Pathophysiology Final Study Guide
advertisement

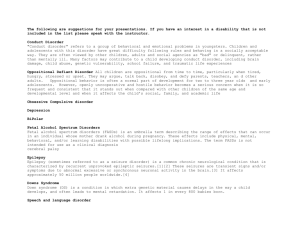
Pathophysiology Final Study Guide Patho Section 1 Cell & Tissue Function/Dysfunction Atrophy: decrease in size of cells. Hypertrophy: increase in cell size. Hyperplasia: increase in number of cells. Metaplasia: mature cell type is replaced by a different mature cell type. Dysplasia: cells vary in size & shape within a tissue. Anaplasia: undifferentiated cells with variable nuclear & cell structure. Neoplasm: tumor. Cell Damage Ischemia: oxygen deficit due to respiratory or circulatory problems. Hypoxia: reduced oxygen in tissue. Oxygen Deficit: decreased energy production, loss of Na pump ↑ intracellular Na. Temperature: inactivation of some enzymes, damages organelles, protein coagulation, disruption of cell membrane. Micro-organisms Abnormal Metabolites: caused by genetic disorders or altered metabolism. Nutritional Deficits Cell Death Apoptosis:programmed cell death controlled by genetics. Necrosis:lysis of a cell, cell components leak into blood. Liquification:dead cells liquefy due to release of enzymes. Coagulation:cell proteins are altered or denatured causing coagulation. Caseous:form of coagulation necrosis, thick, yellowish, cheesy. Fat: fatty tissue is broken down into fatty acids. Tissue Damage from Chemicals Exogenous: from environment. Endogenous: from inside the body, Tissue Damage from Physical Agents Hypothermia: vasoconstriction, ↑ blood viscosity, hypovolemic shock ↓ blood pressure. Hyperthermia: causes general vasodilatation, decrease in circulating blood volume. Radiation: primarily affects actively dividing cells Biological Agents Insects/Animals: direct injection of toxin, transmission of infectious agent, allergic reaction to insect proteins. Food Poisoning Normal Defenses of the Body 1st Line Defense Physical Barriers: unbroken skin, mucous membranes, nasal hair, clots. Fluids: may contain enzymes or chemicals:saliva, tears, gastric, sweat. 2nd Line Defense-non-specific Phagocytosis:neutrophils & macrophages engulf cells, debris, foreign mat. Inflammation: automatic response to cell injury. 3rd Line Defense-specific defense produced by Antibodies Cell Mediated Immunity Cellular Defenses Mast Cells: located in tissue & release histamine & bradykinin. Macrophages: monocytes that enter tissue & act as phagocytes. Interferons: small proteins made by lymphocytes to prevent virus replication. White Blood Cells Granulocytes Neutrophils: work by phagocytosis. Basophils: release histamine leading to inflammation. Eosinophils:combat the effects of histamine. Agranulocytes Monocytes:can enter tissue to become macrophages which function as phagocyte. Lymphocytes: B & T Acute Inflammation Vascular Response: vasodilatation & increased capillary permeability. Cellular Response: migration of inflammatory cells through chemotaxis to injury site to destroy ineffective organism, remove damaged cells, released inflammation mediators. Exudate Serous: watery, mostly fluids, some proteins and WBC’s. Fibrinous: thick, sticky, high fibrin content. Purulent: thick, yellow-green, contains leukocytes, cell debris & microorganisms. Abscess: Pocket of purulent exudates or pus in a solid tissue. Local Effects of Inflammation-Cardinal Signs of Inflammation Redness & Warmth: due to increased blood flow to area. Swelling: shift of protein & fluid into interstitial space. Pain: pressure on free nerve endings, chemical mediators irritate nerves. Loss of Function: edema may restrict movement. Systemic Effects of Inflammation Mild Fever: due to resetting of hypothalamic thermoregulatory set point, release of endogenous pyrogens. Malaise Fatigue Headache Anorexia Treatment of Inflammation: drugs may decrease capillary permeability, reduce number of leukocytes & mast cells. Types of Healing Resolution: minimal tissue damage, cells can repair themselves. Regeneration: damaged tissue is replaced by identical tissue. Replacement: functional tissue replaced by scar or fibrous tissue. 1st Intention: wound is clean, edges are close together with minimal gap. 2nd Intention: large break in tissue, longer healing process with more scar tissue. Scar Formation: fibroblasts proliferate, abnormal amount of collagen. Hypertrophic: overgrowth of fibrous tissue, keloid. Ulceration: blood supply around scar is impaired resulting in tissue breakdown. Wound Staging 1. Partial thickness ulcer-red or pink ie. Sunburn. 2. Partial thickness ulcer-blister, scrape, abrasion. 3. Full thickness ulcer- through dermis. 4. Full thickness ulcer that includes muscle or bone. Drainage Transudate: clear & watery. Serosanginous: clear w/ tinge of red/brown. Contains serum/blood thin & watery. Exudate: creamy yellowish. Contains proteins & WBC’s Thick. Purulent: yellowish. Contains leukocytes and necrotic debris, thick. Infected Pus: hues of yellow, green or blue. Contains pathogens, thick. Venous Insufficiency Clinical Presentation Incompetent Valves medial leg area Inefficient Calf Pump edema Distended Capillary Bed wet wound Decreased Fibrolysis scaring, red base Fibrin Leakage hemosiderin deposits(purple/brown on leg) Trauma Ulcer Documentation of Pulses Normal: 2+ Diminished: 1+ Absent: 0 Arterial Insufficiency: decreased arterial blood supply. Acute(thrombosis) vs Chronic(arteriosclerosis) Characteristics Dry Gangrene: nonviable dry tissue. Wet Gangrene: tissue necrosis + bacterial infection. Drainage w/ odor. Black Gangrene: gangrenous borders, mummified skin. Pain w/ walking=Claudication Skin is atrophic(no hair) slow nail growth & Diminished Pulse Ankle Pressure Index: SBP LE/SBP UE >1 no arterial occlusive disease .9-1 min sx in LE .5-.9 claudication pain(leg pain w/ walking) .3-.5 ischemic rest pain <.3 ischemic w/ tissue necrosis Assessment of arterial flow, skin color w/ elevation/dependency 1. LE Elevation to 60º for 1 minute. Normal=no color change. 2. Lower the LE & record time for color to return.>30seconds means arterial insufficiency. Will look hyperemic(bright red). Immune Response-Third Body Defense Humeral Immunity: antibodies are produced to protect body & stored in blood. Cell Mediated Immunity:lymphocytes are programmed to attack non-self cells. Antigens:immunogens, proteins, polysaccharides, glycoproteins on cell surface. Cells Macrophages:present throughout the body, derived from monocytes, initiate immune response, engulf foreign materialprocess & display foreign antigens & present them to lymphocytes, secrete monokines & interleukins . Lymphocytes:primary cell in immune response, T: has 3 subgroups made in bone marrow & differentiate in thymus, cell mediated immunity, can target certain cells. 1.Cytotoxic T:cells destroy cells bind to antigen & release enzymes 2.Helper T: facilitate immune response by activating & regulating 3.Memory T: remember antigens. B:Made in bone marrow, located in spleen & lymphoid tissue, produce antibodies. Natural Killer:kill tumor or virus infected cells w/o prior exposure Antibodies IgG:most common, can activate compliment, cross placenta, primary & secondary immune response. IgM:can activate compliment, natural antibodies ie. Involved in blood type IgA:not in blood, is in tears, saliva & colostrums. IgE IgD Compliment System:antigen-antibody complex, activated during immune rxn w/ IgG or IgM. Causes cell damage when activated, causes macrophages to release enzymes. Immune Response Primary: 1st exposure to antigen, 1-2 weeks needed for effective antibodies Secondary:repeat exposure to same antigen, effective response in 1-3 days Immunity: Innate-always present. Or acquired. Hypersensitivity Reactions Type 1 Hypersensitivity:allergic rxn, exposed to allergen causes development of IgE’s,activate mast cells and causes inflammation. Ie. Hay fever, allergies, asthma Type 2 Hypersensitivity:cytotoxic hypersensitivity. Antigen on cell membrane reacts w/ circulating IgG’s, activates compliment, cells w/ antigen destroyed. Ie incompatible blood type exposure. Type 3: Immune complex hypersensitivity-antigen & antibody combine forming immune complexes that cause inflammation & tissue destruction. Type 4:Cell Mediated or delayed response by T-lymphocytes. No antibodies present. Ie. Tb test, contact dermatitis. Immune System Malfunction Hypersensitivity: full system immune response to non-noxious stimulus. Asthma: central windpipe or airway disorder. Interventions/Treatment:avoid triggers, medicate. Peak flow 50-80% of person’s best signal moderate attack, >50% below best PF = major attack. Autoimmune Multiple Sclerosis: autoimmune demyelinization of nerves in brain &CNS Classification Clinically Isolated Syndrome-only suffer 1 attack. MS-multiple attacks at least 1 month apart & damage to at least 2 separate CNS areas & r/o all other possible causes. Tests & Measures: MRI, visual evoked potentials, CSF analysis. Interventions: modify disease course, treat attacks, manage sx. Myasthenia Gravis: antibodies destroy Ach receptors at NM junction. Guillen Barre Syndrome: demyelination of peripheral nerves. Fibromyalgia: generalized musculoskeletal pain > 3 months, multiple tender points affecting all 4 quadrants, 11/18 points, 4Kg force painful Rheumatiod Arthritis:autoimmune destruction of joints affects multiple joints in symmetrical pattern, inflammation can affect organs. Scleroderma:affects microvessels causing hypoxia in all tissue. Skin & organs commonly affected. Sjogren’s Syndrome: autoimmune disease » loss of fluid for tears/saliva Hashimoto’s Disease: autoimmune thyroid disease, causes hypothyroidism Graves Disease: hyperthyroidism, Type 1 Diabetes: autoimmune destruction of pancreas cells » no insulin. Inflammatory Bowel Disease: group of disorders with inflammation of intestines Crohn’s: ulcers throughout intestines, except rectum. Ulcerative Colitis: ulcers in lower intestines, may begin in rectum. Immunosufficiency HIV Meningitis: photophobia is red flag. Toxoplasmosis: