A blood-mimicking fluid for particle image velocimetry with silicone
advertisement

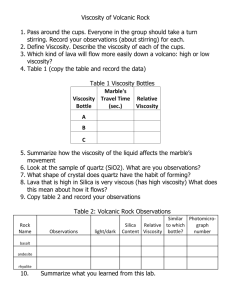
A blood-mimicking fluid for particle image velocimetry with silicone vascular models Majid Y. Yousif 1 David W. Holdsworth2 Tamie L. Poepping3* 1. Biomedical Engineering Graduate Program, The University of Western Ontario, London ON, N6A 3K7 CANADA 2. Robarts Research Institute, The University of Western Ontario, 100 Perth Drive, London ON, N6A 5K8 CANADA 3. Department of Physics and Astronomy, The University of Western Ontario, London ON, N6A 3K7 CANADA *Corresponding author: T.L. Poepping, Phone: +1-519-661-2111 ext 86431, Fax: +1-519-6612033, poepping@uwo.ca ABSTRACT: For accurate particle image velocimetry measurements in hemodynamics studies it is important to use a fluid with a refractive index (n) matching that of the vascular models (phantoms) and ideally a dynamic viscosity matching human blood. In this work, a blood-mimicking fluid (BMF) composed of water, glycerol, and sodium iodide was formulated for a range of refractive indices to match most common silicone elastomers (n=1.40-1.43) and with corresponding dynamic viscosity within the average cited range of healthy human blood (4.4±0.5 cP). Both refractive index and viscosity were attained at room temperature (22.2±0.2°C), which eliminates the need for a temperature-control system. An optimally matched BMF, suitable for use in a vascular phantom (n=1.4140±0.0008, Sylgard 184), was demonstrated with composition (by weight) of 47.38% water, 36.94% glycerol (44:56 glycerol-water ratio), and 15.68% sodium iodide salt, resulting in a dynamic viscosity of 4.31±0.03 cP. KEYWORDS: velocimetry; PIV; blood mimicking fluid; silicone elastomer; refractive index; vascular models; blood flow; Sylgard 184; blood viscosity Introduction Particle image velocimetry (PIV) is an engineering technique used to obtain quantitative flow information. Typically, a flowing fluid is seeded with tiny particles and illuminated with a laser sheet of light, while images are taken in consecutive pairs or series. The images are analyzed to determine the distances traveled by particles, from which velocity vectors are calculated. To use PIV for vascular research, blood vessels can be modeled in transparent phantoms fabricated from different materials, such as glass (refractive index, n=1.47), acrylic (n=1.485-1.492), and silicone (n=1.40−1.44) (Hopkins et al. 2000; Miller et al. 2006; Nguyen et al. 2004; Nishino and Choi 2006; Yip et al. 2004). Silicone is of particular interest due to its versatility, robustness, excellent optical clarity, and ready availability in a two-component liquid form making it easily castable into the required geometry and dimensions with high accuracy. An optimal working fluid for PIV studies should exhibit a refractive index matched accurately to that of the particular phantom material used. As well, for vascular research, a PIV blood-mimicking fluid (BMF) should possess a dynamic viscosity (µ) similar to human blood at normal arterial shear rates, so as to obtain realistic blood-flow modeling. Based on a literature review (Yousif 2009) of recent studies of human blood viscosity, we found an average value from the published viscosity values to be 4.4±0.5 cP (at 37°C) for normal control subjects and moderate large-artery shear rates (Bor-Kucukatay et al. 2008; Carrera et al. 2008; Fehr et al. 2008; Galduroz et al. 2007; Rajzer et al. 2007; Vaya et al. 2008). However, several difficulties arise in finding a PIV BMF with both suitable refractive index and dynamic viscosity. First, the refractive index of the phantom is not always accurately known a priori and can vary (between models or batches) for a given material. Second, the viscosity is typically determined by the same component used to adjust refractive index and thus can’t be adjusted independently. Therefore studies often compromise accurate matching of the viscosity or use suitably scaled models and flow waveforms to achieve hemodynamic