale for Children – Third or Fourth Edition (WISC III or WISC
IV) to obtain a measure of intellectual functioning. All control children attended mainstream Canadian schools, implying an IQ-score in the normal range (i.e. FSIQ > 70).
Ethical approval for this research was provided by the Child Health Research Committee of the University of Calgary and the Calgary Health Region. Parental informed consent was obtained to perform screening tests as well as for full participation in the experimental sessions.
Diagnostic measures
The Wechsler Individual Achievement Test II (WIAT II; The Psychological Corporation,
2002)
The WIAT II was used to identify children with RD. The WIAT II is a comprehensive instrument for the evaluation of academic achievement including reading ability. The three subtests from the Reading Composite of the WIAT II, i.e., Word Reading, Reading
Comprehension subtest, Pseudoword Decoding, were used for identifying RD. Word
Reading assesses pre-reading (phonological awareness) and decoding skills, Reading
Comprehension requires the student to read sentences and short passages and then answer questions about the main idea, specific details or the order of events and Pseudoword
Decoding assesses the ability to apply phonetic decoding skills. The combined scores on the three reading subtests (i.e., Reading Composite) provide a measure of basic reading skills. A score on the Reading Composite below the recommended standard score of 1.65
SD below the mean score (Reynolds, 1984) was used as an indication of RD.
The Movement Assessment Battery for Children (M-ABC; Henderson & Sugden, 1992)
The M-ABC detects motor impairment in children aged 4 to 12 years. Test results are expressed in terms of a Total Impairment score, a Manual Dexterity score, a Ball Skills score and a Balance score, with increased impairment associated with higher scores. The
M-ABC has four age bands (4-6 yrs, 7-8 yrs, 9-10 yrs, and 11-12 yrs), with 8 tasks per age band. Raw scores are converted to normative age-dependent standardized scores, ranging from 0 to 5. These scores are then summed to produce a total score ranging from
0 to 40. A score below the 5 th
percentile on the M-ABC was used as an indication of
DCD.
The Developmental Coordination Disorder Questionnaire (DCDQ; Wilson, Dewey &
Campbell, 1998)
The DCDQ is a 15-item parent report questionnaire that provides information on children’s everyday motor skills, classifying children in DCD, suspect DCD and non-
DCD. Items are scored on a 5-point Likert scale, with response categories ranging from
‘not at all like your child’ to ‘extremely like your child’. The DCDQ results in a Total
Score ranging from 0 to 75. A score below the 10 th
percentile on the DCDQ was used as a
5
Balance Performance in Developmental Disabilities cut off for DCD. To be classified as DCD, children had to perform below the 5 th percentile on the M-ABC and below the 10 th
percentile on the DCDQ.
The Conners Parent Rating Scale- Revised (Long version) (CPRS; Conners, 1997)
The CPRS is a comprehensive standardized checklist for obtaining parental reports of childhood behaviour problems. It covers a broad range of child and adolescent problems following DSM-IV criteria, with a specific focus on detecting ADHD. The CPRS consists of 80 items divided into 14 subscales, with each subscale representing a diagnostic dimension. Parents rate individual items on a 4-point Likert scale (not at all, just a little, pretty much, very much). A profile is generated based on the T-scores, permitting comparisons with normative age and gender groups. The L subscale provides a score on inattention symptoms as described by the DSM-IV, the M subscale provides a score on hyperactive-impulsive symptoms and the N subscale provides a total score of inattention and hyperactive-impulsivity. The CPRS is among the most prominent ADHD rating scales used and has sound psychometrical properties (Collett, Ohan, & Myers, 2003;
Conners, Sitarenios, Parker, & Epstein, 1998). A T-score of ≥ 63 on the L, M and N subscales of the CPRS was used as an indication of ADHD.
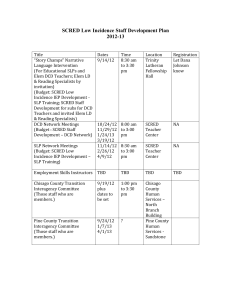
Table 1.
Age, Gender, SES and Estimated FSIQ Distribution across Participant Groups
Characteristics Controls RD DCD DCD/RD
(n = 14) (n = 6) (n = 8) (n = 13)
10.9 (1.5) 11.2 (1.5) 11.4 (1.2) 11.5 (1.1) Mean age in years
(sd)
Male/Female
SES:
Low
Middle
High
Mean FSIQ (sd)
ADHD
8/6
0.0%
28.6%
71.4%
-
0.0%
3/3
0.0%
16.7%
83.3%
98.8 (10.2)
33.3%
5/3
0.0%
25.0%
75.5%
115.8 (3.3)
100.0%
8/5
7.7%
46.2%
46.2%
92.0 (9.0)
46.2%
Note. SD = standard deviation, SES = Socioeconomic Status, FSIQ = Full Scale IQ.
The Blishen index (Blishen, Carroll, & Moore, 1981)
The Blishen Index provides an estimate of socioeconomic status (SES). For families with two parents, the highest SES score was used for that family.
Measures of balance
6
Balance Performance in Developmental Disabilities
Motor assessments included the Balance subtest of the M-ABC and two experimental tasks measuring balance (Static Balance Task) and dynamic postural control (Balance
Perturbation Task).
Both experimental balance tasks were designed to examine the kinematics (e.g., joint angles) and the kinetics (e.g., force aspects) of balance control. In this study, only kinetic data was used.
For the balance tasks, children were tested barefoot, wearing shorts and a T-shirt.
Reflective markers allowing kinematic assessment were placed bilaterally using the
Helen Hayes marker set ( Kadaba, Ramakrishnan, & Wootten, 1990 ). Motion data (120 Hz) were collected with an 8-camera video motion system (EVaRT®, Motion Analysis Corp.,
Santa Rosa, CA) interfaced with a forceplate that recorded 3-D ground reaction forces
(1200Hz; Advanced Medical Technology Inc., Watertown, MA). Muscle activity from the tibialis anterior, lateral gastrocnemius and the soleus was recorded bilaterally (1200
Hz; Biovision, Wehrheim, Germany) with surface electromyography (EMG).
The Static Balance Task consisted of four conditions (5 trials per condition) requiring children to stand still on a force platform: 1) 30 sec. with eyes open (EO); 2) 30 sec. with eyes closed (EC); 3) 30 sec. on a piece of foam (Airex Balance Pad®: L-Group,
St. Louis, MI, with a density of 50 kg/m3) with eyes open (EOF); 4) 30 sec on the foam with eyes closed (ECF). Foot placement was standardized by having the children place the medial borders of their feet at the same width as the markers on the anterior superior iliac spines (ASIS). Children stood with their arms and hands hanging relaxed at their sides.
For the Balance Perturbation Task (5 trials) children wore a belt at waist level that was attached to a rope from the custom build perturbation device. With the child standing on the forceplate and at a time unknown to the child, the perturbation device pulled the rope for the time required for a weight (20% of body weight) to fall 20 cm. This relative force magnitude had been previously determined to be such that balance could be regained without taking a step (Gildenhuys, 2003). Children were instructed to regain balance without taking a step if possible. The time between onset of the perturbation and the child’s response, evidenced by changes in the ground reaction forces and muscle pattern activity patterns were recorded. Children were prevented from anticipating the time of perturbation because a random delay of 0-5 sec varied the time from the trigger to the actual force application. Children wore a pair of industrial headphones during perturbation testing to reduce the likelihood that they would react to sounds produced by the device.
Procedure
To minimize experimenter bias, examiners were blinded to the diagnostic status of the children. Assessments were completed on different days to minimize fatigue or boredom.
On the first day, the M-ABC and the WIAT II reading composite were completed. The children were assessed on the M-ABC and the WIAT II by the first author. Scores on the
WISC-III or WISC-IV were obtained from the files from the Foothills Academy. Every child on the academy is assessed on the WISC-III or WISC-IV by a psychologist of the school. The static balance and balance perturbation tasks were administered on the second day by the research group. The CPRS and the DCDQ were filled out by the
7
Balance Performance in Developmental Disabilities parents while the children were assessed on the balance tasks on the second day. Total time to complete all tasks was approximately 2.5 hours, including breaks.
Due to time limitations, 4 control children could not be assessed on the M-ABC while 10 control children could not be assessed on the WIAT II. Moreover, not all the files of the children with developmental problems from the Foothills Academy contained
FSIQ information. Consequently, the FSIQ of only 18 out of 27 children with developmental problems were included in the analyses.