parasitic infection. Contaminated cat feces in 1st trimester. Histoplasmosis: fungal infection diagnoses based on organ involved Micro-organisms Bacteria-unicellular organisms, no nucleus, divide by binary fission. Cocci-staph, strep, diplococci-pneumococcus Bacilli-tetanus, botulinum. Spirochetes-syphillis, cholerae. Gram Positive: doesn’t retain crystal violet, has outer membrane layer. Gram Negative: retains crystal violet, no outer layer, thick peptidoglycan layer Toxins Exotoxins: produced by gram+ bacteria. Endotoxins: gram- bacteria. Released when bacteria die causing shock. Virus Active Viral Infection: virus attacks host cell injects genetic material, uses host cell to produce viral proteins & nucleic acids. New viruses made in cytoplasm & released by lysis or budding from host cell. Latent Viral Infection: virus enters cell similar to active infection, replicates slowly or delays replication, viral proteins are inserted into cell membrane of host cell causing immune response. Ie. Herpes virus. Fungi: eukaryotic organisms, primarily affect skin or mucous membranes. Protozoa: eukaryotic organisms, usually parasites. Ie. Malaria, dysentary Prions: protein like agent that can change shape of proteins in host cell. Mad Cow. Modes of Transmission Direct Contact Indirect Contact Droplet Aerosol Vector Nosocomial Infections: infections that occur in healthcare setting. Development/Stages of Infection Incubation Period: time of organism entering body to appearance of clinical signs Prodromal Period: infection is developing, nonspecific symptoms. Acute Infection: fully developed infectious disease with peak clinical signs. Chronic Infection: microorganism continues to replicate in body, sx milder. Subclinical Infection: Microbe can reproduce in body but no signs present. Septicemia: bacteria reproducing & circulating in bloodstream. Complimentary Medicine Red Flags: refer to Dr. Chest pain/discomfort, unusual SOB w/ acute pain in chest, arm, throat or jaw, unexplained dizziness, persistent hoarseness or cough, difficulty swallowing, persistent abdominal pain/discomfort, coughing up blood, unexplained weight gain/loss, persistent unexplained fatigue, changes in a mole, change in bowel/bladder habits, blood in stool, unexplained vaginal bleeding, lump in breast or discharge or change in size or shape, changes in testicles, severe HA, blurred vision, sores that don’t heal, persistent unexplained lumps/swelling, persistent back pain even w/ rest, unexplained leg swelling/pain. Screening Lab Fingernails Absent Lunula: anemia, malnutrition. Pyramidal Luluna: trauma or excessive manicures. Red Luluna: cardiovascular disease, collagen disease of vessels, blood CA Mee’s Lines: metal toxicity, chemotherapy exposure. Longitudinal Lines: Addison’s disease, breast CA, melanoma, trauma. Splinter Hemorrhages bacterial endocarditis, lupus, renal failure, psoriasis Terry’s Nails:half& half appearance:edema & anemia »renal/liver disease. Cancerous Moles-asymmetry, border, color, diameter PATHO TEST 2 REVIEW General Cancer Info General Genetics Info Cancer rundown Bladder Cancer : -Early stages bleeding in urine but little no pain -Hematuria 1st sign with changes in urination Breast Cancer: -New lump is most common symptom -Manual palpation better catch than mammogram Cervix cancer: -often asymptomatic -vaginal discharge, abnormal bleeding, pain during intercourse Colorectal cancer: -change in bowel habits most common -Diarrhea, constipation, more narrow stools, blood in stool -Bright blood-lower GI, Dark/black blood-Upper GI Lung cancer: -persistent cough with or w/o chest pain -Feeling of an infection that just won’t go away Prostate cancer: -weak interrupted urine flow, frequent urination esp. @ night Renal cancer: -low back pain, especially if pain not assoc. w/ injury Skin Cancer: -Any new growth on skin should be examined -Spot or bump that changes size, irregular borders -Sore that will not heal Change in bowel/other habits A sore that does not heal Unusual bleeding or discharge Thickening or lump in breast Indigestion or difficulty swallowing, unexplained weight loss Obvious change in wart or mole Nagging cough/hoarseness Fluid/Electrolyte imbalance Water -60% adult body wt, 70% infants, higher % in females Fluid compartments -Intracellular 2/3 water in body -ECF 1/3 *Interstitial 3/4, Intravascular 1/4, Cerebro Spinal Fluid 1% Control Fluid Balance->Thirst mechanism -Antidiuretic Hormone (ADH): fluid output -Aldosterone: Reabsorption of water and sodium -Atrial Natriuretic Peptide (ANP): lowers BP by controlling blood volume EDEMA: fluid excess in interstitial compartment DEHYDRATION: Signs-decreased skin turgor, sunken eyes, low BP, rapid weak pulse, high temp ELECTROLYTES Intracellular electrolytes: potassium, phosphate, magnesium Blood electrolytes: sodium, calcium, less extent bicarbonate EXCESS/DEFICIENT ELECTROLYTE CAUSES of EFFECTS of Excessive sweating, vomiting, diarrhea, insufficient aldosteerone, kidney failure, excessive waterintake Insufficient ADH, loss of thirst mechanism, watery diarrhea, rapid respiration, Diarrhea, diuresis, excessive aldosterone, low dietary intake, Insulin forces K+ into cell Renal failure, deficit aldosterone, leakage of K+ from ICF into ECF, prolonged acidosis (H+ replaces) Hypothyroidism, malabsorption syndrome, deficient serum albumin, increased serum pH HypoMagnesmia Malabsorption of assoc with alcoholism, use of diuretics Impaired nerve conduction, fatigue, mm cramps, Abdom issues, decreased Osmotic pressure in ECFTHUS fluid into cells Fluid shift out of cells, weakness, dry tongue mucous membranes, increased BP Cardiac Dysrythmias, interference with neuromm junc, decreased dig. Tract motility Cardiac dysrythmias, mm weakness common progressing to paralysis, respiratory arrest Increased permeability/ -excitability of nerve membranes,spont stim of skeletal mm, Tetany, weak Heart contractions Depressed neuromm activity -interference with ADH function -increased strength cardiac contractions Neuromuscular hyperirritability heart arrythmia HyperMagnesmia Renal failure Depressed neuromm funct HypoNatremia HyperNatremia HypoKalemia HyperKalemia HypoCalcemia HyperCalcemia Uncontrolled release from bones demineralization from immobil. -increased intake CAUSE(S) GENETIC DISORDERS Angelman syndrome Cri du Chat Downs syndrome X-linked, lose “bit” of chromosome Missing part chromosome 5, mutation at Trisomy 21 Fragile X syndrome Fragile x retardation protein Neurofibromatosis Autosomal dominant, CHARACTERISTICS Flat head. PROTUDING TONGUES odd bouts of Laughter, Balance disorders Hi “CAT-like” cry, webbed toes & fingers, DOWNward slant to wide set eyes, skin tags ant. ears Flat face, Upward slanted eyes, single DEEP crease palm of hand, HYPOtonia (low muscle tone), Large head w/ prominent forehead, boys develop long face, tactile defensiveness Esp. effects nervous syst and skin, birthmarks called café-au-lait, freckles in armpits and groin, purplish RUBBERY lesions on skin GENETIC DISORDERS CAUSE(S) Prader Willi syndrome Chromosome XV Smith-Magenis Syndrome Deletion @ XVII Klinefelter’s Syndrome Men w/ extra X chromosome Turner Syndrome Females w/ only 1 X chromosome Triple X syndrome Extra X chromosome Williams syndrome Random mutation chrom. 4 Cystic Fibrosis Single point mutation CFTR Muscular Dystrophy Dystrophin-over 30 different genetic diseases CHARACTERISTICS Extreme hunger/overeating, obsessed w FOOD, temper tantrums, violent outbursts, @ 1 Y.O. become ravenously hungry Broad nasal bridge, PROTRUDING jaw, ear anomalies, SPEECH & middle ear problems, SLEEP disturbances Sudden Mood changes Teenagers less developed, prepubescent testosterone helps, testosterone levels to diagnose, infertility WEBBED neck!! Underdeveloped BREASTS High BP, Type II diabetes Girls TALL, often not diagnosed, no long term problems 50% retardation, PUFFINESS around eyes, long neck, sloping shoulders, Poor DEPTH perception Life limiting (30s), frequent coughing w/ thick sputum, saltyskin, frequent lung infections, -Duschenne most common (missing dystrophin), affects skeletal & cardiac Muscle -Fascioscapulohumeral-faulty dystrophin -Myotonic; congenital, juvenile, adult, late onset-over 50 ACID-BASE Imbalance -> Normal 7.4, ranges from 7.35 to 7.45 o Enzymes act in narrow pH range 20:1 base to acid ratio Respiratory system- alters carbonic acid levels Acidosis-> CO2 up Kidneys- modifies excretion rates of acids, Most effective control system Acidosis: excess Hydrogen ions Alkalosis: deficit in Hydrogen ions Acidosis HCO3- down Alkalosis HCO3- down **compensation occurs to balance relative ratio (20:1), NOT total concentration BLOOD DISORDERS Hemocrit - proportion of cells (RBC) -indicates viscosity & inc or dec in hydration Hemoglobin: Tetramer-> 4 hemes which carry 1 oxygen each Hemostasis: Hemophilia A: 90% of cases, deficit of clotting FACTOR III, an X-linked recessive trait Hemophilia B: Xmas disease, deficit FACTOR IV Hemophilia C: factor XI, milder form Blood therapies: o Whole blood: for severe anemia o Artificial EPO (stimulates RBC production) o Bone marrow Transplants: some cancers, immune deficiencies, blood cell disease ANEMIAS- can lead to ANGINA or CHF Hemoglobin deficit= reduction in oxygen transport General signs Fatigue, pale face, dyspnea, tachycardia Causes Nutrient deficiency Impaired bone marrow Blood loss or excessive destruction of RBCs Iron deficiency: impairs hemoglobin, very common, usually underlying CAUSE Pernicious Anemia o Large, immature, nucleated erythrocytes(RBCs) o SYMPTOMS-> Tongue large, RED, sore, shiny o Aplastic Anemia o Temporary or permanent impairment or failure of bone marrow o Bone marrow cells replaced by FAT o Cause must be ID’d for prompt treatment & marrow recover or is LIFE threatening Hemolytic anemia o CAUSE: excessive destruction of RBCs via many causes Sickle Cell Anemia-> abnormal hemoglobin o