The 2015 OPPS Rules CMS Website OPPS Final Rule 1613
advertisement

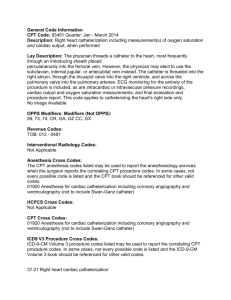
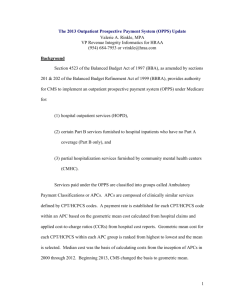
11/14/2014 The 2015 OPPS Rules Proposed Rule Published on July 8, 2014 on the CMS website CMS-1613-P ED Facility Coding Update – 2015 Final Rule D Karen Marsh Published on October 31, 2014 CMS-1618-FC 1052 pages 719 public comments submitted OPPS Final Rule 1613-FC Addenda List CMS Website Addendum http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/HospitalOutpatient-Regulations-and-Notices-Items/CMS-1613FC.html?DLPage=1&DLSort=2&DLSortDir=descending Addendum B Payment Rates and Status Indicators If paid How much CMS-1613-FC Description Common Use A OPPS APC List, SI and payments by APC list B Final payment by HCPCS Code Look up payment rates, Status Indicators C Final HCPCS codes payable by APC Determine which codes are in each APC D1 OPPS Payment Status Indicators Description of each SI D2 Final comment Indicators Indicate new or changed codes E Codes paid only as Inpatient Inpatient only codes J Ranks to determine primary assignment in composite APC Not used L OPPS Out Migration Adjustment Not used M HCPCS codes assigned for Composite APCs What is included in APC 8009 (ED/Observation) N Bypass codes for creating “pseudo” single procedure claims To determine geometric mean for costs Costs for HOP services by HCPC code Frequency stats, cost info Cost – Stats Addendum B Sort by Status Indicator Q1 Packaging with an S/T/V Codes 1 11/14/2014 Addendum D-1 Status Indicators Status Indicator Q1 Q2 Q3 Utilization Increased Outpatient Bundling Definition Paid under OPPS; Addendum B displays APC assignments when services are separately payable. Paid under OPPS; Addendum B displays APC assignments when T-Packaged Codes services are separately payable. Paid under OPPS; Addendum B displays APC assignments when services are separately payable. Addendum M displays composite APC assignments when codes are paid through a composite APC. (1) Composite APC payment based Codes That May Be Paid Through a on OPPS composite-specific Composite APC payment criteria. Payment is packaged into a single payment for specific combinations of services. (2) In other circumstances, payment is made through a separate APC payment or packaged into payment for other services. STV-Packaged Codes Packaging • Increase in number of codes packaged • Impacts services that were previously paid separately • Single payment covers the Comprehensive costs of all services • Continue to expand APCs CMS-1613-FC Addendum D-1 – Final OPPS Status Indicators for CY 2015 Moving towards “Mini DRGs” in the Outpatient Arena APC Advisory Expert Panel http://www.cms.gov/Reg ulations-andGuidance/Guidance/FA CA/Downloads/082514HOP-Panel-MeetingAgenda.pdf Modern Healthcare , July 11, 2014 ACEP Comments Composite APC for Extended Assessment and Management • While costs to beneficiaries in short stay observation are significantly less than the inpatient deductible ($1216 in 2014), we urge CMS to consider options to minimize the financial burden for the beneficiary associated with selfadministered drugs while they are receiving observation services. • We strongly support efforts to count outpatient observation toward the 3-day stay. ACEP Comments on OPPS for 2015 – published on ACEP.org website ACEP Comments Collapsing Outpatient Facility Codes We appreciate that CMS did not finalize its 2014 proposal to reduce the 10 levels of Emergency Department (ED) facility codes and APCs to two and support CMS’ proposal to continue the current policy in 2015. We agree that further analysis is needed to assess any proposed changes in the payment structure for ED visits, particularly since the range of acuity and complexity of patient conditions is so great. Our members’ experience is such that even in instances when patients are judged to be very stable at triage, some