Experimental measures
Postural stability
For the static balance task, three-dimensional forces and moments were used to compute centre of pressure (COP). Using a custom-written program (Matlab v6.1, Mathworks,
Natick, MA), data was resampled to 120 Hz and digitally filtered (recursive 4th order
Butterworth filter with 5 Hz, low pass cutoff). After filtering, COP was computed and used in a measure of postural stability described by Riley, Benda, Gill-Body, & Krebs
(1995). The analysis is based on a phase plane plot of COP displacement and velocity.
From the displacement and velocity data, root mean squared variance of each measure was used to compute an instability parameter. Linear measures of COP motion were also computed, including maximum medial-lateral and anterior-posterior excursion and total area enclosed by the centre of pressure trace. Mean electrical activity over the whole trajectory of 30 seconds of the tibialis anterior, gastrocnemius and the soleus bilaterally was calculated.
EMG latencies
Onset of muscle activity was quantified from the EMG record during each perturbation trial. Data were full-wave rectified and filtered with a recursive 6th order Butterworth filter at 50 Hz. From the processed signal, an interval of baseline electrical activity preceding perturbation was selected using a mouse-driven cursor. Next, the mean signal of that baseline interval plus 3 standard deviations (SD) above the mean was computed and displayed. From this display the time point when the signal increased above the mean baseline level plus 3 SD was selected. The voltage of the resting signal and the time point when the signal exceeded 3 SD were recorded. Muscle onset latency was computed as the time between the onset of the perturbation and the onset of muscle activity.
EMG amplitude
Peak EMG amplitude was computed from integrated data during each perturbation trial.
Data were full-wave rectified. The signal was then integrated over 75 msec intervals.
Baseline activity was computed as the mean integrated signal during a 200 msec interval before the perturbation. Peak amplitude was identified as the largest signal recorded after the onset of the perturbation and before the signal returned to baseline. Peak amplitude was normalized with respect to the baseline integrated signal to allow comparisons across subjects. The time and amplitude of the peak integrated normalized signal were recorded for each trial. For the static balance tasks, mean EMG amplitude was computed from the filtered, rectified data for the entire 30 sec trial for each muscle. Mean amplitude during
8
Balance Performance in Developmental Disabilities the EC, EOF, ECF conditions was normalized to the mean amplitude recorded for the EO condition.
Statistical analysis
Diagnostic measures
Differences between groups regarding demographical data were analyzed with Chisquare tests of association for categorical variables (i.e., gender and SES) and analysis of variance (ANOVA) for continuous variables (i.e., age and FSIQ), followed by Scheffe procedure for post hoc comparisons when significant group effects were found. If significant group differences emerged, those variables were entered in the analysis of M-
ABC and experimental data as covariates.
Measures of motor competence
To study the influence of ADHD on the M-ABC total impairment score and the M-ABC balance subscale score, correlations with the L, M and/or N subscales of the CPRS subscale scores were examined. When the subscales significantly correlated with the total impairment score or balance subscale score, ANOVA’s as described below became
ANCOVA’s with the subscales as covariate. Posthoc contrasts were conducted when significant group differences emerged.
To examine group differences on the M-ABC total impairment and the balance subscale score, ANOVA was used. Scheffe post-hoc comparisons were used to further examine significant group effects.
Experimental measures
Influence of ADHD on the experimental static balance and the balance perturbation variables was analysed by calculating the correlations of the dependent variables with the
L, M and/or N subscales of the CPRS subscale scores. When significant correlations emerged, ANCOVA’s instead of ANOVA’s were conducted with the significant correlating subscales as covariate. Posthoc contrasts were made to further examine significant group effects.
Dependent variables of both the experimental static balance task and the balance perturbation task were examined for the presence of outliers. Scores that were beyond a 3
SD cutoff were eliminated, due to the fact that equipment errors or anticipation for the perturbation could have caused such extreme scores. This led to an elimination of a maximum of data from all the trials of 1 subject per dependent variable examined.
Moreover, to limit the effect of learning and fatigue, the first and the last trial were eliminated from the analysis.
ANOVA’s were used for the group differences on the separate dependent variables from the static balance tasks, including the maximum medial-lateral and anterior-posterior excursion, the total path length of the COP, the average medial-lateral, anterior-posterior and total velocity, the medial-lateral, anterior-posterior and overall instability parameter, the maximum COP area and the mean EMG values of the left and right tibialis anterior, the left and right gastrocnemius and the left and right soleus.
Scheffe post-hoc comparisons were made to further examine significant group effects.
9
Balance Performance in Developmental Disabilities
Group comparisons were conducted using ANOVA’s for the following dependent variables from the balance perturbation task: mean muscles onset and mean muscles amplitude, and baseline electrical activity for the tibialis anterior, the gastrocnemius and the soleus, bilaterally. Scheffe tests were computed when significant group differences emerged. Significance level was set at p = 0.05 for two-tailed tests and trends were defined as p < 0.10.
RESULTS
Sample description
No significant group differences were found for group characteristics (see table 1) except for FSIQ (F (2, 17) = 10.70, p < 0.01). Post hoc comparisons showed a significantly lower FSIQ in the DCD/RD group than the DCD group.
In order to investigate the influence of FSIQ on motor competence and balance, correlations were computed between FSIQ and the M-ABC total impairment score and the M-ABC static and dynamic balance score. The FSIQ was not significantly correlated with the M-ABC total impairment score ( r = -0.07, p = 0.78) or M-ABC static and dynamic balance score ( r = -0.179, p = 0.48). As a result no extra covariates were used in the following analyses.
Diagnostic measures
Table 2 shows the mean score, the standard deviation and the range of the diagnostic assessments per group. As can be seen in the range scores of table 2, some children did not meet the diagnostic criteria of the WIAT II, the M-ABC, the DCDQ and the CPRS as described in the method section. In these cases, however, the information from teachers, parents or physicians was more important for the diagnosis.
Measures of motor competence
In table 3 the means and standard deviations of the scores on the subtest and the total impairment score of the M-ABC are listed per diagnostic group. To study the influence of
ADHD on the M-ABC as well as on the experimental measures, correlations with the L,
M and/or N subscales of the CPRS were examined. When a subscale significantly correlated with the dependent variables, it was added as a covariate in the analysis.
Significant correlations were found between the T-scores on the L and N subscales of the
CPRS and the M-ABC static and dynamic balance scores (respectively: r = 0.49, p < 0.01 and r = 0.44, p < 0.01) and between the T-scores on the L, M and N subscales of the
CPRS and the M-ABC total impairment scores (respectively: r = 0.48, p < 0.01, r = 0.41, p = 0.01, and r = 0.48, p < 0.01). Consequently, in the analysis of the static and dynamic balance scores of the M-ABC, the T-scores on the L and N subscales of the CPRS were entered as covariates; while in the analysis of the M-ABC total impairment score the Tscores
10
Balance Performance in Developmental Disabilities
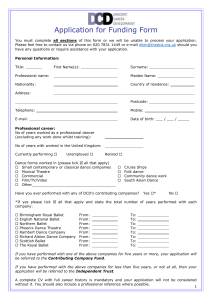
Table 2.
Mean Score, Standard Deviation and Range of the Diagnostic Assessments per Participant Group
Controls RD
(n = 14) (n = 6)
WIAT II reading composite standard score
M-ABC percentile
DCDQ total score
Mean (sd)
108.3
(5.9) a
20.2
(25.6) b
69.5
Range
101 – 113 a
1 – 84 b
57 – 75
Mean (sd)
82.5
(8.7)
36.0
(21.7)
62.8
Range
69 – 96
18 – 79
44 – 75
DCD
(n = 8)
Mean (sd)
102.0
(8.5)
4.5
(8.7)
39.6
Range
90 – 113
1 – 26
22 – 53
CPRS:
T-score L subscale
T-score M subscal
T-score N subscale
49.1
(6.5)
48.0
(5.8)
(6.3)
47.3
(7.9)
40 – 71
43 -63
40 – 61
(10.9)
53.8
(12.1)
52.0
(11.0)
53.3
(12.1)
43 – 74
43 – 66
43 – 72
(11.9)
74.0
(5.8)
78.8
(11.5)
79.0
(5.3)
65 – 82
56 – 90
69 – 85
Note. a n = 4, b n = 10.
DCD/RD
(n = 13)
Mean (sd)
68.7
Range
49 – 88
(11.4)
1.9
(1.4)
46.2
(9.5)
62.3
(11.9)
65.2
(12.2)
65.1
(11.0)
1 – 5
25 – 58
47 – 89
48 – 87
49 – 87
11
Balance Performance in Developmental Disabilities
Table 3.
