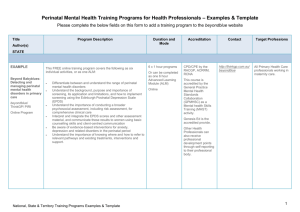
The beyondblue National Postnatal Depression Program Prevention
advertisement

The beyondblue National Postnatal Depression Program Prevention and Early Intervention 2001 – 2005 Final Report Volume I: National Screening Program beyondblue National Postnatal Depression Program VOL I: National Screening Program This report was prepared by A/Prof Anne Buist and Dr Justin Bilszta (National Director and National Project Manager) With the assistance of the State Directors: Prof Jeannette Milgrom (VIC & TAS) Prof John Condon (SA) Dr Craig Speelman (WA) Prof Barbara Hayes (QLD) Prof Bryanne Barnett (NSW) Prof David Ellwood (ACT) This work would not have been possible without the support to the National and State Investigators by: The State Project Managers and Research Teams The beyondblue Board and its Chair, the Hon. Mr Jeff Kennett Ms Leonie Young, Dr Nicole Highett and the beyondblue staff The hospitals involved in the National Screening Program & The thousands of women, and their families, who participated in this initiative and shared their lives with us over the last four years Page 2 of 108 beyondblue National Postnatal Depression Program “This booklet is fantastic and should be provided to everyone. Where can I get one to send to my son and daughter-in-law who are expecting their first baby in Vancouver." Midwife, VIC. VOL I: National Screening Program “In the past (due to experience) we thought we could 'pick' women who were depressed, but am astounded by the numbers we are picking up with screening.” MCHN, WA. “It was reassuring to find out from my MACH nurse that I was in fact not depressed after my son arrived. She helped me to see that my feelings were normal and expected in motherhood.” Postnatal woman, ACT. “Having experienced postnatal depression with my first baby, I felt supported by knowing that midwives were interested in my experience.” Antenatal woman, NSW. “I’m glad that the hospital is concerned with how we feel” Antenatal women, VIC. “Its great to be able to provide women in need with information.” Health worker, QLD. “As a mother who is suffering PND after my twins, the information on your booklet has helped me realize how common the illness is…” Consumer, W.A Clockwise, from top left - mother and baby photo from promotional posters; Janette Brooks, WA project manager, with a stand at PND Awareness Week 2003; Ms Claudinia Daley from TAIHS, Townsville; Prof John Condon, Prof Ian Hickie and Dr Margaret Tobin at the launch of the SA initiative; family photo used on the cover of the twins booklet; Party to celebrate six months of screening at Royal North Shore Hospital, NSW; Prof Jeannette Milgrom, the Hon Mr Michael Wooldridge, A/Prof Anne Buist and Dr Justin Bilszta at the national launch of the PND Program in 2001. Page 3 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program CONTENTS PAGE Executive Summary ...........................................................................................................................8 Recommendations ................................................................................................... 10 National Action Plan To Implement Perinatal Depression Screening....................................... 11 What Are the Problems .......................................................................................... 11 Where To From Here.............................................................................................. 11 Reflections From The National Co-Ordinator ............................................................................. 14 Reflections From Victoria And Tasmania.................................................................................... 15 Reflections From South Australia ................................................................................................. 16 Reflections From Western Australia............................................................................................. 17 Reflections From Queensland........................................................................................................ 18 Reflections From New South Wales .............................................................................................. 19 Reflections From The Australian Capital Territory ................................................................... 20 Vale: Professor Sherryl Pope and Rachael McCarthy ................................................................ 21 Aims & Objectives Of The beyondblue National Postnatal Depression Program .................... 22 1. Establishment and Evaluation of the Introduction of Routine Screening for Antenatal and Postnatal Depression at Major Maternity Hospitals/Health Services in Australia. ................. 23 Overview................................................................................................................... 23 What Have We Learnt? .......................................................................................... 24 Implementation of Perinatal Depression Screening............................................. 25 Evaluation of the Feasibility and Acceptability of Introducing Perinatal Depression Screening .............................................................................................. 27 2. Development of Materials to Address Community and Health Professional Awareness of Perinatal Depression and its Treatment ....................................................................................... 29 Overview................................................................................................................... 29 Health Professional Training ................................................................................. 30 Media and Promotion ............................................................................................. 32 Postnatal Depression Information Booklet ................................................. 33 Postnatal Depression Information Pamphlet............................................... 35 Depression Management Guide .................................................................. 37 Guide To Using The Edinburgh Postnatal Depression Scale...................... 39 Promotional Posters .................................................................................... 40 www.beyondblue.org.au/postnataldepression............................................. 42 Page 4 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program 3. Evaluation of Changes in Health Professional and General Community’s Knowledge of Perinatal Mood Disorders .............................................................................................................. 43 Overview................................................................................................................... 43 Aims .......................................................................................................................... 44 Method ..................................................................................................................... 44 Population ................................................................................................... 44 Health Professionals.................................................................................... 44 6-12 Week Postnatal Women...................................................................... 45 Questionnaires............................................................................................. 45 Experience of Perinatal Depression Screening.................... 45 Knowledge Questionnaire ................................................... 45 The Edinburgh Postnatal Depression Scale......................... 45 Results ..................................................................................................................... 45 Response Rates............................................................................................ 45 Summary of Baseline Findings ................................................................... 46 Demographic Profile of Postnatal Mothers................................................. 46 Emotional Health of Mothers...................................................................... 46 Awareness – Perinatal Depression .............................................................. 47 Awareness – Booklet................................................................................... 47 Health Professional Knowledge.................................................................. 48 Recommendations/Preferences for Treatment ............................................ 48 Changes in Help Seeking Behaviour........................................................... 49 Barriers to Treatment .................................................................................. 49 Discussion ................................................................................................................. 50 Increasing Awareness of Perinatal Depression in Health Professionals and Perinatal Women........................................................................................... 50 Improving Knowledge of Perinatal Depression and its Treatment in Health Professionals ................................................................................................. 50 Improving Health Professional’s Confidence in Treating Perinatal Depression ..................................................................................................................... 50 Improving Access to Services by Perinatally Depressed Women................. 51 Conclusions .............................................................................................................. 51 4. Provision of a National Database of Young Families in Australia ......................................... 52 Overview................................................................................................................... 52 Demographics Overview......................................................................................... 53 Mood Data................................................................................................................ 57 Risk Factors for Antenatal and Postnatal Depression......................................... 60 Demographic Variables............................................................................... 60 Psychosocial Variables................................................................................ 61 Correlation of EPDS and K10/Sphere................................................................... 63 5. Evidence of Efficacy of Early Intervention Initiatives ............................................................ 64 Overview................................................................................................................... 64 Page 5 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Staff Members ................................................................................................................................. 65 Hospitals/Area-Health Services Involved ..................................................................................... 67 Acknowledgements And Thanks ................................................................................................... 68 Appendices....................................................................................................................................... 71 Appendix A – Feedback to Services Document .................................................... 72 Appendix B – Detailed List of Organizations to Receive PND Training ........... 74 Appendix C – Health Professional Training Guidelines...................................... 84 Appendix D – Detailed List of Media and Promotional Activities ..................... 86 TV, Radio and Promotional Activities........................................................ 86 Newspaper and Magazine Articles.............................................................. 96 Appendix E – Detailed list of Conference Presentations and Scientific Articles .................................................................................................................................. 101 Conference Presentations ........................................................................... 101 Scientific Articles.......................................................................................108 Tables and Figures Figure 1. The Perinatal Depression Screening Protocol...............................................................26 Table 1. Health Professionals Screening Experience....................................................................28 Table 2. Groups Involved in Baseline Evaluation (BE) & End Evaluation (EE)......................45 Table 3. Recognition/Awareness of Postnatal Depression in Health Professionals and Postnatal Mothers at Baseline (BE) and End Evaluation (EE) .......................................... 46 Table 4. Demographic Profile of Postnatal Mothers at Baseline (BE), End Evaluation (EE) & National Average 2002............................................................................................................ 47 Table 5. Recommendations/Preferences for Treatment..............................................................49 Table 6. Perceived Barriers to Treatment of Perinatal Depression ............................................50 Table 7. National Demographic Overview.....................................................................................54 Table 8. State Demographic Overview...........................................................................................55 Table 9. Rates of Antenatal and Postnatal Depression by EPDS Scores ................................... 57 Figure 2. Distribution of Antenatal EPDS Score ......................................................................... 58 Figure 3. Distribution of Postnatal EPDS Scores......................................................................... 58 Page 6 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Table 10. Mean EPDS Score and Prevalence Rates for Each State ............................................59 Table 11. EPDS Prevalence: WA Public Patients vs. WA Private Patients .............................. 59 Table12. Odds Ratios: Demographic Variable ............................................................................ 61 Table 13. Odds Ratios: Psychosocial Variables ........................................................................... 62 Table 14. Postnatal Depression (EPDS > 12) Prediction Model ................................................. 62 Page 7 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Executive Summary The beyondblue National Postnatal Depression program is an Australian public health initiative developed and implemented over four years, with a scope that makes it unique on a worldwide level. The Program focused on bringing about change in healthcare for women with perinatal depression, to improve outcomes for them and their families, in order to reduce the potentially devastating consequences on current and future generations. Multidisciplinary teams across seven States and Territories engaged with primary perinatal health care providers, in 43 different health services/regions. This involved over 40,000 pregnant women being screened directly and over 200,000 being reached by the Program’s publicity, educational and/or resource materials. The Program operated at a number of levels: ♦ introduction of routine screening for perinatal depression; ♦ provision of information to women and their families; ♦ education of, and support for, primary healthcare professionals; ♦ a specific focus on detection/intervention in each State. This project collected data on over 40,000 antenatal women and over 12,000 postnatal women. The key preliminary findings include: ♦ in Australia, rates of depression (as recorded on a validated, perinatal specific screening tool, the EPDS) are high in the general postnatal population (15.7%), similar to rates in other Westernised countries; ♦ antenatal rates of depression appear lower than postnatal rates (5.4% - 8.9% depending on cut-off score used) and, when trimester screened is considered, similar to other Westernised countries; ♦ for the first time, the importance of psychosocial risk factors is confirmed for the general Australian perinatal population. In particular, past history of abuse, prior history of depression, anxiety, lack of support, lower socio-economic status and a stressful pregnancy are all key factors; ♦ Indigenous Australian women are at heightened risk of depression, and psychosocial factors are of particular importance in generating this elevated rate. These high rates of depression and identification of key psychosocial risk factors highlight the importance of perinatal universal depression screening. Provision of information and the education of health professionals in depression identification and early intervention strategies must also take place. Universal depression screening has been controversial for a number of reasons. This Program has demonstrated that: ♦ a majority of women found screening acceptable when delivered with as part of routine care with her health provider; Page 8 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program that the standard screening tool used (the EPDS) was appropriate and superior to alternatives; ♦ a standardized, Indigenous version of the EPDS produces similar scores and is more acceptable to Indigenous Australian women; ♦ when screening was combined with information – in particular an information booklet given in pregnancy – screening significantly increased awareness of depression; ♦ help sought by those women who were part of the Program and were either not, or mildly, depressed, decreased. These women were more satisfied with what help they did seek and found the depression information received more useful. This suggests the increased awareness of emotional health issues resulting from this Program decreased need for extra help, and needs be a core part of routine screening so as to make best use of community resources. ♦ Depressed women were more likely than non-depressed women to seek help. However, a significant proportion did not seek help at all, even after screening, indicating substantial barriers. Some ways of overcoming barriers to seeking help were suggested by the following findings: ♦ linking women to their GP, who had been trained to routinely ask about depression, appears a critical step in increasing early identification and intervention; ♦ information about the treatment of depression was helpful in decreasing the reluctance of women to consider using antidepressant medication during the postnatal period; ♦ GP training had helped broaden the GPs range of treatment options; ♦ barriers to seeking assistance were identified in the specific State antenatal interventions and it was found that reluctance to engage was highest among those at high-risk and male partners. The PND Program developed a range of promotional, educational and resource materials which are available on it’s website (www.beyondblue.org.au/postnataldepression). The site includes information in 19 languages other then English, as well as for Indigenous women and multiple birth mothers, and depression management and Edinburgh Postnatal Depression Scale guides for health professionals. Health Professionals were: ♦ empowered to be able to deal with perinatally depressed women when they encountered them as part of their routine work. Provision of pathways-to-care protocols allowed these health professionals to deal with issues that previously they were at a loss to know what to do; ♦ highly supportive of screening and found training helpful; ♦ knowledge levels increased through training, however, midwives remained a group in need of extra training and support for the implementation of routine screening to be feasible; ♦ at each locale, a significant degree of commitment is required to adapt a blueprint for the specific needs and structure of the service, requiring management and service support. A “one-size-fits-all” approach is not appropriate although a blue-print for all services is required to ensure best minimal practice; Page 9 of 108 beyondblue National Postnatal Depression Program ♦ VOL I: National Screening Program teleconferencing to remote and rural areas could also provide education and training, but this was not without technical difficulties and, as elsewhere, needed to be ongoing. The PND Program has become an identified source locally, nationally and internationally for cutting edge information resources and provision of eduction. This is an enviable situation, which needs to be promoted in order to continue the work that has been started over the past 4 years. Recommendations The PND Program recommends: 1. A national advocacy group of key stakeholders be formed. Their task will be to promote the introduction of routine psychosocial assessment and referral pathways and consider relevant training and education needs. 2. Depression screening is a part of routine antenatal and postnatal care. 3. The use EPDS as the best available and most practical screening tool. 4. Use of additional key psychosocial questions to assess risk and planning perinatal care, in particular, level of support, past history of anxiety and depression and current stressors. 5. Antenatal screening in the third trimester. 6. Postnatal screening 6-8 weeks after childbirth. 7. All pregnant women are provided with an information and resource booklet on emotional health in the perinatal period. 8. Specific resources to address the needs particular groups, such as Indigenous, culturally and linguistically diverse, multiple birth mothers and male partners, be supported. 9. Screening programs need to be accompanied by ongoing training and support of all relevant health professionals involved in perinatal care. 10. Each obstetric/area-health service needs to develop a local care-pathway including appropriate referral and allied-health service links Page 10 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program National Action Plan To Implement Perinatal Depression Screening What Are The Current Problems? It has long been identified that services for perinatal women with a mood disorder are spread across many areas of the health sector with inadequate coordination. Where policy development in this area has occurred: ♦ implementation has been poor resulting in many service gaps; ♦ there are significant disparities between States and between private and public systems; ♦ there has been an overemphasis on physical health to the exclusion of emotional health. Research into perinatal depression has shown that: ♦ in primary health care settings, if depression is not routinely asked about, over 50% of cases are missed, highlighting the need for a systematic approach to perinatal psychosocial assessment; ♦ perinatal (i.e. antenatal and postnatal) mood disorders, such as depression and anxiety, are common; ♦ depression has high economic, personal and family costs, with significant potential effects beginning in pregnancy with an impact of maternal depression and anxiety on the developing foetal brain; ♦ during the perinatal period, suicide is the equal (with haemorrhage) leading cause of maternal death in Australia. Where To From Here? The beyondblue National Postnatal Depression Program has been highly successful in raising awareness of the importance of emotional health in the perinatal period, both within the general community and in health settings. The next steps will be to ensure that emotional health becomes a priority agenda item in health and that research is translated into both policy and practice. To date we have: ♦ positioned ourselves as an effective national group advocating for the need of health services to focus an perinatal emotional health; ♦ continued working with at least one “show-case” hospital in each State as an example of how depression-screening can be incorporated into routine perinatal care with appropriate staff training and feedback; ♦ forwarded a submission to the Senate inquiry into perinatal mental health services in Australia; ♦ provided policy advice to Federal & State Governments; ♦ drafted an information document to be sent to all stakeholders involved in the PND Program and all perinatal services in Australia (see Appendix A); Page 11 of 108 beyondblue National Postnatal Depression Program ♦ ♦ ♦ ♦ ♦ VOL I: National Screening Program met with Victorian Department of Health (on a number of occasions, including mental health, & early childhood), President and President elect of the College of Psychiatrists; formed a Perinatal Interest Group as part of the Royal Australian and New Zealand College of Psychiatrists, which meets regularly in three States; a broader group meets in another State; in Queensland, interviews with the Ministers, or their designated representatives, and the National Director in the offices of Family Services, of Child Protection and of Health are in process for September, 2005; formal interviews and contacts of the Queensland Director with The Australian College of Midwives Incorporated in Queensland and nationally; with The Australian and New Zealand College of Mental Health Nurses; and with the Queensland State Unit for Child Health Nurses in Queensland; had discussions with hospital/area-health services, looking at strategies for the implementation of routine screening using the EPDS. Whilst the beyondblue National PND Program is working diligently to focus attention on emotional health within routine perinatal health care, there remain many barriers to it becoming part of care universally. These include: ♦ stretched hospital resources; ♦ differing opinions as to the value of screening and the role of obstetric services; ♦ disparities between the states; ♦ the need for ongoing training and support for health workers; ♦ funding for ongoing resource materials; ♦ reluctance of women to seek help for emotional problems. Following the submission of this report to the beyondblue board, the PND Program anticipates the need for: ♦ formation of a National Advisory Group of key stakeholders. This groups will work with state bodies to ensure that perinatal depression is on the National Health Agenda at a number of levels; ♦ each State forming a Steering Committee of key stakeholders. This will include the State research teams but also broaden to key clinicians, researchers and managers. Their tasks will be to promote the introduction of routine psychosocial assessment and referral pathways and consider relevant training an education needs; ♦ develop a consensus document for perinatal care. NSW has developed an Integrated Perinatal and Infant Care Plan, which the PND Program supports, but this needs to be further developed with the addition of information package and education for a number of health professional groups that come into contact with perinatal women. Importantly, it must be adapted across different setting and States, with particular reference to implementation issues, referral and crossdisciplinary links; Page 12 of 108 beyondblue National Postnatal Depression Program ♦ ♦ ♦ ♦ ♦ ♦ VOL I: National Screening Program provision of support and expertise, through ongoing staff training and education, to hospitals to facilitate implementation of depression screening programs or to take over existing programs; to continue the valuable links between the research involved in the PND Program and to welcome others to work together on the issue; further analysis of the vast amount of data collected with publications locally and internationally; ongoing training and presentations to public, professionals and stakeholders, both locally and internationally, of the data and recommendations in this report; presentation of the findings of the PND Program at the Australasian Marce Conference in Melbourne in September 2005. Seventeen abstracts, either directly involving or related to the PND Program have been accepted by the conference organizers; ongoing research