subsequently require substantial resources. We are also pleased to see recently published research that did not substantiate concerns about “upcoding” in the emergency department (ED) as a result of using EHRs.1 ACEP Comments on OPPS for 2015 – published on ACEP.org website 2 11/14/2014 ACEP Comments Documenting Site of Service We understand the need for accurate data regarding costs, and in that context, we again urge CMS to require hospitals to report the site of observation services, i.e., in a dedicated unit versus an inpatient floor, in order to determine Conversion Factor $74.144 for 2014 Compared to $72.78 in 2014 No QDRP = $72.661 Hospital Outpatient Quality Reporting (OQR) Program In addition to proposing removal and addition of measures, CMS notes that public reporting of the claims-based measure OP-15, “Use of Brain Computed Tomography (CT) in the Emergency Department for Atraumatic Headache” was deferred in previous rulemaking, and that deferral continues. Therefore, we must restate our objections to proposed measure OP-15, and ask CMS to remove this measure from the final rule. ACEP Comments on OPPS for 2015 – published on ACEP.org website CMS-1613-P pages 232 2014 Packaging Packaged Codes Package the following (those related to the ED and OBS) 1. Drugs that function as supplies when used in a diagnostic test or procedure 2. Drugs, that function as supplies or devices when used in a surgical procedurePackaged only 3. Clinical diagnostic lab tests labs and some 4. Procedures described by an “add-on” code add on codes 5. Ancillary services (status indicator “X”) Unconditionally packaged CPT codes – Conditionally packaged CPT codes - SI = N SI = Q1 or Q2 CMS-1601-FC Packaging Rationale Packaging Add on Codes Averaging payments May be more or less on a given patient Multiple interrelated items and services into a single payment to Create incentive for hospitals to provide services efficiently Manage resources with maximum flexibility Encourages hospitals to effectively negotiate with suppliers to reduce the costs of items Encourages hospitals to establish protocols Promotes predictability and accuracy of payments Add on Codes Goal: Become more consistent as a Prospective payment system rather than a fee-for-service system CMS-1613-FC pages 197-198 All add on codes except drug administration are packaged into the primary code CMS-1613-FC 199, 208 3 11/14/2014 Packaging Ancillary Services Q1 Status Indicator Codes • Delete SI “X” • Package with SI “Q1” ( S/V/T on claim) • Refer to SI in Addenda A, B or C CMS-1613-FC page 205 CMS-1613-FC – Addendum C Addendum B Drug Administration Payments Q1 Status Indicator Codes CPT CMS-1613-FC – Addendum B Key Ancillary Packages APC Category 2013 Rate 2014 Rate 2015 Rate 96360 $74.69 $105.90 $108.20 96361 $27.01 $29.50 $32.57 96365 $146.24 $172.18 $173.53 96366 $27.01 $29.50 $32.57 96367 $39.13 $43.78 $53.52 96368 $0 $0 $0 96372 $39.13 $43.78 $53.52 96374 $39.13 $105.90 $108.20 96375 $39.13 $43.78 $32.57 96376 $0 $0 $0 • No new drug admin packaging • 25% decrease for Subsequent IVP • IM > subsequent IVPs • 25% increase in subsequent infused meds Packaging Impact to Hospital Payment Rate Debridement/Lacerations/Burns $98.46 Pulmonary Treatments (Inhalation therapy) $164.56 ECG tracing $78.44 Level I plain Films - Chest, Abdomen, Limbs $59.34 Level II Plain Films – Jaw, Facial bones, Skull, Spine, $94.98 Level I Diagnostic Ultrasound Breast, Fetus, Pelvic $91.66 Level II Minor Procedures Splints, Strapping, Cardiac Monitor $52.35 Level III Minor Procedures – Nosebleed, ABG, NG tube, Foley $131.69 Level II Eye Treatments, remove foreign bodies $100.81 Hospitals are still required to still code according to CPT and CMS rules so that appropriate rate setting can occur in the future Change in reimbursement for Medicare patients – will vary at each site based on current patient population (acuity, drug