Mean Scores and Standard Deviations (SD) of the Movement ABC per Diagnostic Group
Controls (n = 10) RD (n = 6)
Manual dexterity
Ball skills
Static and Dynamic Balance
7.6 (3.6)
1.9 (2.5)
1.8 (1.6)
4.2 (2.9)
0.6 (0.7)
1.4 (1.2)
Total impairment score 11.0 (5.3) 6.5 (2.4)
DCD (n = 8)
10.8 (3.4)
4.1 (2.3)
6.1 (4.5)
21.0 (8.5)
Table 4.
The Test Results of the ANCOVA for the static and dynamic balance Subscore and the Total Impairment Score of the M-ABC
Static and dynamic balance Total impairment score
Group
CPRS TL
CPRS TM
F (df)
3.92 (3,31)
3.47 (1,31)
- p-value
0.02
*
0.07
-
F (df)
6.24 (3,30)
1.10 (1,30)
0.63 (1,30) p-value
<0.01
*
0.30
0.43
CPRS TN 2.85 (1,31) 0.10 0.90 (1,30) 0.35
Note. CPRS TL = T-score on the L-subscale of the CPRS; CPRS TM = T-score on the M-subscale of the CPRS; CPRS TN
= T-score on the N-subscale of the CPRS.
* p < 0.05.
DCD/RD (n = 13)
11.4 (3.0)
3.4 (2.8)
5.9 (3.0)
20.7 (6.2)
12
Balance Performance in Developmental Disabilities on the L, M and N subscales of the CPRS were entered as covariates. ANCOVA’s demonstrated a significant main group effect on the M-ABC static and balance score (F
(3, 31) = 3.92, p = 0.02) and the M-ABC total impairment score (F (3, 30) = 6.24, p <
0.01) (see table 4). Post-hoc contrasts revealed that children with DCD/RD scored worse on the static and dynamic balance tests than children with RD as a single deficit (p = 0.02) and children with DCD (p = 0.02). The children with DCD/RD (p < 0.01) scored also worse on the total impairment score than children with RD (see figure 1). a. b.
7 25
6
Controls
RD
DCD
DCD/RD
**
20
Controls
RD
DCD
DCD/RD
* *
5
15
4
3
2
10
5
1
0 0
Figure 1.
Group Means Adjusted for Covariates for (a.) the Static and Dynamic Balance Tests Score and
(b.) the M-ABC Total Impairment Score.
* p < 0.05.
** p < 0.10.
As demonstrated in table 2 some children of the control group scored below the designated percentile for indication of DCD on the M-ABC. Excluding those subjects from the analyses for the M-ABC total impairment score and static and dynamic subscale score revealed a main group effect for on the M-ABC total impairment score (F(3,25) =
6.61, p < 0.01) with the children with DCD/RD scoring worse than the control children and the children with DCD (p = 0.03). The children with DCD/RD scored also worse on the total impairment score than the children with RD (p < 0.01) (see figure 2). The children with DCD/RD did not differ from the controls on the M-ABC static and dynamic subscale score (p = 0.12).
As can be seen in table 4 none of the covariates significantly influenced the performance on the total impairment or the static and dynamic balance tests of the M-
ABC. A trend was found for the influence of the T-score on the L subscale of the CPRS.
A re-run of the analysis of the group differences for the static and dynamic balance test of the M-ABC with only the T-score of the L subscale of the CPRS as a covariate revealed a trend (F(3,32) = 2.86, p = 0.05). Post-hoc contrasts showed that children with DCD/RD tend to score worse on the static and dynamic balance tests than children with RD as a single deficit (p = 0.06). The T-score of the L subscale of the CPRS did not significantly influence the performance on the static and dynamic balance test of the M-ABC (F (1, 32)
= 0.63, p = 0.44).
13
Balance Performance in Developmental Disabilities
10
5
20
15
25
Controls
RD
DCD
DCD/RD
** *
0
Figure 2.
Group Means Adjusted for Covariates for the M-ABC Total Impairment Score with Children from the Control Group who scored below the Designated Percentile for Indication of DCD Excluded.
* p < 0.05. Children with DCD/RD differed from the Control group and the RD group.
** p < 0.05. Children with DCD differed from the RD group.
Experimental measures
Postural stability
No significant group effects were found for EMG values for the left and right tibialis anterior, the left and right gastrocnemius and the left and right soleus on any of the conditions (i.e., eyes open, eyes closed, eyes open on foam, eyes closed on foam).
Condition: Eyes Open
As demonstrated in table 5 in the EO condition there were no main group effects or trends.
Condition: Eyes Closed
Table 6 shows the significant effect for group in the EC condition indicating a significant group difference in the maximum anterior-posterior excursion of the centre of pressure trace (F(3,37) = 3.50, p = 0.03). Post hoc comparisons showed that children with DCD had a larger maximum anterior-posterior excursion of the COP trace than children with
RD (p = 0.046). Figure 3 displays individual COP traces of a child with DCD and a child with RD in the EC condition.
14
a.
Balance Performance in Developmental Disabilities b.
Figure 3.
Individual COP Traces of a Child with DCD and ADHD and a Child with RD on the Condition with Eyes Closed. a. Child with DCD and ADHD on the EC Condition. b. Child with RD on the EC
Condition
Condition: Eyes Open on Foam
One main effect for group was found on the EOF condition for the maximum mediallateral excursion of the COP trace (F (3, 37) = 3.04, p = 0.04) (see table 7). Post-hoc comparisons revealed that children with DCD had a larger maximum medial-lateral excursion of the COP trace than children with RD (p = 0.06). Furthermore, a near significant main effect for group was found for the total area of the COP trace (F (3, 37) =
2.50, p = 0.07), with children with DCD showing a larger area than children with RD (p =
0.097).
Condition: Eyes Closed on Foam
Table 8 displays for the ECF condition a main effect for group on the instability parameter in the anterior-posterior direction (F (3, 36) = 3.23, p = 0.03). Children with
DCD were significantly more instable in the anterior-posterior direction than children with RD (p = 0.04).
Several near significant main effects of group were found in the ECF condition. A trend for main effect of group was found for the maximum anterior-posterior excursion of the COP trace (F (3, 36) = 2.40, p = 0.08). Post-hoc contrasts indicated that children with
DCD tend to show a larger maximum anterior-posterior excursion of the COP trace than children with RD (p = 0.07). For the analysis of the maximum anterior-posterior excursion of the COP trace an ANCOVA was used with the T-score of the N subscale of the CPRS as a covariate to study the influence of ADHD. The analysis revealed no main effect of the T-score of the N subscale of the CPRS (F (1, 36) = 0.163, p = 0.689): the performance on the N subscale of the CPRS did not influence the performance of the maximum anterior-posterior excursion of the COP trace.
Another near significant main effect of group was found for the total path length of the COP trace (F (3, 36) = 2.48, p = 0.08). Scheffe post-hoc test revealed that children with DCD displayed a longer total path length of the COP trace than children with RD (p
= 0.09). Third, on the average velocity in the anterior-posterior direction a trend for main effect of group was found (F (3, 36) = 2.82, p = 0.05): children with DCD tended to show a faster displacement in the anterior-posterior direction than children with RD (p = 0.06).
The fourth near significant main effect of group was found for the average total velocity
(F (3, 36) = 2.48, p = 0.08), with children with DCD showing a faster displacement than
15
Balance Performance in Developmental Disabilities children with RD (p = 0.09). The fifth near significant main effect of group was found for the
16
Balance Performance in Developmental Disabilities
Table 5.