Genetic condition; autosomal rec., heterozygous R carrier More common n AFRICAN ancestry o Sickle cell crisis occurs when LOW O2 levels When deoxygenated HbS is unstable and crystallizes=sickle shape Thalassemia o Most common blood disorder in world o Abnormal hemoglobin due to missing genes ANEMIAS CONT. Polycythemia o Primary polycythemia->Increased rate of RBC production o Secondary polycythemia-> Increased RBC production due to prolonged Hypoxia Concerns for both: Category Sytemic disease Musculoskeletal Sluggish blood flow Increased BP & hypertrophied heart Indications of Blood clotting Disorders o Persistent bleeding in gums & nose bleeds, bleeding into joint, coughing up/vomiting blood, blood in feces, vomiting, low BP Causes of clotting disorders o Defective platelet function o Long term use of warfarin Hemophilia A (classic) o Most common inherited clotting disorder o Varying severity o Spontaneous bleeding into joints Disseminated Intravsascular Coagulation o Excessive clotting & excessive bleeding in circulation o Clotting factors reduced to dangerous level o Widespread uncontrollable bleeding o HIGH fatality rate THE LEUKEMIAS Acute High proportion of IMMATURE, nonfunctional cells in marrow and circulation Onset is abrupt SIGNS: Frequent uncontrolled infections ,BONE PAIN, Weight loss, fatigue, drowsiness, vomiting Chronic Higher proportion of MATURE cells Insidious onset Mild signs & better prognosis Diagnostics for all leukemias Peripheral blood smears Bone marrow biopsy confirmation Treatment-> Chemo, Biologic therapy using INTERFERONS, Can stimulate immune system Histology: Differential diagnosis of Systemic Pain versus Musculoskeletal Course/duration Relieving Factors Aggravating Factors Quality Intensity Location Associated signs & symptoms Cyclic, progressive symptoms Constant or may come & go Usually NONE : if relieved by rest or position, there is typically cyclic progression of increasing frequency, intensity, or duration until rest/position doesn’t work None specific DEEP, ACHING, throbbing DIFFUSE or waves/spasm Severe if cancer spread to nerves surrounding a visceral organ From Upper back, middle to low back regions. May also be in front of trunk frequently in abdomen over affected organ Jaundice, skin rash, weight loss, fatigue, low-grade fever, muscular weakness, frequent infections Sudden (gradual when related to overuse) Decrease with Rest Increase with use affected region SHARP Depends on if acute, subacute, or chronic Located over injury sight. If severe may also refer proximal and distal to injury sight Usually none- trigger pts may be accompanied by nausea/sweat Patho 3 Cardiovascular Disorders - Gould Ch. 18 -general treatment -Low Na+, fat ->Decrease weight -exercise – Increase HDL, decrease LDL (high and low density lipoproteins) -smoking cessation -Vasodilators, (e.g. nitroglycerin for coronary a.’s) -Beta-blockers – prevent CNS stimulation of heart -Ca2+ channel blockers – decrease contractility of heart - anti-hypertensives – ACE inhibitors (angiotensin converting enzyme – work via renal system), diuretics, cholesterol decreasing drugs, anticoagulates to prevent clots Arteriosclerosis – hardening, narrowing of arteries – fibrous tissue formation (tunica adventicia grows) constriction -caused by hypertension Atherosclerosis – plaque buildup in arteries, “atheromas” -coronary occlusion angina, MI -clot to brain TIA or stroke -clot in periphery can lead to aneurysm Cholesterol -HDL – mostly protein, little fat – carries lipids to liver for excretion -LDL – mostly fat, little protein – carries lipids to cells of body -largely responsible for atheroma formation Risk factors for cardiovasc problems – age, heredity, obesity, sedentary lifestyle, smoking, glycemic control, serum lipids Angina Pectoris – O2 low in heart muscle severe, crushing chest pain, “angere”= “to choke” Myocardial infarction – cell death from O2 deprivation replaced with fibrous tissue -majority occur in left ventricle Congestive Heart Failure -Forward effect – Not enough blood going out, pump FAILURE -Backward effect – CONGESTION of blood behind failing ventricle -One side fails first, ultimately leads to failure of other side -Decreased CO (cardiac output) one side compensation mechanisms – vasoconstriction, water & sodium retention, increased blood volume increased work for the heart -Eventually muscles of affected side weaken congestion behind affected side unaffected side pumps against increased resistance Previously unaffected side weakens Right side failure – systemic congestion Left side failure – pulmonary congestion -pericarditis effusion fibrous adhesions -myocarditis arrhythmias -endocarditis infection of heart valves can lead to fibrosis Dx tests for heart diseases -auscultation – listen to valves -exercise stress test -imaging -doppler blood flow -blood test – can detect enzymes release from infracted myocytes -EKG EKG – usually 12 leads – at least 3 The basics – -P wave – depolarization of atria -QRS complex – depolarization of ventricles -T wave – Repolarization of ventricles EKG Abnormalities -PAC –premature atrial contrx – slight flutter, benign -PVC – premature ventricular contrx – many times benign, can lead to ventricular fib (life threat) -atrial flutter – atria contract quickly, but in rhythm – P waves not always followed by QRS -atrial fibrillation – atria quiver ineffectually (can live without coordinated atrial contraction) -ventricular tachycardia -ventricular fibrillation – will die without swift intervention Heart block – problem with SA node communication with AV node -1st degree AV block – long PR interval – slow communication -2nd – Missing QRS after P wave -3rd – 2 consecutive missing QRS after P waves Auscultation -Sound 1 = tricuspid and mitral valves -Sound 2 = semilunar valves Nervous control of heart -medulla of brain stem – control center of heart -baroreceptors in aorta and internal carotid (peripheral a’s - stretch recepts for BP monitoring) -Autonomic system – increase and decrease HR Vasculature Artery layers -tunica intima –endothelial cells -endothelial cells respond to hormones, signal smooth muscle to contract, relax -tunica media – muscle cells -tunica externa (adventicia) – connective tissue Venous return – thinner walls, valves prevent backflow Hypertension -95% idiopathic -can cause endothelial cells to shear off -epinephrine in blood stream = inhibitory for endothelial cells, excitatory for smooth muscle underneath vasoconstriction and incr. BP -fat deposits in hole in intima atheroma -blood can begin running between tunica intima and media dissecting aneurysm Angiotensin Renin complex -angiotensinogen +renin -Angiotensin I +ACE (angiotensin converting enzyme) -Angiotensin II **ACTION = angiotensin II receptor vasoconstriction, incr. BP Aneurysms -fusiform – bulge in all directions -saccular – sac forms on one side – pooling of blood causing clotting thrombus formed -dissecting – most dangerous – blood runs between tunica intima and media – dissecting aortic aneurysm =ticking time bomb Circulatory shock – severe hypotension -causes = hypovolemic, cardiogenic, septic, distributive (vasogenic, neurogenic, anaphylactic) -compensations – SNS incr. HR, force of heart contraction; kidneys release renin, aldosterone, ADH Diff Dx Kawasaki’s Disease -antibod’s produced against endothelial cells and smooth mm -Presentation – red tongue, rash @ distal extremity, skin sloughing, edema -recovery usually spontaneous Raynaud’s Disease -insufficient blood supplied to distal phalanges – Women>men -prolonged ischemia can gangrene. Venous insufficiency -valves fail due to age, injury, sendentary life, obesity -chronic pooling of blood in LE -brown, blue, purple skin in feet and toes – waste accumulation! -minor trauma large wound! Hard to treat Lymphomas – cancer of T-cells and B-cells -Hodgkins – Tcell; Non-Hodgkins- B-cell -large lymph nodes and spleen -good prognosis if tx’d before metastasis Respiratory Disorders – Gould Ch. 19 How to Breathe – the basics -respiratory muscles contract & thoracic cage expands, creating negative pressure in lungs -air goes in -elastic fibers around alveoli passively contract -air goes out -Sympathetic activation smooth mm relaxation, bronchodilation -alveoli = squamous epithelium – maximizes gas exchange -covered with surfactant – reduce surface tension of fluid, prevent collapse -macrophages! -intrapleural pressure a shade under atmospheric pressure -feeling when you hold breath due to chemoreceptors for CO2. Hypercapnia – Increased CO2 in blood – compensate with hyperventilation Hypocapnia – decr. CO2 – compensate with hypoventilation Hyper/hypoxemia – O2 sats -As more O2 binds to hemoglobin, affinity for O2 rises – aids in acquisition and release of O2. Pneumonia -viral, bacterial, or fungal; 1 lobe or both lungs Tuberculosis -spread by oral droplet, can survive in dry sputum -TB takes root in primary infection stage, symptoms present in reinfection stage -can go dormant for long periods, bacilli walled off in localized area of lung - resurfaces when immune compromised -tissues of lung die in active infection -dx with skin test, chest x-ray, sputum culture -Long multidrug treatment, 6 mos- 1 yr. -grown more resistant to drugs in recent years. Obstructive Pulmonary Disorders – impaired ability to push air out of lungs -Cystic Fibrosis -Single gene mutation -increased mucus in the lungs, increased risk of infections -Lung Cancer -90% smoking related, 3rd most common cancer -can be result of metastasis -Lung Tumor -inflammation and bleeding in lungs cough blood -pleural effusion, pneumothorax -can secrete hormones –“paraneoplastic syndrome” -Asthma -Type 1 hypersensitivity – IgE formed in response to allergen -inflammation of mucosa bronchoconstriction, obstructive mucus -can cause atelectasis –collapse of lung because of airway blockage (-pneumothorax involves a collapsed lung caused by