in perinatal depression, furthering the work of this Program and progressing our understanding of perinatal depression. This includes two established projects: − “EPDS Tool Pilot”. Condon, Alder, Sved-Williams et al. Funded by SA State Government. This continues from the National PND Program, specifically aiming to introduce, and evaluate the use of, the EDPS into child-youth health centres − “Optimisiming Emotional Health During Pregnancy And Early Parenthood”. Buist, Milgrom, Bilszta & Ericksen. Victorian Centre of Excellence Grant. This study aims to further explore the reluctance to seeking treatment for perinatal depression (as evidenced by the National PND Program) and piloting of methods to overcomes this. Applications will also be submitted to other funding bodies, such as NHMRC and NARSAD, to build upon the projects initiated as part of the PND Program. Page 13 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Reflections From The National Co-Ordinator A/Professor Buist is Associate Professor of Psychiatry at Austin Health and University of Melbourne, the current Director of the Banksia House Mother Baby Unit, and former Director of Psychiatry at the Mercy Hospital for Women. Both her research Masters and MD investigated postnatal disorders and she has written and researched extensively in this area, including a textbook for GPs. She regularly teaches to a variety of health professionals on these topics. She has many years clinical and research experience in Women's Mental Health and involvement in the International and Australasian Marcé Society (the latter of which she is the President). In 1999 she was awarded the Organon Travelling Fellowship by the Australian Society of Psychosomatic Medicine and the AMA Women's Health Award. The beyondblue National Postnatal Depression was an ambitious program involving a large number of multidisciplinary teams across Australia in both antenatal and postnatal health care settings. It tackled an enormously important health problem that affects the lives of 13-15% of women and their families. The Program raised community awareness of perinatal depression, investigated early identification and intervention strategies and took the lead in training health professionals in the diagnosis and management of mood disorders during pregnancy and early parenthood. Understanding the particular needs of male partners, multiple-birth families, Indigenous women and women from culturally and linguistically diverse backgrounds, was also a major focus. The Program began its planning stage in 2001 and became operational in 2002, spreading to over 43 antenatal hospitals/area-health services and reaching over 200,000 women and health professionals from a wide range of service providers. Unlike any other project any of us had been involved in, it was not just a research project but also a public health initiative – and a passion. The dedication, enthusiasm and long hours beyond the call of duty from all those involved has been extraordinary. My thanks go to all team members across Australia for bringing together this unique project that would have been impossible without them. It has been a pleasure to know and work with them all. As a result of an enormous amount of hard work, this project has provided a wealth of information on the mental health of women giving birth in Australia, as well as the feasibility and acceptability of perinatal depression screening, usefulness of education program and increasing the awareness of the emotional health needs of women during pregnancy and early parenthood. The beyondblue PND Program, and this report, aims at making a difference - the findings can, and we hope will, be used by health professionals, policy planners and politicians throughout the country to improve the outcomes for all women giving birth, their children and the families that support them. Page 14 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Reflections From Victoria And Tasmania Professor Milgrom is a Professor of Psychology, University of Melbourne and Director of Clinical and Health Psychology at Austin Health. She has been involved in clinical practice and research on mother-infant interaction and postnatal depression since 1978 and has held a Harkness Fellowship in the USA as well as an O’Rourke Fellowship in Paris for working with families and infants. Professor Milgrom developed a model centre for families and infants, the ‘Infant Clinic’ and established the Parent-Infant Research Institute (PIRI) in 2001, which aims to become the pre-eminent body in Australia developing interventions for parent-infant difficulties. Professor Milgrom has published widely in the area and held a number of long-term research grants. She is also active professionally and has held positions in the Australian Association for Infant Mental Health (Victorian Branch) and the College of Health Psychologists of the Australian Psychological Society. Being part of the beyondblue National PND Program has provided us with a unique opportunity to influence the emotional health care of Australian women. We have been privileged to be part of a significant movement in changing practice to ensure that asking women if they are depressed, is considered a critical practice by professionals involved with pregnant and postpartum families. The scope of the program was immense and the opportunity to sample such a large segment of the population has provided us with a wealth of information. The success we have had in rolling it out and witnessing change in attitudes and care within the maternity hospitals and community settings has been fascinating and gratifying. It makes the many challenges we faced as a Victorian team worthwhile, including the sad loss of Rachael McCarthy, one of our team. The lessons learned will stand us in good stead in thinking about future projects and implementing them, and our commitment to continue working with this population has grown. In addition, the PND Program called on researchers around Australia to work together in order to produce a research program and public health initiative that was standardized and of high quality. These national working relationships will set the scene for future collaboration, which strengthens the research community in Australia making it an international leader in the field. It has changed the culture of Australian research in PND with everyone working with a common focus. There have been many rewards in being associated with the high profile of beyondblue. The general promotional activities of beyondblue have supported and contributed to our success and we thank them for their guidance and support. In particular, beyondblue’s approach in budgeting for publications (pamphlets, flyers, posters and booklets) has changed the attitudes of health workers. The impact of these has been extensive and their existence helps training and raising of awareness, which will endure for longer than if, they were not available. In summary, it has been very fulfilling being part of a national body that is having an impact on practice and policy regarding screening for perinatal depression, and women’s lives as a consequence. The “whole is greater that the parts…”- the involvement of multiple sites around Australia has strengthened the impact of the Program, raised its profile both in Australia and internationally, and helped many women and their families. Page 15 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Reflections From South Australia Professor Condon is Professor of Psychiatry at Flinders University of South Australia and Director of Psychiatry at the Repatriation General Hospital in Adelaide. For 15 years he has operated a specialist clinic at Flinders Medical Centre for women referred with problems in the area of psychosocial obstetrics and gynaecology. He has received funding from the NH & MRC for a number of projects, including the determinants of antenatal and postnatal attachment; the impact of the transition to fatherhood on male mental health; adolescents’ idealized attitudes to pregnancy and parenthood; and adolescent pregnancy prevention through interventions targeting young males. Between 1993 and 1999, he was chief examiner of the Royal Australian and New Zealand College of Psychiatrists and is currently a member of General Council of that College. If you ask someone today “Have you heard of beyondblue?”, the answer is most likely to be “Yes, I have”. This affirmation represents the success of the beyondblue PND Program at several levels. Many women have participated in the program and some have been screened two or three times during the program’s duration. These women are very positive about their involvement: a confirmation of their own feelings about their mental health state: whether they are well or otherwise. The primary professional health workers: medical practitioners, midwives and maternal and child health nurses of perinatal women receive objective information which contributes to the clinical management of participating women. Health care providers have received education and skills development, particularly in the country areas in South Australia and have been energised to establish a response to postnatal depression at a regional level. Such processes outline the cross professional roles and responsibilities aimed at the early recognition and prompt treatment of women who experience antenatal and/or postnatal depression. This ensures the longevity of the beyondblue program and thus represents the significance and necessity of such a program in mental health service provision in Australia. The funding of this program has provided a wonderful opportunity to do something really worthwhile in relation to strategic approaches to women’s mental health. This has been too good an opportunity to sit back and be complacent. It has been an honour to contribute to such exciting developments in women’s health care. Page 16 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Reflections From Western Australia From 2001 to Dec 2003 Prof Sherryl Pope was the Western Australian Coordinator of the beyondblue National Postnatal Depression Program. Dr Speelman is currently Head of the School of Psychology and has been the Western Australia co-ordinator since Jan 2004. He teaches in both the undergraduate and postgraduate programmes. His research work is primarily in the field of cognitive psychology, with particular interests in skill acquisition and memory. His recent publications have examined the effects of different types of training on skill transfer, and the relationship between skill acquisition and implicit memory. An additional interest is examining the relationship between implicit expertise and transfer. He is also involved in marrying his previous life as a rock musician with research on memory for music. He is currently writing a book about learning. Since our initial formation, with the employment of the first team member Jocelyn Bristol, the Western Australian beyondblue PND Program team has worked cohesively and with a strong sense of purpose – motivated by our individual beliefs in and dedication to the Program’s goals and by our tireless and enigmatic Coordinator Associate Professor Sherryl Pope. This dedication and strong sense of camaraderie was only strengthened with the tragic and sudden passing of Sherryl Pope. With a renewed energy, the WA team has set out to make the WA project ‘the best in Australia’ and make Sherryl proud. We believe our efforts have been reflected in the quality and quantity of data obtained for the national database from WA and that we indeed have succeeded in making Sherryl Pope proud of her team. Upon reflection, the aspect of the project the team has found the most rewarding is the strong sense that we are making a real difference to people’s lives. This research project has been quite unique in that we have all felt that we are also ‘giving back’ to the community with the provision of resources, education for metropolitan and rural health professionals, and the screening and referrals offered to participants. When depression is picked up through screening, when otherwise it might not have been, and women are supported into seeking help, the long term benefits to these women and their families can be quite profound. “I have undertaken many follow up EPDS by phone on postnatal women and on numerous occasions have dealt with depressed women. At times I have provided the only opportunity these women have had to express their current feelings of, at times, despair. I have linked numerous women into referral agencies so that there depression could be addressed and many times women have expressed thanks and relief to me that they are seeking help as a result of my phone contact” (Jocelyn Bristol, Research Midwife). Personally, each of us has gained valuable skills, contacts and knowledge that we can take with us into future endeavours and feel ‘blessed’ to have been involved with this project and to have had the opportunity to carry on the legacy of Dr Sheryl Pope. Page 17 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Reflections From Queensland Professor Hayes is the foundation Professor of Nursing and foundation Head of School at James Cook University, appointed in 1989. Barbara Hayes is licensed to practice in general nursing, midwifery and mental health nursing. She gained her first research degree at the University of Melbourne and her masters and doctoral degrees at the University of California, San Francisco as a WK Kellogg Fellow. Barbara Hayes has forged her skills in midwifery and mental health nursing with her research training to establish a strong basis for her research into the recognition and management of ante and postnatal anxiety and depression. Working with ease across disciplinary boundaries and within the professions of nursing and midwifery, Barbara Hayes is committed to quality, holistic care to childbearing women. One of her particular concerns is to explore, in full partnership with Indigenous midwives, ways in which culturally sensitive and culturally safe care can be accessible to Indigenous childbearing women. The following is a compilation of thoughts and experiences from all members of the Queensland research team. The following three aspects of context in Queensland provide a unique dimension to the project: (1) Queensland was the only State with a formal program for Indigenous women; (2) the team was based in Townsville but was over a thousand kilometres from three of the sites and over 500 kilometres from others. The experiences can be expressed under the following headings but, in so doing, will lose a lot of evocative detail: (1) Compassion and Commitment; (2) Increased Knowledge and Skill Acquisition; and (3) Appreciation of the national and local team and desire for future involvement. Compassion and Commitment: Every member of the team shared a passion for Women’s Perinatal Emotional and Mental Health. The research team shared a complementary skill mix that enabled members to forge highly effective interpersonal bonds, over long distances, both with the research midwives and with the various Health Service Districts in which the beyondblue project was established. This skill mix ensured that the ‘duty-of-care’ inherent in eliciting ‘informed consent’ was met in highly efficient and effective ways. Members mentioned in their autobiographical accounts “ (it was a) privilege to be part of something that recognized the needs of women from my Indigenous people”; “ privilege to be part of a national study that was so effective in making changes for perinatal women”. Increased Knowledge and Skill Acquisition: All members of the team expressed greatly increased knowledge of perinatal emotional and mental health in a wide range of both Indigenous and non-Indigenous women. Increased skill acquisition in assisting midwives, child health nurses, rural nurses and GPs in early recognition were widely experienced and the generating of robust referral pathways was an outstanding achievement. Appreciation of the national and local team and Desire for future involvement: We acknowledge Professor Anne Buist’s leadership, Dr Justin Bilszta’s national co-ordination, the collegiality of the other state teams in addition to the deep and enduring collegiality of the Queensland team. We deeply regret the ending of the project as the research team developed highly cohesive bonds, which facilitated the achievement of the goals of the project. We appreciate the vision of beyondblue in providing the funding at this crucial time in recognition and management of a major public health problem. We deeply regret the death of two members of the National Team: Associate Professor Sherryl Pope and Ms Rachael McCarthy. Page 18 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Reflections From New South Wales Professor Barnett is a graduate in medicine of the University of Aberdeen and a Fellow of the Royal Australian and New Zealand College of Psychiatrists. She has a doctoral degree from the University of New South Wales, and held a Chair of Perinatal and Infant Psychiatry at that University. Professor Barnett's key interests are the health and wellbeing of infants, children, adolescents and their parents. To that end she has established various services addressing their needs and is involved in an extensive research program on issues relevant to prevention, early intervention and health promotion. She has been involved in many College and other professional committees. She has been President of the Australian Psychosomatic Obstetrics and Gynaecology, the Infant Mental Health and the Australasian Marce Societies and is President Elect of the International Marce Society. She is Chair of the Board of Directors of the Karitane, Caring for Families, organization. Professor Barnett’s team is committed to ensuring that the needs of migrant and indigenous families are appropriately included in policy, planning and implementation. I’m sure I speak on behalf of all beyondblue staff members and associated when I say they we feel very fortunate to have been involved with the beyondblue National Postnatal Depression Program. We are all deeply passionate about improving the mental health of mothers, fathers and their infants and therefore consider ourselves privileged to have been a part of a service that will increase the quality of life for families and consequently the community in general. We are excited about the great work that has been accomplished in this State and hope that the beyondblue program is only the beginning of National acknowledgement of the importance of perinatal mental health. We would like to thank the beyondblue Board for their insight in supporting and funding a perinatal mental health program and allowing us this unique opportunity to research and raise awareness of a public health issue that we know if invested in now will have invaluable benefits for generations to come. I would also like to acknowledge the work of A/Prof Marie-Paule Austin and Dr Nick Kowalenko for co-ordinating the PND Program at Royal Hospital for Women and Royal North Shore Hospital, respectively. Page 19 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Reflections From The Australian Capital Territory Professor Ellwood is a practicing obstetrician and certified sub specialist in MaternalFoetal Medicine who is interested in teaching and research in high risk obstetrics. Currently he is the President of the Perinatal Society of Australia and New Zealand (PSANZ). He is an Executive Member of Women’s Health Australia (WHA). He is also a member of the Advisory Faculty of Advanced Life Support in Obstetrics (ALSO). He is the Past Chair of the Maternal-Foetal Medicine Committee of the Royal Australian & New Zealand College of Obstetricians & Gynaecologists (RANZCOG), and the current Chair of the Research Assessment Sub-Committee, which oversees research training for trainees. He is a Past Chair of the High Risk Obstetric Advisory Group of NSW Perinatal Services Network (HROAG). He is widely published and sits on the Advisory Board of the publication Australian Doctor. Professor Ellwood’s expert opinion is sought in a wide range of pregnancy and birth related legal issues The ACT set a target of recruiting 1000 mothers to the program. This is approximately 20% of the annual birthing population. During 2004, 987 mothers were recruited to study and their response to the program has been very positive. More than 1000 information booklets, posters, pamphlets and booklets were distributed widely. These have proven to be very popular with an increase in requests for information booklets to be made available to community services. There have also been significant steps to improve the pathways to help and support for identified women. Antenatal staff was involved in the development and trial of new management plans, which were well received. It was rewarding to witness first hand how midwives want to help women by being involved in the program. Whilst it has been difficult to estimate the resources required to conduct a complex mental health early identification program, different sites have responded differently to the increased demands on staff time. Some antenatal clinics increased the time available for the booking-in visit to accommodate the addition paperwork and time to talk with mothers. Management supported staff to attend training sessions in the new assessment procedures and referral pathways. Maternal and Child Health Nurses were given extended appointments to accommodate the increased time to administer and discuss screening results. Over time both antenatal and postnatal nurses became more efficient and confident with the new procedures. Generally their attitude to the changed work practices became more positive over time. Midwives and Mach nurses reported that it was important for that increased opportunity for women to talk about their feelings. During the program we all developed greater understanding of the processes involved in introducing new practices and how people work together to overcome the inevitable obstacles. In summary, the beyondblue PND program has generally been very successful and embraced by both health professionals and Canberra mothers. Page 20 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Vale: Professor Sherryl Pope and Rachael McCarthy Sherryl Pope BA (Hons) MPsychology (Clinical) PhD, was Associate Professor of Psychology and Coordinator of the Postgraduate Clinical Program in the School of Psychology at Edith Cowan University, Western Australia and an Honorary Research Fellow of the Women & Infants Research Foundation (WIRF). Sherryl had been involved in Psychology for 25 years working in the areas of Psychiatry, Drugs and Alcohol, Behavioural Medicine and maintaining a successful private practice. Prior to studying psychology she was a Registered Nurse and Midwife. Sherryl was formerly the Chief Clinical Psychologist at King Edward Memorial Hospital for Women from 1989 to 1998, establishing the first specific Clinical Psychology services in a tertiary level Australian Obstetrics, Gynaecology and Neonatal Paediatric teaching hospital. She was Chief Investigator of the Postnatal Depression Prevention Study funded by Healthway for 3 years (19921995) and has been the Chief Investigator of several other large postnatal depression studies in the past decade. Her PhD research investigated couples’ adjustment to parenting and postnatal depression following the preterm or full-term birth of an infant. Sherryl was the Project Consultant for the statewide Childbirth Stress and Depression Project based at KEMH (1995-1998), funded by the National Mental Health Strategy. She was the first author of a systematic literature review concerning postnatal depression published by the NHMRC (2000), that was designed to form the basis for the development of national clinical practice guidelines, and “Postnatal Depression: more than just the baby blues” a consumer guide for national distribution. From 2001 to 2003 Sherryl was the Western Australian Coordinator of the beyondblue National Postnatal Depression Program. Sherryl was an inspiration to all those lucky enough to have worked with her or taught by her and is dearly missed. Rachael McCarthy has been a very dear and valued member of the Victorian Project team. She has worked in the Clinical and Health Psychology Department Austin Health for over 10 years, and as part of the VIC component of the PND Program for three years. Rachael was a talented therapist who had a flare for her work and a real understanding of her patient’s struggles. She worked in a variety of service areas, including: Staff Counselling, Spinal Unit, Banksia House Mother and Baby Unit and our Infant Clinic Rachael has left behind as a legacy, a number of programs that she has been instrumental in developing, evaluating and running over the last few years. She also leaves behind a very large circle of friends, acquaintances and colleagues who are all struggling to come to terms with her passing and the enormous loss that this represents both personally and professionally. Page 21 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Aims & Objectives Of The beyondblue National Postnatal Depression Program The aims and objectives of the beyondblue National Postnatal Depression Program have focused around five key priority areas: 1. Establishment and Evaluation of the Feasibility of Routine Screening for Antenatal and Postnatal Depression at Major Maternity Hospitals/Health Services in Australia. 2. Development of Materials to Address Community and Health Professional Awareness of Antenatal and Postnatal Depression and its Treatment. This was aimed to assist in demystifying perinatal depression and to improve its recognition, so to minimise the impact of depression on women, their partners and families and the wider community. Accessibility was aimed at the maximum number of women, including those from Indigenous and culturally and linguistically diverse backgrounds. 3. Evaluation of Change in Health Professionals and Postnatal Women’s Knowledge and Awareness of Perinatal Mood Disorders as a result of this Program. 4. Provision of a National Database of Young Families in Australia to investigate: ♦ the prevalence of pregnancy-related depression; ♦ importance of different risk factors on the development of depression in an Australian population and; ♦ when best to screen and who is best to perform the screen. 