The β-Endorphin Role in Stress-Related Psychiatric Disorders
advertisement

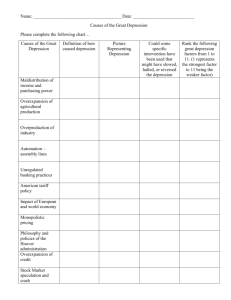
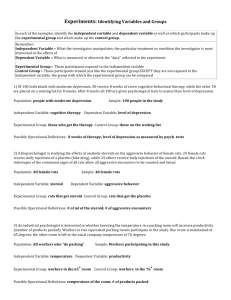
1096 Current Drug Targets, 2009, 10, 1096-1108 The -Endorphin Role in Stress-Related Psychiatric Disorders Avia Merenlender-Wagner, Yahav Dikshtein and Gal Yadid* Neuropharmacology Section, The Mina and Everard Goodman Faculty of Life Sciences and The Leslie and Susan Gonda (Goldschmied) Multidisciplinary Brain Research Center, Bar-Ilan University, Ramat-Gan, Israel Abstract: Long known for its anti-nociceptive effects, the opioid -endorphin is also reported to have rewarding and reinforcing properties and to be involved in stress response. In this manuscript we summarize the present neurobiological and behavioral evidence regarding the role of -endorphin in stress-related psychiatric disorders, depression and PTSD. There is existing data that support the importance of -endorphin neurotransmission in mediating depression. As for PTSD, however, the data is thus far circumstantial. The studies described herein used diverse techniques, such as biochemical measurements of -endorphin in various brain sites and behavioral monitoring, in two animal models of depression and PTSD. We suggest that the pathways for stress-related psychiatric disorders, depression and PTSD, converge to a common pathway in which -endorphin is a modulating element of distress. This may occur its interaction with the mesolimbic monoaminergic system and also by its interesting effects on learning and memory. The possible involvement of endorphin in the process of stress-related psychiatric disorders, depression and PTSD, is discussed. Keywords: Anxiety, depression, post-traumatic stress disorder (PTSD), opioids. INTRODUCTION The involvement of the opioid system in depression and PTSD (post traumatic stress disorder) has been previously studied by several groups. Most of these studies employed pharmacological means, and examined the involvement of the different opioid receptors in these psychiatric diseases. However, an exclusive role for a specific opioid in these diseases had not been thoroughly assessed. Long known for its anti-nociceptive effects, the opioid -endorphin is now known to induce reinforcing properties and to decrease feelings of distress. In this manuscript we provide new data, using animal models, which support the involvement of endorphin in stress-related psychiatric disorders, depression and PTSD. THE OPIOID SYSTEM Opioid Peptides and their Biosynthesis The first endogenous opioids were discovered in the mid80s [1]. Later, researchers succeeded in isolating and characterizing the enkephalins [2], dynorphins [3, 4] and also endorphin [5]. The behavioral and physiological effects of these opiods, such as rewarding and sedative sensations, are similar to those displayed by morphine as they all interact with post-synaptic opiod receptors [6-8]. Most of the endogenous opioids are enzymatically generated from three precursor proteins, proopiomelanocortin (POMC) [9]; prodynorphin (PDYN) [10] and proenkephalin (PENK) [11]; which undergo specific cleavage by proteolytic enzymes to give opiod as well other as non-opiod peptides. The final product is dependent on the enzymes present and can also *Address correspondence to this author at the Leslie and Susan Gonda (Goldschmied) Multidisciplinary Brain Research Center, Bar-Ilan University, Ramat-Gan 52900, ISRAEL; Tel: 972-3-531-8123; Fax: 972-36354965; E-mail: yadidg@mail.biu.ac.il 1389-4501/09 $55.00+.00 involve posttranslational processing as in the case of POMC, to produce several opioid peptides, including -LPH and endorphin [12]. The Opioid - Endorphin -lipotrophin is a fat-mobilizing pituitary hormone [5] which contains an N-terminal fragment known as Metenkephalin and a C-terminal fragment known as -endorphin. The cleavage of POMC generates -lipotrophin, which is later cleaved to produce -endorphin [9]. The cleavage enzyme L-cathepsin has been recently linked with the production of -endorphin through a protease gene knockout and expression study [13]. -endorphin is an endogenous opioid peptide consisting of 31 amino acids which has been demonstrated to be involved in stress-related disorders as well as in other disorders such as obesity, diabetes, and altered immune responses [14-16]. -endorphin can act as a neurotransmitter in the central nervous system and neurons in the brain that synthesize and release -endorphin are located mainly in the arcuate nucleus of the hypothalamus (ArN), the anterior and neurointermediate lobes of the pituitary gland and the nucleus tractus solitaries, and these neurons’ extensions terminate in diverse brain regions [17, 18]. In both humans and rodents, injection of exogenous -endorphin into the intracerebrospinal fluid causes a stronger analgesic effect than that of morphine [1922]. Since it is produced in some regions in the brain that are associated with stress response its role was suggested in the manifestation of some psychiatric diseases [23-25]. Interaction of -Endorphin with the Monoaminergic Systems Several studies show that activation of the opioid system can alter dopamine release. Ventricular infusions of © 2009 Bentham Science Publishers Ltd. -endorphin and strees-related psychiatric disorders endorphin were shown to increase dopamine release in the nucleus accumbens via - and -opioid receptors [26]. endorphin inhibits the GABA-blocking dopaminergic neurons and lead to increase in dopamine release [27]. Furthermore, -endorphin at doses that stimulate dopamine release in the nucleus accumbens is rewarding, as tested by the conditioned place preference paradigm [28]. Interestingly, accumbal -endorphin has a reinforcing effect [24, 29, 30], which suggests that -endorphin is an endogenous mediator of reinforcement, which is a measure of reward feelings using opertant conditioning, and can increase mesolimbic dopaminergic neurotransmission as a secondary target. These findings indicate an opioid-dopamine interaction wherein opioid receptor agonists act at a site upstream from the dopamine synapse in the nucleus accumbens. The dopamineopioid interaction is the evidence of enhanced locomotor response and reward sensitivity to opioid receptor agonists, given systemically or intra-accumbal, following mesolimbic dopaminergic lesions or chronic treatment with dopamine blockers [31, 32]. Our demonstration of a decrease (to ~35% of controls) in -endorphin basal levels in 6-hydroxydopamine-treated rats may be relevant for the understanding of this dopamine-opioid interaction [33]. This result indicates that the basal opioid tone in the nucleus accumbens is under dopaminergic control. The relevance of the dopaminergic system to depression was previously suggested (for review see [34]). Therefore, if -endorphin is modulated by dopamine, it may be a relevant chain in the neurochemical cascade that affects the manifestation of depressive like behavior. Other data [35], as well as those presented herein, demonstrate that extracellular endorphin levels in NAcc (nucleus accumbens) and ArN were altered in response to 5-HT (5-hydroxytryptamine). 5-HT1A is the most widespread serotonin receptor. It is present in both the central and peripheral nervous systems, and controls a variety of different biological and neurological functions. Activation of 5-HT1A receptors has been shown to increase plasma -endorphin levels in animal studies and in healthy humans. In depressed patients who were treated with citalopram for 8 weeks, a reduction was shown in the endorphin response to a 5HT1A agonist. Moreover, the reduction was parallel to the improvement in the patient's condition. Since 5-HT is involved in many psychiatric diseases it is hypothesized that -endorphin might mediate the development of these diseases. There are additional studies that indicate an interaction between -endorphin and 5HT. Treating pregnant rats with -endorphin caused a long- lasting reduction of 5-HT levels in the frontal cortex, hypothalamus and brain stem in the offspring [37]. The evidence of an interaction between -endorphin and monoamines may facilitate the understanding of the role that -endorphin plays in hedonia and motivation, since monoamines were established as key players in both hedonia and motivation. Decreased motivation and anhedonia are core symptoms in depression and are also involved with other psychiatric diseases. Current Drug Targets, 2009, Vol. 10, No. 11 1097 -Endorphin, Opioid Receptors and their Knockout Models There are 3 major types of opioid receptors: (mu), (delta) and (kappa) and they were originally described by in-vivo and in-vitro pharmacology [38]. Several different neural systems are modulated by the opiate receptors. The mu-Opioid receptor gene, OprM, is alternatively spliced into many variants and distributed in the Raphe nucleus and different limbic regions. Studies provide evidence for the region- and neuron-specific processing of the OprM gene and support the possibility of functional differences among the variants [39]. -endorphin has the highest affinity to mu-Opioids receptor. mu-Opioids inhibit GABAergic and the glutamatergic afferents, thereby indirectly affect 5-HT efflux in the dorsal raphe nucleus. In contrast, kappa-opioids inhibit 5-HT efflux independent of their effects on glutamatergic and GABAergic afferents [40]. Mutant mouse strains lacking the genes encoding opioid receptors have been generated utilizing homologous recombination technology. Theses have aided in obtaining evidence suggesting that mu and delta receptors are