Ambulatory 24-hour Esophageal pH Monitoring
advertisement

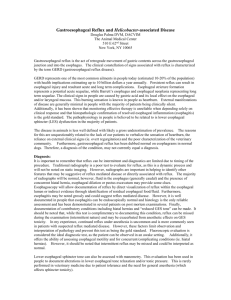
J Clin Gastroenterol 2003;37(1):14–22. © 2003 Lippincott Williams & Wilkins, Inc. Clinical Review Esophageal and Gastric Diseases Ambulatory 24-hour Esophageal pH Monitoring Why, When, and What to Do Christopher G. Streets, MRCS, and Tom R. DeMeester, MD reasons: (1) the technique measures and quantifies the basic pathophysiologic problem of GERD, namely the exposure time of the distal esophagus to excessive gastric juice; (2) the measurement is quantitatively related to the degree of esophageal mucosal injury; and (3) the episodes of gastric juice exposure can be correlated with the patient symptoms. This article discusses why ambulatory 24-hour esophageal pH monitoring has become the “gold standard” for the diagnosis of GERD, how to interpret the results using a variety of pH end points, how to perform the study, and the technical modifications that are being made to improve the test. Abstract The incidence of gastroesophageal reflux disease (GERD) is increasing and if left untreated can lead to significant patient morbidity and even death. The disease results from the abnormal reflux of gastric contents into the distal esophagus causing symptoms in most and subsequent mucosal damage in some. Several investigations can be used to confirm the diagnosis, but most are dependent on the presence of sequelae and complications of the disease. The physiologic test of ambulatory 24-hour esophageal pH monitoring has proved to be the most sensitive and specific diagnostic investigation. It measures increased esophageal exposure to gastric juice by detecting the concentration of hydrogen ions (pH <4) in the distal esophagus. The technique measures gastric juice exposure at a point 5 cm above the manometrically determined upper border of the lower esophageal sphincter. The exposure is measured in components of frequency of reflux episodes, duration of reflux episodes, and accumulated exposure time. The components are integrated into a composite score, which is reproducible, gender and race independent, and correlates with the degree of esophageal epithelial damage determined histologically. The composite score has been shown to be the most reliable measurement of a therapeutic acid suppression regimen or an effective antireflux operation. t is estimated that up to 11% of the US population experience heartburn daily and 30% every 3 days.1 Despite such reports the true prevalence of gastroesophageal reflux disease (GERD) within society is difficult to determine because the disease can also cause a variety of atypical symptoms. Further, it is questionable whether individuals who experience heartburn every 3 days have the disease. Consequently, a number of tests are used by the physician to identify individuals who truly have GERD. These include barium swallow, upper gastrointestinal endoscopy, acidperfusion test, and ambulatory 24-hour esophageal pH monitoring.2 Of these, ambulatory 24-hour esophageal pH monitoring has grown in popularity. This has occurred for 3 DEFINING GASTROESOPHAGEAL REFLUX DISEASE In clinical practice it is important to have an accurate definition of a condition before setting out to investigate and diagnose it. Unfortunately, over time, the lack of a universally accepted definition for GERD has hindered its investigation and confused the literature. Some investigators have used symptoms to define GERD, while others have concentrated on the presence of its complications, such as endoscopic esophagitis. Defining the pathologic process of gastroesophageal reflux using symptoms or complications is fraught with problems, as will be highlighted in the following section. A more sound definition would consider the pathophysiologic abnormality at play, and thus the definition of GERD adopted by the authors is “the abnormal exposure of the esophagus to gastric juice regardless of symptoms or complications.” In most patients gastric juice contains hydrogen ions that can be used as a marker for the reflux of acid gastric juice into the esophagus. The presence of hydrogen ions are detected by monitoring the esophageal luminal pH over a 24-hour period. From the Department of Surgery, Keck School of Medicine, University of Southern California, Los Angeles, California. Address correspondence and reprint requests to Dr. Tom R. DeMeester, Chairman of Surgery, Department of Surgery, Keck School of Medicine, University of Southern California, 1510 San Pablo Street, Suite 514, Los Angeles CA. E-mail: demeester@surgery.usc.edu. WHY ESOPHAGEAL PH MONITORING IS THE GOLD STANDARD FOR THE DIAGNOSIS OF GASTROESOPHAGEAL REFLUX DISEASE The symptoms experienced by individuals considered to have GERD are numerous and varied. Typical symptoms I 14 C.G. Streets and R.R. DeMeester 15 Ambulatory Esophageal pH Monitoring consist of heartburn and regurgitation, while atypical symptoms include hoarseness, wheezing, cough, and chest pain. Although exposing the esophageal mucosa to acidic gastric juice will cause one or more of these symptoms in most patients, reliance solely upon symptoms as an indication of increased esophageal exposure to gastric juice