Clinical profile of pneumocystis Carinli pneumonia
advertisement

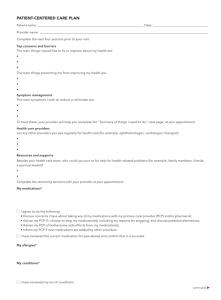
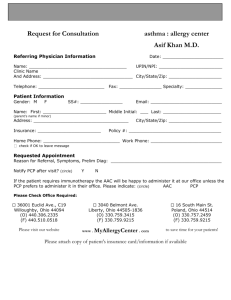
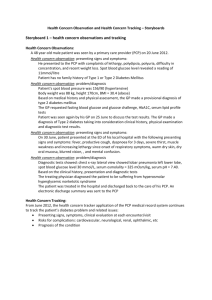
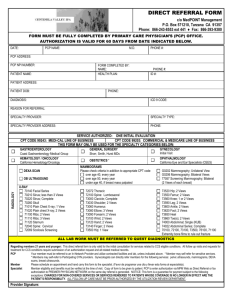
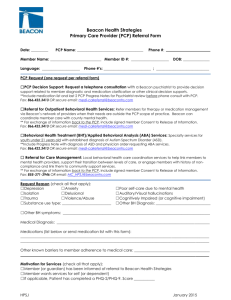
Original Article Ind. J Tub. 2000, 47, 93 CLINICAL PROFILE OF PNEUMOCYSTIS CARINII PNEUMONIA IN HIV INFECTED PERSONS* N. Usha Rani1, V.V.R. Reddy2, A.Prem Kumar1, K.V.V. Vijay Kumar2, G.Ravindra Babu3 and D.Babu Rao4 Summary : Between Dec’97 and Nov’98, out of 120 patients injected with HIV, 23 cases of Pneumocystis carinu pneumonia (PCP) were found and their clinical profiles were studied at the department of TB and Chest Diseases. Andhra Medical College, Visakhapatnam. The diagnosis of PCP was made using CDC criteria based on chest X-ray. It is coacltided that PCP is not an uncommon complication in HIV infected individuals in this country. As many as 65% of PCP cases belonged to the economically productive age group of 21-30 years; 40% were truckers or manual labourers: dry cough, dyspnoea on exertion, low-grade lever were the most common presenting symptoms In patients with initial SP02 less than 90%. the degree of exercise induced oxygen desaluration was more. The yield from induced sputum specimens stained by CMS was 50%. Almost 92% ot the cases showed raised LDH level. Response rate to Cotrimoxazole therapy was 74% and good drug tolerance was observed Nearly 43% of the cases bad coexistent tuberculosis, out of which 90% were having extra-pulmonary tuberculosis. Key words :- Pneumocyslis carinii pneumonia, HIV infection, HIV A tuberculosis INTRODUCTION Prior to 1980s, Pnewnocysfis carimi pneumonia (PCP) was a sporadic cause of pneumonia occurring mainly in a few immune-compromised patients. In 1981, the outbreak of PCP among homosexuals in Los Angeles (USA) led to the recognition of AIDS’2 as a clinical entity. In the West, 75% of individuals infected with HIV developed PCP, sooner or later. The widespread use of primary and secondary prophylaxis led to a decline in the occurrence of PCP, after 1988. In India, although the incidence of HIV infection is rapidly increasing, yet case reports of PCP are scarce in the Indian literature. The increasing numbers of extrapufmonary and atypical forms of pulmonary tuberculosis in our patients led to the suspicion and later confirmation of the co-existing HIV infection in them. The fact that PCP is the most common opportunistic infection in AIDS cases in the West1 prompted us to study the occurrence and clinical profile of PCP cases in southern India. MATERIAL AND METHODS The study was undertaken during a period of one year, from Dec’97 to Nov’98 and 120 patients with HIV infection were recognized among those reporting with various respiratory ailments at the Govt. Hospital for Chest and Communicable Diseases, Visakhapatnam. Out of the 120 cases with HIV infection, 23 cases were presumed to be of PCP, using CDC/ CDSC (Centres for Disease Control/Communiable Disease Surveillance Centre) Criteria. The CDC/CDSC4,5 criteria allow presumptive diagnosis of PCP being made in a HIV infected person with1. Dyspnoea on exertion/non-productive cough of recent onset 2. Chest X-ray showing diffuse bilateral interstitial infiltrates 3. Arterial hypoxaemia 4. No evidence of bacterial pneumonia. All the 23 cases were proved to be HIV positive. The initial positive ELISA test was confirmed by repeat ELISA using different Ag or by Immunocomb/ Immunoblot / Capillus method, after taking informed consent. The study of clinical profile included recording of bio-data, history of risk factors, *Paper presented at the 53rd National Conference on Tuberculosis and Chest Diseases, Bhubaneshwar. Dccemebr 27th To 30 th 1998 1 post graduate Student 2. Asst Professor. 