responsible for reinforcement and that stimulation of kappa receptors triggers aversive effects [41-43]. A -endorphin knockout mouse model has also been generated [44] and these mice demonstrate a selective reward deficit [45]. The examination of this mouse model in stress-related disorders is warranted. STRESS- RELATED PSHYCIATRIC DISORDERS Depression, anxiety and PTSD are the most prevalent psychiatric disorders in the general population. Whereas stressful events are the etiological trigger to develop PTSD, they were also suggested as a concept to explain the etiological and pathophysiological mechanisms of anxiety and major depression. Moreover, vulnerability to depression has been linked to the interaction of genetic predisposition with stressful life events [46-51]. During stress, the synthesis of central corticotropin-releasing hormone (CRF) in the paraventricular (PVN) increases and is released into the hypothalamo– hypophysial portal vascular system [52]. When the peptide reaches the anterior pituitary gland, it binds to CRF- receptors and causes a cascade of intracellular steps that increases POMC gene expression. POMC is a large gene that is translated into many POMC-derived peptides such as ACTH (adrenocorticotropic hormone) and -endorphin (Fig. 1). Thus, activation of the stress system by CRH stimulates the secretion of hypothalamic -endorphin and other POMCderived peptides, which reciprocally inhibit the activity of the stress system [15, 53]. Depression Depression is a mental illness which poses a major public health problem. Major depression usually develops early in life and can last for a lifetime, during which it will impair the overall function (with regard to occupation and social roles), and affect the quality of life [54, 55] of the affected individual. Lifetime prevalence rates of up to 20% for depression have been reported for the mild form of the illness, and 1098 Current Drug Targets, 2009, Vol. 10, No. 11 Yadid et al. Fig. (1). The Opioid's Precursor Proopiomelanocortin and its Cleavage Products. The gene that codes for the precursor proopiomelanocortin (POMC) is transcribed into mRNA which is then translated to a pro-hormone of 241 amino acids. Post translational processing of the large precursor peptide produces several smaller opioid peptides, including -lipotropin, -endorphin and non opioid peptides such as adrenocorticotropic hormone (ACTH), corticotrophin-like intermediate peptide (CLIP) and -, - and - melanocyte-stimulating hormone (MSH). 2%–5% of the U.S. population will suffer from the severe form of major depression [56]. Major depression is defined as a chronic state (at least 2 weeks) of a patient suffering from at least one core symptom and at least four of the following secondary symptoms. The core symptoms are: (i) lack of motivation and loss of interest in practically everything, and (ii) inability to experience pleasure (anhedonia). The secondary symptoms are: (i) loss of appetite, (ii) insomnia [increased amount and decreased latency of rapid eye movement (REM) sleep, as deter-mined by EEG measurements], (iii) motor retardation or agitation, (iv) feelings of worthlessness or guilt, (v) continues fatigue, (vi) cognitive difficulties, and (vii) suicidal thoughts [57]. The following physiological and biochemical characteristics are often observed in depressed patients: (i) chronic pain [50% of the depressed patients suffer from chronic pain [58, 59], (ii) high levels of plasma cortisol [60, 61], (iii) resistance in the dexamethasone suppression test [62], (iv) supersensitivity to cholinergic agonists [63-66], and (v) first degree relatives that also suffer from depressive disorders, i.e, a genetic component [67]. There are several available treatments for depression, which seem to benefit about 50% of patients. These patients show some improvement after receiving antidepressant medications, usually in combination with psychotherapy involving cognitive and behavioral therapies, which together can exert a synergistic effect [68, 69]. The antidepressants are classified into three classes or three generations. The first generation is divided to two main groups: 1. The tricyclic antidepressants that are generally thought to treat depression by inhibiting the synaptic re-uptake of the neurotransmitters norepinephrine and serotonin. 2. The monoamine oxidase inhibitors (MAOI) that inhibit the activity of monoamine oxidase. Thus, preventing the breakdown of monoamine neurotransmitters and thereby increasing their bioavailability. The agents of these classes were discovered by accident. However, the fact that agents that undoubtedly change the chemical balance in the brain can benefit the patients, paved the way to the assumption that there may be chemical changes in the brain that regulate depressive symptoms to begin with. Further research has lead to the development of the second generation of agents, the serotonin-selective reuptake inhibitors (SSRIs) which are widely used today. SSRIs act by inhibiting the reuptake of serotonin after being released into the synapse [70] . The SSRIs are the most commonly used drugs to treat depression [71]. One of the main reasons that the SSRIs are widely used is due to their minority of side effects compared to the first generation drugs. -endorphin and strees-related psychiatric disorders Later, a combination of neurotransmitters was suggested to express faster onset on behavior [72]. It has been suggested that dual-action antidepressants acting on both serotonin and noradrenaline pathways in the brain may offer superior therapeutic benefit over classical antidepressants, particularly in severe depression. This third generation includes agents such as venlafaxine, reboxetine, nefazodone and mirtazapine. Studies showed no convincing differences between third-generation agents and comparators in terms of overall efficacy, relapse prevention and speed of onset [73-76]. The precise mechanism of action of antidepressant medications is yet unknown. Altering neurotransmission should be expected to have an immediate effect on mood. However, all available antidepressants exert their mood-elevating effects only after prolonged administration (several weeks), which means that the mechanism probably involves some sort of drug-induced neuroplasticity. This is consistent with the ability of these agents to benefit a wide range of syndromes besides depression, such as anxiety disorders [77] and PTSD [78]. Post Traumatic Stress Disorder (PTSD) PTSD is a chronic and disabling anxiety disorder that may develop in survivors of a traumatic event [79]. About Twenty percent out of those that were exposed to a traumatic event will develop PTSD. PTSD is currently defined by the coexistence of three clusters of different stress paradigms (re-experiencing, social avoidance and hyperarousal) persisting for at least one month [80]. Previous studies indicated that there are several risk factors for developing PTSD [81, 82]: (i) genetic background in monozygotic twines studies that were exposed to a traumatic event there was 48% correlation in PTSD symptoms. (ii) gender-females have higher risk to develop PTSD as a result of a traumatic event (ii) personal history background (child abuse etc) (iii) Family history of psychopathology (depression, bipolar disorder) (iv) The impact of the traumatic event (v) socioeconomic status (vi) environmental assistance dealing with the trauma. The most common and effective of current treatments are SSRI [83]. Research has pointed out that during the last decade, SSRIs have proven to be effective in reducing PTSD symptoms with the most effective ones being sertraline, fluoxetine, paroxetine and citalopram [83-86]. Other studies do not agree with this statement [87, 88]. The amygdala has been postulated as a crucial site in expression of PTSD pathophysiology. This assumption was further demonstrated in several Positron Emission Tomography (PET) studies. Researchers have shown that the amygdala of PTSD patients is activated during presentation of traumatic stimuli or hidden traumatic stimuli [89-91] and the destruction of this region prevent expression of PTSD [92]. Animal Models for Depression and PTSD Animal models, although limited in their ability to comprehend human complexities, are an invaluable tool in the research of markers for psychiatric disorders in general. A good animal model of clinical conditions should fulfill 4 criteria [93, 94]: Etiological validity, Face validity Construct validity and Predictive validity. Current Drug Targets, 2009, Vol. 10, No. 11 1099 So far the following 18 animal models for depression in humans have been developed: (i) predatory behavior [95, 96], (ii) yohimbine I potentiation [97, 98], (iii) kindling [99-101], (iv) dopa potentiation [102, 103], (v) 5-HTP-induced behavioral depression [104, 105], (vi) olfactory bulbectomy [106-108], (vii) isolation-induced hyperactivity [109-111], (viii) exhaustion stress [112], (ix) circadian rhythms [113], (x) behavioral despair [114-117], (xi) chronic unpredictable stress [118-121], (xii) separation models [118, 122-124], (xiii) incentive disengagement [125], (xiv) intra-cranial self-stimulation [126-130], (xv) learned helplessness [131, 132], (xvi) chronic mild stress (CMS) [133], (xvii) Swim Low-Active (SwLo) line rat [134], and (xviii) FSL rats [135]. The behavior of the FSL rats (Flinders Sensitive Line) resembles that observed in many depressed patients [136], thus the model has face validity. Both FSL rats and depressed individuals are sensitive to cholinergic agonists (cholinergic supersensitivity; [65, 