HYPOTHERMIA
Identifying hypoperfusion in hypothermic trauma patients
InSpectra™ StO2 Tissue Oxygenation Monitor predicts hypoperfusion,
even in hypothermic trauma patients1
Hypothermia (core body temperature of 35°C or less) is
common in severely injured trauma patients, contributing
to poor tissue perfusion and shock. In the treatment
of trauma patients, hypothermia is recognized as a
significant risk factor for grave complications, including
multiple organ dysfunction syndrome (MODS) and
mortality.1,2 Analysis of the 2004 National Trauma Bank
found hypothermic trauma patients had significantly
greater mortality (25.5% vs. 3.0%, P < 0.001) compared
to normothermic trauma patients.2 The study also found
that hypothermic patients had greater base deficits (BD),
higher injury severity scores (ISS), and longer lengths of
stay in the hospital.2 These findings support the need to
rapidly resolve hypothermia during initial resuscitation
of trauma patients.
When trauma patients are hypothermic, inadequate
tissue perfusion can be difficult to identify and assess.
Despite significant advancements in medical technology,
direct assessment of adequate oxygen delivery to body
tissues can be challenging. Clinical measures traditionally
used to identify, monitor and track hypoperfusion
include blood pressure, BD and serum lactate.3–5 These
methods are widely accepted and studies have validated
their use in predicting MODS and mortality; however,
they have limitations. Lactate and BD are intermittent
measures, may be normal in early shock and are affected
by some preexisting medical conditions.6 In addition, as
indicators of global perfusion, blood pressure, BD and
lactate levels may not always be sensitive to peripheral
hypoperfusion.6 Better indicators of hypoperfusion, along
with early identifiers of shock, are critical to initiating
appropriate therapeutic interventions that may result in
better clinical outcomes for the patient.
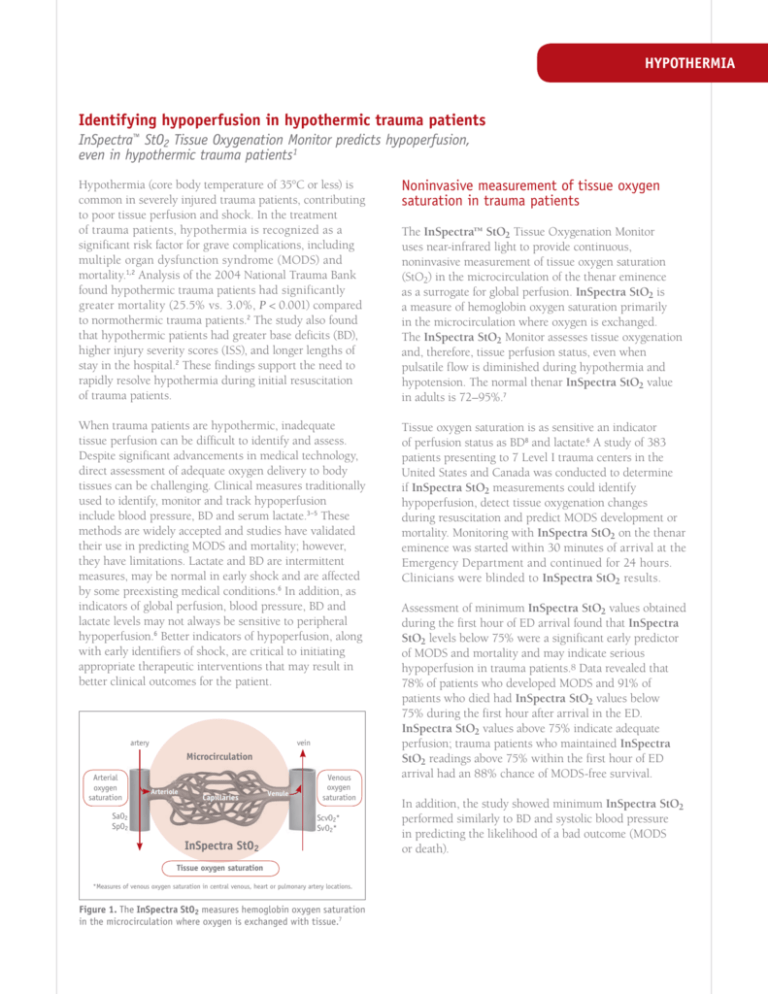
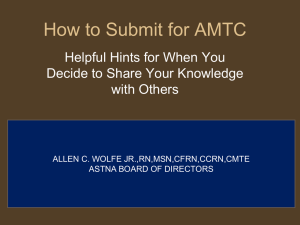
artery
vein
Microcirculation
Arterial
oxygen
saturation
Arteriole
Capillaries
SaO2
SpO2
Venule
Venous
oxygen
saturation
ScvO2*
SvO2*
InSpectra StO2
Tissue oxygen saturation
*Measures of venous oxygen saturation in central venous, heart or pulmonary artery locations.