administration utilization, ancillary services) Ability to track what is packaged CMS-1613-FC – Addendum C 4 11/14/2014 OIG E/M Study Included as an attachment in the OPPS CMS-1613-FC E/M Coding Office of the Inspector General May 2014 OEI-04-10-00181 OIG E/M Study OIG E/M Study Recommendations ED Visits small portion of study 49 charts 8.8% Office of the Inspector General May 2014 OEI-04-10-00181 Page 14 Educate physicians • Review claims from high coding physicians • Follow up on claims that were errors Office of the Inspector General May 2014 OEI-04-10-00181 Page 27 Evaluation and Management Levels Comments and Responses Public Comment • CMS E/M Statistics CY 2013 Medicare E/M Levels CY 2013 CMS Response 50.0% 45.0% Support decision not to propose changing to one ED visit Appreciate support 40.0% Appreciate support One visit level is not appropriate for the ED and it would create a “payment bias” Requires additional study Continue as is for the foreseeable future No comment CMS should work with the AMA to create facility specific ED visit CPT codes If AMA created facility specific CPT codes CMS will consider such codes for OPPS Develop 3 trauma specific HCPCS codes for trauma patients when trauma team is used Will consider as they continue to study Percentage of Total 35.0% Commended CMS on the decision to proceed with caution for any ED visit changes 30.0% 25.0% 20.0% 15.0% 10.0% CMS-1613-FC pages 517-518 5.0% 0.0% EM Levels 2013 99281 1.3% 99282 5.2% 99283 20.0% 99284 45.2% 99285 27.4% 99291 0.9% E/M Level CMS-1613-FC Addendum Cost-Stats 5 11/14/2014 EM Payment Rate Comparisons 2013 / 2014 / 2015 E/M Frequency Table CY 2013 HCPCS 99281 99282 99283 99284 99284 99285 99285 99291 99291 SI V V V V Q3 V Q3 S Q3 APC 609 613 614 615 0615O 616 0616O 617 0617O Payment Rate $60.46 $112.74 $198.31 Total Frequency 275,054 1,077,815 4,179,395 4,829,305 4,623,719 3,314,085 2,415,332 112,709 92,601 20,920,015 . $333.67 . $492.49 . $656.69 % of Total 1.3% 5.2% 20.0% 23.1% 22.1% 15.8% 11.5% 0.5% 0.4% 100.0% % of Total E/M Level 1.3% 99281 5.2% 99282 20.0% 99283 45.2% 99284 27.4% 99285 0.9% 99291 2013 Rate 2014 Rate Level 1 EM Level $51.82 $55.65 2015 Rate $60.46 Level 2 $92.16 $100.91 $112.74 Level 3 $143.36 $166.45 $198.31 Level 4 $229.37 $293.71 $333.67 Level 5 $344.71 $455.93 $492.49 Critical Care $535.86 $634.94 $656.69 100.0% Q3 Composite APC (Observation) 34% of the levels are paid as a composite APC Increases to compensate for ancillary packaging Addendum B – OPPS 2013, 2014, 2015 CMS-1613-FC Addendum Cost-Stats E/M Payment Table Type A versus Type B ED Volume Comparisons Year Type A Type B Total ED Visits 2010 16,263,221 227,463 16,490,684 2011 17,233,890 246,797 17,480,687 2012 18,476,771 243,891 18,720,662 2013 20,920,015 221,156 21,141,171 1% of ED visits are coded as Type B ED Visits Type A EM Level 2014 Level 1 $55.65 Level 2 $100.91 Level 3 $166.45 Level 4 $293.71 Level 5 $455.93 Critical Care $634.94 Type A 2015 $60.46 $112.74 $198.31 $333.67 $492.49 $656.69 Type B 2014 $51.92 $61.67 $91.71 $163.27 $312.43 $634.97 Type B 2015 $62.70 $69.49 $112.93 $198.91 $304.26 $656.69 Addendum B – OPPS 2014, 2015 CMS-1404-FC,1504FC,1525FC_OPPS Median Files by HCPCS/CPT CMS-1613-FC Addendum Cost-Stats CMS-1613-FC Addendum Cost-stats E & M Distribution – Average ALL 35 Public Comments on ED E/M Coding 9/1/2012 – 8/31/2013 2012 30 2013 25 20 15 10 5 0 99281 99282 99283 99284 99285 99291 http://www.publicintegrity.org/2012/09/20/10811/hospitalsgrab-least-1-billion-extra-fees-emergency-room-visits 6 11/14/2014 Outpatient Payer Mix Trauma Activation Rule Can only be paid with Critical Care 99291 What percentage of ED patients are Medicare patients? Code G0390 – Trauma Response Payments”: 2010 payment = $833.93 2011 payment = $924.48 • Based on 122 hospitals 2012 payment = $788.79 • Total volume 4.7 million visits 2013 payment = $914.47 2014 proposed= $961.51 Volume