137] and have serotonergic and dopaminergic abnormalities [182,136], thus the model has construct validity. Both FSL rats and depressed individuals respond positively to chronic treatment with antidepressants, thus the model has predictive validity. Since the FSL rat has fulfilled all three major criteria for determining the validity of an animal model of depression (face, construct, and predictive validities), it appears to be a suitable animal model for studying the neurochemical basis of depression and the neurochemical consequences of antidepressant agents. Unlike most other mental disorders, the diagnostic criteria for PTSD in DSM IV specify an etiological factor, which is an exposure to a life-threatening traumatic event [138]. A number of animal models have been developed, mimicking many of the behavioral and physiological changes seen in PTSD-like behavior. These models use an electric shock [139-142], underwater trauma [143] and restraint stress [144, 145], are the most widely used method of applying a stressor to laboratory animals. Nevertheless, the use of exogenous stimuli that closely mimic those seen in the wild such as exposure to a live predator [146-148], a predatory cue [149-152] or psychological stress [153, 154] might have greater ethological relevance, thereby leading to improved modeling and analysis of fear and anxiety states. Stressed rats tend to show PTSD-like behavior such as increased immobility, decreased grooming and rearing [152], decreased exploratory behavior and decreased food consumption [155]. The 'freezing' response has been used as a behavioral measure of anxiety or fear [156]. Amongst all the unconditioned stressors, the predator stress seems to be the most potent stressor, since its effects on fear/anxiety potentiation can last for 3 weeks [147]. Most studies in animal models for PTSD-like behavior refer to the maladapted group as a uniform population. Others developed an animal model that categorizes PTSD-like behavior individually and in addition they applied it to further monitor the animal over a month in order to determine whether it had PTSD-like behavior. This adapted model includes re-exposure to the traumatic cue in a time-course manner, and showed high face-, contract- and predictivevalidities [157]. 1100 Current Drug Targets, 2009, Vol. 10, No. 11 Opioids and Stress-Related Disorders Endogenous opioid peptides and their receptors are represented throughout corticolimbic structures [158, 159] and their high sensitivity to acute and prolonged aversive stimuli has been documented [160-164]. Herein we will summarize their possible role in depression, anxiety and PTSD. (+/-)-Tramadol, an opioidergic- monoaminergic agent, conceivably displays antidepressant actions in a variety of rodent models [165-169], although the precise contribution of monoaminergic as compared to opioidergic mechanisms to its antidepressant properties remains unclear. Since it has a dual mechanism of action by which analgesia may be achieved via -opioid receptor activation, and enhancement of serotonin and norepinephrine transmission may conceivably exert a degree of antidepressant effect and it was suggested to be of particular value in patients with chronic pain who also suffer from depression [170]. Recent literature supports a potent role of methadone, buprenorphine, tramadol, morphine, and other opioids as effective, durable and rapid therapeutic agents for anxiety and depression [171]. Some studies showed that codeine produced an antidepressant-like effect when administered alone and even an accentuated anti-depressant like effect when administrated at subeffective doses in combination with selective serotonin reuptake inhibitors (fluoxetine or citalopram). In contrast, when codeine was combined with a noradrenaline reuptake inhibitor (desipramine) or with a noradrenaline/serotonin reuptake inhibitor (duloxetine), no such effect was observed. The anti- depressant like effect also remained unchanged with the combination of subeffective doses of codeine and (+/-)-tramadol (the weak -opioid agonist with serotonin/noradrenaline reuptake inhibitor properties) or (-)-tramadol (noradrenaline reuptake inhibitor properties only). Conversely, the combination with (+)tramadol ( -opioid agonist with serotonin reuptake inhibitor properties) produced an increase of the anti-depressant like effect [172]. The existing information indicating the possibility of opioids' neurotransmission in controlling PTSD is mostly circumstantial. Only recently a direct examination of central nervous system opioid function in PTSD was reported, using positron emission tomography (PET) and the selective opioid receptor radiotracer [173] carfentanil. The study separated trauma exposed combat veterans who developed PTSD after combat experience, from trauma exposed combat veterans without PTSD, as well as non-exposed controls indicating changes in -opioid receptor occupancy in limbic forebrain and cortical regions involved in emotional regulation. These alterations are likely to reflect adaptive responses to trauma or stress, or alternatively potential adaptation failures that may be related to PTSD pathophysiology [173]. Another study of acute administration of morphine reported limited fear conditioning in the aftermath of traumatic injury and may serve as a secondary prevention strategy to reduce PTSD development [174]. Involvement of -Endorphin in Depression The results obtained from depressive patients not receiving drug therapy on plasma or CSF -endorphin levels, were Yadid et al. inconsistent [66, 175-179]. Later, using microdialysis, it was enabled to determine of the local release of -endorphin in specific brain regions in vivo. This may lead to a more accurate understanding of the neurophysiological basis of behavioral abnormalities in depression, and the mode of action of drugs used for treating them. The neuronal mechanisms that mediate the beneficial effect of several antidepressants on depressive behavior [180] are not known, but may involve the 5-HT- -endorphin interaction in NAcc and ArN, since some findings [35] demonstrate that extracellular endorphin levels in these areas are altered in response to 5HT. Antidepressants, such as tricyclics and SSRIs, increase 5-HT neurotransmission in the brain [181]. Therefore, this increase in 5-HT neurotransmission should facilitate the release of -endorphin in brain regions, such as the abovementioned, where this opiate can mediate hedonia or motivation [19, 22, 35]. Extracellular levels of -endorphin in the NAcc, as well as behavioral deficiencies associated with depressive behavior, were assessed in and animal model of depression and control rats, before and after chronic antidepressant treatment. Using microdialysis, [35] it was demonstrated that extracellular -endorphin levels were dose dependently increased when artificial cerebrospinal fluid (aCSF) containing 5-HT was applied to the NAcc (Fig. 2). This response was attenuated in FSL rats showing a shift to the right in the dose-response curve [208](Fig. 3). In FSL rats exposed to the same 5-HT treatment, the -endorphin levels increased only slightly, but not significantly. Chronic treatment (18 days) with desipramine or paroxetine did not significantly affect the basal levels of -endorphin in the dialysates obtained from the NAcc of FSL or control Sprague-Dawley rats. However, in FSL rats treated with desipramine or paroxetine, exogenous administration of 5-HT via the microdialysis probe induces increases in extracellular levels of -endorphin, similar to those observed in controls (Fig. 4). In FSL rats chronically injected with saline, exogenous application of 5-HT appeared to slightly affect -endorphin release. However, this 5-HT-mediated effect was minimal compared to that observed in the FSL rats treated with the antidepressants. 5-HT-mediated release of -endorphin in the control Sprague-Dawley rats was not significantly affected by chronic administration of saline or the antidepressants [208]. The basic characteristic symptoms of depressed patients are anhedonia and a lack of motivation, both of which are expressed in the absence of an immediate response to environmental stimuli [182]. Responses to environmental stimuli that activate specific neuronal circuits in the brain involved in mediation of motivation or hedonia (and are likely to involve release of -endorphin) are probably impaired in depressive patients [183]. Chronic, but not acute, treatment with antidepressant drugs, which is necessary for effective treatment of depressive behavior [136] normalizes the 5-HT- - endorphin interaction, probably by affecting neuronal plasticity [184]. Injection of -endorphin into the brain has also rewarding effects [24, 29] and impairment of the reward system was suggested to occur in depression [185]. Therefore a complementary way to address -endorphin role in depression is by its modulating the reward system. -endorphin and strees-related psychiatric disorders Current Drug Targets, 2009, Vol. 10, No. 11 1101 Fig. (2). Increments of -endorphin levels in extracellular fluid of nucleus accumbens in response to exogenous serotonin. Rats were implanted with a microdialysis probe (2 mm length, 20 kDa cutoff value, CMA/10; Carnegie Medicine; Stockholm, Sweden) in their nucleolus accumbens using the Paxinos & Watson the rat brain in stereotaxic coordinates [207]. Artificial cerebrospinal fluid (aCSF; 145 mM NaCl, 1.2 mM CaCl2, 2.7 mM KCl, 1.0 mM MgCl2, pH 7.4) was pumped continuously (1.5 l/min) through the dialysis probe using a microinjection pump (CMA/400, Carnegie Medicine). Experiments were initiated 24 h after surgery in awake, freely moving rats. After collecting baseline, various concentrations of 5-HT were applied locally via the probe for 30 min. Data are mean ± SEM values from six rats. Two-way ANOVA with repeated measurements was conducted. *p<0.001 compared with basal levels by Student–Newman–Keuls post hoc test [35]. Fig. (3). Attenuated effect of exogenously added 5-HT on the extracellular levels of -endorphin in the nucleus accumbens of an animal model of depression (FSL) rats. FSL and Sprague–Dawley (control) rats were implanted with a microdialysis probe in their nucleolus accumbens. The microdialysis probe was perfused with aCSF before and after a 30 min perfusion with aCSF containing 5-HT (bar). (A) A dose–response curve when the peak of the response to each 5-HT concentration (mean±S.E.M. values of five rats in each group) was plotted. ANOVA with repeated measure over time applied to each 5-HT dose separately revealed that only at the 5 M 5-HT (B) a significant strain– sample interaction was obtained (control group: F(4,8)=7.78, P<0.001); FSL group: F(4,8)=1.22, P=0.31), strain x treatment interaction (F(1,8)=2.34, P=0.028). *P<0.05 [208]. 