mechanical damage or a rupture of a small airsac or “bleb” on outside of lung) -presents with hypoxia, respiratory alkalosis (initially due to hyperventilation), cyanosis, cough, tightness in chest, thick mucus, tachycardia -treat with inhalers and glucocorticoids COPDs –progressive degeneration -Emphysema –“pink puffers” – red face, overinflation -destruction of alveolar walls permanent inflation -smoking eliminates anti-trypsin that inhibits enzyme that destroys elastin elastin of alveoli destroyedloss of septae between alveolar sacs decreased surface area for gas exchange -presents with “barrel chest” – ribs fixed in inspiration position -Chronic Bronchitis – “blue bloater” -inflammatory obstruction repeat infections, progressive, irreversible damage of bronchioles -hypertrophy, hyperplasia of mucus glands, fibrosis -Present with constant cough, SOB, cyanosis -treat by Stopping Smoking, O2 supplementation, available vaccinations for at risk infections Emphysema Chronic Bronchitis Alveoli affected Bronchioles affected Septae walls destroyed Increased secretions Some cough Lots of coughing Little sputum Lots of sputum No cyanosis Cyanosis Some infections Frequent infections -Bronchiectasis -permanent dilation of medium-to-large-sized bronchi -caused by recurrent inflammation Restrictive Pulmonary Disorders – impaired lung expansion -often abnormal chest wall or lung inself -Pneumoconiosis -exposure to irritants – coal workers -inflammationfibrosis, “stiff lung” - insidious onset -Vascular Disorders -Fluid collects in alveoli and interstitial fluid -lung expansion decr, O2 in blood decr, -leads to pulmonary hypertension and edema -Pulmonary embolism -blood clot from veins pumped to lungs – deadly -Atelectasis -collapse of lung caused by: obstructed airway, compression (tumor), increased surface tension preventing expansion -small areas asymptomatic, large areas –dyspnea and chest pain -Pleural effusion – “hydrothorax” -fluid in pleural cavity protiens and WBCs follow, respond to inflammation -Incr pressue in pleural cavity, layers separate, prevent expansion -presents with incr RR and HR, cyclic chest pain -Pneumothorax -air in chest cavity, lung collapse -open – air enters through hole in chest cavity; -closed – air in chest cavity from rupture on inside -tension – air allowed to enter cavity, no natural way to remove it -Adult Respiratory Distress Syndrome -rapid, shallow resp, incr HR, confusion -caused by shock, sepsis, burns, multiorgan failure Diff Dx - Sputum -yellow-green = infection -rusty-dark = pneumonia -purulent and foul odor = bronchiectasis -Breathing -labored breathing – obstruction -wheezing, whistling – obstruction of small airways -stridor – high crowing noise – obstruction of small airways Patho 4 Digestive Disorders Digestive System Overview 5 layers of gut wall (inner to outer): mucosa, submucosa, circular muscle layer, longitudinal muscle layer, serosa *Peristalsis (involuntary contractions) occurs in circular and longitudinal smooth muscle layers Stomach Gastrin cells (G cells): initiated by food entering stomach, stimulates chief and parietal cells Intrinsic factor (parietal cells): needed for absorption of vitamin B12 HCL (parietal cells): activates pepsinogen, creates optimal pH ~2, denatures proteins Pepsinogen (chief cells): pepsin not activated until pH of 6 Liver “Metabolic factory of the body” 1)Storage of nutrients 2) Maintains blood glucose 3) Blood reservoir 4) Produces bile, plasma proteins, blood clotting factors, cholesterol/lipoproteins 5) Metabolic processes (detoxification, conversions) Glucose -> Glycogen = Glycogenesis (when glycogen supply low) Protein, Fat -> Glycogen = Glyconeogenesis Glycogen -> Glucose = Glycogenolysis (maintains blood glucose levels) Pancreas Exocrine (secreting digestive enzymes and electrolytes) and endocrine organ Trypsin, chymotrypsin, carboxypeptidase-break proteins Ribonuclease-break nucleic acids Pancreatic amylase-break starch Lipase-break lipids GI tract Ileum=major site of nutrient absorption, villi (folds of mucosa) Large intestine=fluid and electrolyte reabsorption, movement slow to allow absorption of water, vitamin K synthesis (essential for blood clotting) Neural and hormonal control PNS (vagus mainly): increased motility and secretions, SNS: inhibits GI activity Gastrin: increases gastric motility and promotes stomach entering, Secretin: decreases gastric secretions, Cholecystokinin: inhibits gastric emptying Upper GI Tract Disorders (includes differential diagnosis) Disorder Dysphagia Description Difficulty swallowing Esophageal Cancer Squamous cells in distal esophagus, poor prognosis Hiatal hernia Part of stomach protrudes into thoracic cavity Gastric substances reflux into distal esophagus,often seen with hiatal hernia Stomach mucosa inflamed (either acute or chronic) *Helicobacter pylori infection typically present w/ chronic Inflammation of stomach AND intestine Erosion in mucosa Common in proximal duodenum and antrum of stomach (ulcers in general rarely found in large intestine) Gastroesophag eal Reflux Disease Gastritis Gastroenteritis Peptic Ulcers (gastric and duodenal) Stress Ulcers Rapid onset, may form within hours of precipitating event Gastric Cancer Primarily in mucous glands and in antrum or pyloric area, poor prognosis Narrowing and obstruction of pyloric sphinctor Pyloric Stenosis Causes 1) Neurological deficit 2) Muscular disorder 3) Mechanical obstruction -congenital atresia -stenosis -esophageal diverticulum -tumors Chronic irritation -chronic esophagitis -hiatal hernia Decreased competence of lower esophageal sphinctor Acute: Infection, allergies to food, spicy food, excessive alcohol, ulgerogenic drugs Chronic: Most idiopathic Usually an infection 1) H. pylori infection 1) Increased acid-pepsin secretions 2) Inadequate blood supply 3) Excessive glucocorticoid secretion 4) Ulcerogenic subtances Severe trauma: Burns (curling’s ulcers), head injury (cushing’s ulcers) Systemic: hemorrage, sepsis (ischemic ulcers) Gone down bc we have preservatives w/ food May be developmental anomaly or acquired later in life Liver and Pancreas Disorders (includes differential diagnosis) Gallbladder Disorders Cholelithiasis Cholecystitis Cholangitis Choledocholithiasis Description Formation of gallstones* Inflammation of gallbladder and cystic duct Inflammation related to infection of bile ducts Obstruction of biliary tract by gallstones (due to larger stones) *Risk factors for developing gallstones: Women (2x more likely), high cholesterol, obesity, multi parity (several children), use of oral contraceptives or estrogen supplements, hemolytic anemia, alcoholic cirrhosis Disorder Jaundice Description Yellowish color of skin (not disease itself but sign of other disorders) Prehapatic: unconjugated bilirubin elevated Intrahepatic: unconjugated and conjugated bilirubin elevated Posthepatic: conjugated bilirubin elevated Hepatitis Cirrhosis Inflammation of liver Mild: impaired hepatocyte function Severe: necrosis and obstruction of blood/bile flow along w/ impaired hepatocyte function Progressive destruction of liver Stage 1=fatty liver (asymptomatic & reversible) Stage 2= alcoholic hepatitis (irreversible) Stage 3=end stage cirrhosis (liver failure when 80-90% of liver destroyed) Liver Cancer Initial signs mild, diagnosis occurs with advanced stages Acute Pancreat itis Chronic or acute(medical emergency for acute) Spreads to tissue surrounding the pancreas Very painful (different than pancreatic cancer) Chronic in 15% of cases Pancreat ic cancer Adenocarcinoma-most common form Asymptomatic until advanced (metastasizes quickly) Mortality=95% Causes Prehepatic: excessive destruction of RBCs Intrahepatic: disease or damage to hepatocytes Posthepatic: obstruction of bile flow into gallbladder or duodenum 1) Idiopathic (fatty liver) 2) Infection (viral or non-viral)* 1) alcohol (most common) 2) biliary: obstruction of bile flow 3) post-necrotic: linked w/ chronic hepatitis or long-term toxic exposure 4) metabolic Hepatocellular carcinoma (most common primary tumor of liver) Secondary/metastatic cancer (arises from areas served by hepatic vein) Results from auto digestion of the tissue (Premature activation of pancreatic proenzymes) Precipitating factors=alcohol (most common), biliary tract obstruction, gallstones, mumps Risk factors=smoking, pancreatitis, and dietary factors *Viral Hepatitis Hepatitis A: Infectious hepatitis, RNA virus, transmitted by fecal-oral route in areas of inadequate sanitation, no carrier or chronic stage, vaccine available Hepatitis B: Serum hepatitis, DNA virus, incubation period of 2 months, primarily transmitted by infectious blood (may also be sexual transmission or from mother to fetus), carriers asymptomatic but contagious, vaccine available, chronic hepatitis B (ascites) =engorgement of blood vessels, can’t filter toxins anymore Hepatitis C: RNA virus, most common type transmitted by blood transfusion, has carrier state, increases risk of hepatocellular carcinoma Hepatitis D: Delta virus, incomplete RNA virus (needs hepatitis B to produce active infection), transmitted by blood Hepatitis E: RNA virus, transmitted by oral-fecal route, no chronic or carrier state Lower GI tract disorders (includes differential diagnosis) Disorder Celiac disease Description Malabsorption syndrome: prevents further digestion of gliadin (breakdown product of gluten) Atrophy of villi Primarily a childhood disorder Progressive inflammation and fibrosis cause obstructed areas Normally affects small intestines (but may affect any part of GI tract) Inflammation occurs in “skip lesions” Blood and mucous in stool Inflammation starts in rectum and progresses to colon Obstruction of appendiceal lumen, wall inflamed as fluid builds in appendix Occurs in 10% of population Symptoms=LRQ rebound tenderness, periumbilical pain Diverticulum=outpouching of mucosa through muscular layer