Medicare Commercial Medicaid Self Pay Other 882,384 1,229,984 1,216,972 944,888 440,305 2012 payment = $888.97 (99291= 656.69) CMS rejected request to add other E/M codes as eligible in the 2011 rule No specific mention of trauma activation code in the proposed OPPS 2014 or 2015 rules Percentage 18.6% 26.0% 25.7% 20.3% 10.3% Addendum B Final Rules: 2010, 2011, 2012, 2013, 2014, 2015 E/M – National Guidelines CMS-1613-FC page 512 Clinic Visits CMS-1613-FC page 516 ED Visits Observation CMS-1613-FC page 516 7 11/14/2014 Observation -Issues to Watch As mentioned in the CMS OPPS Final Rule for 2013 Time Based Should there be a time limit for Observation, i.e. 24-48 hours Should OBS visits that span >48 hours and are medically necessary automatically qualify for inpatient status Payment Alignment Short Stay DRG versus Outpatient payment structure Physician payment in line with hospital reimbursement Patient Issues Co-payment for outpatient services versus inpatient SNF/ rehab 3 day inpatient requirement to qualify No relevant changes in 2015 Observation Proposal Two Midnight Rule (part of the Inpatient Prospective Payment Rule) Hospital stays that last over a minimum of 2 midnights will be considered to be an inpatient stay Hospital stays that are less than 2 midnights will be considered as an Observation patient Physician should write an order if they anticipate that the physician will require stay of at least 2 midnights Delayed implementation until December 31, 2013 CMS-1599-FC Inpatient PPS Observation Proposal Single Extended Assessment & Management Composite APC (8009) Levels 4/5 ED or clinic E/M visit, critical care or direct referral code Day of admission or 1 day earlier No T status on claim on admission date or 1 day earlier Reimbursement Example Single payment of $1234.22 ED visit level, and any packaged codes (TBD) All Observation hours Any packaged Observation codes Rules Summary Hospital Detailed Bill ED Level (99284/99285 or 99291) must be on claim Observation hours will show on a separate line APC 8009 will show next to E/M level to indicate bundling of E/M and OBS hours Payment will show on the E/M line Observation hours will show as “0” Drug administration will show on separate lines Drug administration will show as reimbursable Lab charges will show on separate lines Lab charges will be bundled and show as “O” Radiology charges will show on separate lines Radiology charges will show as reimbursable Level 4 ED visit, 13 hours of Observation, 2 IV push injections, 5 lab tests and 1 radiology test 8 11/14/2014 Hospital EOB - Medicare Charges versus Reimbursement ED + OBS paid here ED Level Charge Reimbursement E/M Level $1419.50 $833.13 Includes OBS hours Observation Hours $484.25 0 Included in E/M as APC 8009 Drug Administration $322.75 $104.02 Lab $946.25 0 Bundled (new in 2014) Medications $73.75 0 Bundled Misc / Supplies $295.00 0 Bundled $4,555.00 $1,021.70 OBS Hours Drug Admin Lab codes Paid B u n d l e Totals 49 Comments Patient co-payment $272.07 AMA CPT 2014 Update CPT Changes 541 Total Changes – 264 New Codes – 143 Deleted Codes – 134 Revised Codes New CPT Codes 2015 CPT Code 20604 20606 20611 90630 Deleted CPT Codes 2015 New CPT codes effective January 1, 2015 Arthrocentesis, aspiration and/or injection, small joint or bursa (e.g.. Fingers, toes); small joint or bursa (e.g.. fingers, toes) with ultrasound guidance , with permanent reading and recording Arthrocentesis, aspiration and/or joint, intermediate joint or bursa (e.g.. Leg, temporomandibular, acromioclavicular, wrists, elbow or ankle, olecranon bursa) with ultrasound guidance, with permanent reading and recording Arthrocentesis, aspiration and/or joint, major joint or bursa(e.g. shoulder, hip, knee, subacromial bursa) with ultrasound guidance , with permanent reading and recording CPT Code 21800 Deleted codes after December 31, 2014 Closed treatment of rib