Epilepsy 101: Getting Started American Epilepsy Society 1
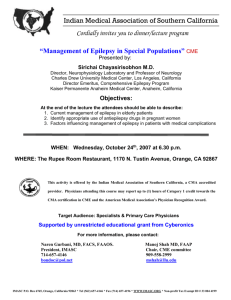
advertisement

Epilepsy 101: Getting Started American Epilepsy Society 1 Epilepsy 101: Getting Started Epilepsy 101 for nurses has been developed by the American Epilepsy Society to prepare professional nurses to understand the general issues, concerns and needs of people with epilepsy, and help them care for people with epilepsy in the general hospital and various community settings. Epilepsy 101 can also be used as an introductory level of learning about epilepsy for neurology nurses caring for people with epilepsy and seizures. American Epilepsy Society 2 Epilepsy 101: Getting Started Epilepsy 101 has 4 learning modules that include the Basics of Epilepsy, Recognition and Care of Seizures and Emergencies, an Overview of Treatment Options, and Patient Education and Self‐Management Approaches. Participants may listen to audio synced to the powerpoint presentation or download the modules and notes in a PDF format. American Epilepsy Society 3 Epilepsy 101: Getting Started Upon completing Module One, the participant will be able to: Describe the role of nursing in epilepsy care. Review common causes and consequences of seizures. Define the spectrum of nursing care for people with epilepsy. American Epilepsy Society 4 People with epilepsy come in contact with nurses in many diverse settings along the health care continuum. These nurses come from a variety of backgrounds and may have varied educational and clinical expertise. The nurse‐patient relationship will vary based on the care setting, the background of the nurse and the unique needs of the patient. 5 Some nurses may serve as advanced practice nurses on neurology or epilepsy units, others may provide direct patient care and education in the clinic setting or in epilepsy monitoring units. Others may be involved doing research on various aspects of epilepsy care or treatment. Others will provide care to people with epilepsy in acute settings like emergency rooms or intensive care settings. Wherever a patient may go in the health care system, there will be a nurse there caring for them who will need to know about epilepsy and how it affects each patient and their family. Care needs will vary with each setting and the role of the nurse in that environment. 6 People with epilepsy often have other heath needs and require primary care treatment in an adult or pediatric settings, as well as in OB/GYN and other specialty settings. It is important for nurses in all settings to have awareness and knowledge of epilepsy in order to provide safe and effective care to these patients. Part of this knowledge set will be to appreciate the unique needs and concerns that patients and their families may have. For example, providing primary care to children with epilepsy will require the nurse to be cognizant of the child’s type of seizure and treatment needs. The nurse should be aware of how other health conditions may affect the child’s seizures the risk for injuries and other comorbid conditions, such as learning, mood and behavioral problems, and how a child’s other health needs may affect treatment of their seizures. Nurses who work in women’s health areas should be cognizant of the unique health needs that women may have due to their epilepsy and how hormonal issues may affect their seizures and treatment. Many women report changes in seizures around times of menses and with hormonal changes that occur with puberty, pregnancy, and menopause. Special needs also arise with consideration of oral contraceptive use and other family planning needs, bone health, and parenting. 7 Since epilepsy is a chronic and often life‐long disorder for many people, community based nurses are also critical members of a person’s team and may be found in schools, group homes, nursing homes, assisted living facilities, day programs, or state/district based nurses in public health, vocational rehabilitation, developmental disabilities, or mental health programs. The nurse’s role may vary in these settings. Of then the nurse is the ‘first responder’ – the person called to assist if someone has a seizure. They may assist or be responsible for administering medications, addressing patient safety concerns, and identifying and addressing factors that could affect a person’ss seizures and safety. Nurses in identifying and addressing factors that could affect a person seizures and safety Nurses in community settings may act as care or case managers who help people find appropriate resources and navigate health care and community resources. Others may be involved primarily as educators of health care and community care providers. 