Mean, Standard Deviation (SD) and Test Results of the COP Characteristics on the Condition with Eyes Open
Mean (sd)
Controls
(n = 14)
RD
(n = 6)
DCD
(n = 8)
DCD/RD
(n = 13)
F(df) p-value
Max. m-l excursion (mm)
Max. a-p excursion (mm)
Total path length (mm)
Avg. velocity m-l (mm/s)
Avg. velocity a-p (mm/s)
Avg. Total velocity (mm/s)
Instab. par. m-l
Instab. par. a-p
19.78
30.05
9.01
10.49
15.57
13.55
15.49
(7.06)
(9.28)
466.92 (127.14)
(3.35)
(2.24)
(4.24)
(4.91)
(3.28)
15.43
25.03
(5.46)
(7.94)
421.79 (193.80)
8.37
9.12
14.06
12.69
13.37
(4.53)
(3.00)
(6.46)
(6.40)
(5.44)
23.96
35.42
11.90
11.56
18.75
17.77
13.37
(8.34)
(9.03)
562.42 (187.72)
(5.15)
(3.00)
(6.26)
(7.67)
(5.44)
16.71
26.49
(5.00)
(6.46)
461.11 (142.59)
9.19
10.10
15.51
13.32
14.74
(3.56)
(2.29)
(4.67)
(5.18)
(3.61)
2.52
2.56
1.13
1.23
1.00
1.12
1.30
1.44
(3,37)
(3,37)
(3,37)
(3,37)
(3,37)
(3,37)
(3,37)
(3,37)
Instab. overall
Max. COP area (mm²)
20.82 (5.40)
415.55 (257.28)
18.67 (7.84)
270.00 (159.40)
25.24 (8.29)
597.28 (364.18)
20.05 (5.76)
317.07 (212.95)
1.48
2.53
(3,37)
(3,37)
Note. Max. = maximum, m-l = medial-lateral, a-p = anterior-posterior, Avg. = average, instab = instability, par = parameter, COP = center of pressure.
0.41
0.35
0.29
0.25
0.07
0.07
0.35
0.31
0.24
0.07
17
Balance Performance in Developmental Disabilities
Table 6.
Mean, Standard Deviation (SD) and p-values for testing the differences between groups of the COP Characteristics on the Condition with Eyes Closed
Mean (sd) F(df) p-value
Controls
(n = 14)
RD
(n = 6)
DCD
(n = 8)
DCD/RD
(n = 13)
Max. m-l excursion (mm)
Max. a-p excursion (mm)
Total path length (mm)
Avg. velocity m-l (mm/s)
Avg. velocity a-p (mm/s)
Avg. Total velocity (mm/s)
Instab. par. m-l
Instab. par. a-p
22.82
34.76
11.53
14.44
20.75
16.75
21.02
(9.66)
(11.26)
622.39 (220.05)
(4.76)
(4.82)
(7.34)
(7.08)
(6.80)
18.68
31.47
(5.60)
(7.60)
551.54 (169.28)
10.43
12.59
18.39
15.28
18.15
(3.73)
(3.85)
(5.64)
(5.52)
(5.08)
28.97
45.83
13.92
16.59
24.46
21.05
23.39
(11.31)
(12.80)
773.54 (228.94)
(4.43)
(4.68)
(7.63)
(6.05)
(5.06)
24.39
32.16
(10.30)
(8.17)
622.68 (181.63)
12.44
13.80
20.89
18.17
20.12
(4.13)
(3.69)
(5.87)
(5.84)
(5.94)
1.36
3.50
0.99
0.87
1.12
1.00
1.17
0.95
(3,37)
(3,37)
(3,37)
(3,37)
(3,37)
(3,37)
(3,37)
(3,37)
Instab. overall
Max. COP area (mm²) ¹
27.18 (9.27)
608.46 (128.82)
23.98 (6.69)
43481 (171.50)
31.78 (9.33)
736.11 (183.66)
27.66 (8.47)
596.73 (114.72)
1.03
0.49
(3,37)
(3,36)
Note. Max. = maximum, m-l = medial-lateral, a-p = anterior-posterior, Avg. = average, instab = instability, par = parameter, COP = center of pressure.
¹ Adjusted means for the covariate T-score on the M-subscale of the CPRS.
* p < 0.05.
0.35
0.40
0.33
0.43
0.27
0.03
*
0.41
0.47
0.39
0.69
18
Balance Performance in Developmental Disabilities
Table 7.
Mean, Standard Deviation (SD) and Test Results of the COP Characteristics on the Condition with Eyes Open and on Foam
Mean (sd)
Controls
(n = 14)
RD
(n = 6)
DCD
(n = 8)
DCD/RD
(n = 13)
F(df) p-value
Max. m-l excursion (mm)
Max. a-p excursion (mm)
Total path length (mm)
Avg. velocity m-l (mm/s)
Avg. velocity a-p (mm/s)
¹
Avg. Total velocity (mm/s)
Instab. par. m-l
Instab. par. a-p 1
30.09 (11.52) 23.32 (6.78)
51.41 (14.05) 45.30 (7.68)
41.88 (18.60)
64.16 (15.97)
33.90 (8.96)
49.23 (15.03)
677.29 (185.18) 658.58 (215.02) 854. 06 (215.03) 713.51 (206.90)
11.73 (4.29) 11.02 (4.20) 15.57 (5.06) 12.65 (4.34)
17.24 (1.51) 16.88 (2.01)
22.58 (1.65) 21.96 (5.87)
16.84 (6.02) 15.61 (5.59)
25.26 (2.12) 24.70 (2.82)
20.41
28.48
22.51
31.04
(2.15)
(7.17)
(7.57)
(3.02)
17.42
23.79
18.35
25.74
(1.34)
(6.90)
(5.92)
(1.89)
3.04
2.56
1.65
1.62
0.59
1.65
1.83
0.95
(3,37)
(3,37)
(3,37)
(3,37)
(3,36)
(3,37)
(3,37)
(3,36)
Instab. overall
Max. COP area (mm²)
30.13 (7.69) 29.12 (6.50)
1078.24 (710.07) 730.73 (298.87)
31.73 (9.34) 31.73 (8.54)
1700.85 (1031.69) 1111.19 (512.07)
1.95
2.50
(3,37)
(3,37)
Note. Max. = maximum, m-l = medial-lateral, a-p = anterior-posterior, Avg. = average, instab = instability, par = parameter, COP = center of pressure.
¹ Adjusted means for the covariate T-score on the M-subscale of the CPRS.
** p < 0.10.
0.04
*
0.07
**
0.19
0.20
0.63
0.19
0.16
0.43
0.14
0.07
**
19
Balance Performance in Developmental Disabilities
Table 8.
Mean, Standard Deviation (SD) and Test Results of the COP Characteristics on the Condition with Eyes Closed and on Foam
Mean (sd)
Controls
(n = 14)
RD
(n = 6)
DCD
(n = 8)
DCD/RD
(n = 13)
F(df) p-value
Max. m-l excursion (mm)
Max. a-p excursion (mm) ¹
Total path length (mm) 2
Avg. velocity m-l (mm/s) 2
Avg. velocity a-p (mm/s) 2
Avg. Total velocity (mm/s) 2
44.22
69.59
1173.42 (381.24) 863.75 (202.04) 1406.32 (393.07) 1229.45 (383.50) 2.48 (3,36)
19.24
29.67
39.13
(26.05)
(22.70)
(8.44)
(8.16)
(12.71)
28.70
59.84
13.83
22.26
28.80
(7.22)
(4.92)
(4.46)
(4.66)
(6.74)
65.36
99.68
23.09
35.73
46.89
(43.56)
(31.71)
(8.57)
(8.70)
(13.11)
48.52
76.72
20.49
31.08
40.99
(16.99)
(21.52)
(6.87)
(9.77)
(12.79)
2.31 (3,37)
2.40 (3,36)
1.75 (3,36)
2.82 (3,36)
2.48 (3,36)
Instab. par. m-l
Instab. par. a-p 2
Instab. Overall 2
Max. COP area (mm²)
28.28
42.76
51.76
2403.43
(15.15)
(11.96)
(18.24)
(2416.40)
19.42
32.39
37.98
(6.09)
(6.18)
(8.03)
1181.83 (297.53)
40.74
53.31
62.70
5055.29
(25.84)
(13.02)
(17.04)
(5076.82)
29.89
45.66
54.79
2552.10
(16.33)
(14.16)
(16.72)
(1424.55)
2.24 (3,37)
3.23 (3,36)
2.55 (3,36)
2.16 (3,37)
Note. Max. = maximum, m-l = medial-lateral, a-p = anterior-posterior, Avg. = average, instab = instability, par = parameter, COP = center of pressure.
¹ Adjusted means for the covariate T-score on the N-subscale of the CPRS.
² n control
= 14, n
RD
= 6, n
DCD
= 7, n
DCD/RD
= 13.
* p < 0.05.
** p < 0.10.
0.09
**
0.08
**
0.08
**
0.17
0.05
**
0.08
**
0.10
0.03
*
0.07
**
0.07
**
20
Balance Performance in Developmental Disabilities overall instability parameter (F(3,36) = 2.55, p = 0.07). Post-hoc comparisons showed that children with DCD tended to be more instable than children with RD. The last near significant main effect of group was for the total area of the COP trace (F(3,37) = 2.16, p
= 0.07), with the DCD group showing larger areas than children with RD (p = 0.098).
