Fluid and Electrolyte Study Guide
advertisement

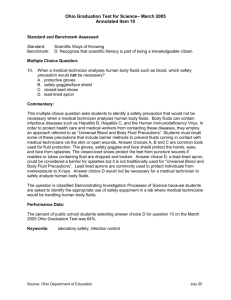
Fluid, Electrolyte and Acid/Base Balance Scientific Knowledge Base: Distribution of Body Fluids Intracellular Fluids (ICF) Fluids within cells 42% of total body weight Two thirds of total body water 28 liters in males 20 liters in females Extracellular Fluid (ECF) Fluid outside of cells Interstitial, intravascular, and transcellular Makes up 17% of total body weight Composition of Body Fluids Electrolyte: An element or compound that, when dissolved or dissociated in water or solvent, separates into ions Ions: Cations: positively charged Anions: negatively charged Movement of Body Fluids Osmosis: Movement of a solute from an area of lesser to one of greater concentration Osmolality Osmolarity Hypertonic Isotonic Hypotonic Diffusion: Random movement of a solute through a semipermeable membrane from higher to lower concentration Filtration: Movement across a membrane, under pressure, from higher to lower pressure Active transport: Movement of ions against osmotic pressure to an area of higher pressure Fluid Intake Regulated by thirst Osmoreceptors monitor serum oncotic pressure; when osmolality increases, the hypothalamus stimulates thirst Ex: eating salty chips increases oncotic pressure and stimulates thirst via the hypothalamus Ex: If excess fluid lost in excessive vomitting, diarrhea, or hemorrhage, hypovolemia occurs and the hypothalamus stimulates thirst Average adult intake = 2500 ml (in food and drink) Thirst requires alert state; infants, elderly and those with neuro problems are at risk for dehydration Hormonal Regulation When blood osmolarity increases (increased concentration of salt or decreased fluids): Antidiuretic hormone (ADH) is released which works on kidneys to “save water”. Water is returned to systemic circulation, diluting the blood and decreasing osmolarity. Urine output decreases. Renin responds to less blood reaching the kidney; produces angiotensin I which converts to angiotensin II which causes vasoconstriction and thus increases blood flow to the kidneys (and stimulates release of aldosterone) Aldosterone is released which acts on kidneys to “save salt” and “secrete potassium”. Sodium retention then leads to water retention. Fluid Output Regulation Fluid output occurs via: kidneys, skin, lungs and GI tract Kidneys produce 1200-1500 ml urine/day The body loses about 500ml of fluid through the skin daily Sensible loss= perspiration; insensible loss is continuous and nonperceptual The lungs expire about 400-500ml/water daily (insensible loss) GI tract account for only 100-200 ml/fluid loss per day, but can become a major site of fluid loss because 3-6 Liters of fluid is reabsorbed daily Therefore total fluid gains: 2200-2700 ml/day and total losses are 2200-2700 ml/day Major Electrolytes Cations: Sodium (Na+) Potassium (K+) Calcium (Ca2+) Magnesium (Mg2+) Anions: Chloride (Cl-) Bicarbonate (HCO3–) Phosphate (PO43-) Acid-Base Balance pH is a measure of acidity (lower the pH, the higher the acidity); normally 7.35-7.45 Acidotic normal blood pH alkalotic <7.35 7.35 – 7.45 >7.45 pH is a balance between an acid, carbon dioxide (CO2) which the lungs regulate, and a base, bicarbonate (HCO3), which the kidneys regulate Regulation of Acid-Base Balance Chemical: Carbonic acid and bicarbonate buffer system Biological: Occurs when hydrogen ions are absorbed or released by cells Physiological: Buffers are located in lungs and kidneys Disturbances in Fluid, Electrolyte, and Acid-Base Balances Fluid: Isotonic FV Deficit FV Excess Osmolar Dehydration Water excess Electrolyte: Hyponatremia Hypernatremia Hypocalcemia Hypercalcemia Hypomagnesemia Hypermagnesemia