1102 Current Drug Targets, 2009, Vol. 10, No. 11 Yadid et al. Fig. (4). Effect 5-HT-induced release of -endorphin in the nucleus accumbens of FSL and Sprague–Dawley (control) rats. FSL and Sprague–Dawley (control) rats were treated with saline or antidepressants (paroxetine or desipramine) for two weeks. Thereafter they were implanted with a microdialysis probe in their nucleolus accumbens. The microdialysis probe was perfused with aCSF before and after a 30 min perfusion with aCSF containing 5 M 5-HT. The pick of the stimulation in the various groups after 5HT administration is demonstrated. Mean±S.E.M. values of five or six rats in each group are presented [208]. It is worth to mention that Tramadol, an opioidergic monoaminergic (NA and 5-HT re-uptake inhibitor) agent displays antidepressant actions in a variety of rodent models [165-169], although the precise contribution of monoaminergic as compared to opioidergic mechanisms to the antidepressant properties of tramadol remains unclear. We suggest that impaired 5-HT-induced release of endorphin may be involved in the etiology of depression, and that normalization of this induction by chronic antidepressant treatments mediate, at least in part, the therapeutic action of antidepressant drugs. Involvement of -Endorphin in Anxiety The role of neuropeptides in general and -endorphin in particular in anxiety-related disorders is largely unknown. In humans, acute stress, which is associated with higher anxiety levels, had increased plasma levels of -endorphin [186]. In animal studies, mice with selective deletion of -endorphin demonstrated lower anxiety levels in the zero-maze, a model for a mildly stressful situation [187]. Several others studies address the issue of alcohol-withdrawal induced anxiety and its possible connection to -endorphin in both humans and mice. -endorphin plasma levels were significantly lowered on day 1 and day 14 of alcohol withdrawal relative to control subjects and levels of -endorphin were inversely correlated with anxiety levels [188]. In mice, a direct inverse relationship was noted between -endorphin plasma levels and anxi- ety behavior measured using the elevated plus maze, suggesting that this peptide normally inhibits anxious behavior. However, mice lacking -endorphin demonstrated an exaggerated anxiolytic response to alcohol in this assay [189]. Together, these studies suggest that lowered -endorphin may contribute to anxiety-related behaviors. Involvement of -Endorphin in PTSD In animals exposed to a scent of predators, a prolonged 25% increase in of -endorphin in the ArcN was observed [190]. Exposure to stress enhances release of the endogenous opioid receptor, dynorphin, in several cerebral structures, including the hippocampus and nucleus accumbens [162, 163, 191-193]. An earlier report found lower plasma endorphins in PTSD patients [194], however later findings [195, 196] suggested higher levels of immunoreactive endorphins. Treatment with the opioid antagonists nalmefene and naltrexone has reduced PTSD symptoms like flashbacks and dissociations, intrusions, and hyperarousal [89, 197, 198], whereas activation of opioid receptors by morphine reduced the risk of subsequent development of PTSD symptoms [199]. Only one study directly examined the role of the central nervous system opioid function in PTSD [173]. However, a direct evidence for a specific opiate involvement in PTSD was only recently available by the use of microdialysis and a unique animal model of PTSD. A recent study has measured -endorphin levels both in tissue and in -endorphin and strees-related psychiatric disorders the extra cellular fluid in the amygdala. Table 1 demonstrates the basal levels of tissue content. PTSD rats demonstrated a significant lower concentration of -endorphin then the nonPTSD rats and the naive rats. When extracellular fluid was sampled by microdialysis in freely moving rat during reexposure the traumatic remainder only (without cat scent), the PTSD rat had increased the extraßcellular -endorphin which remained high for two hours post re-exposure to the cue associated with the traumatic event (Fig 5). This may indicate that the mechanism underlying heighten behavioral reaction to the traumatic cue involve inability to maintain a threshold of basal -endorphin release. Hence, -endorphin levels may increase in order to moderate the distress reaction. Massive extracellular release of the -endorphin may further lead to depletion of its cellular storage. Despite the increase in the extracellular fluid -endorphin levels in the amygdala, they did not reach the basal levels of control rats, but they approximate the basal extra cellular fluid endorphin level of non-PTSD rats. These findings support Grisel et al. finding that -endorphin have a significant role in moderating anxiety. Inability to increase -endorphin levels in PTSD might explain the behavioral symptoms of trauma re-experiencing. -Endorphin and Memory The process of learning and memory is obviously involved is stress-related disorders. An involvement of - Current Drug Targets, 2009, Vol. 10, No. 11 1103 Table 1: -endorphin content in the amygdala PTSD rats. Rats were prepared as described in Fig 5 [157]. After separating maladapted (PTSD) from non- maladapted (non- PTSD) rats, their brains were removed and -endorphin was assayed [35] in their amygdala. A marked decrease was measured in the PTSD group that exceeded the decrement indicated of non- PTSD group. (*p<0.01 vs naive, **p<0.0 vs non-PTSD, ANOVA) Naive -endorphin ( g/ml) 157.06±38.71 non-PTSD * 75.86±20.7 PTSD **15.32±4.9 endorphin in post-operative memory in the amygdala was suggested [200, 201]. Additionally, retrieval of avoidance learning is modulated by -endorphin and enhanced by naloxone [202]. In humans, opioid receptor blockade, using a single oral dose of naltrexone, may specifically improve incidental recognition memory following physiological arousal [206]. These findings demonstrate that opioid peptides in general, and -endorphin in particular, mediate alterations in specific aspects of human memory during heightened emotional states and that learning-based interventions can create new memories that may modify existing ones [203]. These studies support a role for -endorphin in learning and memory that may be associated with memoryrelated stress disorders. Fig. (5). Extracellular (CSF) -endorphin level in the amygdala in PTSD and non-PTSD rats re-exposed to cue. Rats underwent a stressful procedure (exposure to a predator scent) over eight weeks experiment as described [157]. On the eighth week rats were defined as maladapted (PTSD-like) or non maladapted) non PTSD-like rats. A week after, microdialysis probes were co-implanted into their basolateral amygdala. During microdialysis sampling, rats were re-exposed to a cue (same bedding without a predator scent). Re-exposure to the cue, increased -endorphin concentration in the extracellular fluid of PTSD rats. This increment stayed significantly higher for two hours following the re-exposure (ANOVA for repeated measure revealed significance. *p<0.05 PTSD vs non PTSD). 