Figure 1. The InSpectra StO2 measures hemoglobin oxygen saturation
in the microcirculation where oxygen is exchanged with tissue.7
Noninvasive measurement of tissue oxygen
saturation in trauma patients
The InSpectra™ StO2 Tissue Oxygenation Monitor
uses near-infrared light to provide continuous,
noninvasive measurement of tissue oxygen saturation
(StO2) in the microcirculation of the thenar eminence
as a surrogate for global perfusion. InSpectra StO2 is
a measure of hemoglobin oxygen saturation primarily
in the microcirculation where oxygen is exchanged.
The InSpectra StO2 Monitor assesses tissue oxygenation
and, therefore, tissue perfusion status, even when
pulsatile flow is diminished during hypothermia and
hypotension. The normal thenar InSpectra StO2 value
in adults is 72–95%.7
Tissue oxygen saturation is as sensitive an indicator
of perfusion status as BD8 and lactate.6 A study of 383
patients presenting to 7 Level I trauma centers in the
United States and Canada was conducted to determine
if InSpectra StO2 measurements could identify
hypoperfusion, detect tissue oxygenation changes
during resuscitation and predict MODS development or
mortality. Monitoring with InSpectra StO2 on the thenar
eminence was started within 30 minutes of arrival at the
Emergency Department and continued for 24 hours.
Clinicians were blinded to InSpectra StO2 results.
Assessment of minimum InSpectra StO2 values obtained
during the first hour of ED arrival found that InSpectra
StO2 levels below 75% were a significant early predictor
of MODS and mortality and may indicate serious
hypoperfusion in trauma patients.8 Data revealed that
78% of patients who developed MODS and 91% of
patients who died had InSpectra StO2 values below
75% during the first hour after arrival in the ED.
InSpectra StO2 values above 75% indicate adequate
perfusion; trauma patients who maintained InSpectra
StO2 readings above 75% within the first hour of ED
arrival had an 88% chance of MODS-free survival.
In addition, the study showed minimum InSpectra StO2
performed similarly to BD and systolic blood pressure
in predicting the likelihood of a bad outcome (MODS
or death).
StO2
Lactate
Base Deficit
Tissue Oxygen Saturation (%)
100
3.0
95
2.0
90
1.0
85
0.0
80
75
–1.0
70
–2.0
65
–3.0
60
E
PR
IN
DU
I
CT
O
PO
N
ST
IN
DU
I
CT
O
N
ST
ER
TO
NO
M
Y
A
ST
RT
B
CP
B
CP
30
M
IN
RE
A
W
RM
IN
G
O
FF
B
CP
O
CL
SU
RE
Arterial Lactate (mmoI/L) and Base Deficit (mEq/L)
HYPOTHERMIA
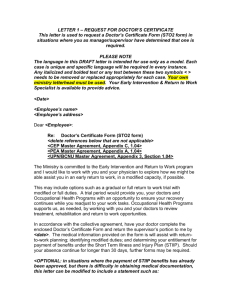
Figure 2. Variation of tissue oxygen saturation (StO2), arterial
lactate and base deficit (BD) over stage of procedure.9
InSpectra StO2 Tissue Oxygenation Monitor
detects subtle changes in oxygen delivery
Changes in tissue perfusion may precede global
indications of shock. To evaluate the ability of the
InSpectra StO2 Monitor to detect subtle changes in
tissue oxygenation in a controlled model of altered
perfusion, InSpectra StO2 was studied in 40 patients
undergoing cardiopulmonary bypass (CPB).9 Vital
signs, invasive blood pressure readings and body
temperature were recorded at 5-minute intervals.
Blood samples were obtained at key points during
surgery and every 30 minutes while on CPB.
Clinicians were blinded to InSpectra StO2 readings.
Study data were grouped by specific stage of the CPB
procedure. Variations in InSpectra StO2, arterial lactate
and BD over the course of surgery are shown in Figure 2.