3. Professor, 4 Professor and Head of Deapartment Correspondence : Dr. G. Ravindra Babn. Professor in Deptt. ol TB and Chest Diseases. Andhra Medical College, Visakhapatnam 94 N. USHARANIETAL presenting symptoms and clinical examination. Sputum direct smear examination for AFB by ZiehlNeelsen’s staining was done in all the cases. Sputum speciments were obtained by collecting induced sputum using 5% hypertonic saline inhalations by nebuliser and specimens were stained by Giemsa/ Gomori Methenamine Silver (QMS) staining procedure at the Department of Microbiology, Andhra Medical College, Visakhapatnam. Routine blood and urine examinations were done. Serum lacto dehydrogenase (LDH) levels were estimated. Mantoux test was done with 5 TU of P.P.D. Exercise oxygen saturation (EOS) measurements were done in all the cases with Ohmeda Pulse Oximeter using Ohmeda finger probes. A 10-min exercise which causes a fall of oxygen saturation pressure (SPO2) to 90% or less or a 2-min exercise which causes a fall of SPO2 by 3% was taken as positive desaturation test 6-9 . ECG echocardigraphy high resolution CT were done in selected cases. All the 23 patients were treated with Cotrimoxazole for 3 weeks. Patients who had initial SP02 of less than 90% and respiratory rate of more than 25 per minute were started on a 3 week course of Prednisolone. Dry cough, Gr. I or II, dyspnoea, low-grade fever were the most common symptoms. Mean duration of symptoms was 1.5 months. Retrosternal discomfort occurred in 13%. Most common coexisting conditions were oral candidiasis, hairy cell leukoplakia and oral ulcers (78%). The most common dermatological manifestation was seborrhic dermatitis (30%). Diarrhoea and mild dehydration were associated in 35%. Clinical examination of the respiratory system in a majority was normal, some showed fine basal crackles with or with out rhonchi. Exercise Oxygen Saturation (EOS) measurements revealed that 74% had initial SPO2 more than 90%, with a mean drop of 4% with exercise, and 26% had initial SPO2 less than 90% with a mean drop of 11 % with exercise (Table 1) Mean drop was more in cases with initial SPO2<90%. Chest X-ray examination showed that 73% had bilateral lower zone or mid and lower zone interstitial shadows and 18% had interstitial and alveolar shadows (Fig. 2). High resolution CT was done in 2 patients; both showed diffused ground glass opacities (Fig. 3). Table 2. Induced sputum test profile in PCP Done in Positive Yield FINDINGS Of the 23 cases of PCP, diagnosis was confirmed by the demonstrtion of cysts (Fig. 1) by GMS/Giemsa stain in 6 cases (26%). Of the 23 cases, 18 (78%) were males, 11 (47%) belonged to the age group of 21-30 years and 40% were truckers or manual labourers. All males gave a history of promiscuous behaviour and casual sex. One female had undergone blood transfusion. Table 1. Exercise oxygen saturation measurement. 10 mts exercise<90% fall/2 mts exercise 3% fall No. % Mean drop Initial SPO2>90% with drop 17 74% 4% Initial SPO2<90% with drop 6 26% 11% Total 23 100% 10 5 50% Trophozoites 6 1 16% Total 16 6 GMS / Gysts Giemsa/ Induced sputum test with 5%, hypertonic saline nebulisation was done in 16 cases and the obtained sputum specimens were examined by GMS / Giemsa staining. Pneumocystis Carinii cysts were demonstrated in 1 out of 6 (16%) cases (Table 2) by Giemsa staining. One patient could not undergo the induced sputum test because she was severely hypoxaemic wifh central cyanosis. Serum LDH level was estimated in 13 cases, increased