Clinical tests in endocrinology based on the negative feedback
advertisement
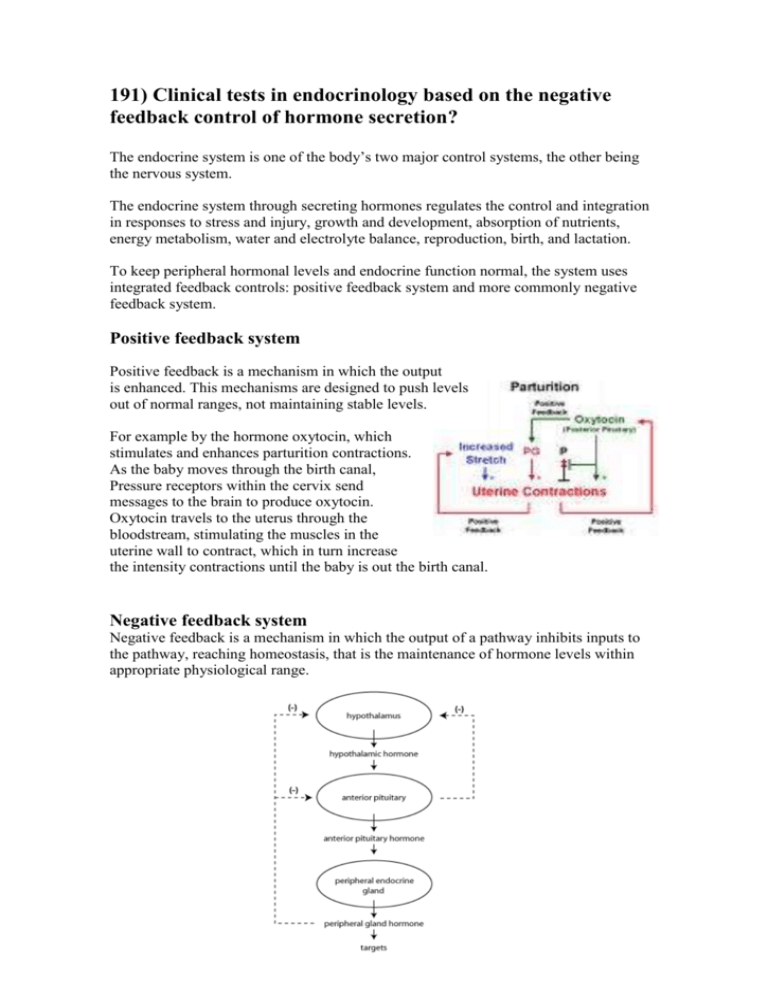
191) Clinical tests in endocrinology based on the negative feedback control of hormone secretion? The endocrine system is one of the body’s two major control systems, the other being the nervous system. The endocrine system through secreting hormones regulates the control and integration in responses to stress and injury, growth and development, absorption of nutrients, energy metabolism, water and electrolyte balance, reproduction, birth, and lactation. To keep peripheral hormonal levels and endocrine function normal, the system uses integrated feedback controls: positive feedback system and more commonly negative feedback system. Positive feedback system Positive feedback is a mechanism in which the output is enhanced. This mechanisms are designed to push levels out of normal ranges, not maintaining stable levels. For example by the hormone oxytocin, which stimulates and enhances parturition contractions. As the baby moves through the birth canal, Pressure receptors within the cervix send messages to the brain to produce oxytocin. Oxytocin travels to the uterus through the bloodstream, stimulating the muscles in the uterine wall to contract, which in turn increase the intensity contractions until the baby is out the birth canal. Negative feedback system Negative feedback is a mechanism in which the output of a pathway inhibits inputs to the pathway, reaching homeostasis, that is the maintenance of hormone levels within appropriate physiological range. Hypothalamic-pituitary- Adrenocortical axis Corticotropin-releasing hormone (CRH) is secreted in the hypothalamus in response to circadian rhythm, stress and other stimuli. CRH travels down the portal system to stimulate ACTH release from the anterior pituitary. Circulating ACTH stimulates cortisol production in the adrenal gland. The cortisol secreted (or any other synthetic corticosteroid administered to the patient) causes negative feedback on the hypothalamus and pituitary to inhibit further CRH/ACTH release. An important place to consider negative feedback inhibition is in evaluating disorders of hypersecretion or hyposecretion of cortisol . Cushing's syndrome is the name given to hypersecretion of cortisol (or hypercortisolism). http://courses.washington.edu/conj/bess/feedback/newfeedback.html In primary hypercortisolism, Cushing's syndrome is due to a tumor in the adrenal cortex, increased negative feedback inhibition has the effect of decreasing secretion of tropic hormones. Therefore, the level of ACTH will be low. Alternatively, Cushing's syndrome might result because of hypersecretion of ACTH, secondary hypercortisolism. Which is caused by a pituitary adenoma (a pituitary tumor). Cushing's syndrome caused by a pituitary adenoma is known as Cushing's disease. In Cushing's disease, both ACTH and cortisol levels will be high. http://courses.washington.edu/conj/bess/feedback/newfeedback.html Tests to confirm Cushing's syndrome Dexamethasone suppression tests Administration of a synthetic glucocorticoid to a normal subject produces prompt feedback suppression of CRH and ACTH levels and thus of endogenous cortisol secretion. Patients with Cushing's syndrome fail to show complete suppression of plasma cortisol levels. -24-hour urinary free cortisol measurements. This is simple, but less reliable. Disease Cortisol ACTH Cushing's disease (pituitary tumor) Adrenal tumor High High High Low Hyposecretion of cortisol is known as adrenal insufficiency. Primary adrenal insufficiency is the disorder originating in the adrenal gland. In primary adrenal insufficiency, there is a release of the pituitary from negative feedback inhibition, and consequently, ACTH levels are high. If there is generalized damage to the adrenal cortex, there will also be hyposecretion of aldosterone. Adrenal insufficiency involving hyposecretion of both cortisol and aldosterone is known as Addison's disease. Secondary adrenal insufficiency (or hypopituitary adrenal insufficiency) describes the situation where abnormally low ACTH levels lead to hyposecretion of cortisol. This can occur after the end of high