EMG latencies
No significant group differences in mean muscle onset latencies were found using
ANOVA. For the EMG baseline activity a main effect for group was found for the left tibialis anterior (F(3,37) = 4.37, p = 0.01), with children with DCD showing a lower baseline than children with DCD/RD (p = 0.03) and a main effect for group was found for the left gastrocnemius (F(3,37) = 3.647, p = 0.02) with children with DCD showing a lower baseline than children with DCD/RD (p = 0.03) (see figure 4).
4000
3500
3000
Controls
RD
DCD
DCD/RD
2500
2000
1500
1000
*
500
*
0 left tibialis anterior left gastrocnemius left soleus
Figure 4.
The EMG Baseline Activity for the Muscles of the Left Leg of the Different Groups.
* p < 0.05.
EMG amplitude
Figure 5 demonstrates the normalized EMG peak amplitudes for the different muscles. A significant main group effect was found for the peak amplitude of the left tibialis anterior
(F(3,37) = 2.88, p = 0.049). Children with RD had significant lower amplitudes than the controls (p = 0.05), but did not differ from other groups. The time of the peak from the left tibialis anterior was also significantly different between groups (F (3, 37) = 5.44, p <
0.01). The peak amplitude of the children with RD occurred later than the peak of both the controls and the children with DCD/RD.
21
Balance Performance in Developmental Disabilities
0,9
0,8
0,7
0,6
0,5
0,4
0,3
0,2
0,1
Controls
RD
DCD
DCD/RD
*
0 left tibialis anterior left gastrocnemius left soleus
Figure 5.
The Normalized EMG Amplitudes of the Peak from the Different Left Muscles.
* p < 0.05.
DISCUSSION
The main purpose of this study was to examine to what extent children with DCD/RD and/or co-existing ADHD differ in their balance performance from children with DCD or
RD as single deficits. Kinetic aspects of balance control were examined using a static balance task and a balance perturbation task. It was hypothesised that balance impairment would increase as a function of co-occurring disorders, with children with combined
DCD, RD and ADHD being most affected. Moreover, an attempt was made to relate the kinetic findings with possible underlying cerebellar abnormalities in children with DCD and RD.
The overall motor competence of the children in the present study as measured with the M-ABC confirmed the expectation that children with DCD combined with RD or DCD as a single deficit are more impaired than children with RD only. As the children with RD in the present study did not meet criteria for DCD, it was not surprising that the
DCD group and the combined DCD/RD group scored significantly higher than the RD only group. This indicates more problems in motor behaviour in children with DCD. It has previously been shown that children with RD perform inferior on the M-ABC than children without developmental disorders (Getchell et al., 2007; Iversen et al., 2005;
Jongmans et al., 2003). However, this is in contrast with the results of the present study, in which children with RD did not perform worse on the M-ABC total impairment score.
A possible explanation could be that children in de studies of Iversen et al. (2005) and
Getchell et al. (2007) were not screened for DCD in advance. Consequently, it cannot be ruled out that children with RD in those studies could also be diagnosed with DCD. In contrast, in the present study all children in the group with RD as a single deficit did not meet the criteria for DCD.
22
Balance Performance in Developmental Disabilities
The balance performance data obtained with the M-ABC in the present study confirmed our hypothesis that balance impairment would increase as a function of cooccurring disorders. Children with DCD/RD tended to demonstrate more problems with the static and dynamic balance tests of the M-ABC than children with RD only.
Furthermore, these results are in accordance with other findings in the literature.
According to Jongmans et al. (2003), children with DCD and co-occurring RD performed worse on the M-ABC than children with RD only, with children with DCD and cooccurring RD scoring particularly low on the balance subtest. The current findings are consistent with previous studies that have found that children with DCD and RD have poor balance skills.
With the knowledge of functional balance differences between the groups, data from the experimental balance tasks may provide enhanced information about the kinetic and EMG aspects of balance. On the EO condition of the static balance task, there were no differences between groups in the mean EMG values for the left and right tibialis anterior, left and right gastrocnemius and left and right soleus, there were also no between group differences in instability parameters and there were no differences between groups in the linear measures of the centre of pressure motion. Children with RD,
DCD or DCD/RD did not differ from control children on any of the kinetic variables when standing still on a force plate with their eyes open. This is in contrast with Geuze
(2003) and Przysucha and Taylor (2004) who found that children with DCD showed larger anterior-posterior displacements of the COP trace and larger sway area of the COP trace in similar balance tasks. In the study of Geuze (2003), the performance of children with DCD resembled the performance of a younger control group. Geuze (2003) hypothesized therefore, that the children with DCD have not automated the control of balance to the extent that the control children have. Moreover, according to Geuze (2003), inefficient muscular activation patterns in the DCD group contributed to balance control problems. The results of the present study, though, do not confirm these findings of
Geuze (2003), which might be due to either a difference between children participating in both studies or a difference in muscles examined. Children with DCD in both the study of
Geuze (2003) and Przysucha and Taylor (2004) where particularly screened for having problems on the balance subtests of the M-ABC, while in the present study, only 37.5% of the children with DCD and 23.1% of the children with DCD/RD showed definite balance problems on the M-ABC balance subtests. Furthermore, Geuze (2003) examined the co-activation between the tibialis and peroneus muscles and the co-activation between the rectus femoris and the semitendinosus muscles, while in the present study, it was the tibialis anterior, the gastrocnemius and the soleus that were examined.
Current results did demonstrate between group differences when children had to stand still on a force plate with their eyes closed. Children with DCD showed a larger maximum anterior-posterior excursion of the COP trace than children with RD in the EC condition. Larger maximum anterior-posterior excursion of the COP trace in children with DCD indicates their tendency to settle in the anterior-posterior plane of displacement when vision is deprived. The pattern of more excursions away from the initial COP location may put children with DCD at greater risk of losing balance when attempting to maintain stance without information from the visual system, if a larger perturbation is present (as cited in Przysucha & Taylor, 2004: Geuze et al., 2002).
23
Balance Performance in Developmental Disabilities
Surprisingly, children with DCD/RD did not differ from the control group or children with RD only on any of the conditions of the static balance task. The presence of
RD does not appear to influence balance performance negatively. It is worth mentioning though, that the DCD/RD group did show, although not significantly, higher means on all the COP measures in all the conditions than the RD group. Previously, Kapoula and Bucci
(2007 ) did find a difference between children with RD and control children. Children with
RD performed significantly worse on balance performance measured by excursion of the
COP trace and the average velocity of the COP displacement than control children when standing still with eyes open. However, children in Kapoula and Bucci’s (2007) study, were not screened for co-occurring motor problems (i.e., DCD) and it is unknown, whether the postural stability problems were due to the existence of a reading problem or possible co-existing motor problems..
The influence of lack of vision on balance control in children with DCD as found in the present study has not been found in previous studies (Geuze, 2003; Przysucha &
Taylor, 2004). Both Geuze (2003) and Przysucha and Taylor (2004) concluded that children with DCD do not over-rely on vision when standing on two legs. This conclusion, however, was based on only the Romberg’s quotient (i.e., the ratio of the variable obtained in the eyes closed and the eyes open condition), while no differences between groups on the separate conditions were calculated. Moreover, another relevant factor which could explain the differences with other studies may be that children with
DCD are more easily fatigued (as cited in Tsai et al., 2008: O’Beirne & Larkin, 1991;
Raynor, 1989). Tsai et al. (2008) and Cherng et al. (2007) also investigated the influence of vision on static postural stability. Compared with studies, the children in the present study were asked to stand still 10 seconds longer per trial and perform 2 to 4 trials more than in the other/previous studies (Geuze, 2003; Przysucha & Taylor, 2004). Children with DCD may need higher fitness levels to maintain their deviant balance control patterns, whereas children without DCD are able to perform a static balance task without any extra effort (Tsai et al., 2008).
In the current study, children with DCD differed from children with RD in terms of the pattern of the COP trace when information from their proprioceptive sensory input was disturbed. In the condition where subjects stood still on a piece of foam with their eyes open, the children with DCD showed a larger maximum medial-lateral excursion of the COP trace than children with RD and tended to show a larger maximum anteriorposterior excursion of the COP trace and a larger maximum COP area than children with
RD. As in the EC condition, it was unexpected that children with DCD did not differ from control children on the EOF condition and those children with DCD/RD did not differ from either the RD only or control group. Further research is required, as an explanation for these results has not yet been found yet. Our results showing that children with DCD had a deviant pattern of more excursions away from the initial COP location when proprioceptive sensory input is disturbed are in line with previous findings. Both
Cherng et al. (2007) and Deconinck et al. (2007) reported that children with DCD displayed a larger COP sway area when proprioceptive information from the feet was manipulated/reduced.