fracture, uncomplicated, each Influenza vaccine, quadravalent (IIV4) split virus, preservative free, for intradermal use. 9 11/14/2014 Revised CPT Codes 2015 CPT Code Immunizations Description only changes (Information Only) Arthrocentesis, aspiration and/or injection, small joint or bursa 20600 (e.g.. Fingers, toes); small joint or bursa (e.g.. fingers, toes) without ultrasound guidance Arthrocentesis, aspiration and/or joint, intermediate joint or 20606 bursa (e.g.. Leg, temporomandibular, acromioclavicular, wrists, elbow or ankle, olecranon bursa) without ultrasound guidance Arthrocentesis, aspiration and/or joint, major joint or bursa(e.g. 20610 shoulder, hip, knee, subacromial bursa) without ultrasound guidance Professional Edition CPT 2015, page 552 Immunizations Modifier 59 Exact vaccine product must be reported Professional Edition CPT 2015, page 552 Modifier -59 Med Learn Reference 10 11/14/2014 Modifier - 59 Modifier -59 • Primary Issues • Why? – Used to define a variety of circumstances – “Incorrectly used as a modifier to bypass the NCCI edits • Identify different encounters – “The most widely used modifier” – OPPS $11B billed lines with -59 “Associated with on considerable abuse and high levels of manual audits” Projected error of $770M • Identify different anatomical sites • Identify distinct services – “CMS is concerned by this pattern of abuse because it siphons off funds…..” CMS Transmittal 1422 CMS Transmittal 1422 Modifier - 59 MODIFIER DEFINITION XE Separate encounter, A service that is because it occurred during a separate encounter XS Separate structure, A service that is distinct because it was performed on a separate organ/structure XP Separate Practitioner, A service that is distinct because it was performed by a different practitioner XU Unusual Non-Overlapping Service, The use of a service that is distinct because it does not overlap the usual components on the main service Modifier - 59 CMS Transmittal 1422 CMS Transmittal 1422 Case 1 Analysis Item Case Studies 2013 2014 2015 E/M Level 99284 $229.37 $293.71 $333.67 EKG 93005 $26.67 $0 $0 Chest X-Ray (Q3) 71020 $45.95 $57.35 $59.34 IVP 96374 $39.13 $105.90 $108.20 SC 96372 x 2 $78.26 $43.78 $53.52 Hydration 96361 x 3 $81.03 $88.50 $97.71 Labs Varies Per lab fees $0 $0 $500.41 (+ Labs) $589.24 $652.44 TOTAL CPT 11 11/14/2014 Case 2 Analysis Case 3 Analysis CPT 2013 2014 2015 CPT 2013 2014 2015 E/M Level 99284 $229.37 $293.71 $333.67 E/M Level 99285 $344.71 $455.93 $492.49 IVP 96374 $39.13 $105.90 $108.20 CT scan head (Q3 70491 $297.15 $249.00 $240.83 MRI head (Q3) 70551 $338.49 $294.78 $286.30 Infused med 96365 $146.24 $172.18 $173.53 EKG 93005 $26.67 $27.12 $0 IVP 96374 x 4 $156.52 $423.60 $432.80 Labs X2 Per fee schedule $0 $0 Labs Varies x3 Per lab fees $0 $0 $663.66 + Labs $721.51 $728.17 $944.62 (+ Labs) $1300.71 $1339.65 Item TOTAL Item TOTAL OBS Case (#9) Analysis Item 2013 2014 2015 E/M Level 99285 $0 $0 $0 Infused med 96365 $146.24 $172.18 $173.53 Add meds infused 96366 x 1 27.01 $29.50 $32.57 IVP add diff meds 96375 x 6 $234.78 $262.68 $195.42 IVP repeats 96376 x 5 $0 $0 $0 Observation G0378 x 16 $0 $0 $0 Observation Composite (8009) Combo ED + OBS hours $798.47 $1199.00 $1234.22 Labs Varies Per lab fees $0 $0 $1207 (+ Labs) $1663.36 $1462.21 TOTAL CPT OBS Case (#10) Analysis 2013 2014 2015 E/M Level Item 99285 $0 $0 $0 EKG (Q1) 93005 $26.67 $0 $0 X-Ray chest 71020 $45.95 $57.35 $59.34 Infused med 96365 $146.24 $172.18 $173.53 Add meds infused 96366 x 20 $540.20 $590 $651.40 IVP add diff meds 96375 x 5 $195.65 $218.90 $162.85 IVP repeats 96376 x 2 $0 $0 $ IM Meds 97362 x 2 $78.26 $87.56 $107.04 Foley Catheter (Q1) 51702 $49.64 $98.25 $0 Observation G0378 x 39 $0 $0 $0 Observation Composite Combo ED + OBS hours $798.47 $1199 $1234.22 Labs Varies x 16 TOTAL CPT Per lab fees $0 $0 $1881 (+ Labs) $2423.24 $2388.38 Ventilator Management in the ED CPT 94002 QUESTIONS 71 12