A decrease in InSpectra StO2 readings from 90% (7%)
to 77% (17%) corresponded to a delayed lactate increase
of 275.6% (221.9%) from baseline. The minimum
InSpectra StO2 value preceded the maximum lactate
level by mean time of 93.9 minutes (86.3 minutes).
In this study, the InSpectra StO2 Monitor reliably
detected subtle changes in oxygen delivery to skeletal
muscle tissue. These changes were identified in real time
and preceded the development of abnormal lactate levels.
While a predictive relationship between InSpectra StO2
and BD was not identified, changes in InSpectra StO2
measurements temporally preceded changes in BD. In
addition, study data support a previous finding7 that
temperature does not influence InSpectra StO2 readings.
These results suggest tissue oxygen saturation can play
an important role in screening critically ill and injured
patients at risk for hypoperfusion.
Hypothermia has no effect on the InSpectra
StO2 Monitor’s ability to assess perfusion
Hypoperfusion may be difficult to identify in
hypothermic trauma patients. To assess the influence of
mild hypothermia and rewarming on InSpectra StO2
measurements, tissue oxygen saturation was studied in
six young, healthy volunteers under general anesthesia.10
In this observational study, each volunteer’s core body
temperature was cooled from approximately 36°C to a
target temperature of 34°C, similar to mild hypothermia
in elective cardiac surgery patients. Core temperature
was maintained at approximately 34°C for 1 hour before
each volunteer was rewarmed. Tissue oxygen saturation
readings were obtained at 5 temperature means (SD):
36.5°C (0.5), 35.5°C (0.5), 34.5°C (0.5), 35.5°C (0.5), and
36.5°C (0.5).
The means (SD) of InSpectra StO2 at each temperature
were 73% (8%), 71% (11%), 67% (14%), 68% (11%),
and 74% (7%). Statistically significant changes in
InSpectra StO2 (P < 0.05) were found at the end of
cooling and rewarming.
The InSpectra StO2 Monitor detects changes in tissue
oxygen saturation during mild hypothermia and
rewarming. High inter-individual variability occurred
during mild hypothermia, suggesting people respond
differently to hypothermia.
HYPOTHERMIA
InSpectra StO2 identifies hypoperfusion and predicts MODS in hypothermic trauma patients
The relationship of early hypothermia to MODS and
mortality among severely injured trauma patients was
studied in a prospective observational study at 7 Level I
trauma centers in the United States and Canada.2 Severely
injured patients with hypoperfusion and need for blood
transfusion were monitored via the InSpectra StO2 and
using traditional clinical variables.
Among 359 severely injured trauma patients,
hypothermia was common (43%), regardless of
geographic location or month of year. Hypothermic
patients were more likely than normothermic patients
to develop MODS (21% vs. 9%, P = 0.003), but did
not have increased mortality rates (16% vs. 12%, P =
0.28). In hypothermic patients, maximum base deficit
(max BD) did not discriminate between those who did
or did not develop MODS, but did predict mortality.
Significant predictors of MODS included minimum
InSpectra StO2 (P = 0.0002) and hypothermia (P =
0.01), but not max BD (P = 0.09). Predictors for mortality
included InSpectra StO2 (P = 0.0004) and max BD (P =
0.01), but not hypothermia (P = 0.74).
Hypothermia is a risk factor for multiple organ failure,
but not mortality. Minimum InSpectra StO2 predicts
MODS and mortality in normothermia and hypothermic
patients. However, the ability of max BD to predict
MODS was blunted by hypothermia.
To learn more about the InSpectra StO2 Tissue
Oxygenation Monitor, its unique ability to monitor
hypoperfusion in hypothermic patients and studies
on the use of InSpectra StO2 in trauma patients,
visit www.htibiomeasurement.com.
References
1.Martin RS, Kilgo PD, Miller PR, Hoth JJ, Meredith JW, Chang MC.
Injury-associated hypothermia: an analysis of the 2004 National
Trauma Data Bank. Shock. 2005;24:114–118.
2.Beilman GJ, Nelson T, Nathens AB, et al. Early hypothermia in
severely injured trauma patients is a significant risk factor for
multiple organ dysfunction syndrome but not mortality [abstract].
Crit Care. 2007;11(suppl 2):S139. Abstract P345.
3.Davis JW, Shackford SR, Holbrook TL. Base deficit as a sensitive
indicator of compensated shock and tissue oxygen utilization.
Surgery. 1991;173:473–476.
