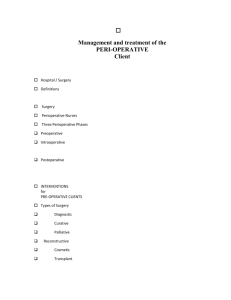
Introduction - Department Intranet
advertisement

The UNOFFICIAL UCD Anesthesiology resident Survival guide 2009-2010 Contributors Sara Cheng, MD, PhD-Editor Rachel Boggus, MD Mindy Cohen, MD Matthew Coleman, MD Georgia Guerra, RN Jay Hacking, MD Kellie Hancock, MD Haley Hutting, MD Gillian Johnson, MD Matthew Koehler, MD Allison Long, MD Estee Piehl, MD Prairie Robinson, MD James Sederberg, MD Cristina Wood, MD 1 TABLE OF CONTENTS INTRODUCTION .................................................................................................................................. 1 BASIC EXPECTATIONS ...................................................................................................................... 2 HOW TO SET UP A ROOM.................................................................................................................. 3 WHAT TO DO AT A CODE .................................................................................................................. 4 GENERAL OR- UNIVERSITY HOSPITAL ........................................................................................... 5 IMPORTANT NUMBERS- UNIVERSITY HOSPITAL ........................................................................... 7 GENERAL OR- VA HOSPITAL ............................................................................................................ 8 GENERAL OR- DENVER HEALTH MEDICAL CENTER .................................................................. 11 IMPORTANT NUMBERS- DENVER HEALTH MEDICAL CENTER .................................................. 14 DHMC PRE-OP/PACU ROTATION .................................................................................................... 15 AOP- UNIVERSITY HOSPITAL ......................................................................................................... 21 IMPORTANT NUMBERS- AOP .......................................................................................................... 22 ACUTE PAIN SERVICE (APS) ........................................................................................................... 23 CARDIOTHORACIC SERVICE .......................................................................................................... 26 THE CHILDREN’S HOSPITAL ........................................................................................................... 28 OBSTETRICS (LABOR AND DELIVERY) ......................................................................................... 31 TRANSPLANT .................................................................................................................................... 35 SAMPLE NOTES ................................................................................................................................ 37 USEFUL WEBSITES .......................................................................................................................... 39 MAPS ................................................................................................................................................. 40 1 Introduction For CA-1 residents: Welcome to the University of Colorado anesthesia residency program! We’re glad you’re here. If you’re reading this, you’ve jumped through a dozen hoops, maybe moved across the country, replaced electrolytes a bazillion times, and ADC VANDIML is your middle name. Congratulations- internship is over! You’re doing what you really want to do, finally- passing gas. That being said, you’re probably a little nervous. It may have been a long time ago that you did any anesthesia! And your daily routine is going to be far and away different from what you’ve been doing this past year. You’re not alone- everyone says the first couple of weeks/months can be very anxiety-provoking. I certainly didn’t sleep very well those first couple of months. Rest assured- read when you can, and come to work every day ready to play ball- you’ll get through it just fine. This little book is meant to help you through your first week at each new hospital. It is meant to be a practical guide to those little daily details that will be second nature to you in a couple of months. It is NOT meant to be a medical reference or a guide to anesthesiology. It was put together by CA-2 and CA-3 residents, for UCD residents only, and is not endorsed by the administration formally. Therefore we take no responsibility for anything wrong or omitted by this guide- it will not substitute for reading, common sense, or talking to your attending. It is simply meant to ease the pain just a little bit, and hey, I’m all about easing the pain. Never hesitate to ask for help when you need it. If you’re in the OR, first call your attending. If he/she is unavailable and you’re in need of urgent help, call the charge attending or page overhead for any available anesthesia attending. Also, don’t hesitate to ask more senior residents for advice about how to set up or prepare for a case…we’re here for you. Finally, everyone goes through tough times during residency at some pointwhen it happens to you, don’t think you’re alone! Talk to your friends, your spouse, a friend in the program whom you trust… it helps to get you through it. For CA-2/3 residents: This edition has new sections for the subspecialty rotations. Let them serve as an introduction and overview for you, as well as a reference for all those pesky codes and phone numbers, etc. We’ve worked many hours on this guide and hope it is helpful. However, it is a work in progress! Please scribble things in this book that you think need to be in the next edition, and share them with next year’s editor… who by the way may be you. I’m outta here… Good luck and have fun! Sara Cheng, MD, PhD Editor 1 Basic expectations SARA CHENG, MD, PHD Here are some pointers to get you up and running. I know, they may sound basic, but people have gotten in trouble multiple times in the past for not doing these things…rather than beating them with a “you should have known” hammer, I think it’s just better to say these things up front: Before starting at each hospital, try your very best to GET A TOUR of the place. At DH, Dr. Humphrey gives a great orientation. At the VA, Dr. Friedman or one of the residents will show you around. At the U, it’s best to find a resident to give you a tour. In July, you’re not expected to have had much time to get an orientation before your first day in the OR. But later in the year, before your first day at a new hospital, PLEASE be proactive and arrange with someone to get a tour. You can do it pre-call or postcall, or after your scheduled cases with an on-call resident. Do NOT be the guy/gal who shows up at 3 PM on their first day for their first call and doesn’t know where the OR is, doesn’t know where to get drugs, etc etc- it is painful for you and uncool for everybody involved. Believe me, it’s happened! Each day, you should find the next day’s OR schedule (emailed to you at the U, on the little podium in the PACS room at the end of the hall at the VA, at the OR bridge at DH). LOOK UP YOUR PATIENTS on the computer and fill out what you can on an H & P form or on Centricity at the U, including recent labs and imaging. At the VA and DH, past anesthetic records are readily available on the computer too and are always useful. Then, even at this stage, try to FORMULATE A BASIC PLAN in your head for each patient (see below). It may be as basic as “I think this patient needs general anesthesia with a tube and no invasive monitors” but that’s still a plan. Then, either find or CALL YOUR ATTENDING about tomorrow’s cases. At the beginning of the year, you should always call your attending to go over the plan for each- this is a basic expectation. It gives them a chance to go over stuff before the busy morning and relieves their anxiety as much as yours. If they don’t call you back or don’t talk very much, then at least you fulfilled your obligation. Later in the year, as you get to know them better and get more comfortable, there will be some attendings for some simple cases you won’t call, but for now- it’s safest to always call the first time you’re working with an attending. If someone establishes themselves as one who doesn’t call back, then now you know. Formulating a plan: take a stab at these basic questions when you present to your attending. What kind of anesthetic does this patient need to have this operation safely and comfortably? (general vs. neuraxial vs. nerve block vs. local anesthesia). If a general, what kind of airway (ETT vs. LMA) and what kind of induction (rapid sequence vs. standard). What drugs will you use? Do you need any additional IV access? Do you need any invasive monitors? Are there co-morbidities that will complicate your management? You will not know the answers to many of these things initially, but have them in the back of your mind and you’ll look like a thinker from the beginning. Every morning, every case: PREPARE YOUR ROOM (see below). SEE THE PATIENT. Look at vitals, do physical exam focusing on heart/lungs/airway. Obtain consent. Talk to your attending. Once you and nursing are ready, start antibiotics/administer pre-med if appropriate and bring patient back to OR. Get your monitors on. Call your attending for induction. POST-OP CHECKS: you are expected to go see your patients if they are still in the hospital within the first day or two after surgery. You should ask them about intraoperative recall, pain control, and any questions/concerns about their anesthetic. Write just a couple of lines in the chart, documenting this conversation. An example: “Anesthesia f/u note: 64 yo POD#1 s/p ex-lap under GETA. Denies recall. Denies complaints. Pain controlled. Questions answered. Signing off.” 2 How to set up a room SARA CHENG, MD, PHD You should always set up a room to be prepared to put a person to sleep under general anesthesia, even if you are planning on using a different anesthetic technique. Patients get too uncomfortable, change their minds, go apneic… you get the idea. The important thing about room setup is that you should use a system consistently. An organized system is a safe one. This is how I do it but there are many ways… 1. Turn on your machine. If your machine has an automatic start-up protocol, start it and follow the directions. Otherwise, start the oxygen sensor calibration, as this takes some time. 2. While that’s going, set up your drugs: a. Emergency drugs to always have drawn up: Succinylcholine 5cc@20mg/ml, Ephedrine 10cc@5mg/ml, Atropine 2cc@0.4mg/ml, Glycopyrollate, 2-3cc@0.2mg/ml, Phenylephrine, several syringes, 10cc@100mcg/ml b. Induction drugs- draw this up only if you’re planning to do a general. Usually propofol 20 cc@10mg/ml, occasionally etomidate if CV unstable or thiopental for craniotomy, lidocaine 3cc@20mg/ml if using propofol through a peripheral IV (propofol burns!) c. Narcotics etc- fentanyl, midazolam, dilaudid- having at least 2 mg of midazolam and 250 fentanyl drawn up is a good start. d. Whatever else you and your attending have discussed. 3. Finish machine checkout: a. Reattach your oxygen sensor. b. Check that monitor is on and displaying appropriately c. Check that backup oxygen canister is full d. Check that the vaporizers are full, that the vaporizer you want (i.e. sevoflurane or desflurane) is present (there are only 2 spots and occasionally you’re want to use a gas that’s not there- you’ll have to ask the anesthesia tech to get it for you), and that the dials turn. e. Check that all gas flow knobs by turning them all on, then turn air off, then turn oxygen offwhen you do, nitrous should go down to off too (safety mechanism). f. Check for circuit leak. g. Check that gas sample line is connected and patent (blow on the end through your mask to see CO2 appear on monitor) h. Check CO2 scavenging canister- all purple=need a new one. 4. Monitors: Put pulse ox and BP cuff at head of bed. Place EKG leads on bed- for 5 lead, green and white on right. If using invasive monitors, make sure you have transducers in room and plugged in, wet down. 5. Airway (SALTT)- suction on and at head of bed, airway (oral) in 2 sizes, laryngoscopes with 2 different blades and light working, tube (endotracheal) in 7.0 and 8.0 sizes with balloon tested, syringe attached, and stylet available), tongue depressor. Also, always good to know where the emergency LMAs are located (in the room or in the anesthesia workroom, depending on your site). Some favorite mnemonics: MSMAIDS (machine check, suction, monitors, airway, IV access, drugs, special/specific to case) MMM SALT (machine, meds, monitors, suction, airway, laryngoscope, tube) All Electric Gadgets Need Proper Stimulation (emergency meds: Atropine/Ephedrine/Glycopyrrolate/(neostigmine)/Phenylephrine/Succinylcholine As always, go over all this with an attending or senior resident during the first week. It seems like a lot but you’ll be able to get it all done in 15 minutes eventually. 