8 Epilepsy 101: Getting Started Although the role of the epilepsy nurse varies depending on practice setting, the core focus remains the same: identifying, assessing, educating and understanding the impact the disorder has on function and quality of life for our patients. This program is intended to provide a core knowledge of epilepsy for nurses working with patients in a general setting, or as an orientation to epilepsy for neuroscience and epilepsy nurses. People with epilepsy often have other heath needs and require primary care treatment in an adult or pediatric settings, as well as in OB/GYN and other specialty settings. It is important for nurses in all settings to have awareness and knowledge of epilepsy in order to provide safe and effective care to these patients. American Epilepsy Society 9 Epilepsy 101: Getting Started Approximately 2.2 million people in the US have epilepsy and 300,000 have their first convulsion each year. 120,000 are children under the age of 18. One in 26 Americans will develop epilepsy within their lifetime. 200,000 new cases of epilepsy are diagnosed each year; for 70% of those diagnosed, there is no known cause. References: IOM (Institute of Medicine) 2012 Epilepsy across the spectrum: Promoting health IOM (Institute of Medicine), 2012. Epilepsy across the spectrum: Promoting health and understanding. Washington DC: The National Academies Press. http://www.epilepsyfoundation.org/answerplace/statistics.cfm. Accessed 8‐16‐ 2011 American Epilepsy Society 10 Epilepsy 101: Getting Started Understanding what the terms epilepsy and seizures mean is the first step. Many myths about seizures and epilepsy still exist that can impact the stigma that surrounds epilepsy. A seizure is just a symptom of a disturbance in the brain and is caused by abnormal electrical discharges in the brain. The term epilepsy just means that a person has had 2 or more seizures, separated by at The term epilepsy just means that a person has had 2 or more seizures separated by at least 24 hours, that are unprovoked and not caused by any known medical condition. When these criteria are met, the person is considered at risk for or having a tendency to recurring seizures. The term seizure disorder is often used instead of the term epilepsy, but the meanings are the same. American Epilepsy Society 11 Epilepsy 101: Getting Started The incidence of epilepsy is highest in children younger than 2 and older than those ages 65 and older. Those over the age of 65 are the largest growing population of new‐onset epilepsy. As the population continues to age, there will be more new cases of epilepsy in the elderly diagnosed each year. American Epilepsy Society 12 Epilepsy 101: Getting Started In the majority of cases of epilepsy, 65%to 70%, the cause of epilepsy is unknown. causes. Other major causes are a result of vascular disease, congenital anomalies, trauma, brain tumors, neurodegenerative diseases, or infections of the central nervous system. American Epilepsy Society 13 Epilepsy 101: Getting Started Causes of epilepsy in infants and children are birth injuries, inborn errors of metabolism and congenital malformations. In childhood and adolescence, most epilepsy is idiopathic, genetic, or a result of an infection to the central nervous system such as encephalitis or meningitis. Idiopathic or cryptogenic epilepsy refers to epilepsy arising spontaneously or from an obscure or unknown cause. Some of these are presumed or found to have a genetic basis American Epilepsy Society 14 Epilepsy 101: Getting Started Many older adolescent and young adults acquire epilepsy as a result of head trauma due to accidents. Many have acute seizures as a result of drug intoxication or drug withdrawal. In older adults the number one cause of epilepsy is stroke, followed by brain tumors, trauma, and degenerative disorders. Acute seizures can occur in the setting of acute metabolic disturbances. American Epilepsy Society 15 Epilepsy 101: Getting Started Many cases of epilepsy develop as post traumatic epilepsy and can be a result of a subtle or severe head injury. The extent and location of the injury may impact the likelihood of developing seizures. Seizures can develop in the acute setting following the injury or may develop later as a result of the injury. Early treatment with AEDS may not affect the probability of developing seizures later on in life. American Epilepsy Society 16 Epilepsy 101: Getting Started Individuals with physical or intellectual disabilities have a higher risk of developing epilepsy, especially those with cerebral palsy or autism. For example, about 30% of children with autism may