levels were observed in 92% of the cases (more than 4601.U./ lit), while 3 cases showed levels more than 1000 I.U. / lit. Mantoux test done with 5 T.U. PPD showed that 65% of the cases were anergic. PCP IN HIV INFECTED PERSONS 95 Fig. 3 HRCT showing bilateral ground gloss opacities Additional treatment with corticosteroids was given toll patients (48%). No adverse effects were observed in 70% of them. Adverse effects like minor rashes, jaundice and methaemoglobinaemia were chest seen in the remaining cases. In all, 43% of the total 23 cases of PCP developed tuberculosis before or after the PCP episode, of which 90% were extrapulmonary, tuberculosis lymphadenitis being the commonest. DISCUSSION Fig, 2 X-Ray showing bilateral mid & lower zone interstitial shadows Clinical response (Table 3) to 3 weeks’ treatment with Cotrimoxazole (CTM) (15/75 mg/kg.bd.wt.) was good. CTM was well-tolerated by 74% of the cases, whether on treatment or prophylaxis. Table 3. Therapeutic profile in PCP Treatment n 3 Weeks of CTM treatment 7 % 30% 3 Weeks of CTM prophylaxis Relapses Deaths 8 2 2 4 35% 9% 9% 17% Total 23 11 100% Absconded + Prednisolone 3 Weeks 47% HIV infection has become a global pandemic. Approximately 60% of HIV positive persons develop AIDS within 12-13 years after infection. India has been categorized as a pattern II country, with the estimated cases of AIDS rising rapidly. The present study was aimed at studying the clinical profile of PCP in HIV infected persons. During the study period, 120 HIV infected persons were presumptively recognised. The proportion of PCP cases in the group was 19%; the observed higher percentage compared to other Indian studies10 may be due to the CDC criteria used for making the diagnosis of PCP. In a HIV infected person, when chest X-ray shows an interstitial pattern, a high index of suspicion is required to work out the case in the PCP direction. Inter-observer variations might have contributed to reporting of a lower incidence of PCP in the Indian studies. A majority of our cases belonged to the age group 21-30 years, similar to that of Mohanty et al10. In the present study, the mean duration of PCP illness was 1.5 months, compared with 28 days and 25 days reported in western studies. 96 N. USHA RANI ET AL In the early stage of PCP, the chest radiograph shows fine bilateral perihiliar diffuse infiltrates which progress to the interstitial alveolar butterfly pattern11. From the hilar region, the infiltrates spread to apices or bases. However, normal X-ray may be seen in 2-34% of the cases. In the present study, all the cases, on account of the method of selection, had bilateral interstitial shadows with perihilar and basilar distribution. The HRCT helps to detect interstitial disease not visible on routine chest radiographs12. Therefore, HRCT is a useful diagnostic tool in the clinical setting of PCP when the chest X-ray is normal. In the present study, P.C. cysts were demonstrated by GMS in 5 out of 10 (50%) cases. The GMS staining is the gold standard for morphological identification of P.C. cysts13. A wide range of variability in the yield of GMS is noted in various studies13-15. Visualisation of clusters of cysts within foamy material clinches the diagnosis. Cup shaped, creascent shaped, banana shaped cysts with capsular thickening are characteristic. Presently, immunofluorescent staining with monoclonal antibodies has replaced GMS and other techniques in western countries. Exercise oxygen saturation measurements (EOS) showed that all the 23 cases had fall of SPO2 with exercise. Six patients had initial SPO,, less than 90%, whose mean drop with exercise was 11 %. EOS results