Neurolocalization Made Easy
advertisement

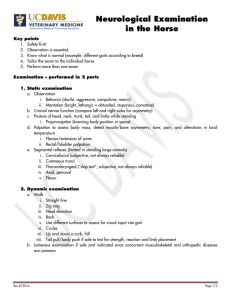
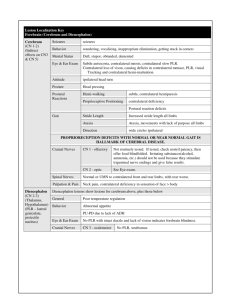
NEUROLOCALIZATION MADE EASY Jared B. Galle, DVM, Diplomate ACVIM (Neurology) Dogwood Veterinary Referral Center 4920 Ann Arbor-Saline Road Ann Arbor, MI 48103 Localizing a neurologic problem to an anatomical region of the nervous system (neuroanatomic localization) is key to making a neurologic diagnosis. I often find that understanding how the anatomic regions work together is intimidating and confusing for most veterinarians. A basic knowledge and understanding of how these regions normally function and interact with each other will make it easier to interpret the neurologic exam findings and make a neuroanatomic localization. This lecture will review the function regionals of the nervous system and neurolocalization. Neuroanatomical Regions The nervous system is divided into anatomical regions based on their functions. These regions function much like our government. The forebrain is similar to the president. It is responsible for making decisions, initiating movements, leading the rest of the body, and controlling behavior. The brainstem is similar to the military. It carries out whatever functions the forebrain tells it to do through cranial nerves and large groups of neurons (upper motor neurons - UMN) that travel down the spinal cord and synapse on lower motor neurons (LMN). It also conveys sensory information to the forebrain and cerebellum through sensory tracts from the limbs. The cerebellum is similar to the CIA. It is responsible for coordinating movements and making sure that the other regions of the nervous system know what’s going on in all the others. The spinal cord and peripheral nerves are an extension of the military (think of them as branches of the military). They carry out the functions generated by the brainstem via motor UMNs and convey information to the forebrain and cerebellum though sensory nerves and tracts. There are eight anatomical regions of the nervous system where a neurologic lesion can be localized: Forebrain, Cerebellum, Brainstem, C1-5 spinal cord segments, C6-T2 spinal cord segments, T3-L3 spinal cord segments, L4-S3 spinal cord segments, and the peripheral nervous system. Neuroanatomic Localization When localizing a neurologic problem, all of the deficits and abnormalities on the neurologic exam should be explained by a single lesion in one anatomical region of the nervous system (“X” marks the spot”). Neurologists are like pirates - we want one “X” on one neuroanatomical region to account for all the deficits detected on our exam. When a single lesion does not account for all deficits (more than one “X”), a multifocal or diffuse disease should be considered. 1. Forebrain: Includes the right and left cerebral cortex (gray and white matter, basal nuclei) and the diencephalon (thalamus, hypothalamus). The forebrain controls behavior, initiates movements, interprets all sensory information, and controls endocrine/autonomic functions. Contralateral (opposite side) sensory and motor deficits are seen with a forebrain lesion. Forebrain Functions Forebrain Deficits/Abnormalities Behavior, personality • Behavior changes • Pacing, wander aimlessly circling, getting stuck in corners, head pressing, “reverse does not work”, not as social, sleeping in different places, urinating/defecating in house All sensory inputs terminates here • Postural reaction deficits • Sensory deficits on face • Vision loss • Decreased superficial sensation Initiates movement • Mild weakness • Seizures Endocrine and autonomic functions • Endocrine disorders (PU/PD, eating abnormalities) • Changes in consciousness and sleep Contralateral proprioceptive deficits with a normal or almost normal gait is a hallmark sign of a cerebral lesion. Another common sign of a forebrain lesion is walking in wide circles toward the lesion side. 2. Brainstem: Includes the midbrain, pons, and medulla oblongata. The brainstem contains large motors centers that project UMNs down the spinal cord that are needed for walking and supporting weight. It also contains regulatory centers for consciousness (ascending reticular activating system - ARAS) and has ten pairs of cranial nerves (3-12) which transmit sensory and/ or motor functions. Ipsilateral (same side) sensory and motor deficits are seen with a brain stem lesion. Brainstem Functions Brainstem Deficits/Abnormalities Motor centers Paresis/Paralysis - moderate to severe Cranial nerves Cranial nerve deficits 3-12 ARAS Alteration of consciousness (depression, stupor, coma) Links postural reactions between forebrain and spinal cord Postural reaction deficits A brainstem lesion rarely causes a single cranial nerve deficit (ie. facial paralysis) without postural reaction deficits and some degree of weakness/paralysis. Most isolated cranial nerve deficits are due to an idiopathic cranial nerve disease. 