3 What to do at a code SARA CHENG, MD, PHD After you have been a CA-1 for approximately 30 days, you will start taking overnight call and will be handed a small, scary, black plastic thing called the code pager. The first several times this thing goes off your heart will start beating very fast and you may briefly contemplate running away. Instead, you will run and grab the airway box, having checked earlier that day that you knew where it was and that it was stocked appropriately, and run your butt over to the patient’s room. Your job as the anesthesiologist is to manage the airway and intubate if needed. On the way there, call your attending and tell them where the patient is so that they’ll meet you there. Once there, eyeball the situation. Is the patient lying there, out of it, but all vital signs on the monitor are stable and there are no people buzzing around? You probably have time to talk to the nurse/team and figure out the history, as well as wait for your attending. Remember the indications for intubation: oxygenation, ventilation, airway protection, operative procedure. On the other hand, is there a full-blown resuscitation going on with an RT or nurse bagging the patient? You’re going to need to intubate. Remain calm and remember one thing: that after 30 days of being an anesthesia resident you may know more about airway management than most of the people in the room. So, your place is at the head of the bed, not milling around talking to people or trying to assemble your stuff. Announce you’re with anesthesia. Push others out of the way if you need to. Try to assess the airway (morbidly obese/no neck/in C-collar or halo/jaw wired shut=BAD) and bag the patient. If it’s difficult, two-hand mask and ask someone else to squeeze the bag. Ask others to assemble the minimum needed for intubation: suction on and within reach, airway (oral), laryngoscope, endotracheal tube, free flowing IV, drugs (induction agent and paralytic). Ask about full stomach (rapid sequence induction with cricoid pressure), if recent potassium was high or if stroke/myopathy present (contraindications to sux), whether blood pressure has been stable (use etomidate over propofol). If the patient is unconscious or almost unconscious then you may not need drugs- just do your DL and if the cords are closed you can push some sux. By the time you’ve started some of this stuff your attending will be there and you guys can get on with intubation together. One very important pearl: ALWAYS take the time to position the patient optimally for intubation, just as you would in the OR. Even if everyone looks very busy and they are in the middle of chest compressions, take the 10 seconds to get everyone to move the bed away from the wall, adjust the height, and boost the patient up in the bed towards you. It could be the difference between a first shot successful intubation and an initial failed laryngoscopy that gets bloody and more difficult. OK, one more very important pearl: Once you’ve successfully intubated, hold on to your tube for dear life until it is safely taped. In the middle of a code, it can easily come out again (an event that caused personal asystole in this author 3 years ago). Some favorite mnemonics: VISA (vent/ambu, IV functioning, suction on and within reach, airway tools) SALT (suction, airway (oral), laryngoscope, tube) 4 General OR- University Hospital CRISTINA WOOD, MD Important people: Program Coordinator: Jan Ratterree, office: 303-724-1758, fax: 303-724-1761, email: jan.ratterree@uchsc.edu Administrative assistant: Suzanne Bullard, office: 303-724-1765, fax: 303-724-1761, email: suzanne.bullard@uchsc.edu. Anesthesia IT: Ken Bullard, ken.bullard@ucdenver.edu. Before you start: You must have your ID badge (use it for parking and getting through doors), codes for Pyxis, Centricity, Clinical Workstation, Med Explore and Care Manager. When in doubt, call Jan or Suzanne, they are lifesavers. Call a resident who is over at the University to give you a tour before starting. Ask Jan about getting set up for Med Explore from home, and Ken about setting up VPN (virtual private network) from home. That way you can do your Centricity pre-ops from home. Centricity: Learning Centricity, the Intraoperative charting system, is paramount before starting a case. If this is your first month of CA-1 year, you will have an orientation scheduled for you at the University prior to starting a case. Otherwise, please contact a “superuser”: either Cara English (720-333-0509), Mary Bidegaray (720-333-0631), Allison Rocco (720-333-0372) or Sarah Figueroa (303-946-4872) for your Centricity orientation about 2 weeks before you are scheduled to come to UCH. If you have any difficulties scheduling this training please contact Leslie Jameson, MD directly (303-333-0869). Weekdays Daily Work Flow Do H&Ps on patients coming into the hospital as best you can with info (including latest labs, EKG, CXR, TTE etc) from Clinical Workstation or Med Explore (for inpatients, vitals will be on Care Manager and you must pre-op and consent these patients the night before). Give yourself at least 30 minutes to set-up your OR before any morning conferences (Monday- Grand Rounds 7:00, Wed- ITE lecture 6:30, Fri- Cardiac lecture 6:30). The techs are great and usually will set up arterial lines and central lines for you, but you may need to do these yourself as well. You can always call the techs to help (see numbers below). Be sure that if you need infusions (i.e. TIVA- total intravenous anesthetic), you have all the pumps you need in the room. If prone cases, be sure to check that you have a prone pillow. Ask the techs. Get patient’s narcotic bag from Pyxis in the PACU (It is called narcotic bag on the list and includes 4mg Versed, 750mcg Fentanyl, 2mg Dilaudid and 400mg propofol). Other meds like Mannitol/Nimbex/Heparin are in the Pyxis/refrigerator in the pod areas between the ORs and lasix/premade Sufentanil syringes are at the pharmacy (window is located in the same hall as the main OR board). You can always call the pharmacy to make up a drip for you. Clark Lyda, the head pharmacist, is always an excellent resource for any and all drug-related questions. All emergency drugs are in your cart in the OR. Make sure you get Centricity loaded up in the OR before you head to pre-op. Arrive in Pre-op around 7:00 (8:00 on Mondays). Find your patient- paper OR schedule in pre-op on countertop shows bed number and nurse ** Learn the preop and PACU nurses/names, they are a wonderful resource and really will help you if you make the effort!**. 1. Complete pre-op H&P in Centricity while talking with the patient. Nurses handwrite vitals in chart, ask where. 2. Sign Pre-op Order sheet (nurses need official order to give IV fluids, EKG, labs, scopalamine patch). 3. Consent the patient. (Check with attending about type of anesthesia first). 4. Start IV if not done already. Try to put in 18 gauge or larger. 5. Verify antibiotics and that they are on the bed, or on the way to the OR. 6. Check with patient’s nurse and the OR nurse before wheeling out. 5 Get patient moved over and start pre-oxygenating first! Put on monitors. I always put on pulse ox first, then BP and while it is cycling, I get on the EKG leads. Call your attending to tell them you are in the OR. All communication at the U is via cell phones. Have all the induction drugs ready to go, even plugged into the IV line. Do not push any drugs yet. Your attending will come in for the induction, have fun!! Remember that OR rooms 1-4 do not have great cell phone service. So have the attending number handy and be ready to call from a land line if need be. Call attending prior to extubation, no exceptions. After transporting to the PACU, help the PACU nurse apply patient monitors and give him/her your report. It’s helpful to take a look at the sheet they fill out so that you can have an idea of what they want to know. Make sure all paperwork in anesthesia packet is signed. There are three parts: PACU orders, billing sheet (blue), confidential incident sheet (purple) Write totals on narcotic bag; make sure they match Centricity totals. No needles! Drop off in metal box next to Pyxis in PACU with patient sticker! Get meds for next case. (If you have quick cases, you may want to pull out multiple narcotics first thing in the morning). Finish Centricity Record and print a copy. Place hard copy with patient’s chart. Usually will get “coffee” (15min), lunch (30min), and “tea” (15min) break. OR schedule with anesthesia assignments comes out around 2pm. It is emailed to us as a PDF and hard copies are available at the OR desk. Look up patients for the next day and call attending the night before to discuss plans. See all inpatients the night before and have the consent signed. Weekday Hours R1: This means overnight call: 3pm-7am. You will finish all of the late cases for the day and all of the emergency overnight cases. R2: Late shift: Start with the first cases of the day (so you need to be there about 6am to set up your room, etc) and you are in house until there are only a couple of rooms going. Usually until 6-8p. R3: Very similar to R2, but you leave a little earlier. Usually 5-7p. R4-Rinfinity: You usually finish and can leave after you have finished your cases, or about 3-5p. Call Nights/Weekend Call Weekday call nights usually arrive at 3pm but always check (look @ relief time on OR/Anes schedule). Check OR board and/or with Anes Charge (85920) to see where you’re needed. Keep your pager on during the day; they may need you to come in a little early if they are very busy. (Never happened to me though). Weekend call is a 12 hour shift, changing over at 7am/7pm. 2 call rooms: 1) Leprino Office Building (near parking garage). 4th Floor, East side, door code is 3-1-2. Then go to the far North side of building to find our call room. 2) SICU anesthesia sleep room- must use if you are carrying the code pager. Door code 0-1-5-8. Code Pagers/Badge When on call you sometimes carry a code pager and badge that should let you in any locked door (does NOT override elevator), if the anesthesia ICU resident is not in house. Codes (See Section “What to do at a code”) Your responsibility is the “A” of the ABCs. Get to the head of the bed, assess need for airway intervention. It’s OK to push RTs, RNs, residents out of the way. Before intubation remember “VISA” V-ventilator or ambu-bag ready?, I- patent IV functioning?, S- suction ready? (is often missing), A- airway tools available? Airway Box Locations 1) main OR anesthesia workroom, 2) in PACU, 3) in SICU supply room on top of fridge (ask any SICU RN). 6 Important Numbers- University Hospital Anes Charge Attg OR front desk RN charge Pre-op PACU OR pharmacy Main pharmacy Anes chief tech Anes techs OR Anes phone OR RN phone Lab pager Lab land line Blood gas lab Centricity Help Hospital Operator Blood Bank 85920 84351 83512 86252 86203 86132 81389 85917 85912,-13,-14 864## (## = rm #) 863## (## = rm #) 266-5040 87086 85309 85915, 85919 720-848-0000 84444 Door Codes Locker Rooms & Faculty Lounge Anes Workroom Call room Leprino 4th floor SICU sleep room (must use when carrying code pager) 04507 2311 312 0158 Other: BICU 8-7583 SICU 8-7586 8-7400 Neuro ICU 8-5490 Engineering (room temp.) 8-8351 303-266-4500 Acute pain 266-6493 Chronic pain 266-7291 Pain Clinic 8-1970 OB Anes. Att. 8-5973 OB Anes. Res. 8-5972 OB Res page 266-5820 OB Anes. CRNA 8-5911 OB 4th front desk 8-5233 OB 5th front desk 8-4111 AOP Charge MD 8-1507 AOP Pre-op 8-1350 AOP PACU 8-1360 7 General OR- VA Hospital HALEY HUTTING, MD; MATTHEW KOEHLER, MD Important People: Dr. Lyle Kirson – head of VA anesthesia Shirley Pfister, RN – pre-op nurse and fund of knowledge about accessing pt records Carrie Shurmantine – Anesthesia Department controller, she handles all badge & ID questions. (303) 3932883. Email: carrie.shurmantine@va.gov John Hawk, PharmD – handles Pyxis concerns (and is a fantastic resource for drugs) Jake Friedman – in charge of resident education, 303-609-3590. Other attendings – Dr. Dev Rai, Dr. Luke Osborn, Dr. Mohammed Javed, Dr. Peter Rowe, Dr. Allison Long (all are super-friendly and excellent teachers) Before you start: You must have your ID badge, scrub codes, parking hang tag, and computer codes. Carrie handles most of these things. Get in touch with her at least a week early if you can. Also, in your first few days you should get Pyxis access (from John) and iStat codes (from Anesthesia techs, for blood gas and ACT). Phone Numbers VA Hospital Main Phone number: (303) 399-8020 All OR communication is done via overhead paging: just ask the circulating nurse to do this for you when you need your attending or you are ready for induction/wakeup. They will also show you how to do it yourself if you like. Door Codes Conference room 4-3-2-1 Anesthesia Workroom 4-3-2-1 Locker room code is the room number (listed on plaque next to door) – many lockers are first-come, first-served, so if it’s empty and it doesn’t have a name on it, you can use it. There are also a few small lockers in the anesthesia conference room for residents (next to the refrigerator) To access locked anesthesia carts: Turn dial to left, then press 1-2-3, then turn dial to the right. Badges and Cards (all of these should be given to you during orientation) General Badge is used for identification and for access to the OR by the locker rooms. Scrub card badge will allow you to access scrubs from the scrub machine next to the locker rooms Parking tag allows you to park in deck across from VA (9th & Clermont St), south of the VA building. Weekdays Daily Work Flow The pace at the VA Hospital is a little more leisurely than it is at the other hospitals, but they are really trying to get cases started on time and speed up turnovers as much as possible. H&Ps for all your cases should be done the day before they are scheduled and discussed briefly with your attending (especially at the beginning of the year). The VA computer system is very thorough but is not accessible from home, so the work has to be done before you leave. Also, if you have cases that have possible blocks for the next day, you should check the block cart in pre-op before you leave and restock it (or ask an anesthesia tech to restock it). Cases start at 07:45 (in the room) Tuesday through Thursday, 08:30 on Monday. You will start your own IV’s, so get there early enough to do this. Also, plan for time to do any blocks/epidurals if indicated. You should plan to be done interviewing the patient by 07:15 (08:15 on Monday). There are four groups that must see a patient before sedation - pre-op holding nurses, surgeons (consent/marking), OR nurses, and anesthesia. Do NOT start your block or give any sedation before verifying that everyone has seen the patient. 