5. Evidence of Efficacy of Early Intervention Initiatives in the following groups: 1. risk of poor parenting in depressed women; 2. culturally and linguistically diverse; 3. rural; 4. Indigenous; 5. fathers/male partners; 6. multiple-birth families. The beyondblue National PND Program provides a leading direction in postnatal disorders for Australia and the world through these priority areas. Page 22 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program 1. Establishment and Evaluation of the Introduction of Routine Screening for Antenatal and Postnatal Depression at Major Maternity Hospitals/Health Services in Australia. Overview The introduction of antenatal and postnatal depression screening and protocols for the sharing of patient information, in 43 antenatal hospitals/area heath services across Australia, has been implemented since 2002. Overall, screening for depression: ♦ had clear advantages of early identification and intervention; ♦ was acceptable to a vast majority of women (85%) – they found the questionnaires easy to complete and were comfortable in doing so; ♦ was acceptable and feasible for those health professional (98%) who were involved . Acceptability and feasibility of screening was closely associated with education and training, as well as increasing levels of awareness. This is discussed further in Section 3 (Evaluation of Changes in Health Professional and General Community’s Knowledge and Awareness of Perinatal Mood Disorders). Some hospitals elected not to, or only partially participate, and it is clear from our experience and results that for routine screening to be implemented the process must: ♦ be supported by all levels of hospital management; ♦ have adequate infrastructure; ♦ develop a site-specific model for identification and management of distressed women; ♦ have as part of it ongoing education and support for staff. Each hospital and area health service will have individual needs and as part of the successful implementation, requires links and supports for the care of depressed women. Such integration requires directive not just from the bottom up, but to be driven also by policy, which prioritises mental health screening as an integral part of perinatal health care. Page 23 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program What Have We Learnt? The PND Program has been a culmination of an enormous amount of work by each of the State-based research teams. For all teams this has been unchartered territory and the learning curve extremely steep. As this Program has been a world-first, the evidence found will guide postnatal depression screening policy, not just in Australia, but also across the world. Aside from the vast database of pregnant and early postnatal women and the large number of depression resources that have been developed, this Program has demonstrated that with the appropriate support and guidance, implementation of depression-screening protocols within primary health care settings can be successfully achieved. Other positives include: ♦ ♦ ♦ ♦ ♦ ♦ the involvement of each state has strengthened the impact of the Program and raised its profile both in Australia and internationally; women and their families are actively interested and willing to participate in a screening process, which assesses mental health and wellbeing. This demonstrates the willingness of women to focus on mental health issues in their childbearing years; establishing depression-screening protocols as part of routine clinical practice has demonstrated that appropriate training for the relevant staff, evaluation systems, referral pathways and community based support services are essential ingredients. ; evaluating the introduction of an accurate prediction tool for postnatal depression. The Program has allowed consultation with key stakeholders about the risk factor tool’s acceptability and feasibility for routine use; establishing the Edinburgh Postnatal Depression Scale (EPDS) as the recognised depressionscreening tool. This includes reviewing current guidelines regarding the use of the EPDS antenatally and postnatally; establishing clear guidelines for the identification and management of maternal depression. These guidelines should include information on the following: − ‘the ideal’ period for antenatal and postnatal screening; − flexible management plans for mothers identified as depressed based on local resources; − recommended interventions based on EPDS results; − which personnel/ professionals should conduct screening; − details about coordination of care with general practitioners and other treating health professionals; − procedures for mothers with suicide risk or safety issues. Areas, which in hindsight, needed further work or provided unexpected problems include: • • implementation of screening in most sites took significantly longer than expected due to factors such as ethics committee requirements or reluctance by staff to implement new procedures; whilst a strength of the Program was the vast experience of the research teams, differences in the views and practices regarding implementation of screening across the states meant Page 24 of 108 beyondblue National Postnatal Depression Program • • • • VOL I: National Screening Program that compromises needed to be made. Whist this doesn’t detract from the final “product”, it highlights that a one-size-fits-all model isn’t the way to go; the original proposal under-estimated the level of work needed in some areas, especially the postnatal screening follow-ups that required extensive work to achieve a statistically acceptable response rate. This has hampered, to some degree, the amount of data that could be collected at this time point; more time was needed to establish the Program so that it operates independently and routinely in all midwifery clinics. The most important aspect of the beyondblue Program is its sustainability in the long term. Changing current midwifery practice so that it evolves and responds to the need to screen all mothers for signs and symptoms of depression requires extensive consultation, training and time; there is an urgent need for longer-term follow-up of screened women to establish what happens to them after they were screened. This will allow us to determine rates of false positive and false negative risk classifications using present screening methods, and will indicate where gaps in service provision may be. Reasons why high-risk women fail to take up services needs to be better understood. The beyondblue Centre Of Excellence has funded a project in this area in it’s last round of research grants (Optimisiming Emotional Health During Pregnancy And Early Parenthood. Buist, Milgrom, Bilszta and Ericksen); even though screening is able to identify women with symptoms of depression being able to get these women to accept referral is a whole new challenge that warrants further investigation and efforts. Implementation of Perinatal Depression Screening Implementation of perinatal depression screening was a complex and time-consuming process. It has involved establishing networks in each areas where women are recruited, development of perinatal depression information for both women and their treating health professionals, obtaining ethics approval, liaison with each of the maternity hospitals and setting up of screening and referral procedures at antenatal clinics. The basic screening protocol is described in Figure 1. Hospitals in each State and the ACT were invited to participate. These were predominately city and suburban public hospitals, whilst a representation of private, rural and remote antenatal services was also included. Some hospitals/area-health services did not take up the invitation to be involved in the PND Program, or did so only partially, for the following reasons: philosophical objection to screening, other current research projects running within the antenatal service, staffing/practical issues and perceived inadequate support from PND Program staff. The implementation procedure has been hard to quantify but is the reason why the PND Program has been so well accepted. Procedures differed not only between the different States, but also between hospitals in the same state. Ethics committee requirements, staff and management attitudes, levels of staff knowledge, availability of appropriate referral pathways and allied-health services and the individual quirks of each hospital, all impacted heavily on the screening protocol. Page 25 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program There are multiple changes required within the hospital and community including changes to clinical practice, administration tasks, data collection, coordination of care and referral patterns. These require extensive consultation with administration and clinical staff as well as management. The stakeholders involved in the change process have varying levels of expertise, knowledge, interest and time available to participate. This issue invariably slows the rate of change as it takes time to manage these issues Figure 1. The Perinatal Depression Screening Protocol, as Designed by the National PND Program From their experiences, each of the States have highlighted the following key criteria for successful introduction of screening: ♦ Raising awareness and increasing understanding – Raising awareness with executive and senior clinicians about the importance of assessment and early intervention for improving longterm outcomes is fundamental to the successful uptake of perinatal psychosocial assessment. ♦ Adequate infrastructure – Fundamental to the successful implementation of psychosocial assessment is the availability of adequate human resources. For the antenatal component this means an appropriate establishment of antenatal clinic midwives to undertake the assessment and a network of staff to follow up, support and case manage clients. The staff network will ideally compromise a social worker, psychologist and psychiatric staff and may include community-based nurses and non-government community based personnel. A designated liaison position for the ongoing oversight of the service linkages and the monitoring of the client’s engagement with services is highly recommended. A similar infrastructure would be required for the postnatal component. Crossover between the antenatal and postnatal period will be vital to ensure continuity of care. ♦ Staff education, training and supervision – Education for staff working within the maternity/postnatal facilities regarding the benefits of early identification and intervention is Page 26 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program essential. Basic, advanced and other relevant training needs to be available to staff on an ongoing basis to account for staff attrition and rotation. Clinical/reflective supervision should also be provided. ♦ Establishment of a steering committee – Key senior maternity service staff from across the health service should participate in planning for the implementation of screening. This committee forum would be used to develop a shared understanding of the concept, ascertain roles and responsibilities identify issues and develop strategies for successful implementation. ♦ Establishment of a local committee to manage implementation – Each hospital implementing screening should have their own committee. This committee will meet regularly discuss local issues and further strengthen the process, assist in the development and dissemination of policies, protocols and other relevant resources, oversee implementation and ensure adequate data collection and analysis. ♦ Utilisation of an existing meeting or establishment of a multidisciplinary intake (postassessment) meeting – Some referrals may be addressed immediately but most will be deferred to a weekly intake meeting for discussion including review of individual psychosocial assessment, allocation of referrals and feedback. A multidisciplinary approach to intake and the development of referral pathways is recommended. ♦ Identify service partners and the role that they play in service delivery to women and their families – Development of a local service and resource directory needs to be undertaken to identify service partners and the specific service that is offered. The information within this resource directory will assist staff in gaining an awareness and better understanding of a range of available resources and services. ♦ Feedback mechanisms established – Feedback mechanisms for clinicians needs to be established at various levels to ensure that appropriate continuity of care is provided. Evaluation of the Feasibility and Acceptability of Introducing Perinatal Depression Screening A random sample of health professionals and postnatal women, involved in education and/or screening, were surveyed at the completion of the project. This is reported fully in Section 3, but included in this survey were questions on the “experience of screening”. In evaluating the impact of screening, 97% of mothers questioned, reported that they had the reason for EPDS being administered explained. Of note 83% of women found the EPDS easy to complete (0.7% found it more than a bit difficult) and 85% were completely comfortable (1.9% were quite or very uncomfortable) in answering the questions. Of those who had a high EPDS score (and who responded to the question – there was a 71% response rate to this question), 81% agreed with the “diagnosis” and 19% did not. Overall, 23% were relieved to be told their EPDS score and what it meant and 31% were at least a little upset. Of those who disagreed with their EPDS score, 26% were at least a little upset, suggesting disagreement did not have a significant relationship to their reaction to being told their score (and Page 27 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program perhaps more likely to be associated with the underlying depression). In using the EPDS we did not diagnose depression; what we did was to screen women who, because they were pregnant or postnatal, were 'at risk' for depression; a diagnosis of depression could only be made later after the woman was assessed using a standardised depression protocol. Experience of screening for health professionals is reported in Table 1. Of note, there was a significant increase in the use of the EPDS by GPs since baseline (20% to 54%); 20% of the GPs had cared for women who been involved in the Program, and received letters and management guide. Table 1. Health Professionals Screening Experience GP MCHN Midwife Use of EPDS (%) 54 89 68.5 Usefulness of EPDS (%) 54% 75% 57% Comfort in Using EPDS (%) 80% 83% 61% Mother’s Comfort in completing EPDS (%) 73% 77% 83% Intent to continue using EPDS (%) 98% 99% 97% For those not screening, the most common reasons given were that they would rather ask about symptoms (60% GPs cp 37% at baseline), or it was not policy to do so (44% MCHN, 47% midwives). For about 10% of MCHNs and GPs, lack of confidence in the instrument was cited. Only two health professionals said they did not believe in routine screening. The results of this study show strong support for the use of the EPDS by both health professionals and women. There are high rates of acceptance, level of comfort and ease of completion with the screening tool. Distress is minimal and appears more related to the underlying condition than the test itself. Introduction of such a program hinges, however, on adequate training and support – which needs to be an ongoing process. From top left - Staff from the family Birthing Centre at the Angliss Hospital VIC; Workers at Uniting Care Connections, Starting Out Program, Ringwood VIC; Photo used on the front page of the PND Program web-site taken from the latest beyondblue TV advertising campaign; Health professionals and a consumer with Jennie Ericksen at the launch of screening at Hamilton Hospital; Family at the launch of the first screening hospital in VIC, the Mercy Hospital Werribee, in August 2002; The Hon Mr Jeff Kennett at the launch of the National PND Program in Sept 2001; photo featured in community newspapers in the Werribee area promoting the PND Program at Werribee Mercy Hospital. Page 28 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program 2. Development of Materials to Address Community and Health Professional Awareness of Perinatal Depression and its Treatment Overview In keeping with the philosophy of beyondblue, a major aim of the National PND Program was a public health initiative to increase awareness of perinatal depression amongst the general community and health professionals. This was achieved by a multifaceted approach: Perinatal Women and Their Families ♦ Screening as many women as possible, and in doing so providing them with information about emotional health in pregnancy and early parenthood (205,000 women received an information booklet about emotional health during pregnancy and early parenthood). This, unlike many similar initiatives, has included information for those from culturally and linguistically diverse backgrounds (Arabic and Vietnamese booklets as well as translations on the PND Program website in 19 languages) and specific information for those having multiple births; ♦ Provision of information postnatally in ALL child health centres in Australia (600,000 pamphlets); ♦ Promotional posters in antenatal clinics, GP clinics and Maternal-Child Health centres; ♦ 244 newspaper/magazine articles; ♦ 215 TV, radio and promotional activities. Health Professionals ♦ Health professionals from 160 different organizations including maternity/obstetrics, maternalchild health, psychology, psychiatry and community & primary mental health, received training in the detection and management of perinatal depression; ♦ 33,500 depression management guides and 25,000 guides to the use of the EPDS have been distributed Page 29 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Health Professional Training The acceptability and feasibility of screening are closely linked to training of health professionals. The need for this was highlighted in our baseline findings of lower recognition of antenatal depression, anxiety about medication in pregnancy and misconceptions about postpartum psychosis. Training was well received and welcomed by a majority of health professionals, with more requested. See Section 3 Evidence for evaluating changes in health professional and general community’s knowledge of perinatal mood disorders for further discussion of this evaluation. A total of 160 groups and organizations received training. A detailed list of these is in Appendix B. The primary focus of training was on three main stakeholders – GPs, midwives and MCHNs. However, the PND Program also provided training to psychiatrists, psychologists, medical students, primary-mental health teams, community-health workers (including Aboriginal healthworkers and women Elders) and health administrators. At the midwife/maternal-child health nurse (MCHN) level, the training focus was on detection and management of perinatal mood disorders: ♦ what are the signs, symptoms and causes of perinatal depression? ♦ how do I talk about perinatal depression? ♦ how do I distinguish between real depression and “just a bad day”? ♦ how do I develop a management plan? ♦ when should I get a GP involved? ♦ what do I do if a woman says when wants to harm herself and/or her baby? ♦ how do I get a woman the help she needs? ♦ I’m not a counsellor, what do I do if a woman wants to tell me everything that’s happened in her life? Considerable time was also taken to training nursing staff on the use of the Edinburgh Postnatal Depression Scale (EPDS). There are many misconceptions and misunderstandings about the use of the EPDS. Training sought to teach the staff how to administer and use the EPDS for investigating perinatal depression, how to interpret “cut-off scores” and using the EPDS as a starting point for discussing psychosocial issues. For General Practitioners (GPs), the training focus was similar (i.e. detection of depression and development of a management plan) but was extended in the areas of: ♦ the use of antidepressant/psycho-active medication during pregnancy and breastfeeding; ♦ management of postpartum psychosis or postnatal depression in the presence of other mental-health disorders ; ♦ consultation and liaison with mental-health specialists; ♦ links with other services and resources. The guidelines developed by the PND Program for the suggested minimum information to be provided at training sessions are in Appendix C. To also assist in training, there has been development of a “Guide to Depression Management” and a “Guide to Using the Edinburgh Postnatal Depression Scale”. Page 30 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Whilst health professionals have been provided with training in the areas where the Program has a presence, there remains the need for both introductory training in those areas new to the PND Program and ongoing training to consolidate knowledge for those already familiar with the Program. To date, our education programs have not targeted professional groups such as obstetricians or paediatricians, thus a continuation of the Program would see a focus on the delivery of educational programs to these specific medical practitioner groups. Consumer input to health professional training, to give a face to the lived experience of perinatal depression, is also required. The PND Program is currently liasing with beyondbabyblues and the various State-based PND support groups, to develop a single training package, which best reflects the clinical, research and consumer knowledge that has been gained over the last three years. From top left: Family photo used on the promotional posters; GP liaison officers from Division of General Practice Northern Tasmania; Midwives and allied health staff at PND training, Northern Hospital Nov 2004; photo used on the front cover of the Arabic PND booklet; Ms Sara Brown, PND sufferer, at the launch of the National PND Program Sept 2001; Launceston General Hospital midwives at the launch of screening Oct 2003; photo used for the front cover of the Vietnamese PND booklet. Page 31 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Media and Promotion Improving the understanding and awareness of the general community and health professionals has been a key priority area for the PND Program To achieve this the Program has taken a number of different approaches: ♦ health professional training – as described in the previous section; ♦ development of information and promotion resources – a postnatal depression information booklet and pamphlet, a series of posters and a website; ♦ active participation in community forums; ♦ presentations at national and international scientific conferences and; ♦ providing journalists, government departments, health services and the coroner’s office with commentary on postnatal depression issues. Over the period that the PND Program has been active, it has participated in: 244 newspaper/magazine articles (see Appendix D, for detailed list) ♦ 215 TV, radio and promotional activities (see Appendix D, for detailed list) ♦ 71,500 web-site visits ♦ 73 scientific conferences (see Appendix E, for detailed list) ♦ Page 32 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Postnatal Depression Information Booklet “Emotional Health During Pregnancy and Early Parenthood” 1st reprint 2nd reprint 3rd reprint The PND information booklet was an important component of the PND Program for two reasons. Firstly, it provided a resource for nursing staff that helped them feel more comfortable and able to deal with women with perinatal distress. Feedback regarding the booklet has been hugely positive and demand for it has far exceeded initial expectations. Secondly, the Program wanted to evaluate the impact of giving women information about depression during pregnancy and early parenthood, during the antenatal period. This booklet was made available to all women who presented during their pregnancy (regardless of whether they participated in the screening program or not), with the exception of women in WA who received a similar booklet but at delivery. The booklet has under gone three reprints since 2001 and the last version has involved beyondbabyblues, incorporating parts of their “When the babyblues won’t go away” booklet. A total of 205,000 copies of “Emotional Health…” have been printed and distributed, both nationally and internationally. Such has been the success of “Emotional Health…”, a version for families with multiple births (eg twins, triples, etc) has also been developed. This booklet, whilst similar in content to the original version, discusses some of the issues particular to having a multiple birth, such as assisted reproductive technology, the impact on older siblings and hospitalisation. This booklet, which was produced as part of the Western Australia intervention, was developed with the assistance of the Australia Multiple Birth Association (AMBA). A total of 13,000 copies of the multiples version of “Emotional Health…” have been printed and distributed, both nationally and internationally. Page 33 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program A key component of the PND Program has been to provide information for women and families from culturally and linguistically diverse backgrounds. Materials for this group are minimal, with the Community Practitioners and Health Visitors Association (CPHVA) of the UK producing a series of 5 booklets (Arabic, Urdu, Somali, Urdu and Bengali). Working Women’s Health, a Melbourne based organization that provides multilingual health education, advocacy, training, and research, also has postnatal depression information in a number of different languages and formats. 