Orthotics Review
advertisement

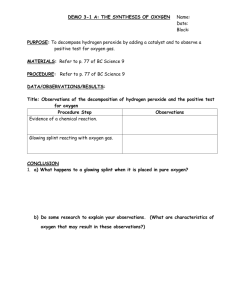
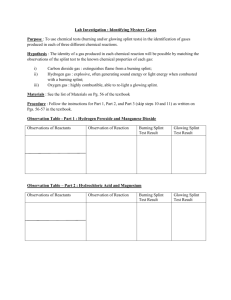
Orthotics Exam Review Spinal Orthosis Mechanics End-point control – has top & bottom to semi-immobilize joints/areas Total contact – whole surface touched…decreases rotation 3-point system – 2 forces on direction, 1 force opposite in middle Counter-pressures – brace contact doesn’t allow movement in a given direction Cervical Orthoses Soft foam – kinesthetic reminder Rigid plastic – mild control for soft tissue injury…no rotation control Philadelphia – soft tissue damage up to C4 or stable Fx 2 & 4-poster – adjustable limits…endpoint control SOMI – endpoint control…don in supine…can’t put into MRI Minerva CTO – total contact, extra-stable Philadelphia…hot & hard to don HALO – can do distraction…limits ALL mvmt…invasive History of Orthotics Back to 5th Dynasty Scoliosis bracing early 1900s Certifying Organizations – ABC or BOC Perry – Biomechanical abnormalities of Post-Polio patients and the implications for orthotics management Post-Polio Pts have normal sensation & motor control Only need orthoses if substitutions are inadequate / cause joint overuse Most common is drop-foot…substitution taken is excessive hip flexion use dorsi-assist device Goals of LE Orthoses P! by forces around joint (try to distribute forces over as great an area as possible Assist locomotion & stability Maintain deformity correction Influence muscle tone Shoewear Environmental protection…support…shock absorption Good shoe needed for many orthoses…and for efficient gait Poor shoe may shearing…cause deformity…lead to fall Sole – welt, outsole, inner sole, shank Upper – vamp, tongue, rear quarters Heel – cushioned or beveled Reinforcements – widen toe box, shank, counter Lifts for leg length discrepancy of it locked KAFO on one side Heel wedge for varus/valgus Rocker bottom for improved rockers Beveled/cushioned heel for lever arms for force on LR Heel flares for rolling medial or lateral Metatarsal pad for pressure shifting Metatarsal bar for pressure during toe-off Metal vs. Plastic Considerations Edema / swelling (use metal) Heat resistance & environmental temp. Sensation / skin integrity Cosmesis (usually prefer plastic) Weight limit 180lbs for plastic Shoe choice Weight of brace for metal Orthotics Exam Review KAFOs 3-point system controls excess knee flexion in stance Use anterior offset joint for genu recurvatum (usually Post-Polio) Useful in unlocked position for proprioception or severe medial-lateral instability Bilaterally… energy cost… velocity (more than wheelchair)… shoulder forces Drop locks vs. bail locks AFOs Ground reaction knee extension moment during stance For weakness/spasticity… stability…indirectly stabilize knee Rigid for…severe PF spasticity/tone…mild gastroc tightness… DF/KF moment… tibial progression…use cushioned/beveled heel Articulating to control DF/PF Dorsi Stop / Dorsi Assist – weak PFs, excess DF stance, excess PF swing, tibial control Leaf spring is dorsi assist – correct foot drop, no tibial control, mild calf weak/tight Polyarticulating for more precise adjustment Beekman – Effects of a DFstopped AFO on walking in incomplete SCI patients DFstop AFOs don’t disrupt calf muscle recovery postSCI DFstop AFOs gait speed & step length DF stop AFOs better knee position stance limb stability No change in PF or Quad function…but pretibial function Lehmann – Gait abnormalities in hemiplegia: correction by AFO Main AFO benefits: speed & normalize heel strike via PFstop Poorly adjusted/locked AFO difficulty of gait…KF moment knee instability Rancho ROADMAP KAFOs & RGOs (<3+/5 quads &/or proprioception) AFO not KAFO if: intact knee proprioception, but <3+/5 quads Unlocked KAFO if: ipsi <3+/5 quads…w/o proprioception ipsi <3+/5 & contra >3+/5 quads…knee HE ROM available Locked KAFO if: ipsi <3+/5 & contra >3+/5 quads…w/o knee HE ROM (B) Locked KAFO if: Bilat <3+/5 quads…no contractures, flexible, strong UEs AFOs (>3+/5 quads &/or intact proprioception) No AFO if: ok strength, ok proprioception, no PF spasticity weak ankle…PF >4/5 or norm DF & PF during gait…DF >4/5 Locked AFO if: proprio or PF spasticity/contracture…Berg <43 PFstop AFO if: proprio or PF spasticity/contracture…Berg >43 DFstop+ass AFO if: weak ankle…PF <4/5 or excess DF or PF during gait…DF <4/5 DFstop AFO if: weak ankle…PF <4/5 or excess DF or PF during gait…DF >4/5 DFass AFO if: weak ankle…PF >4/5 or norm DF & PF during gait…DF <4/5 Why Splint? Prevention – undesired motion or contraction, pain, edema, hematoma Increase – ROM Protect – nerve, tissue, function, healing position Support – joints, tissues Common Dx: carpal tunnel, spasticity, Jt Arth, contracture, burn, OA/RA, Fx Key anatomy to preserve Arches – proximal transvers, distal transverse, longitudinal (palm can flatten & cup) Web spaces – allow opposition & grasp (tripod & key) Orthotics Exam Review Precautions Pressure areas – epicondyles, olecranon, cubital tunnel, ulnar styloid, axilla, want 2/3 up forearm Edema widen splint, widen straps, use kinesiotape under splint Vascular insufficiency loosen splint, widen straps, don’t use hot material Thin tissue use prefab splint, bubble out area, breathable material Watch out for cognitive level Splint types Static – no moving parts Limit mvmt, affect all joints they cross Ex: resting hand, wrist cock-up Dynamic – rigid base w/ adjustable elastic component Provide torque, assist w/ ROM program, help gliding Serial Static / Serial Cast – no moving parts; non-removable & circumferential Series of static splints to ROM Splint Construction Use 2/3 of forearm Flare & fold edges…round internal & external corners Conform to unequal pressure material strength by adding contours Consider comfort, function, cosmesis, integration into Tx, wearing schedule Maintaining splint Wash w/ warm water & soap…not in a machine Don’t put near heat Don’t try to modify at home…stick to schedule & note any discomfort Bring to each PT session Inspect skin every time it’s removed (if red area >15min, notify PT) Custom splinting Heat material to 150-160oF Stretchy – polyform & aquaplast – finger / wrist / elbow splint; serial cast; resting hand Mod Stretchy – polyflex & tailor splint – hand / wrist / knee / foot splint; bivalves; equip mod Not Stretchy – ezeform – elbow splint; spasticity; functional positioning Patterns – 2/3 forearm & ½ circumference; mark at MCP of 2 & 5; mark at CMC; 1st & 2nd web space