4.Englehart MS, Schreiber MA. Measurement of acid-base
resuscitation endpoint: lactate, base deficit, bicarbonate or what?
Curr Opin Crit Care. 2006;12:569–574.
5.Moore FA, McKinley BA, Moore EE. The next generation in shock
resuscitation. Lancet. 2004;363(9425):1988–1996.
6.Moore FA. Tissue oxygen saturation predicts the development of
organ failure during traumatic shock resuscitation. In: Faist, E, ed.
International Proceedings of the 7th World Congress on Trauma, Shock,
Inflammation and Sepsis; Munich, Germany, 13–17 March 2007.
Bologna, Italy: Medimond; 2007:111–114.
7.Crookes BA, Cohn SM, Bloch S, et al. Can near-infrared
spectroscopy identify the severity of shock in trauma patients?
J Trauma. 2005;58:1119–1125.
8.Cohn SM, Nathens AB, Moore FA, et al. Tissue oxygen saturation
predicts the development of organ dysfunction during traumatic
shock resuscitation. J Trauma. 2007;62:44–55.
9.Putnam B, Bricker S, Fedorka P, et al. The correlation of nearinfrared spectroscopy with changes in oxygen delivery in a
controlled model of altered perfusion. Am Surg. 2007;73:1017–1022.
10.Ali SZ, Taniguchi Y, Zmoos S, Kurz A. Influence of mild
hypothermia and rewarming on near infrared spectroscopy derived
tissue oxygen saturation [abstract]. Eur J Anaesthesiol. 2006;23
(suppl S37):216. Abstract A-837.
HYPOTHERMIA
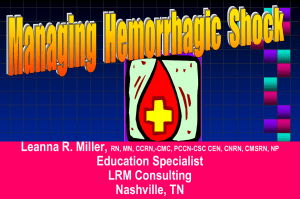
Case Study: Continuous Tissue Oxygenation (InSpectra™ StO2) Monitoring During Resuscitation
BD, HgB, Lactate InSpectra™ StO2, SpO2, SBP, DBP, HR, Temp °C
• An intoxicated male in his 30s was ejected from a vehicle during a high-speed crash
• Patient presented with hypothermia, Grade IV splenic laceration, grade I renal laceration, left hemopneumothorax,
and left femur fracture (fx) upon arrival at the trauma center
• InSpectra StO2 measurements ranged from 53% to 64% despite splenic artery embolization and active rewarming
• InSpectra StO2 readings increased above 75% after additional units of packed red blood cells (PRBC), fresh frozen
plasma (FFP) and cryoprecipitate were administered
160
T.C.
arrival by
To IR
helicopter embolization
140
To ICU
To
CT
120
100
80
60
Bolus
2L LR
1u PRBC
40
1u PRBC
FFP Cryo
Normothermia
Active
warming starts
20
Hypothermia
20
10
0
8:00
9:00
10:00
11:00
12:00
13:00
14:00
15:00
16:00
Time
InSpectra™ StO2
HgB
Lac
SpO2
SBP
Temp °C
DBP
HR
BD
Event Markers
Disclaimer
This case was taken from a prospective multi-site study sponsored by Hutchinson Technology Inc. in which clinicians
were blinded to InSpectra StO2 measurements.1 This case represents an example of a compromised circulation situation
where the InSpectra StO2 monitor’s general indications apply. It is one of several hundred cases from a multi-site,
prospective, observational clinical study and is not intended to represent the general findings of the study.
Reference
1. Cohn SM, Nathens AB, Moore FA, et al. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock
resuscitation. J Trauma. 2007;62:44–55.
Hutchinson Technology Inc.
BioMeasurement Division – USA
Authorized European Representative
European Business Office – Netherlands
tel: 800.419.1007
fax:320.587.1555
biom.usa@hti.htch.com
www.htibiomeasurement.com
tel: +31 26 365 33 71
fax:+31 26 365 33 72
biom.eu@hti.htch.com
Intended Use
The InSpectra™ StO2 Tissue
Oxygenation Monitor is intended for
use as a noninvasive monitoring
system that measures an approximated
value of percent hemoglobin oxygen
saturation in tissue (StO2).
InSpectra is a registered trademark of Hutchinson Technology Inc. in the United States of America, the European Community, Canada, China and Japan.
©2008 Hutchinson Technology Inc. 5018782 A 06/08 All Rights Reserved. Printed in the USA. RX ONLY.
0086