dose glucocorticoid therapy to treat inflammation and autoimmune diseases. Clinical tests if Addison's disease is suspected -Single cortisol measurements are of little value, although a random cortisol below 100 nmol/L during the day is highly suggestive. - Synthetic ACTH stimulation tests Tetracosactid, is given to stimulate adrenal cortisol production. -A 0900 h plasma ACTH level, when high level (> 80 ng/L) with low or low-normal cortisol confirms primary hypoadrenalism. -Serum aldosterone is reduced with high plasma renin activity. Disease Cortisol ACTH Addison's disease (adrenal damage) Hypopituitarism Low Low High Low Parathyroid Hormone negative feedback regulation If calcium decreases, the parathyroid glands sense the decrease and secrete more parathyroid hormone. The parathyroid hormone stimulates calcium release from the bones and increases the calcium uptake into the bloodstream from the collecting tubules in the kidneys. Conversely, if blood calcium increases too much, the parathyroid glands reduce parathyroid hormone production. Both responses are examples of negative feedback because in both cases the effects are opposite to the stimulus. http://www.besthealth.com/besthealth/bodyguide/reftext/html/endo_sys_fin.html Clinical tests for hyperparathyroidsm Several fasting serum calcium and phosphate samples should be performed. Serum PTH. Primary hyperparathyroidism shows hypercalcaemia and hypophosphataemia with detectable or elevated intact PTH levels during hypercalcaemia. There is often a mild hyperchloraemic acidosis. Renal function is usually normal but should be measured as a baseline. Hydrocortisone suppression test: hydrocortisone 40 mg three times daily for 10 days leads to suppression of plasma calcium in sarcoidosis, vitamin D-mediated hypercalcaemia and some malignancies. Primary hyperparathyroidism appears due to parathyroid adenomas which are monoclonal. Secondary hyperparathyroidism is physiological compensatory hypertrophy of all parathyroids because of hypocalcaemia, such as occurs in renal failure or vitamin D deficiency. PTH levels are raised but calcium levels are low or normal, and PTH falls to normal after correction of the cause of hypocalcaemia where this is possible. Tertiary hyperparathyroidism is the development of apparently autonomous parathyroid hyperplasia after long-standing secondary hyperparathyroidism, most often in renal failure. Plasma calcium and phosphate are both raised, the latter often grossly. Clinical tests for hypoparathyroidsm The clinical history and picture is usually diagnostic and is confirmed by a low serum calcium (after correction for any albumin abnormality). Additional tests include: serum and urine creatinine for renal disease PTH levels in the serum: absent or inappropriately low in hypoparathyroidism, high in other causes of hypocalcaemia parathyroid antibodies (present in idiopathic hypoparathyroidism) 25-hydroxy vitamin D serum level (low in vitamin D deficiency) X-rays of metacarpals, showing short fourth metacarpals which occur in pseudohypoparathyroidism. Deficient Parathyroid Hormone Secretion Decreased or a complete absence of parathyroid tissue therefore inadequate PTH is produced. A) Post Surgical: due to injur or removal of parathyroid glands at the time of surgery. B) Idiopathic: deficient PTH secretion without a defined cause (e.g. surgical injury) is termed Idiopathic hypoparathyroidism C) Hypomagnesemia: when magnesium levels are too low, calcium levels may also fall. Resistance to Parathyroid Hormone (pseudo-hypoparathyroidism). The diseased individuals are characterized by hypocalcemia, hyperphosphatemia, but they are distinguished by the fact that they produce PTH in normal values but their bones and kidneys do not respond to it. Even if PTH is given to them in their veins, they do not respond to it. References Kumar and Klark., (2008) Clinical Medicine .Elsevier Inc. James Norman, M.D., F.A.C.S., (1997 – 2008) Endocrinology Overview. (online) Available from: http://www.endocrineweb.com/ Colorado State University. (2006) Endocrine system. (online) Available from: http://www.vivo.colostate.edu/hbooks/pathphys/endocrine/index.html Plagiarism source : 34.8%