Case Study: A 51-Year-Old Man with Recurring Mild-to
advertisement
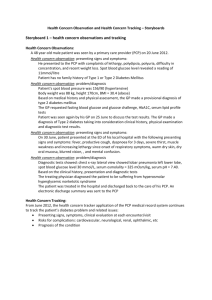
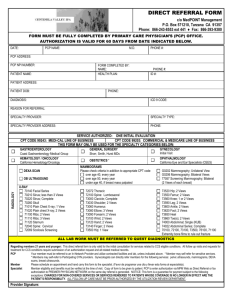
CASE STUDY A 51-YEAR-OLD MAN WITH RECURRING MILD-TO-MODERATE DEPRESSION — Thomas W. Koenig, MD BACKGROUND A 51-year-old man was referred by his primary care physician (PCP) to a psychiatrist in an officebased practice for treatment of recurring mild-to-moderate depression. Mr D. had been taking citalopram 40 mg for 1 year, prescribed by the PCP. His depressive symptoms were said to “wax and wane” during this time, with his current episode considered to be of moderate severity. HISTORY Mr D. is employed as a computer engineer for a large national defense contracting company. He has been employed at this company for 5 years and was promoted to a managerial role approximately 8 months ago. He is happy with the more technical aspects of his work but finds the managerial responsibilities frustrating. However, he was given a substantial pay raise for this promotion and feels compelled to continue as a manager, as his children will be attending college in the next couple of years. Mr D. has been married for 21 years and has 3 children, a son aged 16 years and daughters aged 14 and 11 years. His wife is 50 years of age and a full-time homemaker. He maintains that his marriage is “good.” The rest of his family (siblings and parents) are scattered throughout the country, more than a 1-day drive away. He maintains close relationships with his brother, sister, and parents and tries to see his parents at least once per year. He and his wife are friendly with the neighbors but do not socialize with them. They have Advanced Studies in Medicine ■ no friends in the area whom they would consider to be “close” friends. Mr D. is college educated and has a master’s degree in computer science. He enjoys working in his yard and reading in his spare time. He also stays physically fit by swimming regularly and lifting weights several times per week. Other than his depressive illness over the past year, Mr D. has not had any other psychiatric disorders. He saw a psychological counselor briefly during college when he was having difficulty with his grades. He and his wife also sought marital counseling 12 years ago for about 3 to 4 months, mostly due to the stress of frequent job changes and moving to new cities with 2 small children. Mr D. has no significant medical conditions. He has mild hypertension (130/85 mm Hg) and mild hypercholesterolemia (209 mg/dL). He has no history of surgical procedures, head trauma, or other major medical conditions. He does not smoke. He has no significant family history of any medical or psychiatric disorder. His parents are living (in their late 70s) and in overall good health. TREATMENT HISTORY Mr D. first presented to his PCP 1 year ago with a 3-week history of insomnia, poor appetite, anxiety, and feeling “out of control.” He had lost 15 pounds during that time. His wife had severe menopausal symptoms, his teenage daughter was very rebellious at the time, and he was under a lot of stress at work due to cutbacks (resulting in a heavier workload) and disagreements with one of his several bosses. His PCP diagnosed depression with some anxiety and prescribed citalopram 20 mg once daily. Mr D. returned S15 CASE STUDY to his PCP for a follow-up visit after 2 weeks with minimal symptom improvement. He returned again after another 2 weeks and reported sleeping better and feeling less “weighed down” by his problems. His PCP told him to continue with the citalopram 20 mg for another 6 months. He returned to the PCP at 4 months; his insomnia had returned, and he had a general feeling of fatigue and malaise. He also complained of overall achiness, and dyspepsia that had started several months ago. His PCP increased the dose of citalopram to 40 mg once daily and suggested eliminating caffeine from his diet and doing more stretching or yoga as a relaxation method and to relieve some of the achiness. He also prescribed esomeprazole 20 mg once daily for the dyspepsia. He asked Mr D. to return in 2 weeks if the insomnia was not ameliorated. Mr D. returned in 2 weeks with further complaints of intermittent insomnia. By this time, he had started his new position as a manager and was getting settled, which helped with some of the anxiety, but he was “desperate for some regular sleep.” His PCP prescribed zolpidem as needed for his insomnia and referred him to a psychiatrist to treat his recurrent depression. Mr D. is currently taking citalopram 40 mg once daily, zolpidem 10 mg as needed, celecoxib, and metaxalone 400 mg as needed. His PCP also prescribed massage for his achy muscles, but he is uncomfortable with the idea of a massage by a stranger. PSYCHOSOCIAL ASSESSMENT FIRST SESSION Mr D. feels that he is currently experiencing moderate stress at work. His workday is very full but manageable. His daughter’s teenage rebellion seems to have settled down and his wife’s menopausal symptoms have improved. He and his wife took a long vacation this past winter by themselves, and he remarked on how much he enjoyed that. He also said he and his wife were making an effort to spend more time together, without the children. SECOND SESSION In the second session with the psychiatrist, Mr D. was asked to again describe the symptoms that led him S16 to seek treatment from his PCP. Mr D. then revealed that his dyspepsia had started more than 1 year ago, as did his sense of “overall aches and pains,” particularly in the lower back (he did not offer this information at the first session). He described his general malaise during that time as “feeling like lead” and being too tired to really deal with anything. He felt he was “just barely getting through 1 day at a time.” Although he felt the citalopram helped, especially when the dose was increased, he never really seemed to be able to “shake off the depression.” He remarks that he is unsure what the psychiatrist can do because he is resistant to taking further medication. He attributes his poor sleep and dyspepsia to stress at work and his low-back pain to being hunched over a keyboard all day. DISCUSSION Mr D.’s diagnosis of mild depression appears to be correct. His depressive symptoms over the past year included insomnia, weight loss, poor appetite, feeling out of control, and feeling “weighed down.” His depression never seemed to resolve completely, despite adequate doses of citalopram. Of note, the physical symptoms present at his first PCP visit were not associated with the depressive symptoms, by either the patient or the PCP. They did not resolve and, as a result, Mr D. never felt able to “shake off the depression.” In fact, it took 2 sessions with the psychiatrist to discover the extent of his physical complaints during the past year. Unresolved or undertreated depression is a useful signal to probe for somatic complaints that may be untreated. Mr D.’s somatic complaints are common among those with depression: dyspepsia, malaise, achiness, and low-back pain. It is common for patients— and even PCPs—to not associate the somatic complaints (especially vague complaints with no apparent discernible cause) with depressive symptoms. In Mr D.’s case, an excuse for each symptom could be found (anxiety over job stress for dyspepsia, poor posture at his desk for low-back pain). More aggressive treatment of the patient’s depression may help to resolve his lingering physical symptoms. Vol. 4 (1A) ■ January 2004