HIV-infected - คณะแพทยศาสตร์ มหาวิทยาลัยเชียงใหม่
advertisement
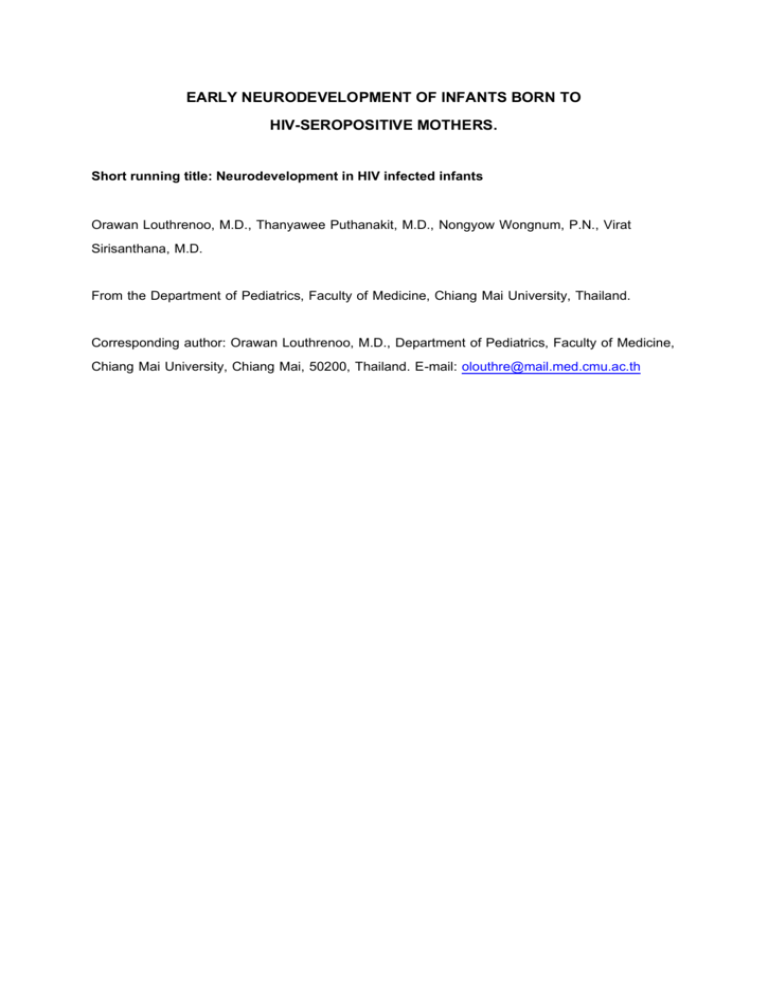
EARLY NEURODEVELOPMENT OF INFANTS BORN TO HIV-SEROPOSITIVE MOTHERS. Short running title: Neurodevelopment in HIV infected infants Orawan Louthrenoo, M.D., Thanyawee Puthanakit, M.D., Nongyow Wongnum, P.N., Virat Sirisanthana, M.D. From the Department of Pediatrics, Faculty of Medicine, Chiang Mai University, Thailand. Corresponding author: Orawan Louthrenoo, M.D., Department of Pediatrics, Faculty of Medicine, Chiang Mai University, Chiang Mai, 50200, Thailand. E-mail: olouthre@mail.med.cmu.ac.th Abstract Objective: To examine neurodevelopment during the first 12 months of life in infants born to HIV infected mothers. Methods: Infants born to HIV infected mothers receiving prenatal zidovudine monotherapy, who were followed at the Infectious Disease Clinic, Chiang Mai University Hospital, were enrolled in this study. Neurodevelopmental assessment was administered at the age of 12 months by using Bayley Scales of Infant Development (BSID). Confirmed HIV infection status was performed at 18 months of age. Results: Thirty-nine infants, 10 infected and 29 uninfected cases, were studied. Demographic and perinatal characteristics including birth weight, length, head circumference, prematurity, maternal age, and maternal education were not different between 2 groups. At 12 months, growth parameters of HIV infected and non-infected groups were not different, but Mental Developmental Index (MDI) and Psychomotor Developmental Index (PDI) were lower significantly in HIV-infected group than non-infected group (MDI=90 vs. 99, p=0.001; PDI=83 vs. 96, p <0.001, respectively). In the HIV infected group, infants with symptomatic HIV infection had lower MDI and PDI scores than asymptomatic ones. Conclusion: HIV infected infants showed early lower developmental scores. Neurodevelopment may be one of the early markers of disease progression of infants with HIV infection within the first 12 months. Key words: neurodevelopment, infants, HIV infection พัฒนาการระยะแรกของเด็กทารกที่เกิ ดจากแม่ติดเชื้อเอชไอวี หัวเรื่องย่อสัน้ : พัฒนาการของเด็กทารกติดเชือ้ เอชไอวี อรวรรณ เลาห์เรณู, พ.บ., ธันยวีร์ ภูธนกิจ, พ.บ., นงเยาว์ วงศ์นุ่ม, ประกาศนียบัตรผูช้ ่วยพยาบาล, วิรตั ศิรสิ นั ธนะ, พ.บ. ภาควิชากุมารเวชศาสตร์, คณะแพทยศาสตร์ มหาวิทยาลัยเชียงใหม่, เชียงใหม่ 50200 ผูร้ บั ผิดชอบบทความ: พ.ญ. อรวรรณ เลาห์เรณู ภาควิชากุมารเวชศาสตร์, คณะแพทยศาสตร์ มหาวิทยาลัยเชียงใหม่, เชียงใหม่ 50200 บทคัดย่อ วัตถุประสงค์ เพื่อตรวจประเมินพัฒนาการในช่วง 12 เดือนแรก ในเด็กทารกทีเ่ กิดจากมารดาติดเชือ้ เอชไอวี วิธกี าร ได้ทาการตรวจประเมินพัฒนาการในเด็กทารกทีเ่ กิดจากมารดาติดเชือ้ เอชไอวีซง่ึ ได้รบั ยา zidovudine ป้ องกันขณะตัง้ ครรภ์ ทีไ่ ด้ตดิ ตามการรักษาในหน่วยโรคติดเชือ้ ตึกผูป้ ่ วยนอกกุมารเวชกรรม โรงพยาบาลมหาราชนครเชียงใหม่ เมือ่ อายุ 12 เดือนโดยใช้ Bayley Scales of Infant Development (BSID) และทาการตรวจยืนยันสถานะการติดเชือ้ เอชไอวีของเด็กเมือ่ อายุ 18 เดือน ผลการศึกษา เด็กจานวน 39 คน ติดเชือ้ 10 คนและไม่ตดิ เชือ้ 29 คนไม่พบความแตกต่างของลักษณะทางสังคมและภาวะระหว่างการตัง้ ครรภ์ ซึง่ รวมถึงน้าหนัก ความยาว และเส้นรอบวงศีรษะแรกคลอด การคลอดก่อนกาหนด อายุและการศึกษาของมารดาระหว่างเด็กทัง้ สองกลุ่ม ทีอ่ ายุ 12 เดือนการเจริญเติบโตไม่มคี วามแตกต่างแต่ค่าดัชนีของพัฒนาการทัง้ Mental Developmental