1st reprint 2nd reprint 1st reprint 2nd reprint The PND Program has worked closely with a number of organizations, including Working Women's Health, NSW Multicultural Health Communication Service, NSW Transcultural Mental Health Centre, Karitane, Fairfield Health Service and the Office of Women’s Health in Vienna, to produce postnatal depression information in the following languages: Vietnamese, Arabic, Assyrian, German, Greek, Bosnian, Chinese, Croatian, Farsi/Persian, Indonesian, Japanese, Khmer/Cambodian, Korean, Lao, Macedonian, Punjabi, Serbian, Spanish, Thai and Turkish. All these resources are available in pdf format via the PND Program website. The Arabic and Vietnamese versions have also been printed in hard-copy format as part of the NSW antenatal initiative (see NSW Antenatal Intervention Report in Vol II, for further discussion). A total of 57,000 copies of the Arabic and Vietnamese-language versions of “Emotional Health…” have been printed and distributed, both nationally and internationally. An evaluation of the usefulness of the booklet in presented in Section 3. The National Project Manager has also collaborated closely with the Office of Women’s Health, Vienna, Austria, in the production of their postnatal depression information booklet. This version contains information from “Emotional Health……” and there is acknowledgement of the PND Program and beyondblue. Page 34 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Postnatal Depression Information Pamphlet Whilst the PND information booklet has proved immensely popular, its physical format has not always been appropriate. In particular, a number of organizations have sought PND information that can be placed on display boards and/or taken home by individuals whilst for example, waiting to visit a GP or MCHN. As a result, the PND Information Pamphlet was developed. In essence, the pamphlet is an abbreviated version of the booklet – covering areas such as the difference between postnatal depression and the baby-blues, what to do if you have postnatal depression, how partners can help and where to get help. The benefit of having this additional resource is that it can be placed on notice boards and display holders, which don’t accommodate the booklets size and shape. To facilitate distribution of the pamphlet, the Program entered into a 6-month agreement with INFOMED. INFOMED are a brochure, poster and information distribution service, which currently delivers resource material to 930 GP clinics across Australia. As part of this service, they place in each general practice, an information board containing brochures on a wide variety of health–related topics. The PND Program employed INFOMED to stock their information boards with copies of the PND pamphlet and also provide each clinic with an information pack containing Page 35 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program a letter of introduction, copies of the English-language and Arabic versions of the PND information booklet, the GP management and EPDS guides and information about beyondblue, ybblue and blueVoices. INFOMED also delivered to each practice copies of the PND promotional posters ensuring that at least one of the posters was displayed in the waiting room. By entering into this arrangement, the number of GPs receiving information about PND and beyondblue significantly increased and, more importantly, exposure of the Program to the general public was also be increased. All States have also been active in promoting the pamphlet to MCH services. In both Victoria and South Australia, every MCH centre received copies of the pamphlet, as well as the other PND resources. In all States, details of the pamphlet were widely advertised and demand for copies has been strong. A total of 600,000 copies of PND information have been printed and distributed, both nationally and internationally. Page 36 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Depression Management Guide As part of the depression-screening initiative, a key component of the PND Program has been to liase with GPs regarding changes in their patient’s mood during the perinatal period. This has brought to the surface a number of difficulties - i) many GPs lack the experience and training in dealing with people with a mental illness; ii) those GPs with mental health training often don’t have experience with perinatal mental illness and; iii) a mental illness in pregnancy and the early postnatal period has specific challenges, in particular the use of medication during this period. The PND Program recognised these problems and developed a guide to assist GPs with management of depression during the perinatal period., This guide covers the areas of how to make a diagnoses of depression (including DSM-IV criteria, major risk factors for postnatal depression and other causes of depressives symptoms), how to develop a management plan (eg when referral to a psychiatrist should be made, when to use medication, how to mobilise family/partner support and the different types of counselling available) and the use of medication during the perinatal period. Importantly, in all states, relevant contact numbers for medication information were included as well as links to local MCH services and details of specialist mother-baby or general mental-health services. Uptake of the guide has been broad. In Victoria, the Australia Capital Territory and Northern Territory the guide has been endorsed by the peak bodies for divisions of general practice Page 37 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program (GPDV, ACTDGP and GPPHCNT, respectively), whilst nationally gplearning, an online education service managed by the Royal Australian College of General Practitioners, has added the guide to a postnatal depression case-study for GP training. As well as general practitioners, use of the guide has been picked up by midwifery staff/students, MCHNs, psychologists/psychotherapists, obstetricians, social workers and perinatal depression researchers. A total of 33,500 copies of the depression management guide have been printed and distributed, both nationally and internationally Page 38 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Guide To Using The Edinburgh Postnatal Depression Scale Another area that the PND Program has recognised as inhibiting successful detection of perinatal mood disorders is a lack of understanding by health professionals of the use of depressionscreening instruments. In particular, health professionals knowledge of the Edinburgh Postnatal Depression Scale (EPDS), one of the most widely used perinatal depression screening instruments, needs significant improvement. Whilst a majority of professionals have heard of the scale, many do not understand how to use it or how to interpret the results of it. Because of this, the PND Program developed “The Edinburgh Postnatal Depression Scale – A Guide to Use” which discusses to the importance of screening for depression during pregnancy and early parenthood, and guidelines for administering the EPDS. It also includes a sample of the EPDS, information on how to interpret cut-off scores and tips for further investigation As with the depression-management guide, uptake of the EPDS guide has been broad – GPs, midwifery staff/students, MCHNs, psychologists/psychotherapists, obstetricians, social workers and perinatal depression researchers. Requests from consumers have also been high – evidence that women are taking a more pro-active approach to their care and seeking out information that they can share with their treating health professional. A total of 25,000 copies of the EPDS guide have been printed and distributed, both nationally and internationally. Page 39 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Promotional Posters To promote the PND Program and beyondblue, a series of promotional three posters were developed. These have been distributed to numerous organizations including antenatal clinics/hospitals, GP clinics, MCH centres, community health centres, Universities, Centrelink and high schools. Of these, the mother-infant poster has proved the most popular and engaging. One criticism of the remaining two posters, in particular the family poster, is that women aren’t able to identify with the image as it presents “the perfect family” which is often vastly different from their own circumstances. It is also interesting to note the different approach taken by the PND Program compared to, for example, the Community Practitioners and Heath Visitors Association (CPHVA) in the UK. Page 40 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program They have also developed a poster series in English, as well as Arabic, Urdu, Chinese, Somali and Bengali. The images used in their posters are of women with a neutral expression or, in the case of the two English posters, women in obvious distress. Unlike the PND Program, the CPHVA posters also list symptoms of depression. The effectiveness of the posters has not been evaluated as part of this report. Anecdotal evidence suggests, however, they are useful and raise the issue of perinatal depression in a nonconfrontational way. It may, however, be of use to modify the posters by making them more informational (eg by adding a list of the symptoms of depression) and by using images of women from culturally and linguistically diverse backgrounds. A total of 15,000 copies of the promotional posters have been printed and distributed, both nationally and internationally Page 41 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program www.beyondblue.org.au/postnataldepression The development of the PND Program website, as a satellite site of the beyondblue website, has proved has been a vital component of the activities of both organizations. Although, in our original proposal, there was no facility for a website, the PND Program recognized the importance for there to be a presence of the web – allowing 24hr access to information and the opportunity for people from overseas to see the approach Australian researchers are taking to the investigating perinatal mood disorders. In the period Jan 2005 – July 2005, there were 71,500 visits to the web-site The five most popular pages, in order, were – the Homepage (18337 visits), Educational Materials (4390 visits), About the PND Program (3315 visits), Personal Experiences (2866 visits) and Frequently Asked Questions (3024 visits). Requests for information, through the website, have come from Australia, New Zealand, England, Scotland the USA, Canada, Italy, Germany, Vienna, Finland, Russia, Hong Kong, Israel, and Pakistan. Page 42 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program 3. Evaluation of Changes in Health Professional and General Community’s Knowledge of Perinatal Mood Disorders Overview Prior to commencement, and at completion of the PND Program, postnatal women and health professionals involved in perinatal care were surveyed with respect to their knowledge and attitudes to perinatal depression and its treatment. Women surveyed in the end evaluation had all been involved in the program receiving at minimum the information booklet and EPDS. Health professionals had received at minimum the management guide and in most cases, training. At baseline evaluation the health professionals, particularly MCHN and GP’s over midwives, had a significantly higher knowledge of and ability to recognize depression than postnatal women. There were significant differences in treatment preferences, most strongly between the pharmacological preferences of the GP’s and that of natural therapies by the women. After involvement in the study, postnatal women: ♦ were better able to recognize and assess their own symptoms and coping; ♦ showed marked improvement in the ability to recognize depression in a hypothetical situation (though still significantly less than health professionals); ♦ were more accepting of the use of antidepressant medication postnatally; ♦ reluctance remained to consider medication antenatally; ♦ decreased their help seeking behaviour in the non-depressed group and had increased satisfaction with the help they did receive and; ♦ a significant number of women with high EPD scores did not seek treatment, even if they agreed with the “diagnosis” of depression. The booklet appeared to have the strongest impact on those of low to moderate EPDS scores and when given in pregnancy rather than at delivery. There was a significant increase in perinatal depression knowledge in MCHN and GPs (the latter showing the greatest improvement) but with a decrease in that of midwives, highlighting the importance of more intensive training and support for this group. GP’s relied less on mental health professionals, with no increase in barriers or a negative impact of the PND Program’s implementation. The importance of the GP link to screening was highlighted by a significant number of depressed women not raising depression as an issue, even when midwives or MCHNs had suggested this to them. Page 43 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Aims 1. To assess the effectiveness of the beyondblue National PND program in: ♦ increasing awareness of perinatal depression in treating health professionals and perinatal women; ♦ improving knowledge of perinatal depression and its treatment in treating health professionals; ♦ improving health professional’s confidence in treating perinatal depression; ♦ improving access to services by perinatally depressed women. 2. To assess the feasibility and acceptability of routine screening antenatally and postnatally for depression. Method Ethics approval was received from 43 maternity hospitals/area health services. At the commencement of the project, meetings were held with key stakeholders, including the College of General Practitioners, State Divisions of General Practice (DGP) and Primary Mental Health Care coordinators. Articles about the program appeared in a number of divisional newsletters and widely distributed publications for GPs. Population Evaluation was concentrated in the regions in which the PND Program operated, prior to commencement and at its completion. A baseline evaluation (BE) of women and health professionals (GPs, Maternal-Child Health Nurses and Midwives) assessing knowledge, level of depression and services accessed was conducted (Buist et al x 1 accepted; 1 submitted) prior to the PND Program commencing. At the end evaluation (EE), a random sample of postnatal women who had participated in screening, and of health professionals was sent questionnaires evaluating the project, with a stamped addressed return envelopes. This was conducted one to three years after introduction, by the PND Program, of routine screening. Health Professionals Health Professionals were asked to complete: 1. Information about their own professional experiences including type of professional training, years of experience, how often they deal with perinatal problems and how they manage with them, methods of diagnosing pregnancy-related depression, ‘barriers to successful treatment, and the impact on their practice of seeing perinatal emotional problems; 2. Experience of perinatal depression screening; 3. Knowledge questionnaire; 4. Vignette of a woman with perinatal distress and options for management. Page 44 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program 6-12 Week Postnatal Women Women were asked to complete: 1. Survey of Services Used. Basic demographic information, problems during pregnancy and questions relating to the adequacy of support were asked. Information about any additional help sought and feelings of ante or postnatal depression and anxiety were gathered. Questions about treatment sought for depression and the perceived satisfaction with the treatment received were also asked. This was also recorded at baseline; 2. Experience of being involved in the screening program; 3. Edinburgh Postnatal Depression Scale; 4. Vignette of a woman with perinatal distress and options for management. Questionnaires Experience of Perinatal Depression Screening Participants were asked about their involvement with the program, with questions on a likert scale of usefulness of the educational material and the degree of comfort in completion and use of the EPDS (health professionals were asked for their feedback/impressions from their patients as well as their own comfort in administration). Women were also asked if they had been told they scored positive and what their reaction/response to this was. Knowledge Questionnaire This consisted of ten multichoice questions about definition, frequency and treatment of postnatal depression developed by Watt & Pope (1997). The Edinburgh Postnatal Depression Scale The EPDS was administered as a screening tool for possible current depression. The EPDS, a widely used 10-item questionnaire developed for screening for PND in the community, has good reliability and validity, and has also been validated for use in an Australian population. This was administered at maternal-child health services. Results Response Rates The overall numbers of responses to the baseline and end evaluation surveys are recorded in Table 2; not all respondents completed all questionnaires. Response rates varied from state to state and between professional groups, from 20% to 80%. Table 2. Groups involved in Baseline Evaluation& End Evaluation Respondent Postnatal Mothers MCHN Midwives GPs Baseline Evaluation 525 338 569 246 End Evaluation 627 302 377 237 Page 45 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Summary of Baseline Findings Although knowledge level was similar among professional groups, MCHNs had higher levels of awareness of perinatal depression. Both GPs and MCHNs were more likely than midwives to recognize the need for providing help to women with emotional distress. Depression was more likely to be considered postnatally than antenatally in all groups, with GPs most likely to provide this diagnosis. GPs had a significant propensity to recommend antidepressants, and midwives to select non-specific medications. There are significant differences between health professionals and postnatal women in the recognition of depression associated with childbirth (Table 3), with women having a low awareness of perinatal depression. In addition, women have a strong preference for natural therapies, in contrast to GPs pharmacological approach. Though those with higher EPDS scores were more likely to go for help, this was more likely to be sort for general and baby related issues than for their own depression Table 3. Recognition/Awareness of Postnatal Depression in Health Professionals and Postnatal Mothers at Baseline (BE) and End Evaluation (EE). * p<0.01, women cp health professionals GP MCHN Midwives Mothers Recognition BE EE 97% 95% 90% 85% 89% 89% 47%* 60%* Need for Help BE EE 93% 90% 90% 90% 83% 85% 67%* 67%* Demographic Profile of Postnatal Mothers Demographics of the mothers at baseline and end evaluation were compared and presented in Table 4. The samples were statistically similar with respect to country of birth and English being first language (98%). They differed however on parity and marital status, and income though with respect to the latter only 6.0% left income unanswered at the end evaluation compared to 13.7% at baseline. Emotional Health of Mothers The mean EPDS score of postnatal women was lower at end evaluation (4.9 cp to 5.8, p < 0.001), but with a similar proportion of women with elevated scores >12 (6.9% at baseline, 7.3% at end evaluation). With respect to mode of delivery, of note, those who had a normal birth or elective Caesarean were more likely to be feeling positive about the birth experience (69% & 62%, respectively) than those who had emergency Caesarean sections (26%) or forceps delivery (36%). Page 46 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Of women who had no problems breastfeeding, 84% were continuing to breastfeed; of those who had difficulties only 22% continued. For 83% mothers who felt supported by their partner, this was closely related to the ease with which they reported managing parenting (p < 0.0001). Table 4. Demographic profile of postnatal mothers at Baseline (BE), End Evaluation (EE) & National Average 2002(♠ABS Census 2001, women > 15 years of age; * Australian Institute of Health and Welfare, “Australia’s Mothers and Babies 2002” (women who delivered in 2002), December 2004) Classification Born in Australia Age (average yrs) First Child Married Income up to $20,000 Income $20,001 – $40,000 Income $40,001 – $60,000 Income > $80,001 Mode of Delivery – Vaginal Mode of delivery – LUSC BE (%) 81 64 71.6 EE (%) 80 31 55 62.7 13.9 27.2 28.4 12.1 - 18.7 21.1 27.9 16.7 63 (9% assisted) 28 (12% elective, 16% emerg.) National Ave. 2002 (%) 77.9* 29.4* 41.1* 50.3♠ 62.1 (10.8% assisted)* 27* Awareness – Perinatal Depression There was no change between baseline and end evaluation in the positive awareness of depression by health professionals, with no differences between states. GPs were at both evaluations the least likely to miss the diagnosis (i.e. lowest negative awareness). Of note postnatal mothers showed a significant increase in identifying the hypothetical woman as being depressed – from 47% at baseline to 60% at the end evaluation (Table 3) with no change in whether they thought she needed assistance. This suggests that, at baseline and end evaluation, women felt the hypothetical woman needed help and the Program had resulted in them better identifying why she need help i.e. that she may be depressed. This still remained significantly lower than the health professionals, however. Relevant to this, there was significant decrease from baseline to end evaluation in the number of women who had a low EPDS and who thought they were depressed or anxious; from 24% to 15%. This again suggests the Program impacted on understanding of depression and what are “normal adjustment difficulties”. Awareness – Booklet Overall, 81% of mothers remembered receiving the “Emotional Health During Pregnancy and Early Parenthood” booklet. When this was broken down by State, just over half (54%) of women who were given the booklet at delivery (WA) recalled getting it. In other States, where the booklet was given during pregnancy, up to 87% of women recalled receiving it. Page 47 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program 35% of women reported reading the book at least a few times and only 16% reported not reading it at all. Of those who read the booklet, 54% found the material to be of some help, and another 24% were unsure. Having a high EPDS was not found to be related to reading the booklet, but those women with EPDS <13 were more likely to find it helpful. Health Professional Knowledge Whilst there were no differences in levels of experience between the two samples (baseline and end), GPs had had significantly more years of experience than the nurses, and the MCHNs more years of experience than the midwives. At baseline evaluation, the mean knowledge scores were similar for the three groups of health professionals. Over the time of the Program, there was significant improvement in the GPs knowledge levels (mean result 65% at baseline, increased to 69% at end evaluation, p = 0.019), bringing them to a similar level as the MCHNs (mean 69% at baseline, 68% at end evaluation). Knowledge was lowest in the midwives, and this decreased over the Program (64% at baseline, 59% at end evaluation, p < 0.05). It is likely this occurred because, in this sample, less of the midwives had received training compared to the other health professionals (see below). Of GPs, 66% felt that they had appropriate training to manage mood disorders during the perinatal period - 13% having attended beyondblue workshops, 24.6% “in-house” training, 30% had attended Sphere training and 33% drug company sponsored training. Only 0.4% of GPs received no training in PND management. Of MCHNs, 58% felt they had adequate training - 72% reported “in-house” training, 22% attended a beyondblue workshop whilst 11.5% had received no training at all. Of midwives, only 32% felt they had adequate training, with 42.4% receiving no training; 40% had “in-house” training and 16% attending a beyondblue workshop. Recommendations/Preferences for Treatment For GPs the most common recommendations for antenatal and postnatal care was counselling, antidepressants and referral to a mental health specialist. Both at baseline and end evaluation, postnatal depression was more likely than antenatal depression to be recognized and treated. At end evaluation, there was less reliance by GPs on referral to a mental health professional (83% down to 67%); this also decreased for MCHN suggesting training and support was successful in helping them manage more women with postnatal depression. A summary of key recommendation for treatment is shown in Table 5. At both time periods there was a higher preference towards antidepressants in health professionals than the mothers. At end evaluation, postnatal women, however, were more likely to consider use of antidepressant postnatally than they had at baseline. Page 48 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Table 5. Recommendations/Preferences for Treatment at End Evaluation (Baseline Evaluation figures in parenthesis) *p<0.05; ***p<0.001, women compared to health professionals Treatment Psychological Antidepressant GPs Antenatal Postnatal 77% 86% 78% 99% MH specialist 47% Social work Referral to GP Antipsychotics - 67% (*83%) 18% MCHNs Postnatal 80% 96% Midwife Antenatal 59% 55% - 91% 21% 59% - Mothers Antenatal Postnatal 29%*** 73%* (*53%) - 8% There were a number of differences noted between groups on recommendations of treatment that did not change over time; in general these can be summarized by GPs adopting more of a medical model, and less likely to favour naturopathy, self help, yoga and vitamins and minerals than the nursing groups. Midwives in turn were more likely to favour naturopathy, St John’s Wort, a special diet and sleeping tablets than MCHNs, who favoured GP referral more than the midwives. Changes in Help Seeking Behaviour At baseline, 64% women had sought help; this had decreased to 43% at end evaluation. However, 66% of women with a high EPDS score, compared to 42% of women with a low EPDS score, sought help – so whilst the % of depressed mothers seeking help hadn’t changed from baseline to end evaluation, there was a significant decrease in those with a low EPDS score seeking help. Of those women with a high EPDS score, 30% ignored the advice to seek help, and this was independent of whether they agreed with the score or not. Satisfaction with supports was significantly increased, from 46% mothers at least moderately satisfied at baseline, to 77% at end evaluation. There was a trend towards depressed mothers not being as satisfied with the treatment received, but this did not reach statistical significance (p=0.06). Barriers to Treatment Health professionals identified a number of barriers to treatment, with significant differences between the three groups. GPs noted that up to 50% of women who had an EPDS score >12 and who came to see them, did not raise the possibility of depression, emphasising the importance of the health professionals need to do so and to link-in with the perinatal services providing depression screening. GPs heightened awareness of depression most likely explains the increase since baseline of the their ability to pick-up on the women’s reluctance to raise the issue of depression (see Table 6). Of particular importance is the finding that there was no apparent increase in barriers and negative impact on GPs from the PND Program routinely advising women with high EPDS scores to seek their assistance. Page 49 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Table 6. Perceived Barriers to Treatment of Perinatal Depression; Baseline Evaluation (BE) results in parenthesis. Reason Unavailability of resources Reluctance of mothers to seek help Reluctance of family Time pressure Economic GP (BE results) 50% (47%) 51% (19%) 24% (23%) 39% (82%) 20% (31%) MCHN 43% 70% 39% 51% 24% Midwife 22% 58% 21% 33% 17% Discussion Increasing Awareness of Perinatal Depression in Health Professionals and Perinatal Women The most striking finding of the baseline study was the differences in levels of awareness of depression between health professionals and postnatal mothers, with a high level of awareness of postnatal depression in GPs and low level of awareness of depression in women. The high level of recognition was maintained over time in all the health professionals, but with no significant improvement in awareness of antenatal depression. However, there was a highly significant impact on the women’s awareness of depression (47% to 60%) and acceptance of antidepressant medication postnatally (53% to 73%), suggesting that the combination of posters, media campaign and antenatal booklet was highly successful in achieving its aim. Improving Knowledge of Perinatal Depression and its Treatment in Health Professionals Improving Health Professional’s Confidence in Treating Perinatal Depression The Program tackled this aim with a variety of training programs and provision of management guides. This was most successful with GPs, whose knowledge increased significantly. They were more satisfied that they were able to care for perinatal women, and were doing so more with less referrals to specialists. There was no apparent negative impact, though lack of resources remained an issue. The Program was less successful in improving knowledge and confidence in midwives. GPs and MCHNs were already identifying women with depression as part of their practice prior to the introduction of the PND Program; until this Program, antenatal emotional health care was largely ignored in most of the hospitals. Nearly half (42.2%) of the midwives still had not received training after the Program, compared to 0.4% GP’s and 11.5% MCHN who had not; this suggests more training is required. Factors such as rosters and lack of exposure to training for those midwives on the ward rather than the antenatal clinic may need to be considered in the delivery of such training. The midwives perceived a great need for training and it is likely that for routine screening to be successful, training and support needs to be more frequent than this Program offered. Despite this however, the midwives were very positive about the benefits of the program, and supported its continuation if ongoing support and training were provided. Page 50 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Improving Access to Services by Perinatally Depressed Women Whilst this program did not provide new services, it was anticipated that through better links and referral paths that more women with depression/stress would access their GP and other support services. One concern from a number of stakeholders at the commencement of the program was that this might create an unsustainable deluge on already existing services. Our results suggest that with better emotional care and information in pregnancy, those women who are not depressed are better informed and less likely to access services, but when they do they are more satisfied; depressed women may have a tendency to be less satisfied. Depressed women are more likely to access help though still not necessarily for themselves, emphasizing the importance of linking perinatal screening to GPs. Thirty % of women do not specifically respond to the advice given to them because of the screening process – possibly because some disagree with the EPDS score, but other issues (eg stigma) appear to be more relevant. Conclusions A key task of the beyondblue National PND Program was to assess the impact of a high level of increased information and education provision on relevant health professionals and perinatal women with respect to changes in awareness, knowledge and recommendations or access to treatment, with an assessment of any adverse impact on services of an increased demand. This was achieved by carrying out a baseline evaluation prior to the programs implementation and a repeat of this after implementation. This evaluation demonstrated: ♦ an increased awareness of depression in postnatal women, with improved self evaluation; ♦ an increase in GP knowledge; ♦ the importance of training and support in the implementation