3. Cerebellum: Regulates and coordinates movement by controlling the rate, range, and force on the ipsilateral side (same side) of the body. It also plays a role in maintaining balance with the vestibular system. The cerebellum does not initiate movement. A cerebellar lesion typically causes exaggerated movements (hypermetria), ataxia without weakness, and intention tremors. A menace deficit can also be seen with a cerebellar lesion. Cerebellar deficits are easy to remember if you use the acronym HAT - the cerebellum is a HAT for the brainstem. Cerebellum Functions Cerebellum Deficits/Abnormalities Maintains and coordinates movement • Hypermetria • Ataxia • Tremors (intention) • 4. Spinal Cord: The spinal cord starts at the foramen magnum and extends to the 6th lumbar vertebra in dogs and the 7th lumbar vertebra in cats. It tapers to the conus medullaris. The spinal cord is divided into four functional segments: C1-5, C6-T2, T3-L3, and L4-S3. It contains sensory tracts and upper motor neurons (UMN) which are located in the white matter along the periphery of the spinal cord. The spinal cord also contains lower motor neuron cell bodies (LMN) in the grey matter which are the beginning of peripheral nerves. The spinal cord is responsible for relaying sensory information (proprioception and nociception) from the limbs to the forebrain and cerebellum, and for relaying UMN information from the brainstem to the LMNs. The UMN stimulates the LMN cell bodies to produce a gait. The UMN are primarily facilitatory to flexor muscles and inhibitory to extensor muscles. The UMN also inhibits the LMN component of the reflex arc. The LMNs are located along the entire spinal cord but for localization purposes, the ones routinely evaluated are located in the C6-T2 (thoracic limb reflexes) and L4-S3 (pelvic limb reflexes) spinal cord segments. The deficits seen with a spinal cord lesion are dependent upon which functional segment is affected (ie. C1-5, C6-T2, T3-L3, L4-S3). The location of a lesion determines which limbs are affected and whether there are UMN or LMN signs in the limbs. If the UMN going to those limbs is affected, UMN signs will be seen. If the LMN going to those limbs is affected, LMN signs will be seen. UMN Signs LMN Signs Paresis/Paralysis Paresis/Paralysis Normal or exaggerated reflexes Decreased or absent reflexes Normal or increased tone Decreased or absent tone Prolonged muscle atrophy Neurogenic atrophy (rapid) Large, turgid, hard to express bladder Atonic, easily expressed bladder C1-5 Myelopathy: A lesion in these segments can result in deficits in all limbs (postural reaction deficits, tetraparesis/tetraplegia) because it affects sensory tracts coming from and UMN going to the forelimbs and pelvic limbs. Reflexes are normal or increased with a lesion in these segment. An UMN bladder can also occur. C6-T2 Myelopathy: A lesion in these segments can result in deficits in all limbs (postural reaction deficits, tetraparesis/tetraplegia). It affects the LMN going to the forelimbs, the UMN going to the pelvic limbs, and the sensory tracts coming from all limbs. Forelimb reflexes are decreased to absent, while pelvic limb reflexes are normal to increased. An UMN bladder can also occur. T3-L3 Myelopathy: A lesion in these segments can result in deficits in the rear limbs (postural reaction deficits, paraparesis/paraplegia). The forelimbs are normal. It affects sensory tracts coming from and UMN going to the pelvic limbs. Pelvic limb reflexes are normal to increased. An UMN bladder can also occur. L4-S3 Myelopathy: A lesion in these segments can result in deficits in the rear limbs (postural reaction deficits, paraparesis/paraplegia). The forelimbs are normal. It affects sensory tracts coming from and LMN going to the pelvic limbs. Pelvic limb reflexes are decreased to absent. Anal tone may also be poor to absent, and the perineal reflex may be decreased to absent. A LMN bladder can also occur. Spinal Cord Lesion Forelimb Signs Pelvic Limb Signs C1-5 myelopathy UMN UMN C6-T2 myelopathy LMN UMN T3-L3 myelopathy Normal UMN L4-S3 myelopathy Normal LMN Peripheral Nervous System (Neuromuscular) The peripheral nerve, skeletal muscle, and neuromuscular junction are grouped into the same neuroanatomic localization. A lesion affecting one of these components of the peripheral nervous system results in varying amounts of weakness. Weakness can be seen in both cranial nerves and peripheral nerves in the limbs. A key feature to help distinguish a peripheral nervous system lesion from a central nervous system lesion is that postural reactions are typically intact with a peripheral nervous system lesion, whereas they are delayed or absent with a central nervous system lesion. Other neurologic deficits include: reduced or absent reflexes, decreased or absent muscle tone, exercise intolerance, and neurogenic atrophy. Peripheral Nervous System Lesion Forelimbs Rear Limbs Peripheral nerve, neuromuscular junction, skeletal muscle LMN LMN References available upon request