8 All patients go to the PACU EXCEPT patients being admitted to the ICU go directly to the ICU (even if extubated). Also, after hours and weekends, patients will go to ICU for wake up only since there are no evening/weekend PACU nurses. Propacks are stored in the pre-op area. Please return them after transport and plug them in to charge. Since the VA is a smaller hospital with fewer ORs, everyone needs to help out in order for things to run smoothly. If you have a cancelled or delayed case, try to get your own breaks/lunch and give breaks to others if you have time - be proactive. On non-call days you usually go home around 16:00 - 17:00. On call days, you stay until the last room is finished. One of the things that is different about the VA is that you relieve the CRNAs at 15:00, but they may be hiring a “late float” CRNA to help with late afternoon cases. Printed schedules for the next day are located in the radiology room under the podium. Changes are frequent, so make sure to check the white board in pre-op for the latest schedule. Make sure to check the board for a blue triangle (pending labs, usually tox screen) or orange rectangle (anesthesia NP workup available). Pharmacy All non-controlled substances are stored in the anesthesia cart or the anesthesia workroom (cabinet or fridge). Controlled substances are in the pharmacy in PACU (overhead page pharmacist if closed at lunchtime). After hours (3pm) and on weekends, you will need to get controlled substances from the Pyxis in PACU. Check with John Hawk to get set up with access to this. Place all narcotics in a plastic bag along with a drug count sticker (on top of Pyxis) and place it in the drop box in the pharmacy door at the end of your case. Equipments and meds for peripheral nerve blocks located in the block cart and the “block room” in pre-op. Ropivicaine and clonidine is in the pharmacy. Paperwork 3-4 photocopies of your anesthetic record should be made after each case: the original goes to the PACU nurse, one copy goes to the pharmacy with your returned controlled substances, one copy goes in the folder in the lounge (for record-keeping), and one copy goes to the ICU nurse (if applicable). Intra-op: you should complete an anesthetic record, an H&P, and a time-in/time-out/antibiotic administration sheet, QA sheet, and delay sheet. Pre-op evaluations (Shirley Pfister or Terra Sharp): On complex pts, Shirley or Terra will do a pre-op evaluation and write the H&P for you. A copy will either be pinned up on the cork board in the lounge or in the top left file cabinet in the lounge (filed by year of surgery and alphabetically). Check CPRS if you can’t find the copy. Check VISTA for previous anesthesia records. Also, if the patient has had an operation within the last calendar month, you can check the brown folder in the conference room for a copy of their anesthetic record. Post-op Orders are written in CPRS in the PACU. They should include an IV narcotic, a PO narcotic, and an anti-emetic at the minimum. Blood paperwork – There is paperwork that accompanies each unit of transfused blood. Make sure to check with your attending because they need to sign this. Call & Weekends Call at the VA is HOME CALL (yea!). Keep your individual pager on. There is no VA-specific pager. Surgery resident will call you when a case needs to go at night or on the weekend. Get information about patient. Ask if surgery attending knows about the patient and when they will be ready to start. Also verify that surgery resident is calling the nursing supervisor, who will call in OR nurses. The process from first phone call to case start usually takes at least one hour. Talk to your attending – some want to be called immediately, some want to be called when the nurses arrive. Any calls for ED anesthesia or difficult airways should be immediately discussed with the attending (do not come in first). When in doubt, call your attending. 9 Try to clean up your anesthesia machine after night/weekend cases (pick up monitors, throw away drugs, etc) Weekend call is also Home Call, but you are also in charge of the acute pain service, so you may have to come in and round in the morning (see below). In general, anesthesia is not responsible for intubations outside of the OR. There are some circumstances when we do get involved. Any questions, call attending. Also, there is always a separate anesthesia team on for cardiothoracic. If you get called for a CT case, pass it on. Acute Pain Service The VA is the only hospital that has you follow the pain service before you have you APS rotation, so make sure you get all of your questions answered before you start a weekend call. Ask Dr. Osborne for the instruction sheet on epidural management at the VA. You will round on the patient, write orders, and write an APS note in CPRS on each weekend day. There is an epidural clipboard in the anesthesia conference room that has one sheet of paper for every epidural patient (document level, infusion, and verify that a note is written each day). Over the weekend, the call person rounds on all epidural patients. During the week, generally the resident who placed the epidural rounds on the patient. However, it is ultimately the call person’s responsibility to make sure that a note is written in CPRS. Acute Pain Service Keys: 1. Write order to hold sq Heparin on mornings you are pulling an epidural. 2. Write order to restart Heparin one hour after epidural is pulled. 3. Discuss with primary team. All pain meds by primary team after epidural d/c’d. 4. Make sure all epidural catheters come out with the catheter tip intact and document this. Lectures: Mon (07:00) – Grand Rounds teleconferenced from Univ. Tues (06:40) – Lecture in 4th Fl. Conference Room Tues (15:30) - if available - Lecture teleconferenced from University. Wed (06:15) – ITE lecture teleconferenced from Univ. Thurs (06:40) – Lecture in 4th Fl. Conference room Fri (06:30) – Lecture in 4th Fl. Conference room *Teleconferenced lectures are viewed in the 3rd floor Pathology conference room. If the door is locked, the key can be found in the pathology office. If the pathology office door is locked, that key is located in the Histology lab. See Dr. Osborne for detailed instruction sheet how to set up teleconference. The scavenger hunt for the key can be time consuming, so lectures can also be viewed live on the intranet now (computers in the anesthesia conference room). *Make sure to check the schedule on the door of the anesthesia conference room. Residents are scheduled to give one lecture each month. * Friday is usually QA or CCC (Clinical Case Conference) = oral board style VA Computers Get all codes for general access and CPRS access through IRMS (1st floor by Clermont entrance). Make sure to set up a signature code in order to be able to sign orders and view images through VISTA Talk to John Hawk if you are unable to write orders, you may need to sign some narcotic paperwork through pharmacy office Old Anesthesia Records and EKG’s are viewed by going under the “Tools” tab in VISTA and accessing “VISTA IMAGING” from the drop-down menu. 10 General OR- Denver Health Medical Center ALLISON LONG, MD; RACHEL L BOGGUS, MD Important people: Residency administrator: Dr. Jack Humphrey Medical Education Coordinator: Laura Rendon, Phone: 303/436-6029; Email: Laura.Rendon@dhha.org Senior Secretary: DeVindra Randall; Phone: 303/436-8375; Fax: 303/436-6548; Email: DeVindra.Randall@dhha.org Speak to DeVindra Randall at least 1-2 weeks prior to your arrival to arrange the following: -parking -ID badge -locker assignment and code to the lock -scrub machine code -who to call for computer access codes -Pyxis access code *Contact Dr. Humphrey prior to your arrival to arrange a tour before your actual start day Phone numbers- At DH they generally use an overhead paging system to reach attendings, anesthesia techs, etc. After picking up the phone, you press “page” and then say your message (“Dr. Sawyer please call room one” or “Anesthesia tech, please bring the glidescope to room 1”) then hang up the phone. If you pick up the phone, press “page”, then hear a busy signal then someone else is paging overhead at that time and just try again in a few seconds. Door codesResident call room- 1924 Anesthesia work room- locked after 11p.m., key is the same one that opens the call room; it is in the lock box outside of the call room (after 11p.m. you should keep the key with you) Locker rooms- are not locked Weekdays Most patients go to the pre-op clinic and the H&P will be completed for you. Find them in the file folder in the “bull-pen.” If it’s not there, they either did not go to the pre-op clinic and you can do it in the a.m. or it is still being completed and may show up by morning. If you are scheduled to take care of an INPATIENT, you should see them and complete the green H&P form before you go home the night before. Generally, attendings do not expect you to call them the night before to discuss cases. The OR schedule for the next day is available in the early afternoon and is in the bull-pen. Arrive 30 min prior to conferences to set your room up. Get all medications (including narcotics) out of the Pyxis in your OR room. Make sure to label/date/time all your meds because they fill the Pyxis in the mornings and they find meds in there that are not labeled they will throw them away. Mondays- Grand rounds are teleconferenced to DH at 7 a.m. Lectures other days of the week are from 6:45-7:15 a.m. in the lunch room- see bulletin board in that room for exact days as some days there are no lectures. After conference (or before if you have time) see your pt in pre-op. Marker board has pt’s name and chair location. Complete H&P/Consent/IV access (usually nurses do the IVs unless they are difficult in which case they will give it a try or two then call you). After all consents have been signed pt can have premedication and can be pushed back to the OR in their chair. Don’t transport patients past the main OR board, go around (it violates HIPPA). Overhead page your attending when you are in the room if you have not already seen them. 11 Unused narcotics have to be “wasted” with another resident, CRNA, or attending by having them witness you discard medications at a Pyxis machine. Ask someone how to do it. You can save all leftovers throughout the day until you have some time to do this, just stick a patient sticker on each syringe. Call Nights/Weekends Weekday call (C1) - be ready to go at 3 p.m. Check board or contact charge to see where to go. Weekend call is 12 hr shifts 7a.m. to 7 p.m., 7 p.m. to 7 a.m. *When you arrive for call, check that the trauma rooms (OR 1 and 5) have been set-up. See following page on trauma room set-up. It is important to have them set-up, as there is usually no time when a trauma patient is on their way up to the OR. Float- arrive at 11a.m., start day by giving lunch breaks, you will be the last to leave on this day Late- arrive at usual morning time and you will be the 2nd to last resident to leave O- You are not on call, arrive at usual morning time and you will likely be relieved around 3 pm. This is pretty consistently true at DHMC, which is lovely. Code pager- you will carry this when you are on call. The float CRNA will give it to you and you can hand it off post-call to the new float CRNA Codes- same responsibility as other hospitals- primarily airway (see Section “What to do at a code”) Airway box location- It is just inside the anesthesia workroom to the left of the door when you walk in. The Glidescope and fiberoptic card are also stored in this room. You may occasionally get paged to bring these things to a patient’s bedside. 