and ongoing process of screening; ♦ more training is required for midwives; ♦ further training needs to continue to emphasize antenatal depression, particularly for midwives; ♦ further work is needed to help depressed women access appropriate services; ♦ there was no significant negative impact of screening on service use, rather it seems that emotional health was incorporated into appointments that were already occurring, with greater health professional awareness of the need to raise the issue and not rely on the woman to do so and more confidence to be able to manage locally. Page 51 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program 4. Provision of a National Database of Young Families in Australia Overview Over forty thousand women were screened for depression across Australia, the majority of which were in public hospitals in major cities. The screened population included samples from rural & remote populations, as well as private hospital patients. Further analysis over the next months will reveal more detailed insight. Summaries of the key preliminary findings are presented here. This study confirms high levels of distress in perinatal women, with rates of postnatal depression (as per EPDS scores) as similar to other Westernised countries - 15.7% of women scored >9 postnatally. Antenatal rates, depending on the cut-off score used, were lower than postnatal rates at 5.4% if >14, the currently favoured cut-off score, was used. This, however, is misleading as lower rates were recorded in NSW (half the total sample recruited) who screened in 1st trimester, when rate are lower. When the trimester screened is taken into account, rates of depression are again, similar to international figures. Comparison of the EPDS with two other screening instruments (K10 and Sphere) confirmed the need for a specific tool, such as the EPDS, for perinatal women. State differences were noted in depression rates, with NSW and WA having lower rates both antenatally and postnatally than other States. Factors possibly contributing to this include: ♦ different demographics variables in the samples, eg higher socio-economic status & education levels (both States), higher culturally and linguistically diverse background population (NSW); ♦ earlier timing of antenatal screening (NSW); ♦ long-standing depression- screening and psychosocial assessment program (both States). Risk factors for antenatal and postnatal depression were similar, and generally consistent with previous studies, but with some differing relative importance: ♦ past history of abuse, anxiety and depression were the strongest predictors for depression; ♦ stress, mood and medical complications through pregnancy were also significant risk factors; ♦ emotional and/or practical support was important, but appears to be more generic rather than specifically from partner; ♦ lower socio-economic status was a significant risk factor for depression; ♦ higher education, age and socio-economic status were generally protective ; ♦ young mothers were particularly at risk; ♦ a culturally and linguistically diverse background appeared somewhat protective for antenatal depression and a slight risk for postnatal depression; ♦ being Indigenous increased the risk of perinatal depression. Page 52 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Demographics Overview Forty thousand, three hundred and thirty three (40,333) pregnant women were recruited to the depression-screening component of the PND Program, from all States and the ACT, excluding the NT. The largest number of women was recruited from NSW (21285; 52.8%), reflecting the procedures, policies and networks already established in this State. The smallest number of women was recruited from Tasmania (749; 1.9%). The data includes 611 (1.7% of overall sample) Indigenous women. Postnatal data was collected from 12,535 women. The average age of the pregnant women was 30 years (range 14 - 54 years), with a mean of 2.5 pregnancies and 1.1 children. An overview of the national demographic data is presented in Table 7. In summary: ♦ 74% of women were Australian-born similar to the 2002 national average of 77.9%; ♦ the largest ethnic group involved were those from Asia (8%) and New Zealand/Oceania (5.0%); ♦ 42% of women achieved Year 12 as their highest level of education, with 22.4% completing a Bachelor degree or higher; 14.3% of women did not complete their schooling; ♦ the sample recruited was predominantly from the public sector, with 1114 women from private hospitals and 255 at a birth centre. This represents 3% of the total sample, and is significantly smaller than the 30% women who delivered privately in Australia in 2002. This is particularly relevant and needs consideration in the interpretation of the results as lower socio-economic status (SES) and lower education levels have been indicated as risk factors for depression; ♦ a small sample of women who delivered in rural regional and remote centres were also recruited – 2517 women (6.5% of total sample). Demographic data by State is provided in Table 8. In summary: ♦ the average age of women was similar in each State but with more in the <21 years age bracket in QLD and TAS & in the >35 years age bracket in WA; ♦ WA and QLD had the highest numbers of Indigenous women participating; ♦ all but two states had similar levels of Australian born women; NSW had a higher number of other ethnic groups. TAS had the highest Australian-born group; ♦ women were recruited to the PND Program at different times during their antenatal period. This was necessary as the recruitment protocols were adapted to the practicalities of the individual hospital/area-health services. The average recruitment time was 26 weeks gestation - ACT/SA/VIC at 28-30 weeks, NSW & TAS at 16-18 weeks, QLD at 20 weeks and WA at 33 weeks; ♦ higher education levels were noted in women from ACT and WA and lower in QLD; ♦ ACT women had a significantly higher joint income; this data was not available on NSW however; ♦ married/Defacto status was higher in ACT, NSW and VIC and lowest in QLD; ♦ medical complications of pregnancy, particularly varicose veins, excessive vomiting and diabetes were significantly higher in the QLD than other States. Page 53 of 108 beyondblue National Postnatal Depression Program VOL I: National Screening Program Table 7. National Demographic Overview Demographic Variable Total Number of Women Recruited to national Screening Program Average Age (yrs) Number of living children Number of previous pregnancies Estimated weeks pregnant (when recruited) Aboriginal/Torres Strait Islander Country of Birth - Australia - New Zealand/Oceania - Europe & America (North & South) - Africa (All)/Middle East - Asia Main Language Spoken at Home - English - European - Asian - African/Middle Eastern - Other Level of Education Completed - Did not finish school - High School (Yr 7-12)/Apprenticeship - Certificate/Diploma Level - Bachelor Degree/Grad Dip/Grad Certificate Level - Postgraduate Degree Joint Income - Up to $20,000 - $20,001 - $60,000 - $60,001 - Greater than $80,001 - Do not wish to divulge Occupation - Managers & Administrators - Professional OR Semi Professional Medical/Health/Science, Building, Finance & Other Worker - Tradesperson & Related Worker - Secretarial, Administrative or Financial Workers/Specialist Clerical or Sales Worker/General Clerical or Sales, Security, Personal Service or Domestic Worker - Plant, Machinery or Vehicle Operator - Labourer & Related Worker - Student, Unemployed or Other Marital Status - Married/De Facto - All other including “No partner” Medical Problems With Current Pregnancy - High blood pressure - Bleeding/threatened miscarriage - Excessive vomiting - Varicose veins, haemorrhoids or similar - Bladder or kidney infection - Diabetes - Other PND Program 40,333 30.3 1.1 2.5 26.2 3.3% National Ave. N/A 29.4# 1.7♠ N/A N/A 3.6%# 74.4% 5.0% 9.3% 3.2% 8.0% 77.9%# 2.5%# 7.1%# 3.3%# 9.3%# 84.6% 1.8% 7.8% 4.5% 1.3% 79.2%@ 6.7%@ 4.8%@ 1.4%@ 2.0%@ 14.3% 42.5% 20.9% 18.7% 3.7% N/A N/A 15.4%@ 11.9%@ 1.4%@ 11.6% 48.3% 27.5% 12.7% 3.6%@ 38.8%@ 42.4%@ 1.7%@ 2.7% 30.0% 5.7%@ 32.6%@ 5.0% 41.4% 3.0%@ 47.2%@ 1.1% 3.8% 16.3% 2.5%@ 7.0%@ 14.3%@* 82.3% 22.1% 50.3%@^ 49.7%@$ 5.6% 9.0% 18.3% 21.2% 4.0% 10.5% 6.9% N/A N/A N/A N/A N/A N/A N/A N/A – Data not available or not collected # - from Australian Institute of Health and Welfare, “Australia’s Mothers and Babies 2002”, December 2004 @ - from Australian Bureau of Statistics, National Census, 2001 * - Student and Unemployed only; ^ - ABS does not have a classification for “De facto”; $ - ABS does not have a classification for “No partner” ♠ - from the Household, Income and Labour Dynamics in Australia (HILDA) study (www.livinginaustralia.org/index) Page 54 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Table 8. State Demographic Overview Demographic Variable Total Number of Women Recruited Average Age (yrs) Number of living children Number of previous pregnancies Estimated weeks pregnant (when recruited) Aboriginal TS Islander (% state total) Country of Birth - Australia - New Zealand/Oceania - Europe & America (North & South) - Africa (All)/Middle East - Asia Main Language Spoken at Home - English - European - Asian - African/Middle Eastern - Other Level of Education Completed - Did not finish school - High School (Yr 7-12)/Apprenticeship - Certificate Level/Diploma Level - Bachelor Degree/Grad Dip Level - Postgraduate Degree Joint Income - Up to $20,000 - $20, 001 - $60, 000 - $60, 001 - Greater than $80, 001 - Do not wish to divulge Marital Status - Married/De facto - All other including “No partner” ACT 984 (2.4%) 30.7 0.8 2.1 28.5 1.1 NSW 21285 (52.8%) 30.4 1.0 2.7 16.1 N/A VIC 5079 (12.6%) 30.7 1.3 2.3 28.5 1.2 TAS 749 (1.9%) 28.8 1.7 2.3 18.4 3.6 SA 3355 (8.3%) 30.4 0.9 2.3 29.7 1.5 WA 4840 (12%) 30.9 0.9 2.3 33.2 4.4 QLD 4041 (10%) 28.9 1.5 2.5 19.3 7.2 84.3 2.0 6.4 1.2 6.0 50.3 8.4 13.5 8.0 19.8 83.9 3.7 6.4 1.3 4.7 96.1 1.1 1.6 0.7 0.3 84.3 1.7 9.2 0.8 4.0 74.2 4.0 12.7 3.7 5.6 87.6 6.6 3.7 0.5 1.5 94.7 0.8 2.7 0.2 1.6 73.5 2.8 14.0 8.1 1.6 94.3 1.0 1.7 0.9 2.0 99.6 0.0 0.3 0.0 0.1 95.9 1.3 1.7 0.3 0.9 94.8 1.1 2.2 1.6 0.3 98.6 0.3 0.4 0.1 0.7 4.8 34.2 19.1 31.2 10.6 13.2 37.5 20.9 23.6 4.7 14.3 42.8 22.3 17.7 2.9 9.3 57.8 16.3 14.5 2.2 18.6 44.2 19.8 15.1 2.4 12.7 37.6 21.1 23.3 5.2 16.6 48.2 21.5 11.8 1.8 6.1 30.6 54.6 8.7 N/A N/A N/A N/A 8.9 48.1 31.3 11.8 19.9 52.9 20.5 6.8 11.1 51.5 22.0 15.4 13.2 45.7 26.6 14.4 12.8 52.5 23.4 11.3 91.1 2.2 92.2 7.5 87.1 4.1 79.2 11.6 83.0 6.3 80.0 3.9^ 70.6 11.9 Page 55 of 108 beyondblue National PND Program Final Report Demographic Variable Occupation - Managers & Administrators - Professional OR Semi Professional Medical/Health/Science, Building, Finance & Other Worker - Tradesperson & Related Worker - Secretarial, Administrative or Financial Workers/Specialist Clerical or Sales Worker/ General Clerical or Sales, Security, Personal Service or Domestic Worker - Plant, Machinery or Vehicle Operator - Labourer & Related Worker - Student, Unemployed or Other Medical Problems With Current Pregnancy - High blood pressure - Bleeding/threatened miscarriage - Excessive vomiting - Varicose veins, haemorrhoids or similar - Bladder or kidney infection - Diabetes - Other VOL I: National Screening Program ACT NSW VIC TAS SA WA QLD 8.9 31.6 3.1 46.2 2.5 26.0 2.1 17.3 1.0 21.1 2.4 37.1 3.5 27.5 6.4 40.3 3.9 17.7 4.1 43.2 3.6 33.8 5.2 45.4 6.6 50.1 4.6 40.2 0.1 0.4 12.2 0.2 0.7 28.3 1.4 3.3 19.4 1.1 2.9 39.1 0.9 9.0 17.4 1.6 2.3 N/A 0.6 6.0 17.5 2.6 11.7 8.5 18.7 4.3 2.4 8.1 N/A N/A N/A N/A N/A N/A N/A 5.1 9.9 10.0 12.3 3.4 2.7 6.5 2.5 13.5 12.2 10.7 6.0 1.3 5.5 3.9 8.0 10.1 16.4 4.0 1.7 4.3 10.6 7.8 13.1 18.1 4.9 5.7 12.0 2.6 8.5 43.6 43.1 3.3 35.5 3.1 N/A – Data not available or not collected ^ - does not include “No partner” Page 56 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Mood Data Internationally, the Edinburgh Postnatal Depression Scale (EPDS) is the most widely accepted screening instrument used in the perinatal period. The EPDS was developed by Cox, Holden & Sagovsky (1987), and was designed to allow screening of postnatal depression in the primary care setting. It excludes some symptoms that are common in the perinatal period (tiredness, sleep disturbance, irritability) that other depression instruments include, as such symptoms do not differentiate between depressed and non-depressed postnatal women. As a screening instrument, the EPDS should only be used to assess a woman’s mood over the past seven (7) days. High scores do not themselves confirm a depressive illness and, similarly, some women who score below a set threshold might have depression. Thus, the EPDS does not provide a clinical diagnosis of depression and it should not be used as a substitute for full psychiatric assessment or clinical judgement. Importantly the EPDS cannot be used to predict whether or not a respondent will experience depression in the future - it can only be used to determine current mood. The EPDS is a 10-item self-report questionnaire. Women are asked to select one of 4 responses that most closely represent how they have felt over the past seven (7) days. Each response has a value of between 0 and 3 and the total EPDS score is calculated by adding the values of the response for each item, resulting in a possible total score range of 0-30. If the woman scores 0-9 the likelihood of depression is considered low; 10-12 the likelihood of depression is considered moderate and; 13 or more the likelihood of depression can be considered high The EPDS was evaluated at several cut-off scores. A score of >12 (i.e. 13 or more) was used in this study, both antenatally and postnatally, to warrant “notification” of high risk of being depressed. The purpose of this was to minimize the number of false positive results. Evidence in the scientific literature has suggested that, where community samples are involved, EPDS cut-off scores of >9 (i.e. 10 or more) postnatally and >14 (i.e. 15 or more) antenatally, are more appropriate. Antenatally, the suggestion is that “15” is a preferred cut off score because of the high incidence of “anxiety” that occurs around this time, falsely elevating the frequency of high scores. The mean EPDS score was 6.9 (SD 4.4) antenatally and 5.4 (SD 4.4) postnatally, the higher mean antenatally reflective of the need for higher cut-off score at this time point. Rates of antenatal and postnatal depression by EPDS score are detailed in Table 9. Table 9. Rates of Antenatal and Postnatal Depression by EPDS Scores Time point and Cut-Off Antenatal EPDS >14 Antenatal EPDS >12 Antenatal EPDS >9 Postnatal EPDS >12 Postnatal EPDS >9 Antenatal & Postnatal EPDS >12 Women with Score (%) 5.4 8.9 19.6 7.6 15.7 2.7 Page 57 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program The distribution of antenatal EPDS scores is shown in Figure 2; postnatal EPDS score are shown in Figure 3. Figure 2. Distribution of Antenatal EPDS Scores Figure 3. Distribution of Postnatal EPDS Scores Page 58 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program The postnatal rates of depression, are consistent with studies in Westernised populations using an EPDS > 9, which generally quote 13-14% (O’Hara & Swain 1996). Our rate, 15.7%, is slightly higher than this and is probably accounted for by a higher number of those at risk, in particular those from lower SES and education level, given our predominantly public hospital population. The mean EPDS score and prevalence rates of the individual states are shown in Table 10. Table 10. Mean EPDS Score and Prevalence Rates for Each State (* p < 0.05; ** p < 0.01; *** p < 0.001) State ACT NSW QLD SA TAS VIC WA Antenatal Mean (SD) 6.5 (4.9) 7.5 (3.9) 6.4 (4.8) 7.0 (4.6) 7.0 (5.6) 6.3 (4.8) 5.6 (4.3) Ante EPDS >9 Ante EPDS >12 Ante EPDS>14 22.5% 17.6%* 21.9% 26.6%*** 28%*** 22.4% 16.9%*** 12.8% 6.2%*** 11.8% 12.8%*** 15.4%*** 12.4% 7.5%*** 7.9% 3.6%*** 6.9% 8.2%*** 9.3%*** 8.0% 4.2%*** Postnatal Mean (SD) 5.9 (4.3) 4.1 (3.9) 5.2 (4.7) 6.2 (4.7) 6.1 (4.5) 5.3 (4.4) 4.9 (4.2) Post EPDS >9 Post EPDS >12 Ante & Post EDPS >12 16% 15%*** 17% 19.6%*** 19%* 15.4% 13%*** 7.1% 6.3%*** 8.3% 10.2%*** 9% 7.6% 6.1%*** 3.5% 1.6%** 3.2% 3.6%** 3.8% 3.1% 2.0%*** Of note, there were significant differences in the prevalence rates of the different EPDS cutoff scores between States - WA and NSW had the lowest rates, whilst SA and TAS the highest. This was significant at all cut-off scores for WA & NSW vs. the other States and SA & TAS vs. the other States, except for postnatal EPDS >12 for TAS. The differences noted might be explained by the different demographic profile of the States and will require further analysis. Women in WA were older, better educated, had higher incomes and were more likely to be professionally employed than women from either SA or TAS. When the WA scores were broken down into those who delivered in a private hospital vs. a public hospital, those women who delivered privately were less likely to score a high EPDS than those who delivered the public system (Table 11). Table 11. EPDS Prevalence: WA Public Patients vs. WA Private Patients (* as proportion of each group in WA sample) System WA Public* WA Private* Ante EPDS >9 17.6% 10.2% Ante EPDS >12 8.1% 2.0% Ante EPDS>14 4.5% 1.8% Post EPDS >9 13.5% 8.7% Post EPDS >12 7.6% 0% Ante & Post EDPS >12 2.1% 0.7% NSW data showed similar rates of professional occupation & higher income to WA. However, for NSW, the low prevalence of EPDS cut-off scores appears most likely to be due to the timing of the antenatal screen - 16 weeks or less decreasing the chance of having a high EPDS score (see Odds Ratios, Table 12). This is consistent with other studies – a meta-analysis by Bennett et al Page 59 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program 2004, concluded the prevalence of depression (EPDS > 12) was 7.4% in the first trimester, increasing to 12.8% and 12% in the 2nd and 3rd trimesters, respectively. The overall antenatal rate in this study is somewhat lower than that reported in Bennett et al, but is similar when viewed by State and trimester screened. Postnatally, prevalence rates in NSW were similar to the other states and may be influenced by the higher rates of women from culturally and linguistically (CALD) backgrounds. Of note, the ACT has higher income levels, higher rates of professional occupation and data for public and private deliveries (and lower CALD groups than NSW) – and rates of high EPDS are consistently higher than NSW, WA and NSW, and in both delivery settings. What NSW and WA also have in common, separating them from other States, is that they both have been screening for some time prior to this PND Program commencing, suggesting a positive longer term effect of screening (i.e. for reducing EPDS scores and decreasing the number who remain high throughout). Risk Factors for Antenatal and Postnatal Depression Odds Ratios (95% CI) of key demographic and/or psychosocial variables, considered to be important risk factors in perinatal depression, were calculated for both antenatal and postnatal depression. Here we present with the cut offs for both as an EPDS >12, but the pattern is similar for EPDS >9 and >14 (antenatally). The key factors were found to be the same in both, and in those who were depressed at both times. These are presented in Tables 12 and 13. Demographic Variables The strongest risk factors to emerge from demographics are Indigenous background, socioeconomic status and absence of a partner. Younger age (<21 years) and medical complications were also important. As Indigenous women have an increased risk of having all these factors, they are clearly a group that is at particular risk. Of the Indigenous women in this sample, 19% had antenatal EPDS > 12 (13%, >14), 12% postnatal EPDS >12, 6.3% EPDS >12 both antenatally and postnatally. Conversely, older age, higher education and socio-economic status are all protective. Of interest, and possibly contributing to the lower antenatal EPDS scores in NSW, is the potential somewhat protective factor of a CALD background for antenatal depression, particularly if you are born in Australia but to a CALD family. Whilst 8.9% of the total group of women had an antenatal EPDS >12, 9.3% of the English spoken at home group did, compared to 5.2% who spoke European languages, 5.8% who spoke Asian languages and 4.6% who spoke African/Middle Eastern languages. The implication is that the second generation receives the cultural benefits such as elevated importance of pregnancy of the country of origin without the trauma of migration and dislocation. Further analysis of this is required. Page 60 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program The cultural benefits of a CALD background, however, are not maintained postnatally, where a CALD (Asian and African/Middle Eastern but NOT European) background is a slight risk factor for postnatal and for continuing depression (antenatally and postnatally) – possibly the group who are most traumatised by their immigration / experiences in their country of origin, and/or are separated from families and communities, or the realities of the culture in which they are living taking effect. Rural residence does not in itself appear to be a significant risk factor, but an analysis of the rural women in Victoria compared to the urban women, suggested higher rates of elevated EPDS scores in the rural women (8.5% of rural women had postnatal EPDS>12 compared to 6.7% of the urban group used for comparison), in part related to higher rates of other risk factors in rural women i.e. they were more likely to be single and from a lower socio-economic background. Table12. Odds Ratios: Demographic Variables Risk Factor Indigenous Born outside Australia English not spoken at home (Asian /middle eastern) Aged <21 years Age >35 years Higher education High income (>$60,000 per annum) Low Income (<$20,000 per annum) Rural residence No partner Number of children Number of pregnancies Stage of pregnancy at 1st screen: 16 weeks vs >16 weeks Medical complications Ante Odds Ratio 2.4 (1.7 – 3.4) 0.99 (0.84 – 1.16) 1.3 (1.1 – 1.7) Post Odds Ratio 1.8 (1.2 – 2.8) 1.0 (0.8 – 1.2) 1.1 (0.8 – 1.5) Ante & Post Odds Ratio 2.6 (1.5 – 4.4) 1.0 (0.7 – 1.3) 1.4 (0.9 – 2.3) 1.7 (1.2 – 2.4) 0.84 (0.72 – 0.98) 0.64 (0.55 – 0.75) 0.57 (0.47 – 0.69) 1.7 (1.2 – 2.4) 0.84 (0.72 – 0.98) 0.65 (0.54 – 0.77) 0.57 (0.47 – 0.69) 1.7 (1.2 – 2.4) 0.8 (0.7 – 1.0) 0.6 (0.4 – 0.7) 0.57 (0.47 – 0.69) 2.8 (2.4 – 3.4) 2.8 (2.4 – 3.4) 2.8 (2.4 – 3.4) 0.76 (0.60 – 0.95) 2.3 (2.0 – 2.7) 1.2 (1.1 – 1.3) 1.2 (1.1 – 1.3) 0.8 (0.5 – 1.2) 1.2 (1.0 – 1.5) 1.9 (1.6 – 2.2) 1.14 (1.07 – 1.23) 1.15 (1.09 – 1.21) 0.8 (0.5 – 1.2) 0.98 (0.68 – 1.42) 2.4 (1.9 – 3.1) 1.3 (1.2 – 1.4) 1.2 (1.1 – 1.3) 0.8 (0.5 – 1.2) 1.8 (1.6 – 2.0) 1.6 (1.4 – 1.9) 1.6 (1.3 – 2.6) Psychosocial Variables Psychosocial variables give the strongest indicators to risk of depression, in keeping with previous research. Support and partner relationship are probably the most consistent risk factors that have been associated with postnatal depression in previous studies. This study confirms the importance of support postnatally and establishes that it is also a factor antenatally. Of note, the presence or absence of a partner rather than their emotional support from them appears important, suggesting physical help rather than emotional is important, as is support from others rather than just partner such as mother. Page 61 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Table13. Odds Ratios: Psychosocial Variables * includes depression (major & minor), anxiety, eating disorder and difficulty accepting being pregnant Risk Factor Past History of Abuse No available support Perfectionist personality Emotional Problems in current pregnancy* (range of disorders) High daily hassles Past History of Depression and anxiety Past history of Anxiety Mother emotionally unsupportive Partner emotionally unsupportive Ante Odds Ratio 3.6 (3.2 – 4.2) 3.2 (2.4 – 4.3) 2.4 (2.1 – 2.8) 12.9 (10.9 – 15.2) Post Odds Ratio 3.1 (2.7 – 3.7) 2.6 (1.9 – 3.7) 2.2 (1.9 – 2.5) 4.9 (4.2 – 5.8) Ante & Post Odds Ratio 4.1 (3.2 – 5.2) 4.2 (2.7 – 6.4) 3.5 (2.7 – 4.6) 16.4 (11.7 – 22.8) 3.0 (2.5 – 3.6) 7.8 (6.1 – 6.9) 2.3 (1.8 – 2.8) 6.1 (4.7 – 8.0) 3.3 (2.5 – 4.3) 13.4 (9.4 – 19.1) 3.1 (2.3 – 4.3) 1.0 (0.8 – 1.2) 3.3 (2.4 – 4.6) 1.3 (1.1 – 1.6) 4.5 (2.6 – 7.6) 1.2 (0.9 – 1.7) 0.56 (0.45 – 0.71) 0.4 (0.5 – 0.8) 0.6 (0.4 – 0.8) An analysis of a subsample of women comparing in detail those who were single to those who had supportive partners and those who had unsupportive partners revealed that the latter subgroup had the highest risk i.e. an unsupportive partner was worse than no partner at all, a supportive partner affording the most protection. Some studies have also highlighted the importance of family of origin that is supported here, with mother’s support and a history of abuse being significant risk factors. The strongest predictor of antenatal and postnatal depression is however a past history of anxiety or depression and emotional problems in pregnancy. The antenatal EPDS score itself accounts for approximately 25% of the postnatal variation. A model to predict postnatal depression (as defined by EPDS > 12) looked at the risk factors outlined above. The final model for best predication is presented in Table 14. Table 14. Postnatal Depression (EPDS >12) Prediction Model Factor Any emotional problems Any illness Life stresses Perfectionist Higher income Lower income Partner support OR (95% CI) 2.6 (2.1 – 3.2) 2.1 (1.7 – 2.5) 1.4 (1.2 – 1.5) 1.6 (1.3 – 1.9) 0.8 (0.6 – 0.9) 1.4 (1.0 – 1.8) 0.8 (0.7 – 0.9) Significance p < 0.0001 p < 0.0001 p < 0.0001 p < 0.0001 p < 0.05 p < 0.05 p < 0.0001 Page 62 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program If antenatal EPDS score was included in the model, any emotional problem, any illness, perfectionism and pattern support remained in the model. Life stresses approached significance but income was no longer significant. Correlation of EPDS and K10/Sphere In a subsample of the overall group (n=1083), women completed two alternative screening tools in addition to the EPDS – the K10 and Sphere. Both these tools had been used and standardised in Australian community samples, but not on perinatal women. A linear model did not apply and for both tools the percentage variation was very small, suggesting no relationship between the EPDS scores and that on K10 or Sphere. This finding is most likely due to two factors; one, the EPDS rates the previous week, whereas the other two tools look at the prior month; two (and most importantly), that the EPDS, though it has been criticized antenatally for picking up excessive “normal” anxiety (hence the move to use a higher cut off score antenatally), it has less questions focusing on this than either of the other tools and none on physical symptoms. Hence, the K10 and Sphere are picking up on some of the “normal” features of pregnancy and appear unreliable at this time. This finding highlights the importance of the use of a tool in perinatal women that has been designed specifically for perinatal women. Page 63 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program 5. Evidence of Efficacy of Early Intervention Initiatives Overview Each State as part of the overall project, sought to build on current expertise and services to expand and evaluate an intervention for perinatal depression. As a result of the breadth of expertise of the State directors and their teams, this section of the project was diverse, but with implications for women across Australia. In summary: ♦ ♦ ♦ ♦ ♦ ♦ ♦ ♦ ♦ ♦ ♦ Queensland, Western Australia and NSW all developed information material for specific groups of women that had not been available to them before. With the exception of the Indigenous material (more specific to Palm Islanders/Mt Isa, but has been made available as a base for other Indigenous groups), these have been made available on the web and in hard copy to women in all States; mothers who have a “multiplies” birth are at particular risk and have significant unaddressed needs; in Victoria a self-help intervention program for pregnant women and their partners, to cope with the emotional transition