Post Test - AMC Academic Systems
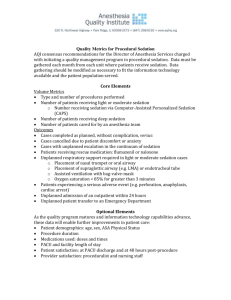
advertisement

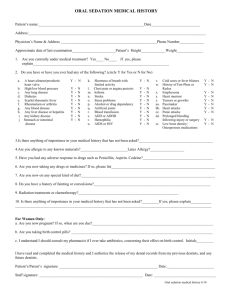
Albany Medical Center Procedural Sedation 2007 Post Test 1. The pre-sedation requirements of a patient undergoing moderate sedation include: a. Completion of Aldrete score b. Continuous monitoring of airway, respiratory status, head position, color and pain c. Administer fluid challenge per credentialed practitioner for hypotension d. Completion of the pre-procedural sedation checklist and assessment form 2. Oxygen therapy during moderate sedation a. Is administered on all patients b. Should only be used if the patient has respiratory symptoms c. Is administered when the patient’s baseline O2 sat is less than 95% d. Is never utilized 3. Continuous EKG monitoring must be utilized during moderate sedation EXCEPT when the patient a. Appears nervous or agitated- Ramsay 1 b. Has cardiovascular disease or is undergoing a procedure in which dysrhythmias are anticipated c. Is a child without a cardiac history undergoing a procedure not expected to induce arrhythmias d. Is overweight and over the age of 50 4. Prior to the administration of procedural sedation the following items must be prepared, operational, and immediately available: a. Continuous pulse oximetry, airway equipment, and cardiac monitor b. Supplemental oxygen, bag-valve-mask ambu, and reversal agents c. Suction equipment, automated blood pressure monitor, emergency cart and age appropriate defibrillator d. All of the above 5. The minimum number of people that need to be available when administering moderate sedation to adults are: a. 1- a service resident b. 2- the credentialed attending physician performing the procedure and the credentialed RN monitor c. 3- the attending physician performing the procedure, the credentialed physician prescribing the sedation and the credentialed RN monitor d. There is no required number 6. Which of the following statements about opioids and apnea is true? a. Apnea can occur even in responsive patients b. Apnea is an unlikely, uncommon adverse reaction c. Apnea does not usually lead to cardiac arrest d. Apnea does not occur, since the main effect of opioids is analgesia 7. Which of the following statements about midazolam (Versed) is true? a. It is half as potent as diazepam b. It is best used in the 5mg/ml formulation c. It is three times as potent as diazepam d. It has a slower onset of action than diazepam 8. Which of the following statements about the use of benzodiazepines in procedural sedation is true? a. The total initial dose should be decreased when administered with an opioid b. Adjustment in dosing is needed when giving an opioid c. Adjustment in dosing is needed with advanced age d. All of the above 9. Which of the following statements about using naloxone (Narcan) to reverse opioid effects is true? a. It should be given in small increments and titrated to patient response b. It should be given as an IV continuous drip c. It does not antagonize the respiratory system d. It should only be used in children 10. Which of the following can not be diluted and can irritate veins: a. Fentanyl (Sublimaze) b. Midazolam (Versed) c. Flumazenil (Romazicon) d. Diazepam (Valium) 11. Which of the following must be given slowly as rapid infusion may cause hypotension and respiratory depression: a. Fentanyl (Sublimaze) b. Midazolam (Versed) c. Flumazenil (Romazicon) d. Diazepam (Valium) 12. Which of the following is 100 times more potent than morphine and has a shorter half-life: a. Fentanyl (Sublimaze) b. Midazolam (Versed) c. Flumazenil (Romazicon) d. Diazepam (Valium) 13. Which of the following is a benzodiazepine antagonist: a. Fentanyl (Sublimaze) b. Midazolam (Versed) c. Flumazenil (Romazicon) d. Diazepam (Valium) 14. If hypotension develops during procedural sedation, which intervention should the RN initiate: a. Fluids as KVO and elevate legs b. Initiation of a fluid challenge per credentialed practitioner c. Bolus dose of dopamine followed by continuous drip d. Stimulate patient and instruct to take deep breaths 15. Guidelines for patients at discharge after procedural sedation should include: a. Written release of the hospital or health care agency from responsibility b. Discussion of all potential side effects of the agents used c. Where to follow-up for continued care d. Written information outlining restrictions and safety information to the patient and/or family 16. After receiving morphine and diazepam for sedation, the patient loses consciousness and becomes dusky in appearance as the oxygen saturation decreases rapidly from 95% to 85%. Reasonable initial responses include all of the following EXCEPT: a. Administration of oxygen at 100% b. Administer reversal agents c. Consider assisted ventilation d. Continue the procedure and recheck patient in 2 minutes 17. During moderate sedation, how frequently are vital signs monitored in a patient who responds to voice and commands (MRS 3)? a. Every 2 minutes b. Every 5 minutes c. Every 10 minutes d. Every 15 minutes 18. Doses of benzodiazepines should be reduced when used in combination with other CNS depressants and in the following populations: a. Elderly patients b. Patients who are pregnant c. Patients with cardiovascular disease d. Patients with a baseline Ramsay score <3 19. Desired effects of procedural sedation include all of the following except: a. Relaxation and cooperation b. Improvement in the quality of diagnostic tests c. No response to noxious stimulation d. Pain score of < 3 20. Moderate sedation is defined as: a. A state that allows a person to tolerate an unpleasant procedure while maintaining adequate cardiopulmonary function and the ability to respond purposefully to verbal or tactile stimulation b. A controlled state of sedation whereby the patient is not easily aroused and is unable to respond c. A depressed level of consciousness whereby the patient can maintain a patent airway but does not respond to physical stimulation d. A drug induced depression of consciousness during which patients do respond purposefully to verbal commands either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patent airway and spontaneous ventilation is adequate. 