When both vision and proprioceptive information were absent children with DCD were expected to lose their balance. In the ECF condition, where vision and proprioceptive information were reduced/lacking, the children with DCD indeed showed
24
Balance Performance in Developmental Disabilities more instability in the anterior-posterior direction on the instability parameter than children with RD. Moreover, the children with DCD tended to have; (i) a larger maximum excursion of the COP trace in the medial-lateral and the anterior-posterior direction; (ii) a longer total path length of the COP trace; (iii) a larger area of the COP trace; (iv) a faster displacement in the anterior-posterior direction; (v) a faster displacement overall and; (vi) tended to be more instable overall during the 30 seconds trials than children with RD.
The maximum sway amplitude (i.e. maximum excursion of the COP trace and the area of the COP trace) can be interpreted as a measure of the degree of destabilization at the most unstable moment of the trial and the mean sway velocity (i.e. velocity of the displacement) as a measure of sway dynamics during the entire duration of the registration. Thus, when both vision and proprioception are disturbed, children with DCD have more difficulties maintaining balance at both the most unstable moment of the trial and during the entire duration of the trial. This is in accordance with the studies of
Deconinck et al. (2007) and Cherng et al. (2007) who found that children with DCD demonstrate larger COP sway area’s and larger mean sway velocities on a comparable static balance task.
As to the study’s question regarding the influence of co-occurring ADHD, measured by the L, M and N subscale score of the CPRS on balance performance, the influence did not seem to be present in this study. This result contrasts with the findings of Hofstetter (2007) who found that children with ADHD had more stability problems and scored higher than the controls on medial-lateral excursion, anterior-posterior excursion, total path length and velocity on the same static balance task standing on firm surface with eyes open. However, also in the Hofstetter (2007) study children were not screened for DCD in advance. Consequently, it is unknown whether the stability problems were due to ADHD or possible co-existing motor problems.
Taken together, the children with DCD, RD and/or ADHD who participated in the present study performed the EO condition of the static balance task similar to the control children. Adequate balance control requires a very accurate tuning and integration of three sensory inputs; visual, proprioceptive, and vestibular input (Forssberg & Nashner,
1982; Peterka, 2002). Therefore, the lack of differences between the groups in the EO condition of the static balance task may indicate that children with DCD, children with
RD and children with combined DCD/RD were able to integrate visual, proprioceptive and vestibular feedback for postural control in stance. The different patterns and extended stability problems seen in children with DCD when vision and/or proprioception are reduced/minimized may designate a deficit in sensorimotor organization. This might be concluded from the results demonstrating that children with
DCD show greater instability and larger excursion away from the initial COP location, a greater COP area as well as a faster displacement of the COP than children with RD when vision and/or proprioceptive information from their feet was reduced. Considering that the children with RD performed similar to the control children as described above, and that it is unclear why children with DCD did not differ from controls, the current results are consistent with other studies investigating the influence of vision and proprioceptive information on static postural stability. Previous studies have reported that children with DCD show greater postural sway amplitude than controls when vision and/or proprioceptive information were disturbed (Deconinck et al., 2007; Cherng et al.,
25
Balance Performance in Developmental Disabilities
2007; Tsai et al., 2008). It appears that the children with DCD had difficulties to scale the present information from their sensory inputs (re-weighting). Skilful sensory reweighting requires an adequate detection of missing or disturbed information and a compensation of the sensory contributions by increasing reliable and reducing less reliable inputs in response (Deconinck et al., 2007). Grove and Lazarus (2007 ) support the hypothesis that children with DCD have difficulty with sensory re-weighting, and more specifically, with the functional use of vestibular feedback when both vision and proprioception are disturbed for maintaining postural control. Using the Equitest Sensory
Organizational Test (EQSOT
TM
) they also found that children with DCD demonstrate significantly impaired postural stability under conditions in which vestibular feedback was the only accurate source of orienting feedback for postural control. The increase in postural sway may indicate that children with DCD in the present study may not be able to rely on somatosensory information from their feet to control balance when vision is removed and may not be able to rely on vision when somatosensory information is disturbed. Moreover, when both somatosensory and visual information were disturbed, children with DCD may not be able to rely on vestibular feedback. These findings suggest that children with DCD have difficulties with sensory re-weighting, and that the impaired balance control in children with DCD may be due to a deficit in sensory organization.
A commonly held view is that effective postural control not only requires proper sensory organization, but also motor response organization (Nasher, Shupert, Horak, &
Black, 1989). The process of motor response organization depends upon normal sensory organization and involves the execution of coordinated and properly scaled neuromuscular responses to either internal or external perturbations of the centre of mass
(Nasher, et al., 1989). In the present study, the groups did not differ in mean EMG values for the tibialis anterior, the gastrocnemius and the soleus bilaterally, in none of the conditions of the static balance task. Thus, current results of the static balance task do not suggest a problem in motor response organization as a response to internal perturbations in children with DCD, RD or DCD/RD compared to children without developmental disorders.
Neuromuscular response to external perturbations was examined with the balance perturbation task. Results do not show pronounced differences between the groups on muscular response. Children with DCD showed a lower EMG baseline activity of the left tibialis anterior and the left gastrocnemius than children with DCD/RD, but they did not differ from children with RD or control children.
The RD group demonstrated lower EMG amplitudes of the left tibialis anterior than the controls and the peak of the RD group occurred later than the peak of both controls and the DCD/RD group but not than the DCD group. Lower EMG amplitude and later response of the left tibialis anterior may imply a difference in the reaction of taking a step to regain balance after perturbation. Whereas some children did not need to take a step, others took a step as a last remedy to regain balance and some children even took a step right away. It might be that children with RD did not need to step away or only use the step as last remedy to regain balance...
The response to external unexpected perturbations has been examined before in both children with RD only and children with DCD only. Body movements as measured by a triaxal accelerometer over the trunk on a similar balance perturbation task have been
26
Balance Performance in Developmental Disabilities described before in children with RD (Moe-Nilssen, Helbostad, Talcott, & Toennessen,
(2003). In addition, neuromuscular response as measured by EMG electrodes from the tibialis anterior, the gastrocnemius, the soleus, the rectus femoris and the semitendinosus bilaterally on a similar perturbation task has been described in children with DCD (Geuze,
2003). Corresponding with the results of Moe-Nilssen et al. (2003) and Geuze (2003), children with RD or DCD in the present study did not respond differently on the perturbation task than control children. Consequently, children with RD and/or DCD do not seem to show a different neuromuscular response to external perturbation than typically developing children.
Evidence of deficits in balance performance in the present study was hypothesized to support previous suggestions of cerebellar dysfunction in children with DCD and/or
RD. Deficits in balance performance, however, have only been found in children with
DCD/RD on the M-ABC and in children with DCD as a single deficit on the experimental static balance task when sensory feedback was disturbed. As the cerebellum is particularly important for processing input from the sensory receptors to provide precise timing for coordinated, smooth movements of the body (Martin, 2003), problems in sensory organization in children with DCD may point to a cerebellar dysfunction in this population. Moreover, cerebellar deficits typically results in increased postural sway during standing (Diener et al., 1984; Dichgans & Diener, 1985). Current evidence that children with DCD showed more postural instability which might be due to problems with sensory organization may imply cerebellar abnormalities in these children.
Nevertheless, the expected deficits in balance in children with RD or DCD/RD are lacking in the present study. As a consequence, little evidence exists for cerebellar involvement in balance performance in DCD in this study. Furthermore, balance problems provide only indirect evidence of cerebellar involvement in motor performance of children with DCD. Electrophysiological or fMRI studies may be a possible sources of information to provide direct evidence of a cerebellar deficit in DCD and/or RD.