is inaccurate. In the absence of endoscopic esophagitis, there are many other disorders that can cause similar symptoms. These include diffuse esophageal spasm, achalasia, esophageal carcinoma, peptic ulcer disease, pyloric stenosis, cholelithiasis, and coronary artery disease. It also needs to be appreciated that reflux disease may include elements of duodenogastric reflux and esophagopharyngeal reflux. The symptoms of duodenogastric reflux are more gastric in character and include epigastric pain, nausea, vomiting, postprandial fullness, and belching. Symptoms of the esophagopharyngeal reflux are more respiratory in character, and include choking, chronic cough, wheezing, and hoarseness. In an individual with reflux disease, these atypical symptoms may be present to such a degree that they mask the typical symptoms of heartburn or regurgitation. Making a diagnosis of increased esophageal acid exposure based only on the presence of typical symptoms can overlook disease in a considerable number of patients. Indeed, the sensitivity (ie, the ability to detect GERD when it is known to be present) of the typical symptom heartburn is 68% and its specificity (ie, the ability to exclude GERD when it is known to be absent) is 63%.3 Making the diagnosis of increased esophageal acid exposure based on the presence of atypical symptoms is even more problematic. Consequently, atypical symptoms should be investigated as a possible manifestation of reflux disease and typical symptoms should be investigated if patients fail to respond to therapy or if invasive therapy is planned, because no one symptom complex is all inclusive for the diagnosis of GERD. It is important to appreciate that many patients with atypical symptoms may have functional dyspepsia and GERD is not the diagnosis. Further, relying solely on atypical symptoms as an indicator for increased esophageal acid exposure can encourage the inappropriate and nonspecific use of acid suppression therapy; an example is the knee-jerk prescription of proton pump inhibitors in patients with persistent symptoms after antireflux surgery, 76% of whom have been shown to have normal esophageal acid exposure.4 Persistent esophageal exposure to gastric juice does not cause mucosal injury, such as ulceration, esophagitis, stricture and Barrett metaplasia in all individuals.5 Consequently, it is not possible to define the disease by the presence of mucosal injury. Endoscopy, while able to identifying mucosal injury caused by the disease, may lead to the false conclusions that those patients without mucosal injury do not have GERD. Since about half of the patients with symptoms of GERD will not have gross mucosal injury, endoscopy has a diagnostic sensitivity of 62%. Muco- sal injury, when present however, is a reliable sign of increased esophageal exposure to gastric juice and has a specificity of 96%.6 On rare occasions esophagitis may be caused by unrecognized drug induced chemical injury. Experience with other diagnostic tests for GERD have been disappointing. A barium esophagogram rarely demonstrates the reflux of barium from the stomach into the esophagus. Rather, it focuses on the anatomic alterations associated with the disease such as hiatal hernia, Schatzki ring or stricture. Consequently it has a diagnostic sensitivity of 40% and a specificity of 85%.7 The Bernstein test, in which 0.1N hydrochloric acid is infused alternately with normal saline into the esophagus while asking the patient to report their symptoms, has a sensitivity of 84% and a specificity of 83%. Its real value is in measuring the sensitivity of the esophagus to acid gastric juice.7 In contrast, 24-hour esophageal pH monitoring has the highest sensitivity and specificity for GERD, both 96% (Table 1). The reason is that other tests infer the presence of acid in the esophagus, and are thus liable to error, whereas 24-hour esophageal pH monitoring actually measures the amount of esophageal exposure to gastric juice.6 The American Gastroenterological Association has recognized the importance of documenting the presence of GERD and recommends the use of ambulatory esophageal pH monitoring to (1) document abnormal esophageal acid exposure in an endoscopy-normal patient who is being considered for antireflux surgery; (2) evaluate patients after antireflux surgery who are suspected to have ongoing abnormal reflux; (3) evaluate patients with either normal or equivocal endoscopic findings or reflux symptoms that are refractory to proton pump inhibitor (PPI) therapy; (4) detect reflux in patients with chest pain after a normal cardiac evaluation; (5) evaluate a patient with suspected otolaryngologic manifestations (laryngitis, pharyngitis, chronic cough) of GERD; and (6) document concomitant GERD in an adult onset, non-allergenic asthmatic suspected of having reflux-induced asthma.8 Recently the measurement of effectiveness of acid suppression therapy has emerged as a further indication for 24-hour esophageal pH monitoring. It has been shown that inadequate medical therapy, while effective in controlling symptoms may allow continued reflux with microscopic injury to the esophageal mucosa.9 Experience with 24-hour esophageal pH