to parenthood, was found highly acceptable. However, general practitioners and maternal and child health nurses need to be more centrally involved in the program to increase uptake by women; Indigenous women score no differently on the language specific EPDS than on the mainstream EPDS, or on the suicidal ideation question (Q10) an in depth analysis of the issues related to depression in Indigenous perinatal women reveals the high importance of psychosocial stressors; long distance education was successful at increasing awareness and knowledge but like the other education packages, needs ongoing training, and was not without technical difficulties that could be improved with flexible formats; a low-cost, self-help intervention was beneficial and potentially feasible on a large scale; interventions with at risk women, male partners and Arabic women all showed significant issues of reluctance to seek assistance, but with benefits for those who did. Understanding and overcoming these barriers remains the key to increasing early intervention, in association with routine screening; a more in depth analysis and pilot intervention into Vietnamese and Arabic women showed benefits of telephone counselling and psychosocial interventions; despite some difficulties recruiting at risk women, a low cost minimal intervention can be of benefit and if tied in with screening could increase those women receiving appropriate assistance; male partners were particularly difficult to engage (alternatives such as web-based packages should be utilised) and suggests a larger cultural change is required before a primary intervention involving them is likely to be successful. REPORTS FROM THE DIFFERENT STATE BASED ANTENTAL INTERVENTION INITIATIVES CAN BE FOUND IN VOLUME II OF THIS REPORT Page 64 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Staff Members National Office A/Prof Anne Buist, National Co-ordinator (2001 – 2005) Dr Justin Bilszta, National Project Manager (2001 – 2005) Victoria and Tasmania Prof Jeannette Milgrom, State Co-ordinator (2001 – 2005) Ms Jennie Ericksen, State Project Manager (2001 – 2005) Dr Alan Gemmill, Senior Research Officer (2001 – 2005) Ms Melina Ramp, Senior Research Assistant (Dec 2002 – 2005) Ms Kate Neilson, p/t Research Assistant (2001 – 2004) Mr Christopher Holt, p/t Research Assistant (2004 – 2005) Toward Parenthood Intervention Team Ms Bella Saunders, Clinical Psychologist (2001 – 2005) Ms Elizabeth Loughlin, Clinical Psychologist (2001 – 2005) Ms Yolanda Romeo, Clinical Psychologist (2001 – 2005) Ms Bronwyn Leigh, Health Psychologist (2001 – 2005) Ms Rachael McCarthy, Clinical Psychologist (2001 – 2005) Students – Bronwyn Leigh, Ying Zhi Gu, Melissa Tang, Eddie Tan, Jessica Rowe, Clare Heaney, Brooke Ellis, Michelle Puttick, Penny Koutsouridis & Megan Andrews South Australia Prof John Condon, State Co-ordinator (2001 – 2005) Ms Ann Alder, State Project Manger (2001 – 2005) Ms Liz Gamble, Senior Research Midwife (2001 – 2005) Ms Carolyn Corkindale, Associate Researcher (2001 – 2005) Dr Anne Sved-Williams, Associate Researcher (2001 – 2005) Western Australia Prof Sherryl Pope, State Co-ordinator (2001 – Dec 2003) Dr Craig Speelman, State Co-ordinator (Jan 2004 – 2005) Ms Janette Brooks, State Project Manager (2002 – 2005) Ms Colleen Ball, Research Midwife (2001 – Dec 2004) Ms Jocelyn Bristol, Research Midwife (2001 – 2005) Ms Sandy McClean, Research Midwife (2002 – 2005) Ms Monica Howard, Research Assistant (2003 – 2004) Ms Debbie Lien, Research Assistant (2003 – 2004) Mr James Humphreys, Data Management (2001 – 2005) Queensland Prof Barbara Hayes, Queensland Director (2001 – 2005) Ms Beryl Buckby, Assistant Qld Project Manager (Nov 2003 – Feb 2004) Queensland Project Manager (Feb 2004 – 2005) Page 65 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Ms Renee McAllister, Queensland Project Manager (2002 – Feb 2004) Ms Justine Doherty, Assistant Qld Project Manager (August – Dec 2003) Ms Janese McCulley, Assistant Qld Project Manager (April 2004 – 2005) Dr Alistair Campbell, IT Consultant (2003 – 2005) Ms Lynore Geia, Indigenous Consultant/Research Assistant (June 2002 – Dec 2004) Ms Margaret Egan, Indigenous Consultant/Research Assistant (Feb 2004 – 2005) Ms AnneMarie Lawrence, Research Midwife (The Townsville Hospital) (Sept 2002 – Dec 2004) Ms Jackie Bowen, Research Midwife (Cairns Base Hospital)(Nov 2002 – June 2003) Ms Lesley Williams, Research Midwife (Cairns Base Hospital) (June 2003 – Jan 2005) Ms Alison Thwaites, Research Midwife (Mackay Base Hospital) (Feb 2004 – Sept 2004) Ms Justine Collins, Research Midwife (Mackay Base Hospital) (July 2004 – Jan 2005) Ms Ruth McKitrick, Research Midwife (Ipswich Hospital) (April 2004 – March 2005) Ms Cheryl Hewlett, Research Midwife (Logan Hospital) (June 2004 – March 2005) Ms Lynda Steward, Research Assistant/Midwife (Townsville) (Sept 2004 – 2005) Ms Annette Kelly, Research and Admin Support (June 2003 – Aug 2004) Ms Maryanne Martin, Research and Admin Support (Sept 2004 – 2005) Ms Tara MacDonald, Prof Hayes Admin Support (2003 – 2005) Ms Annette Riley, Research Assistant (Indigenous Initiative, Mt Isa) (April 2004 – Dec 2004) Ms Claudinia Daley, Research Assistant (Indigenous Initiative, Townsville) (June 2003 – March 2005) Ms Annie Eaton, Research Midwife, Birthcare-Mackay (Dec 2004 – March 2005) New South Wales Prof Bryanne Barnett, State Co-ordinator and Senior Investigator SWSHAS (2001 – 2005) Dr Stephen Matthey, Research Director (2001 – 2005) Ms Janan Karatas, Research and Liaison Officer (Sept 2003 – 2005) Ms Leanne Agius (August 2002 – July 2003) Ms Robby Taouk, Project Officer Arabic Component (March 2002 – Dec 2004) Ms Thu Tram Lee (March 2002 – July 2003) Ms Hanh Tran (February 2004 – Dec 2004) Ms Jane Phillips, Research Assistant IPC (2002 – 2003) A/Prof Marie-Paule Austin, Senior Investigator Royal Hospital for Women (2001 – 2005) Dr Susan Priest, Project Co-ordinator Royal Hospital for Women (2001 – 2005) Ms Sabine Merz, Research Assistant (2004 – 2005) Dr Nick Kowlenko, Senior Investigator Royal North Shore (2002 – 2005) Ms Yvonne McCann, Co-Investigator, Royal North Shore (2002 – 2005) Ms Karen Saint, Senior Research Assistant (2003 – 2005) Australian Capital Territory Prof David Ellwood, State Co-ordinator (2003 – 2005) Ms Rebecca Reay, State Project Manager (2003 – 2005) Ms Maureen Scott, Research Officer (March 2004 – 2005) Page 66 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Hospitals/Area-Health Services Involved A total of 43-hospitals/area health services were involved in screening and/or collecting data for the beyondblue PND Program. They were: Victoria and Tasmania ♦ Werribee Mercy Hospital ♦ Austin Health ♦ Royal Women’s Hospital ♦ Angliss Hospital ♦ Northern Hospital ♦ Hamilton Base Hospital ♦ Launceston General Hospital ♦ Starting Out Program, Connection, Uniting Care ♦ Banyule Community Health Service ♦ Wodonga Regional Health Service South Australia ♦ Women’s & Children’s Hospital ♦ Flinders Medical Centre Western Australia ♦ King Edward Memorial Hospital ♦ Osborne Park Hospital ♦ Mercy Private Hospital Queensland ♦ Townsville, Cairns, West Moreton (Ipswich), Redcliffe/Caboolture, Logan-Beaudesert and Mt Isa Health Service Districts; Mater Hospital in Townsville; Birthcare, Mackay. ♦ Royal Brisbane Hospital (distribution of education booklets only) ♦ State Intervention with Indigenous Women: Townsville Aboriginal and Islander Health Service (Townsville), Palm Island, Yapatjarra and Child Health (Mt Isa) New South Wales ♦ Royal North Shore Hospital ♦ Ryde, Hornsby & Manly Hospitals ♦ Royal Hospital for Women, Randwick ♦ St George Hospital, Kogarah ♦ Liverpool, Fairfield, Bankstown and Campbelltown Hospitals Australian Capital Territory ♦ The Canberra Hospital ♦ Child, Youth and Women’s Health Program ♦ Calvary Public and Private Hospitals Page 67 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Acknowledgements And Thanks First and foremost, the beyondblue National Postnatal Depression would like to sincerely thank the thousands of women, and their families, who participated in this initiative and shared their lives with us over the last four years. We would also like to acknowledge the hundreds of health professionals who gave their time and support to the Program. In particular, we would like to thank the following people and organizations for their ongoing assistance and support: National ♦ Dr Denny Meyer, Faculty of Life and Social Sciences, Swinburne University of Technology ♦ Dr Annie Solterbeck, Statistical Revelations ♦ Marie Homer and Optima Press Pty Ltd ♦ All-Villa Printing ♦ Working Women’s Health ♦ Community Practitioners and Health Visitors Association, United Kingdom ♦ Office of Women’s Health, Vienna, Austria ♦ Australasian and International Marce Societies ♦ INFOMED ♦ Dept of Psychiatry, University of Melbourne ♦ Veterans Psychiatry Unit, Austin Health Victoria ♦ All the management and staff at each of our screening hospitals and community agencies: Werribee Mercy Hospital, Northern Hospital, Launceston General Hospital, The Angliss Hospital, Western District Health Service Hamilton Hospital, The Royal Women's Hospital, Wodonga Regional Health Service Wodonga Hospital, Banyule Community Health Service and Uniting Care Connections. ♦ The General Practitioners who have involved themselves in the treatment of the many women identified through this program and to those who have involved themselves in the training provided to enhance their skills to respond to women with depression in their practices. ♦ Victorian MCHN and Tasmanian FYCH nurses who have always worked with these women and have embraced this program. ♦ The women who have given their time at such a busy stage of their life to help increase our knowledge about perinatal depression by consenting to complete the research questionnaires. ♦ The General Practice Divisions Victoria Mental Health Reference group, ♦ Anne Diamond, Primary Mental Health Care Development and Liaison Officer ♦ The Divisions of General Practice in Victoria ♦ Louise Ryan, South West Health Postnatal Depression Project Worker ♦ Jenny Kelly, Barwon Health Postnatal Depression Project Manager and Catharina Dumaresq, Project Worker ♦ Beth Gemmill, St John Of God Geelong Page 68 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program South Australia ♦ Prof. Marc J.N.C. Keirse, Professor and Head of Dept, Department of Obstetrics, Gynaecology & Reproductive Medicine, Flinders University ♦ Associate Professor Robert Bryce (Clinical Director, Obstetrics & Gynaecology), Flinders Medical Centre ♦ Ms Margaret Smith (Acting Divisional Director, Flinders Women & Children Division), Flinders Medical Centre ♦ Ms Sue Coppi (Clinical Midwifery Manager, Ambulatory Women’s Health Services), Flinders Medical Centre ♦ Ms Julie Pratt (Clinical Midwifery Consultant, Birth Centre), Flinders Medical Centre ♦ Ms Sue Cross (Mental Health Liaison Extended Care Nurse), Flinders Medical Centre ♦ All midwives, Women's Health Clinic, Flinders Medical Centre ♦ All midwives, Birth Centre, Flinders Medical Centre. New South Wales – Royal Hospital for Women ♦ Helen Jarman, Deputy Director of Nursing Royal Hospital for Women ♦ Wendy-Sue Forder, Nurse Unit Manager, Royal Hospital for Women, Outpatient Midwifery Clinic ♦ All Midwives that took part in the beyondblue Program at Royal Hospital for Women New South Wales – SWSAHS ♦ Midwives from the antenatal clinics for collecting the data ♦ Thanks to all sites distributing the booklets ♦ Child and Family Health nurses, general midwives and community women from across Sydney South West Area Health Service - Western Zone for participating in Knowledge and Attitudes study ♦ The IPC program for allowing beyondblue to build on their existing systems and procedures ♦ The CALD women who assisted us in the making of the beyondblue Arabic and Vietnamese resources ♦ The Division of Women and Child Health at Liverpool for acknowledging the importance of perinatal mental health and embracing programs like IPC and beyondblue National Postnatal Depression Program ♦ The 'Obstet' consortium for allowing us to share their psychosocial data New South Wales – Royal North Shore ♦ Catriona Andronicos (OBSTET Database Manager), Northern Sydney Health ♦ Rhonda Bignell (Antenatal Clinic, Nurse Manager) & all midwives working in the Antenatal Clinic, Hornsby-Kur-ring-gai Hospital (H-K) ♦ Shirley Burgoyne & Carmel O'Colmain (Maternity Discharge Planners), Royal North Shore Hospital (RNS) ♦ Cathy Boot (Midwifery Educator), RNS ♦ Kirsty Brown (Nurse Manager, Antenatal Clinic) & her staff at RNS ♦ Sue Coats (Midwifery Educator,) Manly Hospital ♦ Jacqueline Evans (Nurse Manager, Antenatal Clinic) & her staff at Manly Hospital ♦ Geraldine Gilroy & Sheena Jackson (Midwifery Educators), H-K Page 69 of 108 beyondblue National PND Program Final Report ♦ ♦ ♦ ♦ ♦ ♦ VOL I: National Screening Program Samantha Harrop (Receptionist, Maternity), RNS Yvonne McCann (Divisional Manager, Women's, Children & Family Health), RNS Pamela Rawling (Maternity Department - Nurse Unit Manager) Manly Hospital Janice Sim (Clinical Midwifery Consultant), H-K Rohini Singh (Administrative Officer, Delivery Suite, Maternity), RNS Carolyn Smith (Divisional Manager, Maternity and Child & Family Health Service), H-K Western Australia ♦ Department of Psychological Medicine, King Edward Memorial Hospital ♦ Social Work Services, Osborne Park Hospital ♦ Antenatal Clinic Staff at King Edward Memorial Hospital, Osborne Park ♦ Hospital and Mercy Hospital ♦ Anna Roberts, General Practice Division of WA ♦ Community Midwifery WA ♦ Women and Infants Research Foundation, King Edward Memorial Hospital ♦ School of Psychology, Edith Cowan University ♦ Dr Jann Marshall and Western Australia's Child Health Nurses ♦ The Australian Multiple Birth Association Queensland ♦ School of Nursing Sciences, James Cook University, Townsville. ♦ Queensland Health and the Townsville, Cairns, Mackay, Logan-Beaudesert, West Moreton Health Service Districts, their associated Ethics Committees, and Birthcare, Mackay. ♦ Without the active and strategic support of Child Health Centres in Cairns, Townsville, Mackay, Ipswich and Logan the assessment and care of women at risk of depression would not have been the seamless process it turned out to be. ♦ Midwives, Child Health Nurses, Social Workers, Psychologists, General Practitioners and other Allied Health Professionals who assisted the program in numerous ways by participating, accepting referrals, or smoothing the research process. ♦ Queensland Health, the Palm Island Council, the Boards of Yapatjarra (Mt Isa), and the Townsville Aboriginal and Islander Health Service, the Elders and others who participated in reference groups. Australian Capital Territory ♦ The Canberra Hospital public maternity unit ♦ Community Midwifery Program, TCH ♦ Calvary Hospital private and public maternity units. ♦ Child Youth and Women's Health Program ♦ ACT Division of General Practice ♦ Mental Health ACT ♦ Aboriginal Health Service ♦ Post and Antenatal Depression Support and Information Inc (Pandsi) ♦ Families First at Greater Southern Area Health Service Page 70 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Appendices A. Feedback to Services Document B. Detailed List of the Organizations to Receive PND Training C. Health Professional Training Guidelines D. Detailed List of Media and Promotional Activities E. Detailed List of Conference Presentations and Scientific Articles Page 71 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Appendix A – Feedback to Services Document DRAFT EMOTIONAL HEALTH CARE IN PREGNANCY & POSTPARTUM Key Findings and Recommendations: The beyondblue National PND Program What was the Program? This program involved 43 antenatal hospitals/area-health services across Australia over 2001-5 in assessing the feasibility and acceptability of routine perinatal depression screening. Information was collected from the largest sample of Australian women ever screened for depression to help better understand the risks and their potential solutions. Why does perinatal depression matter? Perinatal (antenatal/postnatal) depression affected 15.7% of the 40,000 Australian mothers who were involved in the program. There are significant long-term impacts on women’s mental health and parenting, on their partners and on the developmental prospects of their children. Prevention does not appear effective so early intervention, with best-practice, evidenced-based treatments, offers the best outcome. What did the Program find? Screening with the Edinburgh Postnatal Depression Scale was highly acceptable to (85%) women and simple to complete. Staff also found screening feasible but only with appropriate support and education. High depression scores were stressful for screening staff to deal with, however, with established care pathways they became comfortable with their ability to help the women who need it. Distress was related to high screening scores (i.e. the depression) rather than the screening process itself. Routine screening gives the best possible opportunity to ensure that over half of the women that would be otherwise missed will be identified. Identification alone does not ensure treatment will be sought, this it must be combined with staff education, support and facilitation of pathways to care. Provision of information in pregnancy enabled women to be better informed about mental health issues. Given this information, women at risk of depression were better able to assess their own mental state and reported better satisfaction with their support and networks after the program than before. Page 72 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Key Recommendations 1. Depression screening can and should be a routine part of antenatal and postnatal care; 2. The highest time of risk is in the third trimester and is the ideal time to screen; 3. The EPDS is an ideal screening tool for assessing mood status; 4. Key questions for assessing risk and assistance in planing included level of available support, past history of anxiety & depression and current life stresses; 5. Care pathways including appropriate local referrals and service links need to be developed; 6. An information and resource booklet on emotional health in the perinatal period should be provided to all pregnant women in Australia; 7. There is a need for resources specific to certain groups such as CALD women, Indigenous women and multiparous women; 8. Midwives and doctors offering screening obstetric care are in an ideal position to distribute depression information and undertake psychosocial assessment as a routine part of their holistic care of women and their families. The National & State Directors of the beyondblue National PND Program Anne Buist & Jeannette Milgrom, University of Melbourne (Psychiatry & Psychology) Bryanne Barnett & Marie-Paule Austin, University of NSW (Psychiatry) Nick Kowalenko, University of Sydney (Psychiatry) John Condon, Flinders University (Psychiatry) Barbara Hayes, James Cook University (Nursing) Craig Speelman, Edith Cowan University (Psychology) David Ellwood, Australian National University (Obstetrics) Page 73 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Appendix B – Detailed List of Organizations to Receive PND Training Title National Office Postnatal Depression Parenting with a Mental Illness The National Postnatal Depression Project: The implication for divisions Women, Hormones & Mental Illness The National Postnatal Depression Program Postnatal Depression – an evening seminar. Parents with a Mental Illness – Issues for risk assessment Postnatal Depression The National Postnatal Depression Program Semester 10: Psychiatry National Postnatal Depression Program Information seminar of the National Postnatal Depression Program PND for overseas trained Doctors Parenting with a Mental Illness Women’s Mental Health Issues Children with parents who have a mental illness Children with parents who have a mental illness Postnatal Depression and the National PND Program Page 74 of 108 Source/Event Date Southern Region General Practitioners Barwon Health & Geelong Clinic Mental Health Network, GPDV GP Meeting, Bundoora, Victoria GP Training Seminar – Westgate Division of General Practice (12 GPs) Angliss Hospital (20 MW/MCHNs) Child Protection Practitioners Forum: A Professional Development Opportunity Postnatal Depression Twilight. St Vincent’s & Mercy Private Hospital Education Comm. Information Seminar on postnatal depression Launceston General Hospital Faculty of Medicine, Dentistry & Health Sciences, University of Melbourne Northern Hospital. Melbourne. South West Postnatal Depression Forum, Warrnambool Jean Hales Foundation. February 2002 February 2002 May 2002 July 2002 October 2002 Protective Services Victoria Panel Discussion - The Australian Unity Wellbeing Index. Dept of Human Services. Induction Program. Melbourne Dept of Human Services. Induction Program. Melbourne. Postnatal Depression & Mental Health Issues March 2003 March 2003 November 2002 November 2002 November 2002 December 2002 Feb 2003 Feb 2003 February 2003 March 2003 March 2003 March 2003 June 2003 beyondblue National PND Program Final Report VOL I: National Screening Program RWAV – Overseas Training Doctor Program The Hidden Enemy – Postnatal Depression The Hidden Enemy – Post Natal Depression Parenthood and mental Illness: including postpartum disorders Depression in Women The Wide Umbrella of Postnatal Depression SPHERE Presentation Women with Postnatal Depression Women with Postnatal Depression Efficacy of Clinical Supervision for Postnatal Depression Clinical Presentations The Legacy of child abuse: learning’s from the past and changing the future Postnatal Depression in Australia – the beyondblue PND Program Introduction to women’s mental health and depression, Postnatal Depression, Depression and the menopause, Premenstrual dysphoric disorder, Drug and non-drug treatment options SPHERE Presentation PND. Presentation to Obstetricians/Clinicians. PND. Presentation to Health Professionals. SPHERE Presentation PND & Effects on the Child Page 75 of 108 for the Parturient Woman. Benchmark Education for Midwives (50 MW) Echuca, Victoria. Mercy Learning Centre, Mercy Hlth Service, Albury. Wodonga Hospital, Wodonga 2nd Yr PM/Mpsychiatry Adult Psychiatry 1. Mental Health Research Institute Darwin Meeting (GPs & Psychiatrists) The Early Motherhood Service, Integrated Primary Mental Health NE Victoria (30 Psych nurses, GPs & MCHNs) Otway DGP (15 GPs) Dandenong Midwives Association. Annual General Meeting (30 MW) Dandenong Midwives Association. Annual General Meeting. Clinical Supervision in Nursing Practice: Giving voice to action. Ballarat. Launch of Safe from Harm: Professional development and eduction resource for Nurse. Aust Nursing Federation, Victorian Branch. Depression & Anxiety Consumer Research Unit, National Instit. of Health & Human Sciences, Australian National University Women’s Mental Health and Depression. Presentation to Knox Division of General Practice Bendigo & District DGP (10 GPs) Geelong Hospital (8 MW) Geelong Hospital (15) GPs Geelong Div of General Practice (12 GPs) Albert Road Clinic, Melbourne (10 July 2003 August 2003 August 2003 September 2003 November 2003 November 2003 November 2003 November 2003 November 2003 November 2003 December 2003 April 2004 May 2004 May 2004 May 2004 May 2004 May 2004 October 2004 beyondblue National PND Program Final Report VOL I: National Screening Program PND Workshop Women’s Mental Health Postnatal Depression Postnatal Depression “Breaking the Cycle: Early detection and early intervention.” PND: Implications for our region. Victoria Postnatal Depression Focus Group with to evaluate the program Update of program progress One-day workshop – “Postnatal Depression." Included assessment and treatment and the National Postnatal Depression Program. Workshop ‘Treating Postnatal Depression’. Training Midwives 11/2 hours 10 midwives Training day “Getting Ahead of Postnatal Depression Program” to Training session with. EPDS and Postnatal depression. 