1104 Current Drug Targets, 2009, Vol. 10, No. 11 CONCLUDING REMARKS AND PERSPECTIVES Current pharmacological treatment for depression is based on the use of drugs that act mainly by enhancing brain serotonin and noradrenaline neurotransmission. Although complete remission of symptoms is the goal of any depression treatment, many patients fail to attain or maintain a long-term, symptom-free status. In view of this, there is an intense search to identify novel targets for antidepressant therapy. Some antidepressants which increase the availability of noradrenaline and serotonin through the inhibition of the reuptake of both monoamines lead to the enhancement of the opioid pathway [204]. Endogenous opioid peptides are co-expressed in brain areas known to play a major role in affective disorders and in the action of antidepressant drugs. Therefore, opioid peptides and their receptors are potential candidates for the development of novel antidepressant treatment. Actually, opioids have been used for centuries to treat a variety of psychiatric conditions with much success but lost popularity in the early 1950s with the development of non-addictive tricyclic antidepressants and monoamine oxidase inhibitors. The combination of monoamine agents with opiod's agents even at subeffective doses may increase the antidepressive and anxiolytic efficacy. Tramadol has dual mechanisms of action by which analgesia may be achieved via -opioid receptor activation, enhancement of serotonin and norepinephrine transmission may conceivably exert a degree of antidepressant effect. Therefore, it was suggested to be of particular value in patients with chronic pain who also suffer from depression [170]. Nonetheless, recent literature supports the potent role of methadone, buprenorphine, tramadol, morphine, and other opioids as effective, durable, and rapid therapeutic agents for anxiety and depression [171]. Some studies showed that codeine produced an antidepressant-like effect when administered alone and even an accentuated anti-depressant like effect when administrated at subeffective doses in combination with selective serotonin reuptake inhibitors (fluoxetine or citalopram)[172]. The existing information indicating the possibility of opioids' neurotransmission in controlling PTSD is far circumstantial [173]. One study, acute administration of morphine, limited fear conditioning in the aftermath of traumatic injury and may serve as a secondary prevention strategy to reduce PTSD development [174]. -endorphin is a potent - and - receptors agonist. It was demonstrated to induce motivation and hedonia, the two main symptoms lacking in depression, and as such may have a role in controlling depressive behavior. -endorphin has also interesting effects on post-operative memory and retrieval of avoidance [205]. In humans, opioid receptor blockade improves incidental recognition memory following physiological arousal, indicating its role in memory during heightened emotional states [206]. This may explain why memories can be selectively modified under stressful events, such as those experienced by PTSD patients. While abuse of opioids may occur, several large studies have demonstrated that the incidence of abuse is rather low, about one case per 100,000 patients [170]. As well, all reported combinations of antidepressants with opioidreceptor's activation were without effects on motor behavior in animal models. Yadid et al. Currently, some evidence supports the possibility of endorphin neurotransmission in controlling depression and PTSD. Therefore, understanding the role of -endorphin in the modulation of the anti-distress and post-operative memory may assist in providing potential therapeutic strategies for the prevention of relapse to depressive state and PTSD. Such treatments may be more efficient compared to currently available treatments. REFERENCES [1] [2] [3] [4] [5] [6] [7] [8] [9] [10] [11] [12] [13] [14] [15] [16] [17] [18] [19] [20] [21] Terenius L, Wahlstro A. Inhibitor(s) of narcotic receptor-binding in brain extracts and cerebrospinal-fluid. Acta Pharmacologica et Toxicologica 1974; 35: 55. Hughes J, Smith TW, Kosterlitz HW, Fothergill LA, Morgan BA, Morris HR. Identification of two related pentapeptides from the brain with potent opiate agonist activity. Nature 1975; 258: 577-80. Goldstein A, Tachibana S, Lowney LI, Hunkapiller M, Hood L. Dynorphin-(1-13), an extraordinarily potent opioid peptide. Proc Natl Acad Sci USA 1979; 76: 6666-70. Goldstein A, Fischli W, Lowney LI, Hunkapiller M, Hood L. Porcine pituitary dynorphin: complete amino acid sequence of the biologically active heptadecapeptide. Proc Natl Acad Sci U S A 1981; 78: 7219-23. Bradbury AF, Smyth DG, Snell CR. Lipotropin: precursor to two biologically active peptides. Biochem Biophys Res Commun 1976; 69: 950-6. van Ree JM. Reinforcing stimulus properties of drugs. Neuropharmacology 1979; 18: 963-9. Goeders NE, Lane JD, Smith JE. Self-administration of methionine enkephalin into the nucleus accumbens. Pharmacol Biochem Behav 1984; 20: 451-5. Belluzzi JD, Stein L. Enkephalin may mediate euphoria and drivereduction reward. Nature 1977; 266: 556-8. Nakanishi S, Inoue A, Kita T, Nakamura M, Chang AC, Cohen SN, et al. Nucleotide sequence of cloned cDNA for bovine corticotropin-beta-lipotropin precursor. Nature 1979; 278: 423-7. Kakidani H, Furutani Y, Takahashi H, Noda M, Morimoto Y, Hirose T, et al. Cloning and sequence analysis of cDNA for porcine beta-neo-endorphin/dynorphin precursor. Nature 1982; 298: 245-9. Comb M, Seeburg PH, Adelman J, Eiden L, Herbert E. Primary structure of the human Met- and Leu-enkephalin precursor and its mRNA. Nature 1982; 295: 663-6. Overview of the Endogenous Opioid Systems: Anatomical, Biochemical and Functional Issues. In: Akil H, Bronstein D, Mansour A, eds. Endorphins Opiates and Behavioral Processes. Wiley: New York 1988. Funkelstein L, Toneff T, Mosier C, Hwang SR, Beuschlein F, Lichtenauer UD, et al. Major role of cathepsin L for producing the peptide hormones ACTH, beta-endorphin, and alpha-MSH, illustrated by protease gene knockout and expression. J Biol Chem 2008; 283: 35652-9. Berczi I, Chalmers IM, Nagy E, Warrington RJ. The immune effects of neuropeptides. Baillieres Clin Rheumatol 1996; 10: 227-57. Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annu Rev Physiol 2005; 67: 259-84. Dalayeun JF, Nores JM, Bergal S. Physiology of beta-endorphins. A close-up view and a review of the literature. Biomed Pharmacother 1993; 47: 311-20. Zakarian S, Smyth DG. beta-Endorphin is processed differently in specific regions of rat pituitary and brain. Nature 1982; 296: 250-2. Bloom FE, Rossier J, Battenberg EL, Bayon A, French E, Henriksen SJ, et al. beta-endorphin: cellular localization, electrophysiological and behavioral effects. Adv Biochem Psychopharmacol 1978; 18: 89-109. Tseng LF, Wang Q. Forebrain sites differentially sensitive to betaendorphin and morphine for analgesia and release of Metenkephalin in the pentobarbital-anesthesized rat. J Pharmacol Exp Ther 1992; 261: 1028-36. Loh HH, Tseng LF, Wei E, Li CH. beta-endorphin is a potent analgesic agent. Proc Natl Acad Sci U S A 1976; 73: 2895-8. Foley KM, Kourides IA, Inturrisi CE, Kaiko RF, Zaroulis CG, Posner JB, et al. beta-Endorphin: analgesic and hormonal effects in humans. Proc Natl Acad Sci U S A 1979; 76: 5377-81. -endorphin and strees-related psychiatric disorders [22] [23] [24] [25] [26] [27] [28] [29] [30] [31] [32] [33] [34] [35] [36] [37] [38] [39] [40] [41] [42] [43] [44] [45] [46] Bloom F, Segal D, Ling N, Guillemin R. Endorphins: profound behavioral effects in rats suggest new etiological factors in mental illness. Science 1976; 194: 630-2. Kreek MJ. Effects of opiates, opioid antagonists and cocaine on the endogenous opioid system: clinical and laboratory studies. NIDA Res Monogr 1992; 119: 44-8. Roth-Deri I, Green-Sadan T, Yadid G. Beta-endorphin and druginduced reward and reinforcement. Prog Neurobiol 2008; 86: 1-21. Van Ree JM, Niesink RJ, Van Wolfswinkel L, Ramsey NF, Kornet MM, Van Furth WR, et al. Endogenous opioids and reward. Eur J Pharmacol 2000; 405: 89-101. De Vries TJ, Shippenberg TS. Neural systems underlying opiate addiction. J Neurosci 2002; 22: 3321-5. Di Chiara G, North RA. Neurobiology of opiate abuse. Trends Pharmacol Sci 1992; 13: 185-93. Spanagel R, Herz A, Bals-Kubik R, Shippenberg TS. Betaendorphin-induced locomotor stimulation and reinforcement are associated with an increase in dopamine release in the nucleus accumbens. Psychopharmacology (Berl) 1991; 104: 51-6. Doron R, Fridman L, Yadid G. Dopamine-2 receptors in the arcuate nucleus modulate cocaine-seeking behavior. Neuroreport 2006; 17: 1633-6. Simmons D, Self DW. Role of Mu- and Delta-Opioid receptors in the nucleus accumbens in cocaine-seeking behavior. Neuropsychopharmacology 2009; 34: 1946-57. Churchill L, Roques BP, Kalivas PW. Dopamine depletion augments endogenous opioid-induced locomotion in the nucleus accumbens using both mu 1 and delta opioid receptors. Psychopharmacology (Berl) 1995; 120: 347-55. Stinus L, Cador M, Le Moal M. Interaction between endogenous opioids and dopamine within the nucleus accumbens. Ann N Y Acad Sci 1992; 654: 254-73. Roth-Deri I, Zangen A, Aleli M, Goelman RG, Pelled G, Nakash R, et al. Effect of experimenter-delivered and self-administered cocaine on extracellular beta-endorphin levels in the nucleus accumbens. J Neurochem 2003; 84: 930-8. Yadid G, Friedman A. Dynamics of the dopaminergic system as a key component to the understanding of depression. Prog Brain Res 2008; 172: 265-86. Zangen A, Nakash R, Yadid G. Serotonin-mediated increases in the extracellular levels of beta-endorphin in the arcuate nucleus and nucleus accumbens: a microdialysis study. J Neurochem 1999; 73: 2569-74. Anwer J, Soliman MR. Ethanol-induced alterations in betaendorphin levels in specific rat brain regions: modulation by adenosine agonist and antagonist. Pharmacology 1995; 51: 364-9. Tekes K, Gyenge M, Hantos M, Csaba G. Effect of beta-endorphin imprinting during late pregnancy on the brain serotonin and plasma nocistatin levels of adult male rats. Horm Metab Res 2007; 39: 479-81. Martin WR. Opioid antagonists. Pharmacol Rev 1967; 19: 463-521. Zhang Y, Pan YX, Kolesnikov Y, Pasternak GW. Immunohistochemical labeling of the mu opioid receptor carboxy terminal splice variant mMOR-1B4 in the mouse central nervous system. Brain Res 2006; 1099: 33-43. Tao R, Auerbach SB. mu-Opioids disinhibit and kappa-opioids inhibit serotonin efflux in the dorsal raphe nucleus. Brain Res 2005; 1049: 70-9. Gaveriaux-Ruff C, Kieffer BL. Opioid receptor genes inactivated in mice: the highlights. Neuropeptides 2002; 36: 62-71. Kieffer BL, Gaveriaux-Ruff C. Exploring the opioid system by gene knockout. Prog Neurobiol 2002; 66: 285-306. Simonin F, Valverde O, Smadja C, Slowe