monitoring has shown that there are several reasons for increased esophaTABLE 1. Diagnostic tests for gastroesophageal reflux disease. Test Barium esophagogram Upper gastrointestinal endoscopy Bernstein test Ambulatory 24-hour esophageal monitoring Sensitivity Specificity 40 68 84 96 85 96 83 96 16 geal acid exposure, all of which can, but not always give rise to symptoms of gastroesophageal reflux disease. They are: (1) over-distension of the stomach from swallowed air or gluttony resulting in transient loss of the lower esophageal sphincter (LES) barrier, (2) persistent loss of the LES barrier, (3) ineffective esophageal clearance of physiological reflux due to poor esophageal body motility and/or reduced saliva production, (4) gastric acid hypersecretion, and (5) delayed gastric emptying secondary to neuromuscular disease or outflow obstruction. HOW TO INTERPRET ESOPHAGEAL PH MONITORING—THE COMPOSITE SCORE Continuous esophageal pH monitoring has been available since the early 1960s,10 but the work of Johnson and DeMeester11 in the 1970s simplified the procedure and provided a method of interpreting the data obtained. The probe measures and records continuously the esophageal pH 5 cm above the upper border of the LES during a 24-hour period. Precise location of the pH probe is important since the lower or higher it is placed in the esophagus, the more or less physiologic esophageal acid exposure will be recorded. Consequently, normal values for acid exposure vary with the location of the probe. Further, placing the probe at 5 cm allows for the upward movement of the LES on swallowing without the threat of having the probe dip into the acidic environment of the stomach. Of particular interest in analyzing the 24-hour pH record is the time the esophageal pH is less than 4. This cut-off was chosen for a number of reasons: (1) at pH 4 normal subjects first begin to experience the symptom of heartburn;12 (2) the digestive enzyme pepsin, a key contributor to esophagitis, is activated at a pH of less than 4;13 (3) in normal subjects, without GERD, the esophageal pH is greater than 4 for a median of 98.5% of the 24-hour monitored period.14 Consequently, measuring the time the esophagus is exposed to pH less than 4 over a 24-hour period enables (1) quantitation of the time the esophageal mucosa is exposed to gastric juice, and how and when that exposure occurs (ie, in several long episodes or many short episodes; during the day, after meals or when asleep, (2) quantitation of the time it takes for the esophagus to clear refluxed acid, and (3) correlation of esophageal acid exposure with the patient’s symptoms.15 A 24-hour period is necessary so that measurements are made over 1 complete circadian cycle, and allows for determining the effect of physical activity and body position on esophageal acid exposure, such as running, lifting, bending, etc.16 At the authors’ institution, all ambulatory pH studies are carried out over a 24-hour period. This typically provides 20 to 22 hours of interpretable data. Other investigators have reported that shorter periods of recording yield similar results. In 1985, Walther and DeMeester showed that an 8-hour study, equally divided into upright and supine posi- J Clin Gastroenterol, Vol 37, No. 1, 2003 tions was an excellent predictor of the 24-hour pH score.17 More recently, Dobhan and Castell demonstrated that a 16hour overnight pH recording (4.00 PM to 8.00 AM) provided a reliable measurement of 24-hour esophageal acid exposure.18 Using the single measurement of the percent time the esophageal pH is below 4 during the 24-hour period, although concise, does not reflect how the exposure occurred (ie, in a few, long episodes or in several short episodes). This aspect is important, as the effect of a single long episode on the esophageal mucosa can be more significant than several short episodes. This is analogous to rapidly passing one’s hand in and out of the flame of a candle without pain, in contrast to leaving the hand in the flame for an equivalent but continuous period. The latter is likely to produce a serious burn. Consequently, to quantitate esophageal acid exposure more completely, 2 additional assessments are necessary: the frequency of the reflux episodes and their duration. Therefore, to provide a holistic measurement of esophageal acid exposure the following units are used: 1. The cumulative time the esophageal pH is below 4 expressed as a percentage of the total, upright and supine time; 2. The frequency of the reflux episodes expressed as the number of episodes per 24 hours; and 3. The duration of the episodes expressed as the number of episodes greater than 5 minutes per 24 hours and the time in minutes of the longest episode recorded. In some situations it can be helpful to know the time that the esophageal pH is above 6, 7, and 8 to quantitate the alkaline exposure. In this situation there cannot be absolute confidence that an increase in alkaline exposure is due to the reflux of gastric juice with a high pH, although this is the most common cause. Other causes for increased alkaline exposure are increased saliva secretion, oral bacterial contamination from diseased teeth and