similarity. Additionally, it is often desirable to do cross-modality comparison studies (Poepping et al. 2010), thus requiring accurate matching of viscosity across studies; for example, in-vitro ultrasound studies typically use a well-established BMF (Ramnarine et al. 1998; Teirlinck et al. 1997), with dynamic viscosity of 4.1 cP achieved using ~10% (by weight) glycerol in water (to achieve an appropriate acoustic velocity) plus dextran to increase the viscosity further. Finally, since refractive index and viscosity are known to be temperature dependent, it is important to attain both properties at the same working temperature. Unfortunately, a PIV BMF that demonstrates a refractive index matching with silicone and a dynamic viscosity similar to blood, both at the same temperature (and preferably room temperature), is not readily described in the literature. A blood analogue commonly used in the PIV literature is a composition of glycerol and water (Lim et al. 2001; Nguyen et al. 2004; Raz et al. 2007). However, to attain a refractive index ≥1.40 requires at least 40% (by volume) of glycerol, which results in a dynamic viscosity >5.0 cP at 20°C (i.e. >80th percentile of average human blood viscosity), and the higher concentrations needed for larger refractive index will result in even higher viscosity. Another possible fluid, which has been modeled empirically by Nguyen et al. (Nguyen et al. 2004), uses combinations of diethyl phthalate (DEP) and ethanol for a BMF with a wide range of refractive index and viscosity values at different temperatures. The model shows good results for matching the refractive index of various silicone elastomers, but the resulting viscosity values are again lower than human-blood viscosity. For example, the model shows a refractive index of 1.44 for a mixture (by vol.) of 55.6% DEP and 44.4% ethanol, but requires chilling to a temperature of 16.9°C to achieve a kinematic viscosity of >3 cP (3.327 cSt). To obtain refractive indices below 1.44 would thus require lowering the DEP ratio, but this will further decrease the viscosity, as it represents the more viscous component (about 10x that of ethanol) (Nguyen et al. 2004). Furthermore, it requires a temperature-control system for chilling the fluid, with standard room temperatures resulting in even lower viscosities, and a sealed system to avoid rapid evaporation (and resultant cooling). A three-component BMF composed of different relative quantities of water, glycerol and sodium iodide (NaI) has been introduced in the literature, but the described formulations are for use with high refractive-index models fabricated from acrylic (n = 1.485-1.492) or glass (n=1.474) (Fontaine et al. 1996; Grigioni et al. 2001; Kadambi et al. 1990; Morsi et al. 2000; Sankovic et al. 2004; Sastry et al. 2006; Yagi et al. 2006) and thus not directly suitable for silicone elastomers (n = 1.40-1.44). Consequently, the various PIV fluids of previous work mentioned in the literature demonstrate either a match of refractive index with silicone models or a viscosity close to blood, but none demonstrates a simultaneous match of the two properties. Here we introduce a method for formulating a BMF for use at room temperature with a range of refractive indices matching to most commonly used silicone elastomers, while simultaneously exhibiting acceptable dynamic viscosity to mimic human blood. Methods In this work, Sylgard-184 silicone (Dow Corning Corp., Midland, MI, USA) was used to cast anthropomorphic phantoms of vascular models (Fig. 1) for studying hemodynamics at the bifurcation of the common carotid artery. Based on in vivo geometric characterization (Smith et al. 1996), phantoms were manufactured with idealistic artery dimensions, using a lost-material casting technique (Poepping et al. 2004; Poepping et al. 2010; Smith et al. 1999). A flow loop, with temperature-controlled mixing bath and Abbe refractometer (ATAGO NAR-3T, ±0.0001 precision), was used to determine the refractive index of the silicone vascular