S, Kitchen I, Dierich A, et al. Disruption of the kappa-opioid receptor gene in mice enhances sensitivity to chemical visceral pain, impairs pharmacological actions of the selective kappa-agonist U-50,488H and attenuates morphine withdrawal. EMBO J 1998; 17: 886-97. Slugg RM, Hayward MD, Ronnekleiv OK, Low MJ, Kelly MJ. Effect of the mu-opioid agonist DAMGO on medial basal hypothalamic neurons in beta-endorphin knockout mice. Neuroendocrinology 2000; 72: 208-17. Hayward MD, Pintar JE, Low MJ. Selective reward deficit in mice lacking beta-endorphin and enkephalin. J Neurosci 2002; 22: 82518. Biegler P. Autonomy, stress, and treatment of depression. BMJ 2008; 336: 1046-8. Current Drug Targets, 2009, Vol. 10, No. 11 1105 [47] [48] [49] [50] [51] [52] [53] [54] [55] [56] [57] [58] [59] [60] [61] [62] [63] [64] [65] [66] [67] [68] [69] [70] [71] Danese A. Genetic opportunities for psychiatric epidemiology: on life stress and depression. Epidemiol Psichiatr Soc 2008; 17: 20110. El Hage W, Powell JF, Surguladze SA. Vulnerability to depression: what is the role of stress genes in gene x environment interaction? Psychol Med 2009; 39: 1407-11. Miura H, Ozaki N, Sawada M, Isobe K, Ohta T, Nagatsu T. A link between stress and depression: shifts in the balance between the kynurenine and serotonin pathways of tryptophan metabolism and the etiology and pathophysiology of depression. Stress 2008; 11: 198-209. Medvedev A, Igosheva N, Crumeyrolle-Arias M, Glover V. Isatin: role in stress and anxiety. Stress 2005; 8: 175-83. Shekhar A, Truitt W, Rainnie D, Sajdyk T. Role of stress, corticotrophin releasing factor (CRF) and amygdala plasticity in chronic anxiety. Stress 2005; 8: 209-19. Pintor L, Torres X, Navarro V, Martinez de Osaba MA, Matrai S, Gasto C. Corticotropin-releasing factor test in melancholic patients in depressed state versus recovery: a comparative study. Prog Neuropsychopharmacol Biol Psychiatry 2007; 31: 1027-33. Nikolarakis KE, Almeida OF, Herz A. Stimulation of hypothalamic beta-endorphin and dynorphin release by corticotropin-releasing factor (in vitro). Brain Res 1986; 399: 152-5. Bakish D. New standard of depression treatment: remission and full recovery. J Clin Psychiatry 2001; 26: 5-9. Weissman MM, Leaf PJ, Tischler GL, Blazer DG, Karno M, Bruce ML, Florio LP. Effective disorders in five United States communities. A Psychol Med 1988; 18: 141-53. Angst J. Epidemiology of depression. Psychopharmacology (Berl) 1992; 106 Suppl: S71-4. Whybrow PG, Akiskal HS, McKinney WT. Mood Disorders: Toward a New Psychobiology. Plenum Press: New York 1984. von Knorring L, Perris C, Eisemann M, Eriksson U, Perris H. Pain as a symptom in depressive disorders. part II: relationship to personality traits as assessed by means of KSP. Pain 1983; 17: 377-84. von Knorring L, Perris C, Oreland L, Eisemann M, Eriksson UPH. Pain as a symptom in depressive disorders and its relationship to platelet monoamine oxidase activity. J Neural Transm 1984; 60: 19. Meltzer HY, Lowy MT. The serotonin hypothesis of depression. In: Meltzer HY, Lowy MT, eds. Psychopharmacology: The Third Generation of Progress. Raven: New York 1987; pp. 513-26. Maes M, Meltzer HY. The Serotonin Hypothesis of Major Depression. In: Bloom FE, Kupfer DJ, eds. Psychopharmacology The Fourth Generation of Progress. Raven; New York 1995; pp. 93344. Stokes PE, Pick GR, Stoll PM, Nunn WD. Pituitary-adrenal function in depressed patients: resistance to dexamethasone suppression. J Psychiatr Res 1975; 12: 271-81. Janowsky DS, Risch SC, Ziegler M, Kennedy B, Huey L. A cholinomimetic model of motion sickness and space adaptation syndrome. A t Space Environ Med 1984; 55: 692-6. Janowsky DS, Risch C, Parker D, Huey L, Judd L. Increased vulnerability to cholinergic stimulation in affective-disorder patients [proceedings]. Psychopharmacol Bull 1980; 16: 29-31. Janowsky DS, Overstreet DH. The cholinergic hypothesis of depression. Psychopharmacology: The Fourth Generation of Progress. Raven: New York 1995; pp. 944-57. Risch SC. beta-Endorphin hypersecretion in depression: possible cholinergic mechanisms. Biol Psychiatry 1982; 17: 1071-9. Gershon ES, Berrettini W, Nurnberger JI, Goldin LR. Genetics of afective illness. In: Meltzer HYE, Ed. Psychopharmacology: The Third Generation of Progress. New York: Raven; 1987: 481-92. Bauer M, Adli M, Baethge C, Berghofer A, Sasse J, Heinz A, et al. Lithium augmentation therapy in refractory depression: clinical evidence and neurobiological mechanisms. Can J Psychiatry 2003; 48: 440-8. Bschor T, Bauer M. Efficacy and mechanisms of action of lithium augmentation in refractory major depression. Curr Pharm Des 2006; 12: 2985-92. Owens MJ. Selectivity of antidepressants: from the monoamine hypothesis of depression to the SSRI revolution and beyond. J Clin Psychiatry 2004; 65: 5-10. Taylor MJ, Freemantle N, Geddes JR, Bhagwagar Z. Early onset of selective serotonin reuptake inhibitor antidepressant action: sys- 1106 Current Drug Targets, 2009, Vol. 10, No. 11 [72] [73] [74] [75] [76] [77] [78] [79] [80] [81] [82] [83] [84] [85] [86] [87] [88] [89] [90] [91] [92] [93] [94] [95] [96] [97] tematic review and meta-analysis. Arch Gen Psychiatry 2006; 63: 1217-23. Cooper-Kazaz R, Apter JT, Cohen R, Karagichev L, MuhammedMoussa S, Grupper D, et al. Combined treatment with sertraline and liothyronine in major depression: a randomized, double-blind, placebo-controlled trial. Arch Gen Psychiatry 2007; 64: 679-88. Olver JS, Burrows GD, Norman TR. Third-generation antidepressants: do they offer advantages over the SSRIs? CNS Drugs 2001; 15: 941-54. Watanabe N, Omori IM, Nakagawa A, Cipriani A, Barbui C, McGuire H, et al. Mirtazapine versus other antidepressants in the acute-phase treatment of adults with major depression: systematic review and meta-analysis. J Clin Psychiatry 2008; 69: 1404-15. Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments metaanalysis. Lancet 2009; 373: 746-58. Montgomery SA, Baldwin DS, Blier P, Fineberg NA, Kasper S, Lader M, et al. Which antidepressants have demonstrated superior efficacy? A review of the evidence. Int Clin Psychopharmacol 2007; 22: 323-9. Irons J. Fluvoxamine in the treatment of anxiety disorders. Neuropsychiatr Dis Treat 2005; 1: 289-99. Robert S, Hamner MB, Ulmer HG, Lorberbaum JP, Durkalski VL. Open-label trial of escitalopram in the treatment of posttraumatic stress disorder. J Clin Psychiatry 2006; 67: 1522-6. Davidson JR, Stein DJ, Shalev AY, Yehuda R. Posttraumatic stress disorder: acquisition, recognition, course, and treatment. J Neuropsychiatry Clin Neurosci 2004; 16: 135-47. DSM. Diagnostic and Statistical Manual of Mental Disorders (DSM IV). American Psychiatric Press: Washington, D.C. 1994. Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991: 216-22. Jang KL, Stein MB, Taylor S, Asmundson GJ, Livesley WJ. Exposure to traumatic events and experiences: aetiological relationships with personality function. Psychiatry Res 2003; 120: 61-9. Schoenfeld FB, Marmar CR, Neylan TC. Current concepts in pharmacotherapy for posttraumatic stress disorder. Psychiatr Serv 2004; 55: 519-31. Nutt D DJ, ed. Post-Traumatic Stress Disorder Diagnosis, Management and Treatment. Taylor & Francis: London 2000. Davidson JR, Stein DJ, Shalev AY, Yehuda RJ. Posttraumatic stress disorder: acquisition, recognition, course, and treatment. Neuropsychiatry Clin Neurosci 2004; 16: 135-47. Van Der Kolk BA. The psychobiology and psychopharmacology of PTSD. Hum Psychopharmacol 2001; 16: S49-64. Tang SW, Helmeste D. Paroxetine. Expert Opin Pharmacother 2008; 9: 787-94. Liebert R, Gavey N. "There are always two sides to these things" Managing the dilemma of serious adverse effects from SSRIs. Soc Sci Med 2009; 68: 1882-91. Glover H. A preliminary trial of nalmefene for the treatment of emotional numbing in combat veterans with post-traumatic stress disorder. Isr J Psychiatry Relat Sci 1993; 30: 255-63. Rauch SL. A symptom provocation study of posttraumatic stress disorder using positron emission tomography and script-driven imagery. Arch Gen Psychiatry 1996; 53: 380-7. Rauch SL. Exaggerated amygdala response to masked facial stimuli in posttraumatic stress disorder: a functional MRI study. Biol Psychiatry 2000; 47: 769-76. Koenigs M, Huey ED, Raymont V, Cheon B, Solomon J, Wassermann EM, et al. Focal brain damage protects against post-traumatic stress disorder in combat veterans. Nat Neurosci 2008; 11: 232-7. Bloom FE, Kupfer DJ. Psychopharmacology: The Fourth Generation of Progress. Raven Press: New York 1995. Clement Y, Calatayud F, Belzung C. Genetic basis of anxiety-like behaviour: a critical review. Brain Res Bull 2002; 57: 57-71. Horowitz ZP. Elective block or rat mouse killing by antidepressants. Life Sci 1965; 4: 1909-12. Ueki S. Mouse-killing behaviour (muricide) in the rat and the effect of antidepressants. In: Langer SZ, Takahashi R, Segawa T, Briley M, ed. New Vistas in Depression. Pergamon Press; New York 1982; pp. 187-94. Malick JB. Yohimbine potentiation as a predictor of antidepressant action. In: Enna SJ, Malick JB, Richelson E, eds. Anti- Yadid et al. [98] [99] [100] [101] [102] [103] [104] [105] [106] [107] [108] [109] [110] [111] [112] [113] [114] [115] [116] [117] [118] [119] [120] [121] depressants: Neurochemical, Behavioral and Clinical Perspectives. New York: Raven; 1981: 141-55. Quinton RM. The increase in the toxicity of yohimbine induced by imipramine and other drugs in mice. Br J Pharmacol Chemother 1963; 21: 51-66. Babington RG. Antidepressives and the kindling effect. In: Fielding S, Lal H, eds. Antidepressants. Futura, Mount Kisco: New York 1975; pp. 