12 Guidelines for Trauma Room Set-up at Denver Health Anesthesia Machine, Circuit, and Work Area Standard anesthesia machine set-up and checked out, including suction Two functional laryngoscope handles and selection of blades Three prepared endotracheal tubes (7.0, 8.0, and 9.0) with stylets and 12 cc syringe in place Oral airways (80 mm and 90 mm) and tongue depressor 16f NG tube Esophageal temperature probe Monitors ECG cables deployed with electrodes attached, paper in ECG recorder Non-invasive BP cuff deployed at head of bed under mattress Pulse ox deployed on circuit tree Art line set-up on transducer with wet down pressure bag, pressure cable connected to machine. Second pressure module and cable available should CVP be needed Fluids, Warmers, IVs Two Level I warmers assembled with (1) D-50, and (1) D-100 style tubing, stop cock, extension, and 1000 cc bag of LR, not wet down until needed One 250 cc bag NS with 400 mg dopamine, and one 250 cc bag NS with epinephrine (4 amps) taped to their sides and IMED tubing placed in plastic bag hanging on Level I One two chamber IVAC pump Drugs Available with labeled syringes but not drawn up Etomidate Vecuronium Emergency drugs prepared and stored in top drawer of Pyxis Atropine 400 mcg/ml Succinylcholine 20 mg/ml Ephedrine 5 mg/ml Neosynephrine 100 mcg/ml Epinephrine 2 syringes: syringe 1 – 10mcg/ml, syringe 2 – 100 mcg/ml Invasive Lines Arterial catheter start kit bundled and available Triple lumen catheter and Cordis introducer on top of anesthesia machine IV start kit bundled and available 13 Important Numbers- Denver Health Medical Center Attending In Charge (AIC) 123-118 OB CRNA 123-104 Anesthesia Call Resident 123-102 Calling from outside: Bridge Blood bank SICU OR nursing phone OR anesthesia phone 303-436-xxxx 68061 66929 68333 680xx 630xx Attending Physicians Herren, Michelle Bui, Camelia Chandler, Mark Duke, James Humphrey, Jack Juels, Alma Kumar, Sunil Lockrem, John Meyer, Eric Michel, Theresa Miller, Howard Packer, Mac Sawyer, Mike Valdivieso, Ron Pager 303/201-4160 303/206-7654 303/208-1730 303/540-3983 303/851-4182 303/208-7049 303/208-0485 303/207-1950 303/266-2413 303/208-0272 303/540-3982 303/891-3465 303/206-9785 303/208-1220 Practice Manager Cottrell, Judy CRNAs Adams, Heather Bosso, Jennifer Bradley, John Ebeling, Steven Faughnan, Gretchen Feldaverd, Brad Ford, Christie Harenberg, Jennifer Mejia, Tina Moffitt, Aimee Morgan, David Phillips, Susan Quist, Barbara Singer, Fred Strittmater, Elton Taber, Alexis Temple, Michael Tubac, Gregory Warnecke, Doug Wehrman, Amy Winckler, Chris Pager 303/208-0840 303/208-0636 303/206-4959 303/206-2197 303/206-7646 303/206-4972 303/206-7657 303/461-8269 303/206-4043 303/206-4437 303/208-6121 303/266-7324 303/855-0795 303/760-6971 303/208-8857 303/461-1754 303/206-1725 303/461-0698 303/826-5718 303/207-8897 303/201-2257 OR Nurse Manager Andis, Ann Pager 303/826-2570 Phone Ext. 66492, I.C. 27 Phone Ext. 68377, I.C. 77 OR Clerical Super. Higgins, Stephanie Phone Ext. 66573 Support Staff Camp, LeeAnn Randall, DeVindra Phone Ext. 68378, I.C. 79 68375, I.C. 83 Pre-operative Clinic Goldsmith, Kathy NP Pre-Op Center Phone Ext. 65995 65990 Anesthesia Technicians Dallas, Rueben Montoya, Sophia Mantano, Liz Snelling, Ron von Holdt, Kevin 123-339 123-325 123-146 123-105 123-905 14 Pre-Op/PACU rotation- Denver Health Medical Center Rachel L. Boggus, MD This is a rotation spanning 1 month – 2 weeks of it will be spent in the pre-op clinic and 2 weeks will be spent in the PACU. Dr. Chandler mans the pre-op weeks and Dr. Sawyer mans the PACU weeks. They will decide how to split up the month for you – usually it is 2 weeks of PACU first then 2 weeks of pre-op clinic but this is not set in stone. Speak to Drs. Chandler and Sawyer to confirm the order you will be doing these in. PACU GOALS This is a fairly straightforward rotation: your goal is to hang out in the PACU for the majority of the day taking care of any issues that may arise. These include: airways problems, regional nerve blocks, any orders that the nurses may need that are not already written on the PACU order sheet, cardiovascular problem (high BPs, arrhythmias, etc), calling consults if needed (neuro for altered mental status, cards for arrhythmias or ST changes, etc.). DAILY SCHEDULE When you are on the PACU rotation you are expected to attend morning conferences. This includes grand rounds on Monday and any 6:45am lectures that are on the schedule (which Dr. Duke emails you; it can also be found posted in the anesthesia lounge). If there are no lectures that morning arrive around 7-730 UNLESS you are planning to do a pre-op nerve block for a patient who is the first case of the day; then you are going to need to arrive earlier to get the block done and still allow time for the OR resident or CRNA to get the patient back to the room on time. It is helpful if you look at the schedule the day before to see if any of the first cases may need pre-op nerve blocks – if so, plan on arriving a little earlier that day so you can get the block cart set up, etc. When you arrive at the PACU at 7/730ish introduce yourself to the PACU nurses so they know you will be around to help that day. If they don’t know you are there then sometimes they call the attending directly and you miss out on valuable learning. They are very good about coming to you for any issues that may arise. They also are very good at letting you know if a patient may need a block. There is a small computer nook in the back of the PACU – this is your “home base.” Start out there and read/study/drink coffee/do whatever. When you see a patient arrive to the PACU get up and help the patient get settled in – attach monitors, change the O2 from the tank to the wall O2, etc. The PACU nurses appreciate your help. Then stay there and listen to the report. After report ask the OR anesthesia provider if they anticipate any issues. Check on the patient every 10-15 minutes or so to be sure they are doing ok. Repeat this process for every patient that comes to the PACU. If there are major issues with a patient or if you are going to have to call a consult for something always make sure to run it by the attending for that case. The days on PACU usually end around 3-4pm (sometimes you may stick around later if you are waiting for a patient to come out who you are planning on blocking). You don’t have to ask anyone for “permission” to leave, just leave when you feel it is appropriate. DOING BLOCKS ON THE PACU ROTATION Check out the schedule the day before to see if any of the first cases may need blocks. If so, run it by whomever the attending will be and see if they want to do the block pre-op or post-op. If they want to do it pre-op you will need to arrive earlier that day to get the block done as mentioned above. If they want to do it post op then you can arrive at your normal time. For all other patients who may need blocks and ARE NOT the first case of the day you can wait until that day to see what the attending wants to do. 15 When you arrive in the morning get an OR schedule and highlight all possible cases that may need blocks. Talk to the attendings for these cases and see if they want to do blocks. If they do not, stop here. If they do, ask whether they want to do the block pre-op or post-op. Also see if they want to use ultrasound. Write that down on your highlighted OR schedule. Once you have determined a patient is a candidate for a block and confirmed the attending will do a block, check in the APC/pre-op area and talk to these patients AND CONSENT THEM for blocks. Try to catch the patients as soon as they get there so you not hold up the OR team when they are trying to do everything in their 20 minute turnover window. Consent them in the APC regardless of whether they are getting a pre-op or post-op block. 4a. If the attending wants to do the block pre-op get it set up as soon as the patient gets there. Find out when the patient is supposed to arrive. You can also let Scott, the APC charge nurse, know that you will be blocking that patient and he can call the PACU to let you know when they arrive. When the patient gets there let the pre-op nurse do their paperwork and get the IV in then make sure the anesthesia and surgical HP/consents are done (if they aren’t then you cannot give the patient any sedation). Then take the patient over to the PACU and ask the nurses where you can do your block. You can’t do blocks in the pre-op area because there is not enough room and there is not adequate monitoring equipment. Hook the patient up to the EKG, BP, pulse ox. The block cart and ultrasound are always in the PACU near the nurse’s office. If the ultrasound is gone someone may be using it for a central line or something. Just page the anesthesia tech overhead and have them bring it to you. Get your block equipment all set up, then page your attending and do the block. Keep the patient on the monitors in the PACU and keep an eye on them until the OR team is ready to take them back. 4b. If you are going to do the block post-op STILL CONSENT THEM FOR IT PREOPERATIVELY (see #3). Then have the block cart all set up for when they come out. When they come out of the OR help get them settled in and listen to report. Then get all set up for your block and then call the attending and do it up. There is paperwork that needs to be filled out for blocks. It is located on the side of the block cart. Fill out this paper, have your attending sign it, and attach it to the OR packet that the OR team fills out and turns in. MAKE SURE YOU FILL OUT A BILLING SHEET FOR THE BLOCK (this is the same white sheet you fill out when in the OR). You can either fill out a brand new one or just add what you did to the one the OR team has already filled out. Make sure to check “ultrasound” if you used ultrasound. Dr. Ciarillo asks that you take a sticker and get a contact number for each patient you block. Call them 2 days after you block them to see how the block worked and see you they are doing. Pre-Op GOALS You will be working in the pre-op clinic. Your goal is to evaluate patients preoperatively and determine if they need any further work up/labs/testing. You will also be ordering any meds or lab tests you think will be beneficial the morning of surgery. Also, you will be filling out the anesthesia H&Ps and consents. Write down any issues you may anticipate very clearly on the H&P so the OR team will be aware. Also, answer any questions the patient may have regarding anesthesia. DAILY SCHEDULE A few days before the start of your pre-op rotation call up Kathy Goldsmith, the NP (stands for both nurse practitioner and nicest person alive) that runs the pre-op clinic. You can reach her at 65990 or 65995. Go down to the pre-op clinic and she will give you a little tour/orientation. To get to the pre-op clinic enter through the main entrance you normally do. However, where you normally turn left and go by the main street café to get to the OR, instead walk straight in and go straight (towards the urgent care center). When you reach the entrance to the urgent care center just look to the left you will see a sign that says anesthesia clinic and there you have it. 16 You usually arrive about 8am – you are not expected to attend the morning lectures while on the pre-op clinic rotation. There is a workroom in the back of the clinic that is your “home base.” Kathy will print you out a list of patients who are coming in that day. Look over the list and if there are any really sick patients , patients getting big surgeries, or patients with big-time medical problems let Kathy know and she will let you see the “more complicated” patients. When the patients arrive they will get their vitals taken and usually an EKG then the nurse will put them in a room. There is a yellow room and a blue room. The color of the file folder the nurse gives you with their files in it will either be yellow or blue and this is how you know what room they are in. Anyhow, the nurse will put them in the room then give you their file with all their paperwork in it. The paperwork included in this file contains basically everything from their computer file printed out for you, the surgical H&P and consent, and the day of surgery order form (the day of surgery order form is yellow and will become important later). There are usually a lot of papers in this file. Go through all the papers before you see the patient and start filling out their green H&P form from the papers. As you are going through the papers make 3 piles: 1. Can be thrown away/not important papers (50 pages of EKG from a stress test, duplicate sheets, etc.) 2. Important papers that should be stapled to the anesthesia H&P (notes from the PCP, most recent med list, copies of echo results) 3. Surgery’s papers (their consent form and H&P will also be in the packet) and the yellow day of surgery order sheet. These 3 piles are all going to go to different places so it is important to separate them. Once you have gone through the entire packet and have all sheets separated into piles, discard all the useless sheets into the paper shredder. Leave the other 2 piles and you will deal with them after you see the patient. Then go see the patient. Go through the H&P form with them and fill it out as completely as possible. Bring your stethoscope and do a mini-physical exam. Then go through the anesthesia consent form with them and have them sign it. Answer any questions they may have. Also consent them for blocks if they may be candidates. Then they can leave UNLESS you think they need labs. If they need labs you must fill out a lab sheet and give it to the nurse and she will draw the labs for you. You should also make a note on your H&P that you drew labs that day so the OR team will know to look in the computer for labs. If you order labs they get those drawn and then they can leave right afterwards. You then go back to the workroom and finish any last things on the H&P. RIP OFF THE WHITE CARBON COPY OF THE H&P (the H&P is a green packet that has a white carbon copy attached to it so when you fill it out there is the green part you wrote on and also the white carbon copy on the back) AND STAPLE IT TO THE PILE OF IMPORTANT PAPERS YOU GATHERED FROM THEIR FILE. So, you have the carbon copy of the H&P and the important papers pile stapled together – you then take this up to the front of the office and put it in the slot designated to go up to the anesthesia bull pen. The nurse will take these upstairs and file them later on. You are then left with the green anesthesia H&P, the blue anesthesia consent form you just did, the surgical H&P/consent, and the yellow day of surgery order form. If you want to order any meds or labs for the morning of surgery (albuterol neb, pepcid, bicitra, urine pregnancy test) there is place on the yellow form for this. Look under “anesthesia” and write your orders there and sign them. Once you are completely done with the yellow day or surgery order form and your H&P, paper clip them to the surgery forms and your consent form (so you will have your green H&P, your blue consent, surgery’s H&P and consent, and the yellow day of surgery order form) and PUT THESE BACK IN THE BLUE OR YELLOW FILE FOLDER YOU WERE GIVEN AND PUT 17 THE FILE INTO THE FILE CABINET UNDER THE DATE OF THEIR SURGERY. The file cabinet is right next to your workroom. Then you fill out a billing sheet and drop it off in the basket in the front of the office. Kathy will show you how to fill out the billing sheet – it is very simple, you just circle stuff. Repeat this process for all patients until all patients have been seen. Patients are usually scheduled up to 4pm so you can get out of there around 430/5ish. If you have any questions about how to do anything just ask Kathy. She knows all. If you see any very complicated patients that you think may need to be cancelled or may need further testing review them with Dr. Chandler THE DAY YOU SEE THEM. If Dr. Chandler is not there then just grab any attending. Make a plan for that patient and order any consults or further tests they may need. 18 SICU Rotation- University Hospital JAY HACKING, MD; JAMES SEDERBERG, MD Door Codes Call Room 0158 Store Room 642 Storage Room (Site Rite ultrasound for line placement) 2007 Schedule There are two residents on at a time, and there are basically four days: 1. Call- come in and round, stay all day and overnight. That day the call person’s job is to get the other resident home as quickly after rounds as possible. That means doing all of the scut work, etc... 2. Post call- After rounding your fellow resident should get you out of there ASAP. 3. Short day- This is the day the other resident is on call, and you should leave quickly after rounds. 