The many trends found in the present study may imply that more rigorous control over experimental factors, such as children’s age band, sample size, and the heterogeneity of the groups might lead to different more reliable results. First, it is not before the age of
12 that children use sensory information to maintain balance like adults ( Peterson, Christou,
& Rosengren, (2006 ). It may be that the youngest children in the current study used the sensory information differently than the older ones. Consequently, smaller age bands may lead to more reliable results. Secondly, a larger sample size will lead to more reliable results, since the power estimation prior to the start of this project was 80% when a sample of 20 children per group was present. Thirdly, Nolan, Grigorenko, & Thorstensson
(2005 ) found age related differences in the development of postural control between boys and girls. Therefore, it was concluded that there is a need to study both genders separately when investigating balance performance in children. The present study did not differentiate between boys and girls due to the small number of participants. Investigating the influence of gender might lead to more reliable results in future studies. Finally, children diagnosed with DCD may show a variety of symptoms and therefore, their performance on the balance tasks may differ accordingly.
Also of note is the fact that 16 out of the 27 children in the experimental groups were diagnosed with co-occurring ADHD, which might have influenced balance performance (Buderath et al., 2008). The presence of ADHD in children with DCD
27
Balance Performance in Developmental Disabilities and/or RD in the present study did not seem to be of influence on balance performance.
The L, M and N subscale of the CPRS examining hyperactive-impulsive and inattentive symptoms of the DSM-IV (American Psychiatric Association, 1994) ADHD symptom list as observed by the parents were used as covariates to examine the influence of ADHD on balance performance. These subscales however, were not the only measures used to diagnose ADHD in this study and may have provided biased results. Three children with a low CPRS score indicating no ADHD were diagnosed with ADHD by a physician while this information was not used in the analyses. Moreover, four children with a CPRS score indicating ADHD were not diagnosed with ADHD by a physician and as a result, the CPRS score might have been misleading. The optimal design for this study would have been to compose separate groups for children with co-occurring ADHD; however, the sample size of the present analyses was too limited for this purpose.
In conclusion, the present study shows that children with DCD/RD perform poorly on the balance subtests of the M-ABC and children with DCD perform poorly on the static balance task in those conditions when at least one of the required sensory inputs was disturbed. The different patterns and stability problems in children with DCD may indicate a deficit in sensorimotor organization. Assumptions about a possible underlying cerebellar deficit from these results should be taken with caution, because the expected problems with balance associated with the cerebellum in children with RD as cooccurring disorder or as a single deficit were not present. Future studies should investigate DCD and RD as separate diagnostic categories and always screen children with RD for co-occurring DCD, as children fulfilling the criteria for both developmental disorders may be distinguishable in terms of their perceptual-motor abilities.
ACKNOWLEDGMENTS
This research project has been performed within the framework of the master study
Human Movement Sciences of the Rijksuniversiteit Groningen. Financial support for this research was provided by the Alberta Centre for Child, Family and Community Research.
I would explicitly like to thank my supervisors, Libbe Kooistra and Marina Schoemaker, for all support and guidance. A special thanks to the investigative team: Barbara Ramage,
Ion Robu, Susan Crawford and Gordon Bullivant. This study would not have been possible without the pilot subjects and of course, most importantly, the participants and their parents.
REFERENCES
American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders
(4 th ed., DSM-IV). Washington, DC: American Psychiatric Association.
Berquin, P.C., Giedd, J.N., Jacobsen, L.K., Hamburger, S.D., Krain, A.L., Rapoport, J.L., et al.
(1998). The cerebellum in attention-deficit/hyperactivity disorder: A morphometric study.
Neurology, 50 , 1087-1093 .
Blishen, B.R., Carroll, W.K., & Moore, C. (1987). The 1981 socioeconomic index for occupations in Canada. Canadian Review of Sociology and Anthropology, 24, 465-488.
28
Balance Performance in Developmental Disabilities
Brookes, R. L., Nicolson, R. I., & Fawcett, A. J. (2007). Prisms throw light on developmental disorders. Neuropsychologia, 45, 1921-1930.
Brooks, V.B. (1986). The neural basis of motor control. Oxford University Press, New York.
Brooks, V.B., & Thach, W. (1981). Cerebellar control of posture and movement. In: Brooks, V.B.
(Ed.), Handbook of Physiology.
American Psychology Society, Motor Control, Washington,
DC, pp. 877-946.
Buderath, P., Gärtner, K., Frings, M., Christiansen, H., Schoch, B., Konczak, J., et al. (2008).
Postural and gait performance in children with attention deficit/hyperactivity disorder. Gait posture, article in press.
Castellanos, F.X., Giedd, J.N., Marsh, W.L., Hamburger, S.D., Vaituzis, A.C., Dickstein, D.P. et al. (1996). Quantitative brain magnetic resonance imaging in attention-deficit hyperactivity disorder. Archive of General Psychiatry, 53 , 607-616.
Castellanos, F.X., Giedd, J.N., Berquin, P.C., Walter, J.M., Sharp, W., Tran, T. et al. (2001).
Quantitative brain magnetic resonance imaging in girls with attention-deficit/hyperactivity disorder. American Journal of Psychiatry, 58, 289-295.
Castellanos, F.X., Lee, P.P., Sharp, W., Jeffries, N.O., Greenstein, D.K., Clasen, L.S. et al. (2002).
Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American Medical Association, 288,
1740-1748.
Cherng, R., Hsu, Y., Chen, Y., & Chen, J. (2007). Standing balance of children with developmental coordination disorder under altered sensory condition. Human movement science, 26, 913-926.
Collett, B., Ohan, J., & Myers, K. (2003). Ten-year review of rating scales. VI: Scales assessing externalizing behaviors. Journal of the American Academy of Child and Adolescent
Psychiatry, 42 , 1143-1170.
Conners, C.K. (1997). Conners’ Rating Scales-Revised: Users Manual. Toronto: Multi-Health
Systems Inc.
Conners, C. K., Sitarenios, G., Parker, J. D., & Epstein, J. N. (1998). The revised Conners' Parent
Rating Scale (CPRS-R): factor structure, reliability, and criterion validity. Journal of
Abnormal Child Psychology, 26(4), 257-268.
Deconinck, F. J. A., De Clercq, D., Van Coster, R., Oostra, A., Dewitte, G., Savelsbergh, G., J.,
P., et al. (2007). Sensory contributions to balance in boys with developmental coordination disorder. Adapted physical activity quarterly, 25, 17-35.
Dichgans, J., & Diener, H.C. (1985). Postural ataxia in late atrophy of the cerebellar anterior lobe and its differential diagnosis. In: M. Igarashi and F.O. Black (Eds.), Vestibular and Visual
Control on Posture and Locomotion Equilibrium. Basel: Karger, p. 282-289.
Diener, H.C., Dichgans, J., Bacher, M., & Guschlbauer, B. (1984). Characteristic alterations of long-loop “reflexes” in patients with Friedreich’s disease and late atrophy of the cerebellar anterior lobe. Journal of Neurology, Neurosurgery & Psychiatry, 47 (7), 679-685.
Durston, S., Hulshoff Pol, H.E., Schnack, H.G., Buitelaar, J.K., Steenhuis, M.P., Minderaa, R.B. et al. (2004). Magnetic Resonance imaging of boys with attention-deficit/hyperactivity disorder and their unaffected siblings. Journal of the American Academy of Child and
Adolescent Psychiatry, 43, 332-340.
Fawcett, A.J., & Nicolson, R.I. (1994). Persistent deficits in motor skill of children with dyslexia.
Journal of Motor Behavior, 27, 235–240.
Fawcett, A. J., & Nicolson, R. I. (1999). Performance of dyslexic children on cerebellar and cognitive tests. Journal of Motor Behavior, 31, 68–78.
Finch, A. J., Nicolson, R. I., & Fawcett, A. J. (2002). Evidence for a neuroanatomical difference within the olivo-cerebellar pathway of adults with dyslexia. Cortex, 38, 529-539.
29
Balance Performance in Developmental Disabilities
Forssberg, H., & Nashner, L.M. (1982). Ontogenetic development of postural control in man -
Adaptation to altered support and visual conditions during stance. Journal of Neuroscience, 2,
545-552.
Getchell, N., Pabreja, P., Neeld, K., & Carrio, V. (2007). Comparing children with and without dyslexia on the movement assessment battery for children and the test of gross motor development. Perceptual and motor skills, 105, 207-214.
Geuze, R.H. (2003). Static balance and developmental coordination disorder. Human Movement
Science, 22, 527-548.
Geuze, R. H. (2005). Postural control in children with developmental coordination disorder.
Neural Plasticity, 12, 183-196.
Gildenhuys, A. (2003). Development and validation of an experimental technique for studying dynamic stability during standing (microform). (Thesis (MSc), University of Calgary, 2003).
National Library of Canada, 279.