Index (MDI) และ Psychomotor Developmental Index (PDI) ต่ากว่าในเด็กทีต่ ดิ เชือ้ (MDI=90 และ 99, p=0.001; PDI=83 และ 96, p <0.001 ตามลาดับ) ในกลุ่มเด็กทีต่ ดิ เชือ้ เด็กทีแ่ สดงอาการของโรคเอชไอวีมคี ่าดัชนีของพัฒนาการต่ากว่าเด็กทีไ่ ม่มอี าการ สรุปผลการศึกษา เด็กทีต่ ดิ เชือ้ เอชไอวีแสดงพัฒนาการช้าได้ตงั ้ แต่ช่วงแรกของอายุ พัฒนาการอาจเป็ นตัวบ่งชีอ้ นั หนึ่งทีบ่ อกถึงการดาเนินโรคในเด็กทีต่ ดิ เชือ้ เอชไอวีในช่วงอายุ 12 เดือนแรก คาสาคัญ: พัฒนาการ, เด็กทารก, การติดเชือ้ เอชไอวี HIV infection often causes impairment of growth and development in children. Numerous observational data describe neurological involvement and developmental delay in pediatric HIV infection.1-6 Neurological abnormalities are related to a primary HIV infection or may be from HIV-related morbidity. The most common neurological findings in children with HIV infection include progressive encephalopathy, nonprogressive developmental delay, and motor dysfunction.1, 7 Failure to gain weight could also be a direct consequence of HIV infection, secondary to HIV-related illness, or be associated with adverse social environment and may occur later. Immunological markers were identified to be associated with disease progression. Neurological involvement and impaired developmental milestones are often early markers of HIV infected infants as well and may precede other signs of disease progression.8, 9 Therefore, the purpose of this study is to examine neurodevelopment on the mental and motor functioning during the first 12 months of life in infants born to HIV infected mothers. Methods Study population: From January 2001 to December 2002, infants born to HIV infected mothers who were followed up in the Infectious Disease Clinic, Chiang Mai University Hospital were enrolled. Oral informed consent was obtained from their parents. At the time of this study, zidovudine monotherapy is included in standard perinatal care,10, 11 so all of the mothers received prenatal zidovudine. Measurement: Demographic characteristics and perinatal history were obtained by interviewing mothers and from medical records. Growth and neurodevelopmental assessments were performed at 12 months of age using the Bayley Scales of Infant Development (BSID).12 The BSID consists of mental and psychomotor scales. It is widely used to evaluate sensory-perceptual acuity, discrimination and response ability, problem solving ability, verbal communication, and motor coordination and skills for infants from 0-42 months of age. The neurodevelopmental assessment was performed by the developmental pediatrician (O.L.). Prematurity was adjusted as per instructions for calculating developmental scores. Results are described as Mental Developmental Index (MDI) and Psychomotor Developmental Index (PDI) which have an average of 100 and a standard deviation of 15. A score of MDI or PDI less than 85 is considered below average. The HIV infection status of infants was documented and confirmed at 18 months of age. Because HIV status was not certain in infants at 12 months of age, there was a natural blinding of the examiner during this time. The study was approved by the Research Ethics Committee of Faculty of Medicine. Statistical analysis: Data were analyzed by using the SPSS 10.0 program (SPSS Inc, Chicago, IL). A Chi square for