4. Long day- This is the other resident’s post call day so you get them out ASAP, and stay until admissions come out of the OR. Usually 5 PM or so but is variable. Arrange things with the CT resident so you get them out at a reasonable time and vice versa. Then back to call and start the rotation all over again. It’s basically like being an intern again. Pre-Rounds I usually get there about 6 AM depending on how many patients there are. Since we are cross-covering CT (more on that later) you round with the CT team each morning, so you might want a little time before rounds to start gathering your info. First, talk to the resident on call and see if anything happened to your patients overnight (they bled, they coded, etc…), and see if there were any overnight admissions that need to be seen. There are templates for daily notes so grab a stack of those, and start at the computer and using Care Manager write down Is/Os, vitals, labs, new radiology, etc… Then go around and see your patients, perform a quick and focused exam. Next I would always write my assessment and plan and write any orders that are urgent (transfuse, replace ‘lytes, etc…), and finish filling in the days’ note for that patient. If time permits then write orders for the next days labs, films, etc. as well to save time later. Make sure everyone is seen by the time rounds start. Rounds SICU rounds usually start at 8 AM (9 AM on Mondays) in the room on the west side with the PACS computer to look at Chest films, CT rounds start at 6:30 AM at the CT patient’s room who has the lowest room number. Rounds are variable and attending dependent, and you go from room to room and read off of your note to the attending. What is helpful is to have the resident not presenting to grab the chart and write any orders that might come up then, and make sure there are orders for the next AM. Once rounds finish, get the post-call/short resident out and the remaining resident does any work that still needs to be done. Rest of the day Then I would usually go check the OR board and see what might be coming to you out of the OR and if time permits start a brief accept note on them to make it easier later on (get on Centricity to get the scoop). There are always surprises, some cases that say “ICU” don’t come and some that you don’t expect to do come, but at least you have some idea. Accepting a patient When you get a patient the primary team should write all the admit orders. You see the patient, do a focused physical exam, get pertinent info from Centricity or the resident doing the case (brief medical history, airway, I/O’s, drugs given, drips, IV access, invasive monitors, etc…), and write a brief accept note. Then follow up on labs and replace/fix things that might come up. Some teams are VERY hands on (transplant, sometimes white 19 surgery), and some don’t care what you do (ENT, ortho). See if patient needs any lines (central or arterial), you often need to swap out a Cordis for a triple lumen catheter to give the nurses more ports. CT Cross Cover We cover the CT ICU patients when on call, which is a relatively new development in our program, and is therefore both good and bad. It is important to round with them on call day (so you know what to expect) and post call so you can tell them what happened if necessary. The fellows are great and readily accessible (most of the time) and feel free to call them with any questions, and ALWAYS call if you are going to give blood, make changes to pressors, or if there is any change in pt status. They want to know what’s going on. When you Pearls 1. Never transfuse a transplant patient without talking to their team first. 2. Call your attending with any major issues, or with any questions, they would rather you call than not, and they only do 1 week at a time, so it’s not as bad for them. 3. Talk to the nurses about what they might need IF you might get the chance to lay down, it will save you some calls. 4. There is always an in-house intensivist to call if you need help with a line or if there are any questions. 5. Call CT fellow with any questions, but gather information about hemodynamics and ins/outs first, get specific numbers from nurse (i.e. chest tube 2 put out 100 in the last hour etc). 6. When extubating, get ABG on CPAP, weaning parameters, and then text page the attending with your plan and give them a way to call back if they have questions. Then wait a few minutes and extubate. 7. Ask for help if you need it, from nurses, CT residents, other anesthesia residents or attendings, etc… 20 Outpatient Anesthesia (AOP) - University Hospital MATTHEW COLEMAN, MD Important people: AOP charge: John Armstrong, MD Pharmacy: Mary Cousins, Carol Mckinney, Liz Lyke Anesthesia Techs: Johnny Lawerence, Andrea Flores Before you start: Know the lay of the land; Preop and PACU, ORs, GI, Pharmacy, Anesthesia workroom, Locker rooms, storage room where block equipment is stored, and lounge. Your Pyxis codes will work the same as the AIP. ORs include AOP 8, 9, 11-17, GI (except 13). Schedule and Call Schedule: Tuesday – Friday 630 to 3-5 pm (rarely there past 5 pm). Mondays you’ll be scheduled at the AIP, usually covering R2 or R3. Call: Expect to be on call 1 Saturday night during the month, 2 if they are strapped for people, or if there are 5 weekends in the month. Cases: Most of the time you’ll be doing Ortho cases that require blocks, with a few days in the month doing ENT, gyn, dental, etc. You will not likely do any GI or eyeballs. The current agreement is that the residents in the AOP start and finish their rooms (almost all of the time). You are not expected to take over CRNA rooms if you finish early, and they will not take over your room unless it is well past 5 pm. If you are out before noon, you should help give some lunches and make sure there are no potential add-ons. Call the charge before taking off. OR Logistics Arrive in Pre-op around 7:00, unless you will block the first patient, shoot for 6:45. If you would like a locker at the AOP, there are usually a few empty ones you could claim for the day. There is also a scrub machine available at the AOP. Most patients are pretty healthy and the preops can usually be done in the morning if you’re quick. Give yourself more time if you’re doing urology, gyn, GI, dental, ENT as these patients sometimes have more extensive histories. Also plan ahead with your ortho cases, as most of them get blocks. Pharmacy: Get patient’s narcotics bag from the pharmacy. You can pick up your entire day of narcotic bags at once. Just sign your name next to each patient on the preprinted pyxis form, and take the bags. Also pick up anticipated drugs for the day, e.g. propofol, ketorolac, local for blocks, and phenylephrine sticks (in the pharmacy refrigerator). Pharmacy hours are 6:30 am – 5:00 pm Anesthesia Techs and Workroom: The workroom is located on the southwest side of the AOP near OR 16. Call Russ Ingram prior to starting to make sure you have a code to the workroom. Anesthesia techs arrive later than at the AIP and are usually not available to help get ready for your first cases. So, be ready to get in the workroom, get LMAs, pumps, etc. Also, be prepared to turn over your OR room from the day before if the techs left prior to cases finishing. The block cart and ultrasound (US) are located in a storage closet located at the entrance of the preop area. Ask the charge nurse to let you in if you get there early. Blocks: the block cart contains sterile block trays and US covers in the bottom drawer. The block tray contains the drape, syringes, three-way stopcock, tubing, epi, sterile guaze, and iodine. In preparation for a block, pull out a tray, US cover, the drugs (usually 0.5% Bupiv or 1.5% Mepiv or a combo of both), and the needle. 21 Be sure and print a copy of the US images, as this is needed to bill for the US. Fill out a centricity procedure form, print it, staple a copy of the US image and put it with the chart. Important Numbers- AOP Anes Charge Attg RN charge Pre-op PACU AOP pharmacy Anes techs 84439 81508 86252 86203 81391 84459 OR 8 9 11 12 14 15 16 17 Anes phone 82201 81375 81342 81412 81419 81423 81421 81159 RN phone 83208 83209 82511 81412 81414 81415 81416 81417 Lab pager Lab land line Blood gas lab Centricity Help Hospital Operator Blood Bank 266-5040 87086 85309 85912 720-848-0000 84444 Door Codes Anes Workroom get your code from Russ Ingram 22 Acute Pain Service (APS) Prairie Robinson, MD; Estee Piehl, MD; Kellie Hancock, MD Important people: Director, Acute Pain Service: Dr. Matt Fiegel Administrative Assistant: Suzanne Bullard, office: 303-724-1765 APS advanced practice nurses: Robert Montgomery and Lynn Hornick Acute pain is a different month since you are not in the OR. You will be placing pre-operative regional nerve blocks and epidurals for post-operative pain management. You will also be managing patients with epidurals and nerve block catheters on the floor. It can be hectic at times, and being very organized is key as you will be managing orders and checking out drugs for many different patients over the course of the day. There is a lot of paperwork! Reading/ Preparation The main focus of this rotation is the placement and management of thoracic epidurals and lower extremity blocks. Upper extremity blocks are rare on APS, but you will do them. Cater your initial reading to local anesthetics, lower extremity blocks, and neuraxial anesthesia. As always, try to invest some time in getting an orientation tour from the previous resident. It is helpful to familiarize yourself with the block cart, basic set-up for a nerve block, and paperwork prior to starting. Resources At the beginning of the rotation, you will get a notebook from Suzanne. It has your reading schedule for the month, several informative articles, and some examples of how to fill out the paperwork. There are also guides on epidural and spinal dosing of narcotics and local anesthetics that you will use daily. The textbook provided while you are on APS is excellent. A useful adjunctive website is www.nysora.com. It includes detailed directions, pictures, and videos on how to do the different blocks. Dr. Fiegel is another important resource, especially when it comes to ultrasound-guided blocks. He gives a great interactive, practical lecture that involves looking at your own anatomy with ultrasound. (That way you’ll know if you’re one of those freaks without a right-sided IJ.) Make sure you make time to go through this with him before you start the 3rd week of APS. Daily Workflow For the first several days, Rob and Lynn (the advanced practice nurses on the service) will be around a lot to show you how to fill out the documentation, help with set-up, and talk about acute pain management. You will find that Rob and Lynn are extremely helpful and knowledgeable. If you have questions and your attending is not available, they will usually have the answer. They have loads of experience in pain management, so don’t forget to use them as a resource. As in everything, your days are often attending dependent. You are expected to look at the OR schedule when it comes out (usually around noon each day) with the pain attending or a pain nurse. Mark "block" next to each patient that is a likely candidate for a block or epidural. Note the number of first case blocks. If there are multiple procedures, the regional nerve blocks are your priority. (The order of priority is lower extremity block, upper extremity block, thoracic epidural, and finally lumbar epidural.) If you are unable to do all of the blocks/epidurals, you should touch base with the anesthesia resident who will be doing the case to make sure they are planning on doing the block/epidural. If you are working with Dr. Fiegel, you will be able to do multiple first case blocks, because he helps with the consent and set-up. AM Set-up 23 It is helpful, especially on busy days, to have syringes ready to use. Prepare the day before by having a bag of premade 20cc syringes, because you will go through them quickly. A total knee uses 4-20cc syringes, and bilateral knees use 8-20cc syringes, so you can go through your bag quickly. It is also helpful to have premade syringes ready to draw up fentanyl and versed. When you arrive (usually around 6:30am), you can draw up your local anesthetic for your first few cases. See anesthesia attending preference below for the local anesthetic of choice. To make a 1:400,000 epi concentration (which you will use for most blocks), add 0.07ml (yes, less than 0.1cc) epi with the TB syringe to a 30ml vial. Pre-procedure workup In the morning, see your patient and do a targeted H&P. You are NOT expected to do the full pre-op H&P in Centricity, but you need enough information to do a safe regional anesthetic. Major things to assess: 1) Surgical site—where is the incision? 