phantom. An initial solution was prepared with a refractive index around the lower bound of silicone elastomers at 1.40. This fluid was composed (by weight) of 50.21% water, 39.14% glycerol (5350-1, Caledon, Georgetown ON, Canada), and 10.65% NaI salt (7920-1, Caledon). The resulting glycerol-towater ratio of 44:56 was held constant during the experiment. A peristaltic pump was used to circulate the fluid from an in-line mixing container on a magnetic stirrer, through the silicone phantom placed over grid paper, and then an Abbe refractometer (ensuring consistent temperature for subsequent refractive-index measurements) before returning. Sodium iodide salt was accurately weighed and added in regular increments (~0.5% by weight), allowing ~30 minutes for it to completely dissolve between increments, continuing until a formulation was achieved with a refractive index matching to the specific phantom. For each new concentration, images were recorded to monitor the distortion of grid lines (Fig. 2), and the refractive index was precisely measured using the Abbe refractometer. A match in refractive index was visually detected by way of elimination of discernible distortion of the grid lines. All measurements were performed at 22.2±0.2°C. Based on the experimental results for the above refractive-index measurement for the phantom, five fluid samples were prepared with the same initial relative concentration of glycerol-to-water (44:56 by weight) and five different concentrations of NaI in order to achieve a range of refractive index values spanning ~1.40-1.43. For greater flexibility to select the refractive index and dynamic viscosity independently, and considering that viscosity of glycerol (1490 cP at 20°C) is a thousand times higher than that of water (1.002 cP at 20°C) (Weast 1969), a second series with lower viscosity was prepared using a lower glycerol-to-water ratio (40:60 by weight) and again with incremental NaI content to achieve the same range of refractive indices. For each sample in the two series, refractive index was precisely measured using the Abbe refractometer. Kinematic viscosity was measured using a Cannon-Fenske viscometer, and density using a volumetric flask and digital scale. Dynamic viscosity was calculated from the product of kinematic viscosity and density. All measurements of refractive index, kinematic viscosity, and density were repeated five times for each concentration, with mean and standard deviation calculated for each set. All measurements were performed at a temperature of 22.2±0.2°C. Finally, sensitivity to temperature change was investigated for the refractive index and dynamic viscosity, such as might occur between or during experiments. Measurements were made over a range of working temperatures from 20-25°C using a sample fluid composed (by weight) of 47.38% water, 36.94% glycerol (44:56 glycerol-to-water ratio), and 15.68% NaI salt. All data was fit using an N-dimensional regression model (D’Errico 2006) as a linear or secondorder polynomial function, as specified for each fit given in the results. Results Figure 2 demonstrates the visual monitoring of the distortion of underlying grid lines under ambient lighting with different fluids in the phantom. Minor distortion, as demonstrated in Fig. 2B for a fluid refractive index of 1.4112±0.0001, was gradually eliminated with additional NaI until the distortion was no longer visually discernible (Fig. 2C); this remained so for a range of fluid refractive indices from 1.4132 to 1.4148 (i.e. 0.0016 or 0.1%), before distortion was again apparent. Thus the refractive index of the Sylgard-184 phantom was indirectly determined to be 1.4140±0.0008, with uncertainty equivalent to approximately ±0.5% by weight of NaI. The formulation with refractive index of 1.4140±0.0001, corresponding to the centre of the optimal range, was composed of 47.38% water, 36.94% glycerol, and 15.68% NaI salt. The resulting average fluid density was 1.244±0.002 g/mL, and the average dynamic viscosity was 4.31±0.03 