of colon Diverticulosis=asymptomatic Diverticulitis=inflammation of diverticula (very painful) Symptoms=cramping, tenderness nausea, fever, elevated WBC, do NOT see blood in stool Early diagnosis essential Symptoms=alternating diarrhea and constipation, bleeding,weight loss, anemia, fatigue, red blood in stool, pain doesn’t often occur Most diagnosed cancer next to skin cancer Causes Autoimmune disease (1% of US population) -defect in intestinal enzyme Intestinal Obstruction Lack of movement of intestinal contents (most common in small intestine) Peritonitis Inflammation of peritoneal membranes Symptoms: sudden severe and generalized abdominal pain, abdominal distention, dehydration, low blood pressure,tachycardia, vomiting Mechanical obstruc. -tumors, adhesions, etc Functional obstruc. -impairment of peristalsis -Ex: spinal cord injury 1) Chemical peritonitis: caused by foreign chemical in peritoneal (bile, chyme, etc) 2) Bacterial peritonitis: direct trauma affecting intestines, ruptured appendix 1) Abdominal surgery (infection may develop) 2) Pelvic inflammatory disease in women Crohn’s disease (included in chronic Inflammatory Bowel Disease) Ulcerative Colitis (included in chronic IBD) Appendicitis Diverticular Disease Colorectal Cancer Genetic factor (often occurs during adolescence) Genetic factor (often occurs during 2nd or 3rd decade) Fecalith, gallstone, or foreign object cause obstruction May be genetic link Most from adenomatous polyps (polyp does not always mean cancer!) Risk factors: familial multiple polyps, long-term ulcerative colitis, diet low in fiber (why susceptibility has increased) Irritable Bowel Syndrome 1) Change in bowel motility that is associated with pain 2) Must be there 12 weeks out of the year 3) Do NOT see blood in stool Urinary Disorders Urinary System Overview Kidney Nephron=functional unit of the kidney (>1 million), consists of renal corpuscle (filtration unit) and renal tubule ADH-prevents water loss (increases reabsorption of water in distal convoluted tubules and collect. duct) Aldosterone-prevents water loss (increases sodium reabsorption in distal convoluted tubules) ANP-allows water loss in response to high blood pressure Glomerular rate: 1)afferent arteriole dilation=increased filtrate 2) efferent arteriole constriction=increased filtrate 3) afferent arteriole constriction=decreased filtrate Renin (kidney) ↓ ACE (lung) ↓ Angiotensinogen → Angiotensin I → Angiotensin II (plasma) vasoconstrictor (Renin secreted in response to reduced afferent arteriole blood flow) Urinalysis Cloudy-presence of large amounts of protein, blood, bacteria, and pus Blood: if large amount=increased glomerular permeability or hemorrhage, if small amount=infection, inflammation or tumors in urinary tract Dark color-hematuria, excessive bilirubin, highly concentrated urine Unusual smell or odor-infection, diet, or medication Elevated BUN and creatine=failure to excrete nitrogen waste Metabolic acidosis (low pH, low bicarbonate)=failure of tubules to control acid/base balance Urinary System Disorders (includes differential diagnosis) Disorder Urinary Tract Infection Description Lower=cystitis and urethritis (hyperactive bladder and reduced capacity), may have systemic signs w/ painful urination Upper=pyelonephritis (in one or both kidneys: purulent exudate and abscess block blood and urine flow), Cause E.coli Predisposing factors=incontinence, retention of urine, direct contact w/ fecal material Glomerulonephritis Nephrotic Syndrome Bladder cancer Vascular Disorders Adult Polycystic kidney disease Polycystic disease in children Acute Renal Failure Chronic Renal Failure Kidney Stones Wilms Tumor Diabetic Neuropathy Reflux Neuropathy Incontinence systemic sign of high fever *can lead to renal failure* Decreased GFR rate (decreased urine output, elevated blood pressure and edema) Metabolic acidosis Bloody, foamy urine and pain Increased permeability in glomerular capillaries Hypoalbuminemia,increased aldosetrone, severe edema Often develops as multiple tumors Early signs:hematuria and dysuria Thickening/hardening of walls and small arteries Reduces blood to kidney-stimulation of renin (increases blood pressure) Manifests around 40 Multiple cysts in both kidneys-leads to chronic renal failure Manifested at birth, child dies in first month or is stillborn Rapid onset Metabolic acidosis and hyperkalemia Ogliuria, increased serum urea Gradual, irreversible destruction of kidneys (<10%=end stage) Asymptomatic w/ up to 40% left Symptoms later on=polyuria with dilute urine, anemia, fatigue Axotemia=renal insufficiency<25% Calcium (sharp),magneisum, uric acid, cystine 1-5mm can be passed Usually unilateral and gives purely kidney symptoms Leading cause of chronic renal failure 1/3 ppl on dialysis have Type 1 diabetes, 2/3 have Type 2 Flow of urine from bladder to upper tract Can lead to end stage renal disease 1)Stress: most common Ex:sneeze Acute poststreptococcal glomerulonephritis caused by presence of anti-streptococcal antibodies Predisposing factors: working w/ chemicals (analine dyes, rubber, aluminum), smoking, recurrent infections, heavy analgesics intake Some normal w/ aging Autosomal dominant gene on chromosome 16 Autosomal recessive mutation 1) Acute bilateral kidney diseases 1) Prolonged/severe circulatory shock or heart failure 2) Nephrotoxins 3) Mechanical obstruction 4) Burns 1) Chronic kidney disease 2) Polycystic disease 3) Systemic disorders 4) Low-level nephrotoxin exposure over long time Most common tumor in children, defects in tumorsuppressor on chromosome 11 Primary (congenital) Secondary (obstruction) Associated with hypertension Associated w/ aging, most 2)Urge: spasm 3)Overflow: can’t fully empty bladder 4)Functional: bladder normal, something else keeps them from going to bathroom Ex: spinal cord injury common in women Dialysis-provides filtration and reabsorption (hemodialysis=blood moves from shunt into machine, 3x per week for 4 hours)(Peritonal dialysis= peritoneal membrane serves as semipermiable membrane, usually done at home during night) Endocrine System Differential Diagnosis Gigantism Acromagly- thicker skull and jaw (occurs after joint plates fuse) Hyperthyroidism Common cause=Grave’s disease Common symptoms=exopthalmos, goiter, heat intolerance, and anxiety Hypothyroidism Very familial, 4X more likely in women Common symptoms=weight gain, cold intolerance, fatigue Myxedema- lots of fluid (would not pit), can look like fibromyalgia bc of muscle aches and trigger point tenderness, sparse hair, brittle nails, may have buffalo hump Thyroid storm-dumps T3 and T4 into system -> causes tachycardia, fever, and agitation Thyroid cancer Very treatable, most are benign (only 5% malignant and they normally dont metastasize) Palpation will be painless, unilateral, and in one spot Parathyroid glands Maintain calcium levels between bone and blood Parathyroid cancer=can’t easily be distinguished from thyroid cancer Renal glands Release epinephrine and aldosterone Trousseau’s sign- positive sign would be tremors and twitching bc of nerve or muscle irritability (Non specific sign) Chvostek’s sign-elicit this by having the patient relax face and then the therapist taps the facial nerve, watch for twitch of mouth or side of face Addison’s Diseases (hypoadrenal)- autoimmune, skin changes color to a slight grey Cushing’s Syndrome (hyperadrenal)- too much glucocorticoids in system, can cause muscle wasting, bone demineralization, and ligaments to be lax, might see buffalo hump on back (does NOT feel like fluid) Diabetes (fasting plasma glucose >126mg/dL) Action of insulin-when insulin gets to cell, it makes glucose transporters close to membrane (Below 100 mg/dL is normal for FPG) Type 1=autoimmune (insulin producing B cell destruction), typically under age 20 Risk factors: sibling has Type 1, parents have type 1 Type 2=obesity (insulin resistance...receptor not binding to insulin as well, pancreas intact), hyperglycemia develops slowly, may have genetic predisposition, 85-90% of all diabetes Risk factors: overweight, over 45 yrs old, inactive, women who had a baby over 9ilbs, low HDL Gestational=associated with type 2, glucose intolerance w/ pregnancy, increased risk of diabetes later on, if continues >6 weeks after pregnancy...no longer GDM Acute Hyperglycemia Early signs: blood sugar >180mg/dL, blurred vision, thirsty, ketones,dry skin, increased urination, tired Late signs: blood sugar >240mg/dL, nausea/vomiting, deep/rapid breathing, large ketones in urine, fruity breath, some diabetes pts don’t sense changes bc of neuropathy Acute Hypoglycemia Caused by: over treatment w/ insulin, missed meal, exercising when insulin peaking, stress Early signs: tachycardia, hunger, headache, dizziness, sweating, shaking, pale skin, tingling around mouth, Late signs: slurred speech, confusion, sudden moodiness, clumsy or jerky movements, seizures, pass out Treatment: Act quickly! Test blood sugar after attempting to raise it with 15 grams of fast acting sugar...if <70 repeat, if >70 eat meal/snack (always assume they will drop 50 mg/dL while exercising) Obesity **Nursing/Allied health professions have greater risk of injury due to rising obesity trends** Underweight = <18.5 Normal weight = 18.5-24.9 Overweight = 25-29.9 Obesity = BMI of 30 or greater Subcutaneous vs. Intra-abdominal fat Subcutaneous fat needed for thermal control Abdominal obesity=most important factor in determining pre-diabetic state (1 out of 5 US adults have metabolic syndrome), want to avoid fat around organs (especially liver) Hormone regulation Fat=largest/most active endocrine organ, releases 50 hormones, Adiponectin=hormone that signals brain we are full (as fat cell gets bigger, releases less of this) More macrophages recruited with obesity, causing chronic inflammation Lifestyle=big factor (obesity trends with US Pima Indians vs Mexican Pima Indians) Epigenetics= We can