2) Cardiopulmonary status. 3) Allergies. 4) Is the patient on any medications that affect coagulation or does the patient have any existing diseases that might affect coagulation status (i.e. liver disease)? Is there any reason to order coags? 5) Any history of pre-existing neuropathy? 6) Any previous history of regional anesthesia? 7) Is there unusual anatomy that might make regional anesthetic difficult or unsafe (i.e. it may difficult to place an epidural in a patient with multiple back surgeries)? Obtain consent for your regional technique plus the surgical anesthetic. Ask your attending for the appropriate facts to convey to the patient regarding risks. Things that should always be covered—risk of bleeding, infection, nerve injury, new or worse pain, reaction to local anesthetic. Procedure Grab a sheet of stickers for each patient you block and set them aside. You will need them for the paperwork and orders. The patient needs to have monitors on prior to starting the procedure. The pre-op nurse needs to be present and a time-out done that includes procedure site, allergies, and planned block. Do not give sedation unless ALL consents, including surgical consent, are done. After the block, make sure and get a print-off of the vitals. The nurses can show you how to print them. You will need to attach the recorded vitals to the procedure note. Don’t forget to tell the pre-op nurse what sedation and local were given. It will take a few days to learn which pharmacy orders and post-op orders are needed for which type of block. Attendings Dr. Fiegel—He is currently in charge of APS, goes out of his way to help you, and does a lot of teaching. He will help you keep up with the paperwork and procedure notes and will help you get set up and get consent. He usually prefers 30cc 0.5% bupivicaine or 0.5% ropivacaine for the femoral and lumbar plexus. He prefers 30 cc 0.25% bupivacaine or 0.25% ropivacaine for the sciatic block. Dr. Fiegel is very liberal with sedation and often uses up to 5 cc of fentanyl, so you will probably want to check out 2 of versed and 5 of fentanyl when working with him. He will want you to work on doing the blocks with nerve stimulation and will move on to ultrasound once you are comfortable with stimulation techniques (usually week 3). Dr. Ramirez—He likes 0.5% ropivicaine or 0.375% bupivicaine for lumbar plexus blocks, popliteal and femoral blocks with 1:400,000 epinephrine, mepivicaine 1.5% for the sciatic blocks. Get set up, draw your landmarks and then call him in. He will occasionally have you add clonidine 50mcg-100mcg to the ropivicaine (especially for amputations). Dr. Hendrickse, Dr. Schiffer, Dr. Shindell, Dr. Shiffrin – These attending are flexible. They usually don’t have strong opinions on the local anesthetic used. 24 Tips on Meds It’s important to remember that you will be checking out a lot of narcotics for multiple patients in rapid sequence or at the same time. You have to turn in empty bags with the patient’s name even if you give all of your drugs, so make sure you put a patient sticker on a pharmacy bag when you take out a controlled substance from Pyxis. It can be a couple hours between when you give the med and when you do the procedure note, so it’s easy to forget what you gave to which patient on a busy day. Pick a system that will help you keep track. You can write on the OR schedule what meds were checked out and given for each patient. Alternatively, you can record it on each individual bag as you go. Another word about meds: You will often have multiple blocks in rapid sequence, especially on Mon, Tues and Fri. On those days, you will need to draw up several doses of local for blocks prior to the start of the day. You need to get all these vials out of the Pyxis without overcharging someone at the beginning of the day. The easiest way to do this is to charge one vial of local (i.e. ropivicaine) to the first patient, but when the door opens take out 4-5 vials and draw these up into syringes. Then, charge the vials to each individual patient as you go along during the day when you take out narcotics. That way you charge everyone for the appropriate drugs but can still be ready to go before the first patient. Charting All blocks need to be charted in Centricity. The process is simple and self-explanatory, but it’s important to enter your name, your attending’s name, and the appropriate sedative drugs on the procedure note. Pharmacy will track you down if the narcotics aren’t accurate. Staple the vitals to the printed note, and Rob or Lynn can show you where to leave them. 25 Cardiothoracic Service PRAIRIE ROBINSON, MD; SARA S. CHENG, MD, PHD The cardiothoracic month is pretty tiring but you sure learn a lot! Things to do before you get started (highly recommended to reduce start-up pain): 1. Get handouts and the book "Cardiac Anesthesia" from Suzanne Bullard 2. Get a 15 minute lowdown from Russ Ingram (head anesthesia tech) on the Baxter pumps and Swan box 3. Get a tour on the heart room set-up from a resident who's done CT Things to read before you get started: 1. Cardiopulmonary physiology and anesthesia chapters in Morgan and Mikhail 2. Website written by Dr. Seres: http://www.uchsc.edu/anes/residency/cardiacfellowshipsyllabus.php. There are a couple of things that need updating (ie. aprotinin is no longer used), but otherwise it's very good and exactly the way he wants things. 3. Cardiac Anesthesia (Hensley/Martin/Gravlee: NOTE THE LAST AUTHOR). The one part I think is really useful beforehand is the 1 page section in the Chapter "Anesthetic Management during CPB" entitled "The CPB Sequence," so you know what the heck they are doing over there. Things to read as you lose that "deer in the headlights" look (these make for great onbypass reading): 1. More of the Hensley book 2. More on TEE (Shanewise et al. Anesth Analg 1999 is the definitive paper on the topic) Heart Room set-up checklist (I kept this exact list on a little card in my pocket and never got caught missing something big even if it was emergent and everyone was going crazy) Equipment: ETT (#8,9), Baxter pumps x 2, Level 1 primed with NS, pacing box (batteries working?), oximetric swan box, TEE machine/probe, BIS, triple transducer, aline supplies- be prepared to start the aline in pre-op, 2nd IV supplies, cordis, swan, sonosite, ABG syringes (heparinized), ACT syringes (not heparinized) Drips: Normal saline 500 cc bag (this will be your carrier,and you will add the Amicar to this bag after heparin administration), nitroglycerin (200 mcg/ml in 250 cc bottle, start at 0.1 mcg/kg/min), epinephrine (4 mg into a 250 cc bag equals 16 mcg/ml, start at 0.01 mcg/kg/min), insulin drip (if diabetic), vasopressin (attending dependent) Drugs: FastTrack box and Heart Resuscitation box from Pyxis, fentanyl 3 x 20 cc, midazolam 2 x 10cc, phenylephrine 5 x 10 cc, ephedrine 10 cc, epinephrine 2 x 10 cc (16 mcg/ml pulled from drip bag, can also double dilute the glass vial in drawer to a 100mcg/ml and 10mcg/ml concentration), nitroglycerin 0.2mcg/cc in 10 ml x2 (20 mcg/ml diluted from drip bag), atropine, glycopyrrolate, vecuronium, sux, etomidate, esmolol 10 cc, HEPARIN 30 cc kept drawn up at all times!, protamine (do not draw up until nearing the end of bypass), Amicar 5G x2, calcium 1 gram, lidocaine 20 cc, magnesium 2 gm. Other stuff to check: is there blood in the fridge? (need it at start of case esp with redo- they might rip the heart open during sternotomy- it has happened!) Following is an outline of the flow of the cardiac cases that go on bypass and things to think about during each period. The first couple of times you do this, the attending will be with you and show you where/how to hook up some of this stuff. Pre-bypass: Patient should have one large bore IV to go to sleep with, cardiac induction (midazolam, fentanyl, etomidate, paralytic) place another large bore IV (14 or 16g), A line placement if not done in preop, right sided IJ cordis, float swan if indicated, place BIS, OG to remove gastric contents, bite guard for TEE, place the bar across the IV poles, label all of your IV lines both at the bag and on the table. I like to put down blue towels 26 under the patients’ shoulders and tape IV lines down with labels so I always know where they come from and the gauge. Hook your drips to the VIP port of the cordis. Tape down the cordis once the patient is completely positioned so that it is not being pulled on, these have been pulled out during the case or during transport. The attending or CT fellow will place the TEE. Set foley up so that you can easily monitor urine output. Titrate your anesthesia to a BP within 20% of initial pressures. Send baseline ACT/ABG. Also send baseline labs if patient does not have recent labs on file. The surgeon will give you the pacing wires- hook them up to the pacer box, the coronary sinus line will attach to the CVP port, flush this line. For sternotomy: give fentanyl pre sawing 1020 cc (check with attending), hold ventilation!! At aortic cannulation, goal of MAP around 60, SBP 90-100. Prior to going on bypass, dose heparin 300-400u/kg, perfusionist will tell you the dose. 3 minutes later draw ACT, give to perfusionist. Usual goal is >400 (CT attending dependent). So you may have to give more, set the timer again and recheck an ACT. Give 5g of Amicar after the heparin, prior to bypass initiation. Put the other 5g of amicar in your NS carrier and run at 1g/hr. Empty the foley prior to bypass and note the amount. Chart cross clamp and bypass times or ask nurse if you miss it. You may need to redose your paralytic, narcotics, midazolam right at or right after bypass initiation. Bypass: Stop ventilating when pump flows adequate, turn off inhalational and O2, redose paralytic, narcotics, midazolam if you haven’t already. Labs are drawn by perfusionist, follow the hct, glucose, lytes and treat as needed. They will transfuse blood. Start/stop drips as needed, goal MAP >40. Turn your machine to CPB mode. Follow UOP, tell perfusionist if less than 100cc/hr. TEE on standby, no warm fluids running. Ending Bypass: Patient will be rewarmed, turn all monitors/alarms on, redose paralytic, versed if needed, when surgeon requests- give lidocaine 100mg and magnesium 2g, note when cross clamp is removed, depending on the rhythm may have to pace, may need more lido or Mg or drips started. Give Ca 1g when requested by surgeon-usually about 20min after cross clamp is off and the heart is beating well. Re-expand lungs, watch the lungs come up, make sure there is no tension on the LIMA graft, turn on vent, and send PT/PTT/CBC/Lytes to lab. Continue to follow ABG. Protamine dose will be given to you by the perfusionist, when asked- give test dose, then give slowly through peripheral IV, tell surgeon when half of the dose is in. After protamine is given draw ACT 3min later. Note off bypass time. Empty urine when off bypass and tell perfusionist total on bypass UOP. Post-bypass: Follow coags/bleeding status and transfuse products as indicated. Repeat TEE exam. Remove TEE, clean up your lines, disconnect PIVs for transport, remove BIS, empty foley, place dressing on cordis, patient remains intubated, to SICU. Take drugs with you- phenylephrine, epi, ephedrine, atropine, paralytic, narcotics, esmolol. One more thing: Teamwork is key on this service. There are 3 residents on service who are kind of a self-contained group, plus a senior “float” resident who participates in the CT call pool. On any given day they might be spread over 3 sites: UCH, VA, and St. Joe's- so helping each other out by calling around when you're done with your cases, doing the pre-ops for the next day at your site so that your friend doesn't have to come over from across town just to do it, relieving the higher numbered call people, keeping clearly labeled stashes of drugs in the fridge for each other- all this stuff helps a lot and can keep you from being totally miserable. 27 The Children’s Hospital GILLIAN JOHNSON, MBBCHIR; CRISTINA WOOD, MD Important people: Program Coordinator: Morris Dressler MD 74820 Administrative assistant: Cindy Garone 76224 or Lindsay Johnson 76226 On Day One: You will be scheduled for orientation. This will include 1. a morning of Epic (computer medical record) training 2. badge collection 3. parking information and access On the first day you may park in the visitor lot out the front of the hospital. On subsequent days you will be ticketed if you do not park in the assigned lot. Your badge will be your method of access to the parking lot, hospital and all departments and doors in the OR (includes anes work room) When you complete orientation please go to the OR and call the charge phone to find out if you are needed. Often you may leave, but you are expected to ask. General Info: Mail boxes are located behind the desk of Lindsay Johnson in the faculty office area (across bridge to admin area and take first right). You will receive meal tickets etc here. Attendings will sometimes run their own room, sometimes work one on one with residents and other times have 2 residents to supervise. There are NO CRNAs. Fellows and residents are equivalent on the schedules. Electronics boards: All patient information is on electronic boards in pre-op, post-op and ORs. Color codes are as follows: Orange: pt in facility. Yellow: pt in pre-op. Purple: pt is checked in with the pre-op area and ready to go the OR. White: pt on the schedule, but not in the hospital yet. Green: in the OR. Blue: in PACU. Pink: Phase II. Weekdays Daily Work Flow Do H&Ps on patients coming into the hospital as best you can using Epic. Give yourself 30 minutes to setup your OR before any morning conferences (Mondays 7:45 then daily at 6:45 in the Pikes Peak conference room on 2nd flr). Get a narcotics box from the cupboard behind the main OR desk. The key is hanging on the half wall next to the secretary. It has a purple cord on it. Sign box out on sheet located on counter below. The box contains drugs that will likely last you all day. Pull up drugs into larger syringes and then draw off smaller volumes for each patient leaving bulk of drug in the bigger syringe. Be CAREFUL not to mix up syringes that you have used in a patient line. My method is to keep needles on all clean syringes and cap all those used on patients. 