Hypochloremia Hyperchloremia Acid-Base: Respiratory acidosis Respiratory alkalosis Metabolic acidosis Metabolic alkalosis Disturbances in Fluids Fluid Volume Deficit (FVD) Body loses BOTH water and electrolytes from ECF in similar proportions (isotonic so serum sodium remains normal) = HYPOVOLEMIA (since initially lost from intravascular compartment) Causes: bleeding, vomitting, diarrhea, fever, use of diuretics, excessive perspiration, decreased oral intake Symptoms: Decreased BP, tachycardia and weak pulse, dry mucous membranes, poor skin turgor, decreased urine output, confusion Labs: increased: urine specific gravity, HCT, BUN Treatment: IV Therapy (isotonic fluids) Fluid Volume Excess (FVE) Body retains both water and sodium in similar proportions in ECF (so serum sodium remains normal) = HYPERVOLEMIA Causes: Excessive intake of sodium in diet or meds Too rapid sodium-containing IVs Diseases that alter regulatory mech: CHF, RF, cirrhosis of liver Symptoms: Weight gain (>2lbs/24hrs), edema, increased BP, crackles in lungs, dyspnea, bounding pulses, distended jugular vein Labs: decreased HCT and BUN (hemodilution) Treatment: fluid and sodium restriction, diuretics Osmolar Imbalances Dehydration Loss of Water Causes: Diabetes, Administration of hypertonic fluids, loss of thrist drive Symptoms: Dry mucous membranes and skin, thirst, irritability, coma Labs: increased sodium and serum osmolality Water Excess Excess of Water Causes: Excess water intake Symptoms: decreased LOC, coma Labs: decreased sodium and decreased serum osmolality Disturbances in Electrolytes Sodium, Potassium, and Calcium Sodium (Na+): 135-145 mEq/L Major influence on maintaining water balance; located in ECF Hyponatremia: lower than normal sodium concentration Hypernatremia: higher than normal sodium concentration; usually due to excess water loss; common symptom dry sticky mucous membranes Potassium (K+): 3.5-5 mEq/L Predominant electrolyte in ICF Body does not conserve it well, so an increase in fluid output results in hypokalemia. (Therefore potassium supplementation is important with diuretics) Hyperkalemia can occur in kidney failure or with potassium sparing diuretics Any potassium imbalance can result in cardiac abnormalities Calcium (Ca2+): 4.5 – 5.5mg/dl Hypocalcemia: low calcium; may cause cramping, numbness, tingling Hypercalcemia: high calcium; may cause N/V, weakness, low LOC, cardiac arrest Magnesium and Chloride Magnesium (Mg 2++) 1.5 – 2.5 mEq/L Hypomagnesium: occurs with malnutrtion and/or malabsorption Hypermagnesium: decreases muscle and nerve function Chloride (Cl-) 95-105 mEq/L Hypochloremia: occurs with sodium loss or loss of HCL acid Hyperchloremia: occurs with decrease in bicarbonate or increase in sodium Both common with acid base imbalance Disturbances in Acid Base Arterial Blood Gases Arterial Blood Gases (ABGs) is best way to evaluate acid-base balance Major components: pH (7.35-7.45): acidotic if less and alklotic if more (see diagram at end of PPT) PaCO2 (35-45): pressure of carbon dioxide (an acid) If hyperventilating (thus “blowing off CO2): less than 35 (respiratory alkalosis) If hypoventilating (thus retaining CO2): greater than 45 (respiratory acidosis) PaO2: (80-100): oxygen pressure in blood SaO2: (95-100%): oxygen saturation HCO3: (22-26): bicarbonate (a base); kidneys excrete or produce it to maintain a normal balance Metabolic acidosis: less than 22 Metabolic alkalosis: greater than 26 ROME You can also remember the acronym ROME. R=Respiratory O=Opposite (meaning that if your PACO2 and pH are of opposite values, you have a resp problem) M=Metabolic E=Equal (meaning that if your values are equal, both inc or both dec, then you have metabolic