cP, which lies within 2.0% of the target range (4.4±0.5 cP) to mimic human blood viscosity. Figure 3 shows the dynamic viscosity as a function of NaI concentration for the two series of fluid samples, corresponding to the two glycerol-to-water ratios. The average refractive index value (from 5 measurements) is noted alongside each corresponding data point. For the upper series, with 44:56 (by weight) glycerol-water, corresponding dynamic viscosity varied from approximately 4.15 to 4.65 cP for NaI concentrations from 7 to 25% (by weight), thus providing a BMF with acceptable viscosity values (±0.5 standard deviation of human blood viscosity) for any material of refractive index between 1.40-1.43. The dynamic viscosity (µ) was best fit to a second-order polynomial function with NaI concentration (x1, % by weight) according to: µ= (6.674x10-4)x12+(7.008x10-3)x1+4.0808 (R2=0.9943) for 44:56 glycerol-water by weight and µ=(1.19x10-3)x12+(1.447x10-2)x1+3.597 (R2=0.9912) for 40:60 glycerol-water by weight. To enable greater extension to other concentrations of NaI and glycerol (x2, % by weight), a 2-D second-order polynomial model is given by: µ=(8.147x10-4)x12+(2.117x10-3)x22+5.127x10-2 (R2=0.9973). It was noted that kinematic viscosity (not shown) was not significantly dependent on NaI concentration and was mainly dependent upon the relative glycerol concentration. The five fluid samples with varying NaI concentration in 44:56 glycerol-water had a kinematic viscosity of about 3.51±0.04 cSt, and the seven with 40:60 glycerol-water had a kinematic viscosity of about 2.96±0.02 cSt. However, the increase in density with increasing NaI concentration, led to the significant increase in dynamic viscosity seen in Fig. 3. Refractive index was found to vary linearly (not shown) with NaI concentration, according to n=(1.680x10-3)x1+1.3877 (R2=0.9981) for 44:56 glycerol-water and n=(1.791x103 )x1+1.3804 (R2=0.9985) for the 40:60 glycerol-water fluid. A linear 2-D regression fit was described by: (1.728x10-3)x1 + (1.326x10-3)x2 + 1.3286 (R2=0.9973). Figure 4 shows the variation of refractive index and dynamic viscosity with temperature, along with the corresponding equations of best fit. Refractive index decreased by 0.0005 (~0.04%) over a 5°C increase in temperature, which is less than the range of uncertainty observed when visually matching the fluid and phantom refractive index (±0.0008). The change in viscosity was more significant, decreasing by 0.75 cP (~17%) over a 5°C increase or 0.3 cP (~7%) for a 2°C increase. Thus for precision better than 10% once the formulation has been optimized for desired refractive index and dynamic viscosity, a temperature-control system should not be needed for room temperature fluctuations less than ±1°C. This BMF has the advantages of being inexpensive (~$20/L), non-volatile, and a low safety risk (either no risk or only mild irritant, non-flammable, and non-reactive according to the components’ Material Safety Data Sheets). One limitation to be noted is that the fluid exhibits a discoloration (yellowing) over time, reportedly caused by the ionization of NaI (releasing of I3- ion) after exposure to air or light for several hours (Narrow et al. 2000). This problem can be treated by easily dissolving 0.1% (by weight) of sodium thiosulphate (Na2S2O3; 8460-1, Caledon) in the BMF to retrieve the original colorless form of the fluid (Narrow et al. 2000). However, phantoms should be rinsed after use to avoid potential staining from the iodide over long-term use or storage. Conclusion A three-component BMF, composed of water, glycerol, and NaI, was characterized for use with castable silicone elastomers of cited refractive index values range from 1.40−1.44 (Hopkins et al. 2000; Miller et al. 2006; Nguyen et al. 2004; Nishino and Choi 2006; Yip et al. 2004). Characterization of the refractive index and viscosity as functions of the glycerol-water ratio and NaI concentration enables the adjustment of the refractive index to accommodate either different