28 The narcotic boxes provide 500 Fentanyl, 20mg morphine, 2mg remifentanil. No sufentanil is available. You can check out as many narcotic boxes as needed. It is important to remember is that ephedrine is considered a controlled substance and must be returned just as narcotics are. Attempt to see your first(and maybe 2nd) patient before going to conference, especially on busy/quick turnover days eg ENT Arrive in Pre-op around 7:15(8:15 on Mondays). Find your patient- check the electronic board showing name and room. Child may be in the play area, you will see a sign on/next to the door to their pre-op room. Make sure you ID the child and find correct parent(s). 7. Complete pre-op H&P. Nurses handwrite vitals on the intra-op chart, along with weight. 8. Consent the patient/parents, nothing to sign but discussion must be had with the family. 9. Remember to talk about who is coming back to the OR with the child. (Emergent cases or children under 12 months – NO parents back to OR). Tell the parents what they are likely to see as the child goes to sleep. Toddlers may fight and it may be upsetting to parents. Most children will wriggle during stage II, so let the parent know that after their eyes are closed and the child is asleep the body will move but they are NOT conscious. The parents do best when fully informed. 10. If doing an inhalation induction ask the child which smell he/she wants for her mask. 11. Versed premed is available as a PO order from you. Ask the parents how they think the child is doing with the process and if they feel that some sedation would be helpful. Most parents will know, especially if this kid is a frequent flyer. 12. If the child is a teen and almost adult size then you may chose IV induction vs inhalational. Discuss this with patient and family and prepared child for either method. 13. Go back to the room and do a final check and put pre-op into Epic while you wait for the child to come back to the OR with the circulating nurse. (This is nice….you do not bring the patients back to the OR) Call your attending to tell them the nurse is coming back with the patient/has arrived with the patient. Get patient up on the OR bed. Use your skills to keep the child engaged and happy while you preoxygenate and give a little nitrous oxide. This is an odorless way of getting the induction started. NOTE – if the patient is a small baby and is asleep then leave the pacifier in and induce before the baby wakes up. This is a very slick way of a no fuss induction. Some kids do better if sat up when induction begins – wrap a warm blanket around their shoulders and hug their arms to their sides as they drift off. Once the child is asleep the circulator will take parents out of the room. Then the attending will take the airway while you get IV access. This can sometimes be a challenge, especially in the chubby 2 yo child. You will quickly improve and learn to use the tools e.g. snake light to help you. Saphenous sticks are common in babies and those getting caudals for urological procedures. PACU orders are done in EPIC and should be complete before leaving the room for the PACU. Many attendings like deep extubations there are a few medical/attending specific exceptions. Take sux/atropine, narcotics and propofol with you to the PACU, you will be a hit with the nurses if you can quiet a “wild” child, so they can chart and get them on the monitor before the child is trying to get out of bed and pull out their IV. In PACU make sure all paperwork in anesthesia packet is signed and that nurses are able to access your order set in EPIC. The anesthetic record comes apart. White sheet stays with patient. Pink sheet goes with you for your drug box and green sheet goes with billing paperwork into tray on PACU desk. Usually will get “coffee” (15min), lunch (30min), and “tea” (15min) break. OR schedule with anesthesia assignments comes out around 4pm. It is emailed to us as a PDF and hard copies are available at the OR desk. Look up patients for the next day and call attending the night before to discuss plans. Call Nights/Weekend Call 29 Weekday call nights usually arrive at NOON. I have never heard of anyone being called in early. You will be joining an attending who has been in a room since 7am. Try to eat before coming to work, so you can relieve them for lunch on arrival. Weekend call is a 24 hour shift, changing over at 7am. Call room: located on the 2nd floor, past the bridge and conference room and through the double doors. There is a bank of call rooms found through a door on the right, labeled, no code needed. Our call room is labeled and the code is 8642. Code Pagers/Badge When on call you carry a code pager and badge that should let you in any locked door and can be used to over-ride the elevator. Pain service phone you will be paged by the pain service RN at about 5pm on call days. They will give you sign out and a spectralink phone. Ask plenty of questions especially about the plan for problems overnight. Keep track of any patients added overnight/changes made. Give report before conference in am. Codes Your responsibility is the “A” of the ABCs. Get to the head of the bed, assess need for airway intervention. It’s OK to push RTs, RNs, residents out of the way. Before intubation remember “VISA” Vventilator or ambu-bag ready?, I- patent IV functioning?, S- suction ready? (is it the right size for this child?), A- airway tools available? (correct size tube for the child?) Types of code: Level One Trauma – MUST attend. Sign in when you arrive. Level Two Trauma – do NOT need to attend Core – MUST attend. Airway Box – NO tackle box at TCH, but you may need to take a glide scope if going to a difficult airway child. Also, no neonatal microcuff tubes on the units, so bring those with you if you know they are needed. Morning after call Pain phone and report to RN coming on/C1 resident on weekends Code pager goes to C2 during the week and C1 on weekends If no pain nurse there at the weekend then you must round on all APS pts. Plan on a couple of hours for rounding, plus discussion with C1 attending. One way to speed this up is to copy previous day’s notes and “pend” them as new notes sometime during the night (ask someone to show you how). Then start seeing patients early, enter any updates, and sign notes. 30 Chronic Pain Clinic SARA CHENG, MD, PHD, GEORGIA GUERRA, RN Important people: Rotation director and Director of University Hospital Pain Clinic: Jason Krutsch, MD Other attendings: Robin Slover, MD (University), Mohammed Javed, MD (VA), Peter Rowe, MD (VA) VA secretary: Carrie Shurmantine – Anesthesia Department controller, she handles all badge & computer questions. (303) 393-2883. Email: carrie.shurmantine@va.gov Charge nurse, University Hospital Pain Clinic: Georgia Guerra, RN (8-1919, Georgia.Guerra@uch.edu) Other office staff: Liz (x81988) and Sara (x 8-2220) work at the front desk, triaging phone calls, making appointments and checking our patients in and out. Matt (x8-1095) is our care team specialist. Matt manages all new patients scheduling and many other office duties. Erni (x81989). She is the surgery scheduler and insurance pre authorization guru. Janelle (x81825) is the radiology tech. He is the person responsible for the procedure room and equipment. He also orders all office supplies. Maritza (x85943) is the MA. She assists the nurses with rooming patients and various other duties. Stephanie (x81832) and Steve are the registered nurses; they advocate patient concerns, assist with procedures, pre and post procedures teaching, conscious sedation, patient phone triage. Nurses are responsible for assessment/adjustment/ filling of pumps and recording settings. Georgia (x81919/pager 266-1417) is the charge nurse for the clinic. In addition to the above, she is responsible for the day to day supervision of the clinic. Ben (x8-2392) is the manager of the clinic. Need I say more! Chronic pain pager: (303) 266-7291 University Clinic phone: (720) 848-1970 Schedule: Dr. Krutsch is the director of the rotation. He is a great teacher, lots of fun, and will give you free advice on spiffy dressing. He decides at the beginning of each week which days you will be at the University and which days you will go to the VA. Occasionally you may get a weekday off! Email him the week before you start your rotation to ask where you should show up on the first day. The two residents on the rotation and the chronic pain fellow will take turns carrying the chronic pain pager for overnight and weekend call. The fellow usually makes this schedule and will arrange this with you prior to the start of the rotation. For one weekend, you will take acute pain service call and have to come in to round on all the APS inpatients. University orientation and tips: Learning how to blow it up with Dr. Krutsch is key. He’ll show you how. Clinic hours are 0730 to about 1630. The patients will check-in at the front desk and then are brought back to an exam room by the nurse for clinical visit note. The staff will bring you the paperwork or place it in the file holder in the provider back office. The nurse will print you the assessment sheet with the room number in the corner. This paper is just for your notes. When you’re done with it, put it in the confidentiality bin in the back office. You will then see the patient and report your assessment to the attending. New patients fill out a health history form on their first day as a new visit which helps you with their assessment. These must be placed in the basket to be scanned as part of their medical record. 31 Procedures: If the staff is aware of the procedure to be done, insurance authorization and teaching will be completed in advance. Only procedures that have been preauthorized are preformed. Check with Matt, a Nurse or Erni if uncertain. Notify a nurse when you have completed the consent and are ready to go to the procedure room. The nurse will take the patient back. This gives you time to set up your meds and review the procedure. Reminder: Consents must be dated and times filled in by both the provider and the patient. Provider preferences are in a green book in the procedure room. Helps with prep/meds. Sedation: The nurse or Dr Krutsch will sedate the patients as ordered. They will want to know about the order as soon as possible. Please allow 15-30 minutes to give a po valium or to start an IV. If you are administering a sedative, please inform the nurse. Sedation H&P must be completed (label all forms) before sedation is given. Orders must also be written and signed by the provider. The nurses will work with you on these forms. Afterwards the patient will be recovered and monitored according to the amount of sedation received. Eye wear: if you do not have your own set, we have disposable to be used in procedure room. Check-out: When a patient is ready to be discharged, a gold Return Appointment Scheduling form is required. This is used to allow the front desk staff to schedule the patient’s next visit, please fill it out completely. RPV= return visit, FLU= procedure that requires fluoroscopy. PRO- Procedure but no Fluoro required. Future sedation needs are marked, if it will be needed. Future procedures: Please fill and give the yellow procedure instruction sheet. Order a test, a consult, PT or OT: Most Lab and diagnostic tests can be ordered on touchworks, ask the provider. Spinal Cord Stimulators: If a stim. is something you would like the patient to consider, you can find the patient instructions as well as give the patient a video and booklet to review. These can be found in the metal cabinet in the physician’s room. The patient will need a psychological consult with a MMPI. Ask the patient to make an appointment to come back for a preop visit after the psych eval is done. When the patient comes back for the preop visit we will get them the surgical dates and postop appointments at that time, not before. You will need to fill out the preop surgery packet, found in the nurse station. The packet must be completed and given to Erni to schedule and authorize the patient’s procedure. If a patient has a pump or implanted SCS, the nurse or attending will show you how to interrogate them. After reprogramming, a printout is made for the patient, the nurse and one to be scanned into the computer. Labels need to be placed on all patient paperwork The attending will teach you about Touchwork-Allscript, dictation and/or typing your notes. They will review with you what needs to go in your notes and will give you templates to make it easier. VA Pain Clinic tips: Hours are from 0730 to about 1600, usually. You will need you badge and working computer codes to write your notes. Make sure that you contact Carrie (contact info above) if you haven’t been there in a while to make sure everything still works. Ask her about the parking situation- it changes whether pain residents can park in the lot or not. The VA clinic is awesome in that it is entirely procedure based- you will be doing only new patient evaluations and blocks. No pain medicine management at all- that is done by the PCP. The pace is slower than at the U, so you won’t be running around like a chicken with its head cut off. The attendings will show you what CPRS templates are useful to use. They will also show you the set-up and the location of meds in the block room, how to consent the patients on the computer, etc. If you do a good job, you can end up doing all of the blocks with attending supervision, since the fellow is not there if you are. Sometimes you might get to do some OR procedures with Dr. Rowe- always an interesting experience to be on the other side of the drape for us- try not to yell at anesthesia, ‘kay? (ie. What’s the hold up? Where’s my patient?) 