prob). Ex. Respiratory Acidosis pH PACO2 HCO3 Ex. Metabolic Alkalosis pH PACO2 HCO3 Types of Acid-Base Imbalances Respiratory acidosis: increased acid level resulting in decreased pH due to excess CO2 retained Ex: patient with COPD retaining CO2 Respiratory alkalosis: decrease in acid level resulting in increased pH due to CO2 being “blown off” Ex: patient anxious and hyperventilating Metabolic acidosis: increased acid level resulting in decreased pH due to loss of HCO3 (Ex: starvation, excessive exercise, DKA, renal failure) Metabolic alkalosis: decreased acid level resulting in increased pH and increased HCO3 (common cause: vomitting and NG suctioning) The Nursing Process Focused Nursing Assessments History: consider who is at risk for imbalance Age (infants, elderly); chronic disease (CHF, RF); recent surgery, trauma or burns; temp extremes; diet history; vigorous exercise; meds (espec. Diuretics) Daily weights (>2lbs/24hrs significant) Vital signs (espec. BP, pulses) 24 hour Intake and Output Input: measure ice chips, foods that become liquid @ room temp, IV meds, tube feedings Output: include urinary output, vomitus, liquid feces, tube drainage, wound drainage; consider insensible losses with diaphoresis and hyperventilation Labs: urine specific gravity, HCT, BUN, electrolytes, ABGs Other focused assessments Urine amount and appearance Skin turgor or edema Mucous membranes Lung sounds Mental status, confusion Common Nursing Diagnoses Excess fluid volume Deficient fluid volume Risk for imbalanced fluid volume Therapeutic Nursing Interventions Facilitate fluid intake when needed (FVD) ID fluids the client likes; avoid caffeine because of diuretic effect; help select foods that are liquid @ room temp Teach family members to offer fluids regularly to clients who cannot meet their own needs Help restrict intake when needed (FVE) Educate that ice chips, gelatin, ice cream are considered fluids; Allow half total volume on day shift Place fluids in small containers so looks “full” Offer ice chips instead of water Avoid salty or sweet foods because cause thirst Require frequent mouth care Restrict dietary sodium if ordered Provide IV fluids as ordered Isotonic fluids commonly used for FVD (Ex: D5W, 0.9NS) Potential problems with IV therapy Infiltration (fluid escapes into subq tissue) Signs: swelling, pallor, coldness, pain at site, decrease in flow rate Tx: Discontinue IV and restart at different site Phlebitis (inflammation of vein) Signs: localized tenderness, redness, warmth and mild edema of vein above insertion site Tx: Discontinue IV and restart at different site. Apply warm moist compresses Infection Signs: fever, chills, malaise, pain, swelling, inflammation or pus at IV site Tx: Discontinue IV, notify MD Prevention: Maintain sterile technique; change tubing q24hrs if agency policy permits Speed shock (infusing IV too rapidly) Signs: pounding headache, rapid pulse, chills, back pain, dyspnea Tx: Discontinue IV, notify MD, monitor VS Fluid Overload (too large of volume infused) Signs: dyspnea, engorged neck veins, increased BP Tx: slow infusion rate, notify MD, monitor VS Embolus (thrombus or air enters vein) Signs: depends on location of infarction (e.g., cerebral, pulmonary): dyspnea, sudden pain Tx: Report any sudden pain or dyspnea immediately Evaluation It is possible for patient’s condition to change rapidly, so monitor closely In acute alterations monitor: Mucus membranes, skin turgor, BP, I/O trend, daily lab results In chronic situations, monitor patient’s ability to follow diet and fluid restrictions and med schedules Routinely review if you have met patient’s expectations for care: “Tell me if I have helped you feel more comfortable.”