gums, or pooling of contaminated saliva in an obstructed esophagus.19 Drift and calibration error of an antimony probe may also be responsible.20 Normal values for the 6 components of the 24-hour test above and below various whole number pH thresholds were originally derived from 50 asymptomatic control subjects and are shown in Table 2. The upper limits of normal were established at the 95th percentile. Figure 1 shows the median and the 95th percentile of the normal values for each component, with patient values denoted by the shaded area. If the value of a symptomatic patient is outside the 95th percentile of normal subjects for the pH threshold selected, he or she is considered abnormal for the component measured. Experience using the threshold of pH 4 has shown a remarkable uniformity in the normal values of the 6 components from centers around the world, indicating that C.G. Streets and R.R. DeMeester 17 Ambulatory Esophageal pH Monitoring TABLE 2. Values for each of the six components of the 24-hour esophageal pH Composite Score at various pH thresholds in normal individuals (n = 50). pH <1 % total time % upright time % supine time No. of episodes No. of episodes >5 Longest episode pH <2 % total time % upright time % supine time No. of episodes No. of episodes >5 Longest episode pH <3 % total time % upright time % supine time No. of episodes No. of episodes >5 Longest episode pH <4 % total time % upright time % supine time No. of episodes No. of episodes >5 Longest episode pH <5 % total time % upright time % supine time No. of episodes No. of episodes >5 Longest episode pH <6 % total time % upright time % supine time No. of episodes No. of episodes >5 Longest episode pH <7 % total time % upright time % supine time No. of episodes No. of episodes >5 Longest episode pH >7 % total time % upright time % supine time No. of spisodes No. of episodes >5 Longest episode pH >8 % total time % upright time % supine time No. of episodes No. of episodes >5 Longest episode min. min. min. min min. min. min min. min. Mean Std dev Med Min 0.01 0.04 0 0.80 0 0.11 0.05 0.13 0 2.46 0 0.41 0 0 0 0 0 0 0 0 0 0 0 0 0.30 0.80 0 12.00 0 2.00 0.10 0.35 0 8.25 0 1.29 0.25 0.69 0 11.73 0 2 0.17 0.31 0.04 5.24 0.04 1.12 0.41 0.84 0.15 6.18 0.20 3.47 0 0.10 0 3.50 0 0.10 0 0 0 0 0 0 2.20 5.30 0.90 27.00 1.00 24.00 1.32 2.05 0.35 19.90 0.45 4.07 2.06 4.56 0.76 25.35 1.00 18.78 0.64 1.07 0.21 11.90 0.38 3.22 0.77 1.39 0.47 8.65 0.83 5.11 0.40 0.50 0 10.50 0 1.40 0 0 0 0 0 0 3.40 6.70 2.70 38.00 5.00 33.00 2.79 4.59 1.19 29.6 1.45 9.90 3.26 6.32 2.32 36.90 4.18 26.95 1.51 2.34 0.63 19.00 0.84 6.74 1.36 2.34 1.00 12.76 1.18 7.85 1.15 1.60 0.10 16.00 0 4.00 0 0 0 2.00 0 0 6.00 9.30 4.00 56.00 5.00 46.00 4.45 8.42 3.45 46.9 3.45 19.8 5.89 9.16 3.86 53.80 4.73 39.40 9.39 4.72 13.63 44.58 5.22 34.09 9.82 4.30 18.77 32.57 5.34 40.56 5.10 3.60 3.56 37.50 3.00 19.95 0.30 0.10 0 5.00 0 1.50 41.90 16.00 68.60 142.00 18.00 202.10 31.96 15.10 54.79 125.15 16.90 128.95 39.45 15.92 64.83 138.43 18.00 189.70 47.61 22.84 75.50 85.10 11.82 334.57 17.55 17.72 24.53 42.96 5.58 177.52 47.05 17.70 84.10 83.00 11.00 325.75 8.30 1.60 7.10 21.00 3.00 22.6 83.00 63.50 99.90 243.00 27.00 679.00 76.48 60.76 99.58 173.60 21.90 626.40 81.74 63.17 99.87 231.18 25.90 666.35 94.92 92.56 97.52 59.72 10.76 757.55 7.52 8.31 9.15 56.11 7.63 271.68 97.75 95.75 100.00 45.00 8.50 737.95 54.30 69.80 39.80 2.00 1.00 131.10 100.00 100.00 100.00 240.00 37.00 1459.00 99.95 100.00 100.00 184.45 23.90 1338.30 100.00 100.00 100.00 227.90 33.70 1458.2 5.08 7.44 2.48 8.38 3.72 24.00 7.52 8.31 9.15 7.87 8.63 26.70 2.25 4.25 0 5.55 2.00 11.55 0 0 0 0 0 0 45.70 30.20 60.20 38.00 59.00 103.70 16.54 28.57 16.09 27.00 13.80 87.77 38.03 30.01 49.92 34.98 47.18 99.41 0.03 0.05 0 1.30 0.02 0.48 0.12 0.18 0 4.86 0.14 1.93 0 0 0 0 0 0 0.80 1.20 0 33.00 1.00 10.4 0.15 0.30 0 6.70 0 5.04 0.64 0.95 0 26.68 0.73 10.02 esophageal acid exposure is similar among normal subjects despite variations in nationality and dietary habit. The first analysis of 24-hour esophageal pH records obtained from patients with typical symptoms of gastroesophageal reflux showed that not all of the 6 parameters 0 0 0 0 0 0 Max 95% 97.5% measured were always abnormal. The component most commonly abnormal was acid exposure during the recumbent period whereas the total number of reflux episodes per 24 hours had the lowest incidence of abnormality. This observation indicated a need to define when the 24-hour pH 18 J Clin Gastroenterol, Vol 37, No. 1, 2003 FIGURE 1. Graphic display of the 6 components of esophageal pH exposure showing the median and 95th percentile levels in 50 normal individuals with whole pH values above and below 6.0 as thresholds. The shaded area represents measurements made in a patient. When the shaded area exceeds the 95th percentile line for a given pH threshold, the patient is considered to have an abnormal value for the component measured. A: Percent cumulative exposure for total time. B: Percent cumulative exposure for upright time. C: Percent cumulative exposure for supine time. D: Number of episodes. E: Number of episodes lasting longer than 5 minutes. F: Length of longest reflux episode. record was abnormal. Even