proportions and a Student t test for continuous variables were used to compare the two groups. A p value of less than 0.05 is considered statistically significant. Results Between January 2001 to December 2002, there were 40 pairs of infants and caregivers enrolled in the study. Because 1 mother refused the blood test to confirmed HIV status at the age of 18 months, 39 infants were studied including 10 infected cases. Perinatal characteristics including birth weight were not different between HIV infected and non-infected infants (Table 1). More male infants were found in the infected group but not statistically different. Infected and uninfected infants were from similar social backgrounds as the mother’s age and education were not significantly different between the two groups. All of the mothers received zidovudine monotherapy prenatally except for one in the non-infected group. At 12 months of age there was no significant difference in growth parameters between HIV infected and non-infected groups (Table 2). Mean MDI and PDI were significantly lower in HIVinfected infants. Abnormal MDI or PDI was found only in HIV infected group. Among 10 infected cases, 5 had non-specific HIV symptoms and had lower MDI and PDI scores than asymptomatic infected and non-infected infants (Table 3). Discussion: Of the 39 infants, 10 were found to be infected at the age of 18 months, confirmed by HIV antibodies. There was no difference in characteristic background including gender, growth parameters at birth, or prematurity. In previous studies,13, 14 birth weight was not associated with HIV infection status of infants born to HIV-infected women, which was consistent with this study. Maternal age and education were similar between infected and uninfected infants. All but one mother in the uninfected group received prenatal zidovudine. All pregnancies were normal labor without a complication of chorioamnionitis which has been reported to be a risk factor for perinatal transmission of HIV.15 At the 12 months of age, when HIV status was not yet definite, growth parameters were not different between infected and non-infected groups. The slower of growth of infected infants can occur from HIV-related symptoms, so asymptomatic cases may not show growth failure. However, neurodevelopment quotients in terms of MDI and PDI were found to be significant lower in infected infants than infants who were HIV exposed but uninfected. The rate of development was reported to be slower in infected infants at 3 months of age which was much slower over time.3 Contrary, it was also reported that the difference of development was not found until 12 months of age.16 The relationship of head circumference and neurodevelopment was not found in this study. Growth impairment might occur later than neurological involvement. A small difference in growth of infected and non-infected infants was found as early as 3-4 months of age before the time of prenatal zidovudine monotherapy.17-19 Below average MDI or PDI score or developmental delay were found only in the infected group. In symptomatic cases, MDI and PDI scores were significant lower than infected infants who had no symptoms. More severe neurological involvement was described in infants with the clinical manifestations of symptomatic