15 nurses MCHN training session 15 nurses Presentation to with feed back from 1st year of screening Psychiatrists) Mildura, MCHN (25 MW/MCHNs) Teleconference, Warrnambool Mental Health Group Facilitation of Pfizer Workshop for General Practitioners. Centonove, Kew (10 GPs) Obstetricians & Gynaecologists. Northpark Private Hospital (12 O&G/MCHNs) Mercy Health Service, Albury (30 MCHNs) May 2005 Mental Health Forum Leongatha Vic Mercy Werribee midwives Werribee Mercy Midwives Queen Elizabeth Centre, Noble Park August 2001 October 2002 December 2002 February 2003 Austin Health Nurses and Psychologists Launceston General Hospital May 2003 June 2003 Shepparton MCHN and PMHT workers MCHN at City of Wyndham Banyule Midwives and antenatal staff Werribee Mercy Hospital Trained midwives, Obstetrician Social Worker, set up NPDP. Visited GP North Launceston General Hospital Division organized mailout for Baseline MCHN training session Whittlesea Meeting with CEO and Midwifery staff. Training about bb program Wodonga Health Service Training 10 midwives RWH Training 3 staff Connections Starting Out Page 76 of 108 November 2004 March 2005 March 2005 April 2005 June 2003 July 2003 October 2003 October 2003 October 2003 November 2003 January 2004 May 2004 May 2004 beyondblue National PND Program Final Report VOL I: National Screening Program MCHN training 6 Nurses NPDP Screening with EPDS NPDP and work of PIRI Midwife training 6 nurses re set up Toward Parenthood screening Training MCHN 5 nurses NPDP and Toward Parenthood protocols Postnatal Depression and NPDP preliminary findings at Northern Hospital NPDP NPDP Training session on EPDS 14 staff Antenatal and Postnatal Depression Postnatal Depression and NPDP and screening with EPDS Workshop presentation – Lifecycle Stage Example, Transition to Parenthood Invited workshop - A Workshop on Interventions following Postnatal Depression targeting both Maternal Mood and the Mother-Infant Interaction. Findings of Beyondblue NPDP and Models of Care NPDP and Screening with the EPDS The role and relevance of the Edinburgh Postnatal Depression Scale NPDP and Screening with the EPDS beyondblue National Postnatal Depression Program- Research Impacting Care The Role and Relevance of the EPDS Toward Parenthood project and NPDP Postnatal Depression Implementation of a Perinatal Mental Health Screening Program. The Page 77 of 108 City of Melbourne City of Melbourne MCHN 6 Austin Health GP Liaison Officer Northern Hospital City of Wodonga Northern Hospital 6 midwives, 1 social worker Study Day Northern Hospital Midwives and allied health obstetricians and consumers 50 City of Wodonga MCHN 5 Wodonga Hospital midwives O’Connell Centre La Trobe University Psychology Students 10 students O’Connell Centre MCHN and mothercraft nurses 14 staff Alma Family Therapy Centre APS College of Health Psychologists, Melbourne June 2004 June 2004 June 2004 July 2004 July 2004 July 2004 July 2004 City Of Banyule MCHN City Of Wyndham MCHN City of Greater Geelong and Barwon Health Women’s and Children’s Services. Surf Coast MCHN 2 hours City of Moonee Valley MCHN Australian College of Midwives Conference Dandenong Hospital Division of General Practice Victoria Primary Mental Health Forum Study Day Northern Hospital Midwives and allied health 40-60 staff GPs Primary Mental Health Policy Forum DHS Vic Forum Exploring Different October 2004 October 2004 October 2004 July 2004 July 2004 August 2004 August 2004 August 2004 August 2004 September 2004 October 2004 November 2004 November 2004 November 2004 December 2004 February 2005 beyondblue National PND Program Final Report VOL I: National Screening Program beyondblue National Postnatal Depression Program Screening for PND in the Community Risk Factors for Antenatal Depression, Postnatal Depression and Parenting Stress NPDP overview. Toward Parenthood NPDP Toward Parenthood NPDP and Treatment for Depression Treatment for Postnatal Depression Treatment for PND Poster presentation and display about NPDP NPDP and screening with EPDS Western Australia Depression in the Perinatal Period: Early Intervention & Prevention Approaches to the Psycho-Social Health and Wellbeing of Pregnant and Post Partum Women 15 MCHN City of Knox 2 hours Angliss Hospital midwives Freemasons Hospital Midwives MCHN City of Yarra 45 mins Panda support group leaders conference 2 hours I day workshop for 10 MCHN at O’Connell Family Centre City of Banyule MCHN Research and Innovation Fair Melbourne University RWH Midwives Trained for screening Osborne Park Hospital, Clinical Update Workshop, Oral Depression in the Perinatal Period: Early Intervention & Prevention Swan Districts Mental Health Service, Oral Depression in the Perinatal Period: Early Intervention & Prevention Health Department of WA Child Health Nurse Clinical Update, Oral The beyondblue National Postnatal Depression Early Intervention & Prevention Nickol Bay Hospital, Karratha, Oral Program Depression in the Perinatal Period: Early Intervention & Prevention Strategies Full day facilitated workshop for local Health Professionals, Geraldton WA Depression in the Perinatal Period: Early Intervention & Prevention Strategies Swan/Kalamunda Health Service, Oral The beyondblue National Postnatal Depression Early Intervention & Prevention Facilitated Rural Mental Health Teleconference, Program Oral The beyondblue National Postnatal Depression Early Intervention & Prevention Lecture for Clinical Master of Psychology Program – WA Intervention “You, Me & Baby Makes Three” students, Edith Cowan University Depression in the Perinatal Period: Early Intervention & Prevention Strategies King Edward Professional Development Week, Oral The beyondblue National Postnatal Depression Early Intervention & Prevention Mercy Private Hospital, Staff Development Program Workshops x 2 Page 78 of 108 March 2005 March 2005 March 2005 April 2005 May 2005 May 2005 May 2005 May 2005 May 2005 June 2002 June 2002 June 2002 July 2002 October 2002 October 2002 October 2002 October 2002 May 2003 May, June 2003 beyondblue National PND Program Final Report VOL I: National Screening Program The beyondblue National Postnatal Depression Early Intervention & Prevention Program Resources The beyondblue National Postnatal Depression Early Intervention & Prevention Program Resources Depression in the Perinatal Period: Early Intervention & Prevention Strategies ‘Better Outcomes – Better Incomes’ Workshop, General Practice Division WA ‘Partnerships’ Conference, General Practice Division WA King Edward Memorial Hospital Midwife Refresher Course, Oral The beyondblue National Postnatal Depression Early Intervention & Prevention Mental Health Training Workshop, General Program Resources Practice Division WA The beyondblue National Postnatal Depression Program Community Midwifery WA, Training Workshops x 2 Perinatal Mental Health in Australia: Research & Clinical Practice Edith Cowan University, 4th year psychology students, Oral Screening for PND: The beyondblue National Postnatal Depression Program Postnatal Depression Professionals Association, Oral Emotional health during pregnancy and early parenthood: early intervention North Metropolitan Health Service (NEST), and treatment Inner Metro Child Health Nurses Training Workshop Screening for depression during pregnancy and early parenthood Australian Association for Cognitive Behaviour Therapy (WA) Inc. Mental Illness…and Motherhood King Edward Memorial Hospital Professional Study Day Queensland Emotional health of Childbearing women Two-day presentation and workshop for Aboriginal Health Workers, women Elders and other Indigenous women at Palm Island Screening for depression: The beyondblue PND program, reliability and Undergraduate program, School of Psychology, validity of the EPDS James Cook University The beyondblue National Postnatal Depression Program: Equipping Child Statewide Mail-Out to Queensland Child Health Health Professionals to manage emotional health of Childbearing Women Centres The beyondblue National Postnatal Depression Program: Screening for Migrant Resource Centre Mental Health Antenatal and Postnatal Depression; Grief, Loss and Depression in Awareness and Access Project, Townsville Childbearing women West Moreton Health District: Screening for Antenatal and Postnatal Midwives, neonatal nurses and birth suite Page 79 of 108 September 2003 October 2003 October 2003 November 2003 March 2004 March 2004 April 2004 May 2004 May 2005 May 2005 July 2004 Aug-Sept 2004 Aug-Sept 2004 Sept 2004 Sept 2004 beyondblue National PND Program Final Report VOL I: National Screening Program Depression The beyondblue National Postnatal Depression Program: Antenatal and Postnatal Depression and the EPDS Logan Health District: Screening for Antenatal and Postnatal Depression The beyondblue National Postnatal Depression Program: Screening for Antenatal and Postnatal Depression The beyondblue National Postnatal Depression Program: Antenatal and Postnatal Depression and the EPDS The beyondblue National Postnatal Depression Program: Antenatal and Postnatal Depression and the EPDS Follow-up training re screening for post-natal depression (Indigenous program) Emotional Health of Childbearing Women: Do we take it for granted? Follow-up training re screening for post-natal depression (Indigenous program) Screening for postnatal depression in Childbearing women Screening for postnatal depression. Feedback and description of screening The beyondblue National Postnatal Depression Program: Ending well, Screening for Antenatal and Postnatal Depression Screening for postnatal depression in Childbearing women Page 80 of 108 midwives Undergraduate program for Nurses in Mental Health Series, James Cook University Midwives, neonatal nurses and birth suite midwives University and Health Care Administrators: University College, Alesund, Norway Undergraduate program for nurses in the mental health series, University College, Molde, Norway Postgraduate program for nurses and social scientists, University College, Molde, Norway Palm Island Health Workers Australian Catholic University, Sydney Australia. Invited presenter of the 2004 Victor J. Couch Public Lecture. Palm Island Health Workers Education, training and support for Aboriginal health Workers at Yaptajarra (Community Controlled Health Centre) and at the child Health Centre, Mt Isa One day education and training for perinatal and family Aboriginal Health Workers (Mixed Gender) at Palm Island The Steering Committee of the Mums and Babies Unit, Townsville Aboriginal and Islander Health Service Health Administrators, Midwives, Child Health, other Health Professionals: Mackay Health Service District Education, training and support for Aboriginal health Workers at Yaptajarra (Community Controlled Health Centre) and at the child Health Centre, Mt Isa Sept 2004 Oct 2004 Sept 2004 Sept 2004 Sept 2004 Sept 2004 Oct 2004 Oct 2004 Dec 2004 Dec 2004 Feb 2005 Feb 2005 Feb 2005 March 2005 beyondblue National PND Program Final Report VOL I: National Screening Program The beyondblue National Postnatal Depression Program: Ending well, Screening for Antenatal and Postnatal Depression: A Health District Perspective Screening for postnatal depression The beyondblue National Postnatal Depression Program: Ending well, Screening for Antenatal and Postnatal Depression: A Health District Perspective The beyondblue National Postnatal Depression Program: Ending well, Screening for Antenatal and Postnatal Depression: A Health District Perspective The beyondblue National Postnatal Depression Program: Equipping General Practitioners to manage emotional health of Childbearing Women The beyondblue National Postnatal Depression Program: Equipping Rural Nurses to manage emotional health of Childbearing Women New South Wales 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & PND assessment & management Tresillian Home Visiting Family Intervention Program: Work in Progress Building Better Beginnings 'beyondblue' the National PND Program 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & in NSH Page 81 of 108 Health Administrators: Cairns Health Service District April 2005 One day education and training for perinatal and April 2005 family Aboriginal Health Workers (Mixed gender) at Palm Island Health Administrators: West Moreton Health April 2005 Service District Health Administrators: Logan Health Service District April 2005 Townsville Division of General Practitioners Mail-Out Australian Association for Rural Nurses MailOut May 2005 Obstetrics & Gynaecological Meeting RNS Maternity Department RNS Student Doctors, RNS Maternity staff RNS LNS PND Interest Group Maternity staff RNS & Ryde Hospitals Hornsby-Kur-ring-ai Perinatal Mental Health Interest Group C&FHS Queenscliff HC Ryde Perinatal Health Promotion Committee Mona Vale Hospital Maternity staff Northern Beaches PND Interest Group Mater Hosp Maternity staff LNS Div of GPs Manly Hospital Maternity staff February 2003 February 2003 February 2003 March 2003 April 2003 July 2003 August 2003 May 2005 August 2003 September 2003 October 2003 November 2003 November 2003 February 2004 February 2004 beyondblue National PND Program Final Report VOL I: National Screening Program 'beyondblue' the National PND Program & in NSH 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management Postnatal Depression Management and 'beyondblue' the National PND Program 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management Perinatal Mental Health 'beyondblue' the National PND Program & PND assessment & management 'Breaking the Cycle - Early detection & early intervention' South Australia 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management Page 82 of 108 Hornsby Hospital Maternity staff Manly Hosp Maternity staff Hornsby Hosp Maternity staff Student MWs at University of Technology, Syd Lower North Shore Division of General Practice February 2004 March 2004 April 2004 August 2004 August 2004 Student Doctors, RNS Maternity staff, North Shore Private hospital St. John of God, Burwood Bowral DGP H-K-H Perinatal Mental Health Interest Group Mercy Learning Centres, Albury November 2004 February 2005 February 2005 March 2005 April 2005 May 2005 Women’s and Children’s Hospital Obstetrics Division Women’s and Children’s Hospital Maternity Division Flinders Medical Centre Obstetrics Division Flinders Medical Centre Maternity Division Women’s and Children’s Hospital Grand Ward Round Women’s and Children’s Hospital Maternity staff Modbury Hospital Maternity staff Flinders Private Hospital Maternity staff Ashford Private Hospital Maternity staff Calvary Private Hospital Maternity staff Southern Division of General Practitioners Women’s and Children’s Hospital Maternity staff update Southern Division of General Practitioners Central Division of General Practitioners Upper Eyre Health Service, Streaky Bay August 2001 September 2001 October 2001 October 2001 November 2001 November & December 2001 April 2002 May 2002 June 2002 July 2002 July 2002 November & December 2002 August 2003 September 2003 May 2004 beyondblue National PND Program Final Report VOL I: National Screening Program 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management 'beyondblue' the National PND Program & PND assessment & management Page 83 of 108 Lower Eyre Health Service, Port Lincoln, Kangaroo Island Health Service, Kingscote, Alice Springs Health Service, Alice Springs, NT Darwin Mental Health, NT Health Department Flinders University of SA Bachelor of Midwifery Central Division of General Practitioners South East Health Area, Mt Gambier Health Service South East Division of General Practitioners Leigh Creek Hospital, Leigh Creek Child and Youth Health Modbury Child and Youth Health Salisbury Child and Youth Health Norwood Child and Youth Health Marion Port Pirie Hospital Maternity Staff Flinders University of SA Bachelor of Midwifery May 2004 June 2004 August 2004 August 2004 November 2004 September 2004 March 2005 March 2005 May 2005 June 2005 June 2005 June 2005 June 2005 June 2005 June 2005 beyondblue National PND Program Final Report VOL I: National Screening Program Appendix C – Health Professional Training Guidelines Training in Perinatal Mental Health Issues Suggested Minimum Information 1. Antenatal 1.1 Current depression and/or anxiety ♦ Symptoms – what is normal and what is not ♦ Identification/diagnosis by screening questionnaires ♦ Management overview, including issues of level of severity and chronicity, and comorbidity eg personality disorders ♦ Use of psychotropic medication in pregnancy ♦ When to refer to a specialist (see also 2.8) 1.2 Groups at risk antenatally of developing PND or PNA (anxiety) 1. Identification by history or screening 2. Use of the EPDS 3. Management 2. Postnatal 2.1 Types of mood changes/adjustment disorders postnatally ♦ Normal mood changes ♦ Adjustment disorders/anxiety ♦ Blues ♦ Puerperal psychosis including brief outline ♦ PND ♦ Related disorders (eg GAD, phobias, PTSD) 2.2 Assessing postnatal mood ♦ Symptoms and findings including physical conditions i.e. differential diagnosis ♦ Overview of management including issues of level of severity and chronicity, and co-morbidity (eg personality disorders) ♦ When to consult/refer to specialist mental health services (see also 2.8) ♦ Use the Management Guide to help develop an individual management plan with patient & partner input (if applicable) 2.3 Men and PND ♦ Men and their perinatal mood changes ♦ Impact on male partner and responses to depressed mother ♦ Effects on relationships esp. libido ♦ What men can do to help with PND Page 84 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program 2.4 Infant development & PND ♦ Effects and ways of managing 2.5 Extended family and PND ♦ What grandparents etc can do to help 2.6 Medication ♦ Psychotropic medication in pregnancy and breastfeeding 2.7 Community supports ♦ Self-help groups, child and youth health etc 2.8 Referral ♦ When to consider referral and what options are available 2.9 Counselling skills ♦ This will depend on the time available ♦ May include either the BATHE technique (from Anne Sved-Williams), CBT (which is also covered by the Sphere program) or any other counselling technique favoured Page 85 of 108 beyondblue National PND Program Final Report VOL I: National Screening Program Appendix D – Detailed List of Media and Promotional Activities TV, Radio and Promotional Activities Headline/Title/Event National Office Postnatal Depression Parenting with a Mental Illness beyondblue Postnatal Depression Project beyondblue Postnatal Depression Project The National Postnatal Depression Program: Implementation issues and proposed outcomes Update on the beyondblue National PND Program & progress in Tasmania Mother-Baby Postnatal Depression and the National PND Program Life Cycle Depression in Women Pregnancy and lactation. Special topics in pharmacotherapy Psychosocial Assessment of Mothers and Infants Postnatal Depression in Australia – the beyondblue PND Program Psychosocial Assessment of Mothers and Infants. Pregnancy, Breastfeeding and Psychotropic Medications Page 86 of 108 Source/Event Promoting Women’s Mental Health, Banksia House Mother Baby Unit, Austin Health Annual Meeting, Family Care Sisters & Mercy Health & Aged Care Board of Governance Royal Australian College of General Practitioners – Victoria. Maternal & Child Health Sub-Committee, Royal Australian College of General Practitioners Hunter Valley, N.S.W Postnatal Depression Professional Forum. Launceston Orygen Youth Health Postnatal Depression & Mental Health Issues for the Parturient Woman. Benchmark Education for Midwives. Medical Meetings. Park Hyatt, Melbourne 4th year MPM. Austin Health, Management Strategies for Child & Family Services Conference. Melbourne Depression & Anxiety Consumer Research Unit, National Instit. of Health & Human Sciences, Australian National University. Canberra. Management Strategies for Child & Family Services Conference. Melbourne 2nd Yr PM/Mpsychiatry Adult Psychiatry 1. Date October 2001 October 2001 November 2001 November 2001 August 2002 May 2003 May 2003 June 2203 July 2003 August 2003 May 2004 May 2004 May 2004 August 2004 beyondblue National PND Program Final Report Postnatal Depression - the latest from beyondblue Responding to Maternal Depressive Illness National PND Program Implementation of a National Perinatal Mental Health Screening Program: The beyondblue National Postnatal Depression Program Implementation of a National Perinatal Mental Health Screening Program: The beyondblue National Postnatal Depression Program Implementation of a National Perinatal Mental Health Screening Program: The beyondblue National Postnatal Depression Program Implementation of a National Perinatal Mental Health Screening Program: The beyondblue National Postnatal Depression Program The Development of a National Perinatal Depression Screening Program in an Australian Population The Development of a National Perinatal Depression Screening Program in an Australian Population Queensland The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood – combined presentation The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood – Page 87 of 108 VOL I: National Screening Program Mental Health Research Institute Helping Mothers in the 1st Year, Nurse Education Unit. Peninsula Health. Mental Health in the Young: A Challenge to the Community Workshop. Royal Children's Hospital, Melbourne Perinatal Psych Group Francis Perry House, Carlton, Victoria St Vincent’s and Mercy Private Hospital, Melbourne, Victoria Postnatal Depression Study Day, St John of God Hospital The Benefit of Knowing, Bass Coast Regional Shire, Wonthaggi Wiener Frauengsundheitsprogramm Friedrich Schimdt-Platz, Rathaus, Vienna October 2004 October 2004 March 2005 October 2004 November 2004 November 2004 October 2004 October 2003 Community Practitioners and Health Visitors Association, London, England November 2003 Australian Psychological Society – Townsville August 2001 James Cook University, incoming midwifery students (Practice 1 & 3) Townsville District Health Service May 2002 May 2002 Mental Health Services – Townsville District June 2002 Institute of Women’s & Children’s Health June 2002 beyondblue National PND Program Final Report telepsychiatry links The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood – (networking) The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood (Professor Anne Buist) VOL I: National Screening Program Townsville Hospital, Midwives & Social Work Department June 2002 Townsville Hospital floor midwives education July 2002 Steering committee for postnatal issues: Townsville District Health Service QHealth-Family Care (early intervention program) Program Townsville Aboriginal & Islander Health Service July 2002 TAIHS- Medical and nursing staff October 2002 TAIHS-Indigenous focused October 2002 Faculty of Medicine, Health and Molecular Sciences, JCU Research Day Infant Management & Parenting Scheme October 2002 October 2002 Child & Youth Mental Health Service November 2002 Sphere November 2002 July 2002 October 2002 The Townsville Hospital: Consultant psychiatrists, December 2002 Obstetricians, Senior General Medical Practitioner, Senior Midwives, Child Health Nurses, Allied Health Professionals, Floor Midwives The beyondblue National Postnatal Depression Program – information and Consultant psychiatrists, Obstetricians, Senior March 2003 education regarding Depression in pregnancy & early parenthood (sponsored General Medical Practitioners, Senior Midwives by Pfizer) and Child Health Nurses, Allied Health Professionals, Clinic/Unit Midwives The beyondblue National Postnatal Depression Program – information and Cairns Base Hospital - Institute for Women’s & March 2003 Page 88 of 108 beyondblue National PND Program Final Report education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and education regarding Depression in pregnancy & early parenthood The beyondblue National Postnatal Depression Program – information and Page 89 of 108 VOL I: National Screening Program Children’s Health Clinicians & Consumers Townsville Division of General Practice; April 2003 2 x Townsville Community Health Centres April 2003 Cairns Base Hospital – Mental Health Services June 2003 Mount Isa Centre for Rural & Remote Health June 2003 Mt Isa District Health’s Service Grand Rounds – GPs, Psychologists, Medical Students & Other Health Professionals Mackay – Mental Health Services June/July 2003 June 2003 Mt Isa – Integrated Mental Health Services June 2003 Mt Isa & Mackay – Child Health Services June 2003 Mt Isa Base Hospital – Indigenous Liaison June 2003 Mt Isa, Community Health Centre Indigenous Team North West Queensland Primary Health Care Team Mt Isa Integrated Mental Health – Indigenous focus Yapatjarra Health Centre – Indigenous health team June 2003 Palm Island Council – Indigenous initiatives – Council and lay members Q Health Northern Zone Manager (Mackay to Cape York) Palm Island – Director of Nursing, Chief Medical July 2003 July 2003 August 2003 September 2003 September 2003 September 2004 beyondblue National PND Program Final Report education regarding Depression in pregnancy & early parenthood NQ Post-Natal Distress Support Group: Information Booklet Western Australia Launch of the beyondblue National Postnatal Depression Early Intervention & Prevention Program The beyondblue National Postnatal Depression Early Intervention & Prevention Program Launch of the beyondblue National Postnatal Depression Early Intervention & Prevention Program The beyondblue National Postnatal Depression Early Intervention & Prevention Program The beyondblue National Postnatal Depression Early Intervention & Prevention Program Depression in the Perinatal Period: Early Intervention & Prevention The beyondblue National Postnatal Depression Early Intervention & Prevention Program – Associated Postgraduate Research Projects The beyondblue National Postnatal Depression Early Intervention & Prevention Program: A Preliminary Analyses The beyondblue National Postnatal Depression Program: Early Intervention & Prevention Strategies It’s Postnatal Depression Awareness Week Raising Awareness of PND N/A New light shed on depression beyondblue the National Depression Initiative Page 90 of 108 VOL I: National Screening Program Officer, Integrated Mental Health team, Antenatal & Postnatal Clinic staff NQ Post-Natal Distress Support Group: For October 2004 Families, By Families, With Families. Information Booklet Launch Channel 31 ‘Face the Facts’ 2 x Interviews December 2001 Women’s Health Care House, Perth, Oral January 2002 Official WA Launch of the Program at Edith Cowan University Edith Cowan University, Oral February 2002 Health Department of WA Mental Health Symposium, Oral King Edward Memorial Hospital Midwives, Oral Women & Infants Research Foundation, Workshop King Edward Memorial Hospital Lunchtime Lecture Series, Oral General Practice Divisions WA, Mental Health Officers, Oral 7 x Promotional Displays: King Edward Memorial Hospital, King Edward Family Birth Centre, Osborne Park Hospital, Mercy Private Hospital, Edith Cowan University School of Psychology, ECU Psychological Services Centre Radio Fremantle, On-air Interview Radio National, On-air Interview Wanneroo Times, Newspaper Article Women & Infants Research Foundation, Teenage Parents Festival March 2002 March 2002 July 2002 December 2002 February 2003 April 2003 November 2003 December 2003 January 2004 January 2004 September 2004 beyondblue National PND Program Final Report Raising Awareness of PND Raising Awareness of PND Results of the beyondblue National Postnatal Depression Project for Families with Multiple Birth Children Australian Capital Territory Postpartum Depression in Australia: The beyondblue Postnatal Depression Program: A/Prof Anne Buist. The lived experience of postnatal depression: radio interview with ACT Consumer and Rebecca Reay Postnatal Depression Seminar: The National Postnatal Depression Program: The ACT experience of the National Postnatal Depression Program Victoria Identification, Assessment and Management of Maternal Depression. Is it enough to use Depression Improvement as an Outcome Measure with Postnatal Depression Treatment? The Parent-Infant Interaction Day long planning seminar on health promotion and PND on needs, identification of women, provision of services Maternal and Child Health Nurse Information session Maternal and Child Health Nurse Information session Information session Maternal and Child Health Nurse Information session Maternal and Child Health Nurse Information session Maternal and Child Health Nurse Information session Maternal and Child Health Nurse Information session Maternal and Child Health Nurse Information session Grand Round, Austin Health Page 91 of 108 VOL I: National Screening Program Radio West, On-air interview Twin Cities Radio, On-air interview Australian Multiple Birth Association, State (WA) Committee AGM November 2004 December 2004 May 2005 National Institute of Human and Health Sciences: Australian National University ABC Radio Canberra April 2004 ACT Division of General Practice Rydes Hotel, Maunka, ACT 2XX Radio Canberra August 2004 April 2004 June 2005 Centre for Community Child Health Seminar New Directions in Assessment and Management of Infant Distress. Royal Children’s Hospital Research Week Austin Health August 2001 November 2001 Moreland City Council January 2002 City of Wyndham City of Whitehorse Northern Birthing Support Service City of Whittlesea City of Whitehorse City of Darebin City of Nillumbik City of Moreland Antenatal Depression- Enhancing the parent-infant relationship. (Victorian component of the beyondblue NPDP) February 2002 February 2002 February 2002 May 2002 May 2002 May 2002 June 2002 June 2002 July 2002 beyondblue National PND Program Final Report Maternal and Child Health Nurse Information session Health professionals Information session Midwife Information session Midwife Information session Midwives and interested health professionals info session Primary Mental Health Team presentation on Depression Management and NPNP PND Information evening - various health professionals including GPs, MCHNs, midwives, social workers, etc. Maternal and Child Health Nurse Information session Invited speaker - Postnatal Depression. Information session for Antenatal Educators Information session for Family Birth Centre midwives Meeting with PR dept to publicize NPDP in local paper and to extend screening to further clinics Presentation about the NPDP ½ day workshop on NPNP and PND to health professionals Information session on NPDP Information session with midwives Regional meeting with MCHN Coordinators Information session on NPDP “Australia talks back” - guest presenter “Behind Closed Doors” - presenting the research, profiling best practice. Mental Health Reference group meeting Invited speaker - Postnatal Depression Postnatal Depression and General Practice What is the effect of maternal depression on the infant? What Helps? Page 92 of 108 VOL I: National Screening Program City of Manningham Whittlesea PND Interest Group Werribee Mercy Hospital Angliss Hospital Northern Hospital Western, Westgate and South-West Divisions of General Practice August 2002 September 2002 September 2002 October 2002 October 2002 October 2002 Angliss Hospital November 2002 City of Whitehorse Rotary Club of Whittlesea, Whittlesea Angliss Hospital Angliss Hospital Angliss Hospital December 2002 December 2002 December 2002 December 2002 February 2003 Obstetric Audit at the Northern Hospital Warrnambool PND forum Wyndham MCHN Angliss Hospital Boroondara MCHN Eastern Regional Meeting of MCHN co-ordinators Radio National Greater Shepparton Postnatal and Antenatal Depression Forum GPDV Rotary Club of Ivanhoe, Ivanhoe Division of General Practice Victoria Primary Mental Health Forum Australian Association of Infant Mental Health. February 2003 February 2003 March 2003 March 2003 March 2003 March 2003 April 2003 May 2003 June 2003 June 2003 June 2003 September 2003 beyondblue National PND Program Final Report Research and clinical findings. PND and beyondbabyblues launch Beyondblue National Postnatal Depression Program Information session on NPDP to new mothers group Presentation to clinic about NPNDP Invited speaker - Postnatal Depression Information session on NPDP Information session on NPDP Display and posters