silicones, batch-to-batch variance for a given material, or even different types of materials, while maintaining a consistent dynamic viscosity appropriate for modeling blood. Acknowledgements The authors would like to acknowledge Hristo Nikolov for phantom fabrication. Financial support is acknowledged from the Heart and Stroke Foundation of Ontario (grant #T-6427). The Natural Sciences and Engineering Research Council of Canada (TLP), Canadian Institutes of Health Research Training Fellowship in Vascular Research (MYY). References Bor-Kucukatay M, Keskin A, Akdam H, et al. (2008) Effect of thrombocytapheresis on blood rheology in healthy donors: Role of nitric oxide. Transfusion and Apheresis Science 39:101-108 DOI 10.1016/j.transci.2008.07.004 Carrera LI, Etchepare R, D'Arrigo M, et al. (2008) Hemorheologic changes in type 2 diabetic patients with microangiopathic skin lesions. A linear discriminant categorizing analysis. Journal of Diabetes and Its Complications 22:132-136 DOI 10.1016/j.jdiacomp.2007.06.001 D’Errico J. (2006) "Polyfitn" (http://www.mathworks.com/matlabcentral/fileexchange/10065), MATLAB Central File Exchange. Last retrieved July 9, 2010. Fehr M, Galliard-Grigioni KS, Reinhart WH (2008) Influence of acute alcohol exposure on hemorheological parameters and platelet function in vivo and in vitro. Clinical Hemorheology and Microcirculation 39:351-358 DOI 10.3233/ch-2008-1102 Fontaine AA, Ellis JT, Healy TM, Hopmeyer J, Yoganathan AP (1996) Identification of peak stresses in cardiac prostheses - A comparison of two-dimensional versus threedimensional principal stress analyses. ASAIO Journal 42:154-163 Galduroz JCF, Antunes HK, Santos RF (2007) Gender- and age-related variations in blood viscosity in normal volunteers: A study of the effects of extract of Allium sativum and Ginkgo biloba. Phytomedicine 14:447-451 DOI 10.1016/j.phymed.2007.06.002 Grigioni M, Daniele C, D'Avenio G, Barbaro V (2001) The influence of the leaflets' curvature on the flow field in two bileaflet prosthetic heart valves. Journal of Biomechanics 34:613621 Hopkins LM, Kelly JT, Wexler AS, Prasad AK (2000) Particle image velocimetry measurements in complex geometries. Experiments in Fluids 29:91-95 Kadambi JR, Chen RC, Bhunia S, Dybbs AZ, Edwards RV, Rutstein A (1990) Measurement of Solid-Liquid Multiphase Flow Using Refractive-Index Matching Technique. Laser Anemometry / - Advances and Applications:477-487 Lim WL, Chew YT, Chew TC, Low HT (2001) Pulsatile flow studies of a porcine bioprosthetic aortic valve in vitro: PIV measurements and shear-induced blood damage. Journal of Biomechanics 34:1417-1427 Miller P, Danielson K, Moody G, Slifka A, Drexler E, Hertzberg J (2006) Matching index of refraction using a diethyl phthalate/ethanol solution for in vitro cardiovascular models. Experiments in Fluids 41:375-381 DOI 10.1007/s00348-006-0146-5 Morsi YS, Sakhaeimanesh A, Clayton BR (2000) Hydrodynamic evaluation of three artificial aortic valve chambers. Artificial Organs 24:57-63 Narrow TL, Yoda M, Abdel-Khalik SI (2000) A simple model for the refractive index of sodium iodide aqueous solutions. Experiments in Fluids 28:282-283 Nguyen TT, Biadillah Y, Mongrain R, Brunette J, Tardif JC, Bertrand OF (2004) A method for matching the refractive index and kinematic viscosity of a blood analog for flow visualization in hydraulic cardiovascular models. Journal of Biomechanical EngineeringTransactions of the ASME 126:529-535 DOI 10.1115/1.1785812 Nishino K, Choi J-W (2006) Index-Matching PIV for Complex Flow Geometry. In: Kobe, Japan Poepping TL, Nikolov HN, Thorne ML, Holdsworth DW (2004) A thin-walled carotid vessel phantom for doppler ultrasound flow studies. Ultrasound in Medicine and Biology 30:1067-1078 DOI 10.1016/j.ultrasmedbio.2004.06.003 Poepping TL, Rankin RN, Holdsworth DW (2010) Flow patterns in carotid bifurcation models using pulsed Doppler ultrasound: Effect of concentric versus eccentric stenosis. Ultrasound Med Biol (accepted) Rajzer MW, Klocek M, Wojciechowska W, Palka