113-24. Babington RG, Wedeking PW. The pharmacology of seizures induced by sensitization with low intensity brain stimulation. Pharmacol Biochem Behav 1973; 1: 461-7. Goddard GV, McIntyre DC, Leech CK. A permanent change in brain function resulting from daily electrical stimulation. Exp Neurol 1969; 25: 295-330. Everett GM. The DOPA response potentiation test and its use in screening for antidepressant drugs. In: Garattini S, Dukes MNG, eds. Antidepressant drug Amsterdam. Excerpta Medica: Amsterdam 1967; pp. 164-7. Sigg EB, Hill RT. The effect of imipramine on central adrenergic mechanisms. . In: Brill H, ed. Neuro-psycho-phar-macology. Excerpta Medica: Amsterdam 1967; pp. 367-72. Nagayama H, Hingtgen JN, Aprison MH. Pre- and postsynaptic serotonergic manipulations in an animal model of depression. Pharmacol Biochem Behav 1980; 13: 575-9. Nagayama H, Hingtgen JN, Aprison MH. Postsynaptic action by four antidepressive drugs in an animal model of depression. Pharmacol Biochem Behav 1981; 15: 125-30. Cairncross KD, Wren A, Cox B, Schnieden H. Effects of olfactory bulbectomy and domicile on stress-induced corticosterone release in the rat. Physiol Behav 1977; 19: 485-7. Cairncross KD, Cox B. A new model for the detection of antidepressant drugs: Olfactory bulbectomy in the rat compared with existing models. J Pharmacol Methods 1978: 131-43. Cairncross KD, Cox B, Forster C, Wren AF. Olfactory projection systems, drugs and behaviour: a review. Psychoneuroendocrinology 1979; 4: 253-72. Einon D, Morgan MJ, Sahakian BJ. The development of intersession habituation and emergence in socially reared and isolated rats. Dev Psychobiol 1975; 8: 553-9. Sahakian BJ, Robbins TW. Isolation-rearing enhances tail pinchinduced oral behavior in rats. Physiol Behav 1977; 18: 53-8. Sahakian BJ, Robbins TW, Morgan MJ, Iversen SD. The effects of psychomotor stimulants on stereotypy and locomotor activity in socially-deprived and control rats. Brain Res 1975; 84: 195-205. Hatotani N, Nomura J. Changes of brain monoamines in the animal model for depression. In: Langer SZ, Takahashi R, Segawa T, Briley M, eds. New Vistas in Depression. Pergamon Press: New York 1982; pp. 65-72. Baltzer V, Weiskrantz, L. Antidepressant agents and reversal of diurnal activity cycles in the rat. Biol Psychiatry 1973; 10: 199209. Porsolt RD, Anton G, Blavet N, Jalfre M. Behavioural despair in rats: a new model sensitive to antidepressant treatments. Eur J Pharmacol 1978; 47: 379-91. Porsolt RD, Bertin A, Jalfre M. Behavioral despair in mice: a primary screening test for antidepressants. Arch Int Pharmacodyn Ther 1977; 229: 327-36. Porsolt RD, Bertin A, Jalfre M. "Behavioural despair" in rats and mice: strain differences and the effects of imipramine. Eur J Pharmacol 1978; 51: 291-4. Porsolt RD, Le Pichon M, Jalfre M. Depression: a new animal model sensitive to antidepressant treatments. Nature 1977; 266: 730-2. Katz RJ. Animal models and human depressive disorders. Neurosci Biobehav Rev 1981; 5: 231-46. Katz RJ, Roth KA, Carroll BJ. Acute and chronic stress effects on open field activity in the rat: implications for a model of depression. Neurosci Biobehav Rev 1981; 5: 247-51. Katz RJ, Sibel M. Animal model of depression: tests of three structurally and pharmacologically novel antidepressant compounds. Pharmacol Biochem Behav 1982; 16: 973-7. Katz RJ, Sibel M. Further analysis of the specificity of a novel animal model of depression--effects of an antihistaminic, antipsychotic and anxiolytic compound. Pharmacol Biochem Behav 1982; 16: 979-82. -endorphin and strees-related psychiatric disorders [122] [123] [124] [125] [126] [127] [128] [129] [130] [131] [132] [133] [134] [135] [136] [137] [138] [139] [140] [141] [142] [143] [144] [145] [146] Kaufman IC, Rosenblum LA. The reaction to separation in infant monkeys: anaclitic depression and conservation-withdrawal. Psychosom Med 1967; 29: 648-75. McKinney WT Jr, Bunney WE Jr. Animal model of depression. I. Review of evidence: implications for research. Arch Gen Psychiatry 1969; 21: 240-8. Hinde RA, Leighton-Shapiro ME, McGinnis L. Effects of various types of separation experience on rhesus monkeys 5 months later. J Child Psychol Psychiatry 1978; 19: 199-211. Klinger E, Barta SG, Kemble ED. Cyclic activity changes during extinction in rats: a potential model of depression. Anim Learn Behav 1974; 2: 313-6. Barrett RJ, White DK. Reward system depression following chronic amphetamine: antagonism by haloperidol. Pharmacol Biochem Behav 1980; 13: 555-9. Kokkinidis L, Zacharko RM. Response sensitization and depression following long-term amphetamine treatment in a selfstimulation paradigm. Psychopharmacology (Berl) 1980; 68: 73-6. Leith NJ, Barrett RJ. Amphetamine and the reward system: evidence for tolerance and post-drug depression. Psychopharmacologia 1976; 46: 19-25. Leith NJ, Barrett RJ. Effects of chronic amphetamine or reserpine on self-stimulation responding: animal model of depression? Psychopharmacology (Berl) 1980; 72: 9-15. Simpson DM, Annau Z. Behavioral withdrawal following several psychoactive drugs. Pharmacol Biochem Behav 1977; 7: 59-64. Maier SF, Seligman ME. Learned helplessness. Theory and evidence. J Exp Psychol 1976; 105: 3-46. Maier SF. Learned helplessness and animal models of depression. Prog Neuropsychopharmacol Biol Psychiatry 1984; 8: 435-46. Willner P. Validity, reliability and utility of the chronic mild stress model of depression: a 10-year review and evaluation. Psychopharmacology (Berl) 1997; 134: 319-29. Weiss JM, Cierpial MA, West CH. Selective breeding of rats for high and low motor activity in a swim test: toward a new animal model of depression. Pharmacol Biochem Behav 1998; 61: 49-66. Overstreet DH. The Flinders sensitive line rats: a genetic animal model of depression. Neurosci Biobehav Rev 1993; 17: 51-68. Overstreet DH, Friedman E, Mathe AA, Yadid G. The Flinders Sensitive Line rat: a selectively bred putative animal model of depression. Neurosci Biobehav Rev 2005; 29: 739-59. Janowsky DS, Overstreet DH, Nurnberger JI Jr. Is cholinergic sensitivity a genetic marker for the affective disorders? Am J Med Genet 1994; 54: 335-44. Nutt D, Davidson JRT, Zohar J, eds. Post-traumatic Stress Disorder Diagnosis, Management and Treatment. Taylor & Francis, A Martin Dunitz Book: London 2000. Garrick T, Morrow N, Shalev AY, Eth S. Stress-induced enhancement of auditory startle: an animal model of posttraumatic stress disorder. Psychiatry 2001; 64: 346-54. Koba T, Kodama Y, Shimizu K, Nomura S, Sugawara M, Kobayashi Y, et al. Persistent behavioural changes in rats following inescapable shock stress: a potential model of posttraumatic stress disorder. World J Biol Psychiatry 2001; 2: 34-7. Pynoos RS, Ritzmann RF, Steinberg AM, Goenjian A, Prisecaru I. A behavioral animal model of posttraumatic stress disorder featuring repeated exposure to situational reminders. Biol Psychiatry 1996; 39: 129-34. Servatius RJ, Ottenweller JE, Natelson BH. Delayed startle sensitization distinguishes rats exposed to one or three stress sessions: further evidence toward an animal model of PTSD. Biol Psychiatry 1995; 38: 539-46. Richter-Levin G. Acute and long-term behavioral correlates of underwater trauma-potential relevance to stress and post-stress syndromes. Psychiatry Res 1998; 79: 73-83. Liberzon I, Krstov M, Young EA. Stress-restress: effects on ACTH and fast feedback. Psychoneuroendocrinology 1997; 22: 443-53. Torres IL, Gamaro GD, Vasconcellos AP, Silveira R, Dalmaz C. Effects of chronic restraint stress on feeding behavior and on monoamine levels in different brain structures in rats. Neurochem Res 2002; 27: 519-25. Adamec RE, Burton P, Shallow T, Budgell J. NMDA receptors mediate lasting increases in anxiety-like behavior produced by the stress of predator exposure--implications for anxiety associated with posttraumatic stress disorder. Physiol Behav 1999; 65: 723-37. Current Drug Targets, 2009, Vol. 10, No. 11 1107 [147] [148] [149] [150] [151] [152] [153] [154] [155] [156] [157] [158] [159] [160] [161] [162] [163] [164] [165] [166] [167] [168] [169] Adamec RE, Shallow T. Lasting effects on rodent anxiety of a single exposure to a cat. Physiol Behav 1993; 54: 101-9. Cohen H, Zohar J, Matar M. The relevance of differential response to trauma in an animal model of posttraumatic stress disorder. Biol Psychiatry 2003; 53: 463-73. Cohen H, Benjamin J, Kaplan Z, Kotler M. Administration of highdose ketoconazole, an inhibitor of steroid synthesis, prevents posttraumatic anxiety in an animal model. Eur Neuropsychopharmacol 2000; 10: 429-35. Cohen H, Kaplan Z, Kotler M. CCK-antagonists in a rat exposed to acute stress: implication for anxiety associated with post-traumatic stress disorder. Depress Anxiety 1999; 10: 8-17. Dielenberg RA, Hunt GE, McGregor IS. "When a rat smells a cat": the distribution of Fos immunoreactivity in rat brain following exposure to a predatory odor. Neuroscience 2001; 104: 1085-97. Morrow BA, Redmond AJ, Roth RH, Elsworth JD. The predator odor, TMT, displays a unique, stress-like pattern of dopaminergic and endocrinological activation in the rat. Brain Res 2000; 864: 146-51. Funada M, Hara C. Differential effects of psychological stress on activation of the 5-hydroxytryptamine- and dopamine-containing neurons in the brain of freely moving rats. Brain Res 2001; 901: 247-51. Makino S, Shibasaki T, Yamauchi N, Nishioka T, Mimoto T, Wakabayashi I, et al. Psychological stress increased corticotropinreleasing hormone mRNA and content in the central nucleus of the amygdala but not in the hypothalamic paraventricular nucleus in the rat. Brain