about NPDP VOL I: National Screening Program Victorian Branch Meeting Bowen Centre, Hawthorn South West Health Program Launch Hamilton City of Kingston University Psychology Clinic East Hawthorn Playgroup Barwon South West Regional Midwives Forum MCHN 24 hour crisis telephone service Melbourne University Research and Innovation Fair Austin Health GP liaison Officer meeting Northern Hospital GPDV Mental Health Reference Group La Trobe University Rotary Club Glen Eira, Glen Eira Royal Children’s Hospital November 2003 November 2003 February 2004 February 2004 March 2004 March 2004 March 2004 May 2004 Information session on NPDP Study Day presentation to health professionals and consumers Information session on NPDP Invited speaker - Postnatal Depression Invited speaker - Postnatal Depression Seminar for Graduate Diploma in Mental Health Sciences,– Attachment Theory and Research Invited speaker - Antenatal Support following Depression – Enhancing the Grand Round, Austin & Repatriation Medical parent-infant relationship. (Victorian component of the beyondblue National Centre, Heidelberg Project The National Postnatal Depression Program – prevention and early intervention) Antenatal Support Following Depression. The National Postnatal Depression Research Week Austin Health Program in Victoria and Tasmania June 2004 July 2004 July 2004 August 2004 August 2004 August 2004 Screening for postnatal depression in routine primary care: Properties of the Edinburgh Postnatal Depression Scale Models of Care: Evaluating a best practice model for treating postnatal depression Research Week Austin Health October 2004 Research Week Austin Health October 2004 Page 93 of 108 August 2004 October 2004 beyondblue National PND Program Final Report South Australia beyondblue National PND Program beyondblue National PND Program New South Wales PND and beyondblue Interview for Body & Soul Information on beyondblue activities at RHW PND and beyondblue PND and beyondblue PND and beyondblue PND and beyondblue PND and beyondblue -linking NESB women to mental health Services Perinatal Depression and BB PND Program PND and beyondblue PND and beyondblue PND and beyondblue Parents with Mental Illness - Breaking the Cycle beyondblue - National Postnatal Depression Program Antenatal screening, what are the benefit and risks? beyondblue beyondblue beyondblue beyondblue beyondblue beyondblue Page 94 of 108 National Postnatal Depression Program National Postnatal Depression Program National Postnatal Depression Program National Postnatal Depression Program National Postnatal Depression Program National Postnatal Depression Program VOL I: National Screening Program Grand Round, Flinders Medical Centre, Adelaide. Grand Round, Women’s and Children’s Hospital, Adelaide. August 2001 September 2001 Malcolm Elliot 2UE Radio Channel 9 GP Forum Interviewed on Radio National “Life Matters” Donna Maria RHW Perinatal Mental Health Review Regional Obstetric Social Workers meeting held at RHW Multicultural Womens Group September 2002 September 2002 November 2002 November 2002 November 2002 November 2002 February 2003 Statewide GP day at UNSW on Women’s Health Train the Trainer workshop. SESAHS GP Day Breaking the Cycle: Early Intervention in Infancy: Transforming the Next Generation (Launch of Area Health Policy) You, Me and attachment conference. Early Agendas – Issues in Infant and Maternal Mental Health (Royal Australian and New Zealand College of Psychiatrists) (I Hickie, Keynote Speaker) Karitane Open day Perinatal and Infant services networking forum beyondblue partnership lunch Arabic Radio Western Community Radio – Arabic (2M FM) 2000 FM (Assyrian Radio) February 2003 February 2004 February 2004 April 2004 April 2004 August 2004 August 2004 June 2004 June 2004 August 2004 May 2003 June 2003 July 2003 beyondblue National PND Program Final Report beyondblue - National Postnatal Depression Program beyondblue - National Postnatal Depression Program beyondblue - National Postnatal Depression Program beyondblue - National Postnatal Depression Program Page 95 of 108 VOL I: National Screening Program SBS Vietnamese Radio Obstetric and Gynaecological health Professionals, RNS Midwifery Parent Educators, Lower North Shore Area Lower North Shore Clinical Research Support and PND Interest Group March 2003 March 2003 February 2003 March 2003 beyondblue National PND Program Final Report VOL I: National Screening Program Newspaper and Magazine Articles Headline/Title National Office WA Uni aims to prevent postnatal depression Screening for new mothers National focus on birth depression Plans to erase mothers’ fear New plan to fight post-natal blues New study to focus on postnatal depression beyondblue program launched The National Postnatal Depression Program beyondblue Postnatal Depression Program launched Test tackles birth blues Sad Lullabies Postnatal blues Program soon to bear fruit GP s offered PND courses When motherhood brings you down New aid for postnatally depressed Postnatal Depression in the Far North Largest study into baby blues begins Quizzing mothers-to-be helping to fight the baby blues Dads, Dummies and Demons Postnatal depression test okay before birth Help for depressed mums Beating the baby blues Page 96 of 108 Source ABC News Online The Age The Heidelberger Herald Sun Progress Press Peoplefocus Obstetrics & Gynaecology Forward Together. Quarterly Bulletin of the National Secretariat of National Council of Women of Australia Women’s Health in Focus Sunday Herald-Sun Who Magazine Medical Observer Medical Observer Colesbaby magazine Sunday Age Dona Maria Pre & Postnatal Support Network – Network News ninemsn website The Age Sunday Life Medical Observer Letters to the Editor, Herald-Sun Newspaper Herald-Sun Newspaper Date September 2001 September 2001 September 2001 September 2001 October 2001 October 2001 3(4): December 2001 December 2001 December 2001 December 2001 April 2002 May 2002 May 2002 Autumn Edition 2002 July 2002 Winter 2002 August 2002 August 2002 August 2002 November 2002 December 2002 March 2003 beyondblue National PND Program Final Report Consider SSRI does before giving birth, expert says Wife suicidal before killings National Postnatal Depression Program by 'beyondblue' Maternal depression – does it matter to the kids Down but not out Baby blues Fall from Grace Swimmer dives into the blues of birth, death and postnatal despair Fatal does of the blues The sharp edge of postnatal depression Program to help mothers New mums on the edge Beyond a mother’s control The birth of the blues Depression test urged Screen for antenatal depression: expert Queensland Pregnancy help Raising the profile of baby blues Beyond the baby blues Mum study to uncover baby blues Book for post-natal depression screening NQ Post-Natal Distress Support Group: Information Booklet Emotional health during pregnancy Emotional health during pregnancy Page 97 of 108 VOL I: National Screening Program Medical Observer Weekly The Age Synergy the newsletter of Multicultural Mental Health Australia Every Child Coles baby magazine Sydney Morning Herald on-line New Idea The Age Herald Sun Vicdoc Heidelberg leader New Idea The Age Good Weekend Herald Sun Medical Observer Weekly Townsville Bulletin Outlook – JCU Bulletin Rural Nurse Cairns Post The North West Star NQ Post-Natal Distress Support Group: For Families, By Families, With Families. Information Booklet Launch The Australian Psychological Society Ltd: Queensland State Newsletter Queensland state newsletter February 2004 February 2004 No 2, 2004 10(4): Spring 2004 Spring 2004 March 2004 August 2004 September 2004 September 2004 October 2004 October 2004 November 2004 December 2004 February 2005 March 2005 March 2005 October 2001 November 2001 November 2001 August 2002 July 2004 September 2004 October 2004 November 2004 beyondblue National PND Program Final Report Western Australia Postnatal depression studied Helping mums beat the blues Raising Awareness of PND Abuse link to baby blues Abuse linked to baby blues Childhood abuse a factor in motherhood depression Postnatal study New light shed on depression The beyondblue National Postnatal Depression Project for Families with Multiple Birth Children The beyondblue National Postnatal Depression Project for Families with Multiple Birth Children Progress of the beyondblue National Postnatal Depression Program Depression During Pregnancy & Early Parenthood The beyondblue National Postnatal Depression Project for Families with Multiple Birth Children Depression During Pregnancy & Early Parenthood beyondblue the National Depression Initiative Stress Stress Information Booklet Advertisement Ante and Postnatal Depression: Risk Factors, Symptoms and What Can I Do? Depression During Pregnancy and Early Parenthood Page 98 of 108 VOL I: National Screening Program The West Australian, Newspaper Article Sunday Times Newspaper, Feature Article Radio Fremantle, On-air Interview The West Australian, Newspaper Article Herald Sun, Newspaper Article Avon Valley Advocate, Newspaper Article Guardian Express, Newspaper Article Wanneroo Times, Newspaper Article Australian Multiple Birth Association National Journal/Magazine, Article Australian Multiple Birth Association Local Club Newsletters – Nationally, Article x 68 Postnatal Depression Professionals Association Newsletter Australian Multiple Birth Association National Journal/Magazine, Article Perth & Districts Multiple Birth Association Newsletter, Article Australian Multiple Birth Association Local Club Newsletters – Nationally, Article x 68 Women & Infants Research Foundation, Teenage Parents Festival Australian Multiple Birth Association National Journal/Magazine, Article Australian Multiple Birth Association Local Club Newsletters – Nationally, Article x 68 Premiepress: The Psychology of Infancy, Advertisement for Information Booklets Twin Talk – Northern Territory Multiple Birth Club Newsletter Twin Talk – Northern Territory Multiple Birth Club Newsletter August 2002 October 2002 December 2003 December 2003 December 2003 December 2003 December 2003 January 2004 Issue 31, Vol 9 May 2004 June 2004 July 2004 Issue 32, Vol 10 July 2004 July 2004 August 2004 September 2004 September 2004 October 2004 Vol 5(4), December 2004 March 2005 April 2005 beyondblue National PND Program Final Report Results of the beyondblue National Postnatal Depression Project for Families with Multiple Birth Children Australian Capital Territory Postnatal Depression to go under national spotlight Launch of ACT component of National beyondblue Postnatal Depression Program beyondblue Postnatal Depression Launch Victoria Study of birth and the blues Baby blues plan a first Quizzing mothers to be helping to fight the babyblues Survey to life the spirits of mums Postnatal Depression Research The beyondblue National Postnatal Depression Program Depression after giving birth strikes 1 in 10 Trust in yourself South Australia Launch of South Australian postnatal depression initiative South Australian postnatal depression program launched in Adelaide Partners enlisted in the fight against postnatal depression Tracking the signs of postnatal depression One in five new mums who can’t beat depression. Fathers help beat the blues Baby blues can hit before birth Pregnancy depression ignored and untreated Beyondblue Opening our eyes to depression in Murray Bridge Page 99 of 108 VOL I: National Screening Program Australian Multiple Birth Association, State (WA) Committee AGM May 2005 The Canberra Times The Canberra Chronicle April 2004 April 2004 Division Action: Monthly Newsletter for the ACT Division of General Practice April 2004 The Werribee Times The Werribee Banner The Age Northern Hospital Newsletter Mercy Health News Division of GPs newsletter – Northern, North East Valley, North West Melbourne, Westgate, Western Knox, Eastern Ranges and Whitehorse The Age Mother & Baby August 2002 August 2002 August 2002 October 2002 November 2002 March/April 2003 The Advertiser The Advertiser Flinders Journal, Flinders University, V12:18 The Advertiser The Advertiser The Advertiser The Advertiser The Advertiser Public Forum, The Age September 2001 October 2001 November 2001 February 2001 June 2003 August 2004 September 2004 February 2005 February 2005 January 2004 June/July 2004 beyondblue National PND Program Final Report New South Wales Child & Adolescent Psychiatry, RNSH 'beyondblue' at Royal North Shore Hospital Depression drive is banishing the blues 'beyondblue' the National PND Program Beating the baby blues, step by step 'beyondblue' at Royal North Shore Support is the key to beating baby blues beyondblue National Postnatal Depression Program Beyond the baby blues: program offers new hope Depressed new mothers reluctant to seek help Screening program raises awareness Baby blues beyondblue National Postnatal Depression Program beyondblue National Postnatal Depression Program 'beyond the baby blues for RNSH and Ryde mums' Marie-Paule Austin and beyondblue The Birth of the baby blues 'beyondblue' at Northern Sydney Health Page 100 of 108 VOL I: National Screening Program Northern Sydney CAMHS news Northern Sydney Child & Adolescent Mental Health Service News Liverpool Champion (Community Newspaper) Northern Sydney Div of General Practitioners Newsletter Sydney Morning Herald RNS News Sydney Morning Herald SWSAHS Division of GPs newsletter Sydney Morning Herald Sydney Morning Herald Sydney Morning Herald Sydney Morning Herald The Future Arabic Newspaper El Telegraph Arabic Newspaper Royal North Shore & Ryde News Sunday Telegraph Sydney Morning Herald HKR Div of General Practice Newsletter December 2002 February 2003 March 2003 March 2003 May 2003 May 2003 August 2003 October 2003 December 2003 December 2003 March 2004 March 2004 March 2004 March 2004 July 2004 November 2004 February 2005 August 2004 beyondblue National PND Program Final Report VOL I: National Screening Program Appendix E – Detailed list of Conference Presentations and Scientific Articles Conference Presentations Conference National Office The Australia Society for Psychiatric Research Annual Scientific Meeting 10th Annual National Conference, Royal College of Nursing, Australia. Darling Harbour, Sydney. Marce Society International Biennial Scientific Meeting, Sydney, NSW Marce Society International Biennial Scientific Meeting, Sydney, NSW The 27th Congress of the World Federation for Mental Health. Melbourne 3rd General Practice Divisions of Vic Conference. Melbourne Vic. Presentation Title Authors Format Date The National Postnatal Depression Program The National Postnatal Depression Program – Reaching out to women in pregnancy and postpartum period The National Postnatal Depression Program To Screen or Not to Screen for Perinatal Depression? – That is the Question… Screening for Postnatal Depression Buist, A.E & Bilszta, J.L.C. Poster Buist, A.E (Keynote Speaker) Oral December 2001 February 2002 Buist, A.E & Bilszta, J.L.C. Poster Buist, A.E., Milgrom, J., Condon, J., Boyce, P., Austin, M-P., Ellwood, D., Hayes, B., and Pope, S. Buist, A.E Oral Oral February 2003 Ericksen, J., Bilszta, J.L.C., Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Poster April 2003 Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Oral July 2003 Ericksen, J., Bilszta, J.L.C., Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Poster July 2003 Buist, A.E., Oral October 2003 The National Postnatal Depression Program – Enhancing the Quality of GP & Perinatal Service Partnerships Joint AAIMH/Marce Society The National Postnatal Depression Conference. Building Better Beginnings. Program: National Baseline Adelaide Survey Joint Australian Association for Infant The National Postnatal Depression Mental Health/Marce Society Program – Enhancing the Quality Conference of GP & Perinatal Service Partnerships Harplands Hospital, Stoke-On-Trent, The Australian National Postnatal England. Depression Program: results of the Page 101 of 108 September 2002 September 2002 beyondblue National PND Program Final Report World Association of Infant Mental Health 9th World Conference. World Association of Infant Mental Health 9th World Conference. 2nd International Women’s Mental Health. Washington. USA Postpartle Depression: Muttergluck gluckliche Mutter Vienna, Austria Marce Society International Biennial Scientific Meeting, Oxford, UK Marce Society International Biennial Scientific Meeting, Oxford, UK RANZCP 40th Annual Congress. Sydney. Postpartum International. San Jose, California, USA VOL I: National Screening Program baseline survey of public and professional knowledge of postnatal depression. The National Postnatal Depression Program - Enhancing the quality of GP & perinatal service partnerships The National Postnatal Depression Program The Australian National Postnatal Depression Program Implementation of a National Perinatal Mental Health Screening Program: The beyondblue National Postnatal Depression Program The Australian National Postnatal Depression Program Screening for perinatal depression using the Edinburgh Postnatal Depression Scale – Experiences of the beyondblue National Postnatal Depression Program The Mental Health of Women Giving Birth in Australia 2002-4. The beyondblue National Postnatal Depression Program The Mental Health of Australians – Results of the beyondblue Australian PND Program Barriers to prevention – the findings of the beyondblue Page 102 of 108 Ericksen, J., Bilszta, J.L.C., Buist, A.E., Milgrom, J., Barnett, B., Condon, J., Hayes, B., & Pope, S Poster January 2004 Buist, A.E., & Bilszta, J.L.C Poster Buist, A.E., Oral January 2004 March 2004 Bilszta, J.L.C Oral May 2004 Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Ericksen, J., Bilszta, J.L.C., Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Oral September 2004 September 2004 Buist, A.E., Barnett, B., Condon, J., Austin, M-P., Kowalenko, N., Milgrom, J., Hayes, B., and Brooks, J. Oral May 2005 Buist, A.E. (Keynote Speaker) Oral June 2005 Buist, A.E., Barnett, B., Condon, J., Austin, M-P., Kowalenko, N., Milgrom, Oral June 2005 Oral beyondblue National PND Program Final Report VOL I: National Screening Program Australian PND Program Australian Capital Territory Therapies that work Conference. 28th June 2004 Burgmann College ANU Counselling Centre, Canberra The 2004 twilight seminar Western Australia Perinatal Society of Australia & New Zealand, Hobart Australian Multiple Birth Association WA Annual State Conference, Bunbury Joint Australian Association for Infant Mental Health/Marce Society Conference, Adelaide Telethon Institute for Child Health Research Australian Twin Registry Conference, Perth International Marce Society Conference, Oxford King Edward Memorial Hospital Stars Symposium/Conference, Perth Australian Multiple Birth Association National Conference, Brisbane Page 103 of 108 J., Hayes, B., and Brooks, J The National Postnatal Depression Reay Rebecca Program: What works for Postnatal Depression? ‘Beyondblue Tales’- the Reay, Rebecca experience of women in the beyondblue program Oral June 2004 Oral November 2004 ‘This Isn’t What we Expected’: the Impact of Reality in the Transition to Parenthood The beyondblue National Postnatal Depression Project for Families of Multiple Birth Children A Preliminary Analysis of the First 500 Women in the West Australian beyondblue Cohort The beyondblue National Postnatal Depression Project for Families of Multiple Birth Children The beyondblue National Postnatal Depression Project for Families of Multiple Birth Children Depressive Symptoms during the Perinatal Period in Women who Deliver at King Edward Memorial Hospital: Preliminary Results of the National beyondblue Program The beyondblue National Postnatal Depression Project for Pope, S. Oral March 2004 Brooks, J. Oral May 2004 Pope, S., & Brooks, J. Poster July 2004 Brooks, J. Oral August 2004 Brooks, J. Poster September 2004 Brooks, J. Oral September 2004 Brooks, J. Oral October 2004 beyondblue National PND Program Final Report VOL I: National Screening Program Families of Multiple Birth Children Scheduled… 14th Biennial Australasian Human Development Conference, Perth 14th Biennial Australasian Human Development Conference, Perth Australian Multiple Birth Association National Conference, Hobart Queensland Australian College of Midwives Australian College of Midwives, Inc. Invited keynote address – Annual State Conference Townsville Health District: Women’s Health Exposition. Australasian Marce Conference Australasian Marce Conference Page 104 of 108 Results of the Western Australian Cohort of the beyondblue National Postnatal Depression Program Emotional Health for Families with Multiple Birth Children Results of the beyondblue National Postnatal Depression Project for Families of Multiple Birth Children Brooks, J., Doherty, D., & Speelman, C. Poster July 2005 Brooks, J., Doherty, D., & Speelman, C. Poster July 2005 Brooks, J. Oral October 2005 Keynote address: The beyondblue National Postnatal Depression Program Birthing in the tropics: Women and midwives seeking wisdom in childbearing Women’s Health Exposition: A celebration of womanhood. Hayes, B.A. Oral July 2004 Hayes, B.A. (Keynote speaker) Oral July 2004 Hayes, B.A. Queensland: Regional and Rural Dimensions Impacting on the Emotional Health of Childbearing Women Queensland: Postal Antenatal and Postnatal Screening of Regional and Rural Women in the beyondblue National Postnatal Depression Project – A Buckby, B., Hayes, B.A., McCulley, J. Invited March introductory 2005 & summary speaker & chair Poster Sept 2005 Hayes, B.A., McCulley, J., Buckby, B. Poster Sept 2005 beyondblue National PND Program Final Report Australasian Marce Conference New South Wales Rural Mental Health Conference beyondblue - National Postnatal Depression Program Early Agendas – Issues in Infant and Maternal Mental Health (Royal Australian and New Zealand College of Psychiatrists) RANZCP 40th Annual Congress. Sydney. South Australia Australasian Midwifery Expo 2004: Voices Coming Together Australasian Midwifery Expo 2004: Voices Coming Together Victoria Gippsland Psychology Conference, Morwell Jocelyn Wale Seminar, James Cook University, Townsville, Qld. 1st National Conference for “Meeting the Challenges for Children & Families where Parents have a Mental Illness” Page 105 of 108 VOL I: National Screening Program demonstration of Ethical and Clinical Competence beyondblue: Working in partnership with Aboriginal Women and Health Care Workers towards culturally sensitive outcomes for childbearing Indigenous Women at three sites in Queensland Hayes, B.A., Geia, L., Egan, M. Oral Sept 2005 A Lifespan Approach: Setting the Foundation for Early Intervention in Infancy You, Me and Attachment Conference Assessment and early intervention in the antenatal and postnatal period. Kowalenko, N. (keynote speaker) Oral March 2004 SWSAHS staff Poster June 2004 Barnett, B.E.W Oral August 2004 Invited Symposium: Perinatal & Infant Mental Health Symposium Kowalenko, N., Buist AE., Powrie, R. Symposium May 2005 Beyondblue National Postnatal Depression Program Fathers Wellbeing after childbirth Condon, J. Paper Gamble, E. Paper August 2004 August 2004 Milgrom, J. Invited speaker Keynote Mothers, Babies and Postnatal Depression Treating Postnatal DepressionMothers, Infants, and Fathers. “Is it enough to use Depression Improvement as an Outcome Measure with Postnatal Milgrom, J. Milgrom, J., Ericksen, J., DePaola, C., McCarthy, R., & Loughlin, E. Paper October 2001 November 2001 May 2002 beyondblue National PND Program Final Report Melbourne Marce Society Conference International Biennial Scientific Meeting. Sydney Marce Society Conference International Biennial Scientific Meeting Sydney International Congress Of Applied Psychology Symposia XXV 3rd General Practice Divisions Victoria Conference, The Thing about Quality: How and Why? VOL I: National Screening Program Depression Treatment? The Parent-Infant Interaction” A Workshop on intervention following postnatal depression targeting both maternal mood and the mother-infant interaction. Postnatal Depression and Child Development-is the early motherinfant interaction a mediating factor? Treating Postnatal Depression The National Postnatal Depression Program – Enhancing the Quality of GP & Perinatal Service Partnerships Australian Rotary Research Fund Asking Different Questions: A Symposium Canberra. Clinician’s Perspective Joint Australian Association for Infant The National Postnatal Depression Mental Health/Marce Society Program – Enhancing the Quality Conference. Building Better Beginnings. of GP & Perinatal Service Partnerships Annual Women’s Health East The National Postnatal Depression Conference, Moving in from the Program – Enhancing the Quality margins, hope and strategies for of GP & Perinatal Service improving women’s emotional health Partnerships Joint Australian Association for Infant The National Postnatal Depression Mental Health/Marce Society Program: National Baseline Conference Survey Joint Marce Society and Australian Dysfunctional Parent-Infant Association for Infant Mental Health. Relationships following Building Better Beginnings. Depression: An intervention Study th 17 World Congress on Psychosomatic A Randomised Trial of Medicine. Psychological Treatments For Page 106 of 108 Milgrom, J. Ericksen, J., Loughlin, E., Martin, P.R., Negri, L.M., & McCarthy, R.M. Workshop September 2002 Milgrom, J., Ericksen, J., & Westley, D.T. Plenary Session September 2002 Milgrom, J.M. Symposia Ericksen, J., Bilszta, J.L.C., Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Poster November 2002 April 2003 Milgrom, J. Keynote May 2003 Ericksen, J., Bilszta, J.L.C., Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Poster July 2003 Ericksen, J., Bilszta, J.L.C., Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Poster July 2003 Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Oral July 2003 Milgrom, J., Neilson, K., Loughlin, E.E, McCarthy, R., & Ericksen, J. Oral July 2003 Milgrom, J., Martin, P.R., & Negri, L.M. Oral September 2003 beyondblue National PND Program Final Report World Association Of Infant Mental Health Melbourne World Association of Infant Mental Health 9th World Conference. “The Baby’s Place in the World” Annual Scientific Meeting of the Fertility Society of Australia. Adelaide Page 107 of 108 VOL I: National Screening Program Postnatal Depression In Australia The National Postnatal Depression Program – Enhancing the Quality of GP & Perinatal Service Partnerships Toward Parenthood an Antenatal Preparation For Parenthood Program Changing Behaviour to Promote Health and Well-being Ericksen, J., Bilszta, J.L.C., Buist, A.E., Milgrom, J., Barnett, J., Hayes, B., and Pope, S. Poster January 2004 Milgrom,J., McCarthy,R., Saunders,B., Ericksen,J., Romeo,Y., Loughlin,E., Newnham,C. Milgrom, J. (Keynote speaker) Paper January 2004 Oral November 2004 beyondblue National PND Program Final Report VOL I: National Screening Program Scientific Articles Article Title To screen or not to screen – that is the question in perinatal depression Can we prevent chronic mental illness? Authors Buist A, Barnett B, Milgrom J, Pope S, Condon J, Ellwood D, Boyce PM, Austin M-P and Hayes B Druitt, S Postnatal Depression: A guide for GPs Ross J& Baynes A The National Postnatal Depression Program - Enhancing the quality of GP & perinatal service partnerships Recognition and Management of Perinatal Depression in General Practice: Results of an Australian National Survey Ericksen J, Bilszta JLC, Buist AE, Milgrom J, Barnett B, Condon J, Hayes B, & Pope S. Buist A, Bilszta J, Barnett B, Milgrom J, Ericksen J, Condon J, Hayes B, Brooks, J. Health Professional’s Knowledge and Awareness of Perinatal Depression: Results of a National Survey Buist A, Bilszta J, Milgrom J, Barnett B, Hayes B, Austin MP. Page 108 of 108 Journal The Medical Journal of Australia Year 2002 Reference 177 7 Oct., No7: S101-S105 Healthlink: The Health Promotion Journal of the ACT Region. Division Action: Monthly Newsletter for the ACT Division of General Practice Infant Mental Health Journal 2004 Winter 2004 16-17. 2004 Vol 102. April 2004 6-7. 2004 24 (Suppl 6A): 357. Australian Family Physician 2005 Accepted Journal of Psychosomatic Obstetrics & 2005 Gynaecology Submitted