Grove, C. R., & Lazarus, J. C. (2007). Impaired re-weighting of sensory feedback for maintenance of postural control in children with developmental coordination disorder.
Human movement science, 26, 457-476.
Halperin, J., McKay, K. E., Martier, K., & Sharma, V. (1994). Attention, response inhibition and activity level in children: Developmental neuropsychological perspectives .
, in Advances in child neuropsychology , Springer Verlag: M. Tramontana and S. Hooper, Editors.
Henderson, S.E., & Sugden, D.A. (1992). Movement Assessment Battery for Children. London,
U.K.: The Psychological Corporation.
Hofstetter, H., (2007). Differentiating motor deficits in children with Attention Deficit
Hyperactivity Disorder or Fetal Alcohol Spectrum Disorder. (Thesis (MSc), University of
Groningen, 2007). Bibliotheek Sociale Wetenschappen, 61.
Horak, F.B., & Diener, H.C. (1994). Cerebellar control of postural scaling and central set in stance. Journal of Neurophysiology, 72 (2), 479-493.
Iversen, S., Berg, K., Ellertsen, B., & Tønnessen, F. (2005). Motor coordination difficulties in a municipality group and in a clinical sample of poor readers. Dyslexia, 11, 217-231.
Jongmans, M.J., Smits-Engelsman, B.C.M., & Schoemaker, M.M. (2003). Consequences of comorbidity of developmental coordination disorders and learning disabilities for severity and pattern of perceptual-motor dysfunction. Journal of Learning Disabilities, 36, 528-537.
Kadaba, M.P., Ramakrishnan, H. K., & Wootten, M.E. (1990). Measurement of Lower Extremity
Kinematics During Level Walking. Journal of Orthopaedic Research, 8, 383-392.
Kaplan, B. J., Wilson, B. N., Dewey, D. M., & Crawford, S. G. (1998). DCD may not be a discrete disorder. Human Movement Science, 17 , 471-490.
Kapoula, Z., & Bucci, M., P. (2007). Postural control in dyslexic and non-dyslexic children.
Neurology, 254, 1174-1183.
Loram, I. D., Maganoris, C. N., & Lakie, M. (2005). Human postural sway results from frequent, ballistic bias impulses by soleus and gastrocnemius. Journal of physiology, 564, 295-311.
Lundy-Ekman, L., Ivry, R., Keele, S., & Woollacott, M. (1991). Timing and force control deficits in clumsy children. Journal of Cognitive Neuroscience, 3, 367–376.
Martin, J. H. (2003). Neuroanatomy, text and atlas, third edition. New York: The Mc Graw-Hill
Companies.
Moe-Nilssen, R., Helbostad, J., Talcott, J., & Toennessen, F. (2003). Balance and gait in children with dyslexia. Experimental Brain Research, 150, 237–244.
Morton, S.M., & Bastian, A.J. (2004). Cerebellar control of balance and locomotion.
Neuroscientist,10, 247-259.
Mulder, M. J., Baeyens, D., Davidson, M. C., Casey, B. J., Van den Ban, E., Van Engeland, H., &
Durston, S. (2008). Familial vulnerability to ADHD affects activity in the cerebellum in addition to the prefrontal systems. Journal of the American Academy of Child Adolescent
Psychiatry, 47, 68-75.
30
Balance Performance in Developmental Disabilities
Nashner, L. M., Shupert, C. L., Horak, F. B., & Black, F. O. (1989). Organization of posture controls: An analysis of sensory and mechanical constraints. Progress in Brain Research, 80 ,
411–418.
Nicolson, R. I., Fawcett, A. J., Berry, E. L., Jenkins, H., Dean, P., & Brooks, D. J. (1999).
Association of abnormal cerebellar activation with motor learning difficulties in dyslexic adults. The Lancet, 353, 1662-1667.
Nolan, L., Grigorenko, A., & Thorstensson, A. (2005). Balance Control: Sex and Age Differences in 9- to 16-Years-Olds. Developmental Medicine & Child Neurology, 47, 449-454.
O’Hare, A., & Khalid, S. (2002). The association of abnormal cerebellar function in children with
Developmental Coordination Disorder and Reading Difficulties. Dyslexia, 8, 234-248.
Peterka, R.J. (2002). Sensorimotor integration in human postural control. Journal of
Neurophysiology, 88, 1097-1118.
Peterson, M.L., Christou, E., & Rosengren, K.L. (2006). Children achieve adult-like sensory integration during stance at 12-years-old. Gait and Posture, 23, 455-463.
Piek, J.P., & Skinner, R.A. (1999). Timing and force control during a sequential tapping task in children with and without motor coordination problems. Journal of the International
Neuropsychological Society, 5, 320-329.
Pitcher, T.M., Piek, J.P., & Barret, N.C. (2002). Timing and force control in boys with attention deficit hyperactivity disorder: subtype differences and the effect of comorbid developmental coordination disorder. Human Movement Science, 21 (5-6), 919-945.
Przysucha, E.P., & Taylor, M.J. (2004). Control of stance and Developmental Coordination
Disorder: The role of visual information. Adapted Physical Activity Quarterly, 21, 19-33.
Przysucha E., P., & Taylor, M., J. (2007). The nature and control of postural adaptations of boys with and without developmental coordination disorder. Adapted Physical Activity Quarterly,
25, 1-16.
Psychological Corporation. (2002). Wechsler individual achievement test second edition examiner’s manual. San Antonio: Psychological Corporation.
Raynor, A. (2001). Strength, power, and coactivation in children with developmental coordination disorder. Developmental Medicine and Child Neurology, 43 676-684.
Riley, P.O., Benda, B.J., Gill-Body, K.M., & Krebs, D.E. (1995). Phase plane analysis of stability in quiet standing. Journal of Rehabilitation, Research, and Development, 32, 227-235.
Smits-Engelsman, B.C., Wilson, P. H., Westenberg, Y., & Duysens, J. (2003). Fine motor deficiencies in children with developmental coordination disorder and learning disabilities: an underlying open-loop control deficit. Human Movement Science, 22 , 495-513.
Steger, J., Imhof, K., Coutts, E., Gundelfinger, R., Steinhausen, H.C., & Brandeis, D. (2001).
Attentional and neuromotor deficits in ADHD. Developmental Medicine & Child Neurology,
43, 172-179.
Stoodley, C.J., Fawcett, A. J., & Nicolson, R. I. (2006a). Balancing and pointing tasks in dyslexic and control adults. Dyslexia, 12, 276-288.
Stoodley, C.J., & Stein, J.F. (2006b). A processing speed deficit in dyslexic adults? Evidence from a peg-moving task. Neuroscience Letters, 399, 264-267.
Stoodley, C.J., Harrison, E.P., & Stein, J.F. (2006c). Implicit motor learning deficits in dyslexic adults. Neuropsychologia, 44, 795-798.
Stoodley, C.J., Fawcett, A. J., Nicolson, R. I., & Stein, J. F. (2005). Impaired balancing ability in dyslexic children. Experimental Brain Research, 167, 370-380.
Sugden, D. A. (2006). Proceedings from the Leeds consensus statement ’06:
Developmental
Coordination Disorder as a Specific Learning Difficulty . Leeds: United Kindom.
Sundermier, L., Woollacott, M., Roncesvalles, N., & Jensen, L. (2001). The development of balance control in children: comparisons of EMG and kinetic variables and chronological and developmental groupings. Experimental brain research, 136, 340-350.
31
Balance Performance in Developmental Disabilities
Tsai, C., Wu, S. K., & Huang, C. (2008). Static balance in children with developmental coordination disorder. Human movement science, 27, 142-153.
Valera, E. M., Faraone, S. V., Biederman, J., Poldrack, R. A., & Seidman, L. J. (2005).
Functional neuroanatomy of working memory in adults with attention-deficit/hyperactivity disorder. Biological Psychiatry, 57, 439-447.
Valera, E. M., Faraone, S. V., Murray, K. E., & Seidman, L. J. (2007). Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biological Psychiatry, 61, 1361-
1369.
Wechsler, D. (1991). Manual for the Wechsler Intelligence Scale for Children-Third Edition.
New York: Psychological Corporation.
Wechsler, D. (2003). The WISC-IV technical and interpretive manual.
San Antonio:
Psychological Corporation.
Wilson, B.N., Dewey, D., & Campbell, A. (1998). Developmental Coordination Disorder
Questionnaire (DCDQ).
Calgary: Alberta Children's Hospital Research Center.
32