may vary depending upon the extent or the timing of occurrence of PCP. Serum LDH level estimation in a useful screening test2 u. Increased levels were observed in 92% of the cases in the present series. It is also useful to monitor the response to theaphy. Co-existent tuberculosis was seen in 10 out of 23 cases of PCP. Some cases of extrapulmonary tuberculosis developed PCP while on antituberculosis theraphy, within 2-10 months. Three cases of PCP developed tuberculous lymphadenitis after 3 months of the PCP and 2 cases of pulmonary tuberculosis developed PCP while on treatment for 3 months. Since 20% of HIV infected persons can progress to AIDS in 5 years, not only can cases of extra-pulmonary tuberculosis but even pulmonary forms of tuberculosis develop PCP, sooner or later. Response rate to 3 weeks of Cotrimoxazole in our cases was 73% i.e. almost the same as 75% and 60% in other studies2. Only 8% in the present study had major adverse reactions. Any HIV infected person with interstitial pattern on chest X-ray and or dry cough should be suspected of having PCP and should be further investigated. Diseases like interstitial fibrosis, interstitial edema, lymphangitis and carcinomatosis may mimic PCP on X-ray, but they are rare in the younger age groups. Absolute eosinophilic count helps to rule our tropical pulmonary eosinophilia which also may mimic PCP. The CDC criteria can be used for making a presumptive diagnosis of PCP. Diagnostic techniques like Bronchoalveolar Lavage/Trans bronchial Lung Biopsy16,17 may be used in cases who do not respond to Cotrimoxazole theraphy in 5-7 days. In fact, extrapulmonary tuberculosis cases may receive primary prophylaxis with Cotrimoxazole since the drug is well tolerated. REFERENCES 1. John. F.Murray and John Mills pulmonary infectious complications of HIV infection part-I and II; State of Art.AmRev.Respir.Dis. 1990,141.1356 and 1582 2. StewartJ. Levine, Pneumocystis carinii, Clinics in Chest Medicine, 1996, 17,665 3. Wallace J.M. Rao, A.V.Glassroth, J et al : Respiratory illness in persons with AIDS, Am.Rev Resp.Diseases, 1993, 148; 1523 4. Centres for Disease Control, Pneumocystis carinii Pneumonia- Los Angeles MM. W.R. 1980, 30; 250 5. Centres for Disease Control, Update on AIDS • United States, MM.W.R 1982. 31; 507 6. Christos Chouaid, Dominique, Maillard : Cost effectiveness of non-invasive 02 saturation, measurement during exercise for the diagnosis of PCP, Am.Rev. RespirDis 1993. 147, 1360 7. G.Faetkenheurer et al : Exercise Oximetry for early diagnosis of PCP, Lancet, 1989.222. 8 Jaume Sauleda, Joaquim, GEA et al. Simplified exercise test for differential diagnosis of PCP in HIV, Thorax 1994;49; 112 9. D.E.Smith, J.Wyatt, AMc.Lucky el al: severe exercise hypoxaemia with normal or near normal X-rays in PCP. Lancet, 19S8. 5, 1049 10. K.C.Mohanty, Sudhir Nair: Changing trend of HIV infection in patients with respiratory diseases in Bombay since 1988. Ind.J.Tub. 1994,41,147. 11. Fishman’s pulmonary disease and Disorders III edition, IIvolume, section 20, Chapter 150-2313. 12. Laurence, Huang and John D.: AIDS and Lung, Medical clinics of North America, No.4, July 1986. 80, 775 13. Kirsch C.M. Jenes. W.A.: Analysis of induced sputum for the diagnosis of recurrent PCP, Chest 1992. 102, 1152 14. Zaman.M.K. White D.A. Serum LDH levels and PCP Diagnostic and prognostic significance. Am. Rev. Resp. As 1988. 137; 769 15. Robert F.Miller, David.M.Mitchell, Pneumocystis carinii Pneumonia, AIDS and lung update 1995, Thorax; 1995.50: 191 16. Tin. J.V. Bien. H. J, Detsky A.S- Bronchoscopy Vs empirical therapy in HIV patients with presumptive PCP Am.Rev.Resp.Dis,.1993. 148.370