HIV infection.20 The study sample was too small to evaluate the effects of HIV status and other variables, such as prematurity and maternal education of less than 9 completed years, that may be associated with low developmental score.8 There were some limitations in this study. The small sample size may affect the statistical result of the study. The study population was not randomized and only some of the demographic data were obtained to compare between infected and non-infected infants. In summary, our findings documented early abnormal neurodevelopmental outcome in pediatric HIV infection which were similar to previous studies conducting prior to the time of prenatal zidovudine.3-5, 16, 21, 22 Larger sample and long-term follow up would give more information. Careful monitoring of developmental growth is a necessary component of comprehensive medical care in infants with HIV infection. References: 1. Fowler MG. Pediatric HIV infection: Neurologic and neuropsychologic findings. Acta Paediatr Suppl 1994; 400:59-62. 2. Pollack H, Kuchuk A, Cowan L, Hacimamutoglu S, Glasberg H, David R, et al. Neurodevelopment, growth, and viral load in HIV-infected infants. Brain Behav Immun 1996; 10:298-312. 3. Gay CL, Armstrong FD, Cohen D, Lai S, Hardy MD, Swales TP, et al. The effects of HIV on cognitive and motor development in children born to HIV-seropositive women with no reported drug use: birth to 24 months. Pediatrics 1995; 96:1078-82. 4. Chase C, Vibbert M, Pelton SI, Coulter DL, Cabral H. Early neurodevelopmental growth in children with vertically transmitted human immunodeficiency virus infection. Arch Pediatr Adolesc Med 1995; 149:8505. 5. Nozyce M, Hittelman J, Muenz L, Durako SJ, Fischer ML, Willoughby A. Effect of perinatally acquired human immunodeficiency virus infection on neurodevelopment in children during the first two years of life. Pediatrics 1994; 94:883-91. 6. Blanchette N, Smith ML, Fernandes-Penney A, King S, Read S. Cognitive and motor development in children with vertically transmitted HIV infection. Brain Cogn 2001; 46:50-3. 7. Mintz M. Neurological and developmental problems in pediatric HIV infection. J Nutr 1996; 126:2663S2673S. 8. Chase C, Ware J, Hittelman J, Blasini I, Smith R, Llorente A, et al. Early cognitive and motor development among infants born to women infected with human immunodeficiency virus. Women and Infants Transmission Study Group. Pediatrics 2000; 106:E25. 9. Llorente A, Brouwers P, Charurat M, Magder L, Malee K, Mellins C, et al. Early neurodevelopmental markers predictive of mortality in infants infected with HIV-1. Dev Med Child Neurol 2003; 45:76-84. 10. Fernandez AD, McNeeley DF. Management of the infant born to a mother infected with human immunodeficiency virus type 1 (HIV-1): current concepts. Am J Perinatol 2000; 17:429-36. 11. Krist AH, Crawford-Faucher A. Management of newborns exposed to maternal HIV infection. Am Fam Physician 2002; 65:2049-56. 12. Bayley N. Bayley Scales of Infant Development 2nd ed. The Psychological Corporation. San Antonio: Hartcourt Brace & Company, 1993. 13. Miller TL, Evans SJ, Orav EJ, Morris V, McIntosh K, Winter HS. Growth and body composition in children infected with the human immunodeficiency virus-1. Am J Clin Nutr 1993; 57:588-92. 