though the 6 components measured provided a means for quantitating gastric juice exposure, the observation that some were abnormal while others at the same time were normal, made it unclear when an individual should be considered to have increased exposure to gastric juice. To solve this problem, the standard deviation of the mean of each of the 6 components measured in 50 normal subjects was used as a weighing factor (Table 3, pH <4). To use standard deviation in this manner it was necessary to deal with the data as though they were parametric. Therefore, an artificial zero point was established 2 TABLE 3. Normal values for esophageal exposure to pH <4 (n = 50). Component Mean SD 95% Total time Upright time Supine time No. of episodes No. >5 min Longest episode 1.51 2.34 0.63 19.00 0.84 6.74 1.36 2.34 1.0 12.76 1.18 7.85 4.45 8.42 3.45 46.9 3.45 19.8 C.G. Streets and R.R. DeMeester standard deviations below the mean value measured in the 50 normal subjects for each particular component even though in some situations this would be below 0 and practically an impossibility, (ie, no individual could have less than 0 reflux. Nevertheless, this allowed a scoring system to be built around the standard deviation as a weighting unit, while treating the data as if they had a normal distribution. Thus, any measured value from a patient could be referenced to this artificial 0 point and, in turn, be awarded points based on dividing the measured value by the standard deviation of the mean of the normal value for the specific component (Fig. 2). The formula used to perform this calculation was: Patient’s value ⳯ 19 Ambulatory Esophageal pH Monitoring 冉 mean − SD 1 +1− SD SD 冊 Mathematical reorganization of this formula gave a simpler version: Component score = Patient value − mean +2 SD The use of the constant 2 is not essential since it altered the magnitude of the score by the same value in every case. However, in practice a constant is used for the convenience of maintaining a positive value when scoring each component. The minimum value of that constant is 1 scoring unit. So the simplified formula for scoring each component in practice is: Component score = Patient value − mean +1 Standard deviation Using the standard deviation of the mean of the normal value for each component weighs each measured component of the 24-hour pH patient’s record according to the dependability and reliability of the measurement. For example, in normal subjects the number of reflux episodes per 24 hours had a very wide standard deviation, resulting in a large number used to weigh the measured value in patients. This rewarded few points for this particular component. In contrast, normal individuals rarely reflux at night. Therefore, the standard deviation for supine reflux is small and consequently, nocturnal acid exposure results in more points or greater weight than other components. A 24-hour pH composite score was obtained by adding the points calculated for each of the 6 components. The upper limit of normal (95th percentile) for the composite score for each whole number pH threshold is shown in Table 4. Comparison of 24-hour pH data from normal subjects from 3 institutions using the pH threshold of less than 4, showed great uniformity and confirmed that the amount of esophageal acid exposure in normal individuals could be quantitated and used to develop diagnostic threshold values.21 Recently the process of reading the pH record has been computerized and the amount of esophageal acid exposure at each whole number pH threshold has been measured. The data are expressed as the percentage time the esophageal pH is below 1, 2, 3, 4, 5, 6 or 7, or above 7 or 8. The number of reflux episodes, the number of episodes lasting longer TABLE 4. Distribution of composite scores at various pH thresholds in normal individuals (n = 50). FIGURE 2. Concept of using the standard deviation as the scoring unit to score the component of the percent time that pH was less than 4 for the total period. Note the establishment of an abstract zero point 2 standard deviations below the mean value for total-period of exposure below pH4 measured in 50 normal subjects. Theoretically, this allows scoring the measurement in patients as though the normal values were parametric. In this example the patient’s total acid exposure below pH 4 is of 4.8% and has a score of 4.41. PH Mean Std Dev Med Min Max 95% 97.5% <1 <2 <3 <4 <5 <6 <7 >7 >8 4.06 6.03 6.01 5.95 6.00 6.00 6.00 6.00 4.94 3.54 4.35 3.99 4.43 4.69 4.23 2.32 4.55 3.90 2.90 4.65 4.75 4.95 4.85 5.95 6.30 4.50 3.80 2.90 3.60 1.50 0.40 0.50 −3.00 −7.40 1.80 3.80 22.40 25.80 16.20 18.00 16.60 15.20 9.00 25.60 29.90 14.20 17.37 14.10 14.72 15.76 12.76 8.55 14.90 8.50 17.80 25.09 15.93 17.64 16.49 14.65 8.89 22.69 9.60 20 FIGURE 3. Graphic display of the composite score used to express the overall result of a 24-hour esophageal pH recording. The lower line represents the median score and the upper line the 95th percentile of 50 normal subjects. The black area represents the composite score of the patient, with increased esophageal acid exposure measured at pH <4. than 5 minutes and the longest reflux episode are also measured for each pH