change which genes we turn on and off by our activitity Pathophysiology Exam 5 Review Acute Neurologic Disorders Neurons and Conduction of Impulses Neurons: highly specialized, non-mitotic cells which conduct impulses through the CNS and PNS Myelin sheath: insulates, speeds up conduction, formed by Schwann cells, Nodes of Ranvier Glial cells: astroglia, oligodendroglia, microglia, ependymal cells Regeneration of Neurons: neuronal cell body damaged = death of neuron; CNS = neurons do NOT regenerate; PNS = neurons may be able to Conduction of impulses: depolarization (sodium influx) generation of action potential repolarization (outward movement of potassium) sodium – potassium pump moves ions into their normal position; myelinated fibers: salutatory conduction = rapid conduction Chemical neurotransmitters: stimulated released into synaptic cleft; inactivated by enzymes or reuptake; postsynaptic neuron dendrites or cells body depolarizes depending on neurotransmitters Neurotransmitters: o Acetylcholine: (excitatory and inhibitory) located: neuromuscular junction, autonomic nervous system (SNS and PNS), peripheral nervous system, CNS o Catecholamines: (excitatory) present in the brain, norepinephrine: neuromuscular junction and SNS, epinephrine: SNS, dopamine o Seratonin: (excitatory) located in the CNS (brain) and GI; regulates behavior, attention, digestive processes; implicated in mood changes o Glutamate: (excitatory) o Y-Aminobutyric acid (GABA): (inhibitory) located in brain Autonomic Nervous System: o Involuntary, motor and sensory innervation: cardiac muscle, smooth muscle, glands, sympathetic/parasympathetic, neural pathway: preganglionic fibers (in brain or spinal cord) postganglionic fibers (outside CNS) Sympathetic Nervous System: o “Fight or flight”; stress response, increase general level of activity: cardio, respiratory, neurologic, Neurotransmitters: preganglionic fibers release acetylcholine (cholinergic); postganglionic fibers release norepinephrine (adrenergic) Parasympathetic Nervous System: o Dominates digestive system, aids recovery after sympathetic activity, vagus N: innervates heart and GI, neurotransmitter: acetylcholine; receptors (cholinergic): nicotinic and muscarinic Acute Neurologic Disorders Problem/Disorder Description Treatment Increased Intracranial Pressure Expansion of fluids/tissue Increase in pressure Ischemia and infarction Herniation Displacement of brain tissue Brain Tumors Vascular Disorders Transient Ischemic Attacks Cerebrovascular Accidents Cerebral Aneurysms Meningitis Brain Abscess Encephalitis Rabies Tetanus Poliomylitis Herpes – Zoster (shingles) Post-polio syndrome Reye Syndrome Guillain – Barre syndrome caused by large mass (clot/tumor) Lesions that cause increased ICP Hemorrahagic (increased ICP) or ischemic Temporary reduction of blood flow in the brain Small mini-strokes occurring continually Connected to dementia Infarction of the brain due to lack of blood Localized dilation in the wall of an artery Bacterial infection of the meninges of the CNS Localized infection; necrosis of tissue Infection of the parenchymal or conn tissue in the brain and spinal cord Viral transmitted by bite of rabid animal or transplantation of contaminated tissues Infection by puncture wound Polio virus; attacks motor neurons of the spinal cord and medulla Caused by varicella – zoster in adults Occurs 10 – 40 years after initial infection Viral infection linked to children treated with aspirin Inflammatory condition of the PNS If accessible then removal Clot busting agents, surgery, glucocorticoids, team approach Surgery before rupture, antihypertensive drugs Antimicrobial therapy, glucocorticoids, vaccines Surgical drainage, antimicrobial therapy Antimicrobial therapy, antiviral drugs (depends on the type of encephalitis) Prophylactic immunization Immunizations advised Immunization available Vaccine available for ages 60+ No immediate cure Recovery usually spontaneous; supportive treatment Chronic Neurologic Disorders Problem/Disorder Hydrocephalus Spina Bifida Description Excess CSF within the skull Non-communicating (flow of CSF through ventricular system is blocked) Communicating: absorption of CSF through subarachnoid villi impaired Failure of the posterior Treatment Diagnostic Tests: alpha – spinous processes to fuse meninges and spinal cord herniated Cerebral Palsy Multiple Sclerosis (MS) Parkinson’s Disease Amyotrophic Lateral Sclerosis fetoprotein (AFP) elevated, ultrasound Surgical repair, OT/PT afterwards Motor impairment due to brain Speech, PT/OT, assistive damage: intellectual function, devices, monitor behavior, communication / hearing/vision, alternate speech, seizures, visual or modes of communication hearing deficits Causes: genetic mutations, abnormal fetal formation, brain damage, difficult delivery, hypoxia (ischemia) Spastic paralysis: hyperreflexia Dyskinetic: loss of coordination with fine movement Ataxic: loss of balance and coordination Progressive demyelination of MRI for diagnosis and neurons in brain, spinal cord, monitoring and cranial nerves Research treatments: Cause: unknown interferon beta – 1b, S&S: blurred vision, diplopia, glucocorticoids scotoma, weakness in legs, PT/OT progressive weakness and Muscle relaxants paralysis, paresthesia, dysarthria, loss of coordination, bladder / bowel / sexual dysfunction, chronic fatigue Progressive degeneration in Removal of cause if known basal nuclei; imbalance Dopamine replacement between excitation and therapy inhibition Anticholinergic drugs Excess stimulation affects Speech/language, PT/OT movement and posture Treatment of respiratory or S&S: resting tremors (“pill urinary tract infections rolling”), muscular rigidity, difficulty initiating movement, postural instability, decreased flexibility, fatigue, lack of facial expressions, propulsive gait, bradykinesia Muscle wasting, progressive Stem cell therapy under (ALS) Myasthenia Gravis (MG) Huntington’s Disease Dementia Alzheimer’s Disease degenerative disease affecting motor neurons Cause: unknown Cognition, sensory neurons, neurons of eye are unaffected Loss of upper motor neurons: spastic paralysis and hyperreflexia Loss of lower motor neurons: Flaccid paralysis, decreased muscle tone and reflexes Autoimmune disorder: autoantibodies to acetylcholine receptors at NMJ S&S: muscle weakness in face/eyes, weakness in arms/trunk, impaired vision and speech, difficulty chewing and swallowing, head droops, upper respiratory infections Rapid, jerky movements, chronic progressive neurodegenerative chorea, hereditary, autosomal dominant (~40 years of age) Progressive atrophy of brain S&S: mood swings, personality changes, restlessness, choreiform movements in arms and face, intellectual impairments Intellectual deterioration that interferes with occupational or social function S&S: impaired cognitive skills, impaired thinking, judgment, and learning, memory loss, confusion, behavioral and personality changes Causes: vascular disease, infections, toxins, genetic disorders Progressive cortical atrophy: neurofibrillary tangles and amyloid plaques investigation Moderate exercise and rest Electronic communication devices Team approach No specific treatment to slow degeneration Diagnostic tests: EMG, serum antibody test, acetylcholine esterase inhibitor Treatment: antiacetylcholine esterase agents, gludocorticoids, plasmaphoresis, thymectomy Diagnositc test: DNA analysis Treatment: no therapy to slow progress, only symptomatic therapy 1st stage: short term memory loss, social withdrawal, no sense of humor Creutzfeld – Jacob Disease (Mad Cow Disease) AIDS Dementia Cause: unknown S&S: onset insidious, behavioral changes (irritability, hostility, mood swings), gradual loss of memory and lack of concentration, impaired learning, poor judgment, decline in cognitive function, memory and language, change in food intake, inability to recognize family, environment unawareness, incontinence 2nd stage: general confused stage, wandering (sundown syndrome) 3rd stage: terminal stage, incontinent, apathetic, institutionalized No diagnostic tests available Treatment: anti-acetylcholine esterase drugs, OT/PT, psychologists, speech therapists, team approach Rapidly progressive Cause: prion ingested or transmitted through contaminated blood S&S: memory loss, behavioral changes, motor dysfunction, progressive disorders, dementia Common in later stages of AIDS, virus invades brain tissue Gradual loss of memory and cognitive ability, impaired motor function Diagnosis: blood tests Fatal: within 6 months = dead Complex Regional Pain Syndrome (CRPS) Pathogenesis: abnormal activity of the SNS, gate control theory, reflexive muscle spasm Stages of CRPS: o Stage 1 (acute): right after injury, weeks to 3 mo., excess sympathetic activity, persistent burning pain and swelling, hyperesthetic, hyperhidrosis, increased nail/hair growth, pain will be severe o Stage 2: dystrophic stage, 3 – 6 mo., persistent pain and stiffness, trophic skin changes, muscle atrophy, flexion contractures, pain exacerbated by stimulus, limb: edematous, cool, cyanotic, mottled, hair loss, cracked brittle nails, skin cool to touch o Stage 3: atrophic stage, ~6 mo., pain can increase or decrease, progressive atrophy of skin, subcutaneous tissue, muscle, and bone, bone demineralization, skin: cool, thin and shiny o Stage 4: existence of stage 4 is questionable, 2+ years, psychosocial level, swelling is gone, atrophy is permanent (muscle, bone, skin), no NOC firing now Definite CRPS: pain and tenderness in extremity, S&S of vasomotor instability, swelling, dystrophic skin changes Probable CRPS: pain and tenderness OR swelling, dystrophic skin changes often present Possible CRPS: vasomotor instability AND/OR swelling, NO pain but tenderness, dystrophic skin changes occasional Doubtful CRPS: unexplained pain and tenderness in an extremity PAIN How we interpret pain: NOC perception