Smoking cessation clinical pathway
advertisement
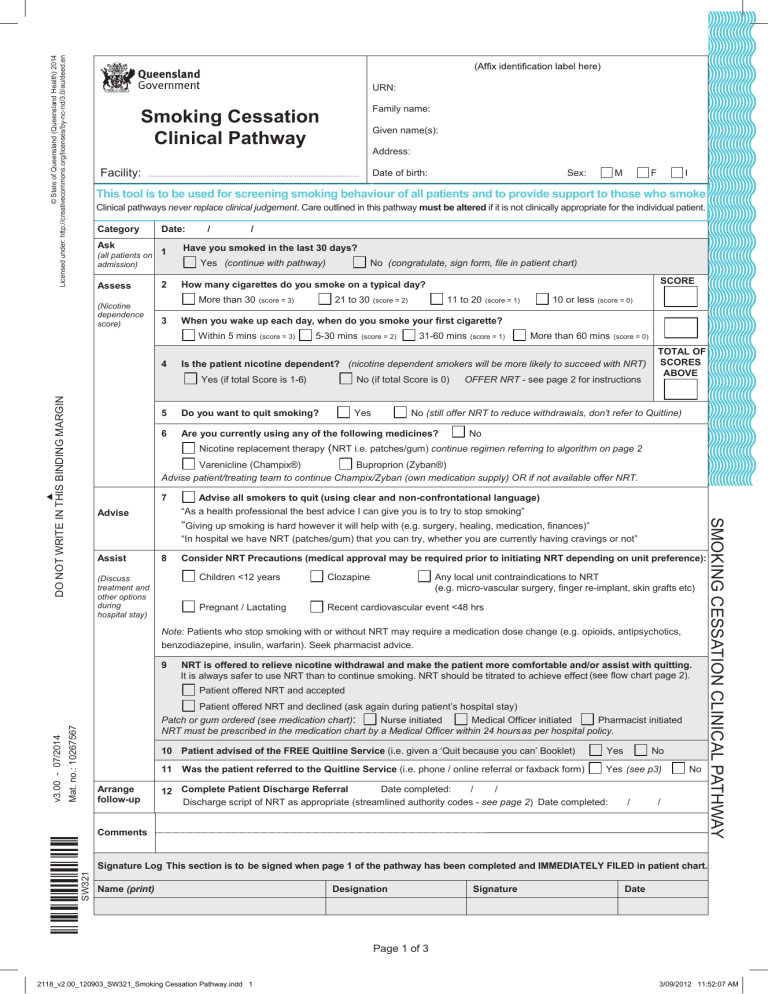
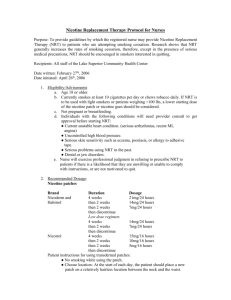
© State of Queensland (Queensland Health) 2014 Licensed under: http://creativecommons.org/licenses/by-nc-nd/3.0/au/deed.en URN: Family name: Smoking Cessation Clinical Pathway Given name(s): Address: Facility: Date of birth: ......................................................................................................... Sex: M F I This tool is to be used for screening smoking behaviour of all patients and to provide support to those who smoke Clinical pathways never replace clinical judgement. Care outlined in this pathway must be altered if it is not clinically appropriate for the individual patient. Category Ask (all patients on admission) Assess (Nicotine dependence score) Date: 1 / / Have you smoked in the last 30 days? Yes (continue with pathway) 2 21 to 30 (score = 3) (score = 3) 5-30 mins 10 or less (score = 1) (score = 0) 31-60 mins (score = 2) (score = 1) More than 60 mins (score = 0) Is the patient nicotine dependent? (nicotine dependent smokers will be more likely to succeed with NRT) Yes (if total Score is 1-6) DO NOT WRITE IN THIS BINDING MARGIN 11 to 20 (score = 2) When you wake up each day, when do you smoke your first cigarette? Within 5 mins 4 SCORE How many cigarettes do you smoke on a typical day? More than 30 3 No (congratulate, sign form, file in patient chart) No (if total Score is 0) 5 Do you want to quit smoking? Yes 6 Are you currently using any of the following medicines? OFFER NRT - see page 2 for instructions TOTAL OF SCORES ABOVE No (still offer NRT to reduce withdrawals, don’t refer to Quitline) No Nicotine replacement therapy (NRT i.e. patches/gum) continue regimen referring to algorithm on page 2 Varenicline (Champix®) Buproprion (Zyban®) Advise patient/treating team to continue Champix/Zyban (own medication supply) OR if not available offer NRT. 7 Advise all smokers to quit (using clear and non-confrontational language) “As a health professional the best advice I can give you is to try to stop smoking” “Giving up smoking is hard however it will help with (e.g. surgery, healing, medication, finances)” “In hospital we have NRT (patches/gum) that you can try, whether you are currently having cravings or not” Assist 8 (Discuss treatment and other options during hospital stay) Consider NRT Precautions (medical approval may be required prior to initiating NRT depending on unit preference): Children <12 years Clozapine Pregnant / Lactating Recent cardiovascular event <48 hrs Any local unit contraindications to NRT (e.g. micro-vascular surgery, finger re-implant, skin grafts etc) Note: Patients who stop smoking with or without NRT may require a medication dose change (e.g. opioids, antipsychotics, benzodiazepine, insulin, warfarin). Seek pharmacist advice. 9 NRT is offered to relieve nicotine withdrawal and make the patient more comfortable and/or assist with quitting. It is always safer to use NRT than to continue smoking. NRT should be titrated to achieve effect (see flow chart page 2). Mat. no.: 10267567 Patient offered NRT and declined (ask again during patient’s hospital stay) Nurse initiated Medical Officer initiated Pharmacist initiated Patch or gum ordered (see medication chart): NRT must be prescribed in the medication chart by a Medical Officer within 24 hours as per hospital policy. Arrange follow-up SW321 ÌSW321cÎ v3.00 - 07/2014 Patient offered NRT and accepted 10 Patient advised of the FREE Quitline Service (i.e. given a ‘Quit because you can’ Booklet) Yes 11 Yes (see p3) Was the patient referred to the Quitline Service (i.e. phone / online referral or faxback form) Date completed: / / 12 Complete Patient Discharge Referral Discharge script of NRT as appropriate (streamlined authority codes - see page 2) Date completed: No / No / Comments SMOKING CESSATION CLINICAL PATHWAY Advise Signature Log This section is to be signed when page 1 of the pathway has been completed and IMMEDIATELY FILED