also have seizures. Stroke, hypoxia, CNS infection, and head trauma increase the chance a person will develop epilepsy. A person with a brain tumor may present with seizures and develop epilepsy and those with neurodegenerative disorders such as Alzheimer’s and multiple sclerosis have a higher risk of developing epilepsy. American Epilepsy Society 17 Epilepsy 101: Getting Started A variety of situations or factors can trigger seizures in an individual with epilepsy or make them more likely to have a seizure including: medication noncompliance, sleep deprivation, stress, accident or injury, concurrent illness such as a urinary tract infection’ upper respiratory infections or other febrile illnesses, hormonal changes during ovulation or with menses, ingestion of drugs or alcohol or environmental stimulus such as flashing lights for those who have photosensitive reflex seizures. It is important for each patient to know if they have triggers so that they can be avoided if possible Additionally identifying possible triggers may lead they can be avoided if possible. Additionally, identifying possible triggers may lead to modifiable lifestyle or environmental factors that if changes, could lessen the likelihood of seizures. American Epilepsy Society 18 Epilepsy 101: Getting Started The risk of dying in people with epilepsy varies according to whether or not there is a known cause of seizures. The risk for those with a known etiology for epilepsy is significantly higher, with 10 years of life lost, as compared to 2 years of life lost for those with no known caused of epilepsy. Approximately 42,000 patients die every year from epilepsy, and the mortality rate may be as high as 19% for those with seizures lasting longer than 30 minutes. In those patients with status epilepticus or generalized tonic‐clonic seizures, mortality may be increased 3‐ to 4‐fold. References: P ll k JM H Pellock JM. Hosp Med. 1999;60:43‐49. M d 1999 60 43 49 DeLorenzo RJ, et al. Epilepsia. 1999;40:164‐169 IOM 2012 (Institute of Medicine). Epilepsy across the spectrum: Promoting health and understanding. Washington, DC: The National Academies Press. American Epilepsy Society 19 Epilepsy 101: Getting Started Epilepsy is often considered a benign condition by many people, one that is easily controlled and not serious. However, people with epilepsy do die as a result of seizures, injuries, suicide and a phenomena known as SUDEP or sudden unexplained death in epilepsy. It’s important to note that many of these causes of death have modifiable risk factors and could be prevented by proper treatment, education and care. The first step in preventing death in epilepsy is to be aware that death is a risk and identify those factors that can increase the patient’s risks. Nurses working with people with epilepsy should talk to the patient’ss caregivers to understand the patient to the patient caregivers to understand the patient’ss risks, what they have been told and risks what they have been told and incorporate safety and risk assessments in patient teaching. American Epilepsy Society 20 Epilepsy 101: Getting Started SUDEP, or sudden unexplained death is epilepsy, is an area of major interest. The term applies to any sudden death in someone known to have epilepsy, when there is no obvious cause for the death found. The numbers of people experiencing SUDEP is unclear as there have not been any population‐based studies done. Frequency has been found to vary from 1 in 10,000 people from a sample of people with newly diagnosed epilepsy, and 9 out of 1,000 people from samples of people being evaluated for epilepsy surgery. This latter group would be considered to have intractable epilepsy. American Epilepsy Society 21 Epilepsy affects individuals to varying degrees. The spectrum of disability it creates is broad, ranging from a very limited effect on the individual to a devastating impact on all aspects of life. For a majority (perhaps as high as 80%) of people with epilepsy, seizures can be substantially reduced or completely controlled and may have limited impact on quality of life although memory and attention may pose additional challenges. For the remaining 20%, epilepsy is truly disabling, marked by frequent seizures, and other impairments, and a dramatically reduced quality of life. life Children whose seizures are not well controlled often experience social, emotional, and academic problems that compromise various stages of development. These problems may extend into adult life, where the same issues become barriers to employment and independence. Question: What are some of the social issues that you think are important to people with epilepsy? 22