14. Tovo PA, de Martino M, Gabiano C, Galli L, Cappello N, Ruga E, et al. Mode of delivery and gestational age influence perinatal HIV-1 transmission. Italian Register for HIV Infection in Children. J Acquir Immune Defic Syndr Hum Retrovirol 1996; 11:88-94. 15. Fowler MG, Simonds RJ, Roongpisuthipong A. Update on perinatal HIV transmission. Pediatr Clin North Am 2000; 47:21-38. 16. Wachtel RC, Tepper VJ, Houck D, McGrath CJ, Thompson C. Neurodevelopment in pediatric HIV infection. The use of CAT/CLAMS. Clinical Adaptive Test/Clinical Linguistic and Auditory Milestone Scale. Clin Pediatr (Phila) 1994; 33:416-20. 17. The European Collaborative Study. Weight, height and human immunodeficiency virus infection in young children of infected mothers. Pediatr Infect Dis J 1995; 14:685-90. 18. Lepage P, Msellati P, Hitimana DG, Bazubagira A, Van Goethem C, Simonon A, et al. Growth of human immunodeficiency type 1-infected and uninfected children: a prospective cohort study in Kigali, Rwanda, 1988 to 1993. Pediatr Infect Dis J 1996; 15:479-85. 19. Louthrenoo O, Sirisanthana V, Rangsiyanond P, Sirakamol D, Sirivatanapa P. Growth and developmental outcome of infants born to HIV infected mothers. Chiang Mai Med Bull 1998; 37:69-73. 20. Belman AL, Diamond G, Dickson D, Horoupian D, Llena J, Lantos G, et al. Pediatric acquired immunodeficiency syndrome. Neurologic syndromes. Am J Dis Child 1988; 142:29-35. 21. Drotar D, Olness K, Wiznitzer M, Guay L, Marum L, Svilar G, et al. Neurodevelopmental outcomes of Ugandan infants with human immunodeficiency virus type 1 infection. Pediatrics 1997; 100:E5. 22. Aylward EH, Butz AM, Hutton N, Joyner ML, Vogelhut JW. Cognitive and motor development in infants at risk for human immunodeficiency virus. Am J Dis Child 1992; 146:218-22. Table 1. Demographic and perinatal characteristics of HIV infected and non-infected infants. HIV-infected HIV-negative p Value (n=10) (n=29) Gender: male 5/10 (50%) 8/29 (28%) 0.25 Prematurity 2/10 (20%) 5/29 (17%) 0.59 Birthweight (gm) 2679 576 2648 420 0.86 Length (cm) 47.4 3.2 46.9 2.6 0.64 Head circumference (cm) 32.4 1.6 32.1 2.4 0.75 Maternal age (yr) 26.5 5.0 28.1 4.9 0.39 Maternal education (yr) 9.5 4.7 9.5 3.1 0.97 Table 2. Growth parameters at 12 months of age and developmental indices of HIV infected and non-infected infants. HIV-infected HIV-negative (n=10) (n=29) 12.3 0.8 12.2 0.2 0.21 Weight (gm) 9194 1683 9305 1177 0.82 Length (cm) 72.4 4.3 73.3 2.8 0.44 Head circumference (cm) 45.4 1.6 44.8 1.4 0.32 Mean Mental Developmental Index 90.0 9.6 99.2 6.4 0.001 Mean Psychomotor Developmental Index 83.3 9.8 96.0 7.9 < 0.001 Abnormal MDI or PDI score 5/10 (50%) 0/29 (0%) < 0.001 Age (mo) p Value Table 3. Mental and Psychomotor Developmental Indices of symptomatic and asymptomatic HIV infected and non-infected infants. HIV-infected HIV-negative p Value Symptomatic (n=5) Asymptomatic (n=5) (n=29) Mean MDI 88.0 13.3 92.0 4.3 99.2 6.4 0.005 Mean PDI 79.2 12.7 87.4 3.6 96.0 7.9 < 0.001 Figure 1 Mental and Psychomotor Developmental Indices in infants of mothers with HIV infection. Mental Developmental Index (MDI) p value = 0.005 120 100 80 60 symptomatic HIV asymptomatic HIV HIV uninfected Psychomotor Developmental Index (PDI) p value = <0.001 120 100 80 60 symptomatic HIV asymptomatic HIV HIV uninfected