threshold. The data for each component are shown graphically in Figure 1 as previously mentioned. A composite score calculated from all the components for each pH threshold can also be expressed graphically (Fig. 3). In 1992, Jamieson et al14 evaluated the sensitivity, specificity, and reproducibility of each of the individual components and the final composite score of 24-hour pH monitoring to diagnose GERD. Using receiver operating curves to compare the true-positive and false-positive rates, the composite score and percent total time pH <4 were shown to be the best discriminators of normal from abnormal, with the composite score slightly better than percent total time pH <4. The study also verified that while percent total time pH <4 was greater in males than in females, the final composite score did not vary with gender. This obviated the need for separate gender-based normal values. It also showed that the setting in which the 24-hour esophageal pH monitoring was performed, in-patient or ambulatory, did not affect the accuracy and reproducibility of the results. This was true in so far as patients could be accurately identified as being normal or abnormal. However, the degree of abnormal exposure was related to the degree of patient activity. J Clin Gastroenterol, Vol 37, No. 1, 2003 For many years, pathologists believed that the only diagnostic criterion for esophagitis was inflammation; however, in 1970, Ismail-Beigi et al22 observed that some patients with clinical symptoms suggestive of reflux had normal or minimal endoscopic abnormalities. These patients on biopsy had hyperplasia of the esophageal squamous epithelium, a finding which they postulated reflected an early histologic manifestation of acid-induced injury. Hyperplasia was defined as being present when the length of the subepithelial papillae of the lamina propria and the width of the basal zone exceeded more than 67% and 15% of the thickness of the mucosa respectfully. Subsequent studies confirmed these observations. Johnson et al23 demonstrated that exposure of the distal esophageal mucosa to acid gastric juice as quantified by 24-hour esophageal pH monitoring could be related to these morphologic findings. The degree of esophageal acid exposure correlated directly with increases in both relative and absolute length of the subepithelial papillae and also to relative basal zone hyperplasia. This relationship was supported by the observation that both papillary length and width of basal zone hyperplasia decreased after antireflux surgery returned the esophageal acid exposure to normal levels. Oberg et al24 performed 24-hour esophageal pH monitoring in patients with and without cardiac mucosa at the gastroesophageal junction. Those with cardiac mucosa had significantly increased esophageal acid exposure as well as other hallmarks of reflux disease, such as a hiatal hernia and defective LES. In 96% of patients the cardiac mucosa was also found to have an inflammatory infiltrate. They concluded that the formation of cardiac mucosa represented the earliest histologic signs of gastroesophageal reflux. In a subsequent publication, this same group observed that in patients with Barrett esophagus, the length of the intestinalized cardiac mucosa correlated with the degree of distal esophageal acid exposure determined by ambulatory 24hour pH monitoring.25 Recently, Campos et al used multivariate analysis to determine the strongest preoperative factors predictive of a favorable outcome after uncomplicated laparoscopic Nissen fundoplications.26 Of all the variables considered, there were 3 that significantly predicted a successful outcome – an abnormal 24-hour pH composite score, a typical primary symptom (heartburn or regurgitation), and symptomatic improvement in response to acid suppression therapy. If all 3 of these factors were present, a good or excellent outcome from anti-reflux surgery was obtained in 97.4% of cases. Further analysis of the data showed that only 75% of patients with typical symptoms that responded to acid suppression therapy, but a normal composite score had a good or excellent outcome. Of the 3 variables, an abnormal composite score was the strongest predictor of success and so emphasizes the importance of 24-hour esophageal pH monitoring in preoperative assessment of patients with GERD. C.G. Streets and R.R. DeMeester Ambulatory Esophageal pH Monitoring PERFORMING THE TEST Twenty-four hour esophageal pH monitoring is usually initiated in the esophageal function laboratory where the pH probe is properly positioned and the patient is outfitted with the monitoring equipment. Prior to the test, the patients must abstain from medication known to affect gastroesophageal motility and gastric acid production (7 days for PPIs, 72 hours for prokinetics, 24 hours for H2 receptor antagonists, and 24 hours for antacids), and take nothing by mouth the night before the study. Written informed consent is obtained and the patient has a nostril anaesthetized with topical 2% lidocaine or 4% cocaine administered with a Q-Tip. At the authors’ institution, transnasal esophageal manometry is performed to accurately locate the upper border of the LES before each