Res 1999; 850: 136-43. Ottenweller JE, Natelson BH, Pitman DL, Drastal SD. Adrenocortical and behavioral responses to repeated stressors: toward an animal model of chronic stress and stress-related mental illness. Biol Psychiatry 1989; 26: 829-41. Feldman RS, Mayer JS, Quenzer LF. Principles of Neuropsychopharmacology. sinauer Associates, Inc.: Sunderland, Massachusetts 1997. Kesner Y, Zohar J, Merenlender A, Gispan I, Shalit F, Yadid G. WFS1 gene as a putative biomarker for development of posttraumatic syndrome in an animal model. Mol Psychiatry 2009; 14: 86-94. Mansour A, Khachaturian H, Lewis ME, Akil H, Watson SJ. Anatomy of CNS opioid receptors. Trends Neurosci 1988; 11: 308-14. Martin-Schild S, Gerall AA, Kastin AJ, Zadina JE. Differential distribution of endomorphin 1- and endomorphin 2-like immunoreactivities in the CNS of the rodent. J Comp Neurol 1999; 405: 45071. Lewis ME, Khachaturian H, Watson SJ. Combined autoradiographic-immunocytochemical analysis of opioid receptors and opioid peptide neuronal systems in brain. Peptides 1985; 6 : 37-47. Mansour A, Fox CA, Akil H, Watson SJ. Opioid-receptor mRNA expression in the rat CNS: anatomical and functional implications. Trends Neurosci 1995; 18: 22-9. Millan MJ. The induction of pain: an integrative review. Prog Neurobiol 1999; 57: 1-164. Millan MJ. Descending control of pain. Prog Neurobiol 2002; 66: 355-474. Nikulina EM, Miczek KA, Hammer RP Jr. Prolonged effects of repeated social defeat stress on mRNA expression and function of mu-opioid receptors in the ventral tegmental area of rats. Neuropsychopharmacology 2005; 30: 1096-103. Hopwood SE, Stamford JA. Multiple 5-HT(1) autoreceptor subtypes govern serotonin release in dorsal and median raphe nuclei. Neuropharmacology 2001; 40: 508-19. Rojas-Corrales MO, Berrocoso E, Gibert-Rahola J, Mico JA. Antidepressant-like effects of tramadol and other central analgesics with activity on monoamines reuptake, in helpless rats. Life Sci 2002; 72: 143-52. Rojas-Corrales MO, Berrocoso E, Gibert-Rahola J, Mico JA. Antidepressant-like effect of tramadol and its enantiomers in reserpinized mice: comparative study with desipramine, fluvoxamine, venlafaxine and opiates. J Psychopharmacol 2004; 18: 404-11. Rojas-Corrales MO, Berrocoso E, Mico JA. Role of 5-HT1A and 5-HT1B receptors in the antinociceptive effect of tramadol. Eur J Pharmacol 2005; 511: 21-6. Rojas-Corrales MO, Gibert-Rahola J, Mico JA. Tramadol induces antidepressant-type effects in mice. Life Sci 1998; 63: PL175-80. 1108 Current Drug Targets, 2009, Vol. 10, No. 11 [170] [171] [172] [173] [174] [175] [176] [177] [178] [179] [180] [181] [182] [183] [184] [185] [186] [187] [188] [189] Yadid et al. Reeves RR, Burke RS. Tramadol: basic pharmacology and emerging concepts. Drugs Today (Barc) 2008; 44: 827-36. Tenore PL. Psychotherapeutic benefits of opioid agonist therapy. J Addict Dis 2008; 27: 49-65. Becker WC, Fiellin DA, Gallagher RM, Barth KS, Ross JT, Oslin DW. The association between chronic pain and prescription drug abuse in Veterans. Pain Med 2009; 10: 531-6. Liberzon I, Taylor SF, Phan KL, Britton JC, Fig LM, Bueller JA, et al. Altered central micro-opioid receptor binding after psychological trauma. Biol Psychiatry 2007; 61: 1030-8. Bryant RA, Creamer M, O'Donnell M, Silove D, McFarlane AC. A study of the protective function of acute morphine administration on subsequent posttraumatic stress disorder. Biol Psychiatry 2009; 65: 438-40. Darko DF, Risch SC, Gillin JC, Golshan S. Association of betaendorphin with specific clinical symptoms of depression. Am J Psychiatry 1992; 149: 1162-7. France RD, Urban BJ. Cerebrospinal fluid concentrations of betaendorphin in chronic low back pain patients. Influence of depression and treatment. Psychosomatics 1991; 32: 72-7. Goodwin GM, Austin MP, Curran SM, Ross M, Murray C, Prentice N, et al. The elevation of plasma beta-endorphin levels in major depression. J Affect Disord 1993; 29: 281-9. Naber D, Pickar D, Post RM, Van Kammen DP, Waters RN, Ballenger JC, et al. Endogenous opioid activity and beta-endorphin immunoreactivity in CSF of psychiatric patients and normal volunteers. Am J Psychiatry 1981; 138: 1457-62. Young EA, Watson SJ, Kotun J, Haskett RF, Grunhaus L, MurphyWeinberg V, et al. Beta-lipotropin-beta-endorphin response to lowdose ovine corticotropin releasing factor in endogenous depression. Preliminary studies. Arch Gen Psychiatry 1990; 47: 449-57. Ward NG, Bloom VL, Friedel RO. The effectiveness of tricyclic antidepressants in the treatment of coexisting pain and depression. Pain 1979; 7: 331-41. Blier P, de Montigny C. Current advances and trends in the treatment of depression. Trends Pharmacol Sci 1994; 15: 220-6. Yadid G, Overstreet DH, Zangen A. Limbic dopaminergic adaptation to a stressful stimulus in a rat model of depression. Brain Res 2001; 896: 43-7. Yadid G, Zangen A, Herzberg U, Nakash R, Sagen J. Alterations in endogenous brain beta-endorphin release by adrenal medullary transplants in the spinal cord. Neuropsychopharmacology 2000; 23: 709-16. Nestler EJ, Terwilliger RZ, Duman RS. Regulation of endogenous ADP-ribosylation by acute and chronic lithium in rat brain. J Neurochem 1995; 64: 2319-24. Fagergren P, Overstreet DH, Goiny M, Hurd YL. Blunted response to cocaine in the Flinders hypercholinergic animal model of depression. Neuroscience 2005; 132: 1159-71 Schedlowski M, Fluge T, Richter S, Tewes U, Schmidt RE, Wagner TO. Beta-endorphin, but not substance-P, is increased by acute stress in humans. Psychoneuroendocrinology 1995; 20: 103-10. Bilkei-Gorzo A, Racz I, Michel K, Mauer D, Zimmer A, Klingmuller D. Control of hormonal stress reactivity by the endogenous opioid system. Psychoneuroendocrinology 2008; 33: 425-36. Kiefer F, Horntrich M, Jahn H, Wiedemann K. Is withdrawalinduced anxiety in alcoholism based on beta-endorphin deficiency? Psychopharmacology (Berl) 2002; 162: 433-7. Grisel JE, Bartels JL, Allen SA, Turgeon VL. Influence of betaEndorphin on anxious behavior in mice: interaction with EtOH. Psychopharmacology (Berl) 2008; 200: 105-15. Received: April 5, 2009 [190] [191] [192] [193] [194] [195] [196] [197] [198] [199] [200] [201] [202] [203] [204] [205] [206] [207] [208] Revised: June 11, 2009 Marinelli PW, Quirion R, Gianoulakis C. An in vivo profile of betaendorphin release in the arcuate nucleus and nucleus accumbens following exposure to stress or alcohol. Neuroscience 2004; 127: 777-84. McLaughlin JP, Marton-Popovici M, Chavkin C. Kappa opioid receptor antagonism and prodynorphin gene disruption block stress-induced behavioral responses. J Neurosci 2003; 23: 5674-83. Millan MJ. The neurobiology and control of anxious states. Prog Neurobiol 2003; 70: 83-244. Shirayama Y, Ishida H, Iwata M, Hazama GI, Kawahara R, Duman RS. Stress increases dynorphin immunoreactivity in limbic brain regions and dynorphin antagonism produces antidepressant-like effects. J Neurochem 2004; 90: 1258-68. Hoffman L, Burges Watson P, Wilson G, Montgomery J. Low plasma beta-endorphin in post-traumatic stress disorder. Aust N Z J Psychiatry 1989; 23: 269-73. Hamner MB, Hitri A. Plasma beta-endorphin levels in posttraumatic stress disorder: a preliminary report on response to exercise-induced stress. J Neuropsychiatry Clin Neurosci 1992; 4: 5963. Kellner M, Baker DG, Yehuda R. Salivary cortisol and PTSD symptoms in Persian Gulf War combatants. Ann N Y Acad Sci 1997; 821: 442-3. Bills LJ, Kreisler K. Treatment of flashbacks with naltrexone. Am J Psychiatry 1993; 150: 1430. Lubin G, Weizman A, Shmushkevitz M, Valevski A. Short-term treatment of post-traumatic stress disorder with naltrexone: an open-label preliminary study. Hum Psychopharmacol 2002; 17: 181-5. Saxe G, Stoddard F, Courtney D, Cunningham K, Chawla N, Sheridan R, et al. Relationship between acute morphine and the course of PTSD in children with burns. J Am Acad Child Adolesc Psychiatry 2001; 40: 915-21. Introini-Collison IB, Ford L, McGaugh JL. Memory impairment induced by intraamygdala beta-endorphin is mediated by noradrenergic influences. Neurobiol Learn Mem 1995; 63: 200-5. McGaugh JL, Introini-Collison IB, Cahill LF, Castellano C, Dalmaz C, Parent MB, et al. Neuromodulatory systems and memory storage: role of the amygdala. Behav Brain Res 1993; 58: 81-90. Barros DM, Izquierdo LA, Medina JH, Izquierdo I. Pharmacological findings contribute to the understanding of the main physiological mechanisms of memory retrieval. Curr Drug Targets CNS Neurol Disord 2003; 2: 81-94. Tryon WW, McKay D. Memory modification as an outcome variable in anxiety disorder treatment. J Anxiety Disord 2009; 23: 54656. Berrocoso E, Sanchez-Blazquez P, Garzon J, Mico JA. Opiates as antidepressants. Curr Pharm Des 2009; 15: 1612-22. Quevedo J, Moretto A, Colvero M, Roesler R, Ferreira MB. The Nmethyl-D-aspartate receptor blocker MK-801 prevents the facilitatory effects of naloxone and epinephrine on retention of inhibitory avoidance task in rats. Behav Pharmacol 1997; 8: 471-4. Katzen-Perez KR, Jacobs DW, Lincoln A, Ellis RJ. Opioid blockade improves human recognition memory following physiological arousal. Pharmacol Biochem Behav 2001; 70: 77-84. Paxinos and Watson G. The Rat Brain in Stereotaxic Coordinates. 4th ed. Diego S, wed. Academic Press; San Diego 1998. Zangen A, Nakash R, Roth-Deri I, Overstreet DH, Yadid G. Impaired release of beta-endorphin in response to serotonin in a rat model of depression. Neuroscience 2002; 110: 389-93. Accepted: June 23, 2009 Copyright of Current Drug Targets is the property of Bentham Science Publishers Ltd. and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.