in patient chart. Name (print) Designation Signature Date Page 1 of 3 2118_v2.00_120903_SW321_Smoking Cessation Pathway.indd 1 3/09/2012 11:52:07 AM URN: Smoking Cessation Clinical Pathway Family name: Given name(s): Address: Date of birth: Sex: M F I THIS PATIENT IS ON THE SMOKING CESSATION CLINICAL PATHWAY. Page 1 of this pathway can be found in the patient chart. Combination NRT Algorithm Commence 1 x 21mg nicotine transdermal patch every 24 hours CEASED SMOKING CONTINUES TO SMOKE Eliminates both smoking and cravings to smoke / symptoms of nicotine withdrawal Reduces smoking but needs extra NRT Add 4mg nicotine gum for continued smoking/cravings If smoking persists and using >10 pieces NRT gum, add a second patch Continue 1 x 21mg nicotine patch for 8 -12 weeks from last cigarette. FOR PRECAUTIONS - See page 1 / product information (adapted from Bittoun, Combination Therapy in the Hard to Treat, JSC, 1:1, 2006) DIRECTIONS ON USE OF NICOTINE REPLACEMENT THERAPY (NRT) • The evidence shows that NRT helps people to quit smoking, doubling long-term success rates. Combination therapy (patch plus gum) is effective for those experiencing significant withdrawal and increases the chances of long term abstinence (Cochrane review 2012). • NRT provides lower nicotine levels than smoking, relief from physiological withdrawal symptoms and does not produce strong dependence. • Most NRT products are available for sale over the counter (non-prescription) and are classified as low risk medications. • Seek medical advice for information on buproprian Hcl (Zyban®), or varenicline (Champix®). Instructions NICOTINE TRANSDERMAL PATCHES 21mg/24hr 1. Apply to clear, dry, non-hairy area of chest, back, upper arm or hip and secure with medicinal tape if required. 2. DO NOT apply to freshly shaven, broken or inflamed skin (can cause irritation). 3. Rotate site daily. 4. Wait at least one hour after adhesion before bathing or showering with the patch. Considerations • Mild patch irritation can be treated by using a steroid cream e.g. 0.02% betamethasone or 1% hydrocortisone. If patient experiences an allergic reaction to the adhesive, cease patches and use 4mg gum. • Apply patch last thing before sleep to allow slow release of nicotine overnight - likelihood of first cigarette of the day “craving” is strongly diminished. • Sleep disturbances including imsomnia and vivid dreams may occur. Patch can be removed at night. NICOTINE ORAL GUM (4mg max 12 pieces per day) Instructions 1. Chew one piece slowly until the taste becomes strong. 2. Rest between your gum and cheek to allow absorption of nicotine into the bloodstream. 3. When taste has faded, chew and park again - repeat for 30 mins. 4. Do not swallow excessively (stomach doesn’t absorb nicotine). 5. Use a fresh piece of gum after about an hour. Considerations • Some people may not like the ‘peppery’ taste. • Amount of time needed in mouth (30 mins out of every hour). • May not be suitable if wearing dentures. • Recommended for use if: pregnant, allergic to patches or as combination therapy. Discharge authority scripting • NRT patches (Nicorette®, Nicabate® and Nicotinell®) are available at a cheaper price on prescription through the Pharmaceutical Benefits Scheme (12 weeks per year). 28 x 2 repeats. • Streamlined authority codes: 4344 Aboriginal and Torres Strait Islander, 4348 in a counselling program, 4307 entering in a program. • See pbs.org.au for more details. PROFESSIONAL DEVELOPMENT AND FURTHER INFORMATION The Statewide Respiratory Clinical Network has information to assist clinicians around nicotine addiction and smoking cessation on the Clinical Access and Redesign Unit QHEPS intranet page: http://www.health.qld.gov.au/caru/networks/respiratory.asp#clinician Dispelling the Myths about NRT Video (11 minutes) http://www.health.qld.gov.au/caru/networks/respiratory.asp#clinician Online Brief Intervention Training (general or maternity and child health version) http://www.sdc.qld.edu.au/elearning The Quitline is available to support