pH study. The manometry catheter is removed and a multi-use glass or a single-use antimony monocrystalline pH catheter is introduced. If there is an interest in monitoring at the alkaline pH thresholds of 7 or 8, a glass probe should be used since it is known that an antimony probe does not provide an accurate measurement of hydrogen ion concentration at pH values greater than 4.20 The probe is calibrated in buffered solutions of pH 7.0, 4.0 and 1.0 prior to insertion. The probe is passed initially into the stomach to confirm that acid is present and that the probe has not coiled in the esophagus. It is then withdrawn until the tip comes to lie at a point 5 cm above the upper border of the LES. The catheter is taped securely to the nose, run over and behind the ear, and connected to a portable digital data recorder worn around the patient’s waist. The patient is instructed to have an active day and remain in the upright or sitting position until retiring to bed in the evening. Also, they are instructed not to eat or drink between their meals, chew gum or smoke. One meal is standardized consisting of a hamburger, fries and milkshake, obtained at McDonalds or Burger King. The other meals consist only of food with a pH between 5 and 7; a list of suitable items is provided to the patients. Each meal must be eaten at 1 sitting and accompanied by only water, milk, coffee or tea. Carbonated beverages, alcohol and fruit drinks are to be avoided. The patient is instructed to lie flat at night with, if possible, only a single pillow and no blocks under the head of the bed. No medication affecting gastrointestinal function is to be taken during the monitored period. A diary of events is kept and includes the beginning and end of mealtimes, the time when the patient went to bed and got up in the morning, and the time and nature of any symptoms experienced. On returning to the esophageal function laboratory the next day, the probe is removed, placed in the 3 buffer solutions to check its calibration and the recorded data transferred to a PC for analysis with a commercial software program. This produces a summary report detailing the vari- 21 ous component values and the calculated composite score for the patient. A postprandial acid exposure is also calculated by measuring the percentage time that the pH is less than 4 during the 2-hour postprandial periods following the standardized meal.27 A NOVEL TECHNIQUE FOR MONITORING ESOPHAGEAL PH The conventional method for measuring esophageal pH consists of a pH electrode located at the end of a long indwelling catheter that passes up the esophagus, along the posterior wall of the pharynx and out the nose. The catheter is uncomfortable and socially embarrassing. Consequently, despite patients being encouraged to pursue their normal everyday activities during the monitoring period, Fass et 28 al have shown that the study significantly reduces refluxprovoking activities. Many patients experienced side effects, such as throat discomfort and runny nose, and felt uncomfortable most of the monitored period. Several, despite encouragement to do otherwise, spent an atypically sedentary day when monitored. To increase the comfort and acceptability of this important diagnostic test, a number of investigators have used radiotelemetric pH monitoring systems.29,30 However, the ability of these early systems to become incorporated into routine clinical practice has been thwarted by a number of problems including electrode drift, battery life, poor signal reception and general unreliability. These systems also required a thread to suspend the radiotelemetric pH capsule at the correct level in the esophagus. The proximal end of the thread was brought out through the mouth and attached to the subject’s cheek. This still caused some oropharyngeal discomfort. Recently a “clip-on” and truly catheter-free radiotelemetric pH capsule, called the BRAVO™ pH monitoring system (Medtronic Inc., Shoreview, MN), has been developed and is currently used at several institutions. The system consists of a small monocrystalline antimony pH sensor that is delivered transnasally and attached to the esophageal mucosa at a point 5 cm above the previously manometrically determined proximal border of the LES. The delivery catheter is then removed. The pH data is transmitted to a remote receiver worn on the patients’ belt. Early experiences indicate that this new technique is not only comparable to the conventional catheter system for quantifying esophageal pH, but is more comfortable and allows the patient to be more active during the test period. Of benefit, a pH electrode that is attached to the esophageal mucosa moves with the mucosa and reduces the risk associated with the catheter pH probes to “dip down” toward the stomach with each swallow and shortening of the esophagus. CONCLUSION Ambulatory 24-hour esophageal pH monitoring allows the measurement of esophageal acid exposure and when 22 J Clin Gastroenterol, Vol 37, No. 1, 2003 expressed by a calculated composite score is an excellent technique for identifying gastroesophageal reflux disease. Since its description in 1974, the 24-hour esophageal pH composite score has proved to be a durable standard to identify and quantify gastroesophageal reflux disease by measuring esophageal acid exposure. The test has a high sensitivity, specificity and reproducibility. A novel radiotelemetric system has currently been introduced with the benefit of making the test more acceptable to the patient. REFERENCES 1. Hunt R. Importance of pH control in the management of GERD. Arch Intern Med. 1999;159:649–657. 