interpretation emotions social Pain: the perception of nociception that is not directly measurable Pain behavior: the observed consequence of a painful experience (distress response); Pain behaviors: verbal, vocal, facial expressions, physical actions, function, social actions Benign pain: not associated with terminal illness vs. Malignant: associated with terminal disease Acute Pain Chronic Pain Recent onset (<3 mo.) >3 mo. Close link with pain generator Loose link with pain generator Not a learned response even though there will be Learned behavior, positive reinforcement for pain pain behavior behavior Objective findings coincide with generator No lab or clinical findings to support pain Unlikely to have errors in stimulus discrimination Pt. may confuse pain with other forms of distressful stimuli Brief in nature lengthy Differential Diagnosis of Chronic Pain Test Wadell’s Signs Mankopf’s Test O’ Donoghue’s Maneuver McBride’s Test Hoover’s Test Description Distracted SLR, rotation of back, superficial tenderness, regional pain, migrating trigger points, sham axial loading of spine, regional weakness Pain should raise pulse rate of person by 5% + AROM > PROM = + sign Stand on one leg and raise other leg to chest = should decrease LBP Supine, hold pt.’s heels off table and have them raise one leg, feel downward pressure if they try to lift the leg Symptom magnifier: magnifying their symptoms vs. Malingerer: knowingly manipulating the system for their own gain, purposely deceiving the health care providers Look at pt’s work history SEIZURES Review types of seizure table Seizure: abnormal discharge of a group of cortical or subcortical neurons Epilepsy: syndrome characterized by experience of recurrent seizures Aura: subjective sensation or motor phenomenon that precedes a seizure (pre-ictal/prodomal) Ictal period: period of abnormal EEG activity; seizure S&S are evident Post-ictal period: period following acute seizure, time of confusion, EEG activity = normal Status epilepticus: series of rapidly repeated epileptic convulsions without any period of consciousness between them Seizures Epilepsy Inappropriate electrical activity Recurrent seizures or neurological syndrome associated with seizures Transient neurological signs (seizure) Seizures occurring with little or no provocation Altered consciousness, involuntary movements, Individual or multiple seizure types; characteristics and disturbed perception often occur may change with age Defined by neurological S&S and EEG patterns Spectrum of seizure types, EEG, clinical settings Etiology: genetic (inherited metabolic abnormalities, lowered threshold to electrical activity of the brain), structural (disturbed cerebral flow, disorders of blood composition), environmental (anoxia, toxins, drug withdrawal), head trauma, idiopathic causes Triggering mechanisms: visually induced, movement induced, hyperventilation, trauma, emotions, hydration/electrolyte imbalance, fever, alcohol or drug withdrawal, premenstrual period, lack of sleep, illness Diagnosis: medical history, diagnostic tests (lab studies, x-rays, lumbar puncture, CT, MRI, EEG), clinical observation Treatment: drugs, surgery, diet, microcomputers, education Differentiate from: disorders of cerebral blood flow or blood constitution, structural, psychiatric conditions, and migraine headaches Mental Health Disorders of Children Autism Spectrum Disorder Autistic disorder, pervasive developmental disorder, and Asperger’s disorder: differ in when the symptoms start, how fast they appear, and severity Cause is unknown; genetic and environmental factors; structural brain abnormalities: larger total brain mass, smaller frontal cortex, abnormal cerebellum S&S: lack of social skills, avoid eye contact and physical contact, echolalia, don’t listen, aggressive or passive (may switch), inflict self injury, resistant to change, diff in expressing needs, tantrums Early indications: no babbling or pointing, no single words, no response to name, loss of language or social skills, poor eye contact, excessive lining of objects, no social responsiveness Later indicators: impaired ability to make friends or initiate conversation, impaired play, echolalia, preoccupation with objects, inflexible adherence to routines and rituals Screening tests: Childhood Autism Rating Scale (CARS), Checklist for Autism in Toddlers (CHAT), Autism screening questionnaire, screening test for autism in 2 year olds Treatment: intensive behavior therapy Attention Deficit Hyperactivity Disorder (ADHD) Inability to focus on one thing in all aspects of life impairing function; diagnosis (must have all 3): inattention, hyperactivity, and impulsivity Tourettes Syndrome Characterized by tics; tics: involuntary, rapid, repetitive, and stereotyped movements of individual muscle groups Transient tic disorder: do not persist for more than 1 year vs. chronic tic disorder: duration over many years (unchanging character) vs. chronic multiple tics: several chronic motor tics vs. Tourettes: multiform frequently changing motor and phonic tics, unknown cause Bipolar Disease Combination of euphoria and depression; in kids: continuous, rapid-cycling, irritable, and mixed symptom state that may co-occur with disruptive behavior disorders School Refusal/Avoidance Refuse to go to school on a regular basis or problem staying in school once there Separation Anxiety Disorder Extreme anxiety when away from home or separated from parents Selective Mutism Fail to speak in situation where speech is expected or necessary Oppositional Defiant Disorder (ODD) Persistent / consistent pattern of defiance, disobedience, and hostility towards authority figures Conduct Disorder Fighting, bullying, intimidating, physically assaulting, sexually coercing, cruel to people and animals, vandalism, theft, truancy, drug and alcohol abuse, precocious sexual activity Adult Mental Health Disorders Dementia, Alzheimer’s, Vascular Dementia (TIAs), Creutzfeld – Jakob, Huntington’s refer to table General Anxiety Disorder Excessive worry for 6+ mo., focus of worry will shift between things Obsessive-Compulsive Disorder (OCD) Persistent, recurring thoughts and obsessions, obsessive behavior with repeated behavios Panic Disorder 3 types of attacks: unexpected, situational, and situationally predisposed Post Traumatic Stress Disorder Follows exposure to a traumatic event; 3 symptoms: relive the disaster, avoidance behavior, emotional detachment from others Social Anxiety Disorder Extreme anxiety about being judged by others or being embarrassed, cause avoidance behavior Specific Phobias Fear is at a level that is inappropriate and recognized as irrational Major Depression Combination of symptoms that interfere with work, sleeping, eating, and social activities Dysthymia Less severe form of depression, chronic, doesn’t interfere with everyday activities Bipolar Disorder Cyclic mood swings with mania and depression Paranoid Personality Disorder Continual mistrust, view everyone as an enemy, hypersensitive, defensive and antagonistic Delusional Paranoid Disorder Persistent non-bizarre delusions without symptoms of any other mental disorder, delusions of being persecuted Schizophrenia Extremely bizarre delusions or hallucinations; hear voices or believe thoughts are controlled Antisocial Personality Disorder Long-standing pattern of a disregard for other people’s rights, can only be diagnosed in ages 18+ Avoidant Personality Disorder Long-standing & complex pattern of feelings of inadequacy, extreme sensitivity, social inhibition Borderline Personality Disorder Labile interpersonal relationships characterized by instability, shallow, impulsive behaviors Narcissistic Personality Disorder Pervasive pattern of grandiosity, need for admiration, lack of empathy Schizoid Personality Disorder Detachment from social relationships and a restricted range of expression of emotion in interpersonal settings Musculoskeletal Disorders Bones classified by shape: long, short, blat, irregular Bone tissue: intercellular matrix (fibers, calcium phosphate, strong/rigid structure) and cells -cytes (mature cells), -blasts (producing cells), -clasts (resorption cells) Bone remodeling: regulated by stress (weight bearing, mm tension) & hormones (growth, PTH) Osteoblasts: make collagen/proteins of matrix; osteoclasts: secrete collagenase/degrading enzymes (regulated by PTH) Bone tissue: compact: outer covering of bone; cancellous (spongy) interior of bone Periosteum: fibrous conn tissue cover over bone; endosteum: osteoblast rich lining of medullary cavity Functions: body movement, body position, stabilize joints, maintain body temp. Skeletal Muscle: bundles of protein fibers covered by conn tissue, striated, voluntary, respiration: aerobic and anaerobic, glycogen for energy Joints: synarthroses (immovable), amphiarthroses (slightly moveable), diarthroses (freely moving) Disorder Description Treatment Fracture Bleeding, local inflammation, necrosis of tissue at the end of the broken bone Osteoporosis Decrease in bone mass and Dietary supplements (calcium, density, loss of bone matrix and vitamin D), weight bearing mineralization activities, PT, fluoride, Predisposing factors: 50+ yrs., bisphosphonates, calcitonin sedentary, hormonal, low BMI, diet, Asian/European ancestry Rickets and Osteomalacia Paget’s Disease Tumors Muscular Dystrophy (MD) Osteoarthritis (OA) Rheumatoid Arthritis Gout Deficit of vitamin D and phosphates, kids = weak bones, adults = soft bones Excessive bone destruction with replacement by fibrous tissue and abnormal bone Common site of secondary tumors, majority of primary tumors are malignant Osteosarcoma: bone pain at rest Chondrosarcoma: cartilage cells (adults) Ewing’s sarcoma: shaft of long bones (adolescents) Autosomal recessive disorders, degeneration of skeletal mm, Duchenne MD most common (boys): deficit of dystrophin, skeletal mm replaced by fat and