I, Kawecka-Jaszcz KL (2007) Relationship between, blood viscosity, shear stress and arterial stiffness in patients with arterial hypertension. Artery Research 1:65-65 Ramnarine KV, Nassiri DK, Hoskins PR, Lubbers J (1998) Validation of a new bloodmimicking fluid for use in Doppler flow test objects. Ultrasound in Medicine & Biology 24:451-459 Raz S, Einav S, Alemu Y, Bluestein D (2007) DPIV prediction of flow induced platelet activation - Comparison to numerical predictions. Annals of Biomedical Engineering 35:493-504 DOI 10.1007/s10439-007-9257-2 Sankovic JM, Kadambi JR, Mehta M, Smith WA, Wernet MP (2004) PIV investigations of the flow field in the volute of a rotary blood pump. Journal of Fluids EngineeringTransactions of the ASME 126:730-734 DOI 10.1115/1.1789529 Sastry S, Kadambi JR, Sankovic JM, Izraelev V (2006) Study of flow field in an advanced bladeless rotary blood pump using particle image velocimetry. In: Lisbon, Portugal Smith RF, Rutt BK, Fox AJ, Rankin RN, Holdsworth DW (1996) Geometric characterization of stenosed human carotid arteries. Academic Radiology 3:898-911 Smith RF, Rutt BK, Holdsworth DW (1999) Anthropomorphic carotid bifurcation phantom for MRI applications. Journal of Magnetic Resonance Imaging 10:533-544 Teirlinck CJPM, Fish P, Hoskins PR, et al. (1997) Validation of a flow Doppler test object for diagnostic ultrasound scanners. TNO Prevention and Health, Leiden, Vaya A, Murado J, Santaolaria M, et al. (2008) Haemorheological changes in patients with systemic lupus erythematosus do not seem to be related to thrombotic events. Clinical Hemorheology and Microcirculation 38:23-29 Weast RC (1969) Viscosity of liquids. In: Weast RC (ed) CRC Handbook of Chemistry and Physics. 49th edn. CRC Press, Clevelend, Ohio, pp. F37-F42 Yagi T, Yang W, Ishikawa D, Sudo H, Iwasaki K, Umezu M (2006) Multiplane scanning StereoPIV measurements of flow inside a spiral vortex pulsatile blood pump. In: 13th Int Symp on Applications of Laser Techniques to Fluid Mechanics, Lisbon, Portugal Yip R, Mongrain R, Ranga A, Brunette J, Cartier R (2004) Development of Anatomically Correct Mock-Ups of the Aorta for PIV Investigations. In: Inaugural CDEN Design Conference, Montréal, Canada Yousif MY (2009) Developing a blood-mimicking fluid for particle image velocimetry with silicone vascular models. MESc dissertation, University of Western Ontario. Fig. 1: Idealized model (A) and transparent phantom (B) of a common carotid artery (CCA, 8.0 mm ID) as it branches into the external (ECA, 4.62 mm ID) and internal (ICA, 5.52 mm ID) carotid arteries. The model on the left shows a severe stenosis (diseased constriction) of the ICA, whereas the phantom on the right has a normal (disease-free) ICA. Fig. 2: Visual monitoring of the match in refractive index based on distortion of grid lines beneath a phantom filled with (A) air, showing high distortion, (B) nearly matched fluid (n=1.4112±0.0001), still showing minor distortion as indicated by the arrows, and (C) optimally matched fluid (n=1.4140±0.0001) with no distortion, as indicated by the arrows. Note the vertical white markers, denoting the flow lumen, and the unintentional stain at the bifurcation apex, which provides a convenient landmark here. Fig. 3: Dynamic viscosity for two series of fluids with different glycerol-to-water ratios (44:56 for upper curve and 40:60 for lower), as a function of percentage sodium iodide in solution, along with curves and equations of best fit. Corresponding average refractive index (n) values are shown as data labels, enabling inter. Error bars represent standard deviation based on 5 repeated measurements. Fig. 4: Dynamic viscosity (dashed line) and refractive index (solid line) each as a function of temperature for a solution with 44:56 (by wt) glycerol-water ratio and 15.68% (by wt) sodium iodide. Corresponding lines and equations of fit are shown using a second-order polynomial fit for viscosity and a linear fit for refractive index. Error bars represent standard deviation of 5 measurements.