21. Which of the following statements about ketamine is false?\ a. Produces dissociative anesthesia b. Can be mixed with midazolam c. Can cause “psychic reactions” d. Is reversed with flumazenil 22. When administering sedation to children versus adults, which age-specific equipment is needed? a. size/volume appropriate airway equipment b. adjustable oxygen administration equipment c. emergency medications d. cardiac monitors 23. Special considerations for the pediatric population include: a. Age-appropriate information on medications, developmental level, methods to decrease separation anxiety, and potential nonpharmacologic interventions b. Automatic monitoring devices c. A pediatric sedation area d. Monitor vital signs 24. A pediatric patient weighs 35 pounds and 0.05 mg/kg IV of midazolam is ordered. The calculated dose for administration is: a. 0.2 mg b. 0.8 mg c. 1.6 mg d. 2.0 mg 25. Thoracic muscle rigidity with poor pulmonary compliance is reported with rapid infusion and high doses of a. Midazolam b. Thiopental c. Brevital d. Fentanyl 26. Which of the following is a correct statement about moderate (conscious) sedation therapy guidelines for NPO status... a. No solid intake for 8 hours b. < 2 years old, NPO of clear liquids for 4 hours c. > 2 years old, NPO of clear liquids for 3 hours d. No breast milk within 4 hours or clear liquids within 2 hours 27. Describe the steps you would take if your patient experiences loss of airway: a. Intubation b. Reposition airway alignment, increase FiO2 to 100%, utilize airway adjuncts, be prepared to assist ventilation c. Increase O2 and monitor oxygen saturation every 2 minutes d. Give Narcan 0.4 mg IVP 28. Patients receiving methohexital are at greatest risk for: a. Respiratory depression b. Vomiting c. Increased intracranial pressure d. Bradycardia 29. Monitoring parameters during procedural sedation for a patient who is cooperative, oriented and tranquil are: a. check vital signs and MRS q 2 minutes X 5, then until MRS is 2 b. check vital signs and MRS q 5 minutes X 2, then q 15 minutes until procedure is complete c. check vital signs and MRS q 5 minutes until procedure is complete d. check vital signs and MRS X 1, recheck if patient deteriorates 30. All of the following are true about pre-medication EXCEPT: a. Pre-medication is the limited use of an individual anxiolytic, sedative, or analgesic medication for the purpose of preparing patients that are anxious, agitated or claustrophobic for a non/minimally painful or invasive procedure b. The Procedural Sedation: Moderate (Conscious Sedation) Protocol does not apply to pre-medication c. The Pre-Sedation check list must be completed before administering any premedication d. Desired response for pre-medication is for patient to remain at MRS 2 31. Which of the following is true about the Mallampati classification? a. This is a screening tool used to determine which patients are at high risk for dysrhythmias b. An airway assessment tool used to determine ease of intubation c. Determines which medications are likely to cause respiratory depression d. Separates patients according to the level of sedation they are expected to experience 32. A 78 year old patient with a history of atrial fibrillation is undergoing procedural sedation. He weighs 68 kg, and his sedation plan includes Fentanyl 150 mcg and Versed 1 mg IVP. Given this patient’s weight, what is the maximum dose of Fentanyl he should receive? a. 68 mcg b. 150 mcg (this dose is appropriate) c. 10 mcg d. None, given his history of dysrhythmias 33. Which of the following statements is true about the effect of Narcan a. Narcan is not effective in reversing the effects of Fentanyl b. Narcan is not effective in reversing the effects of morphine c. Narcan is effective in reversing the effects of Fentanyl d. Narcan is effective in reversing the effects of Versed 34. In the NICU you need to open the Moderate (Conscious Sedation) Protocol, verify that the parental consents are obtained and complete the protocol documentation form in the following situation: a. Versed for aggitatin b. one time dose of morphine sulfate for chest tube insertion c. morphine sulfate titrated to keep infant sedated during bronchoscopy d. fentanyl for ROP laser surgery 35. The infant is receiving fentanyl for analgesia and a dose of 2 mcg/kg is given initially. The infant is 700 grams. The correct dose is: a. 14 mcg b. 1.4 mcg c. 0.14 mcg d. 2 mcg 36. The pre-sedation checklist includes all of the following EXCEPT for: a. Universal Protocol b. Current history and physical examination c. Sedation plan including medications ordered d. Last PO intake 37. Moderate (procedural) sedation applies to the use of Chloral Hydrate in a child under the age of 2 years and ... a. Must be ordered by a licensed independent practitioner credentialed in deep sedation. b. Consent is not required. c. Parents may recover the child. d. Must have a continuous monitoring of BP until reactive. 38. Discharge criteria for a child sedated with Chloral Hydate include that the child be monitored a minimum of 30 minutes post procedure or 60 minutes from the last incremental dose of Chloral Hydrate and… a. Be able to hold head erect, open eyes, and tolerate oral intake. b. Be able to hold head erect and open eyes, c. Is easily wakened. d. Be able to hold head erect, open eyes and have an Aldrete Score of 10. 39. Self-Administered Inhalation of Nitrous Oxide… a. Has an onset of 3-4 minutes and a reversal time of 3 minutes upon interruption of administration. b. Is not to be used as a supplement to other procedural sedation agents. c. May be used during pregnancy. d. Is used with caution pneumothorax.