32 Obstetrics (Labor and Delivery) ESTEE PIEHL, MD Codes: 4th Floor Work Room: 11153 5th Floor Work Room: 11153 All Med Rooms: 84111 Nutrition Rooms: 11153 Women’s Locker Room: 11153 Men’s Locker Room: 6667 Call Room: 0404 OR carts: 1+2 together then 3 Phone Numbers: OB Charge Phone: 8-5973 OB Resident Phone: 8-5972 OB CRNA Phone: 8-5911 Scheduled Meetings: 7am T-F: Team Meeting/ OB signout (we go to Grand Rounds on Mondays) 5pm M-F: OB evening signout (try to make it if you can) 12:30pm on Tuesday: MFM Clinic Meeting One Friday (or more) a month: Care Conference (you will be emailed a time) Reading: As always, Morgan and Mikhail is not a bad place to start. You will also be given 2 big fat readers for OB. Before you start, be sure to at least read the first 2-3 pages of Book 1- these contain basic expectations and the “cookbook” for what drugs to use in different situations. Many residents photocopy the “cookbook” and carry it in their scrubs pocket for reference. Schedule: The schedule on OB is different from every other rotation. You will be working 12 hour shifts from 7am – 7pm or vice versa. The usual schedule is three days, then three nights then three days off. However, this is changed around for any number of reasons and may be way more random than that. It is nice to arrive at 7am in the morning, no doubt, but the schedule is not as nice as it sounds so beware the pitfalls: 1. If this is your first OB month, CHECK YOUR SCHEDULE TO MAKE SURE YOUR FIRST 1-2 SHIFTS ARE DAY SHIFTS. The chiefs work very hard to ensure this is the case but it is in your best interest to double-check. Doing your first OB shift at night is hard because you will less supervision and teaching than during the day. 2. Don’t plan to get much sleep on OB at night. This is not like an OR overnight call where once you knock out the cases on the board you have a good shot of getting a chunk of sleep for the rest of the night. You will get woken up all night. You will always get the first call for any epidurals, c-sections, etc. This is so that we can get the experience that we need. However, it can be downright rough on your fourth overnight. So, it goes without saying, the first day of your three days off, you will probably sleep the whole day. 3. You will be tired by the end of the month. Changing from days to nights and back is really hard on your sleep cycle. So, do what you have to do to get some sleep on your off time: melatonin, Benadryl, Ambien, whatever. Granted, your neighbors might look at you funny if you are drinking wine on your porch at 8am. So keep it in the closet! Just kidding. 33 4. A note for people with kids: It will be a hard month if you have small children because you might not see them a lot. Leaving at 6:30am and getting home around 8pm for 3-4 days in a row might mean that you won’t see them for 3-4 days. (Not much to do about it - just a word of warning. You may want to enlist help/warn your spouse in advance so they don’t kill you.) That said, the OB rotation is a really good one, much loved by all for several reasons: 1. We have great OB attendings who actually like to teach and a good syllabus. The OB attendings are: Joy Hawkins, Brenda Bucklin, Andi Fuller and Matt Fiegel. They all like to teach and will happily discuss any OB topic that you pick for the day provided that there is time. They are usually on service during the days. That is especially helpful in the first month when you have no idea what you are doing. Most of the attendings that cover nights have no particular interest in OB so they let you run the show. They will come help with all C-sections, if possible, but frequently will not come for epidurals in the middle of the night. This is why we all do a lot of days at the beginning of our first month. Make sure that you learn all you can from the OB attendings during days because at night you are often on your own **See the cookbook card at the end of this segment**. 2. Tons ‘o Procedures!!! This, of course, makes any real anesthesiologist’s heart go pitter-pat-pat. The OB attendings have worked very hard to make sure that we get called before the CRNAs for procedures (oh, yeah, BTW there is also a CRNA in house 24-7) so that we can get experience. Again, tough in the middle of the night sometimes, but that is what we are here for. 3. We get every Saturday 7a-7p off. Entirely. As in no resident is in house. Cool, huh? The CRNAs cover the Saturday day shift by themselves so we get it off. Baseball games in the summer, skiing in the winter – you can plan it now! Some pearls… 1. Use the CRNAs as a resource. Many of the CRNAs that do OB have had a lot of OB experience. You can ask them questions, ask them for help, whatever. Don’t forget to call them when the “you know what” hits the fan. They are a really helpful second (or third) set of hands in those situations. 2. OB RNs are very involved with their patients. They really want what is best for their patients. Sometimes that may come across as them trying to push us around. For the majority of them, this is not true. They want us to put epidurals in ASAP so that their patients will not be miserable and in pain. Exactly what we want. However, we all understand that we have to do it safely. 3. Figure out how to restock the carts properly and make up charting packets at the very beginning of the month. We have to restock our own epidural carts from the workroom supplies. Learn how to do it at the beginning so all of the carts aren’t missing stuff by the middle of the month. Also, we have no computer charting on the OB floor (yet) so we have to use the old paper charts. There is a lot of paperwork so make sure that someone shows you how to fill it all out at the beginning. 4. Do paperwork after you put in the epidural. As the OB attendings will teach you, the most common time for crashes to happen after the placement of a neuraxial block is during the first 30 minutes after the block. Therefore, we should personally watch the patient during this time. This is great time to do the goo-gobs of paperwork (rather than before the epidural is placed when the patient is screaming in pain). 34 Transplant SARA CHENG, MD, PHD The main focus of this month is doing liver transplants. You will also spend some time doing kidney transplants as well. The liver recipients may have major derangements in multiple organ systems, and the liver transplantations often involve major hemorrhage, coagulopathy, and hemodynamic instability. These are big cases, but IMHO very satisfying. The teaching on this rotation is excellent, as your attending will rarely leave the room for very long. Important people: Susan Mandell, MD- Head of Transplant Anesthesia. Other attendings: Drs. Fareed Azam, Matthew Fiegel, Adrian Hendrickse, and Matthew Roberts. Anesthesia transplant fellow: Dr. Sara Cheng. Reading: A 3 ring-binder will be given to you by Suzanne Bullard. Get it early and take a look at the OR setup beforehand. Schedule: Deceased-donor liver transplantation is generally a semi-emergency due to the limited ability of the donor organ to tolerate cold ischemia. (Occasionally a live donor case will be done here- rare). Thus, you’ll be on 24-7 call for all but 2 weekends of this month. The rest of the time you will be working in the OR on days. Try to be proactive and ask the charge attending to put you on good cases for the next day’s schedule. It is also good to remind him/her that you are the transplant resident- ideally, you should be relieved relatively early from your daily duties, as you may be called back at any time each night. Keep your eye on the board- you’ll want to know if a transplant is added on for 6 PM, so you can try to get relieved from your room and get some dinner, call your spouse, feed your dog etc. When the OR desk calls you on nights/weekends for a liver transplant, they will usually give you at least 3-4 hours notice, if not more. Always call the desk again before you head into the hospital, as plans may have changed. Remember to ask the patient’s name, MR #, and whether the attending and fellow have been informed. If not, you need to call them. Once you are on your way in, call the OR pharmacy @86132 and order your drips (mannitol, magnesium, vasopressin, phenylephrine, and dopamine) to be tubed to the OR desk. OR set-up: Start your H&P by taking a quick gander at the most recent labs, calculate a MELD at http://www.unos.org/resources/meldpeldcalculator.asp so that you know what you’re up against. Equipment: Belmont rapid infuser, ultrasound, double transducer, at least 4 IV pumps, a-line/PIV bundles, Bair hugger, warmed room. Occasionally you’ll do a PAC or a dialysis catheter for a really sick recipient; check with attending. Drugs: Transplant box from Pyxis, standard emergency drugs, midazolam or lorazapam and fentanyl, propofol/etomidate/thiopental for induction depending on attending preference and pt’s hemodynamics, calcium, sodium bicarb, cisatracurium from pod fridge, epinephrine @10 mcg/ml and 100 mcg/ml. Drips: guess your patient’s weight and set up your drips as follows: magnesium 1 grams/hr, dopamine 2 mcg/kg/min, vasopressin 0.04 units/min, 20% mannitol 30-50 cc/hr. Phenylephrine (high concentration- 200 mcg/ml) should be hung free on a microdripper. Blood: The attending anesthesiologist is in charge of calling the blood bank and designating the case as low, medium, or high risk for massive hemorrhage. These categories are based on current labs and history of previous surgery, and will dictate how much blood is sent to the OR. Make sure this cooler is present before you bring the patient back! 35 Intraoperative management tips: Be sure to read in your notebook about the phases of the surgery (prehepatic, anhepatic, post-reperfusion) and reperfusion syndrome. Check with your attending regarding what induction drugs and intravenous access he or she likes to useeveryone has their preferences. In general, all liver recipients should be treated as full stomach and thus receive a rapid or modified rapid sequence induction with cricoid pressure. Adequate IV access is essential. A reasonable approach is to get as much peripheral access as possible and then decide what kind of central access you need. (ie If you have 2-3 short 14g PIV or a Rapid Infusion Catheter then you can go with a triple lumen in the neck, otherwise you might need a cordis.) Arterial line is standard, pulmonary artery catheter is not unless pulmonary hypertension or cardiac problems are obvious, and a dialysis catheter may be added if needed intraop or postop. Always use the ultrasound for line placement, as coags and platelets will likely be abnormal. Ask your attending what they want to wet down the Belmont with- usually normal saline, as colloid tends to foam. 36 Sample notes There are many different ways to do your documentation on paper charting. Just be sure it is legible and that you document attention to key points. These are just a few examples, be sure to check with your attending or senior resident. 37 Bier block: Pt ID, H&P, Q&A. Consented. Bilat hand 20 g PIV. Abx. To OR6. ASA monitors. NC O2. Sedation. RUE Esmarck. RUE tourniquet up to 250 mmHg @0745. 50 cc 0.5% lidocaine injected smoothly with good venous distention. VSS, no sx of local anes tox. Blankets on upper/lower body. Patient comfy for procedure. ICU transport of intubated patient: Pt ID’d, chart reviewed, IC from power of attorney. Report received from nurse. To OR10 with ambu+O2, aline, EKG, pulse ox. VSS. In situ ETT to machine circuit. ASA monitors. OGT to suction. Eyes taped. Foley to grav. Arms < 90º. All PPP. UBBH. Esoph temp probe. 38 Useful websites Anesthesia department intranet site https://hschealth.uchsc.edu/anes/ Online evaluations www.new-innov.com ACGME case log www.acgme.org/residentdatacollection Online call schedule www.amion.com, password: uco Web-based email access webmail.uchsc.edu UCHSC Health Sciences library http://hsclibrary.uchsc.edu/ ASA homepage http://www.asahq.org ASA calendar of meetings, searchable http://events.asahq.org/ NYSORA website http://www.nysora.com/home.shtml Critical care medicine from U Penn http://www.ccmtutorials.com/index.htm 39 Maps University of Colorado/Anschutz Medical Campus Anschutz Inpatient Pavilion, 12605 E. 16th Avenue, Aurora, CO 80045 40 VA Map 1055 Clermont Street, Denver, CO 80220 Parking is across the street from the VA hospital. 41 Denver Health Medical Center 777 Bannock Street, M.C. 0218, Denver, CO 80204-4507 42 Notes 43 Notes 44 Notes 45