2. DeMeester TR, Johnson LF. The Evaluation of Objective Measurements of Gastroesophageal Reflux and Their Contribution to Patient Management. Surg Clin North Am. 1976;56:39–53. 3. Tefera L, Fein M, Ritter MP, et al. Can the Combination of Symptoms and Endoscopy Confirm the Presence of Gastroesophageal Reflux Disease? Am Surg. 1997;63:933–936. 4. Lord RVN, Kaminski A, Oberg S, et al. Absence of Gastroesophageal Reflux Disease in a Majority of Patients Taking Acid Suppression Medications After Nissen Fundoplication. J Gastrointest Surg. 2002;:3–10. 5. DeMeester TR, Peters JH, Bremner CG, et al. Biology of esophageal reflux disease: Pathophysiology relating to medical and surgical treatment. Ann Rev Med. 1999;50:469–506. 6. Fuchs KH, DeMeester TR, Albertucci M. Specificity and Sensitivity of Objective Diagnosis of Gastroesophageal Reflux Disease. Surgery. 1987;102:575–580. 7. DeMeester TR. Prolonged esophageal pH monitoring. In: Read NW, ed. Gastrointestinal motility: Which test? 1989:41–52. 8. Kahrilas PJ, Quigley EM. American Gastroenterological Association medical position statement: Guidelines on the use of esophageal pH recording. Gastroenterology. 1996;110:1981–1996. 9. Katzka DA, Paoletti V, Leite L, et al. Prolonged ambulatory pH monitoring in patients with persistent gastroesophageal reflux disease symptoms: Testing while on therapy identifies the need for more aggressive anti-reflux therapy. Am J Gastroenterol. 1996;91:2110–2113. 10. Miller FA. Utilization of inlying pH probe for evaluation of acid-peptic diathesis. Arch Surg. 1964;89:199–203. 11. Johnson LF, DeMeester TR. Twenty-four hour pH monitoring of the distal esophagus: a quantitative measure of gastroesophageal reflux. Am J Gastroenterol. 1974;62:325–332. 12. Tuttle SG, Rufin F, Battaneloo A. The physiology of heartburn. Ann Intern Med. 1961;55:292–300. 13. Piper DW, Fenton HB. pH stability and activity curves of pepsin with special reference to their clinical importance. Gut. 1965;6:506–508. 14. Jamieson JR, Stein HJ, DeMeester TR, et al. Ambulatory 24-hr esophageal pH monitoring: Normal values, optimal thresholds, specificity, sensitivity and reproducibility. Am J Gastroenterol. 1992;87:1102–1111. 15. DeMeester TR, Wang CI, Wernly JA, et al. Technique, Indications and Clinical Use of 24-Hour Esophageal pH Monitoring. J Thorac Cardiovasc Surg. 1980; 79:656–667. 16. DeMeester TR, Johnson LF, Joseph GJ, et al. Patterns of Gastroesophageal Reflux in Health and Disease. Ann Surg. 1976;184:459–470. 17. Walther B, DeMeester TR. Comparison of 8- and 16-hour esophageal pH monitoring. In: DeMeester TR, Skinner DB. eds. Esophageal disorders: Pathophysiology and therapy. 1985;589–591. 18. Dobhan R, Castell DO. Prolonged intraesophageal pH monitoring with 16-hour overnight recording. Comparison with “24-hour” analysis. Dig Dis Sci. 1992;37: 857–864. 19. Pellegrini CA, DeMeester TR, Wernley JA, et al. Alkaline gastroesophageal reflux. Am J Surg. 1978;135:177–184. 20. McLauchlan G, Rawlings JM, Lucas ML, et al. Electrodes for 24 hour pH monitoring – a comparative study. Gut. 1987;28:935–939. 21. Richter JE, Bradley LA, DeMeester TR, et al. Normal 24 hour Ambulatory Esophageal pH Values: Influence of Study Center, pH Electrode, Age and Gender. Dig Dis Sci. 1992;37:849–856. 22. Ismail-Beigi F, Horton PF, Pope CE. Histological consequences of gastroesophageal reflux in man. Gastroenterology. 1970;58:163–174. 23. Johnson LF, DeMeester TR, Haggitt RC. Esophageal epithelial response to gastroesophageal reflux. A quantitative study. Am J Dig Dis. 1978;23:498–509. 24. Oberg S, Peters JH, DeMeester TR, et al. Inflammation and specialized intestinal metaplasia of cardiac mucosa is a manifestation of gastroesophageal reflux disease. Ann Surg. 1997;226:522–532. 25. Oberg S, Ritter MP, Crookes PF, et al. Gastroesophageal reflux disease and mucosal injury with emphasis on short-segment Barrett’s esophagus and duodenogastroesophageal reflux. J Gastrointest Surg. 1998;2:547–553. 26. Campos GMR, Peters JH, DeMeester TR, et al. Multivariate analysis of factors predicting outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg. 1999;3:292–300. 27. Mason RJ, Öberg S, Bremner CG, et al. Postprandial Gastroesophageal Reflux in Normal Volunteers and Symptomatic Patients. J Gastrointest Surg. 1998;2:342– 349. 28. Fass R, Hell R, Sampliner RE, et al. Effect of ambulatory 24-hour esophageal pH monitoring on reflux-provoking activities. Dig Dis Sci. 1999;44:2263–2269. 29. Kurt EJ, Kang S. Radiotelemetry pH determination for gastroesophageal reflux. An analysis of 521 cases. Am J Gastroenterol. 1972;58:390–395. 30. Branicki FJ, Evans DF, Ogilvie AL, et al. Ambulatory monitoring of oesophageal pH in reflux oesophagitis using a portable radiotelemetry system. Gut. 1982;23: 992–998.