fibrous conn tissue Degenerative, “wear and tear”, result of increased weight bearing or lifting, articular cartilage damage, surface = rough and worn, bone spurs, narrow joint space, inflammation, lack of ROM, pain, predisposition of falls Autoimmune, chronic systemic inflammatory, rheumatoid factor (RF), synovitis, red, swollen, painful jt., pannus formation, cartilage erosion, fibrosis, ankylosis, atrophy of mm., muscle spasms, contractures, bilateral joint involvement, jt. Becomes fixed and deformed, systemic: fatigue, anorexia, mild fever, generalized aching Unknown cause Deposits of uric acid and crystals in jt. Causing local inflammation, affects single jt. (hallux), redness, swelling, pain Excision of tumor if possible Surgical amputation Chemotherapy Diagnostic tests: ID genetic abnormalities, elevated creatine kinase levels, EMG, muscle biopsy, blood test Treatment: no curative treatment, moderate exercise, assistive devices, PT/OT, massage, ventilator Treatment: assistive devices, mild exercise program, orthotics, massage therapy, PT/OT, acupuncture, glucosaminechondroitin suppletments, injection of synthetic synovial fluid, NSAIDS, analgesics, arthrotomy, jt. replacement Treatment: rest/moderate activity, heat/cold, NSAIDS, glucocorticoids, analgesics, surgery, Drugs Diagnosis: examination of synovial fluid and blood tests Treatment: reduce uric acid levels by drugs and dietary changes Ankylosing Spondylitis Joint fixation, inflammation of a spinal joint, SI and costovertebral joints and intervertebral spaces of axial skeleton, fibrosis and calcification of jts., S&S: LBP, pain when supine, rigid spine; systemic: fatigue, fever, weight loss, iritis Treatment: relieve pain and maintenance of mobility: antiinflammatory drugs, analgesics, daily exercise, PT/OT Patho Test 6 Review Skin- body’s largest organ *Thickest on scalp, palms soles and back (1.4 to 4mm) *Function:barrier, temp regulation, secretion/excretion, vita D production, immunologic, sensation Burns: Superficial burn- epidermis only Partial thickness- papillary layer of dermis Deep partial- damage to reticular layer of dermis Full thickness- entire thickness to subcutaneous tissue Subdermal- beyond skin to bone, fat of muscle Histological Assesment of burn wound: Zone of coagulation (necrosis) Zone of stasis (injury) Zone of hyperemia Epidermal healing Begin in 24-48 hours after burn Epithelial cells detach from basale layer and migrate toward wound, proliferate by mitosis and differentiate into mature epidermal cells Contact guidance and contact inhibition Dermal healing Inflammatory phase Hemostatic events Vascular events Cellular events Fibroplastic stage Fibroblasts Ground substance Tensile strength Collagen synthesis Granulation tissue Wound contraction Maturation phase Hypertrophic scar Keloid Rule of nines: front of leg, front upper torso, front lower torso, entire head, entire arm, each are 9% of body when estimating burn coverage. (Genital area 1%) Treatment of burns: Silicone pressure garments Grafts Allograft, xenograft, cultured skin, dermal substitutes, synthetic skin Splints ***Never put legs in dependent position without compression. Initially don’t move graft site! Ambulation guided by physician. Dermis: made of connective tissue (flexible/ strong), contains nerves(sensory receptors) and blood vessels. Skin accessory structures: hair follicles, sebaceous glands, sweat glands, nails. Subcutanous tissue: below skin includes connective tissue, fat cells, macrophages, fibroblasts, large blood vessels and nerves. Inflammatory Disorders Contact dermatitis: exposure to allergen (soap), sensitization on first exposure. Chemical irritation: doesn’t involve immune response. Urticara (Hives): Type 1 hypersensitivity. Ingestion of substance (shellfish). Lesion pruritic, part of anaphylaxis (check airway for breathing). Atopic dermatitis (eczema)- inherited allergy, moist pruritic rash on face/chest in infants. Dry, scaly in adults. Type 1 hypersensitivity. Treatment: glucocorticoids Psoriasis- chronic inflam. skin disorder, abnormal T- cell activation, excess keratinocytes. Lesions on face scalp elbow and knees. Treatment: gluco. Anti-metabolites, UV light Scleroderma: systemic skin disorder, increased collagen/ inflam. Shiny tight hard areas of skin. May lead to renal failure, intestinal obstruction, respiratory failure. Keratoses: Benign lesion assoc. w/ aging/ skin damage. Seborrheic keratoses- proliferation of basal cells, painless, round, dark, elevated Actinic keratoses- on UV exposed skin, common in fair skinned, looks scaly and may develop into squamous cell carcinoma. Squamous cell carcinoma- painless, malignant tumor of epidermis. From sun, smoking. Slow growing. Good prognosis with early removal. Malignant melanoma: highly metastic skin cancer, multicolored w/ irregular border, grows quickly and changes in appearance. ABC’s of melanoma: increase in Area. Change in Border. Change in Color. Increase in Diameter. Karposi’s sarcoma- occurs in AIDS and other immunocompromised pt.s Purple skin spots. Senescence: biological processes that lead to aging, begins prior to birth. Also the period from onset of old age to death. Cardio changes w/ aging: size/ # of cardiac muscle fibers decrease. Fatty tissue and collagen accumulate. Reduced strength in contraction. Heart valve thickens, less flexible. Less oxygen to heart, cardiac reserve diminished. Arteriosclerosis: loss of elasticity, accumulation of collagen, thickening of arteries Atherosclerosis- hyperlipidemia, accumulation of cholesterol. Common cause of heart attack. Osteoarthritis: degeneration of cartilage in joints. Associated with sports injury Neuro changes with aging: reduction in neurons, lipid accumulation in neurons, loss of myelin, slower response time. Vision changes with aging: lens less flexible, yellow, night/ color vision reduced. Falls account for 70% of all deaths in those over 75. 90% of hip fractures due to fall. Fall intervention: exercise, decrease meds, pressure stockings, gait training, balance exe. Geriatric physical exam should include: Up and Go Test, Tinetti gait and balance test. Reproductive System Menstrual abnormalities Amenorrhea: no menstruation Dysmenorrhea: painful menstruation due to excess release of prostaglandins. PMS Abnormal bleeding: Menorrhagia: increase flow Metrorrhagia: bleeding btwn cycles Polymenorrhea: short cycles less than 3 wks Oligomenorrhea: long cycle more than 6 wks. Endometriosis: endometrial tissue occurs outside uterus. Bleeding/ pain Candidiasis: not sexually transmitted. Caused by fungus. Opportunistic infection by normal flora of vagina. White curdlike discharge. Antifungal treatment. Pelvic Inflammatory disease: infection of uterus, fallopian tubes or ovaries. Originates from lower reproductive tract. Arises from STD, non sterile abortion or postpartum. Potential complications: peritonitis, pelvic abcesses, septic shock. Signs: pain, high temp, guarding, nausea, leukocytosis, purulent discharge. Rx: antibiotic therapy in hospital. Leiomyoma: benign tumor of myometrium, well defined encapsulated masses. Surgery or hormonal therapy for treatment. Ovarian cysts: last 8-12 wks. Multiple small fluid filled sacs requiring surgical removal if bleeding is present. ID with ultrasound. Polycystic ovarian disease: fibrous capsule thickens around follicles of ovary. Hereditary, absence of ovulation and infertility. Hormonal imbalance, amenorrhea, hirstuism. Rx: surgical wedge resection of pharmacology. Fibrocyctic breast disease: cyclic occurrence of nodules or masses in breast tissue Carcinoma of breast: increase after age 20, usually unilateral, metastasis via lymph nodes. Predisposing factors: family hx, BRACA gene, late 1st pregnancy, sedentary lifestyle, smoking, high fat diet. Cervical cancer: usually due to HPV, Pap Smear can ID early. Carcinoma of uterus: vaginal bleeding early sign. Risk factors: over 50 y.o., high dose estrogen without progesterone, obesity, diabetes. Pap smear down not detect. Slow growing but invasive. Ovarian Cancer: no reliable screening, detected by pelvic exam. Risk factors: BRACA gene, early menarche, obesity, late first pregnancy, fertility drugs. Oral contraceptives are protective. Pregnancy terminology: number of term infants, pre- term, abortions, kids currently alive (3-0-03) Avoid modalities on pregnant women. Ectopic pregnancy: implantation outside the uterus Prostatitis: inflammation of prostate. Acute bacterial: gland swollen, tender, bacteria in urine. Non-bacterial: urine has leukocytes Chronic bacterial- gland slightly enlarged, dysuria, frequency/ urgency. Bacterial infection- from e-coli Occurs in: young men w UTI’s, old men w/ prostatic hypertrophy, w/ STD’s, through a catheter and bacteria. Signs: low back pain, decrease urinary stream, muscle aches, anorexia, fever etc. Benign prostatic hypertrophy: signs- obstructed urinary flow, dribbling, nocturia etc. Cancer of prostate: often androgen dependent. Hard nodule on periphery of gland, hesitancy in urinating, recurrent UTI, etc. Diagnosis by serum marker: PSA, prostate specific antigen and prostatic acid phosphatase. Testicular cancer: most common solid tumor cancer in young men. Self exam preventative. Biopsy not performed. Tumor markers: hCG and AFP. Ultrasound Chlamydia: most common STD. Males: itchy, white discharge, painful swollen scrotum. Females: no symptoms until PID or infertility. May infect newborn. Gonorrhea: males: inflammation of urethra Females: asymptomatic until PID. May cause blindness in newborns. Syphillis: chancre at site of infection. Painless firm ulcerated nodule, 3 wks after exposure. If untreated flu like illness with rash. Tertiary stage: dementia blindness. Rx: antimicrobials. Genital herpes: blisters on genitals, itching, painful. Antivirals. Genital warts: HPV, incubation up to 6 months, asymptomatic, may predispose to cervical or vulvar cancer.