and provide information to clinicians on assessing nicotine dependence, pharmacotherapy, behaviour change techniques and on how to approach a conversation with someone about their smoking. You can call 13QUIT (7848) between 7am and 10pm, 7 days to ask questions and get support. . Page 2 of 3 DO NOT WRITE IN THIS BINDING MARGIN Continue for 2 weeks and then try reducing added NRT URN: Family name: Smoking Cessation Clinical Pathway Facility: Given name(s): Address: ......................................................................................................... Date of birth: Sex: M F I REFERRAL TO QUITLINE The Quitline (13 7848) is a FREE telephone counselling service to assist Queenslanders to quit smoking. Encourage a future quit attempt; advise your patient “The best thing you can do for your health is to stop smoking. When you’re ready, phone Quitline 13 QUIT (7848), or talk to your doctor or pharmacist”. Clinicians can refer patients to the service by: 1. Completing this form and fax / email to Quitline. Fax: 3259 8217. Email: 13QUIT@health.qld.gov.au 2. Online and faxback referral forms: http://www.health.qld.gov.au/quitsmoking/health_pro_referral.asp Quit because you can booklets are available in bulk for your service by contacting Quitline 13 QUIT on 13 7848. DO NOT WRITE IN THIS BINDING MARGIN Referring Health Professional name: ................................................................................................................................................................... Profession: General practitioner Dentist Pharmacist Nurse Mental health worker Aboriginal health worker Other (please specify) ………………………………………………………………………… Is the patient of Aboriginal or Torres Strait Islander origin? No Yes, Aboriginal Yes, Torres Strait Islander Yes, Aboriginal AND Torres Strait Islander Would the patient like to speak with a Quitline Aboriginal and/or Torres Strait Islander staff member: Yes No What is the best time and day for Quitline to call the patient? Ask whether the patient wants to be contacted as an inpatient or when Inpatient they leave hospital. Outpatient: expected discharge date / / Monday Tuesday Wednesday Thursday Friday 7am-9am 9am-12pm 12pm-5pm 5pm-8.30pm 8.30pm-10pm Saturday Sunday If patient does not want Quitline to leave a message, please indicate here Patient Email: ......................................................................................................Preferred phone: ..................................................................................... GP FOLLOW UP 1. This page can be given to the patient on discharge to take to their GP to complete the GP referral. 2. If patient referred to Quitline and GP details provided on this form, Quitline will notify patient’s GP of contact. 3. Document smoking status, treatment and referrals in discharge summary. GP name: ............................................................................................................................................................................................................... GP Practice: ................................................................................................................................................................................................................. Suburb: .................................................................................................................................................................................................................. HEALTH PROFESSIONAL CONSENT I confirm that this patient/client consents to receiving a call from the Quitline. _______________________________ Health Professional Signature / Date / Privacy Warning: The information contained in this fax/email message is intended for a patients’s GP / Quitline Staff only. If you are not the intended recipient you must not copy, distribute, take any action reliant on, or disclose ant details of the information in this fax/email to any other person or organisation. Page 3 of 3